How soon does alcohol affect pregnancy
Developmental Timeline of Alcohol-Induced Birth Defects
Developmental Timeline of Alcohol-Induced Birth DefectsMaternal consumption of alcohol (ethanol) during pregnancy can result in a continuum of embryonic developmental abnormalities that vary depending on the severity, duration, and frequency of exposure of ethanol during gestation. Alcohol is a teratogen, an environmental agent that impacts the normal development of an embryo or fetus. In addition to dose-related concerns, factors such as maternal genetics and metabolism and the timing of alcohol exposure during prenatal development also impact alcohol-related birth defects.
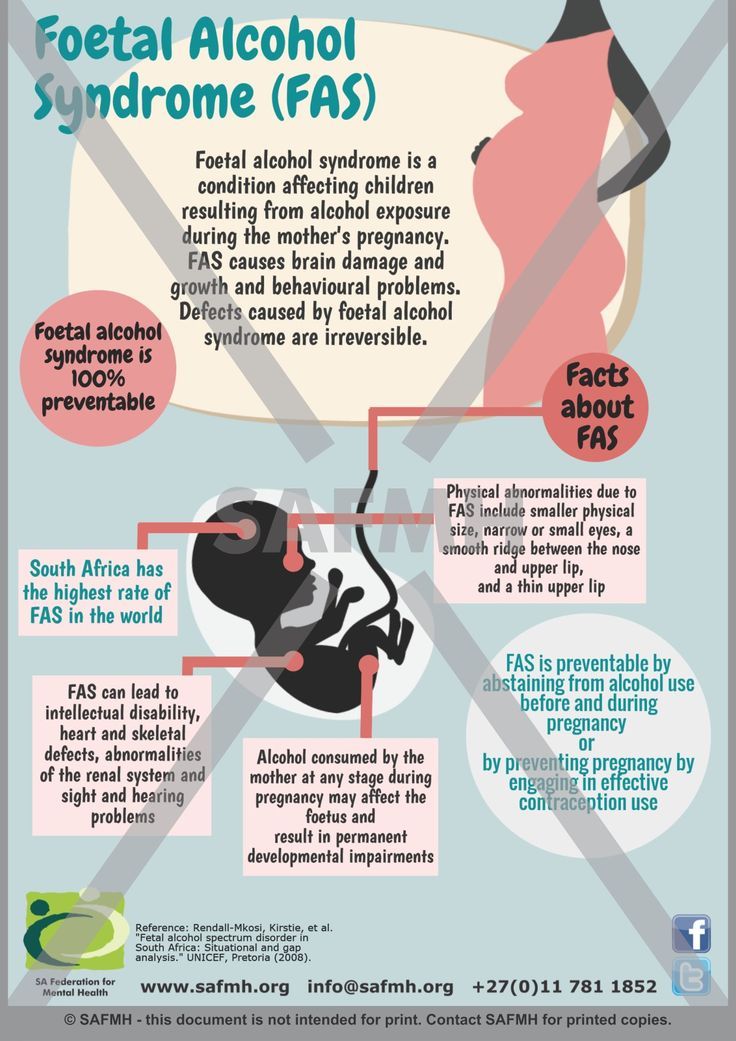
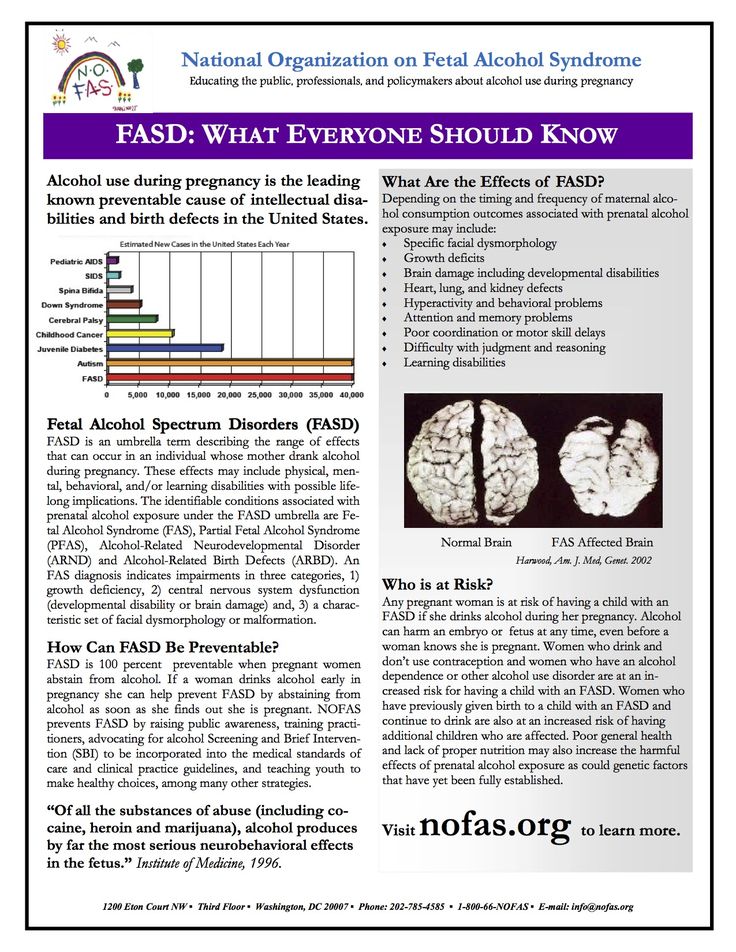
Fetal Alcohol Syndrome (FAS) is the most severe collection of alcohol-related birth defects, and is defined by pre- and post-natal growth retardation, minor facial abnormalities, and deficiencies in the central nervous system (CNS). The effects of alcohol on prenatal development can include much more than those defining criteria, however, and prenatal exposure to alcohol can potentially impact normal development at almost any point in the pregnancy, from embryonic through fetal development.
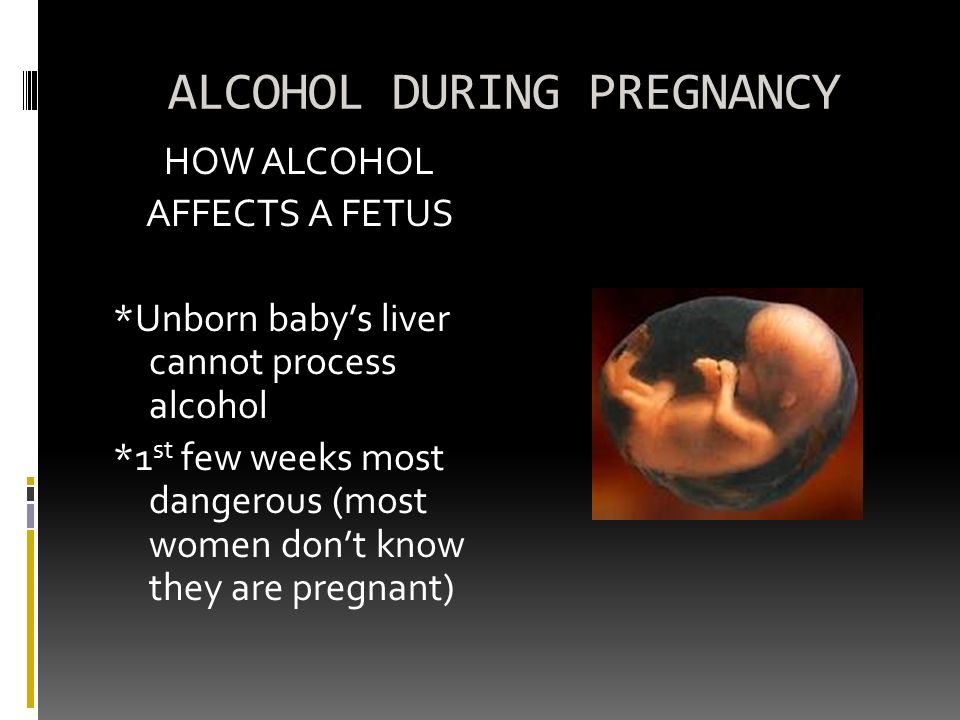
Prenatal development has into two stages, the embryonic stage that comprises the first eight weeks of development after fertilization, and the fetal stage that encompasses the remainder of development. The embryonic stage is the period when body plans are laid out, and the precursors of what will become organ systems are determined. Alcohol introduced at this stage can have significant repercussions depending on the population of cells negatively affected. Those developmental deviations can result in a range of birth defects or may completely arrest the pregnancy if malformations are particularly severe. During the fetal stage, prenatal alcohol exposure still has the potential to negatively impact development, but much less than the massive developmental defects that can result from exposure during the embryonic stage.
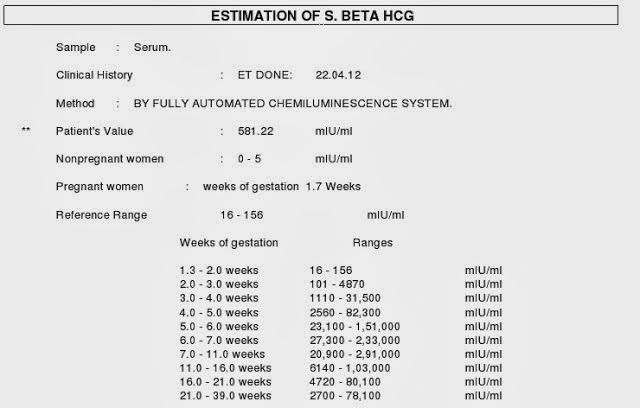
In the first two weeks following fertilization, excessive alcohol consumption does not generally have a negative effect on the zygote and emerging blastocyst (pre-embryo). Maternal consumption of alcohol during this time can prevent proper implantation of the blastocyst in the uterus, resulting in an increased rate of resorption or early termination of the pregnancy, generally before a woman realizes she is pregnant. The potential for the cells in the blastocyst to become any cell lineage in the body generally confers protection against the negative effects that alcohol has on specific cellular populations.
Maternal consumption of alcohol during this time can prevent proper implantation of the blastocyst in the uterus, resulting in an increased rate of resorption or early termination of the pregnancy, generally before a woman realizes she is pregnant. The potential for the cells in the blastocyst to become any cell lineage in the body generally confers protection against the negative effects that alcohol has on specific cellular populations.
It is in the third week after fertilization that specific alcohol-induced birth defects begin to affect the developing embryo. At this point in the developmental timeline, gastrulation commences and the three embryonic germ layers (ectoderm, mesoderm, and endoderm) are set. Between this point and the sixth week after fertilization, when neurulation occurs, the cranial neural crest cell population is vulnerable to alcohol-induced damages. The cranial neural crest cells compose the frontonasal process of the developing embryo, which interacts with the ectoderm to differentiate into facial features. Damage to this cellular progenitor pool can result in the minor midline facial abnormalities characteristic of FAS.
Damage to this cellular progenitor pool can result in the minor midline facial abnormalities characteristic of FAS.
Precursor cells that give rise to the heart also begin to differentiate shortly after the third week and by the fourth week of development, the embryonic heart is already beating. During this rapid period of cardiac development, alcohol can impede the proliferation, migration, and specification of cardiac progenitor cells by prompting either a deficient or toxic levels of retinol (vitamin A) in the developing embryo. Defects that result from those impediments can include atrial and ventricular abnormalities, issues with valve formation, and a potential increase in the risk of heart disease later in adulthood.
The neural plate forms in the third week, the anterior portion of which gives rise to neuroectoderm, tissues fated to form the tissues of the central nervous system (CNS). From this point through the third trimester, the cellular progenitor pools, called radial glia, that will give rise to the CNS become vulnerable to the effects of alcohol. The radial glia signals the creation and migration of neurons and their support cells (glia) during development. Damage to this cellular pool can result in morphological abnormalities and an overall reduction in white matter within the brain. Alcohol also impacts the mechanisms and signaling pathways responsible for the creation of those brain cells, impeding cellular proliferation, differentiation, and survival.
The radial glia signals the creation and migration of neurons and their support cells (glia) during development. Damage to this cellular pool can result in morphological abnormalities and an overall reduction in white matter within the brain. Alcohol also impacts the mechanisms and signaling pathways responsible for the creation of those brain cells, impeding cellular proliferation, differentiation, and survival.
During the third week of gestation, ocular development begins and tissues of the eye are the first component of the central nervous system compromised by the prenatal introduction of alcohol. During this time and continuing forward, the retina becomes vulnerable to the effects of alcohol. At about four weeks after fertilization, the neuroectoderm begins to interact with the surface ectoderm to create tissues that later give rise to the lens and cornea of the eye. In the fifth week following fertilization, the mesoderm surrounding the developing eye begins to give rise to the uvea (iris and other associated muscles), sclera (protective sheath surrounding the eye) and eyelids. The most common defects, microphthalmia and optic nerve hypoplasia arise when prenatal alcohol exposure compromises this developmental cycle.
The most common defects, microphthalmia and optic nerve hypoplasia arise when prenatal alcohol exposure compromises this developmental cycle.
Specific damage to the brain can continue in the sixth and seventh week following fertilization, after the brain has begun to divide into vesicles. At that point, the corpus callosum, a midline structure responsible for the communication between the left and right hemispheres of the brain, becomes vulnerable to alcohol. Prenatal alcohol exposure can result in the underdevelopment or complete agenesis of that structure, which is composed primarily of myelinated axons, and is therefore extremely vulnerable to ethanol’s impact on radial glia progenitor pools.
The eighth week after fertilization is the end of the embryonic stage and the beginning of the fetal stage of pregnancy. Prenatal alcohol exposure still has the potential to negatively impact normal development, but as the majority of organ systems have been determined by this point in time, organ-specific birth defects are not normally expected. The developing central nervous system remains vulnerable to the prenatal exposure of alcohol, particularly in the formation of the cerebellum, and the fetus remains vulnerable in terms of prenatal growth restrictions.
The developing central nervous system remains vulnerable to the prenatal exposure of alcohol, particularly in the formation of the cerebellum, and the fetus remains vulnerable in terms of prenatal growth restrictions.
The cerebellum is one of the last structures of the brain to differentiate during development, with the majority of structures in the brain having begun development earlier. Most cellular proliferation, migration, and synaptic regulation in the cerebellum occur in the third trimester, 24 weeks after fertilization through birth. This period of intense neuronal creation, organization and connectivity is called the brain growth spurt. While the radial glia progenitor pool has already been established by this point in time, alcohol can still impact neural migration and synaptogenesis.
The fetus is not as sensitive to the effects of alcohol as is the embryo, and in the third trimester the fetus begins to self-regulate and redirect resources to cope with environmental damages. Self-regulation is observed in the pre-natal growth deficiencies that accompany FAS, which fall into two broad categories, symmetric or asymmetric intrauterine growth restrictions. If alcohol impacts cellular proliferation in the first and second trimester, or consistently throughout the entire pregnancy, then the growth deficiencies will be symmetric and observed across all parts of the developing fetus. Asymmetric growth restrictions, which result in a normal-sized head but smaller than normal abdominal cavity, may result in the third semester. The head is a normal size because in the third trimester the fetus can redistribute cardiac resources to the command centers of the body, like the brain and heart, at the expense of other less vital processes like digestion.
Self-regulation is observed in the pre-natal growth deficiencies that accompany FAS, which fall into two broad categories, symmetric or asymmetric intrauterine growth restrictions. If alcohol impacts cellular proliferation in the first and second trimester, or consistently throughout the entire pregnancy, then the growth deficiencies will be symmetric and observed across all parts of the developing fetus. Asymmetric growth restrictions, which result in a normal-sized head but smaller than normal abdominal cavity, may result in the third semester. The head is a normal size because in the third trimester the fetus can redistribute cardiac resources to the command centers of the body, like the brain and heart, at the expense of other less vital processes like digestion.
There is no point during development when prenatal alcohol exposure lacks consequences, the occurrence of the more severe birth defects correlates with exposure to alcohol in the embryonic stage rather than the fetal stage.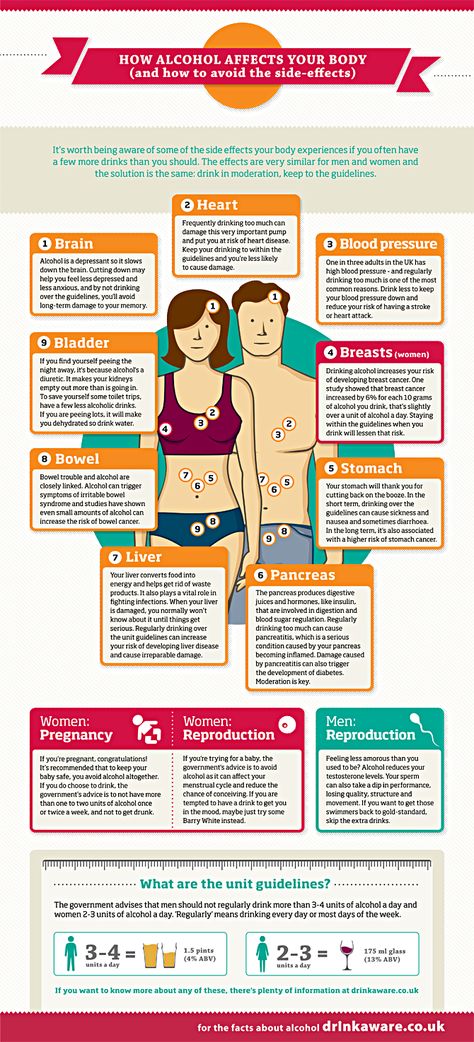 FAS and related alcohol-induced birth defects are an example of what can happen when a mother heavily imbibes alcohol during the course of the pregnancy. In the United States, the Surgeons General caution women against drinking while pregnant and require warnings be displayed on all alcoholic products.
FAS and related alcohol-induced birth defects are an example of what can happen when a mother heavily imbibes alcohol during the course of the pregnancy. In the United States, the Surgeons General caution women against drinking while pregnant and require warnings be displayed on all alcoholic products.
- Armstrong, Elizabeth M. Conceiving Risk, Bearing Responsibility: Fetal Alcohol Syndrome & the Diagnosis of Moral Disorder. Baltimore: The John Hopkins University Press, 2003.
- Bookstein, Fred L., Paul D. Sampson, Paul D. Connor, and Ann P. Streissguth. “Midline Corpus Callosum is a Neuroanatomical Focus of Fetal Alcohol Damage,” The New Anatomical Record 269 (2002): 162–74.
- Dikranian, Krikor, Yue-Qin Qin, Joann Labruyere, Brian Nemmers, and John W. Olney. “Ethanol-Induced Neuroapoptosis in the Developing Rodent Cerebellum and Related Brain Stem Structures,” Developmental Brain Research 155 (2005): 1–13.
- Gilbert, Scott.
 Developmental Biology, 8 ed. Sunderland: Sinauer, 2006.
Developmental Biology, 8 ed. Sunderland: Sinauer, 2006. - Golden, Janet. Message in a Bottle: The Makings of Fetal Alcohol Syndrome. Cambridge: Harvard University Press, 2005.
- Grewal, Jagteshwar, Suzan L. Carmichael, Chen Ma, Edward J. Lammer, and Gary M. Shaw. “Maternal Periconceptional Smoking and Alcohol Consumption and Risk for Select Congenital Anomalies,” Birth Defects Research Part A: Clinical and Molecular Teratology 82 (2008): 519–26.
- Guerri, Consuelo, Alissa Bazinet, and Edward P. Riley. “Foetal Alcohol Spectrum Disorders and Alterations in Brain and Behavior,” Alcohol & Alcoholism 44 (2009): 108–14.
- Rubert, Gemma, Rosa Miñana, Maria Pascual, and Consuelo Guerri. “Ethanol Exposure during Embryogenesis Decreases the Radial Glial Progenitor Pool and Affects the Generation of Neurons and Astrocytes,” Journal of Neuroscience Research 84 (2006): 483–96.
- Saito, Toshikazu, Boris Tabakoff, Paula L.
 Hoffman, Kim Nixon, Masaru Tateno, and Consuelo Guerri. “The Effects of Ethanol on Neuronal and Glial Differentiation and Development,” Alcoholism: Clinical and Experimental Research 29 (2005): 2070–75.
Hoffman, Kim Nixon, Masaru Tateno, and Consuelo Guerri. “The Effects of Ethanol on Neuronal and Glial Differentiation and Development,” Alcoholism: Clinical and Experimental Research 29 (2005): 2070–75.
O'Neil, Erica, "Developmental Timeline of Alcohol-Induced Birth Defects". Embryo Project Encyclopedia (2011-04-24). ISSN: 1940-5030 http://embryo.asu.edu/handle/10776/2101.
Arizona State University. School of Life Sciences. Center for Biology and Society. Embryo Project Encyclopedia.
© Arizona Board of Regents Licensed as Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported (CC BY-NC-SA 3.0) http://creativecommons.org/licenses/by-nc-sa/3.0/
Drinking Alcohol While Pregnant in First 3 Weeks: Is It Safe?
It happens. Perhaps you went off birth control a few months ago to try for a baby, but weren’t expecting to get pregnant so soon.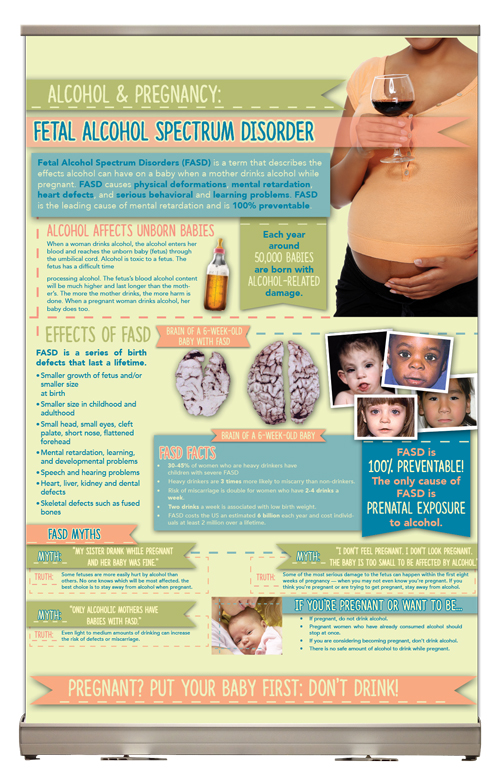 You did cut back on alcohol to up your chances of conceiving, but you continued having a glass of wine here and there.
You did cut back on alcohol to up your chances of conceiving, but you continued having a glass of wine here and there.
Or maybe you weren’t trying to get pregnant at all, and it came as a surprise when you realized that your period was over a week late. Now you’re looking at two pink lines on a home pregnancy test and freaking out about the night out with your girlfriends that you enjoyed a few days ago.
Maybe you’ve even known for a couple weeks that you’re pregnant, but you went ahead and toasted the bride and groom at a recent wedding because your friend told you small amounts of alcohol so early in pregnancy don’t do any harm.
Whatever the case, you’re now worried and want to know what damage, if any, drinking in very early pregnancy can do.
First off, take a deep breath and let go of any guilt or shame that you feel about the past. You’re in a no-judgement zone here. Next, continue reading to learn what the side effects can be — and most importantly, what you can do to ensure good health for you and your baby moving forward.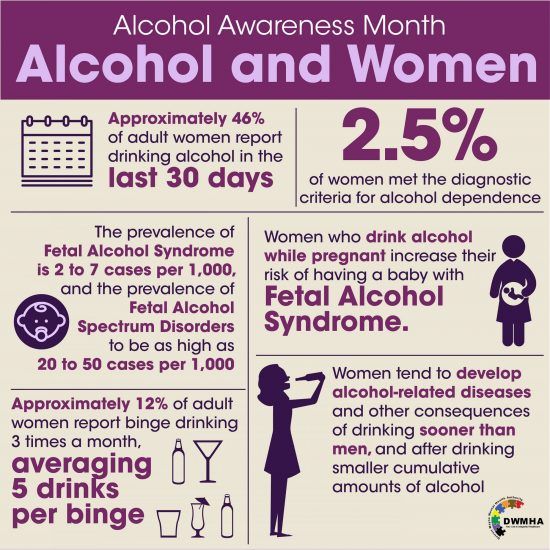
At the very top of its alcohol and pregnancy information sheet — and in bold type, no less — the Centers for Disease Control and Prevention (CDC) advises that women who are trying to become pregnant or could be pregnant shouldn’t drink.
Why? It’s not really about the harm done by what you drink before you’re even pregnant (though this may affect your ability to conceive). It’s that no amount of alcohol at any point in pregnancy has been absolutely proven to be safe.
Since you can be pregnant without knowing it, the CDC is covering the possibility that you’re in the earliest stages of pregnancy — 3 or 4 weeks, often even before your missed period. (Many people don’t know they’re pregnant until they’re already 4 to 6 weeks.)
Like the CDC in the United States, the NHS in the United Kingdom says that if you’re pregnant or planning to become pregnant, avoid alcohol.
Truly specific research around drinking alcohol in very early pregnancy is pretty tricky.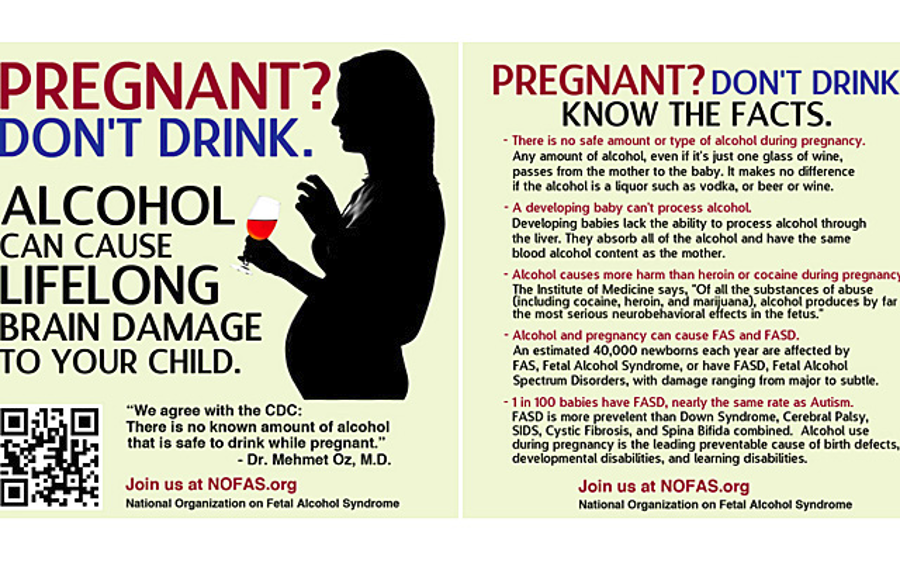 That’s because it would be unethical to put together a study and actually request that any segment of the pregnant population do something (drink alcohol) known to cause harm even some of the time.
That’s because it would be unethical to put together a study and actually request that any segment of the pregnant population do something (drink alcohol) known to cause harm even some of the time.
What we do have: research that looks at people who self-report alcohol use during pregnancy as well as some animal studies. We also have a lot of science backing our understanding of human development in the womb, including brain and central nervous system development starting at week 3 of pregnancy (right after implantation).
In one 2015 study done in mice, researchers gave the animals alcohol at 8 days gestation — roughly equivalent to the early fourth week in a human pregnancy. They found that the offspring of these mice had changes to their brain structure.
The results suggested that early alcohol exposure can alter DNA chemical processes. Embryonic stem cells that change as a result of the mother’s alcohol consumption early in pregnancy could even impact adult tissue later on.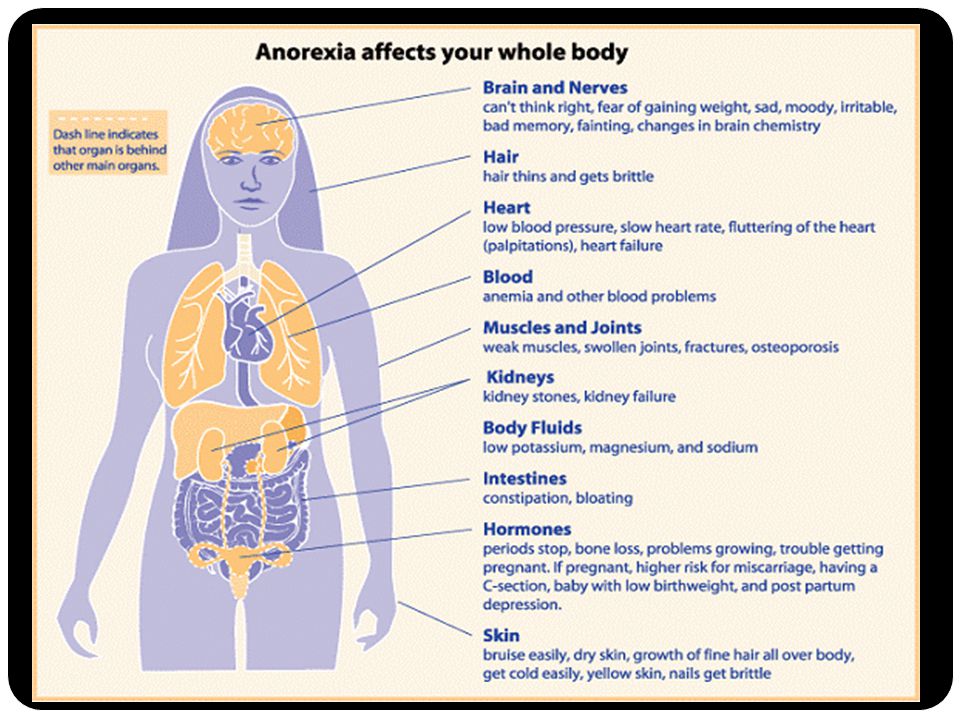
To be a little Captain Obvious here, humans aren’t mice. There’s no way to know at this time if this effect happens in the same way in humans. It’s definitely worth further study, though.
On the other hand, a study published in 2013 looked at 5,628 women who self-reported various amounts of alcohol consumption during early pregnancy. (For the purposes of this study, though, “early” meant all the way up until 15 weeks.)
Researchers looked for common effects of alcohol on pregnancy:
- low birth weight
- high maternal blood pressure
- preeclampsia
- smaller-than-expected size for gestational age
- pre-term birth
They didn’t find a strong correlation between drinking early in pregnancy and an increased likelihood of these complications, so some people take this to mean it’s A-OK. But this study only looked at short-term outcomes (not long-term effects that might not show up until childhood) and not fetal alcohol syndrome disorders (FASDs).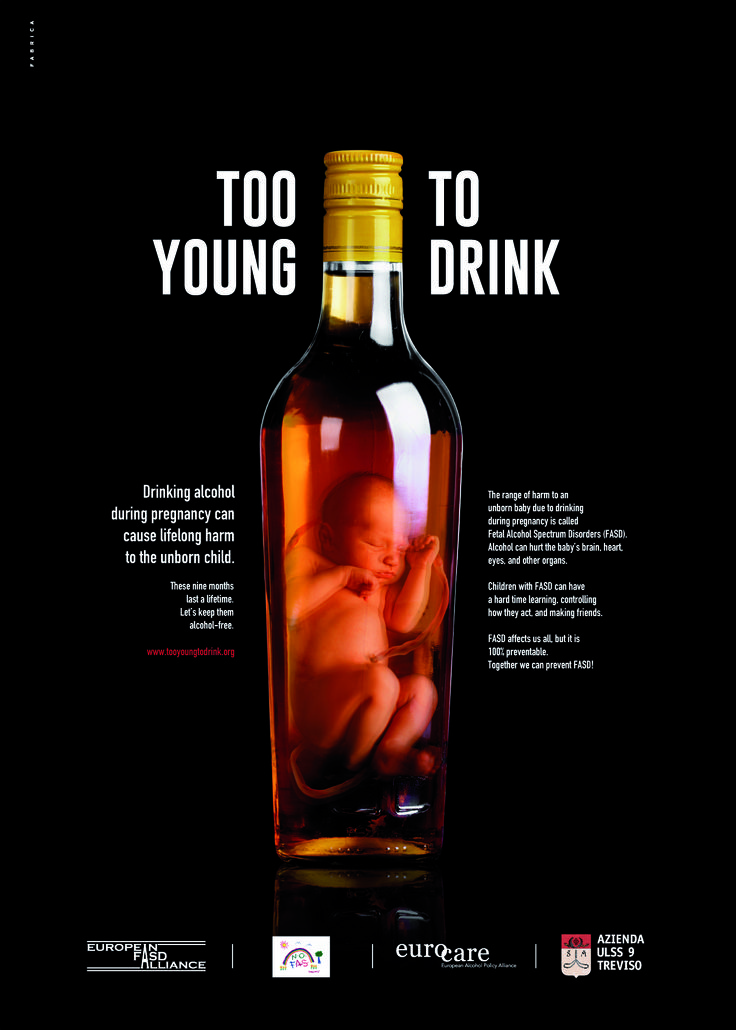
These studies represent two ends of the spectrum — one shows some scary possibilities about changed DNA, and the other suggests no ill effects. Most studies fall more in the murky middle, though.
For example, this 2014 study looked at 1,303 pregnant women in the United Kingdom and their alcohol consumption before pregnancy and during all three trimesters. Results suggested that drinking — even fewer than two drinks per week — in the first trimester increased risk of complications, like lower birth weight and pre-term birth.
And this research published in 2012 suggested that even light drinking in the early weeks could increase miscarriage risk, though the risk goes up with heavier drinking.
It might be accurate to look at all the information out there and say that very light drinking in very early pregnancy doesn’t always (or often) cause problems — but it could. And different people define “light” differently, adding to the confusion. So following CDC and NHS guidelines of no alcohol at any point is the safest option and the one that we recommend.
There are a couple big concerns with drinking early in pregnancy: miscarriage and fetal alcohol syndrome disorders.
It’s an incredibly difficult reality that miscarriages are as common as they are. And even if you do everything by the book, the highest risk of miscarriage is in the first trimester — and it often happens due to issues outside of your control (like chromosomal abnormalities).
Numerous reliable sources and studies (like the one we mentioned above) mention that alcohol use in the first trimester may increase miscarriage risk. Why this happens isn’t entirely clear.
The other big risk is FASDs. Symptoms include:
- pre-term birth
- low birth weight
- neurological problems
- behavioral problems that show up later in childhood
- certain abnormal facial features (thin upper lip, small eyes, missing vertical crease between the nose and lips)
- cognitive difficulties
Here’s something to remember: in-utero human development doesn’t happen all at once.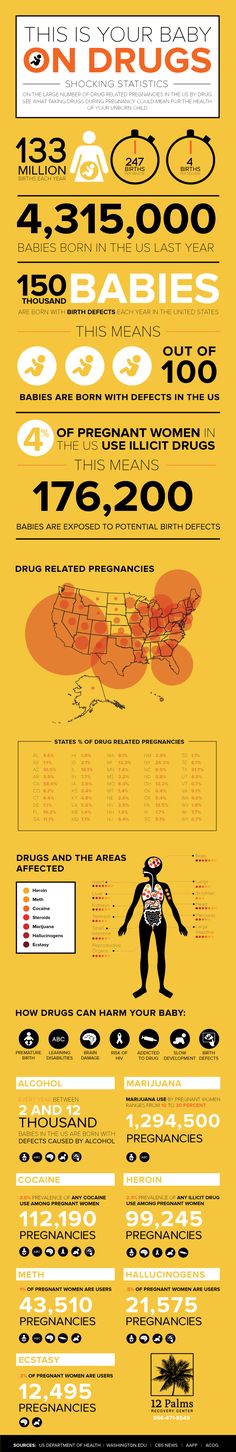 It happens over a 40-week period (more or less, but you know what we mean) and there are many contributing factors.
It happens over a 40-week period (more or less, but you know what we mean) and there are many contributing factors.
And while drinking at any stage of pregnancy should be avoided, both the American College of Obstetricians and Gynecologists and the Royal College of Obstetricians and Gynaecologists say harm from having a little alcohol before you knew you were pregnant is unlikely.
So if you drank alcohol before you realized you were pregnant, the important thing is that you stop now. Your tiny human’s brain has a lot of development yet to go.
Take your daily prenatal vitamin, maintain a healthy diet, avoid undercooked meats and raw or high-mercury fish, and keep your prenatal appointments — these are all wonderful things you can do to promote your baby’s health.
And while we’re on the topic of those prenatal appointments — talk to your doctor candidly about your concerns and let them know that you had alcohol early on.
If you feel uncomfortable chatting with them about things that may affect your pregnancy, find a new doctor.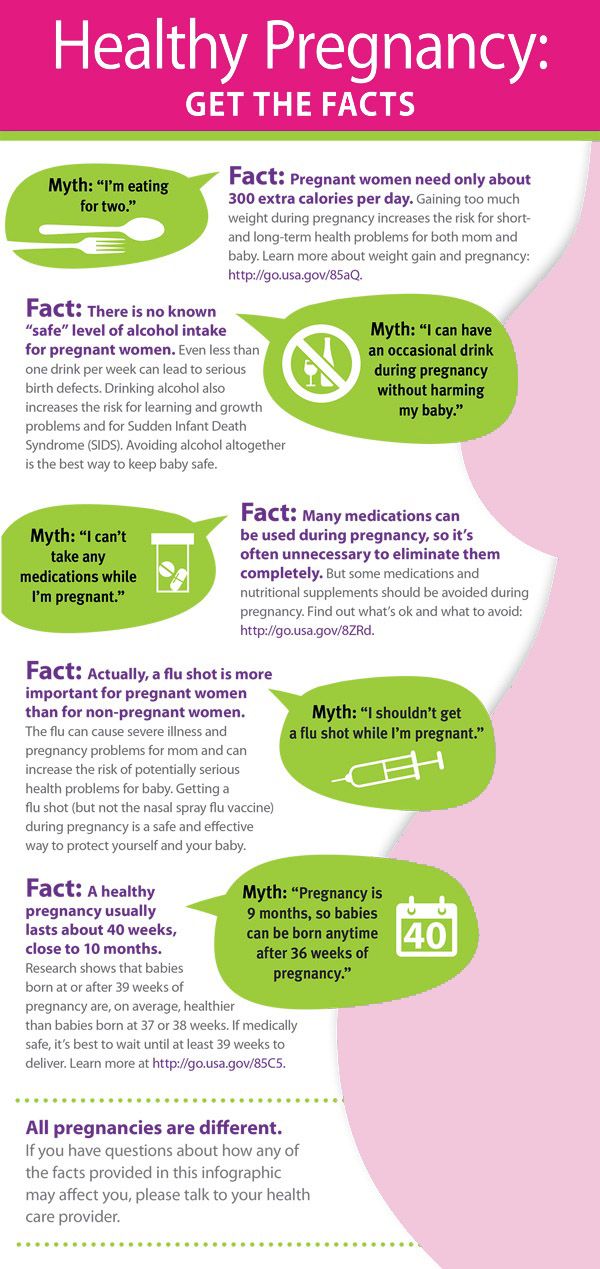 Being able to speak honestly about your health and the health of your baby during pregnancy is crucial to having a healthy, happy nine months.
Being able to speak honestly about your health and the health of your baby during pregnancy is crucial to having a healthy, happy nine months.
ALCOHOL AND PREGNANCY - Outpatient medical facility
The fact that you can not drink alcohol during pregnancy is known to most. However, different situations can arise in life: one woman is planning a pregnancy, continuing to drink alcohol on holidays in order to avoid uncomfortable questions; another drinks a glass of wine, unaware that she is already pregnant; the third during pregnancy cannot cope with the desire to drink beer, believing that "a little bit is possible." Let's look at these situations in more detail.
Alcohol consumption during pregnancy planning.
Alcohol is a toxin that adversely affects the human reproductive system. In women, alcohol consumption leads to disruption of the menstrual cycle and hormonal balance, which significantly affects the ability to conceive. There are also opinions that even episodic alcohol consumption can have a negative effect on the eggs, leading to their inferiority.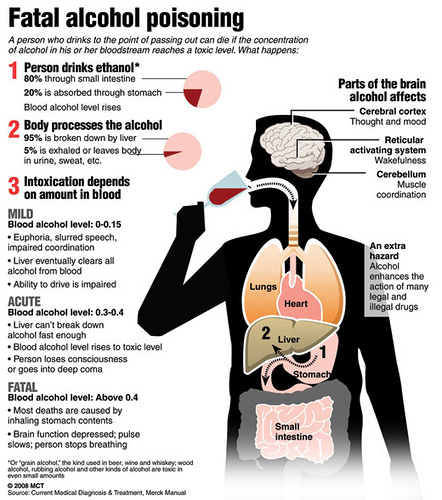 Also, alcohol consumption affects the male reproductive system, significantly reducing the number of sperm capable of fertilization. Therefore, a couple planning a pregnancy should stop drinking alcohol at least 3 months in advance in order to increase the likelihood of conception.
Also, alcohol consumption affects the male reproductive system, significantly reducing the number of sperm capable of fertilization. Therefore, a couple planning a pregnancy should stop drinking alcohol at least 3 months in advance in order to increase the likelihood of conception.
Drinking alcohol in the first weeks after conception.
Without a special examination, a woman usually discovers the fact of pregnancy at 3 weeks after conception, when the next menstruation does not come. By this time, the embryo has already firmly attached to the uterine cavity and began to receive nutrition from the mother's blood. If negative factors, including alcohol, affect him before the moment of attachment, then this will lead to his rejection and death, and he will simply leave the uterus with the next menstruation. Thus, a woman may not know that she was pregnant.
According to most scientists, if alcohol did not disrupt the attachment process and the embryo continued to develop, then this would not lead to the formation of malformations in it.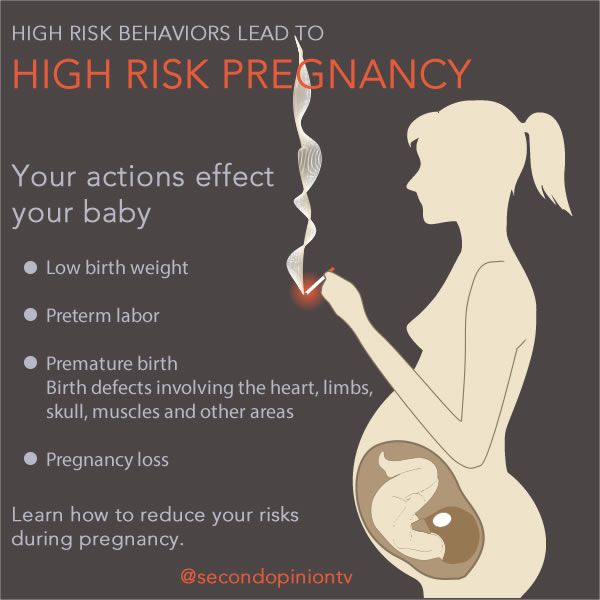 Thus, alcohol accidentally drunk during the first two weeks after conception will either lead to the termination of pregnancy or will not affect its further development.
Thus, alcohol accidentally drunk during the first two weeks after conception will either lead to the termination of pregnancy or will not affect its further development.
Alcohol use in early pregnancy.
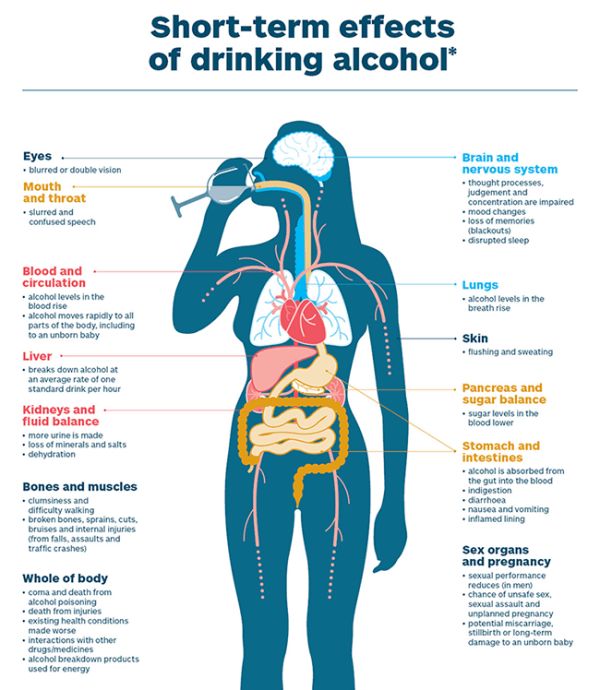
As mentioned above, as early as the 3rd week after conception, the embryo begins to come into contact with maternal blood. This means that all the substances in the mother's blood come to him. including ethyl alcohol. From the 3rd to the 13th week of development, the laying of all the main systems of the body of the unborn child occurs and the effect of alcohol no longer leads to rejection and death of the embryo, but to the formation of malformations and deformities of the nervous, cardiovascular, and digestive systems.
Alcohol use in late pregnancy.
The negative impact of alcohol on the course of pregnancy is observed after the 13th week. Ethanol and its decay products lead to spasm of the vessels of the placenta and umbilical cord, impairing the delivery of oxygen and nutrients, leading to a delay in the development of the fetus, disruption of its nervous system and brain. A prolonged lack of oxygen can even lead to the death of a child. Violation of the nervous system in the prenatal period leads to problems in the later life of the child - such children have reduced stress resistance, problems in learning, in communication, a tendency to mental illness and alcohol consumption.
A prolonged lack of oxygen can even lead to the death of a child. Violation of the nervous system in the prenatal period leads to problems in the later life of the child - such children have reduced stress resistance, problems in learning, in communication, a tendency to mental illness and alcohol consumption.
The systematic use of alcohol during pregnancy leads to the formation of fetal alcohol syndrome in a child - this is a complex of physical, mental and intellectual abnormalities in a child that cannot be treated.
Thus, alcohol and pregnancy are not compatible and it is necessary to refuse it at the planning stage.
You need to understand that one glass of wine, drunk before 2 or after 13 weeks of pregnancy, most likely will not lead to disastrous consequences, but is it worth the risk? Remember that your child will “drink” half of this glass.
What happens to the child if the mother drinks alcohol?
03. 12.2019
12.2019
Alcohol and pregnancy are incompatible - doctors do not get tired of talking about this to expectant mothers. But pregnant women sometimes allow themselves to skip a glass of wine, thinking that nothing bad will come of such an amount. However, alcohol can interfere with fetal development at any stage of pregnancy, even very early.
Studies show that excessive (four or more drinks at a time) and/or regular drinking by an expectant mother puts the fetus at the greatest risk of serious problems. But even a smaller amount of alcohol can be harmful, since there is no safe dose.
Alcohol easily passes from the mother's bloodstream into the child's bloodstream, which can affect the development of the brain and other vital organs, structures and physiological systems of the baby's body, leading to malformations that can begin in a child in early childhood and last a lifetime. The most profound effects of prenatal alcohol exposure are brain damage and associated behavioral and cognitive impairment.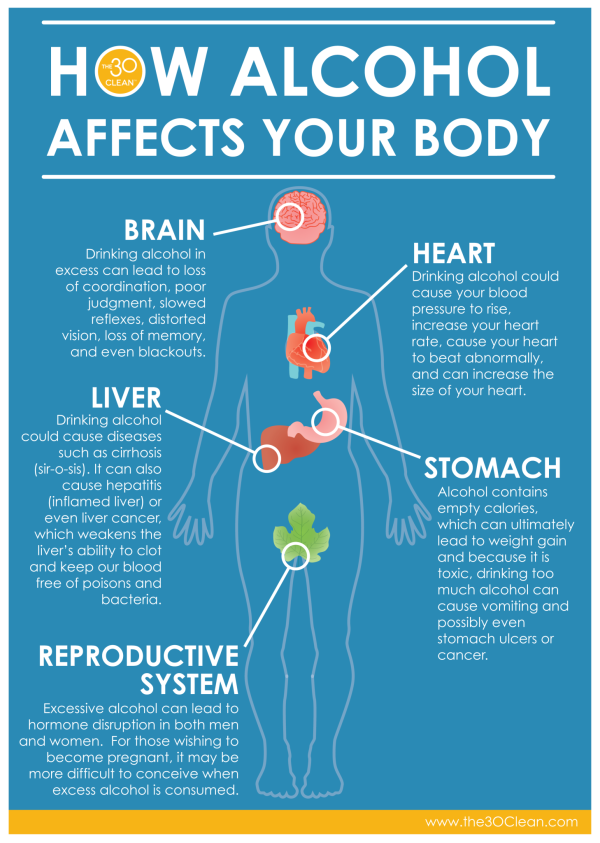
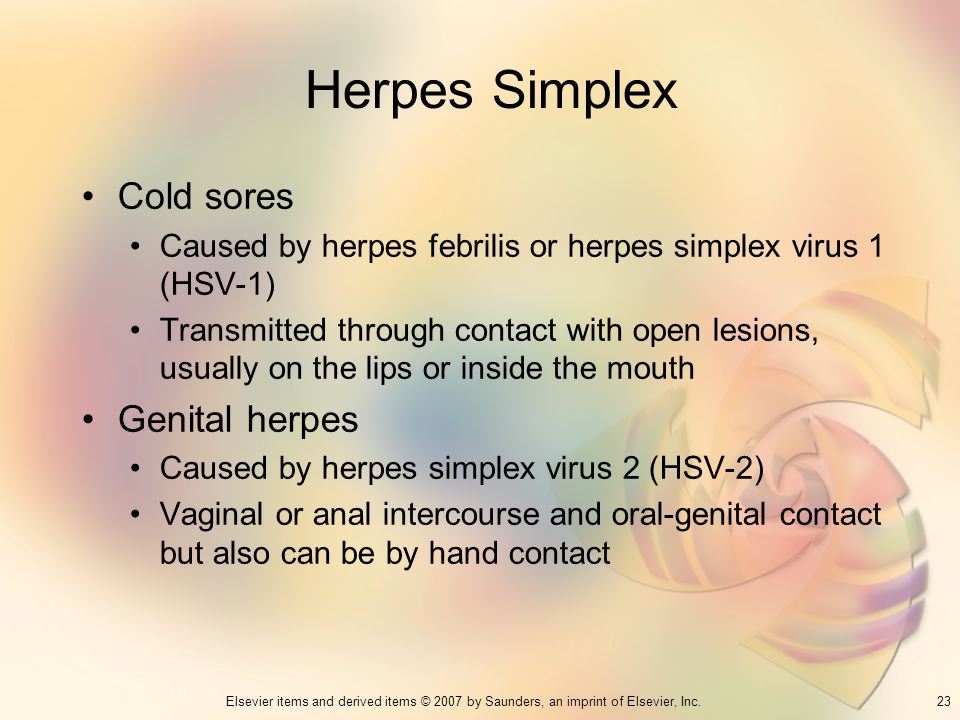
Scientists define a wide range of effects and symptoms caused by prenatal alcohol exposure, termed "fetal alcohol spectrum disorders". These include conditions such as intrauterine alcohol syndrome, alcohol-related nervous system disorder, and alcohol-associated birth defects. All these cases have one common feature - damage to the central nervous system (CNS) as a result of prenatal alcohol exposure to the fetus.
The effect of alcohol on the CNS may be structural (eg, reduction in brain size, changes in certain areas of the brain) or functional (eg, cognitive and behavioral deficits, motor and coordination problems). Extended studies using modern imaging techniques (MRI, CT, etc.) have revealed differences in the structure and activity of the brain that are consistent with neuropsychological testing data, including a disorder in processing information from the senses, changes in cognitive processes and behavior in adults with the disorder alcohol spectrum of the fetus compared to healthy people.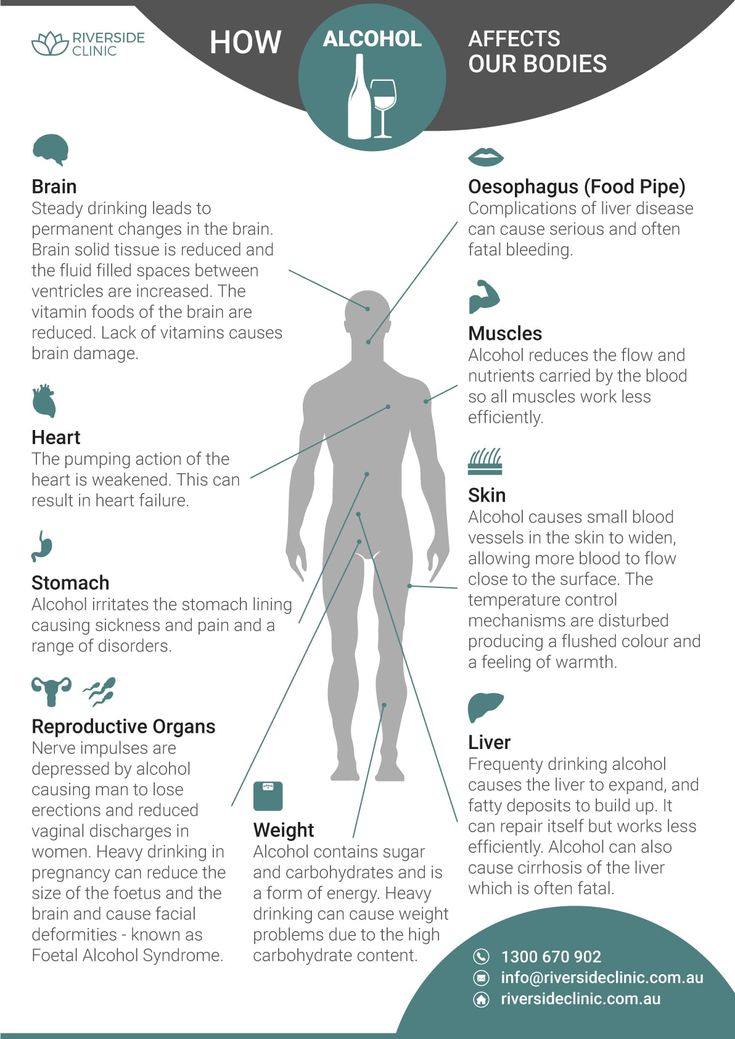
The most profound effects of prenatal alcohol exposure are brain damage and associated impairments in behavioral and cognitive functioning.
How are the disorders different?
Fetal alcohol syndrome was the first form of alcohol spectrum disorder and is still the most well-known syndrome. It manifests itself with excessive alcohol consumption by the expectant mother during the first trimester of pregnancy. The impact of harmful substances on the fetus can disrupt the normal development of not only the brain, but also the face. Thus, in addition to CNS developmental anomalies, the child will have a specific pattern of three facial anomalies: narrow eye openings, a smooth area between the lip and nose (compared to a normal ridge), and a thin upper lip. Also, the baby may experience growth deficiency in utero and (or) after birth.
Partial fetal alcohol syndrome includes only some of the characteristics listed above.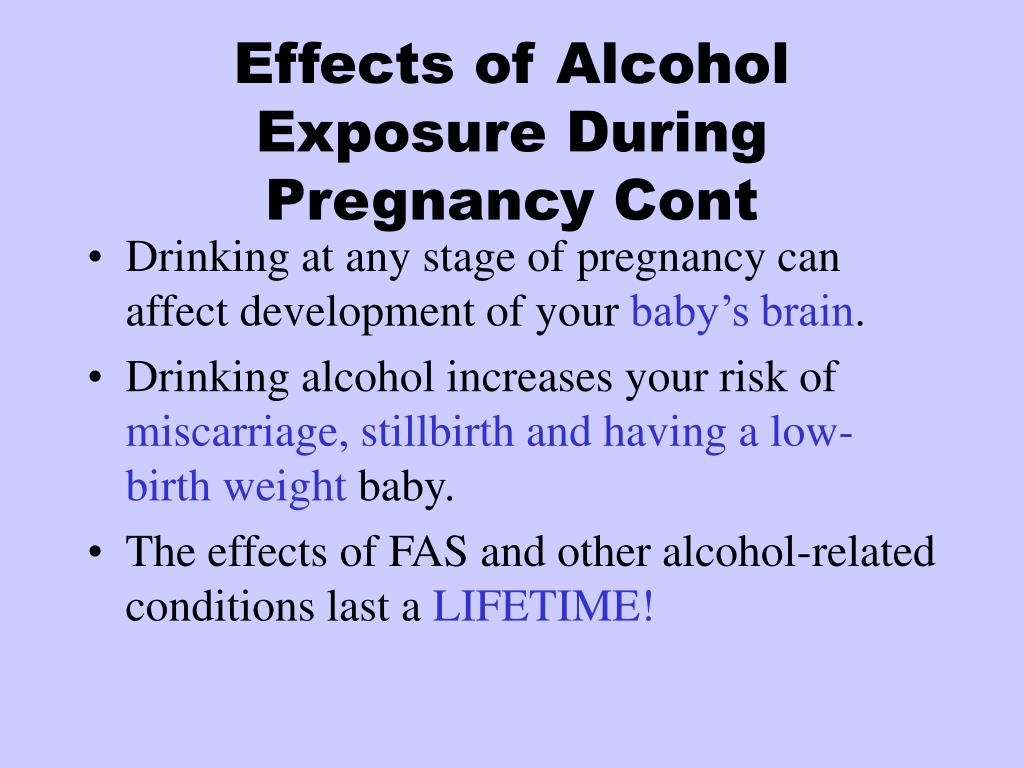
An alcohol-related disorder of the nervous system is characterized by disorders of the central nervous system, which may be structural or functional. Functional impairments include a complex pattern of cognitive (mental) or behavioral problems that do not correspond to the standard level of development at any given age in a child. At the same time, the reasons for this discrepancy cannot be explained by factors other than prenatal alcohol exposure. Facial abnormalities and growth retardation should not be present.
Alcohol-related birth defects include heart, kidney, bone, and other malformations; difficulties with vision and hearing; decreased function of the immune system. They are rarely considered separately, but rather are a secondary disorder that accompanies other fetal alcohol spectrum disorders.
What will happen to the baby in the future?
Every person whose mother may have abused alcohol during pregnancy experiences a combination of everyday turmoil that includes medical, behavioral, educational, or social problems in the following areas:
- learning and memorization;
- understanding and following directions;
- ability to hold attention;
- the ability to control emotions;
- communication and socialization;
- performing daily life skills (eg, eating, bathing, counting money, taking care of personal safety).
People with fetal alcohol spectrum disorder are more likely than others to make bad decisions, repeat the same mistakes, trust the wrong people, and have difficulty understanding the consequences of their actions. They are also more prone to disorders such as attention deficit hyperactivity disorder, depression, impulse control problems, alcoholism and drug addiction.
People with fetal alcohol spectrum disorder are more likely than others to make bad decisions, repeat the same mistakes, trust the wrong people, and have difficulty understanding the consequences of their actions.
Risk factors
Of course, it is impossible to argue that just one sip of champagne during pregnancy can provoke many anomalies in the development of the fetus and affect the psyche of the unborn child. But the medical community recommends completely avoiding any dose of alcohol during pregnancy.
There are risk factors that contribute to the development of undesirable consequences:
- amount of alcohol a pregnant woman drinks at a time;
- frequency of drinking by a pregnant woman;
- the stage of pregnancy at which a woman drinks alcohol, and how much she drinks during the formation of one or another body system in the fetus.
Prenatal alcohol exposure to children can be exacerbated if their mothers are malnourished, overweight, underweight, or smoke…
In addition, studies show that prenatal alcohol exposure affects children more if their mothers live in unfavorable conditions and experience high levels of stress. These may include, for example, social isolation, living in a society where excessive drinking is common and acceptable, and living in a society where resources for prenatal care are limited.
The prenatal effects of alcohol on children can be exacerbated if their mothers are malnourished, overweight, underweight, smoke…
How to help a child?
First aid for a child is the refusal of the expectant mother from alcohol. But if during pregnancy a woman allowed herself to drink alcohol and the child has symptoms of a fetal alcohol spectrum disorder, special tactics of education and training should be applied.