Can you be born with cold sores
Causes, Symptoms, Picture, and Prevention
Birth-Acquired Herpes: Causes, Symptoms, Picture, and PreventionMedically reviewed by Karen Gill, M.D. — By Erica Roth on August 31, 2018
What is birth-acquired herpes?
Birth-acquired herpes is a herpes virus infection that an infant gets during delivery or, less commonly, while still in the womb. The infection can also develop shortly after birth. Babies with birth-acquired herpes get the infection from mothers who are infected with genital herpes.
Birth-acquired herpes is sometimes also called congenital herpes. The word congenital refers to any condition that’s present from birth.
Infants who are born with herpes may have a skin infection or a system-wide infection called systemic herpes, or both. Systemic herpes is more serious and can cause a variety of issues. These issues may include:
- brain damage
- breathing problems
- seizures
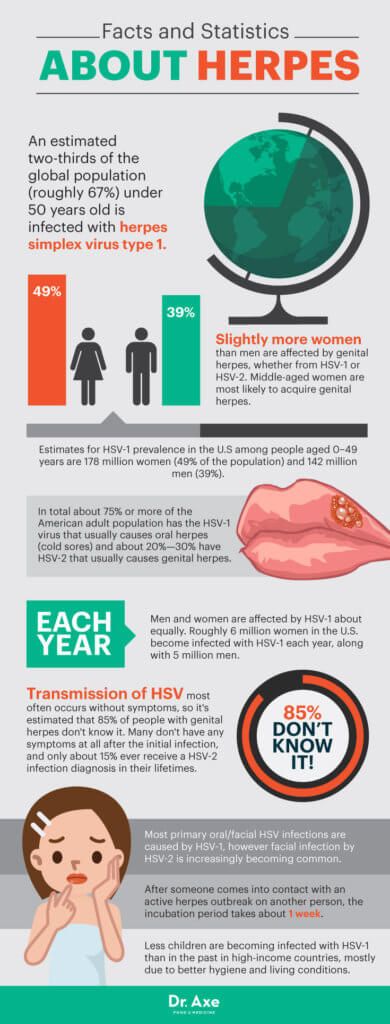
According to Boston Children’s Hospital, herpes occurs in approximately 30 out of every 100,000 births.
It’s a serious condition and can be life-threatening.
Causes of birth-acquired herpes
The herpes simplex virus (HSV) causes birth-acquired herpes. The highest risk for birth-acquired herpes is during a mother’s first, or primary, infection.
After someone recovers from herpes, the virus lies dormant in their body for long periods before it flares up and symptoms appear or reappear. When the virus reactivates, it’s called a recurrent infection.
Women who have active herpes infections are more likely to pass the virus on to their babies during a vaginal birth. The infant comes into contact with herpes blisters in the birth canal, which can cause infection.
Mothers who have a nonactive herpes infection when they deliver can also transmit herpes to their child, particularly if they acquired herpes for the first time during pregnancy.
Most babies with HSV infection are born to mothers with no history of herpes or active infection. This is, in part, because measures are taken to prevent birth-acquired herpes in babies born to mothers who are known to be infected.
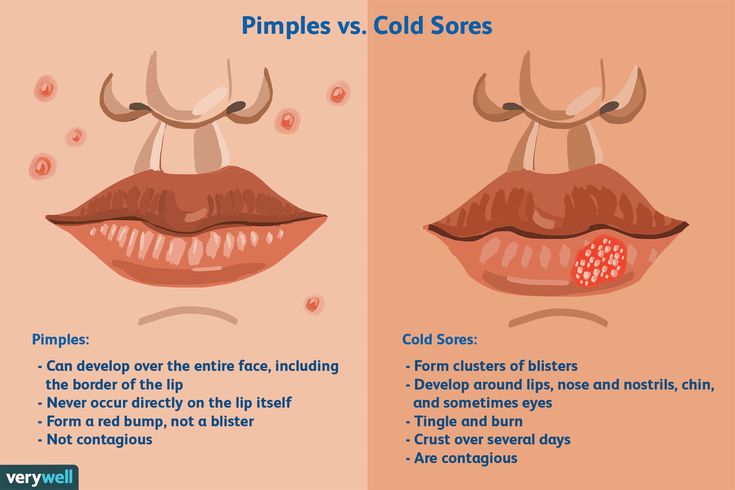
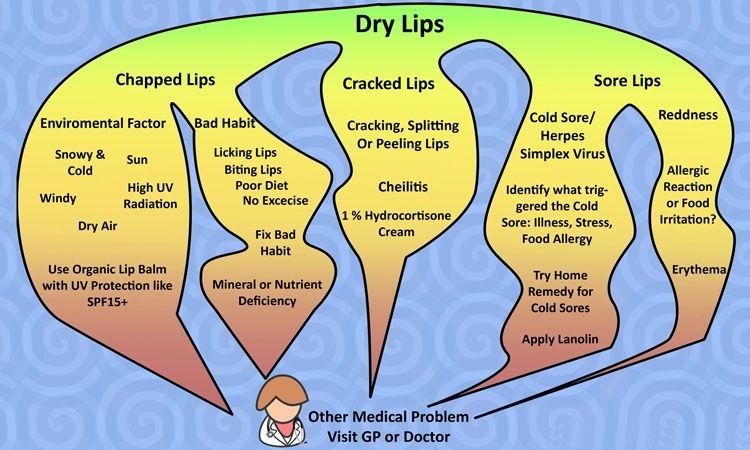
You should note that your infant could also get herpes through contact with cold sores. Another form of the HSV causes cold sores on the lips and around the mouth. Someone who has a cold sore can pass the virus on to others through kissing and other close contact. This would be considered neonatal herpes, rather than birth-acquired herpes, and is usually less severe.
Recognizing the symptoms of birth-acquired herpes
The symptoms of birth-acquired herpes usually appear within the first few weeks of the baby’s life and may be present at birth.
Birth-acquired herpes is easiest to identify when it appears as a skin infection. The baby may have clusters of fluid-filled blisters on their torso or around their eyes.
The blisters, called vesicles, are the same type of blisters that appear on the genital regions of adults with herpes. The vesicles may burst and crust over before healing. An infant can be born with the blisters or develop the sores a week after birth.
Infants with birth-acquired herpes might also appear extremely tired and have trouble feeding.
Complications associated with birth-acquired herpes
The systemic form of congenital herpes, or disseminated herpes infection, occurs when the entire body becomes infected with herpes. It affects more than just the baby’s skin and can cause serious complications, such as:
- eye inflammation
- blindness
- seizures and seizure disorders
- respiratory illnesses
The disease might also affect the baby’s vital organs, including the:
- lungs, causing difficulty breathing and interruption in breathing
- kidneys
- liver, causing jaundice
- central nervous system (CNS), causing seizures, shock, and hypothermia
The HSV can also cause a dangerous condition known as encephalitis, an inflammation of the brain that may lead to brain damage.
Diagnosing birth-acquired herpes
Your doctor will take samples of the blisters (if they are present) and spinal cord fluid to determine if herpes is the cause of illness. A blood or urine test may also be used. Further diagnostic testing might include MRI scans of the baby’s head to check for brain swelling.
A blood or urine test may also be used. Further diagnostic testing might include MRI scans of the baby’s head to check for brain swelling.
Birth-acquired herpes treatment
The herpes virus can be treated, but not cured. This means the virus will remain in your child’s body throughout their life. However, the symptoms can be managed.
Your child’s pediatrician will likely treat the infection with antiviral medications given through an IV, a needle or tube that goes into a vein.
Acyclovir (Zovrax) is the most commonly used antiviral medication for birth-acquired herpes. Treatment usually spans a few weeks and may include other medications to control seizures or treat shock.
Herpes prevention
You can prevent herpes by practicing safe sex.
Condoms can minimize exposure to an active herpes outbreak and prevent transmission of the virus. You should also talk to your partner about their sexual history and ask if they have herpes.
If you’re pregnant and you or your partner have herpes or have had it in the past, discuss your situation with your doctor well before your due date.
You may be given medicine toward the end of your pregnancy to help reduce the chance of passing on herpes to your baby. You may also be able to have a cesarean delivery if you have active genital lesions. A cesarean delivery can lower the risk of passing herpes on to your baby.
In a cesarean delivery, the baby is delivered through incisions made in the mother’s abdomen and uterus. This will keep your baby from coming into contact with the virus in the birth canal.
Long-term outlook for birth-acquired herpes
Herpes is inactive at times, but it can come back repeatedly even after treatment.
Babies with systemic herpes infections may not even respond to treatment and can possibly face several additional health risks. Disseminated birth-acquired herpes may be life-threatening and can cause neurological problems or coma.
Since there’s no cure for herpes, the virus will stay in the child’s body. Parents and caretakers must watch for symptoms of herpes throughout the child’s life. When the child is old enough, they’ll need to learn how to prevent spreading the virus to others.
When the child is old enough, they’ll need to learn how to prevent spreading the virus to others.
Last medically reviewed on August 31, 2018
- Parenthood
- Baby
- 06 Months
Medically reviewed by Karen Gill, M.D. — By Erica Roth on August 31, 2018
related stories
Everything You Need to Know About Oral and Genital Herpes
Herpes and Pregnancy: What You Need to Know
Suppressive Treatment for Genital Herpes in Pregnancy
The Best Baby Booties to Keep Those Tootsies Warm
10 Mini Crib Mattresses and Top Shopping Tips
Read this next
Everything You Need to Know About Oral and Genital Herpes
Medically reviewed by Jenneh Rishe, RN
The herpes simplex virus, also known as HSV, is a viral infection that causes genital and oral herpes. Get the details on key signs, diagnosis, and…
READ MORE
Herpes and Pregnancy: What You Need to Know
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Genital herpes can be transmitted to a baby during pregnancy and delivery.
 If you think you may have genital herpes, be tested and treated before your…
If you think you may have genital herpes, be tested and treated before your…READ MORE
Suppressive Treatment for Genital Herpes in Pregnancy
Medically reviewed by Aleah Rodriguez, PharmD
Women with genital herpes should use antiviral medication throughout pregnancy to decrease the risk of recurrent lesions and of transmission to the…
READ MORE
The Best Baby Booties to Keep Those Tootsies Warm
Medically reviewed by Mia Armstrong, MD
For growing babies, the best baby booties mix style, function, and warmth. Here are our favorites in 11 categories.
READ MORE
10 Mini Crib Mattresses and Top Shopping Tips
Medically reviewed by Carissa Stephens, R.N., CCRN, CPN
The best mini crib mattress is firm enough to fit snugly in a crib and keep your little one comfortable.
READ MORE
Do You Need to Worry When Your Baby Has an Ear Infection?
Medically reviewed by Karen Gill, M.D.
Ear infection in a baby is swelling of the middle ear caused by bacteria or viruses in fluids that collect behind the eardrum. Here's how to know when…
READ MORE
When Do Babies Start to Roll Over?
Medically reviewed by Karen Gill, M.D.
After a few months of your little one staying pretty much where you put them, you may lay them on their play mat and find them halfway across the room.
READ MORE
12 Best Healthy, Scrumptious Kid Snacks for 2022
Medically reviewed by Jillian Kubala, MS, RD
The best remedy for cranky kids on the go? A quick snack. These are a few of our favorite store-bought kid snacks for fighting hunger.
READ MORE
The Best Baby Strollers
Medically reviewed by Carissa Stephens, R.N., CCRN, CPN
We've rounded up the best baby strollers, whether you're looking for a stroller for a newborn, for traveling, for city life, and more.
READ MORE
The 14 Best Bottle Warmers of 2022
Medically reviewed by Karen Gill, M.D.
Whether or not you decide you need a bottle warmer is entirely up to you. If you do decide to go the technical route, we've rounded up the best bottle…
READ MORE
Causes, Symptoms, Picture, and Prevention
Birth-Acquired Herpes: Causes, Symptoms, Picture, and PreventionMedically reviewed by Karen Gill, M.D. — By Erica Roth on August 31, 2018
What is birth-acquired herpes?
Birth-acquired herpes is a herpes virus infection that an infant gets during delivery or, less commonly, while still in the womb. The infection can also develop shortly after birth. Babies with birth-acquired herpes get the infection from mothers who are infected with genital herpes.
The infection can also develop shortly after birth. Babies with birth-acquired herpes get the infection from mothers who are infected with genital herpes.
Birth-acquired herpes is sometimes also called congenital herpes. The word congenital refers to any condition that’s present from birth.
Infants who are born with herpes may have a skin infection or a system-wide infection called systemic herpes, or both. Systemic herpes is more serious and can cause a variety of issues. These issues may include:
- brain damage
- breathing problems
- seizures
According to Boston Children’s Hospital, herpes occurs in approximately 30 out of every 100,000 births.
It’s a serious condition and can be life-threatening.
Causes of birth-acquired herpes
The herpes simplex virus (HSV) causes birth-acquired herpes. The highest risk for birth-acquired herpes is during a mother’s first, or primary, infection.
After someone recovers from herpes, the virus lies dormant in their body for long periods before it flares up and symptoms appear or reappear. When the virus reactivates, it’s called a recurrent infection.
When the virus reactivates, it’s called a recurrent infection.
Women who have active herpes infections are more likely to pass the virus on to their babies during a vaginal birth. The infant comes into contact with herpes blisters in the birth canal, which can cause infection.
Mothers who have a nonactive herpes infection when they deliver can also transmit herpes to their child, particularly if they acquired herpes for the first time during pregnancy.
Most babies with HSV infection are born to mothers with no history of herpes or active infection. This is, in part, because measures are taken to prevent birth-acquired herpes in babies born to mothers who are known to be infected.
You should note that your infant could also get herpes through contact with cold sores. Another form of the HSV causes cold sores on the lips and around the mouth. Someone who has a cold sore can pass the virus on to others through kissing and other close contact. This would be considered neonatal herpes, rather than birth-acquired herpes, and is usually less severe.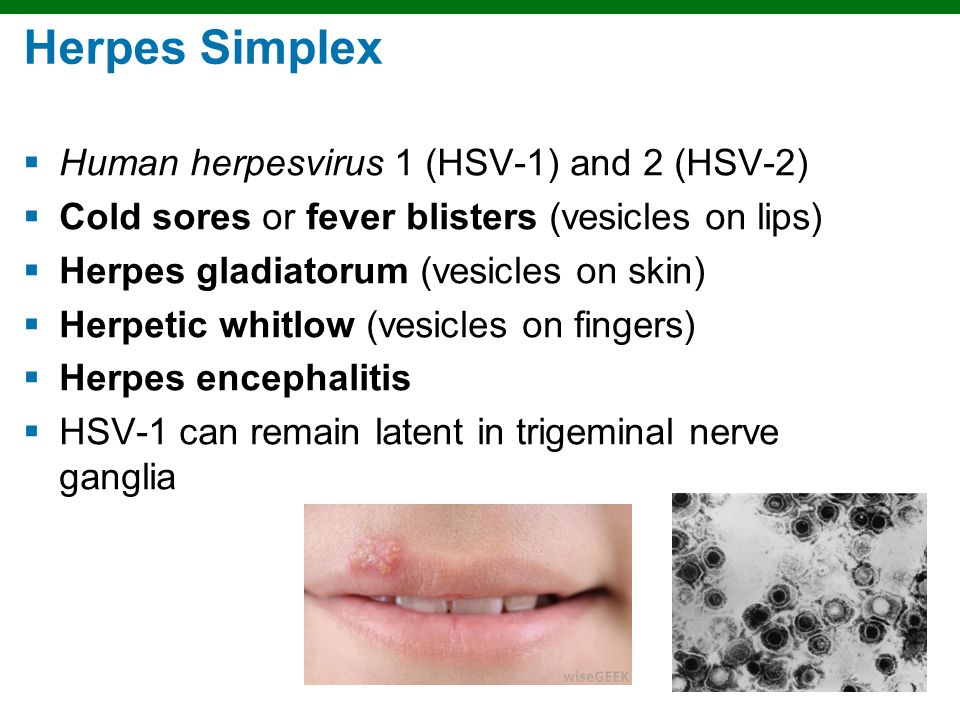
Recognizing the symptoms of birth-acquired herpes
The symptoms of birth-acquired herpes usually appear within the first few weeks of the baby’s life and may be present at birth.
Birth-acquired herpes is easiest to identify when it appears as a skin infection. The baby may have clusters of fluid-filled blisters on their torso or around their eyes.
The blisters, called vesicles, are the same type of blisters that appear on the genital regions of adults with herpes. The vesicles may burst and crust over before healing. An infant can be born with the blisters or develop the sores a week after birth.
Infants with birth-acquired herpes might also appear extremely tired and have trouble feeding.
Complications associated with birth-acquired herpes
The systemic form of congenital herpes, or disseminated herpes infection, occurs when the entire body becomes infected with herpes. It affects more than just the baby’s skin and can cause serious complications, such as:
- eye inflammation
- blindness
- seizures and seizure disorders
- respiratory illnesses
The disease might also affect the baby’s vital organs, including the:
- lungs, causing difficulty breathing and interruption in breathing
- kidneys
- liver, causing jaundice
- central nervous system (CNS), causing seizures, shock, and hypothermia
The HSV can also cause a dangerous condition known as encephalitis, an inflammation of the brain that may lead to brain damage.
Diagnosing birth-acquired herpes
Your doctor will take samples of the blisters (if they are present) and spinal cord fluid to determine if herpes is the cause of illness. A blood or urine test may also be used. Further diagnostic testing might include MRI scans of the baby’s head to check for brain swelling.
Birth-acquired herpes treatment
The herpes virus can be treated, but not cured. This means the virus will remain in your child’s body throughout their life. However, the symptoms can be managed.
Your child’s pediatrician will likely treat the infection with antiviral medications given through an IV, a needle or tube that goes into a vein.
Acyclovir (Zovrax) is the most commonly used antiviral medication for birth-acquired herpes. Treatment usually spans a few weeks and may include other medications to control seizures or treat shock.
Herpes prevention
You can prevent herpes by practicing safe sex.
Condoms can minimize exposure to an active herpes outbreak and prevent transmission of the virus. You should also talk to your partner about their sexual history and ask if they have herpes.
You should also talk to your partner about their sexual history and ask if they have herpes.
If you’re pregnant and you or your partner have herpes or have had it in the past, discuss your situation with your doctor well before your due date.
You may be given medicine toward the end of your pregnancy to help reduce the chance of passing on herpes to your baby. You may also be able to have a cesarean delivery if you have active genital lesions. A cesarean delivery can lower the risk of passing herpes on to your baby.
In a cesarean delivery, the baby is delivered through incisions made in the mother’s abdomen and uterus. This will keep your baby from coming into contact with the virus in the birth canal.
Long-term outlook for birth-acquired herpes
Herpes is inactive at times, but it can come back repeatedly even after treatment.
Babies with systemic herpes infections may not even respond to treatment and can possibly face several additional health risks. Disseminated birth-acquired herpes may be life-threatening and can cause neurological problems or coma.
Disseminated birth-acquired herpes may be life-threatening and can cause neurological problems or coma.
Since there’s no cure for herpes, the virus will stay in the child’s body. Parents and caretakers must watch for symptoms of herpes throughout the child’s life. When the child is old enough, they’ll need to learn how to prevent spreading the virus to others.
Last medically reviewed on August 31, 2018
- Parenthood
- Baby
- 06 Months
Medically reviewed by Karen Gill, M.D. — By Erica Roth on August 31, 2018
related stories
Everything You Need to Know About Oral and Genital Herpes
Herpes and Pregnancy: What You Need to Know
Suppressive Treatment for Genital Herpes in Pregnancy
The Best Baby Booties to Keep Those Tootsies Warm
10 Mini Crib Mattresses and Top Shopping Tips
Read this next
Everything You Need to Know About Oral and Genital Herpes
Medically reviewed by Jenneh Rishe, RN
The herpes simplex virus, also known as HSV, is a viral infection that causes genital and oral herpes.
 Get the details on key signs, diagnosis, and…
Get the details on key signs, diagnosis, and…READ MORE
Herpes and Pregnancy: What You Need to Know
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Genital herpes can be transmitted to a baby during pregnancy and delivery. If you think you may have genital herpes, be tested and treated before your…
READ MORE
Suppressive Treatment for Genital Herpes in Pregnancy
Medically reviewed by Aleah Rodriguez, PharmD
Women with genital herpes should use antiviral medication throughout pregnancy to decrease the risk of recurrent lesions and of transmission to the…
READ MORE
The Best Baby Booties to Keep Those Tootsies Warm
Medically reviewed by Mia Armstrong, MD
For growing babies, the best baby booties mix style, function, and warmth.
 Here are our favorites in 11 categories.
Here are our favorites in 11 categories.READ MORE
10 Mini Crib Mattresses and Top Shopping Tips
Medically reviewed by Carissa Stephens, R.N., CCRN, CPN
The best mini crib mattress is firm enough to fit snugly in a crib and keep your little one comfortable.
READ MORE
Do You Need to Worry When Your Baby Has an Ear Infection?
Medically reviewed by Karen Gill, M.D.
Ear infection in a baby is swelling of the middle ear caused by bacteria or viruses in fluids that collect behind the eardrum. Here's how to know when…
READ MORE
When Do Babies Start to Roll Over?
Medically reviewed by Karen Gill, M.D.
After a few months of your little one staying pretty much where you put them, you may lay them on their play mat and find them halfway across the room.
READ MORE
12 Best Healthy, Scrumptious Kid Snacks for 2022
Medically reviewed by Jillian Kubala, MS, RD
The best remedy for cranky kids on the go? A quick snack. These are a few of our favorite store-bought kid snacks for fighting hunger.
READ MORE
The Best Baby Strollers
Medically reviewed by Carissa Stephens, R.N., CCRN, CPN
We've rounded up the best baby strollers, whether you're looking for a stroller for a newborn, for traveling, for city life, and more.
READ MORE
The 14 Best Bottle Warmers of 2022
Medically reviewed by Karen Gill, M.D.
Whether or not you decide you need a bottle warmer is entirely up to you. If you do decide to go the technical route, we've rounded up the best bottle…
READ MORE
Herpes, cytomegalovirus, Epstein-Barr virus in pregnancy
Expecting a baby is always stressful for the female body, which has to work hard for nine months. And during pregnancy, the expectant mother has a lot of reasons for unrest. Infection with any infectious disease causes serious consequences that negatively affect both the condition of the pregnant woman and the child. Let's consider these diseases in more detail.
And during pregnancy, the expectant mother has a lot of reasons for unrest. Infection with any infectious disease causes serious consequences that negatively affect both the condition of the pregnant woman and the child. Let's consider these diseases in more detail.
Herpes
The concept of "herpes during pregnancy" is too broad and often becomes a cause for unreasonable panic among pregnant women who do not know what and in what cases a threat to their unborn child may appear. It is important for a pregnant woman to have information about all the features of this disease at different stages of pregnancy in order to contact a gynecologist in time and understand when there is really a danger to the fetus when a cold appears on the lips.
If a woman in an interesting position has a recurrent form of the virus, that is, she has already encountered it before pregnancy, almost any manifestation of herpes is not dangerous for the mother and child. A simple herpes virus can only be a threat during pregnancy if it is a primary infection, especially in the early stages, when all the internal organs of the baby are laid and, most dangerously, the neural tube. Only in the case of primary infection in the early stages of pregnancy, up to the second trimester, the virus poses a threat, as it can lead to missed pregnancy, miscarriage, and developmental abnormalities. However, this clinical situation is more likely to be an exception to the rule, because most women repeatedly experience herpes before pregnancy.
Only in the case of primary infection in the early stages of pregnancy, up to the second trimester, the virus poses a threat, as it can lead to missed pregnancy, miscarriage, and developmental abnormalities. However, this clinical situation is more likely to be an exception to the rule, because most women repeatedly experience herpes before pregnancy.
Cytomegalovirus
For a pregnant woman, the virus is dangerous during the primary infection during the expectation of a child. Infection from a sick person with an acute cytomegalovirus infection is the worst option for a pregnant woman, because due to the lack of antibodies in the blood, the virus easily crosses the placenta and has a negative effect on the fetus. According to statistics, infection of the fetus occurs in 40-50% of cases. The degree of adverse effect of the virus on the fetus depends on the duration of pregnancy. If the fetus is infected in early pregnancy, there is a high probability of spontaneous miscarriage or anomalies in the development of the child. If the infection happened at a later date, no fetal malformations are observed, but polyhydramnios often occurs during pregnancy, premature birth and the so-called "congenital cytomegaly" of the newborn are noted. Such children may have jaundice, enlarged liver and spleen, and anemia.
If the infection happened at a later date, no fetal malformations are observed, but polyhydramnios often occurs during pregnancy, premature birth and the so-called "congenital cytomegaly" of the newborn are noted. Such children may have jaundice, enlarged liver and spleen, and anemia.
Eppstein-Barr virus
The Epstein-Barr virus predisposes to premature termination of pregnancy, fetal malnutrition, in newborn children causes damage to the nervous system, organs of vision, recurrent chroniosepsis, hepatopathy and respiratory distress syndrome. However, this virus provokes the listed pathologies only under certain conditions, in the presence of which during pregnancy it becomes dangerous. It is very bad if a pregnant woman has not previously encountered the Eppstein-Barr virus, which is why she does not have antibodies to this virus in her body. If there was still contact, and antibodies were found after treatment, then this is a good sign, because in this case there is nothing to be afraid of. This serves as evidence that if a woman's body is re-infected, it will cope with this dangerous disease on its own. This means that a pregnant woman will not have to take heavy and rather dangerous drugs for the development of the fetus.
This serves as evidence that if a woman's body is re-infected, it will cope with this dangerous disease on its own. This means that a pregnant woman will not have to take heavy and rather dangerous drugs for the development of the fetus.
THERE ARE CONTRAINDICATIONS. YOU NEED TO CONSULT WITH A SPECIALIST
The materials posted on this page are for informational purposes and are intended for educational purposes. Site visitors should not use them as medical advice. Determining the diagnosis and choosing a treatment method remains the exclusive prerogative of your doctor!
Reproductive Health Training CenterReproductive Health Training Center
Having genital herpes does not mean you cannot have children. According to the American Public Health Association (ASHA), only 0.1% of cases of herpes are transmitted during pregnancy from mother to unborn child. Most women with genital herpes successfully carry out pregnancy and give birth to healthy children .
Breast-feeding during herpes recurrence is possible. Except when herpetic eruptions are located on the nipples or mammary gland. If your doctor prescribes oral antiviral drugs during breastfeeding, the question of the advisability of continuing breastfeeding during the course of suppressive therapy should be discussed with your doctor.
The initial episode of genital herpes is usually a tragedy during pregnancy. It is characterized by pronounced manifestations, tk. there are no antibodies in the mother's body that protect against herpes. For the fetus, the risk is especially high when infected with genital herpes in the first and third trimesters. As a rule, fetal death and miscarriage occur in the first trimester. Damage to the developing organs of the fetus, the occurrence of congenital deformities are possible. Infection in the III trimester, especially after 36 weeks of pregnancy, is fraught with damage to the nervous system of the fetus, skin, liver, spleen. Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
HOW TO DETECT THAT I HAVE A PRIMARY EPISODE OF GENITAL HERPES?
What does primary episode mean? It means that in your life there has never been a recurrence of genital herpes and the body has not yet developed protective antibodies to HSV.
In some cases it is difficult to determine: what is it? Whether the first episode of genital herpes in life or the first recurrence with visible symptoms of genital herpes that was previously asymptomatic or with atypical symptoms. The fact is that in most people infected with HSV, the disease is almost asymptomatic. It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo.
It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo. If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
There are no specific methods for preventing the transmission of genital herpes during pregnancy. From non-specific, monogamous relationships, constant use of a condom can be recommended. If it is known that the father of the child is infected with genital herpes, and the mother is not, then you should either completely refrain from sexual activity during pregnancy (until the moment of delivery). Or a man should constantly use a condom + valaciclovir 1 tablet daily throughout the pregnancy. This measure will help to reduce the risk of transmission of genital herpes by 75%.
Should refrain from oral sex. Because if you have never had herpes of the lips in your life, and the husband or father of the child had it, then during cunniling he can bring the herpes simplex virus type I to your genitals. And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
Treatment with acyclovir and valtrex. However, these drugs do not always allow to achieve good success in treatment.
According to the Centers for Disease Control (USA), the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect the development of the fetus. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Against the background of a primary episode of genital herpes, the loss of a desired pregnancy is a severe psychological trauma for both potential parents. But in any case, there is hope. The next pregnancy will proceed already against the background of recurrent genital herpes. After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
Recurrent genital herpes during pregnancy
As blasphemous as it may sound, but recurrent genital herpes is the most favorable option during pregnancy. If a woman before the onset of this pregnancy already had relapses of genital herpes, then the fetus is protected from infection by maternal antibodies that block the action of the herpes simplex virus. There is a 99% chance that your child will not get herpes.
STATISTICS:
During pregnancy, infection of a newborn with the herpes simplex virus from a mother with recurrent genital herpes occurs quite rarely: in approximately 0.02% of cases.
The risk of infection of a child in childbirth from a mother suffering from recurrent genital herpes is less than 1% (According to the study: Brown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L. Effect of serological status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
Effect of serological status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
BEFORE PREGNANCY: Plan the onset of pregnancy , eliminate bad habits from your life, heal chronic diseases, take a course of restorative treatment, cure foci of chronic infection before pregnancy (sore teeth, sinusitis, gastritis).
In some cases, a woman cannot know whether she had recurrences of genital herpes before or not. This happens with herpes that occurs without symptoms or with an atypical course. In addition, it should be borne in mind that, unlike the stronger sex, the female genital organs are “not visible”. In order to find out if you have ever had a relapse, you should do a serological analysis. Donate blood for antibodies (immunoglobulins Ig G & Ig M) to HSV-1,2. If Ig G is present in the blood, then herpes is recurrent - herpes practically does not threaten pregnancy. The Ig G index is qualitative (higher than diagnostic titers). Regardless of the titer (the amount of Ig G & M), you can become pregnant.
Regardless of the titer (the amount of Ig G & M), you can become pregnant.
DURING PREGNANCY:
- When having sex always use a condom ;
- Avoid oral sex
If you get cold sores during pregnancy, you can transfer it to the penis of the father of your unborn child during oral sex. And he will transfer the infection to your genital tract with this member. This can lead to bad consequences for the child. On the other hand, if you allow your husband to cunniling and he has cold sores on his lips, he may bring a different type of herpes to your genitals. That's why it's better not to joke with oral sex during pregnancy - 9You can grind months in the name of a new life.
PROPHYLAXIS DURING PREGNANCY:
To prevent recurrence during pregnancy after 36 weeks, your doctor may prescribe a course of preventive treatment with acyclovir or valaciclovir. During pregnancy, it is better to use acyclovir, manufactured by GlaxoSmithKline under the name Zovirax or Valtrex. Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
According to the Centers for Disease Control (USA), the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect the development of the fetus. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
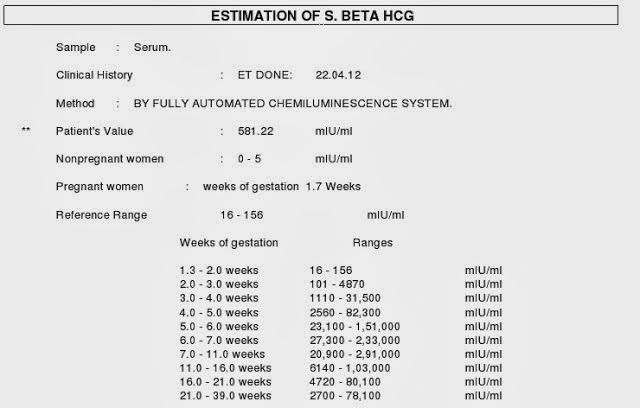
Dynamic monitoring : Examination of pregnant women includes a mandatory three-time ultrasound examination: at 10-14 weeks of gestation, when the thickness of the nuchal space of the fetus is mainly assessed; at 20-24 weeks, ultrasound is performed to detect malformations and echographic markers of chromosomal diseases; an ultrasound examination at 32–34 weeks is performed in order to detect malformations with their late manifestation, as well as for the purpose of a functional assessment of the fetal condition. In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
Treatment: Only under medical supervision and prescription! Outwardly, you can use an ointment based on acyclovir. Ointments and creams are over-the-counter products. The ointment does not affect the fetus, because. it is not absorbed into the blood. To prevent rashes 2 weeks before delivery, the doctor may prescribe valacyclovir or acyclovir orally.
PROPHYLAXIS DURING DELIVERY:
Treatment of the soft birth canal with polyvidone iodine (betadine, vocadine) or other antiseptics during childbirth can reduce the risk of neonatal herpes infection to the child to Genital herpes - abortion or childbirth?
Many women with recurrent genital herpes wonder how their illness might affect their unborn child.
The editor of the server received a letter describing a typical example of the illiterate approach of Soviet doctors to the management of pregnant women with genital herpes:
Professor D ***, from the Chelyabinsk Medical Academy, believes that it is highly undesirable to keep the pregnancy during an exacerbation of genital herpes in the early stages of pregnancy. He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
In developed countries, the optimal tactics for managing pregnant women with genital herpes has long been developed, based not on the private opinion of some “Professor D *** from the Chelyabinsk Medical Academy”, but on the data of long-term clinical studies and observations.
So that someone's subjective opinion does not lead you to an unnecessary abortion, we will tell you once again about what to do if you have herpes and pregnancy.
If a woman has the first time in her life during pregnancy there is a recurrence of genital herpes (primary genital herpes) or if the mother-to-be becomes infected with genital herpes during pregnancy, the fetus may be affected. The fact is that in this case, the mother's blood does not contain antibodies to the Herpes Simplex Virus - immunoglobulins G and Em (Ig G and Ig M), which block the pathological effect of the herpes simplex virus on fetal cells.
In the case of the first recurrence of genital herpes in a woman's life, the virus can penetrate the placenta and multiply in the tissues of the embryo or fetus, which leads to fetal death, miscarriage, congenital deformities, damage to the brain, liver, and other organs of the fetus, non-developing pregnancy. The risk of fetal damage in primary genital herpes is 75%.
If the first recurrence of genital herpes occurs 30 days before delivery, delivery by caesarean section is recommended.
From 36 weeks of pregnancy, a doctor may prescribe Zovirax tablets to prevent the recurrence of herpes.
To prevent infection with genital herpes during pregnancy, it is imperative to use a condom and avoid oral sex, i. a man should not caress the sexual organs of a pregnant woman with his mouth. The reverse situation is allowed.
If a woman had recurrences of genital herpes before pregnancy, then antiherpetic antibodies float in the pregnant woman's blood, which limit the infection and neutralize the virus. These antibodies pass through the placenta to the fetus, protecting it. Therefore, recurrent genital herpes is not so dangerous during pregnancy. In this case, due to herpes, there are no deformities and lesions of internal organs.
In recurrent genital herpes , the baby can become infected during childbirth, passing through the birth canal, where the herpes virus is present. The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
Recurrent genital herpes is not an indication for abortion.
And despite all our clarifications about the relative safety of recurrent genital herpes during pregnancy, sometimes you have to receive such letters: A woman with recurrent genital herpes writes: “And most importantly, herpes is just natural selection. Nature removes lepers, because their offspring are doomed to death, so I don’t even dream of children ... ”It is ignorant to consider yourself a leper and refuse the happiness of motherhood just because you have recurrent genital herpes (the most favorable form for bearing and childbirth). Although, it cannot be ruled out that this is our medical defect.
There is also such a diagnosis as non-primary genital herpes . What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
Use of immunomodulators during pregnancy
The server editor received a letter describing a typical clinical situation:
« I have a problem that requires urgent consultation. My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
In my opinion, the use of immunomodulators during pregnancy is IMPOSSIBLE:
* In this case, herpes on the lips of a woman cannot bring any harm to either the woman or the child.
*Long-term effect of immunomodulatory drugs on the fetus is unknown. As you know, some of these drugs, easily penetrating the placenta into the body of the fetus, can cause congenital deformities in the latter, disorders of the immune system, and increase the risk of developing cancer.