Pregnancy heart monitor
Fetal Heart Monitoring | Johns Hopkins Medicine
What is fetal heart monitoring?
Fetal heart rate monitoring measures the heart rate and rhythm of your baby (fetus). This lets your healthcare provider see how your baby is doing.
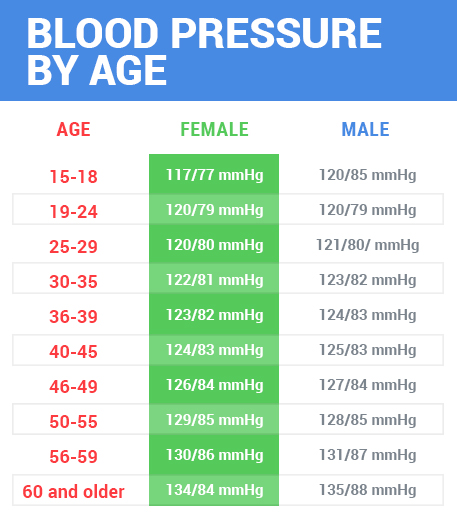
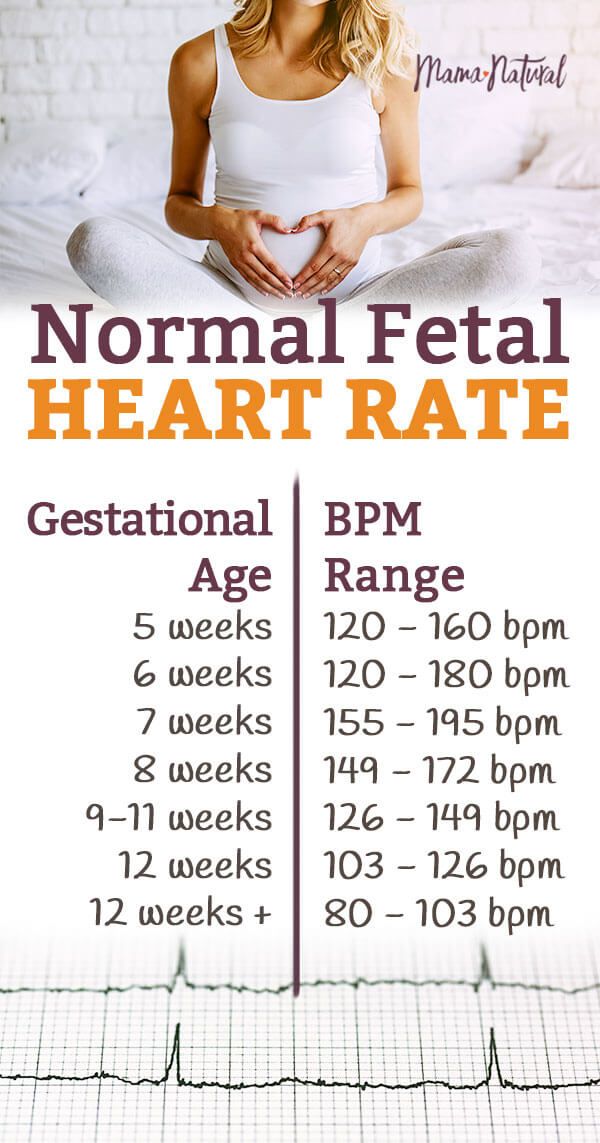
Your healthcare provider may do fetal heart monitoring during late pregnancy and labor. The average fetal heart rate is between 110 and 160 beats per minute. It can vary by 5 to 25 beats per minute. The fetal heart rate may change as your baby responds to conditions in your uterus. An abnormal fetal heart rate may mean that your baby is not getting enough oxygen or that there are other problems.
There are 2 ways to do fetal heart monitoring, external and internal:
External fetal heart monitoring
This method uses a device to listen to and record your baby’s heartbeat through your belly (abdomen). One type of monitor is a Doppler ultrasound device. It’s often used during prenatal visits to count the baby’s heart rate. It may also be used to check the fetal heart rate during labor. The healthcare provider may also check your baby’s heart rate continuously during labor and birth. To do this, the ultrasound probe (transducer) is fastened to your belly. It sends the sounds of your baby’s heart to a computer. The rate and pattern of your baby’s heart rate are shown on a screen and printed on paper.
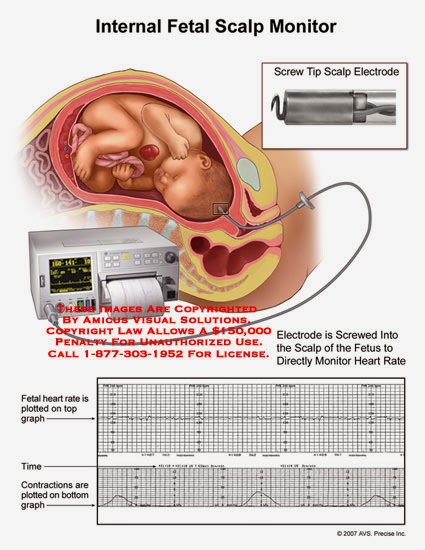
Internal fetal heart monitoring
This method uses a thin wire (electrode) put on your baby’s scalp. The wire runs from the baby through your cervix. It is connected to the monitor. This method gives better readings because things like movement don’t affect it. But it can only be done if the fluid-filled sac that surrounds the baby during pregnancy (amniotic sac) has broken and the cervix is opened. Your provider may use internal monitoring when external monitoring is not giving a good reading. Or your provider may use this method to watch your baby more closely during labor.
During labor, your healthcare provider will watch your uterine contractions and your baby’s heart rate.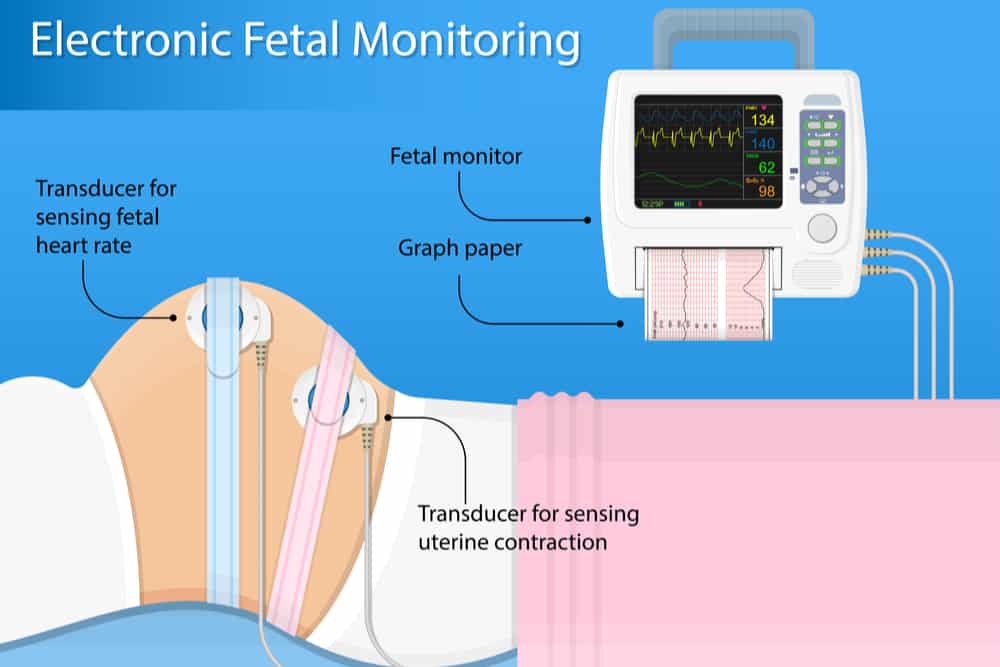 Your provider will note how often you are having contractions and how long each lasts. Because the fetal heart rate and contractions are recorded at the same time, these results can be looked at together and compared.
Your provider will note how often you are having contractions and how long each lasts. Because the fetal heart rate and contractions are recorded at the same time, these results can be looked at together and compared.
Your provider may check the pressure inside your uterus while doing internal fetal heart monitoring. To do this, he or she will put a thin tube (catheter) through your cervix and into your uterus. The catheter will send uterine pressure readings to a monitor.
Why might I need fetal heart monitoring?
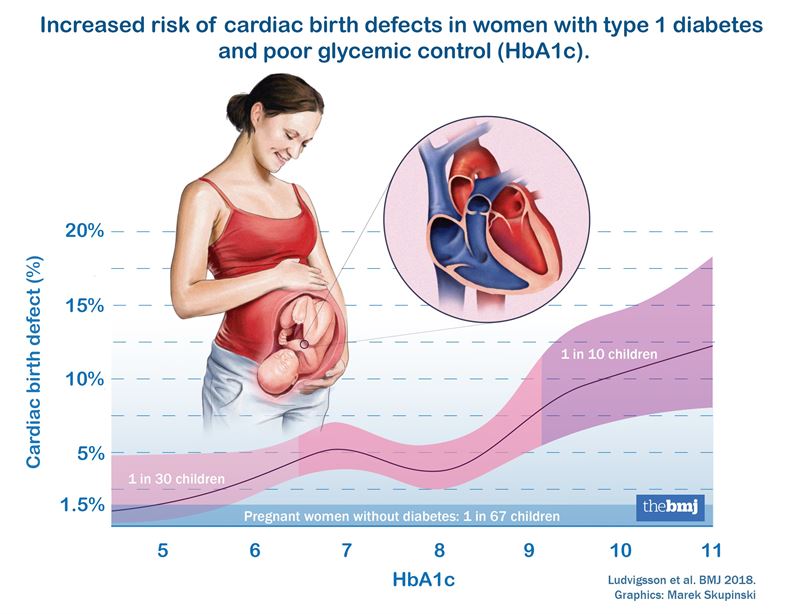
Fetal heart rate monitoring is especially helpful if you have a high-risk pregnancy. Your pregnancy is high risk if you have diabetes or high blood pressure. It is also high risk if your baby is not developing or growing as it should.
Fetal heart rate monitoring may be used to check how preterm labor medicines are affecting your baby. These are medicines are used to help keep labor from starting too early.
Fetal heart rate monitoring may be used in other tests, including:
- Nonstress test.
 This measures the fetal heart rate as your baby moves.
This measures the fetal heart rate as your baby moves. - Contraction stress test. This measures fetal heart rate along with uterine contractions. Contractions are started with medicine or other methods.
- A biophysical profile (BPP). This test combines a nonstress test with ultrasound.
Things that may affect the fetal heart rate during labor:
- Uterine contractions
- Pain medicines or anesthesia given to you during labor
- Tests done during labor
- Pushing during the second stage of labor
Your healthcare provider may have other reasons to use fetal heart rate monitoring.
What are the risks of fetal heart monitoring?
Radiation is not used for this test. The transducer usually causes no discomfort.
You may find the elastic belts that hold the transducers in place slightly uncomfortable.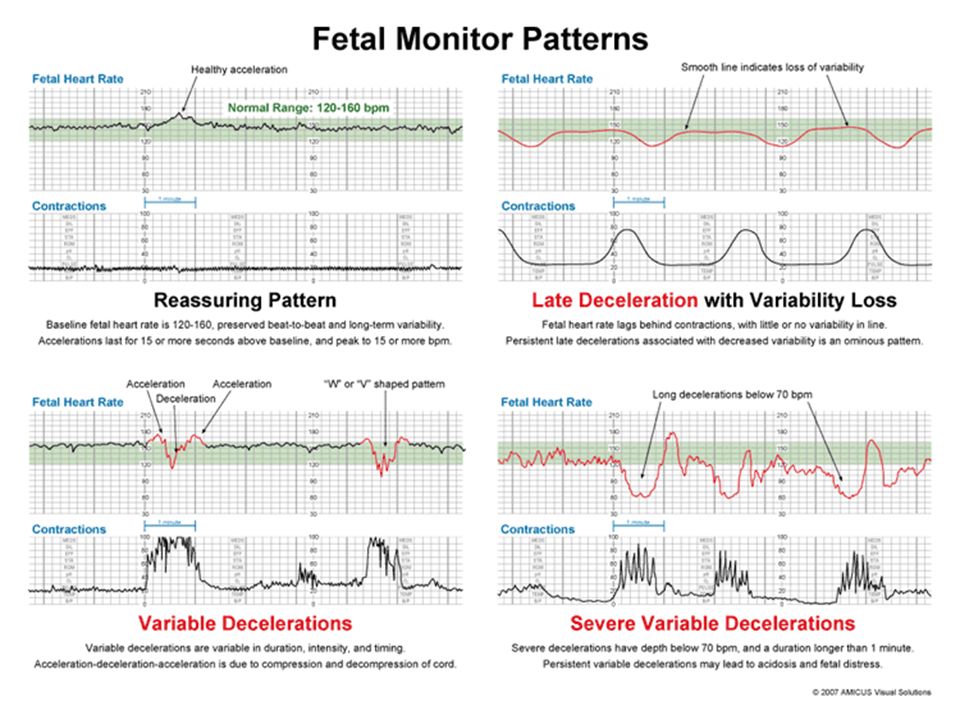 These can be readjusted as needed.
These can be readjusted as needed.
You must lie still during some types of fetal heart rate monitoring. You may need to stay in bed during labor.
With internal monitoring, you may have some slight discomfort when the electrode is put in your uterus.
Risks of internal monitoring include infection and bruising of your baby’s scalp or other body part.
Note: You should not have internal fetal heart rate monitoring if you are HIV positive. This is because you may pass the infection on to your baby.
You may have other risks depending on your specific health condition. Be sure to talk with your provider about any concerns you have before the procedure.
Certain things may make the results of fetal heart rate monitoring less accurate. These include:
- Obesity of the mother
- Position of the baby or mother
- Too much amniotic fluid (polyhydramnios)
- Cervix is not dilated or the amniotic sac is not broken.
 Both of these need to happen to do internal monitoring
Both of these need to happen to do internal monitoring
How do I get ready for fetal heart monitoring?
- Your healthcare provider will explain the procedure to you. Ask him or her any questions you have about the procedure.
- You may be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if anything is not clear.
- The consent form for fetal heart monitoring may be included as part of the general consent for labor and birth.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, or anesthesia.
- If fetal heart rate monitoring is done along with another monitoring test, you may be asked to eat a meal before the test. This can help make your baby more active.
- The amniotic sac must be broken and your cervix must be dilated several centimeters before the internal device can be put in place.
- Follow any other instructions your provider gives you to get ready.
What happens during fetal heart monitoring?
You may have fetal heart rate monitoring in your healthcare provider's office or as part of a hospital stay. The way the test is done may vary depending on your condition and your healthcare provider's practices.
Generally, fetal heart rate monitoring follows this process:
External fetal heart monitoring
- Depending on the type of procedure, you may be asked to undress from the waist down. Or you may need to remove all of your clothes and wear a hospital gown.
- You will lie on your back on an exam table.
- The healthcare provider will put a clear gel on your abdomen.
- The provider will press the transducer against your skin. The provider will move it around until he or she finds the fetal heartbeat. You will be able to hear the sound of the fetal heart rate with Doppler or an electronic monitor.

- During labor, the provider may check the fetal heart rate at intervals or nonstop, based on your condition and the condition of your baby.
- For continuous electronic monitoring, the provider will connect the transducer to the monitor with a cable. A wide elastic belt will be put around you to hold the transducer in place.
- The provider will record the fetal heart rate. With continuous monitoring, the fetal heart pattern will be displayed on a computer screen and printed on paper.
- You may not be able to get out of bed with nonstop external fetal heart rate monitoring.
- Once the procedure is done, the provider will wipe off the gel.
Internal fetal heart monitoring
- You will be asked to remove your clothes and put on a hospital gown.
- You will lie on a labor bed. Your feet and legs will be supported as for a pelvic exam.

- Your healthcare provider will do a vaginal exam with a gloved hand to see how far you are dilated. This may be slightly uncomfortable.
- If the amniotic sac is still intact, your healthcare provider may break open the membranes with a tool. You will feel warm fluid coming out of your vagina.
- Your healthcare provider will feel the part of the baby at the cervical opening with gloved fingers. This is usually the baby’s head.
- The provider will put a thin tube (catheter) into your vagina. He or she will put a small wire at the end of the catheter on the baby’s scalp. He or she will gently turn it on the baby’s skin.
- The provider will remove the catheter and leave the wire in place on the baby’s scalp.
- The provider will connect the wire to a monitor cable. He or she will keep it in place with a band around your thigh.
- You may not be able to get out of bed with nonstop internal fetal heart rate monitoring.
- Once the baby is born, the provider will remove the wire.
What happens after fetal heart rate monitoring?
You do not need any special care after external fetal heart monitoring. You may go back to your normal diet and activity unless your healthcare provider tells you otherwise.
After internal fetal heart rate monitoring, your healthcare provider will check your baby’s scalp for infection, bruising, or a cut. The provider will clean the site with an antiseptic.
Your healthcare provider may give you other instructions, based on your situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
Electronic Fetal Heart Rate Monitoring Test: Procedure & Results
Written by Lisa Fields
In this Article
- What Is Fetal Heart Rate Monitoring?
- Reasons for Fetal Heart Rate Monitoring
- Types of Fetal Heart Rate Monitoring
- Fetal Heart Rate Monitoring Risks
- Fetal Heart Rate Monitoring Procedure
- Fetal Heart Rate Monitoring Results
- Abnormal Fetal Heart Rate Treatments
What Is Fetal Heart Rate Monitoring?
Fetal heart rate monitoring is a process that lets your doctor see how fast your baby’s heart is beating.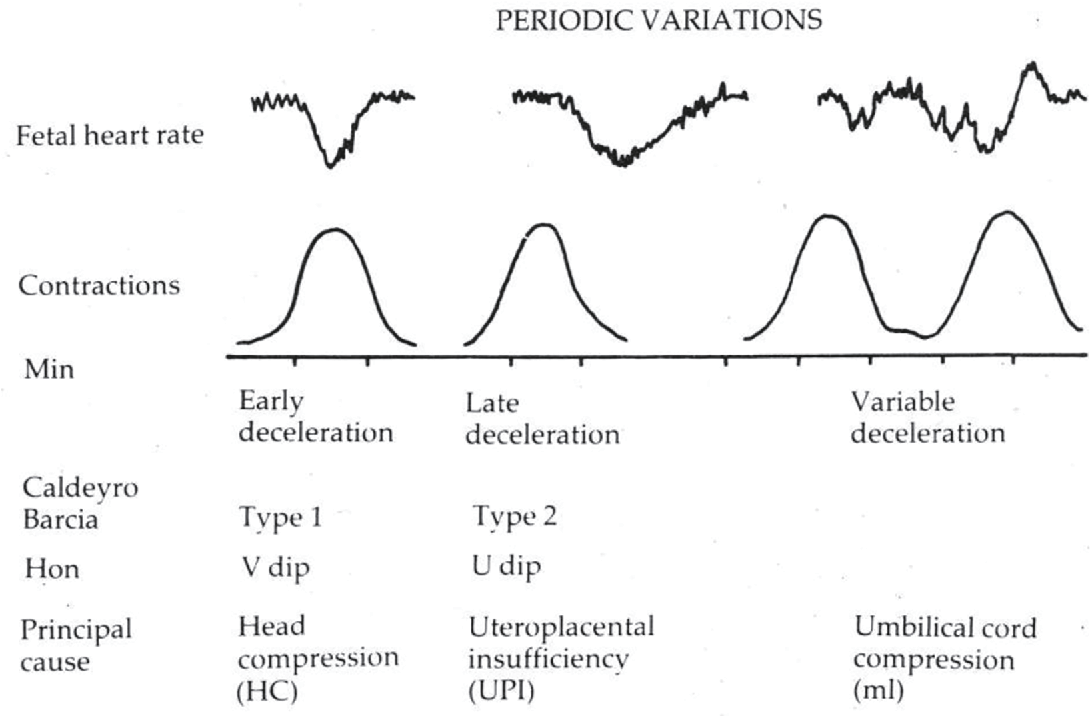 If you’re pregnant, your doctor will want to make sure your baby is healthy and growing as they should. One of the ways they do that is to check the rate and rhythm of your baby’s heartbeat.
If you’re pregnant, your doctor will want to make sure your baby is healthy and growing as they should. One of the ways they do that is to check the rate and rhythm of your baby’s heartbeat.
The doctor is most likely to do this later in your pregnancy and when you’re in labor. They may combine it with other tests for a closer look if you have diabetes, high blood pressure, or any condition that could cause problems for you and your baby.
Reasons for Fetal Heart Rate Monitoring
The doctor is more likely to use fetal heart rate monitoring when your pregnancy is high-risk. You may need fetal heart rate monitoring when:
- You have diabetes.
- You have high blood pressure.
- You’re taking medicine for preterm labor.
- Your baby isn’t growing or developing normally.
The doctor might also use fetal heart rate monitoring to make sure your baby is OK when you’re in labor or if there are other reasons to check your baby’s heart rate.
Types of Fetal Heart Rate Monitoring
The doctor can monitor your baby’s heartbeat in a couple of ways. They can listen for or electronically record the beats from outside your belly. Or once your water has broken and you’re in labor, they can thread a thin wire through your cervix and attach it to your baby’s head.
External monitoring (auscultation): If your pregnancy is going normally, the doctor likely will check your baby’s heart rate from time to time with a special stethoscope or a hand-held device called a Doppler ultrasound. Doctors sometimes call this type of fetal heart rate monitoring auscultation.
If you need it, the doctor might do a special test called a nonstress test, usually starting around week 32 of your pregnancy. It counts the number of times your baby’s heart speeds up during a 20-minute period.
For the test, you'll lie down with an electronic sensor belt around your belly that continuously records the baby's heartbeat.
The doctor also may wrap an electronic sensor belt around you to measure the baby’s heart rate during labor and delivery.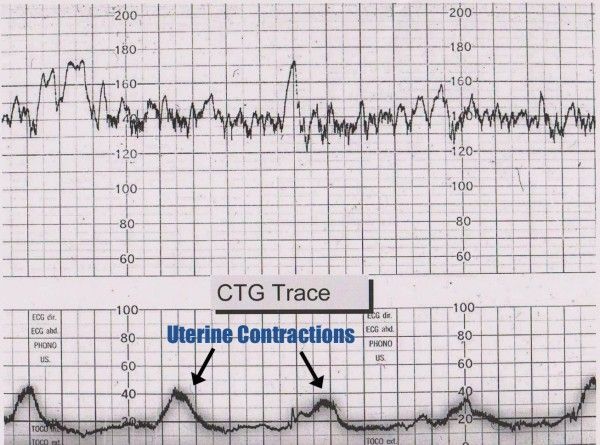 This lets them know if the contractions are stressing your baby. If so, you might have to have your baby as soon as possible.
This lets them know if the contractions are stressing your baby. If so, you might have to have your baby as soon as possible.
Internal monitoring: Once your water breaks and your cervix opens to prepare for birth, the doctor can run a wire called an electrode through it and into your womb. The wire attaches to your baby’s head and connects to a monitor. This gives a better reading than listening to your baby’s heartbeat from the outside.
Fetal Heart Rate Monitoring Risks
External monitoring isn’t risky. It doesn’t hurt or use radiation. If your doctor uses a belt, it might be a little uncomfortable. It also might mean you have to stay in bed during labor.
Internal monitoring risks include:
- Slight discomfort
- Infection
- Bruising or scratching your baby’s scalp
If you’re HIV-positive, you shouldn’t have internal fetal heart rate monitoring. That’s because there’s a risk of passing the infection to your baby. If you have other health conditions, ask your doctor if there are any special risks.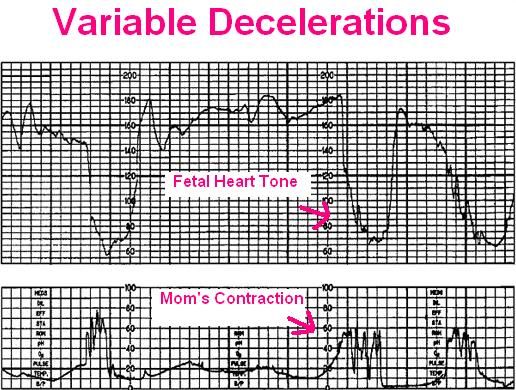
Fetal Heart Rate Monitoring Procedure
Fetal heart rate monitoring could happen in your doctor’s office or at the hospital. The procedure will depend on what type of monitoring you’ll have.
External fetal heart rate monitoring procedure
- Your doctor will ask you to undress and lie down on an exam table or labor bed.
- You’ll get clear gel on your belly.
- Your doctor will press a gadget called Doppler transducer to your belly and move it around.
- You’ll hear the sound of your baby’s heartbeat.
- If your doctor wants to measure the heartbeat continuously, they’ll use a wide belt to hold the transducer in place.
- Your doctor will record the fetal heart rate. You may see it on a computer screen.
Internal fetal heart rate monitoring procedure
- You’ll be asked to undress and lie down.
- You’ll put your feet and legs in supports, like you’re getting a vaginal exam.

- The doctor will check to see if your cervix is dilated.
- If your water hasn’t broken, the doctor may break it.
- The doctor will feel for your baby’s head.
- The doctor will put a thin tube (catheter) with a small wire at the end into your vagina.
- The doctor will put the wire on your baby’s scalp and remove the catheter.
- Once it’s connected to a cable, the wire will record your baby’s heartbeat until a doctor removes it or your baby is born.
Fetal Heart Rate Monitoring Results
A healthy baby’s heart usually beats 110-160 times a minute in the womb. It speeds up when the baby moves. Signs of possible problems include:
- Heart beats slower than 110 beats a minute
- Heart beats faster than 160 beats a minute
- A heartbeat pattern that isn’t normal
- The heartbeat doesn’t go up when the baby moves or during contractions
Lack of a normal heartbeat doesn’t always mean something is wrong with your baby. But it can be a sign that the baby isn’t getting enough oxygen.
But it can be a sign that the baby isn’t getting enough oxygen.
Your results also may be less accurate if:
- You’re obese.
- You or your baby is in the wrong position.
- You have too much amniotic fluid.
Abnormal Fetal Heart Rate Treatments
If your baby’s heart rate isn't what it should be, the doctor may try:
- Changing your positions to move the baby
- Giving you fluids through an IV
- Having you breathe extra oxygen
- Relaxing your uterus with medicine to slow contractions
- Giving you other drugs
If these steps don’t return your baby’s heart rate to normal, you may need to deliver them right away. If your cervix is completely open, the doctor may use a tool called forceps or a special vacuum to help you push the baby out. Otherwise, you’ll have the baby by emergency cesarean section.
CTG during pregnancy: what it is and what it is for
Services and prices
CTG: (Multiple pregnancy)
2000 ₽
CTG: (Fetal cardiotocography)
1600 ₽
Cardiotocography (CTG) is a functional diagnostic method based on recording the fetal heart rate and uterine contractility during pregnancy and childbirth. Cardiotocography is based on the Doppler effect and the principle of ultrasound. An ultrasonic wave is emitted from the transducer, which is reflected from the pulsating fetal heart, changes frequency and is sent back. The electronic system of the monitor registers and converts the signal. This recording is called a cardiotocogram.
Cardiotocography is based on the Doppler effect and the principle of ultrasound. An ultrasonic wave is emitted from the transducer, which is reflected from the pulsating fetal heart, changes frequency and is sent back. The electronic system of the monitor registers and converts the signal. This recording is called a cardiotocogram.
Two sensors are fixed on the belly of the pregnant woman. For better contact with the skin of the anterior abdominal wall, a special hypoallergenic gel is applied. At the point of best audibility of heart beats (usually around the navel), a heart rate sensor is applied, which records the fetal heartbeat. If the patient is pregnant with twins, then two sensors are used at once or measurements are taken in turn. The load cell registers the contractile activity of the uterus and the motor activity of the fetus.
Sometimes the baby's movements are recorded by an additional sensor. During the study, the device makes loud sounds, which should not be frightened. This is the baby's heartbeat. The fetus may change its position during the study, resulting in an incorrect recording. However, thanks to the sound component of the procedure, the doctor can control the correct location of the sensors and rearrange them in time after the child.
This is the baby's heartbeat. The fetus may change its position during the study, resulting in an incorrect recording. However, thanks to the sound component of the procedure, the doctor can control the correct location of the sensors and rearrange them in time after the child.
Cardiotocography, together with the results of other studies, allows you to recognize serious disorders, including fetoplacental insufficiency, intrauterine fetal hypoxia, various anomalies in the development of the fetal cardiovascular system, indirect signs of intrauterine infections, the threat of premature birth.
When and how often is the examination done?
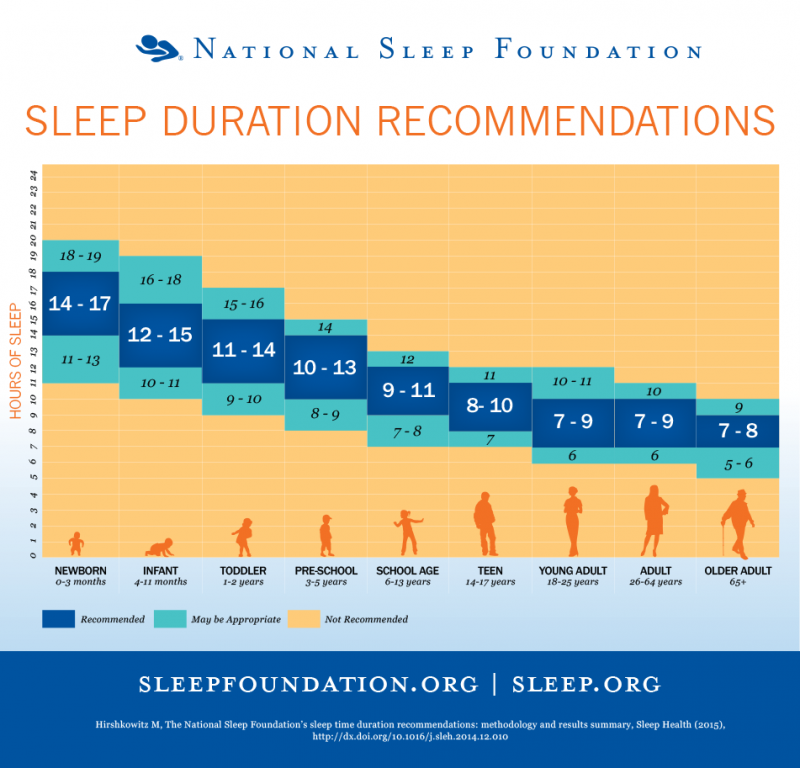
The study is carried out no earlier than 32 weeks. It is by this time that the nervous and cardiovascular systems reach a certain maturity. By 8 months, a myocardial reflex is formed - the relationship between cardiac activity and motor activity of the fetus. At the same time, the activity-rest cycle is established. Rhythmic changes of sleep and wakefulness of the fetus follow each other during the entire remaining period of pregnancy.
Cardiotocography must be performed 2 times during the 3rd semester. However, the frequency of the study is determined by the doctor based on the mother's history, pregnancy history, results of other examinations and risk factors.
Indications for examination
The purpose of cardiotocography is timely diagnosis and detection of fetal disorders. Based on the data of a number of functional diagnostic studies, such as ultrasound, CTG, dopplerometry, anamnesis, the obstetrician-gynecologist chooses the tactics of pregnancy management, treatment, the optimal term and method of delivery.
Indications for additional cardiotocography may include:
- Rh conflict
- Preeclampsia in the second half of pregnancy
- Maternal diseases
- Postterm pregnancy
- History of preterm birth
- Fetal growth retardation
- Pathologies of pregnancy and fetal abnormalities detected by ultrasound
- Oligohydramnios or polyhydramnios
- Multiple pregnancy
- Aggravated obstetric and gynecological history (abortions, miscarriages, premature births preceding this pregnancy)
- Change in the nature of fetal movements (complaints about a decrease or increase in the number of fetal movements per day)
Preparation for the procedure
The study does not require special preparation. However, it is worth considering the duration of the procedure. It will be important for mom to relax and be calm. On the eve of the procedure, it is recommended that a pregnant woman sleep well and relax. On the day of the study, it is worth taking care of a light meal 1-2 hours in advance. And immediately before the procedure, go to the toilet. During CTG, the expectant mother should not be distracted or disturbed by anything. You can take a book or magazine with you, but electronic devices, including the phone, will have to be turned off, as the technique interferes with the recording.
However, it is worth considering the duration of the procedure. It will be important for mom to relax and be calm. On the eve of the procedure, it is recommended that a pregnant woman sleep well and relax. On the day of the study, it is worth taking care of a light meal 1-2 hours in advance. And immediately before the procedure, go to the toilet. During CTG, the expectant mother should not be distracted or disturbed by anything. You can take a book or magazine with you, but electronic devices, including the phone, will have to be turned off, as the technique interferes with the recording.
How long does Cardiotocography take?
The procedure lasts from 30 to 60 minutes, depending on the activity of the baby. After 32 weeks, the fetus is characterized by the presence of periods of sleep and wakefulness. The active state lasts 50-60 minutes, while the calm state lasts 20-30 minutes. When evaluating cardiotocography, the period of wakefulness of the fetus is the leading one. Therefore, the duration of the study may vary.
Therefore, the duration of the study may vary.
Indicators
When analyzing CTG, a number of indicators are taken into account.
- Basal rhythm.
The cardiac sensor records the heart rate, and the cardiotocograph calculates the average fetal heart rate, which remains unchanged for 10 minutes or more. This indicator is called the basal rhythm. Normally, the fetal heart rate is subject to slight changes.
- Rhythm variability.
Rhythm variability is spoken of by the number and amplitude of deviations from the basal rhythm.
- Acceleration periods.
Acceleration is a period of increase in the fetal heart rate by 15 or more beats per minute for 15 seconds or more compared to the basal rhythm.
- Deceleration periods.
Deceleration is an episode of slowing heart rate by 15 heart beats per minute or more lasting 15 seconds or more. Decelerations usually occur in response to uterine contractions or fetal movements.

- basal rhythm within 110-150 bpm
- heart rate variability amplitude - 5-25 bpm
- decelerations absent or sporadic, shallow and very short
- 2 or more accelerations are recorded during 10 minutes of recording. If this type of CTG is detected in a short study period, the recording may not be continued.
- 9-12 - the condition of the fetus is satisfactory
- 6-8 - the fetus is in a state of hypoxia, but there is no threat of death in the next day
- 0-5 - severe hypoxia, threat of intrauterine death
- 1-2 - signs of initial disturbances
- 2-3 - severe violations
- >3 - critical condition.
WHO recommendations The criteria for a normal cardiotocogram are the following:
If your CTG indicators do not match the WHO criteria, then this does not indicate pathology. Cardiotocography is a method that is very sensitive to external influences. The correct interpretation of the results of the examination is possible only by a specialist in conjunction with other data.
Interpretation of results
CTG decoding should be done only by a specialist. This is a difficult process that requires knowledge and experience. Cardiotocogram consists of two types of graphs - tachogram and hysterogram. The tachogram reflects the change in the heart rate of the fetus. Time is measured horizontally, and the number of beats per minute is measured vertically. Thus, the graph deviates downwards with a decrease in heart rate, and upwards with an increase. When measuring the motor activity of the fetus, the indicators are displayed under the tachogram. On the second graph, usually located in the lower part of the cardiotocogram, the force of uterine contraction is displayed.
The tachogram reflects the change in the heart rate of the fetus. Time is measured horizontally, and the number of beats per minute is measured vertically. Thus, the graph deviates downwards with a decrease in heart rate, and upwards with an increase. When measuring the motor activity of the fetus, the indicators are displayed under the tachogram. On the second graph, usually located in the lower part of the cardiotocogram, the force of uterine contraction is displayed.
Initially, a visual interpretation of CTG is performed. However, to reduce the subjectivity of the assessment, it is customary to use rating scales. There are two methods: the Gauthier scale and mathematical analysis.
Gautier's ten-point scale is a questionnaire where the doctor is asked to evaluate the basal rhythm, variability, the number of accelerations, decelerations, and fetal movement. Each of the indicators is rated from 0 to 2 points.
Based on the total scores, a conclusion and recommendations for further observation are formed. This scale has many modifications.
This scale has many modifications.
The second method of evaluation is mathematical. When interpreting computer-processed data, a fetal condition indicator (PSP) is used.
Scores above 2 indicate a dangerous condition that requires hospitalization in a maternity hospital.
The CTG method, like any other, has its drawbacks and errors. In some cases, fetal oxygen consumption may decrease, regardless of the presence of pathology. For example, compression of the umbilical cord by the fetus causes a short-term disruption of blood flow. In this case, cardiotocography will register fetal hypoxia. However, these changes are temporary and if the position of the fetus changes, the blood flow will be restored. Therefore, the conclusion is not a diagnosis, and only a doctor should evaluate and interpret the indicators of the cardiotocogram.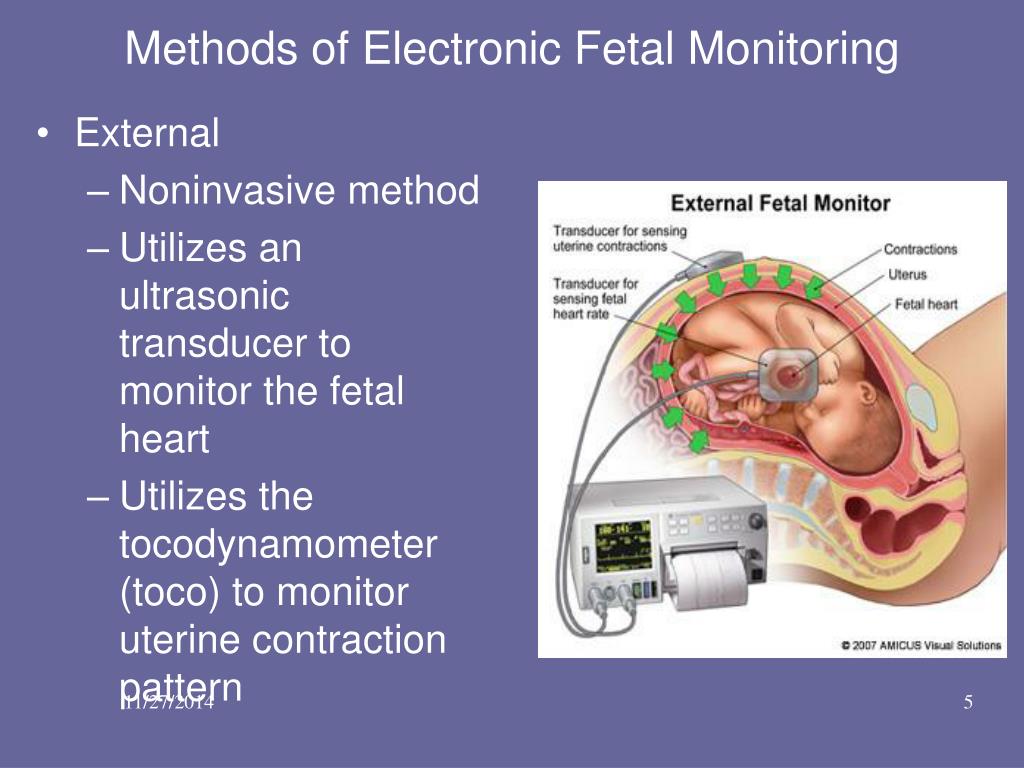
Effect of the procedure on the fetus
Cardiotocography is a study based on the action of ultrasonic waves, the safety of which has been proven by numerous studies and is beyond doubt. The procedure has no contraindications. If necessary, monitoring of indicators using CTG can be carried out several times a day or continuously, as during childbirth.
Back to the list of articles
exp - official distributor of FUJIFILM (HITACHI) for ultrasound
Dear Colleagues - doctors, clinic managers, regional dealers and foreign suppliers. We are glad to welcome you on our site and are ready for cooperation. Rus-exp has been supplying medical equipment to Russian clinics for more than 10 years.
Our main activity is supply of ultrasonic diagnostic equipment FUJIFILM (former HITACHI and ALOKA), made in Japan , whose official importer and we are the distributor of . Ultrasound devices are a necessary and very expensive element of equipping a modern medical center. Our specialists will conduct professional consultations on the choice of an ultrasound device, select the best option for an ultrasound diagnostic room, show the operation of the devices live, carry out installation and instruction, and train doctors to work on the devices. Contacting our company will save your time and buy an ultrasound machine at the best price-quality ratio.
Ultrasound devices are a necessary and very expensive element of equipping a modern medical center. Our specialists will conduct professional consultations on the choice of an ultrasound device, select the best option for an ultrasound diagnostic room, show the operation of the devices live, carry out installation and instruction, and train doctors to work on the devices. Contacting our company will save your time and buy an ultrasound machine at the best price-quality ratio.
| 10/05/2022 | New models ARIETTA 50 and ARIETTA 65 are on sale
|
| 06/06/2022 | We invite doctors to the "Russian Diagnostic Summit 2022" entrance to lecture hall U.
| 03/09/2022 | About the delivery situation due to current events |
| 02/22/2022 | Change of office and warehouse address |
| 09/13/2021 | We invite you to a master class / lecture |
| 09/11/2021 | Updated RUS-EXP catalog for ultrasound devices
|
| 08/26/2021 | We invite doctors to the "Russian Diagnostic Summit 2021"
|
| 06/01/2021 | Combination of HITACHI and FUJIFILM Medical device manufacturers HITACHI and FUJIFILM merged to produce ultrasound, CT and MRI. |
| 01/24/2021 | Special offers for private centers HITACHI F37 ultrasonic devices are available at a special promotional price for private medical centers. |
| 04/01/2020 | Operations during COVID-19 We continue to operate during the COVID-19 epidemic as a supplier and licensed service center for medical equipment. We have a sufficient stock of ultrasonic devices in stock.  We remind you that ultrasound scanners can be used to diagnose pulmonary pneumonia, thus being an anti-coronavirus technique. We remind you that ultrasound scanners can be used to diagnose pulmonary pneumonia, thus being an anti-coronavirus technique. |
| 01/10/2020 | January Specials for Private Centers For the most popular ultrasound model in the HITACHI line - the PROSOUND F37 model. Japanese assembly of the device and sensors. The devices are new. |
| 01/09/2020 | Special price for refurbished expert class device Refurbished HITACHI PROSOUND F75 PREMIER device can now be bought at half the price with a full warranty. |
| 08.09.2019 | Participation in the XXIX International Conference of the Russian Association of Human Reproduction "Reproductive Technologies Today and Tomorrow" LLC "Rus-exp" together with its partner LLC "Intergen" (Moscow) took part in a conference dedicated to reproductive medicine.  From our side, an ultrasound device HITACHI F37 was presented to control the IVF procedure with a special sensor and a steel puncture nozzle. From our side, an ultrasound device HITACHI F37 was presented to control the IVF procedure with a special sensor and a steel puncture nozzle. |
| 02/15/2019 | Supplier No. 1 HITACHI based on the results of 2018 Based on the results of imports in Russia in 2018, our company "Rus-exp" became the importer and supplier No. 1 for the supply of HITACHI ultrasound machines in unit terms. And also took 12th place among all importers (over 230 importers) of ultrasound in the Russian Federation in monetary terms. |
| 02/11/2018 | Supplier No. 1 HITACHI based on the results of 2017 Based on the results of imports in Russia in 2017, our company "Rus-exp" became the importer and supplier No. 1 in the supply of HITACHI ultrasound devices in piece terms.  And also took 16th place among all importers (over 210 importers) of ultrasound in the Russian Federation in monetary terms. And also took 16th place among all importers (over 210 importers) of ultrasound in the Russian Federation in monetary terms. |
| 02/12/2017 | Supplier No. 1 HITACHI based on the results of 2016 Based on the results of imports in Russia in 2016, our company "Rus-exp" became the importer and supplier No. 1 in the supply of HITACHI ultrasound devices in piece terms. |
| 04/01/2016 | Definitive merger of HITACHI and ALOKA into one company Healthcare Business Unit (HHBU). |
| 03/26/2016 | Participation in the Regional scientific and practical conference "New technologies in ultrasound diagnostics and their clinical application" LLC "Rus-exp" together with the representative office of the manufacturer HITACHI took part in the conference in Tver on March 25, 2016 |
| 09/19/2015 | Participation in the exhibition "Medicine Week of Stavropol" Stavropol LLC "Rus-exp" together with a partner LLC "MMC "Perspektiva" (Krasnodar) took part in the exhibition in Stavropol, held from 16 to 18 September 2015 |
 A.). The lecture will be held in Hall Z im. Samoilova October 21, 2021, beginning at 11:30 . UPD: the video of the lecture is available at the link.
A.). The lecture will be held in Hall Z im. Samoilova October 21, 2021, beginning at 11:30 . UPD: the video of the lecture is available at the link.  Our booth P8 ("Reinberga 8") .
Our booth P8 ("Reinberga 8") .