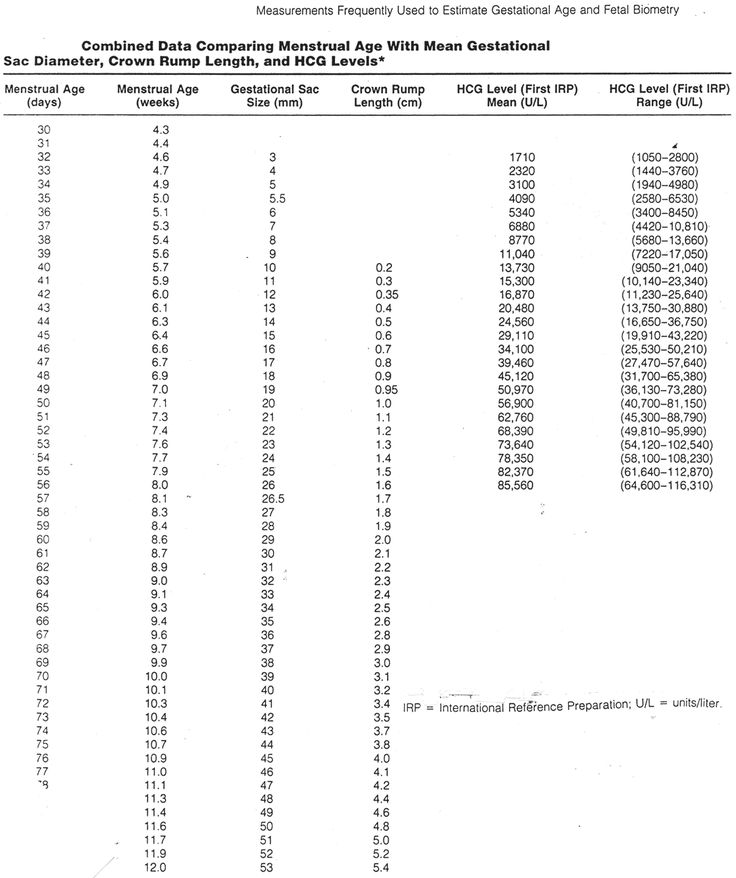
Pregnancy blood levels chart
HCG Levels in Pregnancy & hCG Levels Chart by Week
Human chorionic gonadotropin, or hCG for short, is often referred to as “the pregnancy hormone” because it’s present in large quantities during pregnancy. And it is, after all, the hormone that many at-home pregnancy tests are designed to detect! Find out more about what hCG is, when it’s detectable by at-home pregnancy tests, and what the typical hCG levels are for each of the early weeks of pregnancy.
What Is hCG and When Does Your Body Start Producing It?
Human chorionic gonadotropin (hCG) is known as the pregnancy hormone, as your body produces it in large amounts when you’re pregnant.
Although you can have low levels of hCG in your body at any time, the levels of this hormone tend to rise sharply early on in your pregnancy for two reasons:
About 10 days after conception, the fertilized egg attaches to the lining of your uterus and your body starts to make hCG.
Over the next week or so, hCG levels will increase.
At about 4 weeks pregnant, the egg—now called an embryo—implants further into the uterus and begins to produce even more hCG, which triggers increased productions of other hormones like estrogen and progesterone.
Together, these hormones help build the lining of the uterus and send signals to the ovaries to stop releasing eggs, ultimately stopping your period.
During these early weeks of pregnancy, you may not show any outward signs of being pregnant and you may not even suspect that you’re pregnant! You may, however, experience implantation bleeding when the fertilized egg attaches to the lining of the uterus (as described above). This is normal and may resemble spotting or a light period.
When Can Pregnancy Tests Detect hCG?
Home pregnancy tests often work by detecting hCG in your urine. All of these over-the-counter pregnancy tests work a little differently, so check the instructions in or on the box.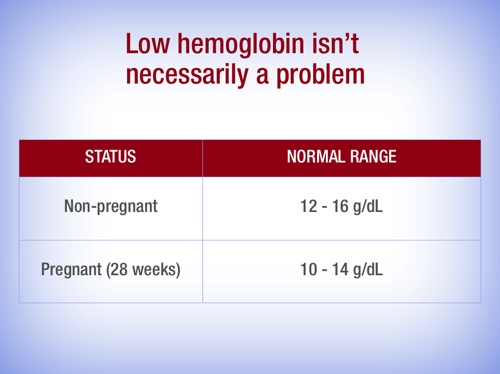 Keep in mind that hCG levels increase over time, so at-home tests are more accurate as your pregnancy progresses. Therefore, a home-pregnancy test that’s taken too early might not detect low levels of hCG and could produce a false negative, meaning the result is negative when you’re actually pregnant.
If you’re wondering when to take an at-home pregnancy test, try one of the following timelines:
Keep in mind that hCG levels increase over time, so at-home tests are more accurate as your pregnancy progresses. Therefore, a home-pregnancy test that’s taken too early might not detect low levels of hCG and could produce a false negative, meaning the result is negative when you’re actually pregnant.
If you’re wondering when to take an at-home pregnancy test, try one of the following timelines:
You might try taking a pregnancy test about three to four weeks after the first day of your last period, as this is when the levels of hCG in your urine will have increased enough to be detectable.
You could wait until around the time you miss your next period, which could be the initial clue that you may be pregnant anyway! By then, the levels of hCG are detectable.
A blood test is the most accurate way to detect hCG levels, because more of the pregnancy hormone is present in the blood than in the urine. Plus, blood tests need less of the hCG hormone to detect a pregnancy, as explained below:
Blood tests.
 Pregnancy blood tests can detect hCG hormone levels as low as 5 to 10 mIU/mL.
Pregnancy blood tests can detect hCG hormone levels as low as 5 to 10 mIU/mL.
Urine tests. At-home urine tests require higher levels of hCG to detect a pregnancy, typically at least 20 mIU/mL.
If your home pregnancy test is positive, your healthcare provider may offer a blood test to check your hCG levels. The results can help your provider confirm your pregnancy and determine how far along you are.
If you’ve just found out you’re pregnant, you can get an estimate of your due date with our Due Date Calculator using either the date of conception or the date of the first day of your last menstrual period!
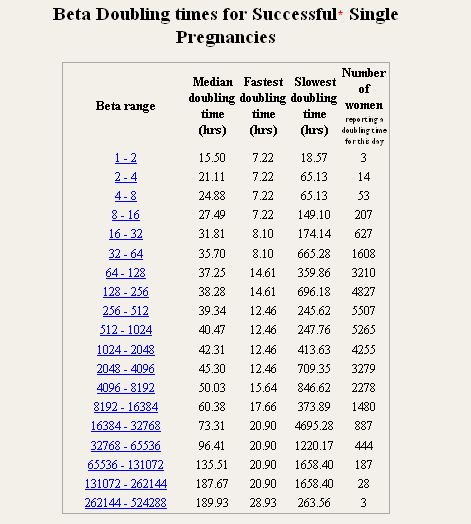
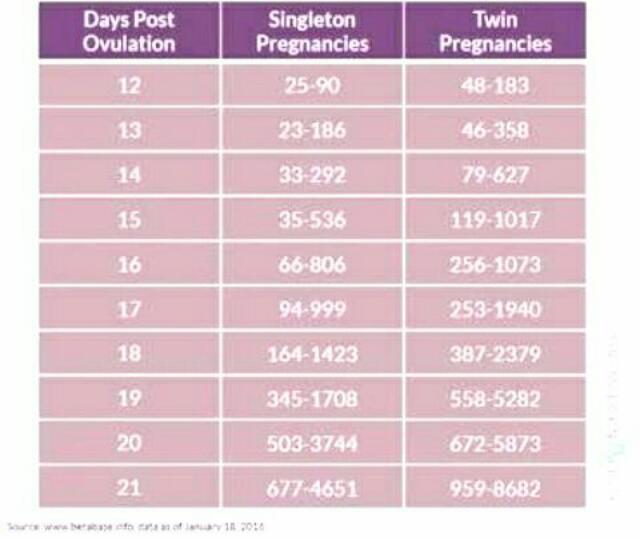
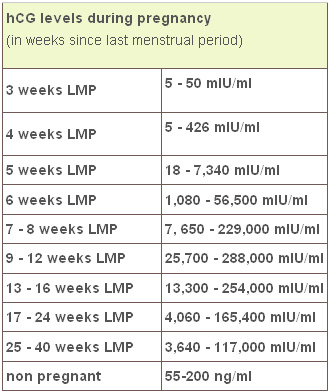
hCG Levels Chart by Week
The week-by-week chart below will give you an idea of how your hCG levels may rise during the first trimester, and then dip slightly during the second trimester. Keep in mind that, if you want your hCG blood test results explained in more detail, your healthcare provider is the best person to ask.
What Does It Mean if You Have High or Low hCG Levels?
It’s important to remember that every pregnancy is different, and you may have lower or higher levels of hCG hormone than what’s indicated in the week-by-week chart above. Most likely, there’s no cause for concern, but your healthcare provider will help you understand what these levels mean.
Low Levels of hCG
Low levels of hCG are normal for non-pregnant women and men. Normally, hCG levels would be less than 5 mIU/mL and less than 2 mIU/mL, respectively, for these groups. If you’re pregnant and experience low hCG levels, it’s important to look at your entire pregnancy as a whole. Your healthcare provider will consider all the factors of your pregnancy to determine why you might be experiencing lower-than-normal levels of hCG. If your provider suspects anything like an ectopic pregnancy, they may perform additional tests to rule it out.
High Levels of hCG
Likewise, high levels of the hCG hormone might not indicate anything out of the ordinary. However, a higher-than-normal level of hCG may be a sign that you’re having twins or triplets! Again, your healthcare provider will work with you to determine an appropriate course of action, if any is needed.
Lower- or higher-than-normal levels of the hCG hormone during your pregnancy might not indicate anything unusual. However, it’s always a good idea to follow up with your healthcare provider as a precaution, regardless of any questions or concerns you have. Read more about other pregnancy symptoms not to ignore.
However, a higher-than-normal level of hCG may be a sign that you’re having twins or triplets! Again, your healthcare provider will work with you to determine an appropriate course of action, if any is needed.
Lower- or higher-than-normal levels of the hCG hormone during your pregnancy might not indicate anything unusual. However, it’s always a good idea to follow up with your healthcare provider as a precaution, regardless of any questions or concerns you have. Read more about other pregnancy symptoms not to ignore.
The Bottom Line
The hCG hormone plays an important role in your pregnancy, and the changing levels of this hormone are just one of many transformations your body will experience as your baby develops.
Although hormonal changes can make you feel a little off from time to time during your pregnancy, try to take these as reassurance that your baby is growing, and you’re getting closer and closer to the day you finally get to meet them.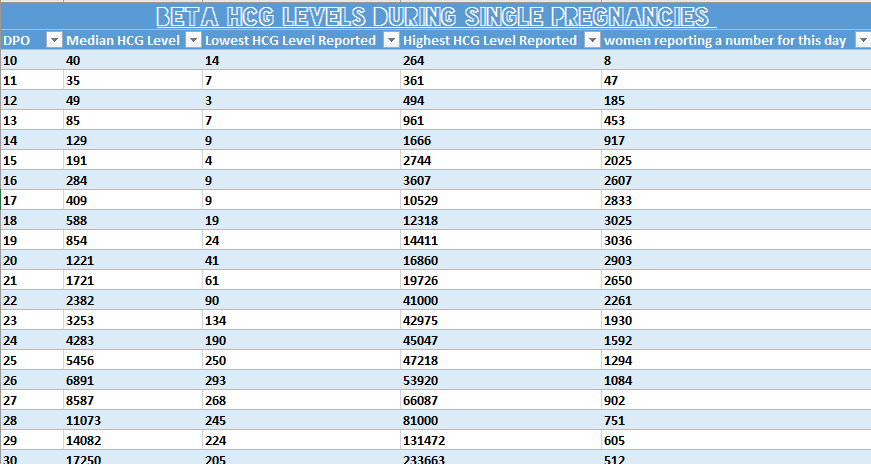 In the meantime, prepare for your baby’s arrival and get rewards on all your diapers and wipes purchases with the Pampers Club app!
Ready to share your pregnancy news with friends and family? Get creative pregnancy announcement ideas in the video below!
In the meantime, prepare for your baby’s arrival and get rewards on all your diapers and wipes purchases with the Pampers Club app!
Ready to share your pregnancy news with friends and family? Get creative pregnancy announcement ideas in the video below!
hCG levels | Pregnancy Birth and Baby
hCG levels | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Human chorionic gonadotropin (hCG) is a hormone normally produced by the placenta. If you are pregnant, you can detect it in your urine. Blood tests measuring hCG levels can also be used to check how well your pregnancy is progressing.
Confirming pregnancy
After you conceive (when the sperm fertilises the egg), the developing placenta begins to produce and release hCG.
It takes about 2 weeks for your hCG levels to be high enough to be detected in your urine using a home pregnancy test.
A positive home test result is almost certainly correct, but a negative result is less reliable.
If you do a pregnancy test on the first day after your missed period, and it’s negative, wait about a week. If you still think you might be pregnant, do the test again or see your doctor.
hCG blood levels by week
If your doctor needs more information about your hCG levels, they may order a blood test. Low levels of hCG may be detected in your blood around 8 to 11 days after conception. hCG levels are highest towards the end of the first trimester, then gradually decline over the rest of your pregnancy.
The average levels of hCG in a pregnant woman’s blood are:
- 3 weeks: 6 – 70 IU/L
- 4 weeks: 10 - 750 IU/L
- 5 weeks: 200 - 7,100 IU/L
- 6 weeks: 160 - 32,000 IU/L
- 7 weeks: 3,700 - 160,000 IU/L
- 8 weeks: 32,000 - 150,000 IU/L
- 9 weeks: 64,000 - 150,000 IU/L
- 10 weeks: 47,000 - 190,000 IU/L
- 12 weeks: 28,000 - 210,000 IU/L
- 14 weeks: 14,000 - 63,000 IU/L
- 15 weeks: 12,000 - 71,000 IU/L
- 16 weeks: 9,000 - 56,000 IU/L
- 16 - 29 weeks (second trimester): 1,400 - 53,000 IUL
- 29 - 41 weeks (third trimester): 940 - 60,000 IU/L
The amount of hCG in your blood can give some information about your pregnancy and the health of your baby.
- Higher than expected levels: you may have multiple pregnancies (for example, twins and triplets) or an abnormal growth in the uterus
- Your hCG levels are falling: you may be having a loss of pregnancy (miscarriage) or risk of miscarriage
- Levels that are rising more slowly than expected: you may have an ectopic pregnancy – where the fertilised egg implants in the fallopian tube
hCG levels and multiple pregnancies
One of the ways of diagnosing a multiple pregnancy is by your hCG levels. A high level may indicate you are carrying multiple babies, but it can also be caused by other factors. You will need an ultrasound to confirm that it’s twins or more.
Levels of hCG in your blood don’t provide a diagnosis of anything. They can only suggest that there are issues to look into.
If you have any concerns about your hCG levels, or wish to know more, speak to your doctor or maternity healthcare professional. You can also call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436.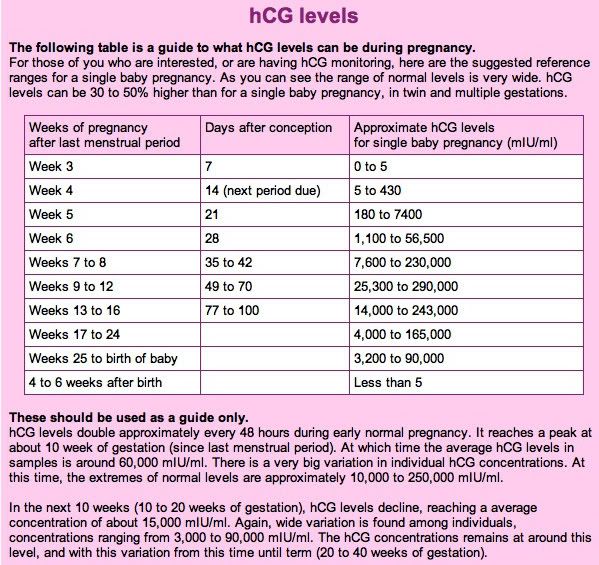
Sources:
NSW Government Health Pathology (hCG factsheet), Lab Tests Online (Human chorionic gonadotropin), UNSW Embryology (Human Chorionic Gonadotropin), Elsevier Patient Education (Human Chorionic Gonadotropin test), SydPath (hCG (human Chorionic Gonadotrophin)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: December 2020
Back To Top
Related pages
- Due date calculator
- Pregnancy tests
- Early signs of pregnancy
Need more information?
Human chorionic gonadotropin - Pathology Tests Explained
Why and when to get tested for hCG
Read more on Pathology Tests Explained website
Pregnancy tests
Find out how a home pregnancy test works.
Read more on Pregnancy, Birth & Baby website
Pregnancy testing - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Beta HCG Test | HealthEngine Blog
A Beta HCG (BHCG or Blood Pregnancy Test) May Be Performed by Your Doctor If They Suspect That You May Be Pregnant, or if You Suspect Pregnancy Yourself!
Read more on HealthEngine website
5 weeks pregnant: Changes for mum
Week 5 of pregnancy is probably when you’ll know that you’re pregnant because your period is missing. There are also subtle changes in your body which are symptoms of pregnancy such as changes to your breasts, and pregnancy symptoms like morning sickness and pregnancy heartburn. These changes are caused by pregnancy hormones, like hCG (human chorionic gonadotropin, produced by the placenta) which is the hormone detected by a pregnancy test.
These changes are caused by pregnancy hormones, like hCG (human chorionic gonadotropin, produced by the placenta) which is the hormone detected by a pregnancy test.
Read more on Parenthub website
4 weeks pregnant: Key points
When you are 4 weeks pregnant your body and your new baby are undergoing rapid changes. The placenta forms and begins producing a hormone called human chorionic gonadotrophin (hCG), which is the substance a pregnancy test detects to confirm you are pregnant. The cells which are growing into your new baby establish membranes which connect them to the placenta and prepare themselves for differentiation into different types of cells, which will occur next week when you are 5 weeks pregnant. These developments may cause you to experience unusual emotions and also cause changes in your body such as darkening of the areolas of your nipples.
Read more on Parenthub website
Week by week pregnancy- 6 weeks pregnant
6 weeks pregnant is a time when embryo development is occurring rapidly and pregnant women often start experiencing pregnancy symptoms like morning sickness. Pregnancy hormone human chorionic gonadotrophin (hCG), the hormone a pregnancy test detects, is usually evident in the woman’s blood in the sixth week of pregnancy. Antenatal care should be provided at a doctor appointment for women who have not already checked their pregnancy health. Find out more about the pregnancy changes which occur this week.
Pregnancy hormone human chorionic gonadotrophin (hCG), the hormone a pregnancy test detects, is usually evident in the woman’s blood in the sixth week of pregnancy. Antenatal care should be provided at a doctor appointment for women who have not already checked their pregnancy health. Find out more about the pregnancy changes which occur this week.
Read more on Parenthub website
5 weeks pregnant: Key points
The fifth week of pregnancy begins around the time your menstrual bleeding is due and is a good time to take a pregnancy test to confirm that you are pregnant. You are also likely to begin experiencing pregnancy symptoms like fatigue, morning sickness and changes to your breasts this week. Your baby is still only about 1.5mm long but it is developing rapidly and taking on a more human form. If you have not already visited your doctor the 5th week of pregnancy is a good time to do so.
Read more on Parenthub website
Molar pregnancy
A molar pregnancy is a type of pregnancy where a baby does not develop. A molar pregnancy can be either complete or partial.
Read more on Pregnancy, Birth & Baby website
Support for Girls - Brave Foundation
Yes, it sounds like in the movies, but food cravings sometimes can be a sign of pregnancy
Read more on Brave Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
The norm of a complete blood count during pregnancy. Hemoglobin, platelets, hematocrit, erythrocytes and leukocytes during pregnancy. Clinical blood test during pregnancy. Hematological changes during pregnancy.
A normal pregnancy is characterized by significant changes in almost all organs and systems to adapt to the requirements of the fetoplacental complex, including changes in blood tests during pregnancy.
Blood test norms during pregnancy: summary of the article
- Significant hematological changes during pregnancy are physiological anemia, neutrophilia, mild thrombocytopenia, increased blood clotting factors and decreased fibrinolysis.
- By 6-12 weeks of gestation, plasma volume increases by approximately 10-15%. The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little.
- Red blood cell count begins to increase at 8-10 weeks of gestation and by the end of pregnancy increases by 20-30% (250-450 ml) of the normal level for non-pregnant women by the end of pregnancy A significant increase in plasma volume relative to the increase in hemoglobin and red blood cell volume leads to moderate decrease in hemoglobin levels (physiological anemia of pregnancy), which is observed in healthy pregnant women.
- Pregnant women may have a slightly lower platelet count than healthy non-pregnant women.
- The neutrophil count begins to rise in the second month of pregnancy and stabilizes in the second or third trimester, at which time the white blood cell count. The absolute number of lymphocytes does not change.
- The level of some blood coagulation factors changes during pregnancy.
This article describes the hematological changes that occur during pregnancy, the most important of which are:
- Increased plasma volume and decreased hematocrit
- Physiological anemia, low hemoglobin
- Elevated white blood cells during pregnancy
- Neutrophilia
- Moderate thrombocytopenia
- Increase in procoagulant factors
- Fibrinolysis reduction
Tests mentioned in the article
How to take blood tests and get a 5% discount? Go to the CIR laboratories online store!
Plasma volume
By 6-12 weeks of pregnancy, the volume of blood plasma increases by about 10-15%.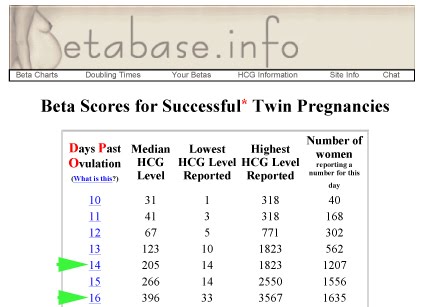 The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little. On average, plasma volume increases by 1100-1600 ml per trimester, and as a result, plasma volume during pregnancy increases to 4700-5200 ml, which is 30 to 50% higher than plasma volume in non-pregnant women.
The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little. On average, plasma volume increases by 1100-1600 ml per trimester, and as a result, plasma volume during pregnancy increases to 4700-5200 ml, which is 30 to 50% higher than plasma volume in non-pregnant women.
During pregnancy, plasma renin activity tends to increase, while the level of atrial natriuretic peptide decreases slightly. This suggests that the increase in plasma volume is caused by insufficiency of the vascular system, which leads to systemic vasodilation (dilation of blood vessels throughout the body) and an increase in vascular capacity. Since it is the volume of blood plasma that initially increases, its effect on the renal and atrial receptors leads to opposite effects on the hormonal background (a decrease in plasma renin activity and an increase in natriuretic peptide). This hypothesis is also supported by the observation that an increase in sodium intake does not lead to a further increase in plasma volume.
Plasma volume immediately decreases after delivery, but rises again 2-5 days later, possibly due to increased aldosterone secretion occurring at this time. Plasma volume then gradually decreases again: 3 weeks postpartum, it is still elevated by 10-15% of the normal level for non-pregnant women, but usually returns to normal by 6 weeks postpartum.
Red blood cells during pregnancy, ESR during pregnancy
The number of red blood cells begins to increase at 8-10 weeks of gestation and by the end of pregnancy increases by 20-30% (250-450 ml) of the normal level for non-pregnant women, especially in women taking drugs iron during pregnancy. Among pregnant women who did not take iron supplements, the number of red blood cells may increase by only 15-20%. The lifespan of red blood cells decreases slightly during a normal pregnancy.
The level of erythropoietin during normal pregnancy increases by 50% and its change depends on the presence of pregnancy complications.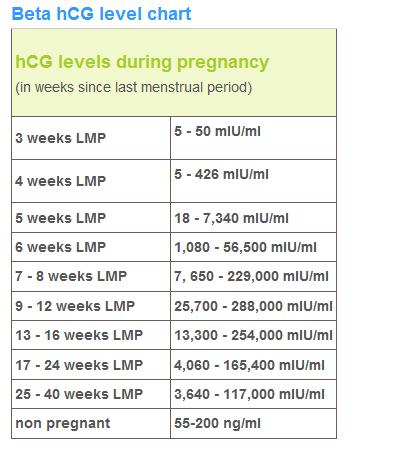 An increase in plasma erythropoietin leads to an increase in the number of red blood cells, which partially provide for the high metabolic oxygen requirements during pregnancy.
An increase in plasma erythropoietin leads to an increase in the number of red blood cells, which partially provide for the high metabolic oxygen requirements during pregnancy.
In women not taking iron supplements, mean red cell volume decreases during pregnancy and averages 80-84 fl in the third trimester. However, in healthy pregnant women and in pregnant women with moderate iron deficiency, the average volume of erythrocytes increases by about 4 fl.
ESR increases during pregnancy, which has no diagnostic value.
Anemia in pregnancy, hemoglobin in pregnancy, hematocrit in pregnancy, low hemoglobin in pregnancy
Decreased hemoglobin in pregnancy
pregnant), which is observed in healthy pregnant women. The biggest difference between the growth rate of blood plasma volume and the number of red blood cells in the maternal circulation is formed during the end of the second, beginning of the third trimester (a decrease in hemoglobin usually occurs at 28-36 weeks of pregnancy). The hemoglobin concentration rises due to the cessation of the increase in plasma volume and the continuation of the increase in the amount of hemoglobin. Conversely, the absence of physiological anemia is a risk factor for stillbirth.
The hemoglobin concentration rises due to the cessation of the increase in plasma volume and the continuation of the increase in the amount of hemoglobin. Conversely, the absence of physiological anemia is a risk factor for stillbirth. Anemia in pregnancy
Defining anemia in pregnant women is difficult because it consists of pregnancy-related changes in plasma volume and red blood cell count, physiological differences in hemoglobin concentration between women and men, and the frequency of iron supplementation during pregnancy.
- The Centers for Disease Prevention and Control defined anemia as hemoglobin levels less than 110 g/L (hematocrit less than 33%) in the first and third trimesters and less than 105 g/L (hematocrit less than 32%) in the second trimester.
- WHO defined anemia in pregnancy as a decrease in hemoglobin less than 110 g/l (11 g/dl) or hematocrit less than 6.83 mmol/l or 33%. Severe anemia in pregnancy is determined by a hemoglobin level of less than 70 g/l and needs medical treatment.
 Very severe anemia is defined as a hemoglobin level of less than 40 g/L and is a medical emergency due to the risk of congestive heart failure.
Very severe anemia is defined as a hemoglobin level of less than 40 g/L and is a medical emergency due to the risk of congestive heart failure.
Women with hemoglobin values below these levels are considered anemic and should undergo routine tests (CBC with peripheral blood smear evaluation, reticulocyte count, serum iron, ferritin, transferrin). If no abnormalities were detected during the examination, then hemoglobin reduced to a level of 100 g / l can be considered physiological anemia with a wide variety of factors affecting the normal level of hemoglobin in a particular person.
Chronic severe anemia is most common among women in developing countries. A decrease in maternal hemoglobin below 60 g / l leads to a decrease in the volume of amniotic fluid, vasodilation of the cerebral vessels of the fetus and a change in the heart rate of the fetus. It also increases the risk of preterm birth, miscarriage, low birth weight and stillbirth. In addition, severe anemia (hemoglobin less than 70 g/l) increases the risk of maternal death.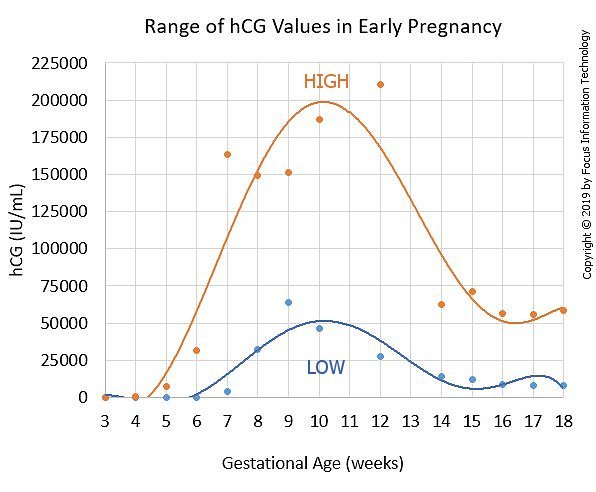 There is no evidence that anemia increases the risk of congenital malformations of the fetus.
There is no evidence that anemia increases the risk of congenital malformations of the fetus.
Severe chronic anemia is usually associated with insufficient iron stores (due to insufficient dietary intake or intestinal worm infestations), folate deficiency (due to insufficient intake and chronic hemolytic conditions such as malaria). Thus, prevention of chronic anemia and improvement of pregnancy outcome is possible with the use of nutritional supplements and the use of infection control measures.
Administering blood and packed red cell transfusions (where safe blood transfusion is available) is a reasonable aggressive treatment for severe anemia, especially if there are signs of fetal hypoxia.
Signs of physiological anemia of pregnancy disappear 6 weeks after delivery, when plasma volume returns to normal.
Iron requirement
In a singleton pregnancy, the iron requirement is 1000 mg per pregnancy: approximately 300 mg for the fetus and placenta and approximately 500 mg, if any, to increase hemoglobin. 200 mg is lost through the intestines, urine and skin. Since most women do not have an adequate supply of iron to meet their needs during pregnancy, iron is usually prescribed as part of a multivitamin, or as a separate element. In general, women taking iron supplements have a 1 g/dL higher hemoglobin concentration than women not taking iron.
200 mg is lost through the intestines, urine and skin. Since most women do not have an adequate supply of iron to meet their needs during pregnancy, iron is usually prescribed as part of a multivitamin, or as a separate element. In general, women taking iron supplements have a 1 g/dL higher hemoglobin concentration than women not taking iron.
Folate requirements
The daily folate requirement for non-pregnant women is 50-100 micrograms. An increase in the number of red blood cells during pregnancy leads to an increase in the need for folic acid, which is provided by increasing the dose of folic acid to 400-800 mcg per day, to prevent neural tube defects in the fetus.
Platelets during pregnancy
In most cases, the platelet count during uncomplicated pregnancy remains within the normal range for non-pregnant women, but it is also possible for pregnant women to have lower platelet counts compared to healthy non-pregnant women. The platelet count begins to rise immediately after childbirth and continues to increase for 3-4 weeks until it returns to normal values.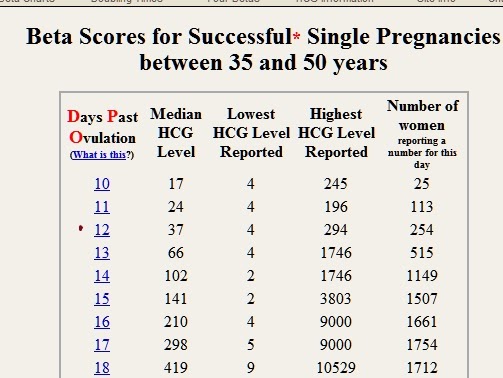
Thrombocytopenia in pregnancy
The most important obstetrical change in platelet physiology during pregnancy is thrombocytopenia, which may be associated with pregnancy complications (severe preeclampsia, HELLP syndrome), drug disorders (immune thrombocytopenia) or may be gestational thrombocytopenia.
Gestational or occasional thrombocytopenia is asymptomatic in the third trimester of pregnancy in patients without prior thrombocytopenia. It is not associated with maternal, fetal, or neonatal complications and resolves spontaneously after delivery. 99/l. The white blood cell count drops to the reference range for non-pregnant women by the sixth day after delivery.
Pregnant women may have a small number of myelocytes and metamyelocytes in the peripheral blood. According to some studies, there is an increase in the number of young forms of neutrophils during pregnancy. Lobe bodies (blue staining of cytoplasmic inclusions in granulocytes) are considered normal in pregnant women.
In healthy women during uncomplicated pregnancy, there is no change in the absolute number of lymphocytes and there are no significant changes in the relative number of T- and B-lymphocytes. The number of monocytes usually does not change, the number of basophils may decrease slightly, and the number of eosinophils may increase slightly.
Coagulation factors and inhibitors
During normal pregnancy, the following changes in clotting factor levels occur, leading to physiological hypercoagulation:
- Due to hormonal changes during pregnancy, the activity of total protein S antigen, free protein S antigen and protein S is reduced.
- Activated protein C resistance increases in the second and third trimesters. These changes have been identified in first-generation tests using pure blood plasma (i.e., not lacking factor V), but this test is rarely used clinically and is of only historical interest.
- Fibrinogen and factors II, VII, VIII, X, XII and XIII are increased by 20-200%.
- Von Willebrand factor rises.
- Increased activity of fibrinolysis inhibitors, TAF1, PAI-1 and PAI-2. The level of PAI-1 also increases markedly.
- Levels of antithrombin III, protein C, factor V and factor IX most often remain unchanged or increase slightly.
The end result of these changes is an increase in the tendency to thrombosis, an increase in the likelihood of venous thrombosis during pregnancy and, especially, in the postpartum period. Along with contraction of the myometrium and an increase in the level of decidual tissue factor, hypercoagulability protects the pregnant woman from excessive bleeding during labor and delivery of the placenta.
APTT remains normal during pregnancy but may decrease slightly. Prothrombin time may be shortened. Bleeding time does not change.
The timing of normalization of blood clotting activity in the postpartum period may vary depending on factors, but everything should return to normal within 6-8 weeks after delivery. The hemostasiogram should not be assessed earlier than 3 months after delivery and after lactation is completed to exclude the influence of pregnancy factors.
The hemostasiogram should not be assessed earlier than 3 months after delivery and after lactation is completed to exclude the influence of pregnancy factors.
The influence of acquired or inherited thrombophilia factors on pregnancy is an area for research.
Postpartum period
Hematological changes associated with pregnancy return to normal 6-8 weeks after delivery. The rate and nature of the normalization of changes associated with pregnancy, specific hematological parameters are described above in the section on each parameter.
Hematological complications during pregnancy
- Iron deficiency anemia.
- Thrombocytopenia.
- Neonatal alloimmune thrombocytopenia.
- Acquired hemophilia A.
- Venous thrombosis.
- Rh and non-Rh alloimmunization. For diagnosis, an analysis is carried out for Rh antibodies and anti-group antibodies.
- A manifestation of a previously unrecognized coagulation disorder, such as von Willebrand disease, most commonly manifests in women during pregnancy and childbirth.
 For screening for von Willebrand disease, an assay is given to assess platelet aggregation with ristocetin.
For screening for von Willebrand disease, an assay is given to assess platelet aggregation with ristocetin. - Aplastic anemia.
Other articles in this section
-
ToRCH infections and pregnancy
What are ToRCH infections, what are the dangers of these infections during pregnancy, how and when is the examination performed, how to interpret the results. Perinatal infections account for approximately 2-3% of all congenital fetal anomalies.
-
Pregnancy Tests at CIR Laboratories
In our laboratory, you can undergo a complete examination in the event of pregnancy, take tests at any time, and in our clinics you can conclude an agreement on pregnancy management.
-
Pregnancy hCG calculator online
The hCG calculator is used to calculate the increase in hCG (the difference between two tests taken at different times).
The increase in hCG is important for assessing the development of pregnancy.
 Normally, in the early stages of pregnancy, hCG increases by about 2 times every two days. As the hormone levels increase, the rate of increase decreases.
Normally, in the early stages of pregnancy, hCG increases by about 2 times every two days. As the hormone levels increase, the rate of increase decreases. -
False positive pregnancy test or why hCG is positive but not pregnant?
When can a pregnancy test be positive?
-
The norm of hCG during pregnancy. Table of hCG values by week. Elevated HCG. Low HCG. HCG in ectopic pregnancy. hCG during IVF (hCG after replanting, hCG at 14 dpo).
hCG or beta-hCG or total hCG - human chorionic gonadotropin - a hormone produced during pregnancy. HCG is formed by the placenta, which nourishes the fetus after fertilization and implantation (attachment to the wall of the uterus).
-
Risk assessment of pregnancy complications using prenatal screening
Prenatal screening data allow assessing not only the risks of congenital pathology, but also the risk of other pregnancy complications: intrauterine fetal death, late toxicosis, intrauterine hypoxia, etc.
-
Parvovirus B19 and parvovirus infection: what you need to know when planning and getting pregnant.
What is a parvovirus infection, how is the virus transmitted, who can get sick, what is the danger of the virus during pregnancy, what tests are taken for diagnosis.
-
Pregnancy planning
Obstetrics differs from other specialties in that during the physiological course of pregnancy and childbirth, in principle, it is not part of medicine (the science of treating diseases), but is part of hygiene (the science of maintaining health). Examination during pregnancy planning.
-
1st and 2nd trimester prenatal screening ("double", "triple" and "quadruple" tests)
Prenatal screening are tests conducted on pregnant women to identify risk groups for pregnancy complications.
-
Testosterone during pregnancy. Androgens: their formation and metabolism during normal pregnancy.
 Hyperandrogenism during pregnancy. "Male" hormones during pregnancy.
Hyperandrogenism during pregnancy. "Male" hormones during pregnancy. During pregnancy, the level of testosterone and other androgens changes. The change in these levels depends, among other things, on the sex of the fetus.
All articles in section
Reticulocytes (blood level determination)
Site searchArticle: 00310
Cost of analysis
in the online store: 7% discount!
Plain
456rubExpress
911 rublesLab:
Regular
490rub
Express
980 rubles
the price does not include the cost of taking biological material
Add to Basket
Analysis results ready
Regular*: same day (subject to return before 12.00)
Analysis submission date:
Completion date:
*excluding the day of delivery.
Express
Where and when you can rent
- Buninskaya alley
- Voykovskaya
- Dubrovka
- Maryino
- Novokuznetskaya
- Podolsk
- Weekdays: from 7.45 to 12.00
- Weekends: from 8.45 to 12.00
Changes in work schedule
Preparation for analysis
General recommendations for testing
On an empty stomach, at least 8 hours after the last meal.
Biomaterial collection
- Blood sampling for laboratory testing
Methods and tests
Microscopy with special stains. Quantitative, ‰
Files
Download a sample of the analysis result
Reticulocytes are the immediate precursors of mature erythrocytes; the indicator reflects the production of erythrocytes in the red bone marrow (assessment of erythropoiesis). The study of the number of reticulocytes is carried out in conditions that are accompanied by blood loss, anemia, after treatment with cytotoxic drugs, bone marrow transplantation.
Test conditions
On an empty stomach (at least 8 hours after the last meal).Also ask:
- Complete blood count (CBC, with leukocyte formula and ESR)
- Urinalysis
- Women's Tumor Panel
- Extended hemostasiogram
Passed with this test:
- Iron (Fe) (blood level determination)
- Unsaturated serum iron-binding capacity (IWBC) (blood level determination)
- Percent Transferrin Saturation (Iron, Transferrin, VLSS and Percent Transferrin Saturation) (blood determination)
- Transferrin (blood level determination)
- Ferritin (blood level determination)
- Erythropoietin (blood level determination)
Tags: reticulocytes, anemia, blood loss, erythrocytes, transplantation, jaundice, iron deficiency anemia, red bone marrow
How to pass tests in the CIR Laboratories?
To save time, place an order for analysis at Online Store ! Paying for an order online, you get a discount 7% for the entire order!
Do you have questions? Write to us or call +7 (495) 514-00-11.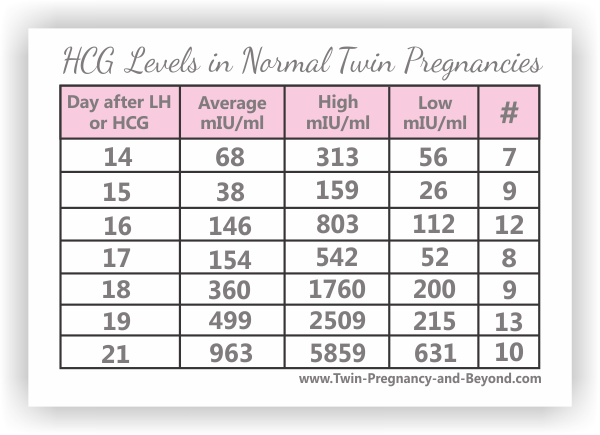 According to the analysis, you can ask a question on our forum and seek advice from a specialist.
According to the analysis, you can ask a question on our forum and seek advice from a specialist.
-
The norm of a complete blood count during pregnancy. Hemoglobin, platelets, hematocrit, erythrocytes and leukocytes during pregnancy. Clinical blood test during pregnancy. Hematological changes during pregnancy.
A normal pregnancy is characterized by significant changes in almost all organs and systems to adapt to the requirements of the fetoplacental complex, including changes in blood tests during pregnancy.
-
Iron deficiency anemia. What tests to take
The most common form of anemia is iron deficiency anemia (IDA), which is diagnosed by clinical and laboratory testing.
-
Serum folic acid, folate status, vitamin B12
Folic acid is a water-soluble vitamin essential for cell division. A lack of folic acid in the body can cause anemia (folate deficiency anemia) and hyperhomocysteinemia.
-
Basic tests in the diagnosis of anemia
Screening examination for the diagnosis of iron deficiency anemia, detection of latent iron deficiency and anemia General blood test, clinical blood test YBC, serum iron-binding capacity Serum iron In preparation.
 ..
.. -
HLA typing
HLA-typing of spouses (histocompatibility of spouses)
HLA antigens (human leucocyte antigens) of tissue compatibility (synonym: MHC - major histocompatibility complex - major histocompatibility complex) -
Tests in children
Pediatrician, PhD Ovsyannikov D.Yu.
- Complete blood count in children, frequent indications
- Children's blood chemistry, common indications
- Hemostasiogram
-
Hemoglobin
Hemoglobin (from Greek Hemo - blood and Latin globus - ball) is a complex protein molecule inside red blood cells - erythrocytes (in humans and vertebrates). Hemoglobin makes up approximately 98% of the mass of all erythrocyte proteins.
Cost of analysis
in the online store: 7% discount!
Plain
456rubExpress
911 rublesLab:
Regular
490rub
Express
980 rubles
the price does not include the cost of taking biological material
Add to Basket
Availability of test results
Regular*: same day (subject to return before 12..jpg)