High blood pressure towards end of pregnancy
High Blood Pressure During Pregnancy
- What are high blood pressure complications during pregnancy?
- What should I do if I have high blood pressure before, during, or after pregnancy?
- What are types of high blood pressure conditions before, during, and after pregnancy?
- More Information
Some women have high blood pressure during pregnancy. This can put the mother and her baby at risk for problems during the pregnancy. High blood pressure can also cause problems during and after delivery.1,2 The good news is that high blood pressure is preventable and treatable.
High blood pressure, also called hypertension, is very common. In the United States, high blood pressure happens in 1 in every 12 to 17 pregnancies among women ages 20 to 44.3
High blood pressure in pregnancy has become more common. However, with good blood pressure control, you and your baby are more likely to stay healthy.
The most important thing to do is talk with your health care team about any blood pressure problems so you can get the right treatment and control your blood pressure—before you get pregnant. Getting treatment for high blood pressure is important before, during, and after pregnancy.
What are high blood pressure complications during pregnancy?
Complications from high blood pressure for the mother and infant can include the following:
- For the mother: preeclampsia, eclampsia, stroke, the need for labor induction (giving medicine to start labor to give birth), and placental abruption (the placenta separating from the wall of the uterus).1,4,5
- For the baby: preterm delivery (birth that happens before 37 weeks of pregnancy) and low birth weight (when a baby is born weighing less than 5 pounds, 8 ounces).1,6 The mother’s high blood pressure makes it more difficult for the baby to get enough oxygen and nutrients to grow, so the mother may have to deliver the baby early.
Discuss blood pressure problems with your health care team before, during, and after pregnancy.
Learn what to do if you have high blood pressure before, during, or after pregnancy.
What should I do if I have high blood pressure before, during, or after pregnancy?
Before Pregnancy
- Make a plan for pregnancy and talk with your doctor or health care team about the following:
- Any health problems you have or had and any medicines you are taking. If you are planning to become pregnant, talk to your doctor.7 Your doctor or health care team can help you find medicines that are safe to take during pregnancy.
- Ways to keep a healthy weight through healthy eating and regular physical activity.1,7
During Pregnancy
- Get early and regular prenatal care. Go to every appointment with your doctor or health care professional.
- Talk to your doctor about any medicines you take and which ones are safe.
 Do not stop or start taking any type of medicine, including over-the-counter medicines, without first talking with your doctor.7
Do not stop or start taking any type of medicine, including over-the-counter medicines, without first talking with your doctor.7 - Keep track of your blood pressure at home with a home blood pressure monitor. Contact your doctor if your blood pressure is higher than usual or if you have symptoms of preeclampsia. Talk to your doctor or insurance company about getting a home monitor.
- Continue to choose healthy foods and keep a healthy weight.8
After Pregnancy
- Pay attention to how you feel after you give birth. If you had high blood pressure during pregnancy, you have a higher risk for stroke and other problems after delivery. Tell your doctor or call 9-1-1 right away if you have symptoms of preeclampsia after delivery. You might need emergency medical care.9,10
What are types of high blood pressure conditions before, during, and after pregnancy?
Your doctor or nurse should look for these conditions before, during, and after pregnancy:1,11
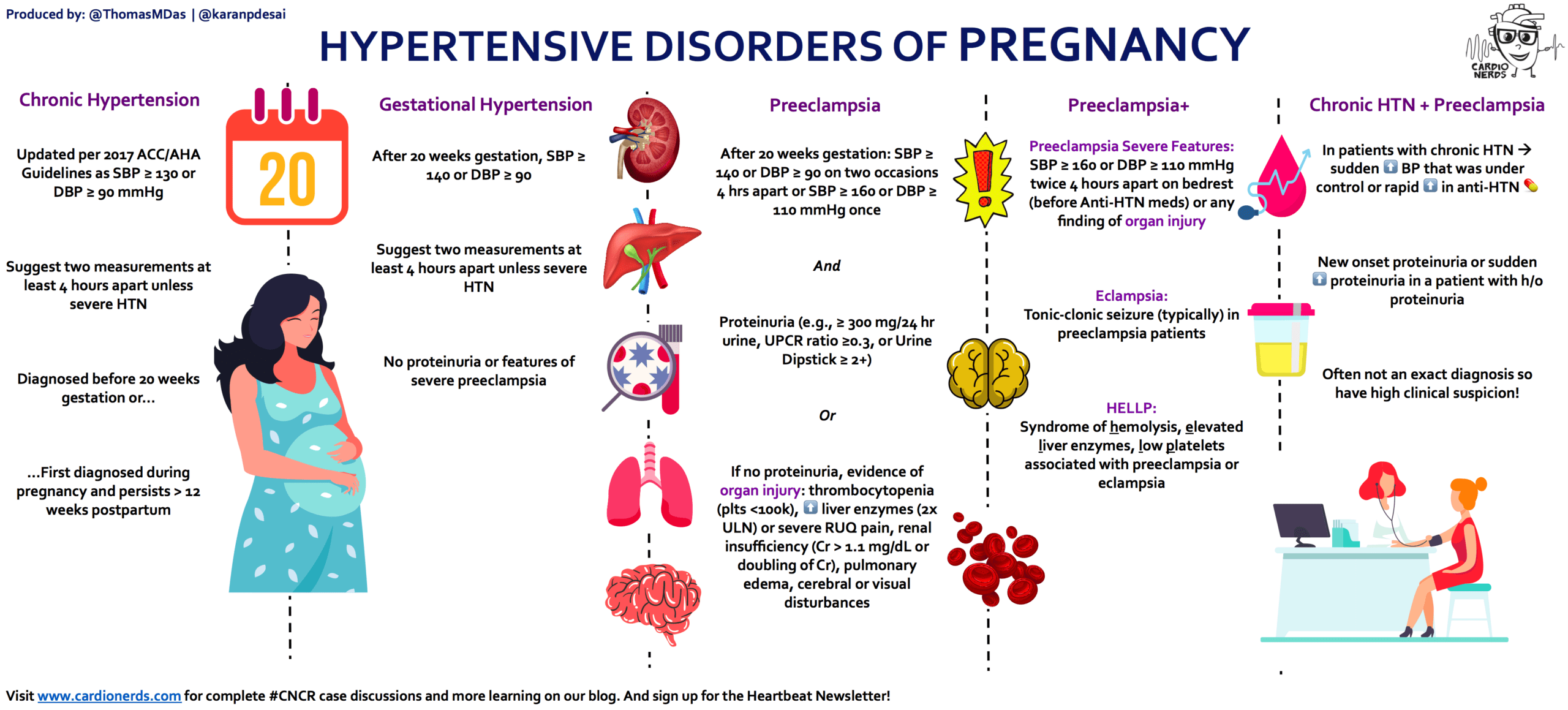
Chronic Hypertension
Chronic hypertension means having high blood pressure* before you get pregnant or before 20 weeks of pregnancy.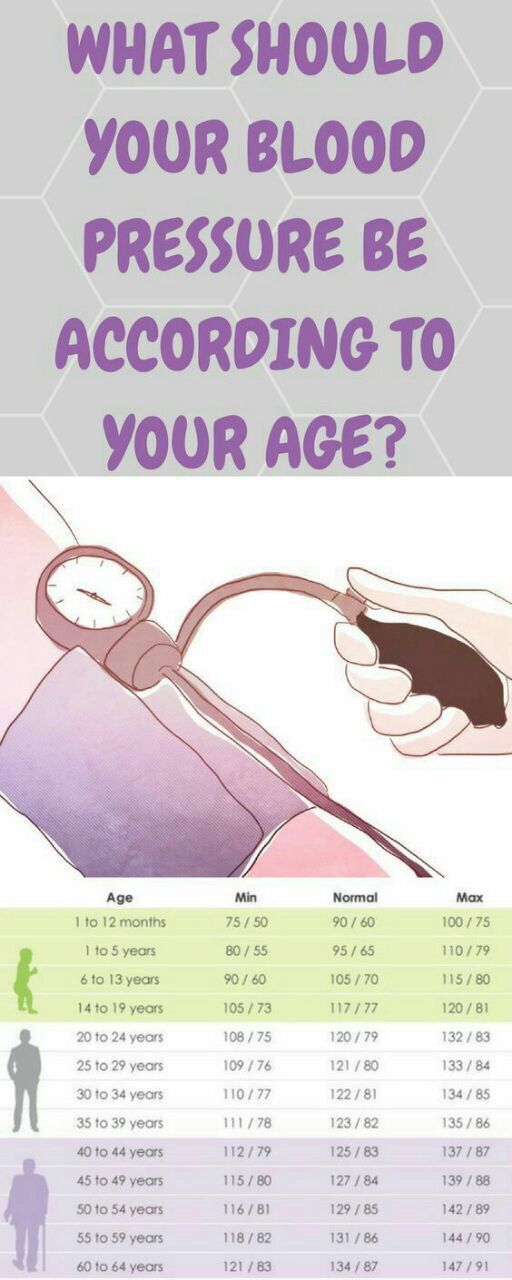 1 Women who have chronic hypertension can also get preeclampsia in the second or third trimester of pregnancy.1
1 Women who have chronic hypertension can also get preeclampsia in the second or third trimester of pregnancy.1
Gestational Hypertension
This condition happens when you only have high blood pressure* during pregnancy and do not have protein in your urine or other heart or kidney problems. It is typically diagnosed after 20 weeks of pregnancy or close to delivery. Gestational hypertension usually goes away after you give birth. However, some women with gestational hypertension have a higher risk of developing chronic hypertension in the future.1,12
Preeclampsia/Eclampsia
Preeclampsia happens when a woman who previously had normal blood pressure suddenly develops high blood pressure* and protein in her urine or other problems after 20 weeks of pregnancy. Women who have chronic hypertension can also get preeclampsia.
Preeclampsia happens in about 1 in 25 pregnancies in the United States.1,13 Some women with preeclampsia can develop seizures. This is called eclampsia, which is a medical emergency.1,11
This is called eclampsia, which is a medical emergency.1,11
Symptoms of preeclampsia include:
- A headache that will not go away
- Changes in vision, including blurry vision, seeing spots, or having changes in eyesight
- Pain in the upper stomach area
- Nausea or vomiting
- Swelling of the face or hands
- Sudden weight gain
- Trouble breathing
Some women have no symptoms of preeclampsia, which is why it is important to visit your health care team regularly, especially during pregnancy.
You are more at risk for preeclampsia if:1
- This is the first time you have given birth.
- You had preeclampsia during a previous pregnancy.
- You have chronic (long-term) high blood pressure, chronic kidney disease, or both.
- You have a history of thrombophilia (a condition that increases risk of blood clots).
- You are pregnant with multiple babies (such as twins or triplets).

- You became pregnant using in vitro fertilization.
- You have a family history of preeclampsia.
- You have type 1 or type 2 diabetes.
- You have obesity.
- You have lupus (an autoimmune disease).
- You are older than 40.
In rare cases, preeclampsia can happen after you have given birth. This is a serious medical condition known as postpartum preeclampsia. It can happen in women without any history of preeclampsia during pregnancy.14 The symptoms for postpartum preeclampsia are similar to the symptoms of preeclampsia. Postpartum preeclampsia is typically diagnosed within 48 hours after delivery but can happen up to 6 weeks later.9
Tell your health care provider or call 9-1-1 right away if you have symptoms of postpartum preeclampsia. You might need emergency medical care.9,10
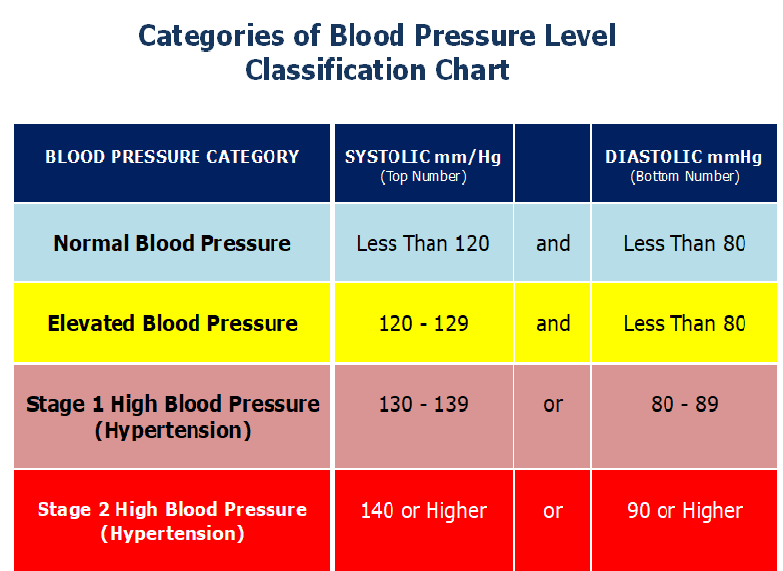
*In November 2017, the American College of Cardiology (ACC) and the American Heart Association (AHA) updated the definition of chronic stage 2 hypertension to mean having blood pressure at or above 140/90 mmHg.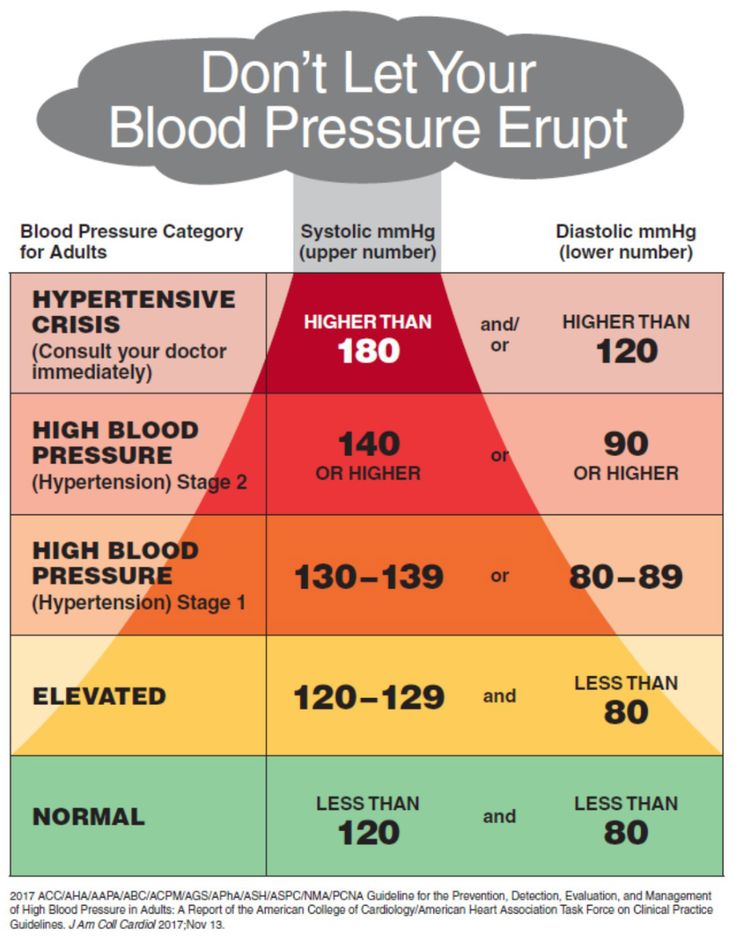 15 The American College of Obstetricians and Gynecologists’ recommendations on hypertension in pregnancy predate the 2017 ACC/AHA’s guideline and definition of hypertension and stage 2 hypertension.
15 The American College of Obstetricians and Gynecologists’ recommendations on hypertension in pregnancy predate the 2017 ACC/AHA’s guideline and definition of hypertension and stage 2 hypertension.
High Blood Pressure in Pregnancy | Preeclampsia
On this page
Basics
- Summary
- Start Here
- Symptoms
- Diagnosis and Tests
- Treatments and Therapies
Learn More
- Related Issues
- Specifics
- Genetics
See, Play and Learn
- Videos and Tutorials
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
What is high blood pressure in pregnancy?
Blood pressure is the force of your blood pushing against the walls of your arteries as your heart pumps blood. High blood pressure, or hypertension, is when this force against your artery walls is too high. There are different types of high blood pressure in pregnancy:
High blood pressure, or hypertension, is when this force against your artery walls is too high. There are different types of high blood pressure in pregnancy:
- Gestational hypertension is high blood pressure that you develop while you are pregnant. It starts after you are 20 weeks pregnant. You usually don't have any other symptoms. In many cases, it does not harm you or your baby, and it goes away within 12 weeks after childbirth. But it does raise your risk of high blood pressure in the future. It sometimes can be severe, which may lead to low birth weight or preterm birth. Some women with gestational hypertension do go on to develop preeclampsia.
- Chronic hypertension is high blood pressure that started before the 20th week of pregnancy or before you became pregnant. Some women may have had it long before becoming pregnant but didn't know it until they got their blood pressure checked at their prenatal visit. Sometimes chronic hypertension can also lead to preeclampsia.
- Preeclampsia is a sudden increase in blood pressure after the 20th week of pregnancy. It usually happens in the last trimester. In rare cases, symptoms may not start until after delivery. This is called postpartum preeclampsia. Preeclampsia also includes signs of damage to some of your organs, such as your liver or kidney. The signs may include protein in the urine and very high blood pressure. Preeclampsia can be serious or even life-threatening for both you and your baby.
What causes preeclampsia?
The cause of preeclampsia is unknown.
Who is at risk for preeclampsia?
You are at higher risk of preeclampsia if you:
- Had chronic high blood pressure or chronic kidney disease before pregnancy
- Had high blood pressure or preeclampsia in a previous pregnancy
- Have obesity
- Are over age 40
- Are pregnant with more than one baby
- Are African American
- Have a family history of preeclampsia
- Have certain health conditions, such as diabetes, lupus, or thrombophilia (a disorder which raises your risk of blood clots)
- Used in vitro fertilization, egg donation, or donor insemination
What problems can preeclampsia cause?
Preeclampsia can cause:
- Placental abruption, where the placenta separates from the uterus
- Poor fetal growth, caused by a lack of nutrients and oxygen
- Preterm birth
- A low birth weight baby
- Stillbirth
- Damage to your kidneys, liver, brain, and other organ and blood systems
- A higher risk of heart disease for you
- Eclampsia, which happens when preeclampsia is severe enough to affect brain function, causing seizures or coma
- HELLP syndrome, which happens when a woman with preeclampsia or eclampsia has damage to the liver and blood cells.
 It is rare, but very serious.
It is rare, but very serious.
What are the symptoms of preeclampsia?
Possible symptoms of preeclampsia include:
- High blood pressure
- Too much protein in your urine (called proteinuria)
- Swelling in your face and hands. Your feet may also swell, but many women have swollen feet during pregnancy. So swollen feet by themselves may not be a sign of a problem.
- Headache that does not go away
- Vision problems, including blurred vision or seeing spots
- Pain in your upper right abdomen
- Trouble breathing
Eclampsia can also cause seizures, nausea and/or vomiting, and low urine output. If you go on to develop HELLP syndrome, you may also have bleeding or bruising easily, extreme fatigue, and liver failure.
How is preeclampsia diagnosed?
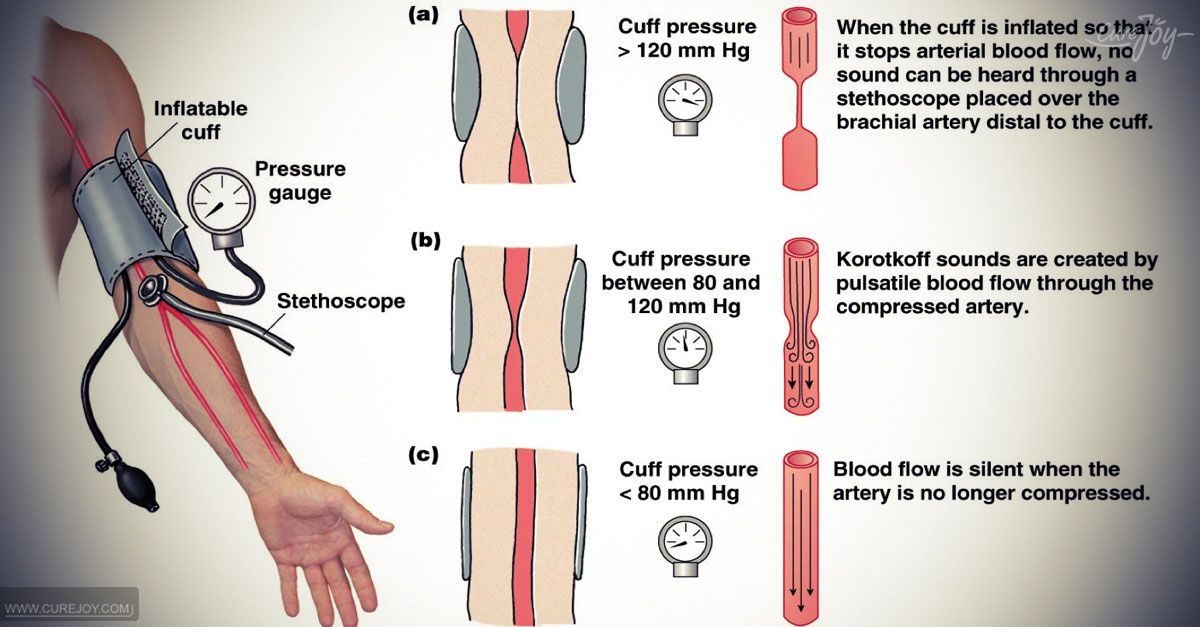
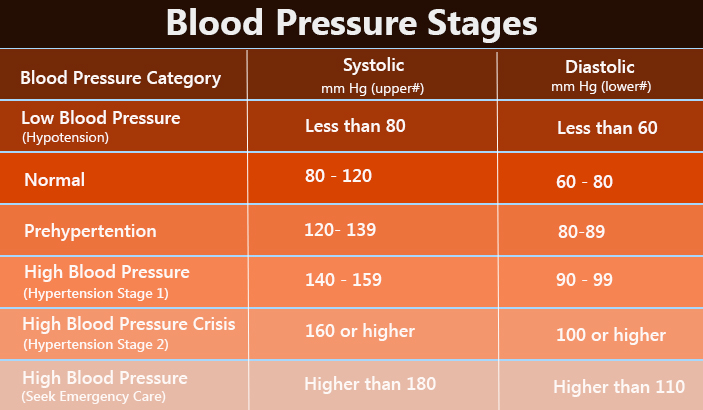
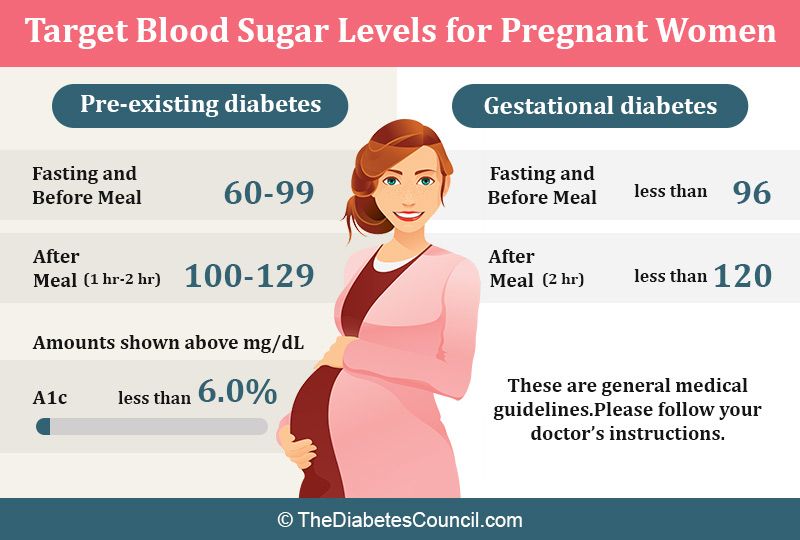
Your health care provider will check your blood pressure and urine at each prenatal visit. If your blood pressure reading is high (140/90 or higher), especially after the 20th week of pregnancy, your provider will likely want to run some tests.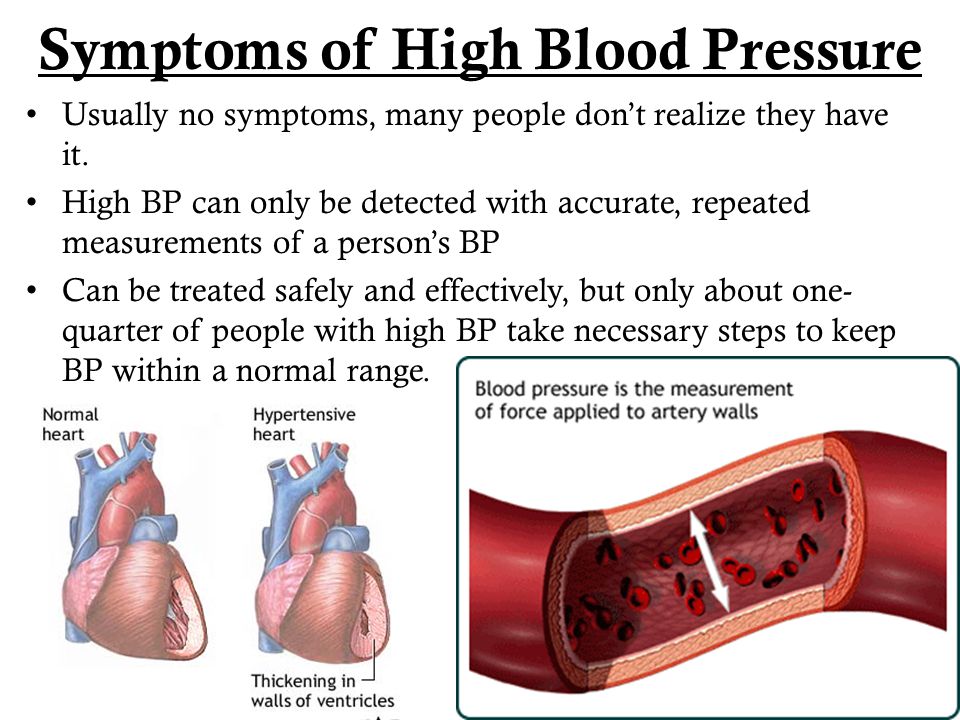 They may include blood tests other lab tests to look for extra protein in the urine as well as other symptoms.
They may include blood tests other lab tests to look for extra protein in the urine as well as other symptoms.
What are the treatments for preeclampsia?
Delivering the baby can often cure preeclampsia. When making a decision about treatment, your provider take into account several factors. They include how severe it is, how many weeks pregnant you are, and what the potential risks to you and your baby are:
- If you are more than 37 weeks pregnant, your provider will likely want to deliver the baby.
- If you are less than 37 weeks pregnant, your health care provider will closely monitor you and your baby. This includes blood and urine tests for you. Monitoring for the baby often involves ultrasound, heart rate monitoring, and checking on the baby's growth. You may need to take medicines, to control your blood pressure and to prevent seizures. Some women also get steroid injections, to help the baby's lungs mature faster. If the preeclampsia is severe, you provider may want you to deliver the baby early.

The symptoms usually go away within 6 weeks of delivery. In rare cases, symptoms may not go away, or they may not start until after delivery (postpartum preeclampsia). This can be very serious, and it needs to be treated right away.
- About Preeclampsia and Eclampsia (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- High Blood Pressure and Pregnancy (Mayo Foundation for Medical Education and Research) Also in Spanish
- High Blood Pressure during Pregnancy (American Academy of Family Physicians) Also in Spanish
- High Blood Pressure during Pregnancy (March of Dimes Birth Defects Foundation)
- What Are the Symptoms of Preeclampsia, Eclampsia, and HELLP Syndrome? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- How Do Health Care Providers Diagnose Preeclampsia, Eclampsia, and HELLP Syndrome? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Magnesium Blood Test (National Library of Medicine) Also in Spanish
- What Are the Treatments for Preeclampsia, Eclampsia, and HELLP Syndrome? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- HELLP Syndrome (American Academy of Family Physicians) Also in Spanish
- What Are the Risks of Preeclampsia and Eclampsia to the Fetus? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Risks of Preeclampsia and Eclampsia to the Mother? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Postpartum Preeclampsia (American Academy of Family Physicians) Also in Spanish
- High Blood Pressure During Pregnancy (Centers for Disease Control and Prevention)
- Who Is at Risk of Preeclampsia? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- ClinicalTrials.
 gov: Hypertension, Pregnancy-Induced (National Institutes of Health)
gov: Hypertension, Pregnancy-Induced (National Institutes of Health) - ClinicalTrials.gov: Pre-Eclampsia (National Institutes of Health)
- Article: Clinical-epidemiological characteristics and maternal-foetal outcomes in pregnant women hospitalised with COVID-19.
 ..
.. - Article: Antepartum and intrapartum stillbirth rates across gestation: a cross-sectional study using...
- Article: The association of serum total bile acid with new-onset hypertension during.
 ..
.. - High Blood Pressure in Pregnancy -- see more articles
- Find an Ob-Gyn (American College of Obstetricians and Gynecologists)
- National Heart, Lung, and Blood Institute
Hypertension in pregnancy
High blood pressure during pregnancy
Changes in blood pressure (BP) in women during pregnancy are observed quite often, which can adversely affect the mother and fetus. Blood pressure is one of the most important indicators of the functioning of the circulatory system in the body. During pregnancy, all organs and systems of the mother work with increased stress, especially the cardiovascular system. Therefore, it is necessary to regularly measure blood pressure to prevent the development of severe complications. At the beginning of pregnancy, blood pressure, as a rule, decreases slightly, which is associated with the action of hormones. In later pregnancy, as the fetus grows and blood flow increases to feed it, blood pressure may increase relative to pre-pregnancy physiological values. Hypertension is said to occur when a pregnant woman's blood pressure exceeds 140/9.0 mmHg However, in women with low blood pressure before pregnancy, arterial hypertension may be at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
Blood pressure is one of the most important indicators of the functioning of the circulatory system in the body. During pregnancy, all organs and systems of the mother work with increased stress, especially the cardiovascular system. Therefore, it is necessary to regularly measure blood pressure to prevent the development of severe complications. At the beginning of pregnancy, blood pressure, as a rule, decreases slightly, which is associated with the action of hormones. In later pregnancy, as the fetus grows and blood flow increases to feed it, blood pressure may increase relative to pre-pregnancy physiological values. Hypertension is said to occur when a pregnant woman's blood pressure exceeds 140/9.0 mmHg However, in women with low blood pressure before pregnancy, arterial hypertension may be at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
Why is high blood pressure dangerous during pregnancy?
High blood pressure during pregnancy poses a great danger to the mother and fetus. Against this background, vasoconstriction occurs and the blood supply to all vital organs, including the placenta, is disturbed. Due to the lack of essential nutrients and oxygen, the process of growth and development of the fetus slows down. There is a serious danger of placental abruption, which is accompanied by bleeding and threatens the life of the mother and fetus. High blood pressure during pregnancy can lead to the development of a dangerous pregnancy complication - preeclampsia. Edema, large weight gain, and the presence of protein in the urine can also be a manifestation of preeclampsia. Very dangerous symptoms of preeclampsia are: headache, blurred vision ("flies", "veil" before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, vomiting. Pre-eclampsia can provoke a formidable complication - eclampsia. In this condition, the pregnant woman loses consciousness and convulsions occur.
Against this background, vasoconstriction occurs and the blood supply to all vital organs, including the placenta, is disturbed. Due to the lack of essential nutrients and oxygen, the process of growth and development of the fetus slows down. There is a serious danger of placental abruption, which is accompanied by bleeding and threatens the life of the mother and fetus. High blood pressure during pregnancy can lead to the development of a dangerous pregnancy complication - preeclampsia. Edema, large weight gain, and the presence of protein in the urine can also be a manifestation of preeclampsia. Very dangerous symptoms of preeclampsia are: headache, blurred vision ("flies", "veil" before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, vomiting. Pre-eclampsia can provoke a formidable complication - eclampsia. In this condition, the pregnant woman loses consciousness and convulsions occur.
Register for pregnancy at the antenatal clinic as early as possible!
A very important feature of arterial hypertension during pregnancy is that often even with high blood pressure numbers, the patient feels normal.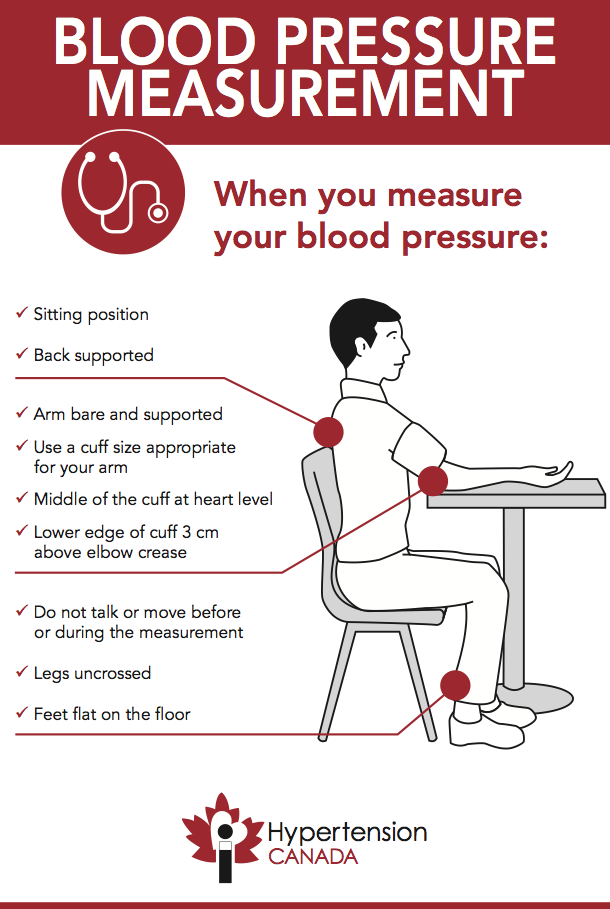 High blood pressure is detected by chance, at the next appearance in the antenatal clinic. The absence of clinical manifestations of elevated blood pressure does not exclude the development of dangerous complications.
High blood pressure is detected by chance, at the next appearance in the antenatal clinic. The absence of clinical manifestations of elevated blood pressure does not exclude the development of dangerous complications.
In order to detect unwanted deviations during pregnancy in time and prevent the development of complications in the mother and fetus, pregnant women need to regularly monitor their blood pressure. It is very important to register for pregnancy in a antenatal clinic in a timely manner. The doctor will promptly detect changes in blood pressure and prescribe the optimal therapy to maintain blood pressure in the normal range. If a woman had high blood pressure before pregnancy, and she is taking medications, it is necessary to adjust the treatment and individually select the drugs that can be taken during pregnancy. To prevent high blood pressure, a pregnant woman should eat a healthy and balanced diet, observe a drinking regimen, and monitor weight gain. The correct recommendations on these issues will also be given by the doctor of the antenatal clinic.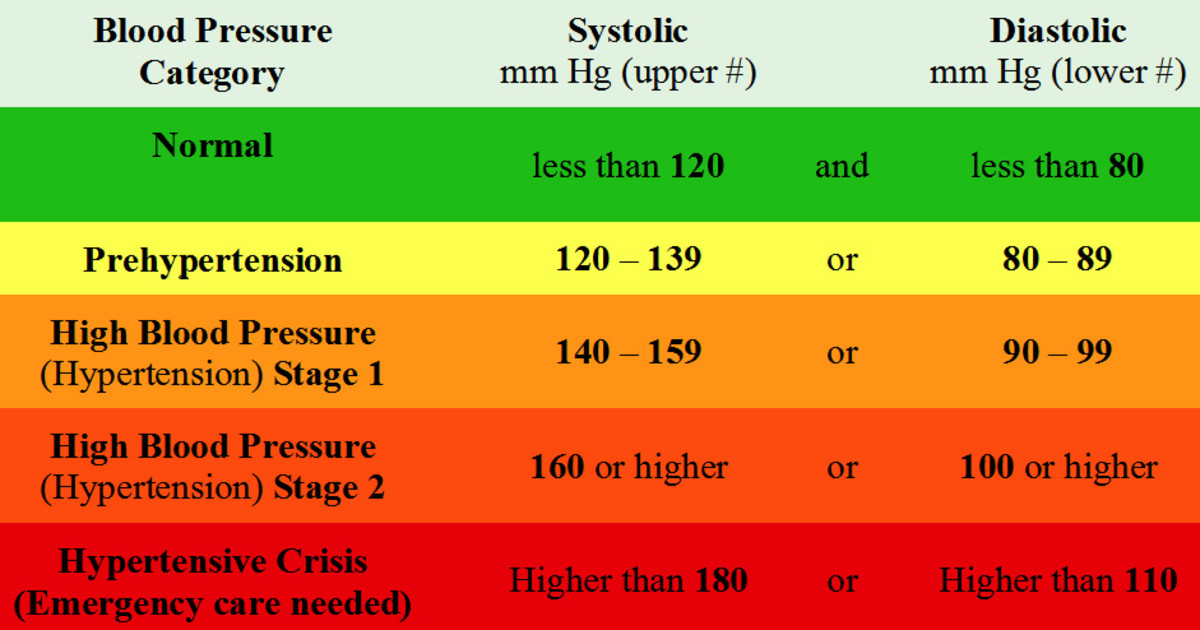 A pregnant woman must follow the recommendations and not violate the prescribed therapy.
A pregnant woman must follow the recommendations and not violate the prescribed therapy.
What to do if a pregnant woman has high blood pressure?
If a pregnant woman regularly monitors blood pressure on her own and notes even a slight increase with good health, she should visit the doctor of the antenatal clinic as soon as possible (before the scheduled next visit). Self-administration of drugs in this case is strictly prohibited. Before visiting a doctor, you can reduce blood pressure by taking a mild sedative based on motherwort or valerian.
If necessary, you can consult with an obstetrician-gynecologist of the remote medical advisory panel of the Ambulance and Emergency Medical Care Station. A.S. Puchkov, Moscow by phone: (495) 620-42-44.
When is it necessary to call an ambulance?
If blood pressure rises suddenly, you feel unwell, urgent hospitalization is necessary, and it is advisable for the patient to immediately call an ambulance team. Such signs as: headache, feeling of flashing dots or "flies", a veil before the eyes, pain in the upper abdomen, nausea, vomiting, agitation or depression, along with this - an increase in blood pressure should alert. There may be a high convulsive readiness, which is manifested by twitching of the muscles of the face, neck, upper limbs, loss of consciousness, convulsions are possible.
Such signs as: headache, feeling of flashing dots or "flies", a veil before the eyes, pain in the upper abdomen, nausea, vomiting, agitation or depression, along with this - an increase in blood pressure should alert. There may be a high convulsive readiness, which is manifested by twitching of the muscles of the face, neck, upper limbs, loss of consciousness, convulsions are possible.
What to do before the ambulance arrives?
First of all, go to bed, if possible, eliminate all unwanted irritants (turn off all sources of noise, close the curtains), do not leave the pregnant woman alone, as convulsions may occur and help will be needed. Give it a position with a raised head end. It is possible to take pressure-lowering drugs prescribed by a doctor. If a woman has not previously taken antihypertensive drugs, then drugs should not be taken on the advice of others.
If an attack of convulsions occurs, the pregnant woman should be laid on a flat surface, turn her head to the side (to prevent aspiration of vomit), protect from damage (cover with a blanket), do not hold physically.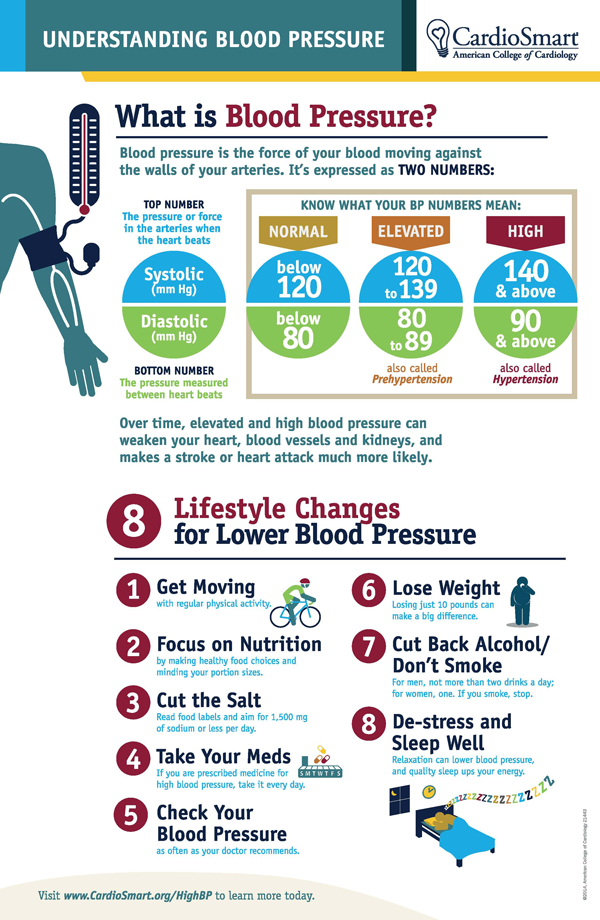 After an attack, clean the oral cavity with a napkin from vomit, blood and mucus. Wait for the ambulance to arrive!
After an attack, clean the oral cavity with a napkin from vomit, blood and mucus. Wait for the ambulance to arrive!
The ambulance will arrive quickly and provide the necessary assistance. Hospitalization in this condition is mandatory. Only in a hospital is it possible to fully monitor the condition of the mother and child, complete therapy and determine the delivery plan.
We wish you health and happy motherhood!
Chief Specialist
in Obstetrics and Gynecology Arkhipova N.L.
Is it safer to induce labor immediately or wait if the mother has elevated but not persistently high blood pressure after 34 weeks of pregnancy?
What is the problem?
Women with high blood pressure (hypertension) during pregnancy or who develop preeclampsia (high blood pressure with protein in the urine or involvement of other organs or systems, or both) can develop serious complications. Possible maternal complications include worsening preeclampsia, seizures and eclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count), placental abruption, liver failure, kidney failure, and breathing problems due to fluid buildup in the lungs. .
.
Delivery usually prevents worsening of hypertension, but a premature baby has other health problems, such as respiratory problems due to lung immaturity. Inducing labor can lead to overstimulation of contractions and fetal distress. Another option is to wait for natural childbirth, carefully monitoring the condition of the mother and child.
Why is this important?
Because there are benefits and risks to both planned preterm birth and expectant management when the mother has high blood pressure towards the end of pregnancy, we wanted to know which was the safest strategy. We reviewed clinical trials that compared planned preterm delivery by induced labor versus caesarean section versus expectant management.
What evidence did we find?
We searched for evidence up to 12 January 2016 and found five randomized trials involving 1819 women. The two studies were large and of high quality and included 704 women with gestational hypertension, mild preeclampsia, or exacerbation of existing hypertension at 34–37 weeks, and 756 pregnant women with hypertension or mild preeclampsia at 36–41 weeks.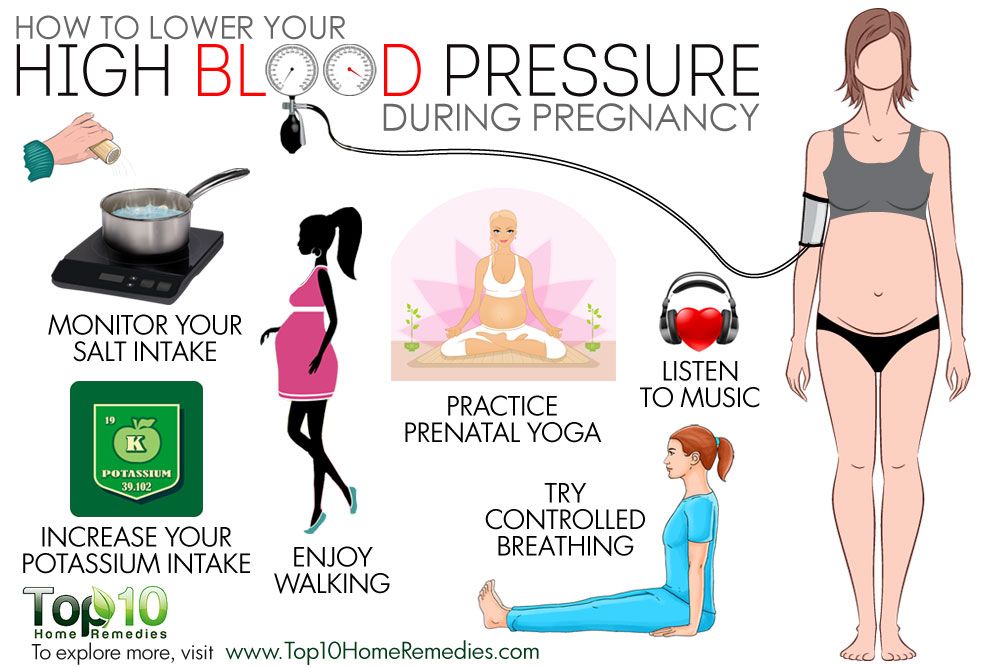 . Few women who had planned preterm births experienced serious adverse outcomes (1459women, high-quality evidence). There was insufficient information to draw any conclusions about the number of children born with poor health and there was a high level of variability between the two studies (1495 infants, low-quality evidence). No difference was found between early planned births and delayed births in terms of the number of caesarean sections (four studies, 1728 women, moderate quality of evidence), or the length of time mothers spent in hospital after delivery (two studies, 925 women, moderate quality of evidence) (or child (one study, 756 infants, moderate quality of evidence). Most preterm infants had respiratory problems (respiratory distress syndrome, three studies, 1511 infants) or were admitted to the neonatal unit (four studies, 1585 infants). A small number of women who gave birth prematurely developed HELLP syndrome (three studies, 1628 women) or serious kidney problems (one study, 100 women).
. Few women who had planned preterm births experienced serious adverse outcomes (1459women, high-quality evidence). There was insufficient information to draw any conclusions about the number of children born with poor health and there was a high level of variability between the two studies (1495 infants, low-quality evidence). No difference was found between early planned births and delayed births in terms of the number of caesarean sections (four studies, 1728 women, moderate quality of evidence), or the length of time mothers spent in hospital after delivery (two studies, 925 women, moderate quality of evidence) (or child (one study, 756 infants, moderate quality of evidence). Most preterm infants had respiratory problems (respiratory distress syndrome, three studies, 1511 infants) or were admitted to the neonatal unit (four studies, 1585 infants). A small number of women who gave birth prematurely developed HELLP syndrome (three studies, 1628 women) or serious kidney problems (one study, 100 women).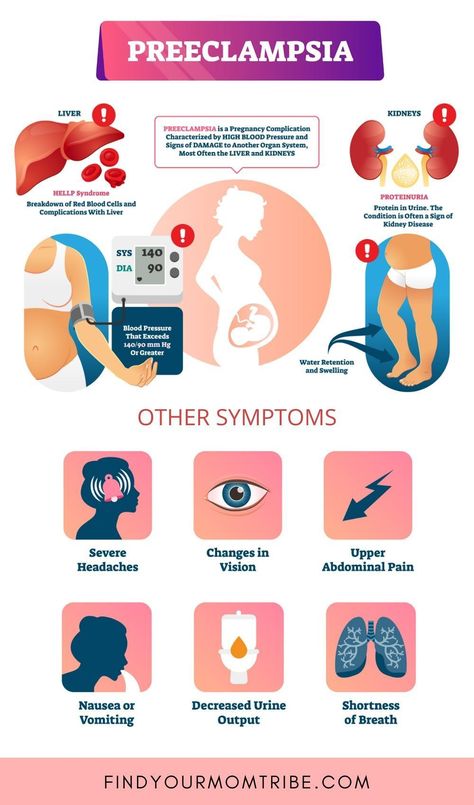
Two studies compared women with preterm labor at 34 to 36 weeks and 34 to 37 weeks of gestation with a control group who followed up to 37 weeks when labor was induced if it did not start spontaneously. Three studies compared women in induced labor with a normal or near-normal duration of pregnancy at 37 completed weeks and between 36 and 41 weeks and women seen before 41 weeks when labor was induced if they didn't start spontaneously. Inclusion and exclusion criteria also differed across the five studies.
Information regarding which study group women belonged to was not withheld from both women and clinicians. Women and staff were made aware of this intervention, which could affect aspects of care and decision making. Most of the evidence was of moderate quality, so we can be relatively confident in the results.
What does this mean?
In general, if labor was induced immediately after 34 weeks of gestation, the risk of complications for the mother was lower and there was generally no apparent difference in the rate of complications for the baby, but information was limited.