Pregnancy rapid weight gain
Pregnancy and birth: Weight gain in pregnancy - InformedHealth.org
Created: June 17, 2009; Last Update: March 22, 2018; Next update: 2021.
It is important for pregnant women to have a balanced diet, both for themselves and their child. This helps them put on a good amount of weight. But how much weight gain is considered to be “normal” in pregnancy? Can mothers-to-be eat as much as they like? And how can they lose weight again afterwards?
“Don’t worry – the weight will soon drop off when you start breastfeeding!”, “Be careful – I never lost the weight after my second baby”, “Eat anything you want – you’re eating for two!”… As with so many issues surrounding pregnancy, it often seems as though everyone has an opinion about weight gain. With all the contradictory advice going around, it can be hard to know what to do.
Most women can simply trust their own appetite when it comes to eating during pregnancy. They don't need a special diet, and can eat what tastes good to them and what feels right. But it may be a good idea for some women to change their diet and get more exercise, including women who are very overweight, gain weight very quickly, or have gestational diabetes.
How much weight gain is “normal”?
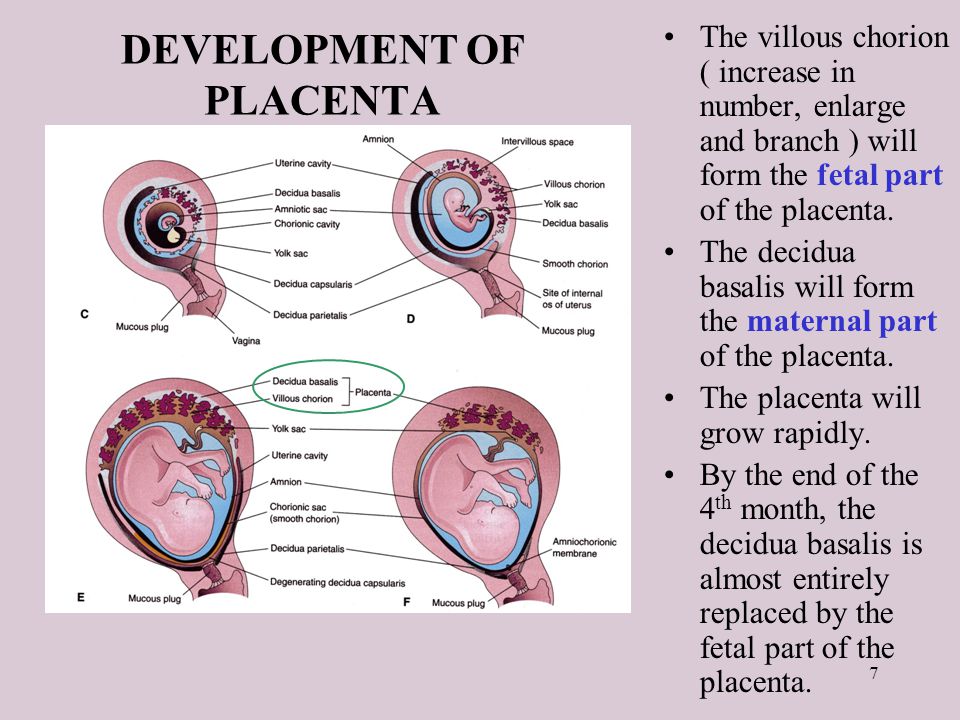
Pregnancy can lead to changes in many of your daily routines and habits, including what you eat and how much exercise you get. But most of all: Women’s bodies change during pregnancy to ensure that their unborn children get enough food and other things that they need. These changes already start happening in early pregnancy, and become more and more noticeable as time goes on. Women gain more weight in the final months of pregnancy than they do in the first few months. This isn't only due to the weight of the growing baby. Much of the weight gained is extra fluid (water) in the body. This is needed for things like the baby’s circulation, the placenta and the amniotic fluid.
Medical guidelines used to be quite strict, with recommendations limiting weight gain to a few kilograms. But there is no standard recommended amount of weight gain that applies to every pregnant woman. The recommendations are now based on women’s pre-pregnancy weight. Petite, underweight women should put on more weight than women who were overweight before they became pregnant.
But there is no standard recommended amount of weight gain that applies to every pregnant woman. The recommendations are now based on women’s pre-pregnancy weight. Petite, underweight women should put on more weight than women who were overweight before they became pregnant.
The body mass index (BMI)
The body mass index (BMI) is the most common way to determine whether people are underweight, overweight or have a normal weight. It measures the relationship between weight and height. A BMI under 18.5 is considered to be underweight, a BMI between 18.5 and 25 is “normal weight,” and a BMI between 25 and 30 is “overweight.” If someone has a BMI over 30 they are considered to be very overweight (obese).
BMI alone is not enough to say whether someone’s weight is likely to cause health problems, though. So being overweight is absolutely fine for many people – unless they develop certain health conditions, such as type 2 diabetes. However, having a BMI above 30 (being obese) increases the risk of related health problems.
Body weight before and during pregnancy
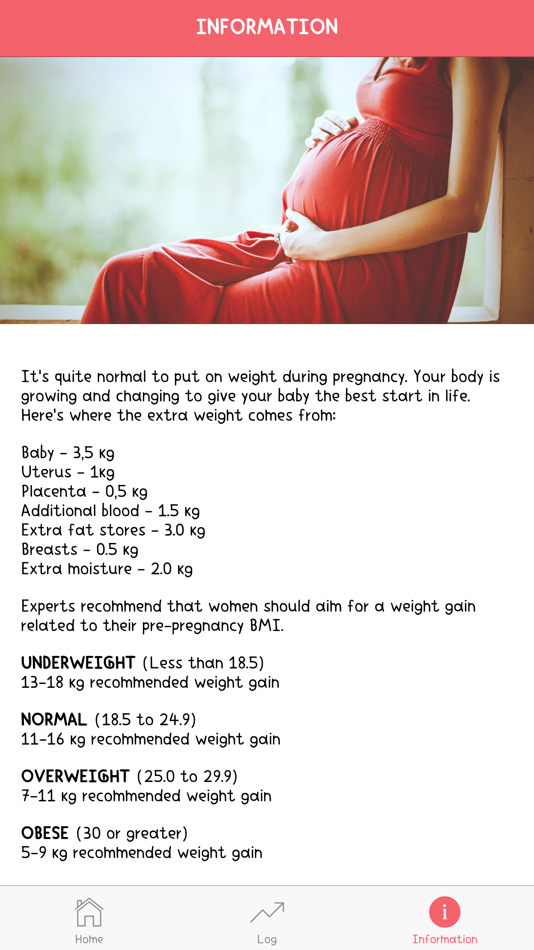
The U.S. Institute of Medicine (IOM) issues guidelines that are followed by doctors around the world. Their recommendations about BMI and weight gain in pregnancy are as follows:
For women who are underweight before pregnancy (BMI of less than 18.5): between 12.5 and 18 kilograms of weight gain during pregnancy.
For women who are of normal weight before pregnancy (BMI of between 18.5 and 24.9): between 11.5 and 16 kilograms of weight gain during pregnancy.
For women who are overweight before pregnancy (BMI of between 25 and 29.9): between 7 and 11.5 kilograms of weight gain during pregnancy.
For women who are obese before pregnancy (BMI greater than 30): between 5 and 9 kilograms of weight gain during pregnancy.
A pregnant woman’s weight alone is not a good indicator of how well her baby is doing – and not even of how fast her baby is growing. That depends on a lot of factors. It is not possible to say for sure how much the baby will weigh at the end of pregnancy. Ultrasound scans and other tests can only give us a rough idea of how the baby is developing and how much he or she might weigh at birth.
It is not possible to say for sure how much the baby will weigh at the end of pregnancy. Ultrasound scans and other tests can only give us a rough idea of how the baby is developing and how much he or she might weigh at birth.
Can putting on too much or too little weight be harmful?
Women who gain a lot of weight in pregnancy have a higher risk of certain health problems and complications during childbirth. For instance, they are more likely to have a very big child with a birth weight of over 4,000 g or 4,500 g (macrosomia), and are more likely to need a Cesarean section.
They are also more likely to have difficulties losing the extra weight after giving birth.
On the other hand, if a woman doesn't gain enough weight and doesn’t get enough different foods in pregnancy, it can harm her growing baby: babies are then often born too early (preterm birth) or often weigh too little at birth.
Very fast weight gain as a sign of health problems
If a woman puts on weight very suddenly, or if she generally gains more than half a kilogram per week, her weight will be monitored by a doctor or midwife. Additional tests and examinations might be needed too.
Additional tests and examinations might be needed too.
Very fast and extreme weight gain (such as 1 kilogram within a week) can be a sign of health problems such as pre-eclampsia. The main symptom of this pregnancy-related condition is high blood pressure, sometimes accompanied by nausea, headaches and dizziness too. Pre-eclampsia can be life-threatening for both the mother and her child, and it needs to be treated by a doctor as soon as possible.
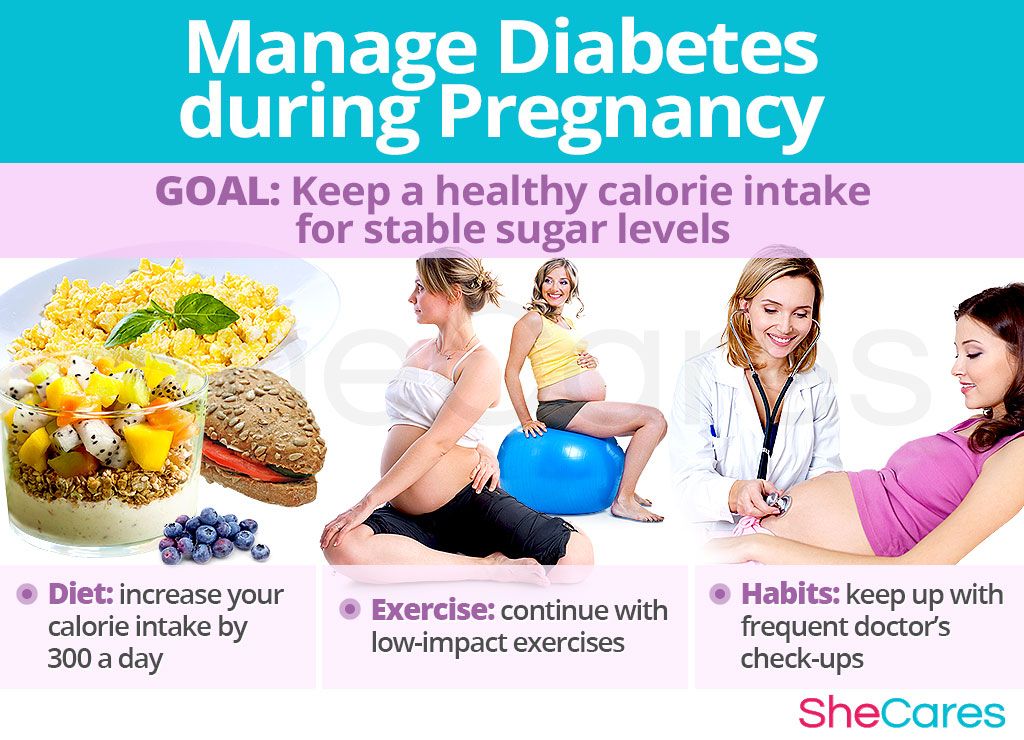
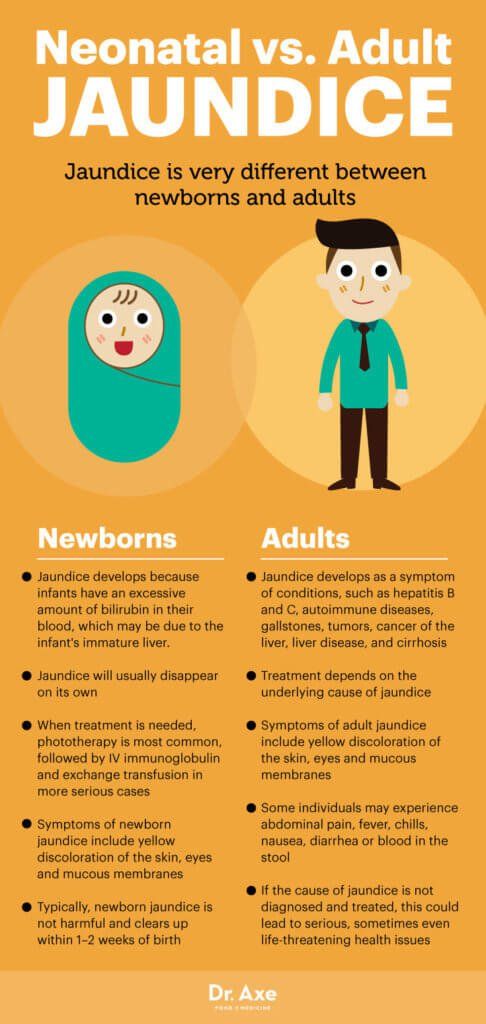
Putting on a lot of weight in pregnancy can increase the risk of women developing diabetes in pregnancy (“gestational diabetes”) – or it can be a sign that they have developed it. Gestational diabetes is where blood sugar levels increase in women who didn't have diabetes before becoming pregnant. Gestational diabetes increases the risk of pre-eclampsia, and can result in the unborn baby putting on a lot of weight. Having a very big and heavy baby can delay the birth and make it more difficult for the woman to give birth to her child naturally (“spontaneously”).
Does avoiding too much weight gain have any advantages?
Paying special attention to diet and getting more exercise during pregnancy may lower certain health risks. This will depend on several factors, including whether the woman is overweight or has gestational diabetes. Research hasn't shown any advantages for women who have a normal weight.
But women who are very overweight (BMI of over 30) can lower their risk of gestational diabetes by changing their diet and getting more exercise. Previous studies haven't shown that this will lower the risk of complications during childbirth or prevent the need for a Cesarean section, though.
Women with gestational diabetes are advised to change their diet in order to lower their blood sugar levels. That can lower the risk of complications during childbirth.
Dietary changes and exercise during pregnancy
Because carbohydrates increase blood sugar levels, women who are very overweight or have gestational diabetes are usually advised to cut down on carbohydrates (“carbs”) while making sure that they still get enough fiber, and to generally eat a balanced diet otherwise. Other common advice includes eating three not-too-big main meals and two to three smaller meals per day.
Other common advice includes eating three not-too-big main meals and two to three smaller meals per day.
The exact dietary changes to be made will depend on things like how much the woman weighs and how much exercise she gets. Getting special advice from a nutritional therapist can help to avoid adverse effects. Pregnant women need to make sure that they get enough calories and important nutrients, which is why they shouldn’t go on a low-calorie diet, for instance.
Doing at least 30 minutes of a strenuous physical activity on about three to four days per week is often enough. Suitable types of exercise include swimming, cycling and brisk walking. Women with a greater risk of preterm birth are usually advised to avoid sports altogether. When in doubt, don't hesitate to ask a gynecologist.
How can underweight pregnant women gain enough weight?
If a woman who is underweight becomes pregnant and finds it difficult to put on weight, she can seek advice from her doctor or midwife.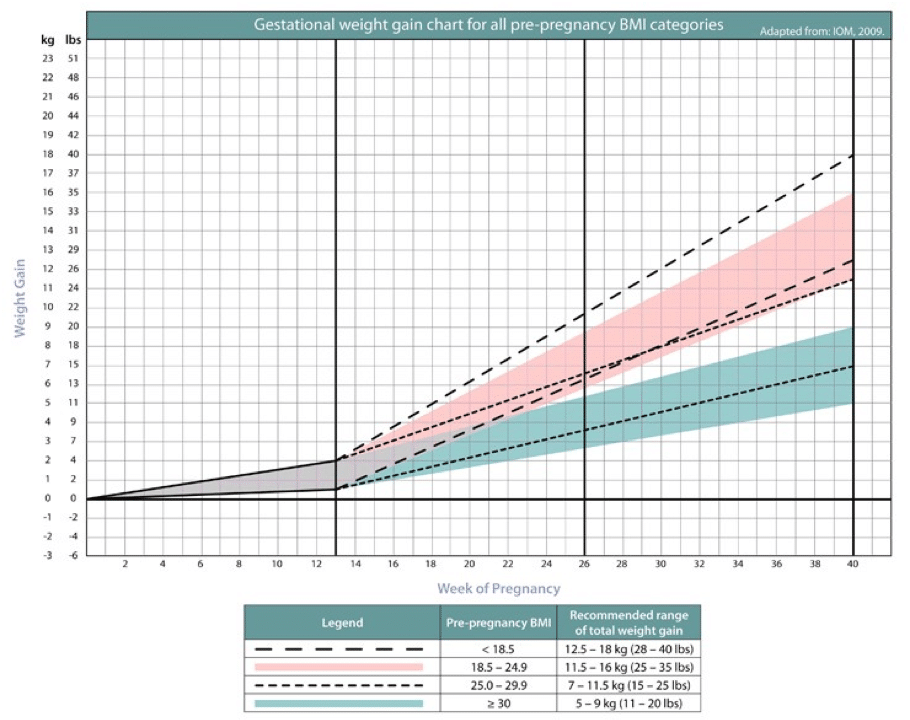 Studies suggest that professional dietary advice can help women gain weight and lower the risk of giving birth too early (preterm birth).
Studies suggest that professional dietary advice can help women gain weight and lower the risk of giving birth too early (preterm birth).
Protein supplements have been found to help some underweight women increase their weight. This lowers the risk of their child being born underweight, as well as reducing the risk of having a miscarriage. However, very protein-rich dietary supplements with a protein content of more than 25% don't appear to help. Research also suggests that these very high-protein products might limit the growth of the baby. So it's important to make sure you get a balanced mix of nutrients. “More” is not “better” in this case.
Does watching your weight prevent stretch marks?
There is no clear answer to this question yet. Although there are many claims about what causes stretch marks and what might help, none of them have been confirmed in good-quality research.
Whether or not women get stretch marks not only depends on how much weight they gain in total. Factors like how fast they gain weight can make a difference too. For instance, gaining a lot of weight very suddenly can cause more stretch marks than gaining weight gradually. But it's not clear whether stretch marks can be prevented by keeping your weight down.
Factors like how fast they gain weight can make a difference too. For instance, gaining a lot of weight very suddenly can cause more stretch marks than gaining weight gradually. But it's not clear whether stretch marks can be prevented by keeping your weight down.
Losing weight after having a baby
Many mothers find that it takes a while before they reach their pre-pregnancy weight again. For some women, breastfeeding and taking care of a baby are enough to melt away the weight gained during pregnancy: It's as though they really need this stored up energy to help get through the first few weeks and months of motherhood.
But most women won't really get close to their pre-pregnancy weight until perhaps six months after giving birth. Women who don't lose weight, or even gain weight instead, might have a higher risk of health problems. These problems could get worse in other pregnancies.
The best way to lose weight is by combining a change in diet with extra physical exercise.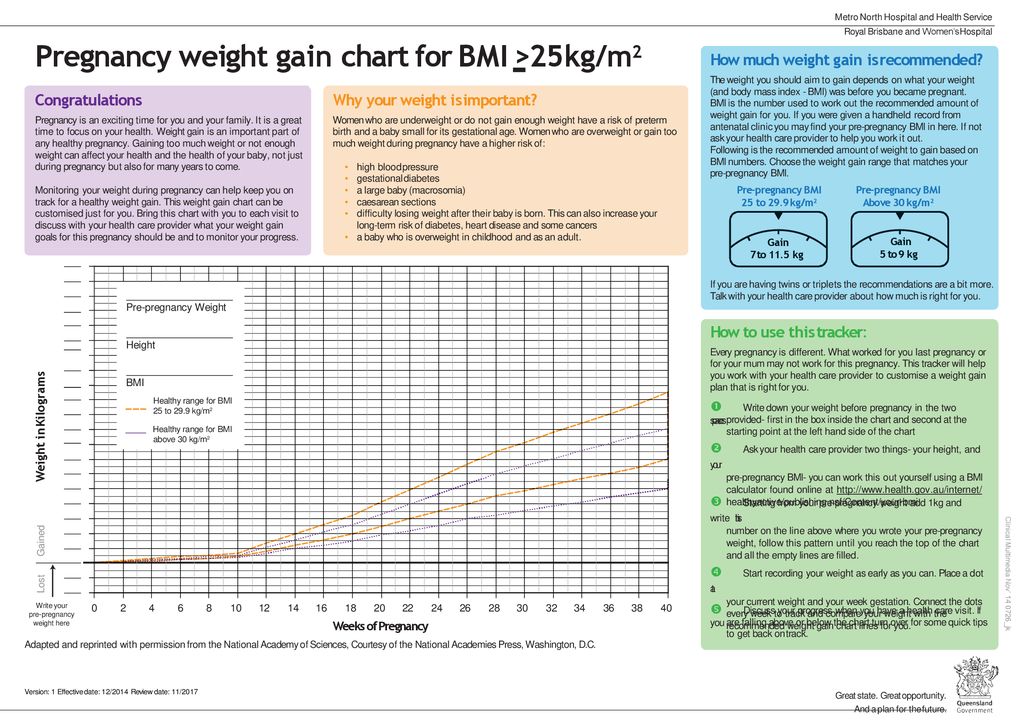 Exercise alone probably won't do much. Programs to help people change their eating and lifestyle habits are often used to try to lose weight. In the research on these programs, women started weight control efforts a month or two after giving birth, and sometimes later. Immediately after birth, mothers need enough nutrients to breastfeed their child, so it is not a good time for them to try to lose weight.
Exercise alone probably won't do much. Programs to help people change their eating and lifestyle habits are often used to try to lose weight. In the research on these programs, women started weight control efforts a month or two after giving birth, and sometimes later. Immediately after birth, mothers need enough nutrients to breastfeed their child, so it is not a good time for them to try to lose weight.
Too much, or too sudden, weight loss can have disadvantages too. For instance, if you go on a diet that is too strict or too one-sided after having a baby, it could reduce the quantity of your breast milk or the nutrients it contains.
How do women feel about their weight in pregnancy and afterwards?
Women are constantly surrounded by (nearly always digitally edited) photos of models with supposedly “ideal” bodies. Pregnant women are confronted with these photos too. This makes it difficult for many of them to be happy with their figure, and it can damage their self-image and enjoyment of their body. The media add to the pressure on pregnant women and mothers by focusing a lot of attention on how quickly celebrities return to their pre-pregnancy figures. But women need to gain weight during pregnancy – and they can't expect to lose it all again within a few weeks after giving birth.
The media add to the pressure on pregnant women and mothers by focusing a lot of attention on how quickly celebrities return to their pre-pregnancy figures. But women need to gain weight during pregnancy – and they can't expect to lose it all again within a few weeks after giving birth.
A lot of women see pregnancy as a time to simply enjoy their belly, curves and the baby growing inside their body – and allow themselves some “time off” from worrying about their size. That can be one of the really pleasant parts of being pregnant.
It could only become a problem if you get too far out of your normal weight range and change your eating habits too much. Then it might be harder to get back to your healthier “pre-baby” weight and lifestyle. Women who don't become very overweight when they are pregnant will probably find it easier to get back to normal afterwards. But you don't have to be thin to be happy and healthy, and have a healthy baby.
Sources
Amorim Adegboye AR, Linne YM.
 Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev 2013; (7): CD005627. [PMC free article: PMC9392837] [PubMed: 23881656]
Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev 2013; (7): CD005627. [PMC free article: PMC9392837] [PubMed: 23881656]Berger AA, Peragallo-Urrutia R, Nicholson WK. Systematic review of the effect of individual and combined nutrition and exercise interventions on weight, adiposity and metabolic outcomes after delivery: evidence for developing behavioral guidelines for post-partum weight control. BMC Pregnancy Childbirth 2014; 14: 319. [PMC free article: PMC4176850] [PubMed: 25208549]
Elliott-Sale KJ, Barnett CT, Sale C. Exercise interventions for weight management during pregnancy and up to 1 year postpartum among normal weight, overweight and obese women: a systematic review and meta-analysis. Br J Sports Med 2015; 49(20): 1336-1342. [PubMed: 25406335]
International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials.
 BMJ 2017; 358: j3119. [PMC free article: PMC6887834] [PubMed: 28724518]
BMJ 2017; 358: j3119. [PMC free article: PMC6887834] [PubMed: 28724518]Lim S, O'Reilly S, Behrens H, Skinner T, Ellis I, Dunbar JA. Effective strategies for weight loss in post-partum women: a systematic review and meta-analysis. Obes Rev 2015; 16(11): 972-987. [PubMed: 26313354]
Magro-Malosso ER, Saccone G, Di Mascio D, Di Tommaso M, Berghella V. Exercise during pregnancy and risk of preterm birth in overweight and obese women: a systematic review and meta-analysis of randomized controlled trials. Acta Obstet Gynecol Scand 2017; 96(3): 263-273. [PubMed: 28029178]
Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst Rev 2015; (6): CD007145. [PMC free article: PMC9428894] [PubMed: 26068707]
Nascimento SL, Pudwell J, Surita FG, Adamo KB, Smith GN. The effect of physical exercise strategies on weight loss in postpartum women: a systematic review and meta-analysis.
 Int J Obes 2014; 38(5): 626-635. [PubMed: 24048142]
Int J Obes 2014; 38(5): 626-635. [PubMed: 24048142]O'Brien CM, Grivell RM, Dodd JM. Systematic review of antenatal dietary and lifestyle interventions in women with a normal body mass index. Acta Obstet Gynecol Scand 2016; 95(3): 259-269. [PubMed: 26610169]
Ota E, Hori H, Mori R, Tobe-Gai R, Farrar D. Antenatal dietary education and supplementation to increase energy and protein intake. Cochrane Database Syst Rev 2015; (6): CD000032. [PubMed: 26031211]
Rogozinska E, Marlin N, Jackson L, Rayanagoudar G, Ruifrok AE, Dodds J et al. Effects of antenatal diet and physical activity on maternal and fetal outcomes: individual patient data meta-analysis and health economic evaluation. Health Technol Assess 2017; 21(41): 1-158. [PMC free article: PMC5572115] [PubMed: 28795682]
Thangaratinam S, Rogozinska E, Jolly K, Glinkowski S, Duda W, Borowiack E et al. Interventions to reduce or prevent obesity in pregnant women: a systematic review.
 Health Technol Assess 2012; 16(31): iii-iv, 1-191. [PMC free article: PMC4781281] [PubMed: 22814301]
Health Technol Assess 2012; 16(31): iii-iv, 1-191. [PMC free article: PMC4781281] [PubMed: 22814301]Wiles R. The views of women of above average weight about appropriate weight gain in pregnancy. Midwifery 1998; 14(4): 254-260. [PubMed: 10076321]
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Second trimester weight gain? That's probably normal!
Home / Preg-U / Science / Research / Gaining Weight “Too Fast” in your 2nd trimester? That’s Probably Normal.
At my 24-week appointment when I was pregnant with my first, I finally felt pretty good, happily ensconced in the “best” trimester. My nausea had faded, my energy was back, and I was working out again after a two-month hiatus.
Then came the weigh-in.
According to my doctor, I had gained “too much weight” in the last month. I was shocked. Up until then, my trajectory predicted a healthy 30 pound gain. But now, she explained, I was projected to gain 40 lbs. Five pounds over the recommended 25-35 lbs.
The lecture began – “Eat only half the sandwich. Don’t eat for two.”
Okay, I’ll confess, at that point, I stopped listening, and started wondering: Does this even make sense?
Is gaining weight in pregnancy really supposed to be constant? The same amount week after week, month after month – as she and her nifty weight gain chart seem to assume?
Should weight gain be consistent throughout pregnancy?
The answer? Of course not.
The good folks at the Institutes of Medicine (IOM) who came up the current weight gain guidelines for pregnant women agree:
“The pattern of Gestational Weight Gain is most commonly described as sigmoidal, with mean weight gains higher in the second than the third trimester across BMI categories, except for obese women”
– IOM 2009 report on pregnancy weight gain, pg. 101.
Unfortunately, the IOM explained this in such obscure researcher-speak that the message may have gotten lost.
In plain English: pregnant women usually gain more weight in their second trimesters than in their third.
Yup, that’s right. A higher second trimester weight gain is normal. You are not doing something wrong. You are not destined to put on too much weight by the end of pregnancy.
A higher second trimester weight gain is normal. You are not doing something wrong.
Go ahead and eat your whole darn sandwich.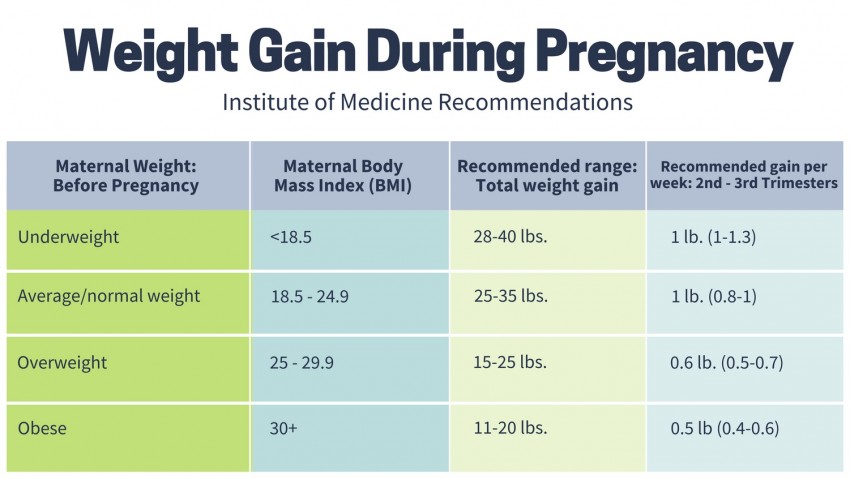
Why do women gain the most weight in their second trimester?
For one, you add a ton of water weight in the second trimester. Did you notice that around month 5 you are suddenly constantly, unquenchable thirst, despite downing what feels like a gallon of water every day? It’s not all in your head, it’s biology.
In your second trimester, your belly swells up with a couple extra pounds of amniotic fluid and a rapidly growing uterus. Welcome to the world, bump! At the same time, your blood volume soars by nearly 50%.
Once you’re past your second trimester, weight gain usually slows down. (Unless you are lucky enough to have full body swelling, which can add an additional seven pounds of water weight in your arms and legs. Isn’t pregnancy fun!)
In your second trimester, your belly swells up with a couple extra pounds of amniotic fluid and a rapidly growing uterus. Welcome to the world, bump!
I do not mean to dismiss the real risks of gaining too much in pregnancy, especially for women who start out pregnancy with a high BMI. Women who go over the IOM guidelines (see below) are at higher risk for C-sections, for large babies with a risk of getting stuck on their way out (ouch!), and for difficulty losing weight postpartum.
Women who go over the IOM guidelines (see below) are at higher risk for C-sections, for large babies with a risk of getting stuck on their way out (ouch!), and for difficulty losing weight postpartum.
Very rapid weight gain (more than 2 lbs in a week) can signal preeclampsia, a serious and dangerous condition involving high blood pressure and protein in your urine. If you notice you a sudden jump in weight in a short period of time, definitely talk to your doctor.
When it comes to second trimester weight gain, keep this in mind:
Weight gain in one week of pregnancy does not predict weight gain in the next week.
So, for the majority of us without specific risk factors, let’s put this “trajectory” idea to rest?
Weight gain in pregnancy is not a steady climb. It’s not meant to be. And gaining a lot during your second trimester weight gain—that’s perfectly normal.
Enjoy your sandwich.
Looking for a perfect week-by-week nutrition guide? Check out our Baby Building Blocks Newsletter! It’s the what, when, why and how of prenatal nutrition.
This article was originally posted on expectingscience.com
YOUR PREGNANCY SMARTS. Delivered.
Sign up for the Preg U Newsletter!
Weight during pregnancy. What increase is considered optimal?
Why is excessive weight gain during pregnancy particularly harmful? What should be the calorie content of the diet? How to build your diet in order to eat varied (and tasty), but at the same time not gain too much? Let's figure it out.
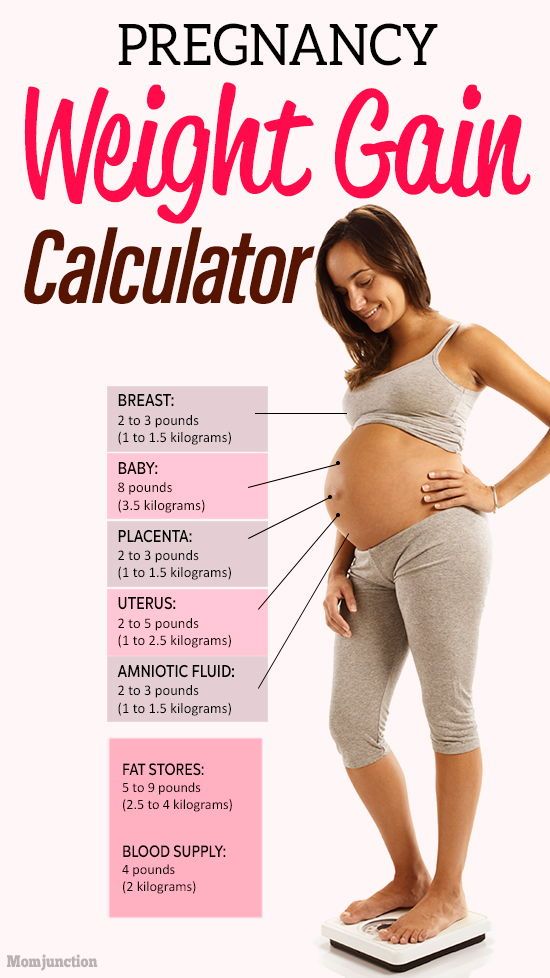
What makes up weight gain during pregnancy?
An increase in the subcutaneous fat layer during pregnancy is a normal and natural process.
While the baby is growing inside you, he needs energy and external protection. But during pregnancy, weight increases not only and not so much due to the adipose tissue of the mother: there is more fluid in the body, the uterus grows, the fetus and placenta develop, and the breasts increase in preparation for the feeding process.
Interestingly, weight loss during the period of toxicosis can later provoke its increase: the body will try to regain what was lost.
Expectant mothers especially actively gain weight in the second trimester and the beginning of the third, but closer to childbirth, a pregnant woman can even lose 1-2 kilograms.
As long as the weight increases more or less evenly and does not go beyond the upper limit of the norm, there is nothing to worry about. But if your weight is rapidly going up, you should be wary.
How to correctly calculate the weight, and what increase is considered optimal?
In Russian obstetric practice, it is generally accepted that the total gain should not exceed 12 kg. for the entire pregnancy. Of these 12 kg. 5-6 accounts for the fetus, placenta, amniotic fluid, another 1.5-2 - for an increase in the uterus and mammary glands, and only 3-3.5 - for the fat mass of a woman.
But this is a general indicator, a kind of "average temperature in the hospital. " The optimal increase is calculated individually and depends on the initial weight of the pregnant woman, her age, the number of fetuses and the size of the child (children), physical activity.
" The optimal increase is calculated individually and depends on the initial weight of the pregnant woman, her age, the number of fetuses and the size of the child (children), physical activity.
WHO recommends that optimal weight gain be calculated based on Body Mass Index (BMI).
It is determined by the formula: body weight (kg) / height squared (m).
| BMI | Recommended weight gain |
|---|---|
| 19.8-26 (normal body weight) | 12.5-15 kg |
| 26.1-29 (overweight) | 11.5 - 14 kg |
| over 29 (obese) | 7-9 kg |
How to calculate the optimal weight gain?
To do this, use the following chart:
- Calculate your BMI: divide your initial weight in kg. for height in meters squared.
For example, your "pre-pregnancy" weight was 60 kg with a height of 170 cm.
BMI = 60: (170 x 170) = 20.76.
- A BMI of less than 18.5 indicates underweight. Indicators from 18.5 to 25 are within the norm, from 25 to 30 are above the norm, and a figure greater than 30 indicates obesity.
- Now that you know your BMI, find the optimal weekly increase in the table and compare it with yours.
| Week of pregnancy | Underweight before pregnancy (BMI less than 18.5) | Normal pre-pregnancy weight (BMI 18.5 to 24.9) | Overweight before pregnancy (BMI over 30) |
|---|---|---|---|
| 4 | 0-0.9 kg | 0-0.7 kg | 0-0.5 kg |
| 6 | 0-1.4 kg | 0-1 kg | 0-0.6 kg |
| 8 | 0-1.6 kg | 0-1.2 kg | 0-0.7 kg |
| 10 | 0-1.8 kg | 0-1.3 kg | 0-0.8 kg |
| 12 | 0-2 kg | 0-1. 5 kg 5 kg | 0-1 kg |
| 14 | 0.5-2.7 kg | 0.5-2 kg | 0.5-1.2 kg |
| 16 | up to 3.6 kg | up to 3 kg | up to 1.4 kg |
| 18 | up to 4.6 kg | up to 4 kg | up to 2.3 kg |
| 20 | up to 6 kg | up to 5.9 kg | up to 2.9 kg |
| 22 | up to 7.2 kg | up to 7 kg | up to 3.4 kg |
| 24 | up to 8.6 kg | up to 8.5 kg | up to 3.9 kg |
| 26 | up to 10 kg | up to 10 kg | up to 5 kg |
| 28 | up to 13 kg | up to 11 kg | up to 5.4 kg |
| 30 | up to 14 kg | up to 12 kg | up to 5.9 kg |
| 32 | up to 15 kg | up to 13 kg | up to 6. 4 kg 4 kg |
| 34 | up to 16 kg | up to 14 kg | up to 7.3 kg |
| 36 | up to 17 kg | up to 15 kg | up to 7.9 kg |
| 38 | up to 18 kg | up to 16 kg | up to 8.6 kg |
| 40 | up to 18 kg | up to 16 kg | up to 9.1 kg |
Recently, doctors are increasingly talking about an individual approach and urge not to panic if the increase is slightly beyond the normal range. When assessing the state of health of a pregnant woman, the doctor focuses not only on weight, but also takes into account the results of tests and examinations and other important indicators.
Why is excessive weight gain dangerous?
Gaining extra pounds can lead to gestational diabetes, hypertension, preeclampsia, or cause a caesarean section.
In addition, excessive weight gain during pregnancy may increase the risk of obesity and associated cardiovascular disease.
What can I do to keep my weight within normal limits during pregnancy?
First of all, consult a nutritionist. If there is no such doctor in the antenatal clinic, it makes sense to contact a specialist on a commercial basis. He will develop an individual diet, which will contain all the useful elements, and will offer to keep a food diary. It will also tell you how to eat right and weigh yourself.
To prevent excessive weight gain during pregnancy, it is enough to follow simple rules of a healthy diet:
- Eat often and in small portions;
- Always keep a “healthy snack” on hand: fresh apple wedges, unsweetened crackers, dried fruit, or sugar-free yogurt;
- Refuse soda, chips, sausages and sausages;
- Minimize sweets;
- Avoid fast food;
- Limit the use of condiments, especially salt, which retains water in the body;
- Choose steamed dishes;
- Eat more fiber-rich foods such as whole grain bread, bran, vegetables;
The diet of a pregnant woman should be varied. Include grains, vegetables, fruits, dairy products, meat and fish, legumes, or nuts.
Include grains, vegetables, fruits, dairy products, meat and fish, legumes, or nuts.
It must be remembered that expectant mothers should never starve and adhere to extreme diets.
How many calories per day do you need during pregnancy?
It is difficult to calculate the energy value per day on your own, and then strictly adhere to a certain number of calories, and it is not necessary, unless it is recommended by a nutritionist or endocrinologist. On average, you can aim for 2000-2500 calories per day, but it is important to understand that the need for calories depends on many factors: age, initial weight, health status and level of physical activity.
When should I be on the alert?
Strictly speaking, it is better for a pregnant woman not to worry and entrust her condition to a doctor who will control the development of pregnancy, analyzes and monitor weight. It is important to take tests to determine the level of fasting blood glucose once a trimester.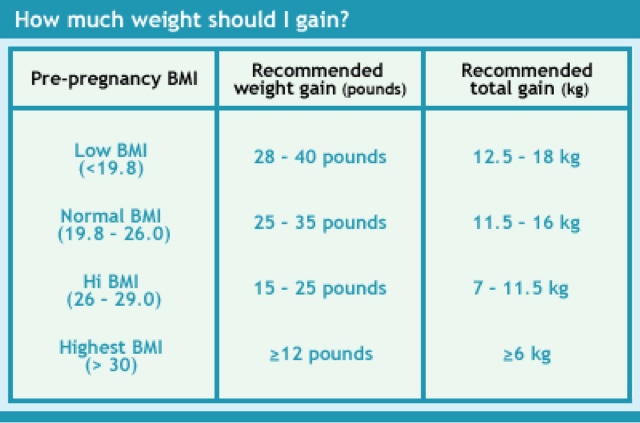 The appearance of glucosuria, an increase in fasting blood glucose (more than 5.5 mmol / l) or an hour after a meal (more than 7.7 mmol / l) indicate the possible development of "diabetes in pregnancy", in connection with which the doctor will prescribe appropriate treatment . In addition, a sharp increase in body weight can cause preeclampsia.
The appearance of glucosuria, an increase in fasting blood glucose (more than 5.5 mmol / l) or an hour after a meal (more than 7.7 mmol / l) indicate the possible development of "diabetes in pregnancy", in connection with which the doctor will prescribe appropriate treatment . In addition, a sharp increase in body weight can cause preeclampsia.
These and other diseases can be dangerous, which is why you need to carefully monitor the body weight during the gestation period, but remember that pregnancy is not the time for strict diets.
When using any materials from the site nutriclub.ru, a link to the site is required.
© Nutriclub, 2020
You will also be interested
- Nutriclub - healthy nutrition and child development
- Pregnancy
- Mom's health and well-being
- weight during pregnancy.
 What increase is considered optimal? - Nutriclub
What increase is considered optimal? - Nutriclub
Weight category - articles from the specialists of the clinic "Mother and Child"
— What norms of weight gain during pregnancy are doctors guided by today?
- The average increase for all nine months is from 9 to 14 kg. The exact figure depends on many factors, but a sharp deviation in one direction or the other from the norm should be alarming. To calculate the allowable increase, the initial weight of the expectant mother should be taken into account: for example, women of a fragile physique (asthenic type) must gain more than initially obese women. In addition, it is important to consider the trimester of pregnancy.
— How does weight change in different trimesters?
- Weight gain throughout pregnancy is uneven: at the very beginning it is almost imperceptible, increases significantly towards the middle and may begin to decrease two weeks before delivery. In the first trimester, both weight gain and weight loss are considered normal. On average, during this period, the expectant mother is gaining from 1.5 to 2.5 kg. In the second trimester, the baby begins to grow actively and the numbers will be different: about 500 g per week for thin women, no more than 450 g for pregnant women with normal weight and no more than 300 g for full ones. In the third trimester, the weight of the expectant mother should not increase by more than 300 g per week.
In the first trimester, both weight gain and weight loss are considered normal. On average, during this period, the expectant mother is gaining from 1.5 to 2.5 kg. In the second trimester, the baby begins to grow actively and the numbers will be different: about 500 g per week for thin women, no more than 450 g for pregnant women with normal weight and no more than 300 g for full ones. In the third trimester, the weight of the expectant mother should not increase by more than 300 g per week.
— Why do pregnant women gain weight?
- Contrary to popular belief, weight gain is not only due to the mass of a growing baby and body fat - they make up about half of the total figure. For nine months, a woman's uterus increases, the volume of circulating blood and intercellular fluid increases, amniotic fluid and the placenta form.
— Why is excess weight dangerous?
- Rapid weight gain is common in multiple pregnancies, underweight women and too young mothers whose bodies are still developing. Often it is the result of normal overeating and requires adjustment of the diet. Diets and fasting days (especially the so-called "hungry") during the period of bearing a child are strictly prohibited even if the pregnant woman is overweight. It is very important to ensure that the baby receives all the nutrients, vitamins and trace elements, so you just need to balance your diet accordingly.
Often it is the result of normal overeating and requires adjustment of the diet. Diets and fasting days (especially the so-called "hungry") during the period of bearing a child are strictly prohibited even if the pregnant woman is overweight. It is very important to ensure that the baby receives all the nutrients, vitamins and trace elements, so you just need to balance your diet accordingly.
Excess weight may occur due to fluid retention, which manifests itself in the form of edema. By the way, this is especially true for working pregnant women: sedentary work provokes stagnation of fluid in the lower extremities and pathological weight gain. In this case, wearing compression stockings, leg exercises and regular walking is recommended.
— Is slow weight gain dangerous, on the contrary?
- Some expectant mothers gain the first kilograms only after the 14th week - usually for petite women who do not have a genetic predisposition to be overweight or women suffering from toxicosis.