Percent of newborns with jaundice
Jaundice | Conditions | UCSF Benioff Children's Hospitals
- Overview
- Types of jaundice
- Signs & symptoms
- Diagnosis
- Treatment
- Where to get care
- Recommended reading
- Support services
Overview
Jaundice is a common condition in newborns, affecting 50 percent to 60 percent of full-term babies and 80 percent of those born prematurely. It can give babies' skin and the whites of their eyes a yellowish tint.
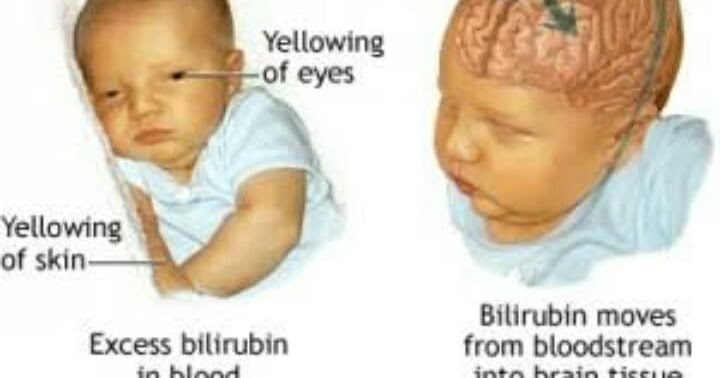
Jaundice is caused by excess levels of bilirubin, which is a yellow pigment produced when old red blood cells break down. Normally, bilirubin passes through the liver and is excreted as bile through the intestines. However, when a newborn's immature liver can't process bilirubin fast enough, it can build up in the blood, making the baby's skin turn a yellowish color.
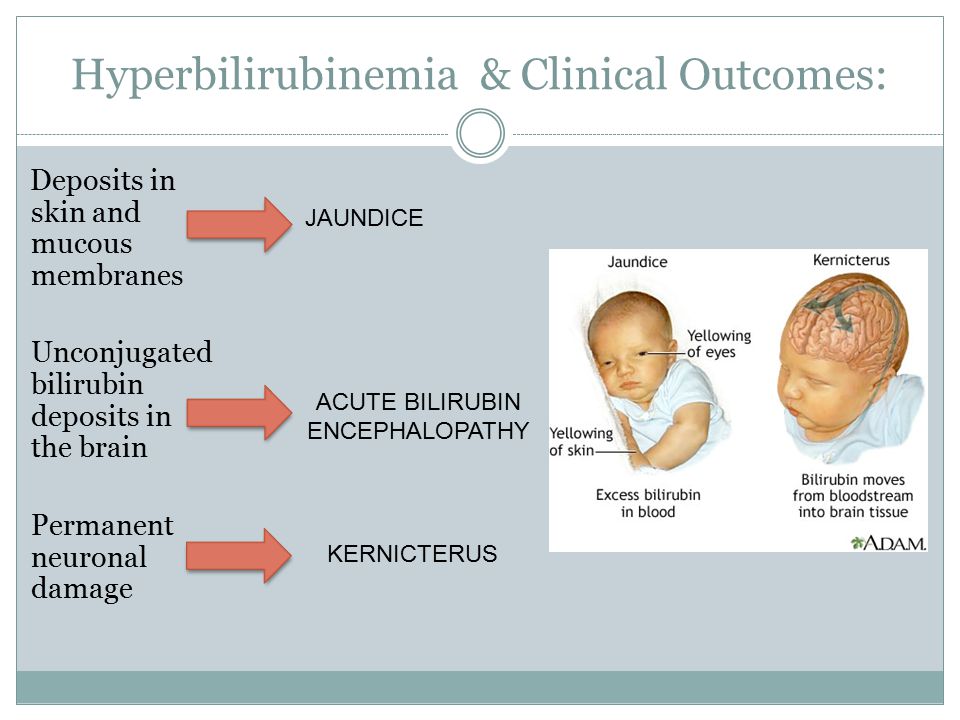
In most babies, jaundice goes away on its own or with mild treatment. However, in some cases when a baby has very high levels of bilirubin, close monitoring and treatment in the Intensive Care Nursery may be needed. If jaundice isn't treated appropriately, babies may experience permanent damage to their nervous system, called kernicterus. Kernicterus is a rare condition that can cause deafness, delayed development or a form of cerebral palsy.
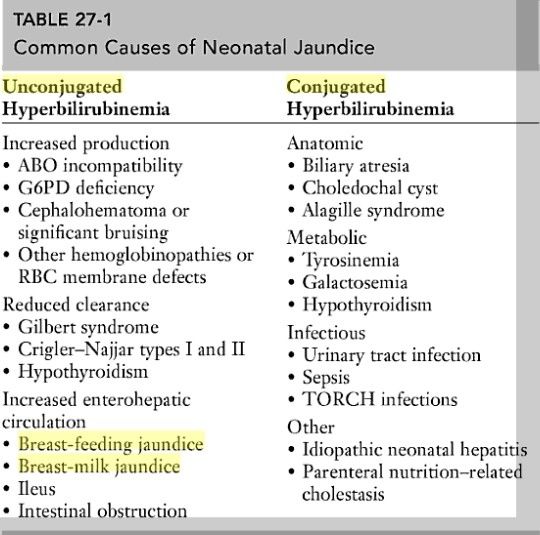
Types of jaundice
There are several types of newborn jaundice. The following are the most common:
- Physiological jaundice — This type of jaundice affects 50 to 60 percent of full-term newborns in their first week, typically three to five days after birth. It occurs when a baby's liver can't sufficiently process bilirubin. Typically this condition disappears within one to two weeks. Because their livers are less mature, premature babies are more likely to have this form of jaundice.
- Blood group incompatibility jaundice — In some cases when a baby and mother have different blood types, the mother produces antibodies that destroy her infant's red blood cells. As a result, bilirubin builds up in the baby's blood.
 This condition may be diagnosed before birth or the first day after birth. In some cases, it can be avoided by treating the mother with a drug that will prevent her from forming antibodies against her baby.
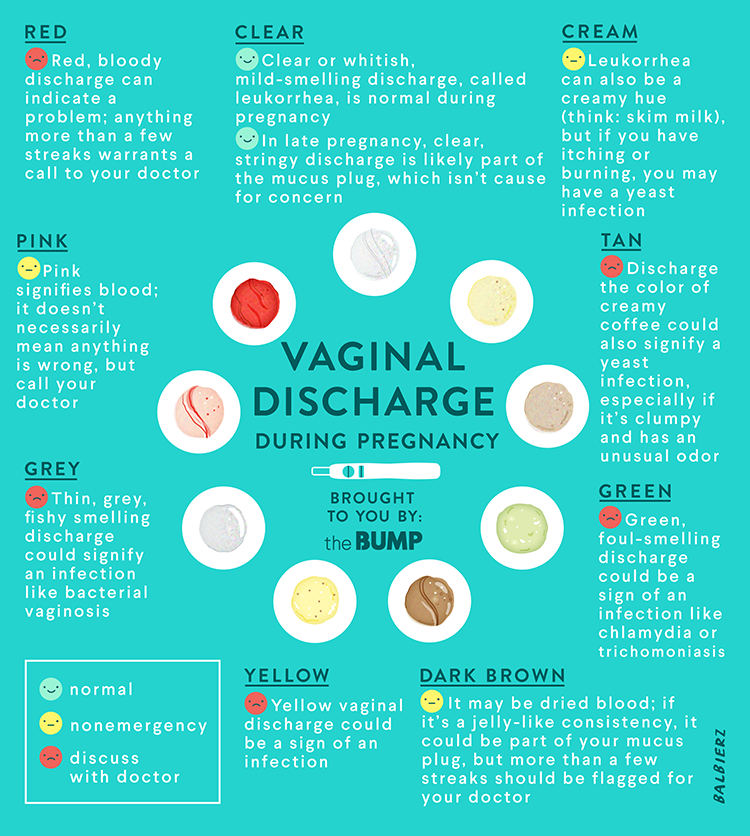
This condition may be diagnosed before birth or the first day after birth. In some cases, it can be avoided by treating the mother with a drug that will prevent her from forming antibodies against her baby. - Breast milk jaundice — A very small number of breastfed babies, roughly one to two percent, develop jaundice because of substances in their mother's breast milk that cause their bilirubin levels to rise.
Signs & symptoms
Although not always obvious, the hallmark symptom of jaundice is a yellowish tint to a baby's skin and the whites of the eyes. Jaundice usually appears two to three days after birth. The yellowish tint typically affects the baby's face first, then the chest and stomach and ultimately the legs. Jaundice may also occur with infection or with certain disorders of the gastrointestinal tract.
Because jaundice can develop in your baby after discharge from the hospital, parents are advised to check their baby's skin tone for a yellowish tint in natural or fluorescent lighting.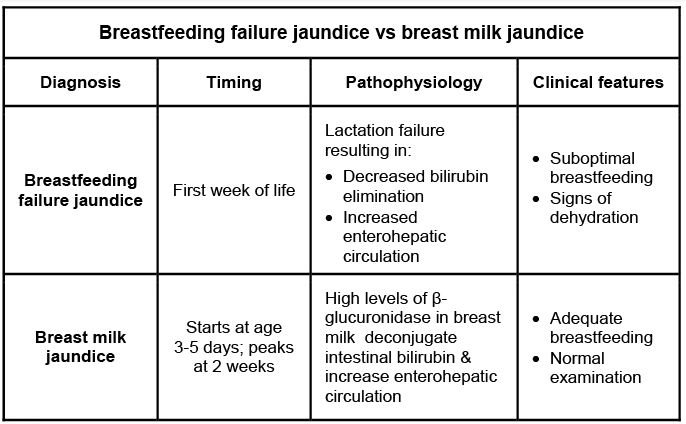 A simple test for jaundice is to press your fingertip to your baby's nose or forehead. If the pressed skin has a yellowish tint, then your baby may have jaundice and you should call your doctor immediately.
A simple test for jaundice is to press your fingertip to your baby's nose or forehead. If the pressed skin has a yellowish tint, then your baby may have jaundice and you should call your doctor immediately.
Diagnosis
In addition to a complete physical examination to check for signs of jaundice, the doctor may also do a blood test to measure the level of bilirubin in your baby's blood. If your baby does have jaundice, the condition and your baby's treatment options will be explained to you before any therapy is started.
Treatment
Mild or moderate forms of jaundice will usually go away without specific treatment after five to seven days, as the baby's liver becomes more mature. In babies with higher levels of bilirubin, close monitoring — and possibly treatment — is needed.
Light therapy, also called phototherapy, is the usual treatment for jaundice. Phototherapy chemically breaks down the bilirubin in your baby's skin to non-toxic forms. During this treatment, your baby is placed under special white or blue light for one to two days.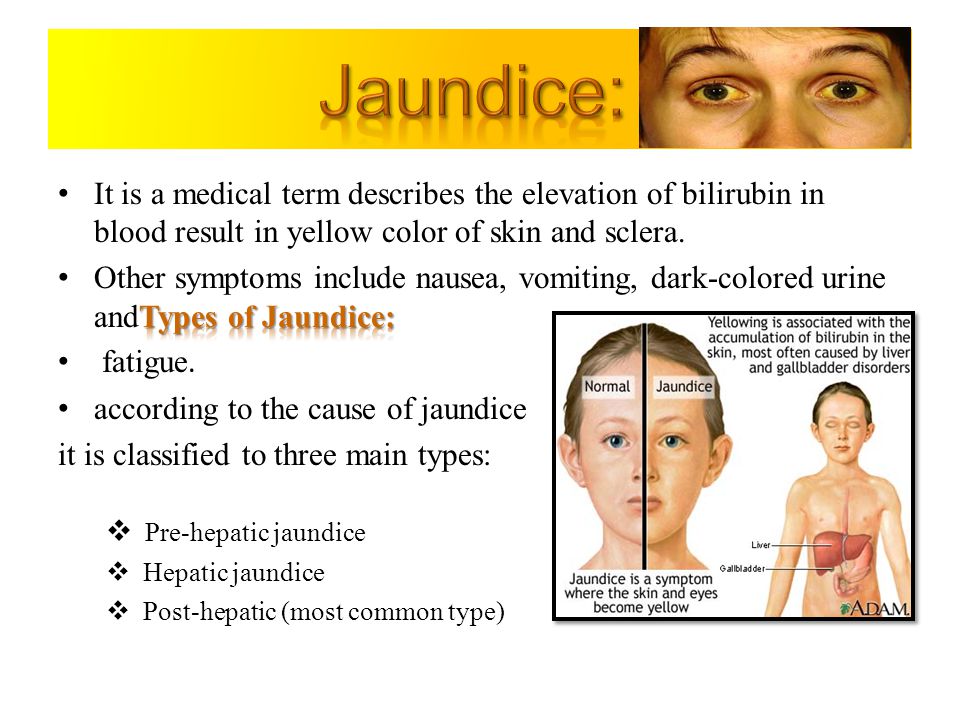 Their eyes will be covered to protect them from the bright lights.
Their eyes will be covered to protect them from the bright lights.
If phototherapy isn't effective, and your baby's bilirubin levels continue to increase, a procedure known as an exchange transfusion may be necessary. During an exchange transfusion, the infant's blood is gradually removed and replaced with donor blood. This procedure removes bilirubin and lowers the bilirubin to safer, non-toxic levels.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.
Where to get care (1)
2
San Francisco / Oakland
Recommended reading
Intensive Care Nursery Glossary
Our glossary explains the terms we use in the intensive care nursery in language that's easy to understand. Learn about chest tubes, respirators and more.
Learn about chest tubes, respirators and more.
Intensive Care Nursery Parents' Guide
Is your baby in the intensive care nursery? Our guide helps you take an active role in your child's care, know what to expect and access support services.
Family Amenities
Family-friendly amenities help you relax and take care of yourself while staying close to your child. We offer lounges, kitchens, showers, breastfeeding rooms and more.
Glogau Teddy Bear Rescue Fund
Families that need additional assistance during their child's hospital stay have access to toys, hotel vouchers and other amenities. Find out more.
Interpreter Services & Communication Assistance
Interpreter services in many languages and TDDs are available for families that need help communicating with care teams. Here's how to access them.
Social Services
Social workers ease the effect of illness, injury and hospitalization on your family with counseling and assistance to help you navigate the challenges.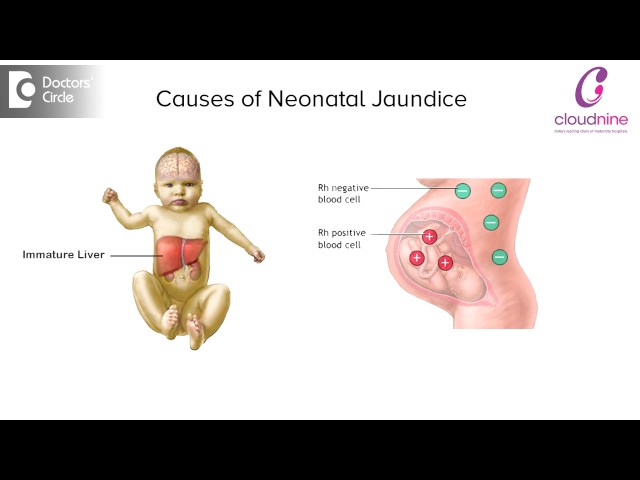
Awards & recognition
Saving future lives
500+ UCSF investigators are researching cures for hundreds of childhood and adult diseases.
Jaundiced Newborn
Is this your child's symptom?
- Jaundice (yellow skin) in a baby during the first 3 months of life (90 days)
- The skin turns a yellow color from high bilirubin levels in the blood
Jaundice and Bilirubin
- Jaundice means the skin has turned yellow.
- Bilirubin is the pigment that turns the skin yellow.
- Bilirubin comes from the normal breakdown of old red blood cells.
- The liver normally gets rid of bilirubin. But, at birth, the liver may be immature.
- Half of babies have some jaundice. Usually it is mild.
- The level of bilirubin that is harmful is around 20. Reaching a level this high is rare.
- High levels need to be treated with bili-lights. That's why your doctor checks your baby's bilirubin levels until it becomes low.

Causes of Jaundice in Newborns
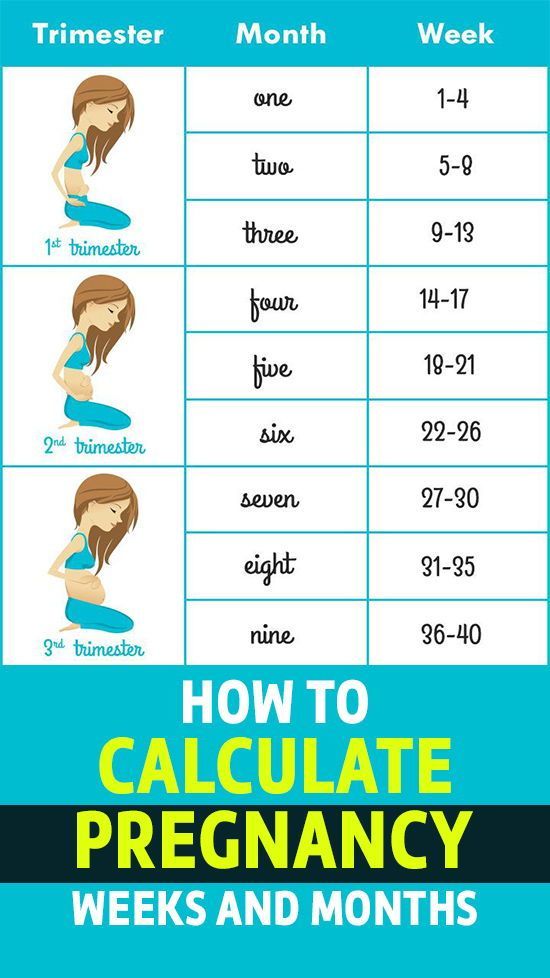
Physiological Jaundice (50% of newborns)
- Onset 2 to 3 days of age
- Peaks day 4 to 5, then improves
- Disappears 1 to 2 weeks of age
Breastfeeding or Malnutrition Jaundice (
5 to 10% of newborns)- Due to inadequate intake of breastmilk
- Onset pattern similar to physiological type
- Also, causes poor weight gain
- Needs close follow-up and weight checks
Breastmilk Jaundice (10% of newborns)
- Due to substance in breastmilk which blocks removal of bilirubin
- Breastmilk intake and weight gain are normal
- Onset 4 to 7 days of age
- Lasts 3 to 12 weeks
- Not harmful
Rh and ABO Blood Group Incompatibility (Serious, but Rare)
- Onset during first 24 hours of life
- Can reach harmful levels
Liver Disease (Serious, but Rare)
- The main clue is light gray or pale yellow stools
- The jaundice doesn't go away
- Causes include liver infection (hepatitis) and liver blockage (biliary atresia)
When to Call for Jaundiced Newborn
Call 911 Now
- Can't wake up
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Dehydration suspected.
 No urine in more than 8 hours, dark urine, very dry mouth and no tears.
No urine in more than 8 hours, dark urine, very dry mouth and no tears. - Fever. Caution: do NOT give your baby any fever medicine before being seen.
- Low temperature below 96.8° F (36.0° C) rectally that does not go up with warming
- Jaundice began during the first 24 hours of life
- Skin looks deep yellow or orange
- Jaundice has reached the legs
- Jaundice worse than when last seen
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- High-risk baby for severe jaundice. Risk factors are: premature baby born at 36 weeks or less, ABO or Rh blood group problem, sib needed bili-lights, bleeding in the scalp, Asian race, breastfeeding problems.
- Whites of the eyes have turned yellow
- Jaundice spreads to stomach (belly)
- You are worried about the amount of jaundice
- You are worried your baby is not getting enough breastmilk
- Yellow, seedy stools are less than 3 per day.
 Exception: breastfed and before 5 days of life.
Exception: breastfed and before 5 days of life. - Day 2-4 of life and no stool in more than 24 hours and breastfed
- Wet diapers are less than 6 per day. Exception: 3 wet diapers per day can be normal before 5 days of life if breastfed.
- 4 or more days old and has not been checked since discharge
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Color gets deeper yellow after 7 days old
- Jaundice is not gone after 14 days of age
- Jaundice began or comes back after 7 days of age
- Stools are white, pale yellow or gray
- You have other questions or concerns
Self Care at Home
- Mild jaundice of newborn
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice for Mild Jaundice
- What You Should Know About Newborn Jaundice:
- Some jaundice is present in 50% of newborns.
- It lasts a short time and will go away. Most often, it is harmless.
- The first place for jaundice to start is on the face.
- Jaundice that is only of the face is always harmless.
- Here is some care advice that should help.
- Some jaundice is present in 50% of newborns.
- Bottle Feed More Often:
- If bottle fed, increase how often you feed your baby.
- Try to feed every 2 to 3 hours during the day.
- Don't let your baby sleep more than 4 hours at night without a feeding.
- Breastfeed More Often:
- If breastfed, increase how often your feed your baby.
- Nurse your baby every 1½ to 2 hours during the day.
- Don't let your baby sleep more than 4 hours at night without a feeding.
- Goal: At least 10 feedings every 24 hours.
- Infrequent Stools Means Your Baby Needs More Milk:
- Breastmilk and formula help carry bilirubin out of the body. Therefore, good feedings are important for bringing down the bilirubin level.

- In the first month, keep track of how many stools are passed daily. The number of stools reflects how much milk your baby is getting.
- If your baby is 5 days or older, he should have at least 3 stools daily. If stooling less than that, it usually means your baby needs more to eat.
- Try to increase the number and amount of feedings per day.
- If you are having any trouble with breastfeeding, consult a lactation expert. Also, schedule a weight check.
- Breastmilk and formula help carry bilirubin out of the body. Therefore, good feedings are important for bringing down the bilirubin level.
- What to Expect:
- Physiological jaundice peaks on day 4 or 5.
- It slowly goes away over 1-2 weeks.
- Judging Jaundice:
- Jaundice starts on the face and moves downward. Try to determine where it stops.
- View your baby unclothed in natural light near a window.
- Press on the skin with a finger to remove the normal skin tone.
- Then try to look if the skin is yellow before the pink color returns.
- Move down the body, doing the same.
 Try to look where the yellow color stops.
Try to look where the yellow color stops. - Jaundice that only involves the face is harmless. As it involves the chest, the level is going up. If it involves the eyes, stomach, arms or legs, the bilirubin level needs to be checked.
- Call Your Doctor If:
- Jaundice gets worse
- Whites of the eyes turn yellow
- Belly or legs turn yellow
- Feeds poorly or has a weak suck
- Baby starts to look or act abnormal
- Jaundice lasts more than 14 days
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 03/06/2023
Last Revised: 12/30/2022
Copyright 2000-2023. Schmitt Pediatric Guidelines LLC.
The norm of bilirubin in newborns - the answer of a pediatrician
What is bilirubin?
Slightly more than half of newborns become noticeably icteric in the first week of life.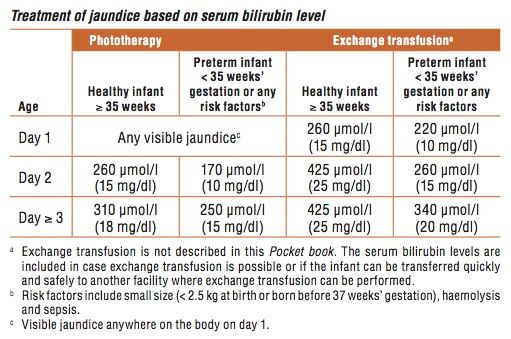 This baby jaundice usually goes away in 2-4 weeks. What causes jaundice in children? Jaundice is a yellowing of the skin and whites of the eyes caused by hyperbilirubinemia - that is, an increase in the concentration of bilirubin in the blood serum.
This baby jaundice usually goes away in 2-4 weeks. What causes jaundice in children? Jaundice is a yellowing of the skin and whites of the eyes caused by hyperbilirubinemia - that is, an increase in the concentration of bilirubin in the blood serum.
Bilirubin is a yellow-orange natural pigment that is released during the natural breakdown of red blood cells - erythrocytes: as a result of the breakdown of hemoglobin to unconjugated bilirubin. The liver rids the blood of excess bilirubin by filtering it and converting it from the free form (unconjugated) to the bound form (conjugated with glucuronic acid), which enters the bile and digestive tract, leaving with the feces, giving it its characteristic color.
Why can the level of bilirubin in the blood rise?
If the level of bilirubin in the blood is higher than normal, this may be due to:
- Red blood cells are destroyed faster than usual.
- The liver does not have time to cope with the disposal of red blood cell waste.

- There is an obstruction in the way in which processed bilirubin is excreted from the liver to the gastrointestinal tract via the biliary tract.
Is neonatal jaundice dangerous?
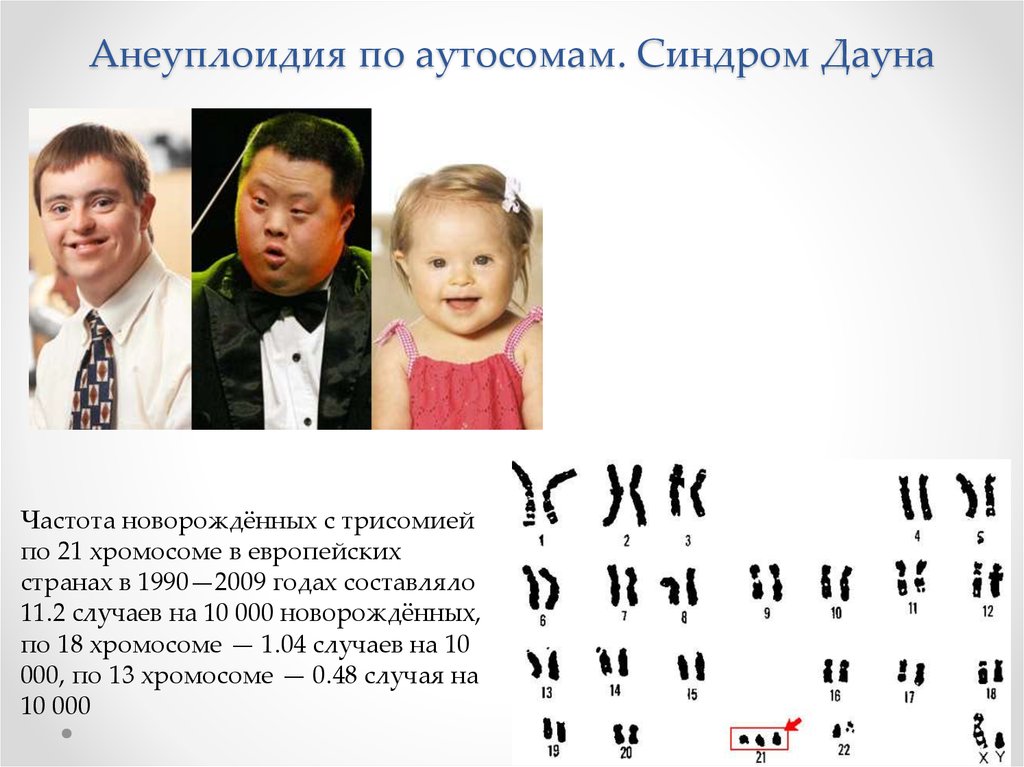
Neonatal jaundice is common among healthy newborns, and in most cases is physiological. In adults and a small proportion of newborns, jaundice is pathological, that is, it means the presence of a disorder that causes it. Some of the more common causes of neonatal jaundice include:
Physiological:
- Physiological hyperbilirubinemia.
- Breastfeeding jaundice.
- Jaundice of breast milk.
Pathological:
- Hyperbilirubinemia due to hemolytic disease.
- Liver dysfunction (eg, caused by parenteral nutrition causing cholestasis, neonatal sepsis, neonatal hepatitis).
Physiological hyperbilirubinemia occurs in almost all newborns. The shorter lifespan of red blood cells in newborns increases the production of bilirubin, and the low level of bacterial microflora in the intestine (which converts bilirubin into an insoluble form),
The shorter lifespan of red blood cells in newborns increases the production of bilirubin, and the low level of bacterial microflora in the intestine (which converts bilirubin into an insoluble form),
in combination with increased hydrolysis of conjugated bilirubin increase enterohepatic circulation, as a result of which the liver cannot cope with excess incoming bilirubin. As a result, bilirubin levels may rise to 308 µmol/L by day 3-4 of life (by day 7 in Asian infants) and then decline.
Breastfeeding jaundice develops in one sixth of infants during the first week of life. Breastfeeding increases the circulation of bilirubin from the intestines to the liver in some children who do not consume enough milk and who are dehydrated and malnourished.
Breastmilk jaundice is different from breastfeeding jaundice. It develops after the first 5-7 days of life and peaks after about 2 weeks. It is believed to be caused by an increased concentration of beta-glucuronidase in the mother's breast milk, which causes an increase in the conversion of insoluble bilirubin back into a soluble (unconjugated) form and its reabsorption in the large intestine.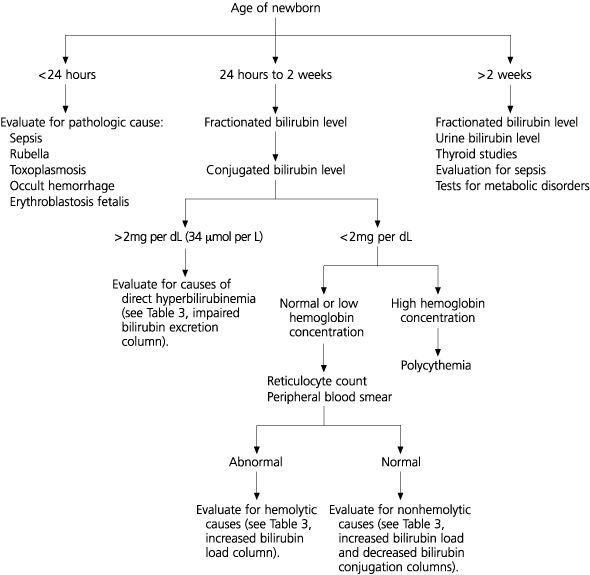
Phototherapy - treatment of jaundice at home.
Special blue light lamps (photo-illuminators) are used for neonatal phototherapy. Treatment takes several days, the duration of therapy is determined by the pediatrician. Photoisomerization of bilirubin occurs in the skin, so the more area of the body used for phototherapy, the more effective the treatment process. The lamp is a bath made of harmless plastic, in the base of which blue light lamps are mounted.
We have prepared an article about phototherapy, as well as information on where to rent the device in St. Petersburg: Phototherapy at home - treatment of jaundice
Pathological jaundice in newborns may be caused by:
- immune and non-immune hemolytic anemia
- resorption (resorption) of hematoma
- sepsis
- hypothyroidism
How to distinguish physiological from pathological jaundice?
Jaundice that develops in the first 24-48 hours of life or persists for longer than 2 weeks is most likely pathological.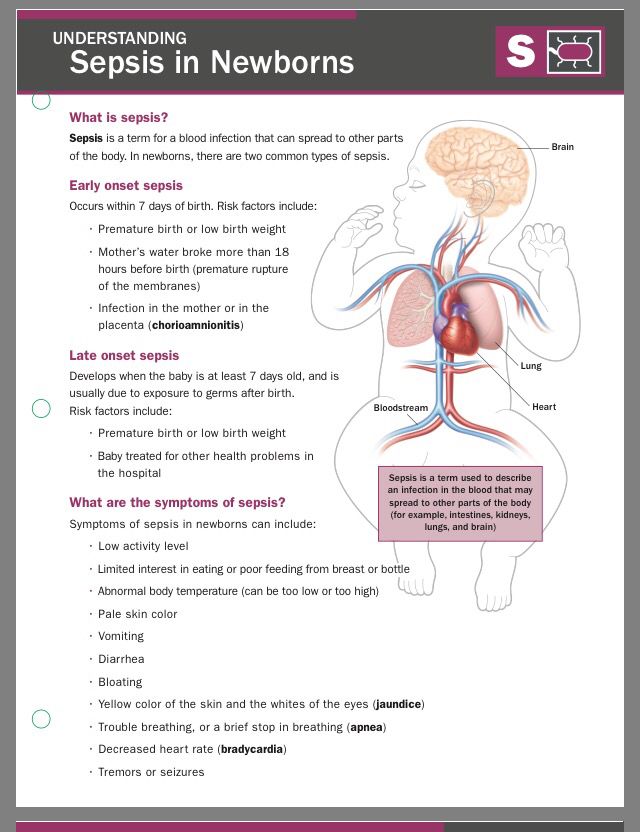
Jaundice that does not appear until 2–3 days of age is most likely physiological.
An exception is pathological jaundice in Crigler-Najjar syndrome, hypothyroidism, or drug exposure, which also occurs after 2-3 days. In this case, the concentration of bilirubin peaks in the first week, rising at a rate of up to 86 µmol/l per day, and may persist for a long period.
Diagnosis of jaundice in children
The diagnosis of hyperbilirubinemia is suspected by the color of the skin and whites of the infant's eyes and is confirmed by measurement of serum bilirubin.
The serum bilirubin level required to cause jaundice varies by skin tone and area of the body, but jaundice usually becomes visible on the whites of the eyes at levels of 34 to 51 µmol/L, and on the face of about 68 to 86 µmol/l. As the level of bilirubin increases, jaundice progresses from the head to the legs, appearing in the navel at about 258 µmol/l, and on the legs at 340 µmol/l.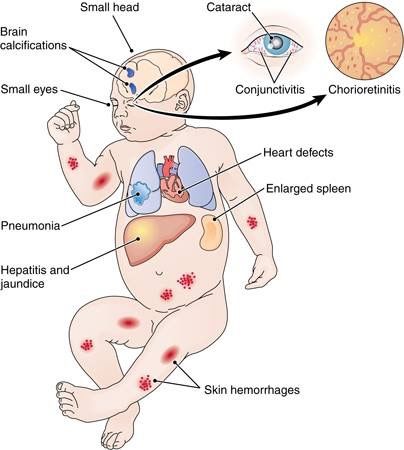
Bilirubin concentration > 170 µmol/l in preterm infants or > 308 µmol/l in term infants requires additional tests for hematocrit, blood smear, reticulocyte count, direct Coombs test, total serum bilirubin and serum direct bilirubin concentration, blood group matching and Rh factor of the baby and mother.
Is physiological jaundice dangerous in babies?
Although the increase in bilirubin in physiological jaundice is not caused by disease and resolves with time, hyperbilirubinemia is neurotoxic, meaning it causes nerve cell damage in the baby. For example, a high concentration of bilirubin in the blood can cause acute encephalopathy, accompanied by a variety of neurological disorders, including cerebral palsy and sensorimotor disorders. An even more severe consequence of the neurotoxicity of an increased concentration of bilirubin may be kernicterus, caused by the deposition of free (unconjugated) bilirubin in the basal ganglia and nuclei of the brain stem.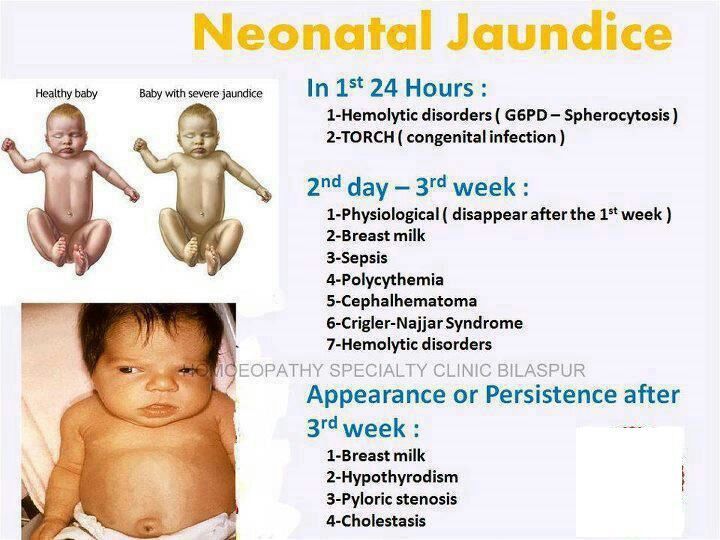 Normally, serum albumin-bound bilirubin remains in the intravascular space, but it can sometimes cross the blood-brain barrier:
Normally, serum albumin-bound bilirubin remains in the intravascular space, but it can sometimes cross the blood-brain barrier:
- High serum bilirubin (acute or chronic).
- With a decrease in the concentration of serum albumin (for example, in premature babies).
- When bilirubin is displaced from albumin by competitive binders (drugs:
- sulfisoxazole, ceftriaxone, aspirin) or free fatty acids and hydrogen ions (eg, in malnourished and starving children).
Infants born less than 35 weeks' gestation have lower threshold levels of bilirubin for treatment because preterm infants are at greater risk of neurotoxicity.
How to lower bilirubin in children?
Treatment of jaundice is aimed at both the cause of the elevated bilirubin concentration and the elimination of the hyperbilirubinemia itself.
Physiological jaundice usually resolves within 1-2 weeks. The use of frequent formula feeding may reduce the incidence and severity of hyperbilirubinemia by increasing GI motility and stool frequency, thereby minimizing enterohepatic circulation of bilirubin.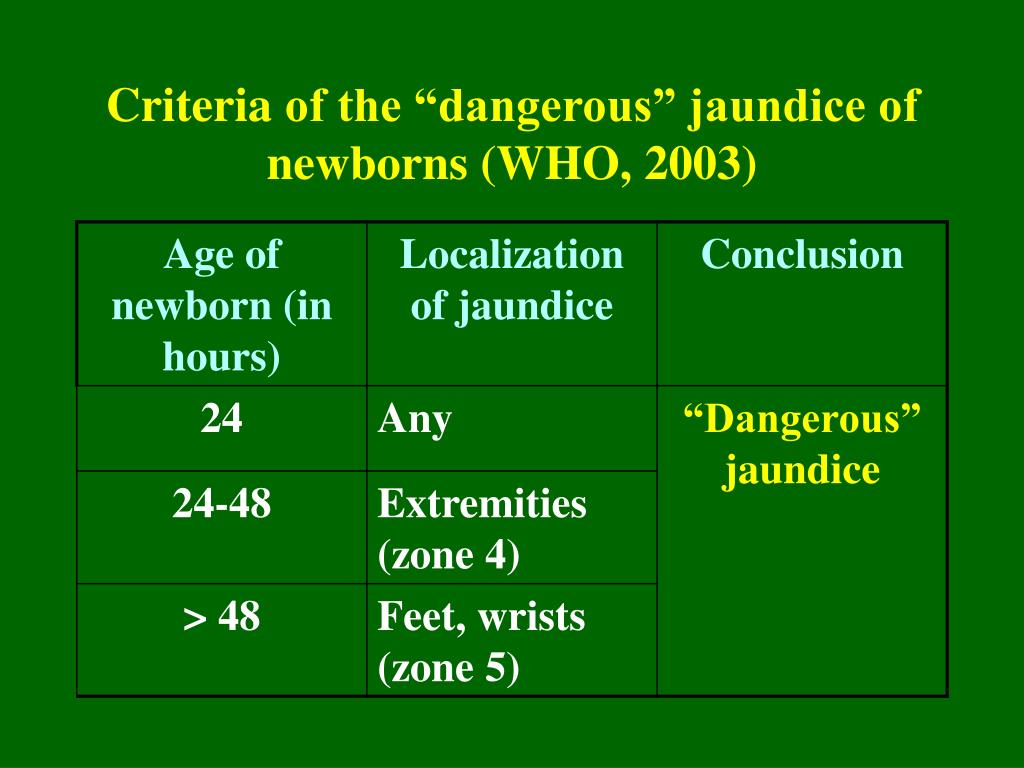 Any type of milk formula can be used.
Any type of milk formula can be used.
Breastfeeding jaundice may be prevented or reduced by increasing the frequency of feedings. If the bilirubin level continues to rise above 308 µmol/L in a full-term breastfed baby, temporary withdrawal of breast milk and switching to formula milk may be required. Stopping breastfeeding is only necessary for 1 or 2 days. At the same time, the mother should regularly express milk in order to resume breastfeeding without problems, as soon as the level of bilirubin in the child begins to decrease.
Also in these cases, the use of phototherapy is indicated: using fluorescent blue light with a wavelength of 425 to 475 nm. Light allows unconjugated bilirubin to be converted into forms that are water soluble and can be quickly excreted from the body by the liver and kidneys. This provides definitive treatment for neonatal hyperbilirubinemia and prevention of severe kernicterus.
Because visible jaundice may disappear during phototherapy even if serum bilirubin remains elevated, skin color cannot be used to assess the severity of jaundice.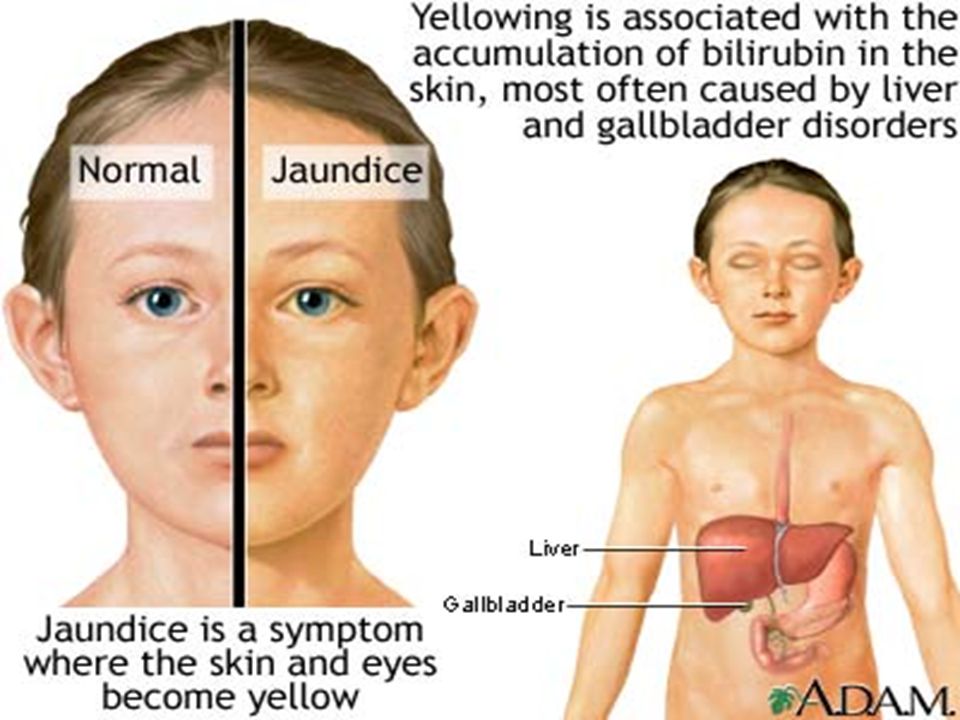 Blood taken to determine bilirubin concentration should be protected from bright light because bilirubin in test tubes can rapidly oxidize when exposed to daylight.
Blood taken to determine bilirubin concentration should be protected from bright light because bilirubin in test tubes can rapidly oxidize when exposed to daylight.
In severe hyperbilirubinemia, a blood transfusion is performed to quickly lower the bilirubin concentration.
\n
- \n
- Red blood cells are destroyed faster than usual.
- The liver does not have time to cope with the disposal of erythrocyte waste" }, { "@context" : "http://schema.org", "@type" : "NewsArticle", "headline" : "Norm of bilirubin in newborns", "image" : "https://virilismed.ru/wp-content/uploads/2019/09/novorozd-768x512.jpg", "articleSection" : "Is neonatal jaundice dangerous?", "datePublished": "2019-11-20T08:00:00+08:00", "dateModified": "2019-11-25T09:20:00+08:00", "author": { "@type": "Person", "name": "MC Virilis" }, publisher: { "@type": "Organization", "name": "Virilis", logo: { "@type": "ImageObject", "url": "https://virilismed.
 ru/wp-content/themes/virilis/img/logo.png" } }, "articleBody" : "Newborn jaundice is common among healthy newborns, and in most cases is physiological." }, { "@context" : "http://schema.org", "@type" : "NewsArticle", "headline" : "Norm of bilirubin in newborns", "name" : "Norm of bilirubin in newborns", "image" : "https://virilismed.ru/wp-content/uploads/2019/09/novorozd-768x512.jpg", "articleSection" : "Phototherapy - home treatment for jaundice", "datePublished": "2019-11-20T08:00:00+08:00", "dateModified": "2019-11-25T09:20:00+08:00", "author": { "@type": "Person", "name": "MC Virilis" }, publisher: { "@type": "Organization", "name": "Virilis", logo: { "@type": "ImageObject", "url": "https://virilismed.ru/wp-content/themes/virilis/img/logo.png" } }, "articleBody" : "For phototherapy of newborns, special blue light lamps (photoirradiators) are used. Treatment takes several days, the duration of therapy is determined by the pediatrician.
ru/wp-content/themes/virilis/img/logo.png" } }, "articleBody" : "Newborn jaundice is common among healthy newborns, and in most cases is physiological." }, { "@context" : "http://schema.org", "@type" : "NewsArticle", "headline" : "Norm of bilirubin in newborns", "name" : "Norm of bilirubin in newborns", "image" : "https://virilismed.ru/wp-content/uploads/2019/09/novorozd-768x512.jpg", "articleSection" : "Phototherapy - home treatment for jaundice", "datePublished": "2019-11-20T08:00:00+08:00", "dateModified": "2019-11-25T09:20:00+08:00", "author": { "@type": "Person", "name": "MC Virilis" }, publisher: { "@type": "Organization", "name": "Virilis", logo: { "@type": "ImageObject", "url": "https://virilismed.ru/wp-content/themes/virilis/img/logo.png" } }, "articleBody" : "For phototherapy of newborns, special blue light lamps (photoirradiators) are used. Treatment takes several days, the duration of therapy is determined by the pediatrician. Photoisomerization of bilirubin occurs in the skin, therefore, the more area of the body used for phototherapy, the more effective the treatment process. The lamp is a bath of harmless plastic, in the base of which blue light lamps are mounted. }, { "@context" : "http://schema.org", "@type" : "NewsArticle", "headline" : "Norm of bilirubin in newborns", "image" : "https://virilismed.ru/wp-content/uploads/2019/09/novorozd-768x512.jpg", "articleSection" : "How to lower bilirubin in children?", "articleBody" : "The treatment of jaundice is aimed at both the cause of the elevated bilirubin concentration and the elimination of the hyperbilirubinemia itself", "datePublished": "2019-11-20T08:00:00+08:00", "dateModified": "2019-11-25T09:20:00+08:00", "author": { "@type": "Person", "name": "MC Virilis" }, publisher: { "@type": "Organization", "name": "Virilis", logo: { "@type": "ImageObject", "url": "https://virilismed.ru/wp-content/themes/virilis/img/logo.
Photoisomerization of bilirubin occurs in the skin, therefore, the more area of the body used for phototherapy, the more effective the treatment process. The lamp is a bath of harmless plastic, in the base of which blue light lamps are mounted. }, { "@context" : "http://schema.org", "@type" : "NewsArticle", "headline" : "Norm of bilirubin in newborns", "image" : "https://virilismed.ru/wp-content/uploads/2019/09/novorozd-768x512.jpg", "articleSection" : "How to lower bilirubin in children?", "articleBody" : "The treatment of jaundice is aimed at both the cause of the elevated bilirubin concentration and the elimination of the hyperbilirubinemia itself", "datePublished": "2019-11-20T08:00:00+08:00", "dateModified": "2019-11-25T09:20:00+08:00", "author": { "@type": "Person", "name": "MC Virilis" }, publisher: { "@type": "Organization", "name": "Virilis", logo: { "@type": "ImageObject", "url": "https://virilismed.ru/wp-content/themes/virilis/img/logo. png" } } } ]
png" } } } ]
\n
Newborn jaundice: causes, treatment, consequences, prevention
Many parents experience newborn jaundice. This is especially true for premature babies, but in babies who were born at term, this is also a common occurrence.
Jaundice develops in the first few days after the birth of the baby, and the change in skin color usually becomes noticeable on the 3rd-4th day, just when the mother and baby return home from the hospital.
Why does this happen and what is the difference between the physiological jaundice of newborns, which does not require treatment, and the dangerous pathological jaundice of newborns? We deal with doctors.
What you need to know about jaundice in newborns
Bilirubin is formed during the breakdown of red blood cells (blood cells that are responsible for transporting oxygen) throughout life and is excreted from the body without problems with the help of the liver.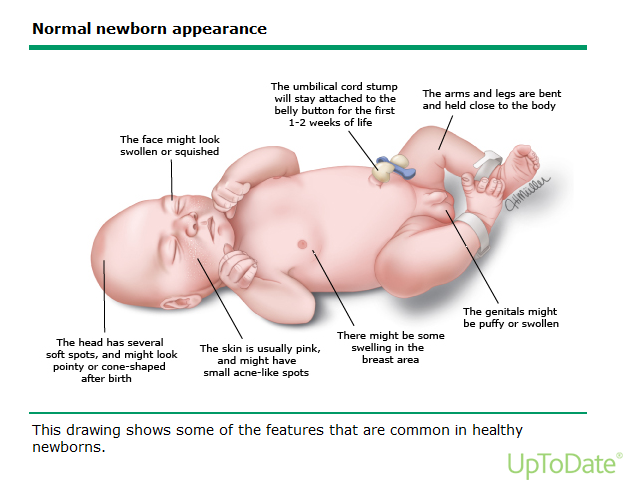 All body systems in a newborn do not work well enough, for example, the liver may not have enough enzymes to break it down and excrete it. Because of this, bilirubin accumulates in the blood, and the skin color becomes yellow. It happens that the whites of the eyes acquire the same shade.
All body systems in a newborn do not work well enough, for example, the liver may not have enough enzymes to break it down and excrete it. Because of this, bilirubin accumulates in the blood, and the skin color becomes yellow. It happens that the whites of the eyes acquire the same shade.
Physiological jaundice differs from pathological jaundice in that the former does not require treatment and resolves on its own. This usually happens after the first month of a baby's life. But the pathological condition is important and needs to be tracked in time. It affects the general well-being, has negative consequences, but with a competent approach, it is treated by a pediatrician or neonatologist.
| Physiological jaundice - a variant of the norm | In the first days of life, many parents experience yellowing of the baby's skin. At the same time, nothing threatens the condition of children, and the shade of the skin is normalized after 7-10 days. The only thing that can overshadow the first days of a baby’s life is vomiting. |
| There are several types of pathological jaundice | Conjugative jaundice develops due to liver enzyme deficiency. Hemolytic jaundice is associated with a change in the structure of red blood cells. And the problem of obstructive jaundice is a violation of the outflow of bile. |
| Things to pay attention to when treating jaundice (in addition to the general condition) | The doctor first of all specifies whether the child has prematurity and other factors that can complicate the course of the disease, whether there is a hereditary predisposition to this disease. It is worth paying attention to the appetite of the baby, and his mother, the level of lactation is also important. |
| There is a "bilirubin encephalopathy" | In this condition, bilirubin enters the child's nervous system due to the fact that there is not enough albumin to neutralize it. |
| Jaundice is not contagious | It cannot be transmitted through droplets. The cause of the disease is the increased breakdown of red blood cells and the insufficient functionality of the liver, which does not have time to process bilirubin secreted in large quantities. |
| When phototherapy is used for jaundice | At risk of hyperbilirubinemia, with physiological jaundice, with incompatibility of the baby's blood type with the mother's blood type, with an increase in bilirubin levels above 5 µmol / l per hour. |
How long does jaundice last in newborns
The duration of jaundice in a newborn depends on the characteristics of the organism. Physiological jaundice usually reaches its maximum on the 3-4th day of the baby's life. Gradual fading begins on days 4-5, and on days 7-14, the child's body completely copes with this condition.
- Parents are not always able to reliably determine whether the baby's jaundice is normal or not. Therefore, this condition is given maximum attention by the medical staff (first in the maternity hospital, then on patronage), - explains Albina Yusupova, pediatric neonatologist Lahta Clinic . - Before discharge in the maternity hospital, doctors examine the child, determine the presence of jaundice, evaluate the skin color in dynamics, whether the yellowness of the skin / sclera increases or not. Often they resort to using a percutaneous method for measuring the level of bilirubin (it is he who gives such staining of the skin) or take blood for analysis. With high numbers, phototherapy is prescribed (a special lamp or mattress). There are no exact numbers for this, it depends on many factors: gestational age (term baby or not), the presence of cephalohematoma or bruising at birth, the color of feces / urine, whether there are concomitant pathologies or not, the blood type of the mother and child, how the mother eats and gains weight Baby.
In most cases, pathological jaundice develops on the first day of a newborn's life. The duration may vary depending on the reason why the child suffers from this disease: sometimes the treatment takes 2 months, and in complex cases where enhanced therapy is required, jaundice can last up to a month.
Higher bilirubin levels have been reported in breastfed neonates with large postpartum weight loss (≥8%), diabetic mothers, low gestational age, and drug induction of labor with oxytocin (2).
Causes of jaundice in newborns
Jaundice can appear in a baby for various reasons. Most often it is the accumulation of bilirubin in the blood. But there are other conditions that newborns face in the first weeks of life.
Bilirubin
Signs of pathology:
- deviations from the normal course of physiological jaundice (earlier or later appearance, prolonged persistence, undulating course),
- appearance of pallor or a greenish tinge of the skin,
- an increase in the concentration of total bilirubin in the blood serum,
- a relative increase in the level of the direct fraction of bilirubin (3).
Unlike physiological, pathological jaundice, as a rule, develops in the first hours after the baby is born. There may be dark urine and discoloration of feces, anemia, and pale skin. The level of bilirubin is very high:
- above 256 µmol/l in children born at term,
- above 171 µmol/l in premature babies.
This condition is called hyperbilirubinemia. The most common cause of its development is hemolysis due to the incompatibility of the blood of the mother and child for erythrocyte antigens.
Other causes
“Pathological jaundice can be caused by several reasons,” says pediatrician Anna Levadnaya, Ph.D., author of the blog about pediatrics . - The most common is an increased breakdown of hemoglobin due to an Rhesus conflict or a blood type conflict between mother and child. Also, the cause of jaundice can be a pathology of the liver or a pathology of excretion of bile into the intestines. In addition, jaundice can be a sign of an infection, hypothyroidism (due to a decrease in thyroid function), polycythemia (an increased level of red blood cells in the blood), intestinal obstruction, or pyloric stenosis (this is a congenital narrowing of the stomach before entering the intestines, which makes it difficult for food to pass through). into it). It can occur with certain medications and for other reasons.
Hepatic jaundice occurs when a child's liver is exposed to viruses or bacteria. It can also develop with hepatitis B and hepatitis C, blood sepsis. At this time, the liver and spleen increase in size, the baby's urine acquires a more pronounced color. Hepatic jaundice is treated comprehensively, primarily by acting on the cause.
Violation of the outflow of bile can cause obstructive jaundice. This happens when the patency of the bile ducts worsens due to malformations, underdevelopment, or the appearance of neoplasms. Here, all attention should be paid to the place where bile accumulates and the reason why it accumulates. After all, it is because of her that the baby may show symptoms of jaundice.
Another cause is neonatal cholestasis. To confirm the diagnosis, it is necessary to make sure that the content of the direct fraction of bilirubin in the blood is more than 15–20% of the total level, an increase in the concentration of cholesterol, beta-lipoproteins, bile acids, as well as alkaline phosphatase and gamma-glutamyltransferase enzymes (3). This pathology occurs due to an increased level of bile acid synthesis, for which the newborn's liver is not ready. It happens that neonatal cholestasis occurs for reasons not related to the work of the liver. For example, against the background of hypoxia or the development of cardiovascular insufficiency.
There is also the so-called breastfeeding jaundice. There are studies that show that in healthy full-term infants who are bottle-fed, the level of bilirubin reaches a peak on the 5th day of life and becomes completely normal, on average, on the 13th day, while with natural feeding, two peaks of bilirubin rise are possible ( 3–5 and 10–15 days of life) with a gradual slow decrease (4). Jaundice from breast milk (from which certain hormones that increase bilirubin levels enter the baby's body) can last up to 6 weeks.
If the doctor makes this diagnosis, he must exclude the presence of hyperbilirubinemia. Because breastfeeding jaundice cannot cause it. If, when HB is canceled for 1-2 days, bilirubin begins to decrease, and yellowness disappears, the diagnosis is confirmed. But with positive dynamics, the abolition of breastfeeding is not required: it is resumed after 1-2 days. During the pause, the mother must definitely express herself in order to maintain lactation at the required level.
Treatment of neonatal jaundice
Physiological neonatal jaundice, as we have already said, does not require treatment. Sometimes pediatricians recommend supplementing such children with water, but only if lactation is established and using a spoon, not a bottle.
As for the pathological jaundice of a newborn, it requires mandatory treatment, which is prescribed by a doctor.
The most effective treatment for this condition is phototherapy. For this, a special lamp with blue light is used: under the influence of ultraviolet radiation, bilirubin breaks down and is excreted from the body of the newborn with urine and feces. The intensity and duration of phototherapy depends on the baby's body weight at birth and the level of bilirubin, which is constantly monitored. As a rule, three-hour sessions under the lamp are prescribed with a break of 2-3 hours. The newborn must be undressed, but the eyes must be protected, the boys also have the genitals.
In severe cases of neonatal jaundice, when the life of the baby is at risk, a blood transfusion may be indicated.
Doctors have almost abandoned the use of drugs to treat neonatal jaundice. Some of them, for example, ascorbic acid and albumin, negatively affect the functioning of the nervous system, the effectiveness of allochol and B vitamins has not been proven, and Karsil and Essentiale have not been sufficiently tested specifically for newborns (3).
- It is important to note that most experts now agree that the appointment of sorbents, drugs such as phenobarbital, Essentiale, LIV-52, the abolition of breastfeeding, UV (ultraviolet blood enrichment), electrophoresis or excessive infusion therapy for jaundice is ineffective ( and it’s not safe for phenobarbital), says Anna Levadnaya.
Consequences of jaundice in newborns
Physiological jaundice in newborns, as we have already noted, goes away on its own and does not bear negative consequences for the health of the baby. But the consequences of pathological jaundice in a newborn can be extremely serious, especially if treatment is not started on time.
— Too high blood levels of bilirubin can lead to brain damage, says Anna Levadnaya. - As a rule, this occurs in children with hemolytic disease according to the Rh factor, with an increase in the level of bilirubin above 298-342 µmol/l. And the higher the level of bilirubin, the higher the risk of encephalopathy.
Prevention of jaundice in newborns
The best prevention of jaundice in newborns is a healthy lifestyle for a mother during pregnancy, giving up bad habits, good nutrition.
In addition, the expectant mother must be tested to detect Rh-negative blood factor. Children born to mothers with Rh-negative blood are at risk for jaundice. After the birth of such babies, they carefully examine and monitor the content of bilirubin in the blood, and also determine the blood type.
- Women who may have a child with hemolytic jaundice are treated already during pregnancy. They are injected with anti-rhesus gamma globulin, and at birth, the child is immediately clamped on the umbilical cord and tested for bilirubin. If, according to the tests, there are indications, then the child is immediately put on phototherapy, - adds neonatologist Nadezhda Shurtakova . - The mother of the baby can also influence the fact that the child does not have jaundice. She needs to feed the baby more on the first day, try to get milk so that the baby does not lose weight. Jaundice often occurs with a large loss of initial weight. Bilirubin is a fat-soluble substance, and if the body of a newborn does not have enough fats, proteins and carbohydrates, then jaundice occurs at certain values of body weight loss.
Mother's milk is the best food for a newborn, it is easily digested, the intestines are stimulated faster, it is populated with beneficial microflora, the necessary enzymes are produced. All this helps the body of the newborn to cope with jaundice faster and more efficiently.
Frequently asked questions and answers
Nadezhda Shurtakova, neonatologist, head of the neonatal department at Maternity Hospital No. 4 (Moscow) answered frequently asked questions.
When is jaundice in newborns considered normal?
There are physiological and pathological jaundice. Physiological jaundice, which appears at the end of the second or third day of life, does not require treatment. Such jaundice is not pronounced and disappears on its own in 7-10 days. Physiological jaundice is present in 80% of children. Such children are discharged home without any additional examinations and treatment.
In what case is the child placed under the lamp and how long does the child need to stay there?
The child is placed under a lamp, for phototherapy, with pathological jaundice. The duration of therapy depends on what causes it.
Hemolytic jaundice of the newborn due to the Rh factor may appear already in the prenatal period, the child may be born with it and need an exchange transfusion. Such children are laid out under the lamp immediately at birth.
Jaundice caused by AB0 incompatibility (blood group incompatibility) appears at the age of 1.5 days. It is necessary to look at a biochemical blood test, and if there are indications, also put the child on phototherapy.
There is also conjugative jaundice, it, like physiological, also appears on the third day, but with it the amount of bilirubin (yellow substance) in the blood is significantly increased. Such children are also subject to phototherapy.
In different situations, phototherapy lasts from 1 to 4 days, usually 2-3 days, it is carried out under the control of biochemical and clinical blood tests. When the indicators are normal, the child is removed from phototherapy.
How long does it take to stay in the hospital if a newborn has jaundice?
Hemolytic jaundice lasts 5-7 days.