Baby position in womb at 36 weeks
Breech position baby: How to turn a breech baby
A breech baby is bottom-down instead of head-down in the womb. You might feel your baby kicking in your lower belly or the pressure of their head under your ribcage if they're in breech position. You can try some natural (unproven) methods of trying to turn your baby, or you may have a procedure in which an ob/gyn manually tries to turn your baby. Most breech babies are delivered via c-section.
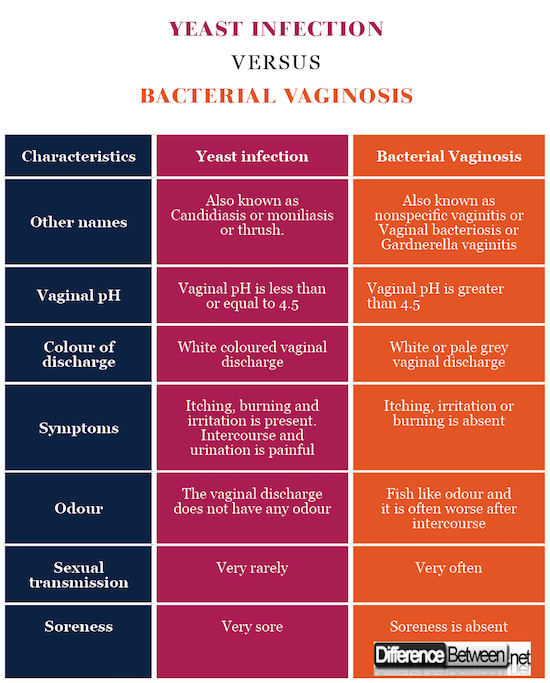
What does it mean when a baby is breech?
Breech is a term used to describe your baby's position in the womb. Breech position means your baby is bottom-down instead of head-down.
Babies are often active in early pregnancy, moving into different positions. But by around 8 months, there's not much room in the uterus. Most babies maximize their cramped quarters by settling in head down, in what's known as a cephalic or vertex presentation. But if you have a breech baby, it means they're poised to come out buttocks and/or feet first.
At 28 weeks or less, about a quarter of babies are breech, and at 32 weeks, 7 percent are breech. By the end of pregnancy, only 3 to 4 percent of babies are in breech position. At term, a baby in breech position is unlikely to turn on their own.
There are several types of breech presentations:
- Frank breech (bottom first with feet up near the head)
- Complete breech (bottom first with legs crossed)
- Incomplete or footling breech (one or both feet are poised to come out first)
(In rare cases, a baby will be sideways in the uterus with their shoulder, back, or arm presenting first – this is called a transverse lie.)
See what these breech presentations look like.
Signs of a breech baby
If your baby is in breech position, you may feel them kicking in your lower belly. Or you may feel pressure under your ribcage, from their head.
By the beginning of your third trimester, your practitioner may be able to tell what position your baby is in by feeling your abdomen and locating the baby's head, back, and bottom.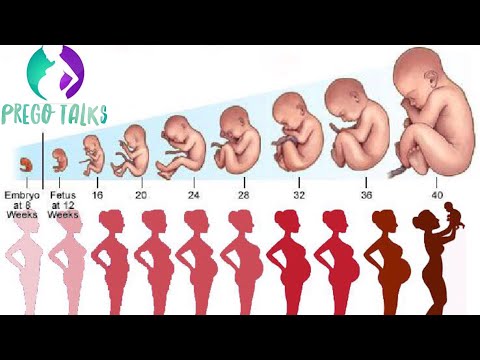
If your baby's position isn't clear during an abdominal exam at 36 weeks, your caregiver may do an internal exam to try to feel what part of the baby is in your pelvis. In some cases, they may use ultrasound to confirm the baby's position.
Why are some babies breech?
We don't usually know why some babies are breech – in most cases it seems to be chance. While sometimes a baby with certain birth defects may not turn to a head-down position, most babies in breech position are perfectly fine. Here are some things that might increase the risk of a breech presentation:
- You're carrying multiples
- You've been pregnant before
- You've had a breech presentation before
- There's too much amniotic fluid or not enough amniotic fluid
- You have placenta previa (the placenta is covering all of part of the opening of the uterus)
- Your baby is preterm
- Your uterus is shaped abnormally or has growths, such as fibroids
- The umbilical cord is short
- You were a breech delivery, or your sibling or parent was a breech delivery
- Advanced maternal age (especially age 45 and older)
- Your baby is a low weight at delivery
- You're having a girl
How to turn a breech baby: Is it possible?
There is a procedure for turning a breech baby. It's called an external cephalic version (ECV). An ob/gyn turns your baby by applying pressure to your abdomen and manually manipulating the baby into a head-down position. Some women find it very uncomfortable or even painful.
It's called an external cephalic version (ECV). An ob/gyn turns your baby by applying pressure to your abdomen and manually manipulating the baby into a head-down position. Some women find it very uncomfortable or even painful.
An EVC has about a 58 percent success rate, and it's more likely to work if this isn't your first baby. It's not for everyone – you can't have the procedure if you're carrying multiples or if you have too little amniotic fluid or placental abruption, for example. Your provider also won't attempt to turn your breech baby if your baby has any health problems.
The procedure is done after 36 weeks and in the hospital, where your baby can be monitored and where you'll be near a delivery room should any complications arise.
Watch a breech baby being turned.
Will I need a c-section if my baby is breech?
It depends, and it's something you'll want to talk with your caregiver about ahead of time. Discuss your preferences, the advantages and risks of each option (vaginal and cesarean delivery of a breech presentation), and their experience.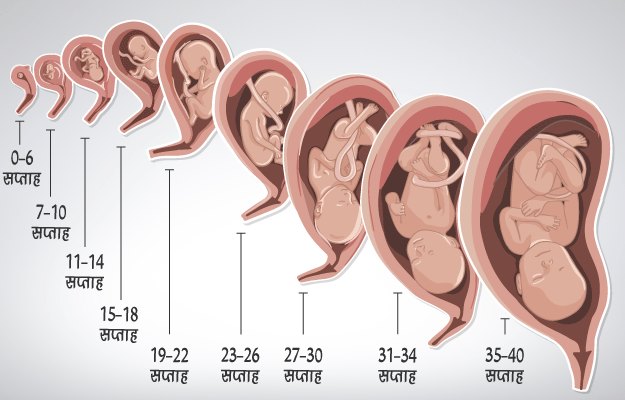 The biggest risk of a breech delivery is when the body delivers but the head stays entrapped within the cervix.
The biggest risk of a breech delivery is when the body delivers but the head stays entrapped within the cervix.
In the United States, most breech babies are delivered via cesarean. You may wind up having a vaginal breech delivery if your labor is so rapid that you arrive at the hospital just about to deliver. Another scenario is if you have a twin pregnancy where the first baby is in the head-first position and the second baby is not. A baby who delivers head-first will make room for the breech baby.
However, the vast majority of babies who remain breech arrive by c-section. If a c-section is planned, it will usually be scheduled at 39 weeks. To make sure your baby hasn't changed position in the meantime, you'll have an ultrasound at the hospital to confirm their position just before the surgery.
If you go into labor or your water will breaks before your planned c-section, be sure to call your provider right away and head for the hospital.
In rare circumstances, if you're at low risk of complications and your caregiver is experienced delivering breech babies vaginally, you may choose to have what is called a "trial of vaginal birth.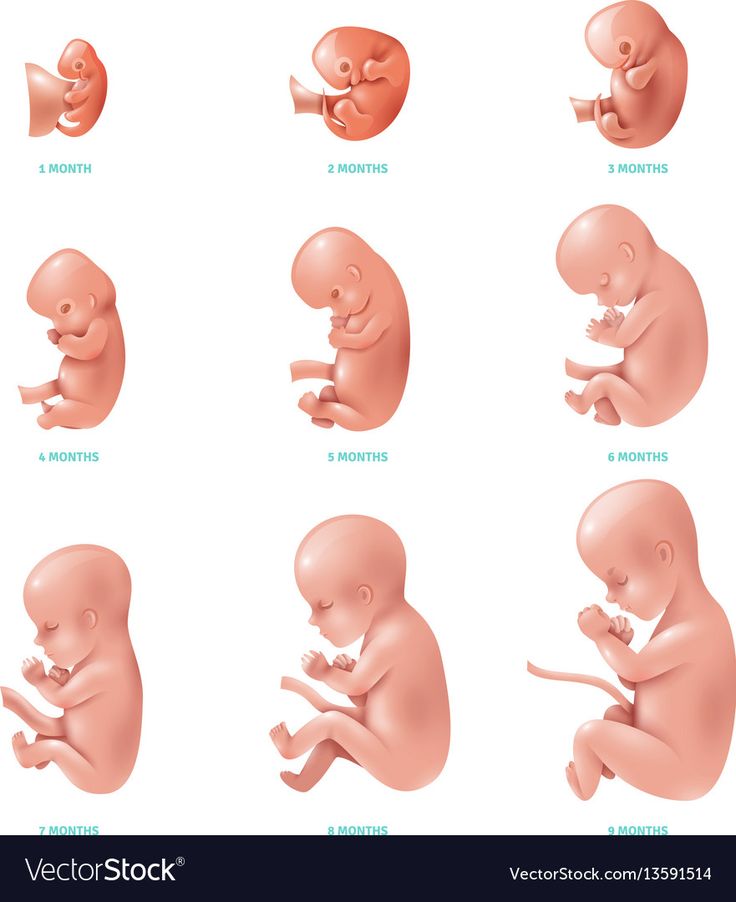 " This means that you can attempt to deliver vaginally but should be prepared to have a cesarean delivery if labor isn't progressing well. You and your baby will be closely monitored during labor.
" This means that you can attempt to deliver vaginally but should be prepared to have a cesarean delivery if labor isn't progressing well. You and your baby will be closely monitored during labor.
How to turn a breech baby naturally
In addition to ECV, there are some alternative, natural ways to try to turn your baby. There's no proof that any of them work – or that all of them are safe. Consult your practitioner before trying them.
Gravity
There's no conclusive proof that the mother's position has any effect on the baby's position, but the idea is to employ gravity to help your baby somersault into a head-down position. A few tips:
- Get into one of the following positions twice a day, starting at around 32 weeks.
- Be sure to do these moves on an empty stomach, lest your lunch comes back up.
- Make sure there's someone around to help you get up if you start feeling lightheaded.
- If you find these positions uncomfortable, stop doing them.

Position 1: Lie flat on your back and raise your pelvis so that it's 9 to 12 inches off the floor. Support your hips with a pillow and stay in this position for five to 15 minutes.
Position 2: Kneel down, with your forearms on the floor in front of you, so that your bottom sticks up in the air. Stay in this position for five to 15 minutes.
Sleeping position
Many women wonder if there are sleeping positions to turn a breech baby. But the positions you use to try to coax your baby head down for a short time shouldn't be used while you're sleeping. (It's not safe to sleep flat on your back in late pregnancy, for example, because the weight of your baby may compress the blood vessels that provide oxygen and nutrients to them.)
The best position for sleeping during pregnancy is on your side. Placing a pillow between your legs in this position may help open your pelvis, giving your baby room to move more easily. Support your back with plenty of pillows, too.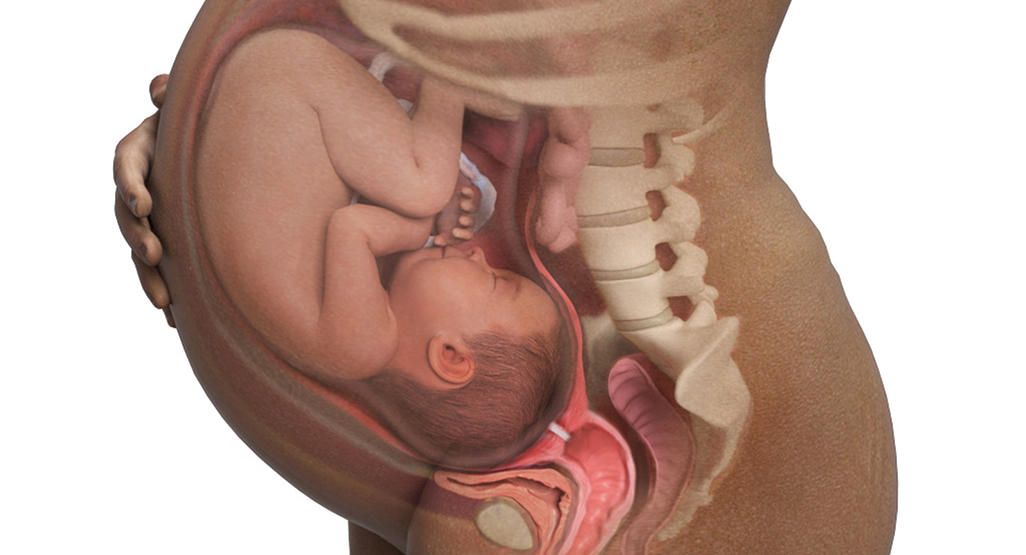 Again, there's no proof that this works, but since it's the best sleeping position for you and your baby, you may as well give it a try.
Again, there's no proof that this works, but since it's the best sleeping position for you and your baby, you may as well give it a try.
Moxibustion
This ancient Chinese technique burns herbs to stimulate key acupressure points. To help turn a breech baby, an acupuncturist or other practitioner burns mugwort near the acupressure point of your pinky toes. According to Chinese medicine, this should stimulate your baby's activity enough that they may change position on their own.
Some studies show that moxibustion in combination with acupuncture and/or positioning methods may be of some benefit. Others show moxibustion to provide no help in coaxing a baby into cephalic position.
If you've discussed it with your caregiver and want to give it a try, contact your state acupuncture or Chinese medicine association and ask for the names of licensed practitioners.
Hypnosis
One small study found that women who are regularly hypnotized into a state of deep relaxation at 37 to 40 weeks are more likely to have their baby turn than other women. If you're willing to try this technique, look for a licensed hypnotherapist with experience working with pregnant women.
If you're willing to try this technique, look for a licensed hypnotherapist with experience working with pregnant women.
Chiropractic care
There's a technique – called The Webster Breech Technique – that aims to reduce stress on the pelvis by relaxing the uterus and surrounding ligaments. The idea is that a breech baby can turn more naturally in a relaxed uterus, but research is limited as to the risks and benefits of this technique. If you're interested, talk with your provider about working with a chiropractor who's experienced with the technique.
Music
This is a safe – and again, unproven – method based on the fact that your baby can hear sounds outside the womb. Simply play music close to the lower part of your abdomen (some women use headphones) to encourage your baby to move in the direction of the sound.
Learn more:
- C-section recovery
- Third trimester pregnancy guide and checklist
- Hospital bag checklist
advertisement | page continues below
Early signs of going into labor
Time to give birth or a false alarm? Learn the early signs of labor, how to tell if it's true labor or false labor, and what happens when labor starts for real.
In late pregnancy, it's easy to wonder if every symptom you're having is an early signs of labor. Are you having Braxton Hicks or "real" contractions? Is that your mucus plug or normal vaginal discharge?
While every woman's experience is different, learning the typical signs of labor can help you feel more prepared when it does happen. While in the movies women have two contractions and deliver a baby, in the real world labor is typically a longer and unmistakable process.
What is labor?
Labor is the process of delivering your baby – and the placenta – from your uterus through your vagina and into the world. Your body will go through different stages of labor during childbirth, and you'll experience a number of telltale signs of each stage. Within those stages are phases, too.
There are three stages of labor. In the first stage, contractions thin (efface) and open (dilate) your cervix. This stage has two phases, the latent phase, when your cervix is slowly dilating from 0 to 6 cm, and the active phase, when stronger contractions dilate the cervix more rapidly from 6 cm to full dilation at 10 cm.
Once you're fully dilated, the second stage starts as your baby descends into the vaginal canal and is birthed. (You'll be pushing during this stage.) The third stage starts with your baby's birth and ends with the delivery of the placenta.
Read more about the stages of labor and delivery.
Early signs that indicate labor is near
In the final days or weeks before your due date, you may notice one or more signs that labor is near. Not all women experience all of these signs – again, this is very individual – but if you do feel like your baby has dropped lower, for example, or you have some mucousy discharge or more Braxton Hicks contractions than usual, you may be close to labor day!
Before you get excited about labor starting, remember that many of these signs and symptoms can precede labor by weeks. Rather than predicting that labor is imminent, these can just be symptoms of being pregnant near your due date.
Still, here are some of the early signs that labor may be near:
Baby has dropped
If this is your first pregnancy, you may feel what's known as lightening a few weeks before labor starts. Lightening means your baby has "dropped" and now rests lower in your pelvis.
Lightening means your baby has "dropped" and now rests lower in your pelvis.
When your baby drops, you might feel less pressure just below your ribcage, making it easier to catch your breath. If you experienced heartburn during pregnancy, it might now improve. (On the downside, you may need to pee more often because your baby's pressing on your bladder.)
If this isn't your first baby, however, lightening may not happen until labor begins.
Loss of the mucus plug
If your cervix begins to efface or dilate significantly as you get close to labor, you may pass your mucus plug – the small amount of thickened mucus that has collected within your cervical canal during your pregnancy. If you see mucus, it's likely a sign that you're dilating – but it can still be some time before labor begins.
The mucus plug may come out in a lump all at once or as an increased amount of vaginal discharge over the course of several days – or even weeks. Without the other signs of labor noted below, you don't need to call your doctor or midwife if you pass your mucus plug.
You have some "bloody show"
You may have noticed more vaginal discharge during pregnancy, thanks to your body's increased estrogen. Normal, healthy discharge is usually creamy white or clear, but it may also be tinged brown, pink, or red. Other colors – such as yellow, green, or gray – may signal an infection or other problem.
When your cervix starts to soften, you may notice pink discharge or bright red blood. This is called "bloody show." Sometimes this happens as you lose your mucus plug (the mucus may be tinged with blood) but it can also happen independently.
Having sex or a vaginal exam can also disturb your mucus plug and result in some blood-tinged discharge or bleeding, even when labor isn't necessarily starting any time soon.
Call your provider if you have bleeding heavier than a period, consistent red bleeding that's not slowing or turning brown, or bleeding in combination with abdominal pain.
Cervix has started to efface and dilate
In the days and weeks before delivery, changes in the connective tissue of your cervix make it soften and lead to dilation and effacement (when your cervix thins and opens).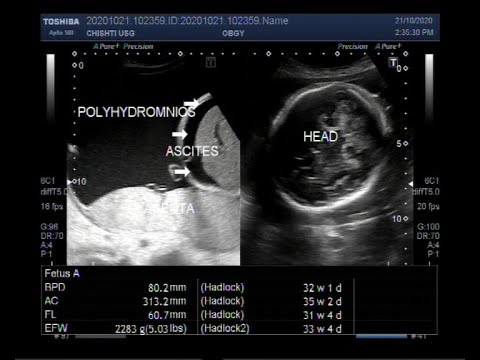
If you've given birth before, your cervix is more likely to dilate a centimeter or more before labor starts. Still, that's no guarantee that labor is imminent.
When you're at or near your due date, your doctor or midwife may do a vaginal exam during a prenatal visit to see whether your cervix has started the process of effacement and dilation. Whether you have this exam is up to you. Cervical exams can be uncomfortable, and they can't predict future labor timing. But exams can be helpful for planning an upcoming induction or for estimating how much time you'll have to get to the hospital if you have a history of fast labors.
Braxton Hicks contractions
You may have experienced Braxton Hicks contractions throughout your pregnancy. If you're having a Braxton Hicks contraction, you'll feel a tightening or squeezing of your uterus, lower abdominal area, or groin. Then it will relax. Unlike true labor contractions, Braxton Hicks contractions are irregular and usually not painful.
More frequent and intense Braxton Hicks contractions can signal that real contractions are coming soon – but not always.
Signs of labor
Labor usually occurs sometime between 38 and 41 weeks. While early signs that labor may be approaching aren't at all clear or dependable, these are reliable signs that you're in real labor:
Contractions
When your uterus contracts, your abdomen feels tight or hard, and you have a sensation of cramping. When the uterus relaxes between contractions, the sensation dissipates. Labor contractions will grow stronger, longer, and more frequent as they cause your cervix to dilate. True labor contractions are too painful to talk through, and they may bring tears to your eyes. Find out more about what contractions feel like according to moms.
You'll want to start timing your contractions – how far apart they are and how long they last. (Time contractions starting from the beginning of one until the beginning of the next.) Your doctor or midwife probably gave you directions about when to come in based on the timing of the contractions. If not, give them a call and ask. These videos explain more about how contractions feel and how to time contractions.
If not, give them a call and ask. These videos explain more about how contractions feel and how to time contractions.
Back pain
If you're having lower back pain along with contractions, it may be a signal that you're having back labor. The pain from back labor continues between contractions, though it may get stronger during contractions.
Back pain usually means that your baby's head is pressing against your lower back, though one theory suggests that the pain may be "referred" from your uterus to your lower back.
Your water breaks
When the fluid-filled amniotic sac surrounding your baby ruptures, fluid leaks from your vagina. It may come out in a large gush or a small trickle, or anything in between. If you're not sure whether your water broke, call your doctor or midwife to discuss your symptoms.
Labor usually follows soon after your water breaks – regular contractions often start before this, but in some cases, the water breaks first.
If your water breaks when you're full term but you're not in labor (not having contractions), it's called premature rupture of membranes (PROM).
If you don't start having contractions on your own within six to 24 hours of your water breaking, your provider will most likely recommend that labor be induced. That's because your baby is more likely to get an infection without the amniotic sac's protection against germs. Most providers will offer you an immediate induction but give you the option to postpone if you want to give labor a chance to start on its own.
If you're leaking amniotic fluid before 37 weeks, it's called preterm premature rupture of membranes (PPROM), and it may mean your baby will be delivered prematurely due to the increased risk of infection.
Whenever your water breaks, call your doctor or midwife. (Call them even if you think your water broke but aren't sure.)
Regardless of contractions, if you're group B strep positive you'll need to start on antibiotics as soon as your water breaks to prevent an infection in your baby.
What is preterm labor?
Labor usually starts between week 37 and week 42 of pregnancy. If you start having regular contractions that cause your cervix to begin to open before you reach 37 weeks of pregnancy, you're in preterm labor. (It's also known as premature labor.)
If you start having regular contractions that cause your cervix to begin to open before you reach 37 weeks of pregnancy, you're in preterm labor. (It's also known as premature labor.)
It can be difficult to tell whether you're having preterm labor or not, because some of the symptoms (like Braxton Hicks and low back pain) may be things you've experienced throughout your pregnancy.
Still, call your doctor or midwife right away if you're having any of the following symptoms before 37 weeks:
- More vaginal discharge than usual
- A change in the type of discharge – if you're leaking watery fluid or your discharge becomes watery, mucus-like, or bloody (even if it's pink or just tinged with blood)
- Any vaginal bleeding or spotting
- Abdominal pain, menstrual-like cramping, or six or more contractions in one hour (even if they don't hurt)
- More pressure in the pelvic area (a feeling that your baby is pushing down)
- Low back pain, especially if it's dull or rhythmic, or you didn't previously have back pain
- Your water breaks, either in a gush or a trickle
If you are – or might be – in preterm labor, your doctor or midwife may give you medications to help your baby's lungs mature, and to protect their brain. You may also receive medicine to stop or slow early contractions. Getting these medications early can improve outcomes for your baby, so be sure to call if you think you may be in preterm labor.
You may also receive medicine to stop or slow early contractions. Getting these medications early can improve outcomes for your baby, so be sure to call if you think you may be in preterm labor.
Am I in labor?
It can be hard to tell at first. But the frequency, length, intensity, and location of your contractions can help you figure out whether you're in true labor or are having Braxton Hicks contractions. How changing positions, walking, and rest affect your contractions provide more clues. Additionally, if you notice any bloody show with your contractions, they're probably true labor contractions.
This chart outlines differences between true and false labor contractions.
| False labor contractions (Braxton Hicks) | True labor contractions | |
|---|---|---|
| Timing | Are irregular and don't get closer together over time | Happen at regular intervals and get closer together over time |
| Length | Vary in length and don't get longer over time (fewer than 30 seconds or up to 2 minutes each) | Start to last longer with each contraction (about 30 to 70 seconds each) |
| Intensity | Are weak and don't get stronger with time (may be weak then strong, then weak again) | Grow stronger and more painful with each contraction |
| Location | Are felt at the front of the abdomen | May start in the back and move to the front, or radiate down into the thighs |
| Effect of moving or resting | Contractions stop when you change position, walk, or rest | Contractions continue even when you change position, walk, or rest |
No matter how well informed you are about the signs of labor, it's normal to have a false alarm. Don't be embarrassed about calling your doctor – or showing up at the hospital – because you think you're in labor when you're not.
Don't be embarrassed about calling your doctor – or showing up at the hospital – because you think you're in labor when you're not.
If you're assessed at the hospital and sent home because you're not in labor yet, your care team will give you specific instructions about changes to look for in the next few days or weeks and when to call or come back.
When to go to the hospital for labor
Toward the end of your pregnancy, your doctor or midwife will most likely give you clear guidelines about when to let them know that you're having contractions, and when you should grab your hospital bag and head to the hospital or birth center.
Your instructions will depend on your individual situation – such as whether you have a high-risk pregnancy or other complications, if this is your first baby, if you're planning a cesarean delivery, and how far you live from the hospital or birth center.
If your pregnancy is uncomplicated, they'll probably have you wait to come in until you've been having contractions that last for about a minute each, occur every five minutes for about an hour, and are very uncomfortable.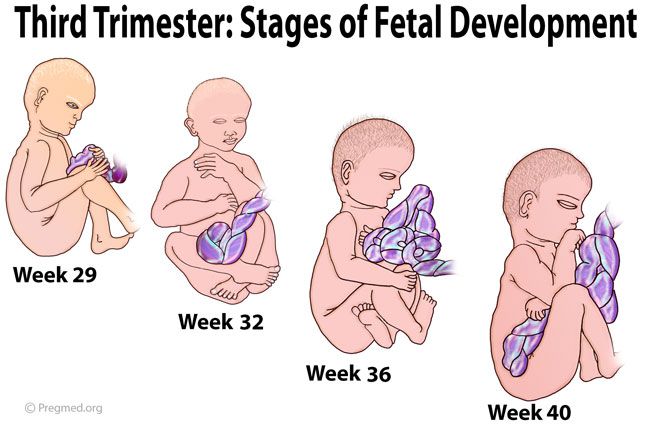
If you're unsure whether it's time, go ahead and call. Doctors and midwives are used to getting calls from women for guidance about whether they're in labor.
When you call, your doctor or midwife will get some clues about your condition from the sound of your voice. They'll want to know:
- How close together your contractions are
- How long each one lasts
- How strong they are (like whether you can continue talking through a contraction)
- If you think your water has broken
- If you're having vaginal bleeding
- If you're feeling the baby move normally
Your provider will also take your obstetric history into account. What number baby is this for you? Did you have fast labors in the past? Have you had a c-section and are you planning to have one this pregnancy? Are you group B strep positive or negative?
- You have signs of labor and have been having pregnancy complications
- You have early signs of labor before 37 weeks
- Your water breaks and you notice meconium in your amniotic fluid (it looks greenish or is streaked with green, brown, or yellow).
 This may be a sign that your baby is under stress.
This may be a sign that your baby is under stress. - You notice that your baby is less active.
- You have vaginal bleeding, constant and severe abdominal pain, or a fever. These may be signs of a problem with the placenta, such as placental abruption, or an intrauterine infection.
- You have symptoms of preeclampsia (a very serious blood pressure disorder) such as abnormal swelling, severe or persistent headaches, vision changes, intense pain or tenderness in your upper abdomen, or difficulty breathing.
If your water breaks, call your provider. They may have you wait at home until you also have regular contractions or a certain amount of time has passed, or they may want you to head to the hospital. (If you tested positive for group B streptococcus, for example, your provider will want you to go to the hospital as soon as your water breaks so you can start taking antibiotics.)
Learn more:
- Pregnancy symptoms you should never ignore
- Labor positions
advertisement | page continues below
36th week of pregnancy: sensations, signs, fetal development
Pregnancy
Article
3. 6/5 277 reviews
6/5 277 reviews
You will soon become a mother. You may notice an increased desire to clean the house or immediately go shopping for children's things. This is a natural state - the period of "nesting" begins.
8 min. for reading By Oksana Negrich Feb. 17, 2022
It is believed that the most suitable period for childbirth is 40 weeks. At 36 obstetric weeks of pregnancy, the fetus is already fully formed, so do not worry if the baby is born a little earlier.
Week 36: Pregnancy
At this stage, your body is preparing for childbirth. It's not so easy to deal with a huge belly anymore. For many women, this is a very uncomfortable period, accompanied by pain in the legs, poor sleep and a constant feeling of fatigue. To everything else, sharp mood swings and the first harbingers of childbirth, in particular training contractions, can be added.
Training contractions
Braxton-Hicks contractions, or false contractions, are contractions of the uterus lasting up to a minute, which are accompanied by a pulling sensation in the lower abdomen or in the lumbar region. The main difference between such contractions and labor is that they are irregular and do not contribute to the opening of the cervix.
Causes:
- Stress or emotional outbursts.
- Increased physical activity.
- Full bladder.
- Dehydration of the body (dehydration).
- Intimacy.
When training contractions appear, the main thing is to try to relax. Start with breathing, try the following techniques:
- Slow inhalation during uterine contraction, then a deep exhalation.
- Slow and deep inhalation through the nose, then sharp and short exhalation through the mouth. Imagine blowing out a candle on a cake.
- Rapid and shallow breathing, but not more than 30 seconds.
When should you see a doctor?
- Prolonged pain, especially drawing pain in the lower back.
- Contractions have become regular.
- The waters have broken.
- The appearance of bleeding.
- The fetus has become less mobile.
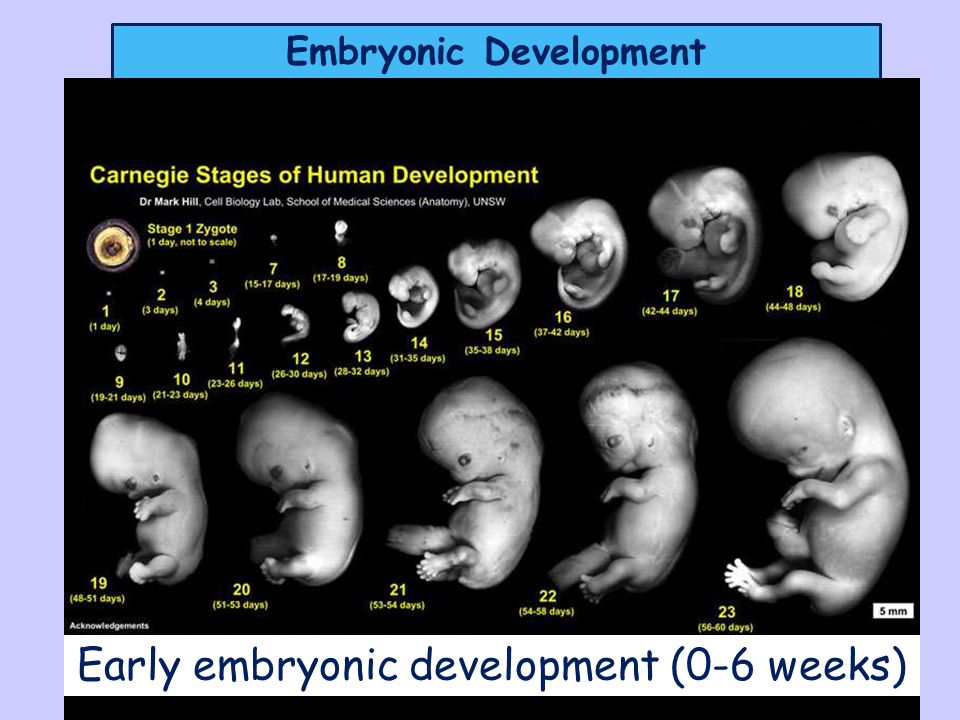
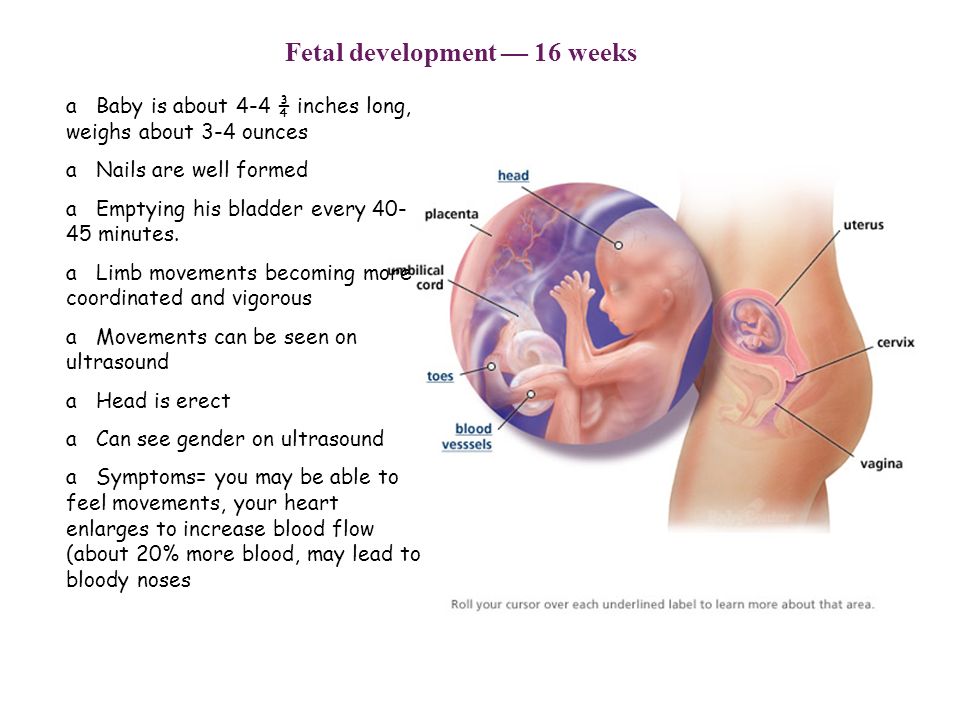
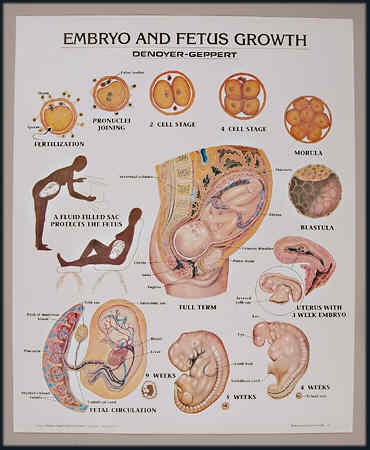
What happens to the fetus at the 36th week of pregnancy
The baby's internal organs are already formed and working at full capacity. The heart pumps blood, providing nutrition to all the tissues of a small organism. The lungs produce the substance needed to open them on the first spontaneous breath, but are not yet ready to sustain breathing without help. Because of this, in medicine it is believed that the baby at 36 weeks is still premature.
The kidneys are already working and even produce urine, which is released into the amniotic fluid. Through a fully mature placenta, the baby receives nutrients and oxygen. The baby's intestines are also functioning, the first feces have already appeared in it - meconium, which will come out within the first day after birth.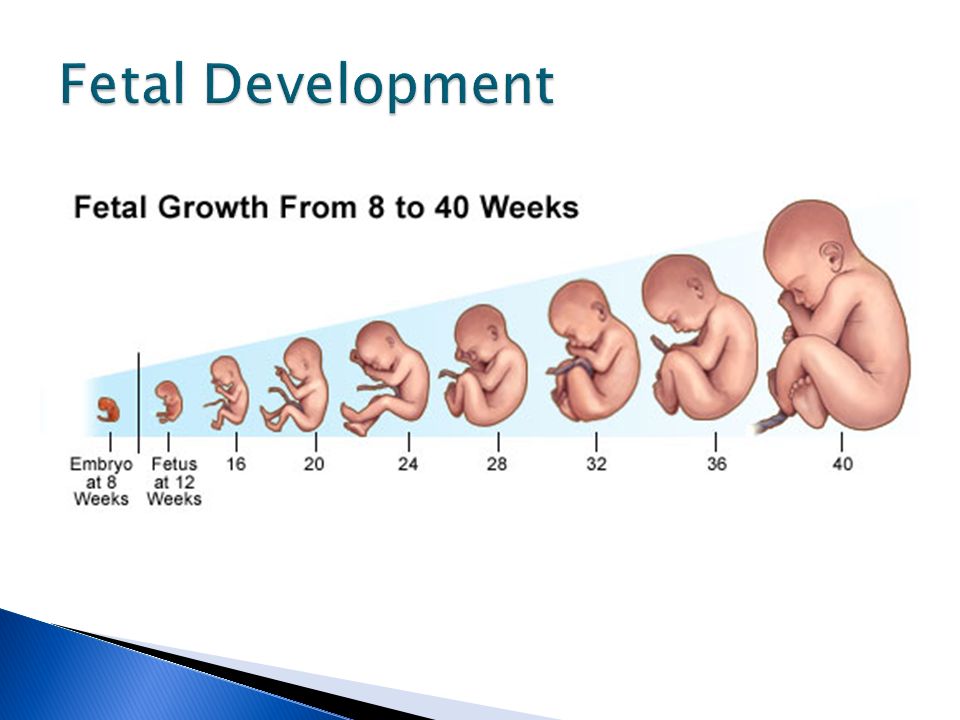
The skeleton of a baby at 36 obstetric weeks of pregnancy is already quite strong. Only the bones of the skull are covered with cartilage to maintain mobility as they pass through the mother's birth canal. The skin of the child is leveled by increasing the amount of subcutaneous fat. The original lubricant gradually disappears from the skin, which protected it from softening under the influence of amniotic fluid.
At 36 weeks pregnant, the baby weighs approximately 2.6 kg and can be up to 47 cm long.
From 36 weeks, the baby develops a sucking reflex, and the baby begins to identify the flavors of the food that the mother consumes.
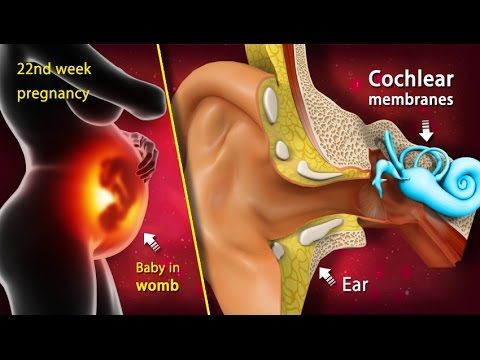
The connection between the baby and parents is getting stronger. Hearing a native voice, the baby's heart beats more intensely, the frequency can reach up to 140 beats per minute.
Fetal position
From the 36th week of pregnancy until delivery, the baby remains in one position. Very rarely, babies roll over in the last week or during the birth process.
If you are pregnant with your first child, it is likely that your baby's head may begin to droop as early as this week. This will allow your lungs and diaphragm to expand a bit and make it easier for you to breathe. If the baby is not in cephalic presentation, discuss delivery options with your doctor.
What happens to the mother at 36 weeks of pregnancy
The most common complaint of women at 36 weeks pregnant is back pain. This is not surprising, because the stomach has shifted the center of gravity of the body, and therefore you have to involuntarily bend in the lumbar zone in order to maintain balance. As a result, the back muscles are too tense, which causes pain. Therefore, it becomes more difficult to walk and lie down.
It is not recommended to lie on your back, as this can compress blood vessels and increase the lack of oxygen. Try to rest while lying on your side. For convenience, buy a supportive pregnancy pillow. You can also put a soft blanket under the sheet.
Your uterus will enlarge so much that you will have to put up with more frequent visits to the toilet - the bladder will be full even from a small amount of liquid you drink.
From the pleasant - from the 36th week of pregnancy, swelling decreases. This is how the body prepares for childbirth. Visually, it may seem that you have lost weight, but do not worry - excess fluid is just leaving the body. Be prepared for the mucus plug, the small clot that closes off the cervical canal during pregnancy, to protect the baby from infections. You can also say goodbye to heartburn and stomach pain.
Read also: Mucus plug and other signs of childbirth
Advice. The last weeks and days before delivery are unforgettable. At every opportunity, observe the movements in the abdomen. You will be able to see the outline of a tiny arm, leg or knee. Try to gently poke your finger back, you will see how the child moves away from him. Such cute games will help you and your partner to strengthen the family bond.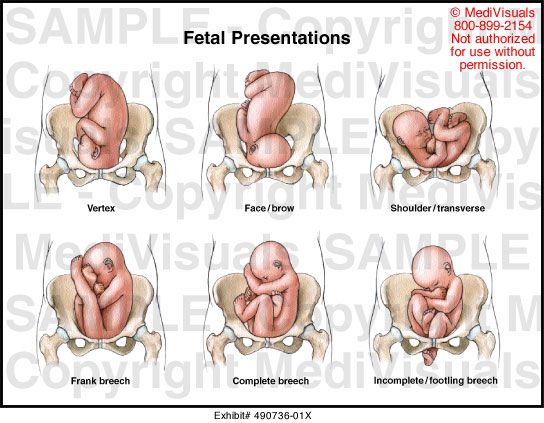
Emotional changes
Shortly before childbirth, you may experience emotional swings, become more vulnerable, suspicious and irritable. An unstable mental state can provoke unwanted painful symptoms:
- cramps in the limbs;
- pain in hip joints, pubis;
- heaviness in the spine;
- prostration;
- nausea.
Remember, the child feels your stress. Take care of yourself and try not to get nervous over trifles.
Read also: Third trimester of pregnancy. Emotions and experiences. Working with feelings
36th week of pregnancy: necessary tests and ultrasound
Each pregnancy is individual, but still there is a list of tests that are mandatory for each woman:
- Urinalysis. Evaluation of kidney function.
- Complete blood count.
- Test for HIV infection and sexually transmitted diseases.
- Blood sugar test.
- Blood test for hormones (TSH, T4, progesterone and others).
- Blood test for torch infection (herpes virus, hepatitis, rubella, lupus, toxoplasmosis, cytomegalovirus).
- Bacteriological examination of urine for latent infections.
- Smear for pathogenic flora and cytology.
- ultrasound. Assessment of the state of the placenta, monitoring of the developmental indicators of the baby and its location in the uterus.
- Cardiotocography (with reduced fetal activity).
In addition to a number of tests, during the examination, the doctor must measure the volume of the abdomen, the weight of the woman and the height of the fundus of the uterus. Also, according to the results of ultrasound diagnostics, the specialist correlates the size of the child with the size of the pelvis of the pregnant woman. In case of an increased risk of not passing the fetus through the birth canal during normal childbirth, a caesarean section may be offered so as not to endanger either the expectant mother or the baby. Therefore, already at the 36th obstetric week of pregnancy, you should discuss all the details with your gynecologist and make a decision.
Therefore, already at the 36th obstetric week of pregnancy, you should discuss all the details with your gynecologist and make a decision.
At 36 weeks' gestation, the fundal height should be approximately 35 cm, with variations of a few centimeters possible.
Read also: 3rd pregnancy screening: timing
36th week of pregnancy: nutrition of the expectant mother
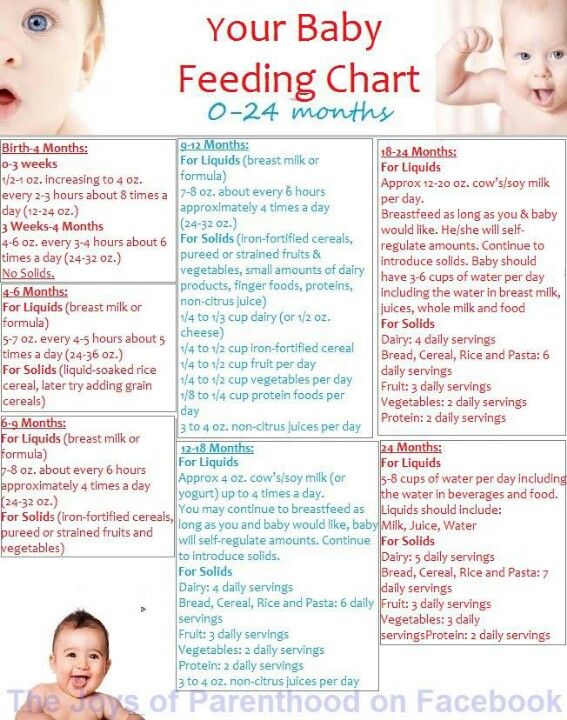
The development of a child inside the womb directly depends on your lifestyle. This is why the foods you eat during these nine months are more important than ever. Research shows that not only genes, but also nutrition during pregnancy can affect a baby's birth weight, as well as future health.
Contrary to the old belief, "eating for two" is not necessary during pregnancy. For example, a "bucket" of eaten fruits will bring you heaviness in the stomach and extra pounds instead of good. If you're at a normal weight, you only need about 450 extra calories a day during your third trimester - that's about one sandwich, half a glass of milk, and an apple.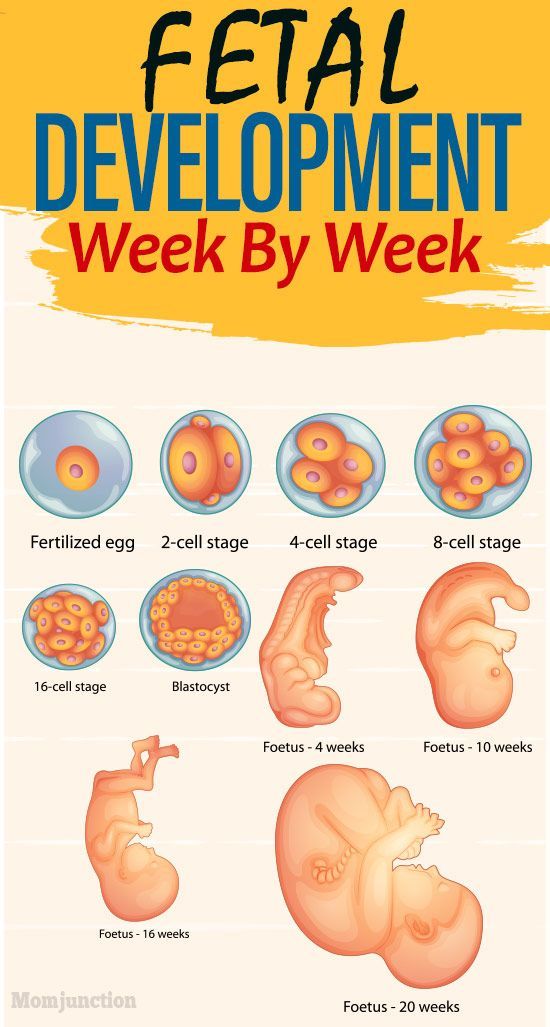
5 Essential Nutrients Your Baby Needs Now
- Folic Acid . This vitamin is important for the development of the child's brain and spinal cord. Eat more leafy green vegetables, dried beans and peas, oranges, and whole grains.
- Protein is the building block for your growing child's body tissues. Protein sources: meat, including lean beef, lamb, pork and poultry, milk, cheese, eggs and soybeans.
- Zinc . During pregnancy, the need for zinc increases by almost 25%. Eating foods like eggs, seafood, red meat, dried beans and lentils, peanuts and whole grains will provide your child with zinc and help build a healthy immune system.
- Omega-3 helps your child's brain and eye development. These beneficial fatty acids are found in egg yolks and fatty fish such as salmon and sardines.
- Iron is an essential component of the blood, responsible for oxygen transport, as well as growth and immune function.
 Make sure you have enough red meat, chicken, eggs, beans, lentils, broccoli, and spinach in your diet.
Make sure you have enough red meat, chicken, eggs, beans, lentils, broccoli, and spinach in your diet.
Dangers and possible problems
Prematurity
Babies born before 37 completed weeks of gestation are considered preterm. The causes may be hormonal disorders or chronic diseases of a woman, pathologies of pregnancy, rarely - intrauterine infection of the fetus. To date, it is possible to predict preterm birth and prolong pregnancy. To do this, check the hormonal background and measure the cervix.
With multiple pregnancies, in most cases, labor begins much earlier than 40 weeks. It's quite normal.
If you experience nausea, vomiting or diarrhea at 36 weeks of pregnancy, this may also indicate the approach of labor or complications.
Oligohydramnios during pregnancy
Amniotic fluid protects the baby's body from infections and bacteria. Sometimes, in about 8% of women, a small amount of amniotic fluid may be observed in the last trimester. The most common signs are pain when the child moves and a small abdomen. This kind of condition can cause premature birth and needs to be monitored by a doctor.
The most common signs are pain when the child moves and a small abdomen. This kind of condition can cause premature birth and needs to be monitored by a doctor.
Discharge: is it worth it to be afraid
At 36 weeks of pregnancy, the discharge becomes more dense, similar to mucus. It is worth paying attention to their color:
- pink or brown indicates the approach of childbirth and is a signal to contact your doctor as soon as possible;
- yellow or green, sometimes gray, may indicate infection, in such cases medical attention is needed;
- red is an alarm, often indicating placental abruption.
Pain in the lower abdomen
One of the reasons may be training contractions, which we wrote about above. But it is possible that this is a symptom of preeclampsia - premature aging of the placenta. It is important to diagnose the problem in time, because this can lead to a delay in the development of the child in the future.
Sex at 36 weeks pregnant
If a woman feels well, doctors do not prohibit intimacy. But sexual intercourse can stimulate contractions: this is due to prostaglandins - active substances that are contained in semen. In addition, you should refrain from lying on your back.
But sexual intercourse can stimulate contractions: this is due to prostaglandins - active substances that are contained in semen. In addition, you should refrain from lying on your back.
36th obstetric week of pregnancy: doctor's advice
Starting at 36 weeks, you can slowly start preparing for the upcoming birth. This includes not only the purchase of necessary things for the first time after the appearance of the baby. It is very important to prepare mentally.
Soon, almost all of your time will have to devote to the little man, so try to rest more and sleep longer. Spending time with your partner will help strengthen your bond.
Physical exercise in the thirty-sixth week of pregnancy is possible, but be careful not to lift heavy objects, so as not to stimulate the activity of the uterus. Suitable exercises with a low risk of injury, such as water aerobics, yoga for pregnancy or breathing
gymnastics. This has a beneficial effect on the respiratory and cardiovascular systems, and can even facilitate the process of childbirth.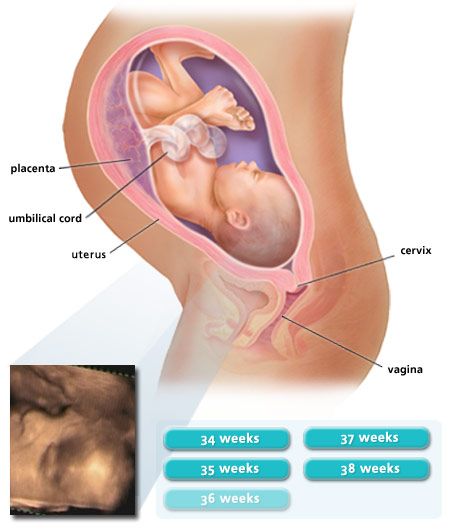
Read also:
Contraindications for training in the third trimester
A set of exercises in the third trimester with fitball
Preparation for childbirth. Kegel exercises
Material approved by doctor Oksana Negrich.
All doctor's articles.
Last reviews
Average customer rating
277 customer ratings
Snapshot of community ratings
- 5 119
- four 40
- 3 38
- 2 40
- one 40
36 weeks of pregnancy what happens to the fetus
During this period, the fetus begins direct preparation for the moment of childbirth and adaptation to the next period of life takes place. In a woman, this period is different in that she can start giving birth at any time.
For the first births, as a rule, the onset is likely to occur at a later period, after thirty-eight weeks.
During this period, a pregnant woman begins the last month of pregnancy, so this is the beginning of a very serious period for her. Since normally, childbirth can begin in a pregnant woman from the thirty-seventh to forty-second weeks, there are only a few days or weeks left before the onset of labor, so it is necessary to plan the place where the birth will take place, it makes sense to get acquainted with a specialist who will deal with childbirth.
Since the unborn child is large and it is quite crowded in the uterus, he moves less often. But there should be at least ten movements in twelve hours of observation. Supervision by a specialist is especially important in breech presentation of the fetus.
Since labor can begin at any time, it is advisable that the woman has all the necessary things for childbirth.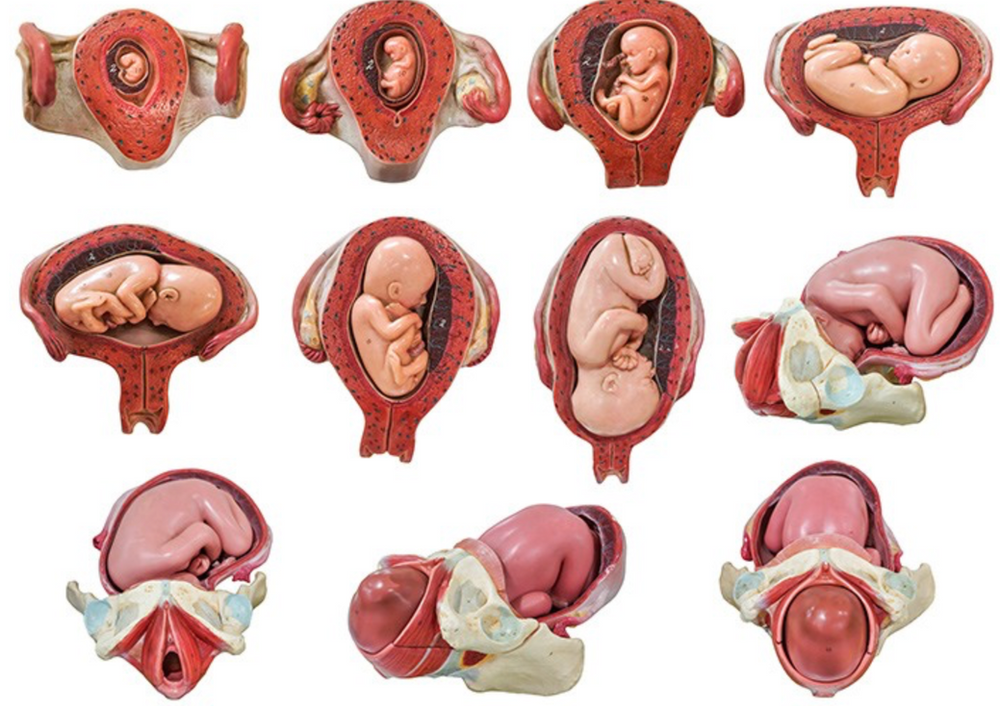
During this period, a woman's belly is so large that it is difficult for her to find comfortable positions for sleeping and resting. She often has back pain. Fetal movements can be perceived as very strong blows to the lower abdomen, to the liver or under the ribs. A woman may feel that her stomach is sinking, after which, subjectively, it becomes easier for her to breathe. This may be a harbinger of a very early onset of labor. After a pregnant woman's stomach sank, most often she disappears the unpleasant sensation that haunted her during pregnancy - heartburn. During this period, frequent lack of sleep begins, as it can be difficult for a woman to find a comfortable position for sleeping. At night, frequent urges to the toilet may disturb.
The weight of the unborn child during this period is usually 2600-2800 g. If this figure is higher, the expectant mother should pay attention to the diet.
It should be borne in mind that during the thirty-sixth week, labor can begin and they can end with the birth of a completely healthy baby.