Pregnancy and head cold
Pregnant with a cold: Treatments, risks, and prevention
Catching a cold during pregnancy will not harm the fetus, but it can be uncomfortable for the person who is pregnant, and they may also worry about which treatments and medications they can use safely.
Colds are very common. The Centers for Disease Control and Prevention (CDC) estimate that adults have an average of 2–3 colds per year.
The chances of catching a cold while pregnant are higher because the immune system is less robust during pregnancy.
According to March of Dimes, catching a cold will not harm a developing fetus, and the pregnant person will typically recover in a week or so.
People are also more likely to catch potentially more serious infections, such as the flu, during pregnancy. This means that taking steps to prevent illness is important during pregnancy.
This article looks at what to consider when treating the symptoms of a cold during pregnancy, how to prevent a cold, and when to see a doctor.
Treating a cold usually means using over-the-counter (OTC) medications. However, many pregnant people worry about whether drugs will affect the fetus.
The Food and Drug Administration (FDA) recommend always talking to a doctor before using any pain medication during pregnancy.
Most OTC drugs contain the same few ingredients to treat cold symptoms. The following sections look at the safety of different types of cold treatments.
Pain relievers
Pain relievers are a group of drugs that reduce pain. Some types also reduce inflammation and fever.
OTC pain medications include:
- acetaminophen, under brand names such as Tylenol
- nonsteroidal anti-inflammatory drugs (NSAIDs), including naproxen, ibuprofen, and aspirin
Research suggests that acetaminophen is the safest pain relief drug to use during pregnancy, with recommendations to use the lowest effective dosage for the shortest time.
An article published in American Family Physician (AFP) reports acetaminophen to be safe to use during all trimesters on its own, but not necessarily in combination with other cold remedies that contain a range of other ingredients.
However, the article states that NSAIDs may carry risks. They recommend avoiding aspirin during pregnancy except for specific uses and avoiding naproxen and ibuprofen during the third trimester.
Prescription drugs tend to be stronger than OTC drugs and are more likely to carry risks.
The FDA note that prescription NSAIDs may increase the risk of pregnancy loss during the first half of pregnancy and that prescription opioids may increase the risk of birth abnormalities when taken in the first trimester.
Severe and persistent pain can lead to serious effects, such as high blood pressure, depression, and anxiety. It is important to weigh the benefits of taking pain relief drugs during pregnancy against the potential risks.
Always talk to a healthcare professional before deciding to take any medication that relieves pain during pregnancy.
Cough suppressants
OTC cough suppressants often contain medications such as dextromethorphan and guaifenesin.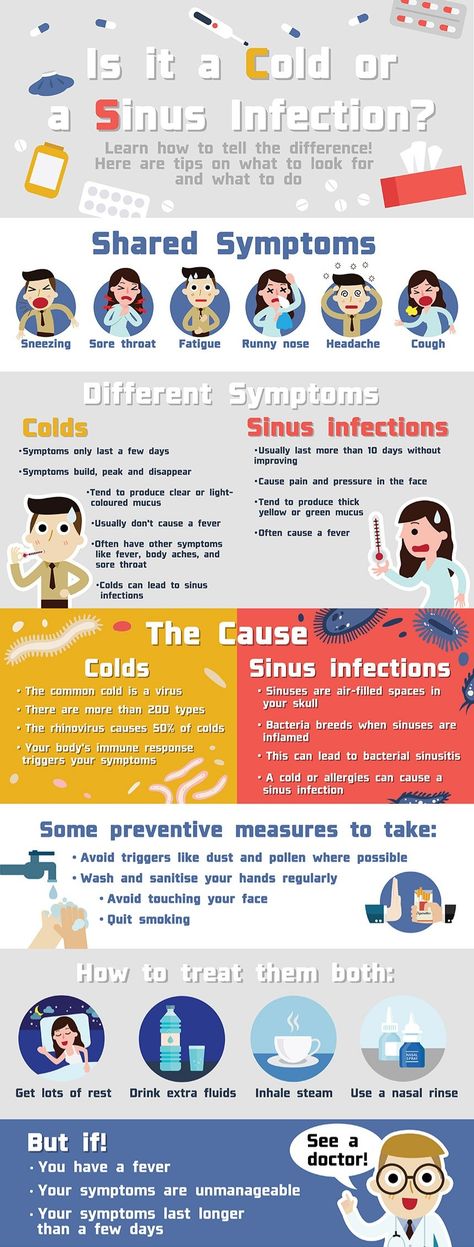
According to the AFP, these medications appear to be safe during pregnancy in the correct doses. However, it may be best to consider drug-free options as the first line of defense.
For example, before using a cough suppressant medication, people can try using herbal or mentholated throat lozenges to ease a cough or sore throat.
Read more about natural cough remedies here.
Antihistamines
Antihistamines are a popular allergy medication that may relieve a runny nose, watery eyes, or sneezing caused by a cold.
Up to 15% of people use antihistamines during pregnancy, and experts generally consider them safe.
According to the American College of Allergy, Asthma, and Immunology (ACCAI), people can use the following during pregnancy:
- diphenhydramine (Benadryl)
- chlorpheniramine (ChlorTrimeton)
- loratadine (Claritin)
- cetirizine (Zyrtec)
Most OTC antihistamines are safe to take in pregnancy as long as a doctor approves them.
Read about some natural antihistamines here.
Decongestants
According to one source, it is safe to take decongestants, such as pseudoephedrine, when directed by a healthcare provider.
However, research has not yet established that decongestants are safe during pregnancy. Some studies suggest that some decongestants, including pseudoephedrine and phenylephrine, may increase the risk of birth abnormalities.
The overall evidence suggests that people use decongestants sparingly during pregnancy, especially during the first trimester.
Saline nasal sprays and nasal strips are safe alternatives for nasal congestion.
Natural remedies
Resting while sick is important to give the body time to focus on recovery. Lying down with the head elevated may help with breathing and stuffiness.
Drinking plenty of water can help people recover from a cold. Juices and smoothies can also provide nutritional intake when people have no appetite.
Many people also use room humidifiers to help clear a stuffy nose and promote a productive cough.
Applying warm compresses to the head, sinuses, and shoulders may help reduce pain and congestion.
Read more about natural remedies for a cold or flu here.
People are also more likely to catch colds and the flu during pregnancy, so it is important to take steps to prevent illness.
To prevent the common cold, the CDC recommend:
- washing the hands often with soap and water for 20 seconds, or using an alcohol-based hand sanitizer when this is not possible
- avoiding touching the face with unwashed hands because viruses that cause colds can enter the body through the eyes, nose, and mouth
- staying away from people who are sick as close contact with others can spread cold viruses.
Light to moderate pregnancy-safe exercises, such as swimming and indoor cycling, can boost the immune system and increase metabolism.
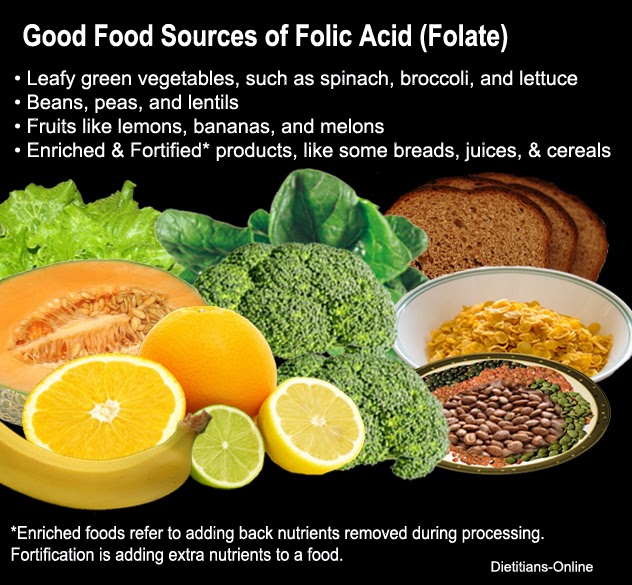
Healthful eating is another important factor in preventing a cold. Focusing on eating a variety of fresh foods can help ensure the body gets the nutrients it needs.
Taking a prenatal vitamin that includes zinc and vitamin C may also help support the immune system and prevent colds.
Many people experience pregnancy rhinitis, which has symptoms similar to a cold.
This occurs due to inflammation and swelling of the mucous membranes in the nose, extra fluid in the body, and changing hormone levels.
Pregnancy rhinitis occurs in around 20% of people. Some people may find it difficult to distinguish rhinitis from a common cold.
The symptoms of pregnancy rhinitis include:
- a runny nose
- congestion
- sneezing
- difficulty breathing
- snoring
A cold during pregnancy is the same as any other cold. The common cold is not likely to not harm the mother or fetus.
People may catch a cold or flu from being around others who are sick. The CDC provide guidance on how to avoid catching the flu.
It is important to know the difference between a cold and the flu. The two have similar symptoms, but the flu tends to be more severe, and a person will usually have a fever.
Read more about pregnancy and the flu here.
If someone experiences a fever during pregnancy, they should contact their doctor to see what steps they can take to reduce the fever to safe levels as quickly as possible.
Having a cold during pregnancy will not usually affect the fetus. Colds are mild illnesses that a person’s immune system can handle relatively easily.
However, the person’s temperature and infections can affect the fetus. If a person is experiencing a fever or other signs of infection, it is essential to speak with a doctor immediately to find the best way to reduce these symptoms.
When a person is pregnant, their body deals with a cold in much the same way as it does at any other time. The symptoms are temporary, and in most cases, the cold will be gone in 7–10 days.
If someone experiences the following symptoms during pregnancy, they should talk to a doctor right away:
- a fever of over 100.4° F
- severe or unusual symptoms
- symptoms that last more than 10 days
- symptoms of the flu
- violent coughing that makes it hard to breathe
Colds are very common during pregnancy, and they are unlikely to harm the pregnant person or fetus.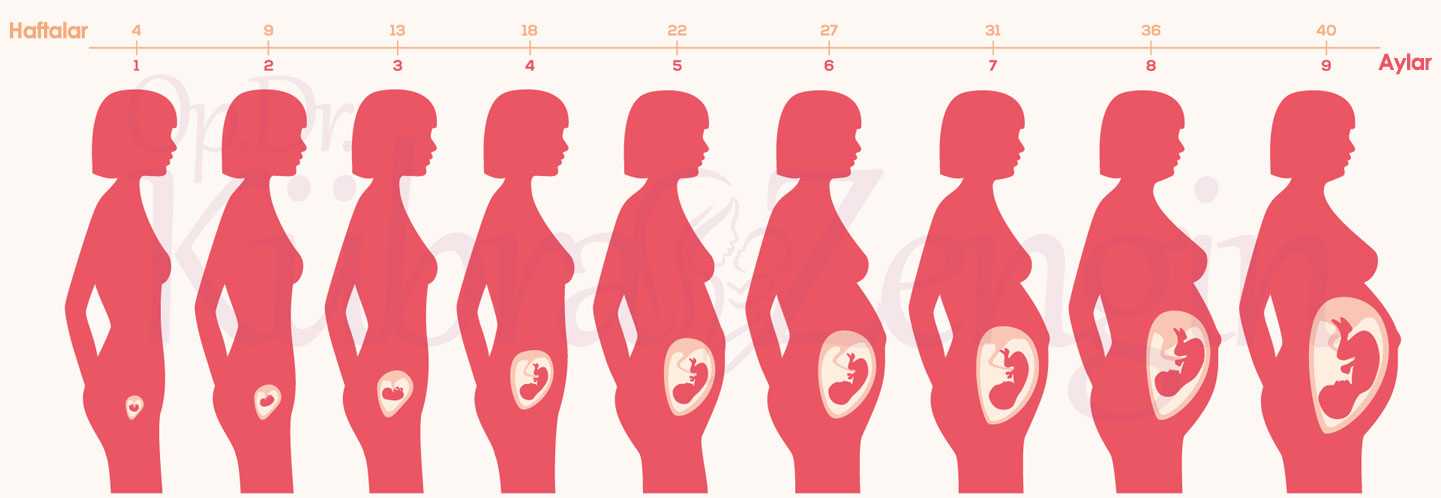
While there are some uncertainties over the safety of OTC cold remedies during pregnancy, most people can relieve their symptoms using gentle home remedies. Most people will feel better in around a week.
Cold or flu: What are the differences?
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Medical News Today only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Colds and the flu are very common seasonal infections. They can have similar symptoms, but there are key differences.
The common cold and influenza, commonly known as the flu, are very prevalent in the winter months.
The main difference between a cold and the flu is that the flu generally has more severe symptoms and possible complications.
Adults catch an average of two or three colds per year, and children get more. The flu is less common, but it still affects about 8% of the United States population each season.
According to the Centers for Disease Control and Prevention (CDC), more than 35.5 million people caught the flu during the 2018–2019 flu season, resulting in close to 34,000 deaths.
This article looks at the differences between a cold and the flu, along with ways to treat the symptoms and prevent these seasonal infections.
There are several key differences between these two illnesses.
Causes
More than 200 different viruses, including rhinoviruses and some coronaviruses (not the one responsible for coronavirus disease 2019, or COVID-19), can cause the common cold.
Influenza viruses are responsible for the flu, with three main types affecting humans: influenza A, B, and C. The most common types during flu season are A and B.
Symptoms
As the common cold and the flu have similar symptoms, it can be tricky or even impossible to know which of these illnesses a person has.
In general, the flu is worse than a cold. While the symptoms of a cold come on gradually, flu symptoms begin abruptly, and they tend to be more intense.
A runny or stuffy nose is more common with a cold. On the other hand, the following symptoms are common with the flu but uncommon with a cold:
- fever — a temperature of 100°F (37.8°C or higher) — that lasts 3–4 days
- muscle aches, particularly in the lower back
- chills
- fatigue or weakness
- a headache
Neither vomiting nor diarrhea is usually associated with the common cold, but both can be present in the flu.
People may have the flu without key symptoms such as fever. To know for sure whether they have a cold or the flu, a person can get a special diagnostic test within a few days of their symptoms starting.
To know for sure whether they have a cold or the flu, a person can get a special diagnostic test within a few days of their symptoms starting.
The symptoms of a cold or the flu are also similar to those of other respiratory illnesses, including COVID-19, which the SARS-CoV-2 virus causes.
Complications
Colds do not usually lead to any further issues, although they can increase the chance of people with asthma having an asthma attack. Conversely, the flu can lead to severe complications, such as pneumonia or bacterial infections. Each year, flu-related complications cause thousands of hospitalizations and deaths.
Most people recover from the flu in a few days to 2 weeks. Cold symptoms, which are generally milder, typically peak within 2–3 days and then get better gradually over a week or two.
Transmission
People can catch colds and flu in the same way. Both viruses are contagious and can transfer to a person who:
- has close contact with someone who has the virus
- breathes in respiratory droplets that contain the virus
- touches a contaminated surface
Learn more about the differences between the flu and COVID-19 here.
For more information and resources to help keep you and your loved ones healthy this flu season, visit our dedicated hub.
Colds are very common respiratory illnesses that are usually due to infections with rhinoviruses.
Colds are one of the most frequent reasons for people missing work or school, with the average adult in the U.S. having more than one each year. Most people will have had many colds from infancy all the way through to later life.
Viruses that cause the cold typically enter the body through the nose and sinuses. In response, the nose creates clear mucus to wash the virus away.
The symptoms of colds appear gradually and peak within 2–3 days. The most common symptoms include:
- a stuffy or runny nose
- sneezing
- sore throat
- coughing
- mucus dripping down the throat
- watery eyes
There is no cure, but colds will get better on their own. People can manage the symptoms by resting as much as possible, drinking plenty of fluids, and using over-the-counter (OTC) cold medicines if necessary.
Complications are rare, and there is normally no need to visit a doctor. However, people with a weakened immune system and those with asthma or another condition that affects the airways could become seriously ill from a cold.
Read more about treating the common cold here.
The flu is a common respiratory illness resulting from an infection with an influenza virus.
The flu is less common than colds, but when it does arise, it is more severe and can have serious complications.
One of the key symptoms of flu is feeling feverish or having a temperature of 100°F or above. However, not everyone with the flu will have a fever.
Common symptoms of the flu include:
- fever or feeling feverish
- chills
- a cough
- sore throat
- muscle or body aches
- runny or stuffy nose, though this is more common with a cold
- headaches
- fatigue
- vomiting or diarrhea, especially in children
It is possible to prevent the flu to a certain extent. The seasonal flu shot protects to a significant degree against complications due to influenza A and influenza B, which are the types that usually cause seasonal epidemics.
The seasonal flu shot protects to a significant degree against complications due to influenza A and influenza B, which are the types that usually cause seasonal epidemics.
Antibiotics do not work against either colds or the flu. Most people who have a cold or the flu will recover within 2 weeks without medical treatment. During this time, they can relieve their symptoms using home remedies.
If a person is at risk for severe flu complications, the CDC recommend prompt treatment with antiviral medications. These drugs can reduce symptoms, shorten the illness by 1–2 days, and prevent serious complications.
Home remedies
OTC drugs can relieve uncomfortable symptoms, including pains, aches, and fever, helping the person feel more comfortable while they recover. Drinking plenty of fluids and getting lots of rest can also speed up recovery.
The following home remedies can also help:
- saline nose drops can help clear a blocked nose
- vapor rubs can make it easier to breathe
- a vapor bath with eucalyptus can ease congestion
- gargling with salt water or sucking on a lozenge can ease the pain of a sore throat
- acetaminophen (Tylenol) and similar medications can relieve aches and pains
Learn more about how to treat colds and the flu at home.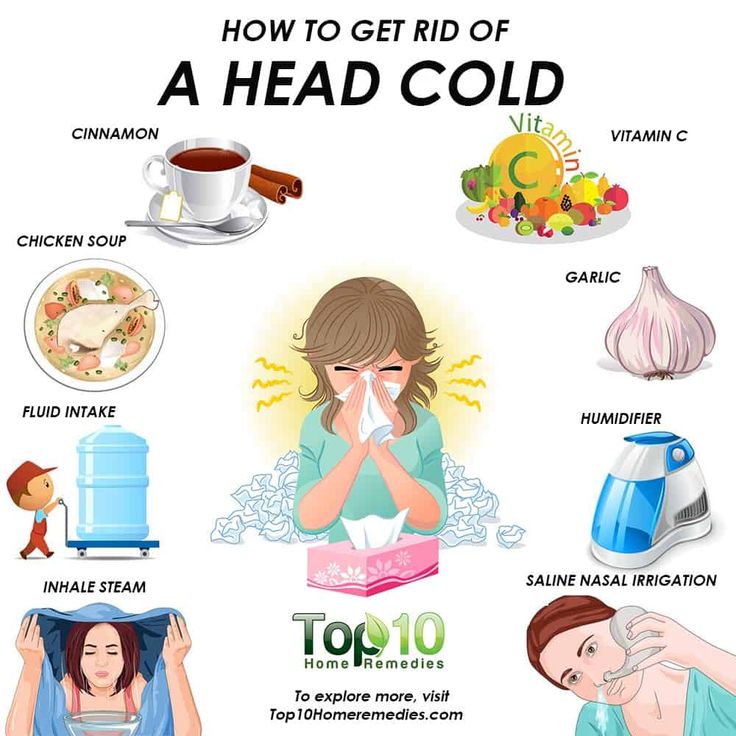
People should seek medical help if they notice any emergency warning signs.
Warning signs in children include:
- fast breathing or difficulty breathing
- bluish lips or face
- chest pain
- dehydration
- dull reactions
- fever above 104°F
Warning signs in adults include:
- shortness of breath or difficulty breathing
- bluish skin color
- persistent chest or abdomen pain or pressure
- dizziness or confusion
- seizures
- a lack of urination
- severe muscle pain or weakness
- fever or cough that improves then worsens
The CDC provide a full list of warning signs.
The best way to protect against the flu is by having an annual vaccination, as this helps the body build immunity against influenza viruses so that it can fight them off more easily.
The CDC recommend that everyone over the age of 6 months get a flu shot every year, with rare exceptions.
The flu shot has a good safety and effectiveness record. Learn more here.
Learn more here.
People can take steps to avoid catching viruses that cause respiratory illnesses and to reduce the risk of them spreading. These steps include:
- avoiding close contact with others when either person is sick
- covering the mouth and nose when sneezing or coughing
- washing the hands regularly and using an alcohol-based hand rub when this is not possible
- avoiding touching the eyes, nose, or mouth
- disinfecting surfaces regularly, especially when someone is ill
- getting plenty of sleep, staying active, and reducing stress, if possible
- drinking plenty of fluids and eating nutritious foods
Due to the COVID-19 pandemic, reducing the spread of respiratory illnesses, including the flu, during flu season is more important than ever.
Read more about how to avoid catching the flu here.
Shop for flu remediesPeople can find a wide range of cold and flu remedies in drugstores, supermarkets, and online.

- saline nose drops
- vapor rubs
- throat lozenges
- Tylenol
The common cold and the flu are seasonal respiratory illnesses that occur as a result of different viruses. The main difference is that the flu can have more severe symptoms and is more likely to cause serious complications and hospitalization.
In most cases, the symptoms of both a cold and the flu are relatively mild, and people can usually manage them at home. However, it is important to look out for warning signs, especially in people with a higher risk for complications.
Pregnancy rhinitis - why does it occur and how to treat it?
Rhinitis of pregnant women is not dangerous, but worsens the quality of life of a woman during pregnancy.Article rating
3. 20 (Votes: 45)
20 (Votes: 45)
Contents
- How long does pregnancy rhinitis occur and how long does it last? nine0004
- Symptoms of pregnancy rhinitis
- Causes of pregnancy rhinitis
- How to distinguish the symptoms of rhinitis during pregnancy from other pathologies?
- Treatment of rhinitis of pregnant women
- General recommendations for pregnant women who have symptoms of rhinitis
- Drugs for the treatment of rhinitis
Rhinitis of pregnancy (nasal obstruction) is a common pathology that occurs in about 30% of expectant mothers. Manifested by a typical triad of symptoms: nasal congestion, difficulty breathing, the presence of mucous secretions. By itself, it is not dangerous, but worsens the quality of life of a woman during pregnancy. The difficulty of stopping the pathology and relieving symptoms lies in the fact that during pregnancy there are restrictions on the use of a number of physiotherapeutic methods and drugs.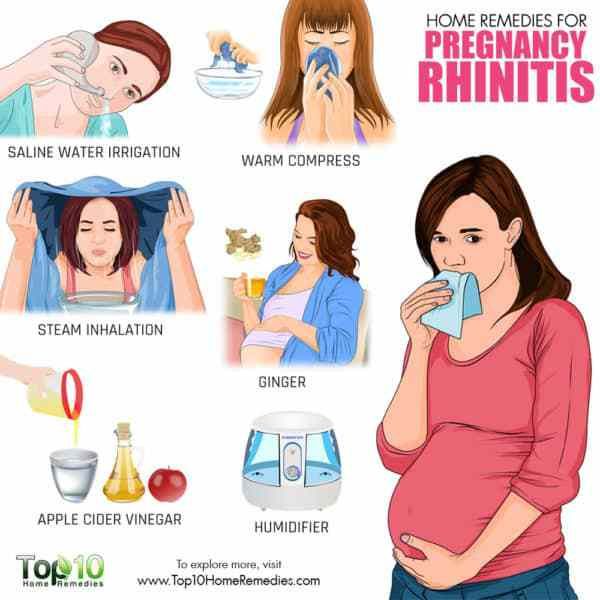 nine0007
nine0007
When does pregnancy rhinitis occur and how long does it last?
Most often, pathology occurs:
- up to and including the 20th week of pregnancy - in this case, rhinitis usually resolves on its own (after about a month or two) and does not manifest itself in the later stages;
- after the 20th week of pregnancy - this condition can continue until childbirth and after them (after 2-3 weeks).
If the symptoms last longer than two months and are not relieved by any independent action (vasoconstrictor sprays are prohibited!), then the cause may be hiding in a chronic disease. nine0007
Symptoms of pregnancy rhinitis
- Difficult nasal breathing, nasal congestion;
- Nasal discomfort, sneezing;
- Presence of clear mucous discharge;
- Feeling of constriction in the region of the nose and sinuses;
- Mild headaches.
Difficulty in nasal breathing in the mother leads to sleep disturbance and hypoxia, which is also felt by the fetus.
Causes of pregnancy rhinitis nine0034
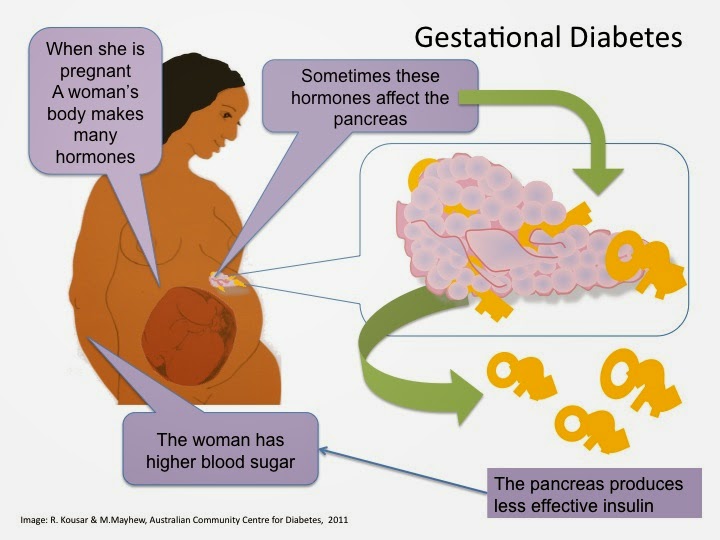
The pathogenesis of the disease is still a controversial issue. Most doctors are inclined to believe that it is of a hormonal nature and is associated with an increased level of estrogen and acetylcholine in the blood serum (as a result), which leads to hyperemia of the nasal mucosa and swelling. The concentration of estradiol, estrone, estriol in the bloodstream of pregnant women increases, in some future mothers, for this reason, the shape of the nose may change, it may increase in size.
There is evidence that pregnant women with symptoms of vasomotor rhinitis have elevated serum placental hormone levels. Another reason that can cause long-term nasal obstruction is the tone of smooth muscle cells under the influence of the inhibitory action of the steroid hormone progesterone. It causes fluid retention in the body and has such a side effect on the nasal mucosa. nine0007
Histochemical studies have shown that nasal congestion may occur due to plethora due to hyperactivity of the parasympathetic nervous system in pregnant women.
How to distinguish the symptoms of pregnancy rhinitis from other pathologies?
Symptoms of rhinitis during pregnancy are really similar to manifestations of other diseases, for example, viral infections, sinusitis. It is difficult for a future mother to distinguish a pathology by external signs, therefore a doctor's consultation is necessary. Our clinic employs specialists with extensive experience who will quickly diagnose and prescribe treatment. nine0007
If the symptoms are accompanied by a sore throat, fever, then this indicates the presence of a bacterial and/or viral infection or other inflammatory process.
With sinusitis, mucous discharge may have a yellowish or greenish tinge. When pressing in the area of the maxillary and frontal sinuses, there are painful sensations, when the head is tilted, the pain may intensify. Also, sinusitis often causes an increase in temperature, while with nasal obstruction, such symptoms are not observed. nine0007
Sometimes rhinitis of pregnancy is confused with allergic rhinitis, which may worsen, there may be sensitization to allergens to which patients have not previously reported sensitivity.
Treatment of pregnancy rhinitis
In our clinic, a thorough diagnosis is carried out in order to exclude diseases similar to rhinitis in terms of symptoms. After the examination, individual treatment is prescribed depending on the severity, severity and indications.
Treatment is complicated by the fact that many drugs can cause contraction of the myometrium and fetal circulation or vasoconstriction with impaired placental function. Therefore, a doctor should prescribe drug therapy, you can not use drugs on your own - they can cause a violation of the development of the fetus. nine0007
General advice for pregnant women with symptoms of rhinitis
- Washing the nose with mild saline solution (2 teaspoons of sea salt per glass of water). Salt solution improves the discharge of nasal mucus and reduces the feeling of congestion.
- Nasal douches (nose washers) are very helpful. You can use regular saline for them.
- Ventilate the room before going to bed, use humidifiers.
 Dry air can exacerbate unpleasant symptoms. nine0004
Dry air can exacerbate unpleasant symptoms. nine0004 - Use a high pillow (or multiple pillows) to sleep with your head well above your torso.
- Walking in the fresh air before going to bed is useful.
- Do morning exercises and breathing exercises several times a day to reduce the symptoms of hypoxia.
- Do not wear perfume and stay away from smokers.
Do not use vasoconstrictor nasal drops during pregnancy as they may cause vasomotor rhinitis. nine0007
Preparations for the treatment of rhinitis
Preparations for use during pregnancy are selected with great care and individually. Pregnant women are not given oral systemic corticosteroids, although their effect on the fetus is not fully understood. In some cases, the doctor prescribes corticosteroids in the form of aerosols. Oral antihistamines are also not prescribed due to the increased risk of embryopathies. The choice of physiotherapy is also limited, because most methods negatively affect the development of the fetus. nine0007
nine0007
If you suffer from rhinitis, headaches or other unpleasant symptoms, we advise you to see a doctor immediately. Timely treatment is the key to the quality of life of the mother, which is very important for bearing the fetus. And also allows you not to miss other more serious diseases that can adversely affect the health of the mother and child.
Important! Do not use drugs that were prescribed to you by a doctor before pregnancy, or drugs prescribed to someone else. nine0007
Rhinitis during pregnancy usually does not pose a threat to either the fetus or the mother, but improper treatment can lead to unpredictable consequences.
Seeing a doctor early can help keep you healthy.
Don't delay treatment, call now. We work around the clock in Moscow.
tel.: 8 (499) 501-15-53 (24 hours)
Rhinitis in pregnancy
Otorhinolaryngologist, surgeon at GMS Clinic Oleg Abramov talks in his article about rhinitis of pregnancy (hereinafter referred to as RH). nine0007
nine0007
It was no coincidence that I chose this topic after a series of publications on the social network about allergic rhinitis (hereinafter referred to as AR), as recent studies note that although the cause of RB is not completely clear, the combination of AR, which is especially poorly controlled together with RB, can lead to severe nasal congestion, to insufficient oxygen supply, and, as a result, to increased fatigue, irritability, frequent SARS, sleep disturbance, which can certainly affect the development of the fetus. Moreover, the presence of AR is associated with snoring in women during pregnancy, and together they can provoke the development of sleep apnea syndrome (stopping breathing during sleep), which leads to arterial hypertension, preeclampsia, slowed fetal growth and low Apgar scores. Therefore, the relevance of this problem is only growing. nine0007
Definition and concept
Rhinitis of pregnancy is a disease accompanied by nasal congestion and discharge, periodic sneezing without signs of inflammation, allergies, or other causes. This condition can occur in any trimester of pregnancy and usually resolves within two weeks after delivery.
This condition can occur in any trimester of pregnancy and usually resolves within two weeks after delivery.
Occurrence
Nasal congestion is a very common problem during pregnancy (occurs in about 65% of cases), which can occur due to various reasons. RB, according to various sources, occurs in 9-40% of cases, and in one of the last observations there is an increasing incidence, that is, most of all RB is observed in the 3rd trimester - 38.9%, including those who did not have problems in the 1st and 2nd trimesters.
Causes and mechanism of occurrence
The mechanism of occurrence is not fully understood, and it is believed that RB occurs due to hormonal changes, in particular, under the influence of progesterone, estrogen, hCG and other hormones, the concentration of which gradually increases during pregnancy. Some authors believe that the occurrence of RB is associated with the worsening of concomitant AR. Some studies show that hormonal action leads to relaxation of the smooth muscles that make up the vessel wall of the nasal mucosa, resulting in nasal congestion. Such findings are supported by other studies that show that oral contraceptives cause similar effects in the nasal cavity (but not in everyone). Other studies show that elevated body mass index, overweight, multiple pregnancies provoke or aggravate RB. nine0007
Such findings are supported by other studies that show that oral contraceptives cause similar effects in the nasal cavity (but not in everyone). Other studies show that elevated body mass index, overweight, multiple pregnancies provoke or aggravate RB. nine0007
Progression and potential risks
RB, in the absence of adequate treatment, has an adverse effect on the course of pregnancy and can lead to the development of rhinosinusitis, which is especially difficult to tolerate in the 3rd trimester. On the other hand, pregnancy is a special period in a woman's life, during which a large number of drugs are prohibited, and ENT pathologies, these restrictions have not been spared either. Very often I hear at the reception: "Doctor, I'm pregnant and I've been suffering with my nose all this time, but the doctors tell me - there's nothing to be done, I need to endure it." On the other hand, the opposite situation is often observed: “Doctor, I am pregnant and I cannot live without vasoconstrictor drops. ” These situations, of course, are not correct, since on the one hand there is a way out and optimal treatment, and on the other hand, constant exposure to vasoconstrictor drugs is not a way out of the situation at all. nine0007
” These situations, of course, are not correct, since on the one hand there is a way out and optimal treatment, and on the other hand, constant exposure to vasoconstrictor drugs is not a way out of the situation at all. nine0007
Diagnostics
At the moment, there is no specific test to confirm or exclude RB. The diagnosis is made on the basis of the patient's complaints and the exclusion of other pathologies of the nasal cavity.
Choice of therapeutic tactics
Saline solutions
Before considering more serious medications, we should start with our favorite saline solutions. It should be noted that we are not talking about ordinary saline solutions, but hypertonic saline solutions (with an increased salt content, approximately 19-23 g/l). Such sprays are sold in all pharmacies, but they will not be sold to you right away (you need to ask). Several studies have noted significant efficacy in reducing congestion when used in AR, chronic rhinosinusitis. Also, comparative studies show their greater effectiveness compared to conventional isotonic solutions. Examples: Physiomer - hypertonic solution (my favorite), Aqualor-congestion, or Aqualor-severe runny nose, Aquamaris Strong.
Also, comparative studies show their greater effectiveness compared to conventional isotonic solutions. Examples: Physiomer - hypertonic solution (my favorite), Aqualor-congestion, or Aqualor-severe runny nose, Aquamaris Strong.
As is known from past publications, intranasal glucocorticosteroids (iGCS) are the most effective in the treatment of AR today. They have proven efficacy in reducing nasal congestion, as well as nasal itching and watery eyes, and allow adequate control of symptoms. But, given their hormonal effect and possible harmful effects on the fetus, there are certain risks in their use. It should also be noted that at the moment there are no studies that provide reliable data confirming the danger of their use. Modern ICS — mometasone (nasonex, desrinit) and fluticasone (avamys, flixonase) has a very low systemic bioavailability, less than 1% and proven efficacy, thus can be considered as initial therapy for RB. The studies did not reveal a statistically significant relationship between the development of fetal defects and the use of these drugs.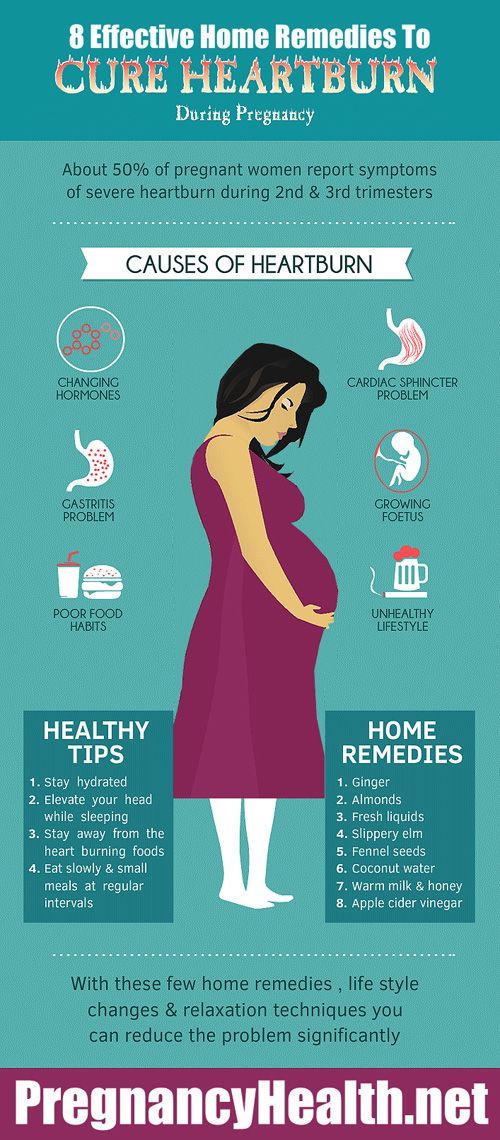 nine0007
nine0007
Who are the FDA in the US and why is everyone listening to them?
Everything is very simple (it’s a pity that everything is not so simple with us). I copy the explanation from Wikipedia: “An agency of the US Department of Health and Human Services, one of the federal executive departments. The department is engaged in quality control of food products, medicines, cosmetics, tobacco products and some other categories of goods, and also monitors compliance with legislation and standards in this area. nine0007
Budesonide (Tafen Nasal) is classified as category B according to the FDA's classification for drug effects on the fetus, which means that there is evidence that the drug is safe to use during pregnancy. The bioavailability of budesonide is 33%. This drug has moved from group C to group B, thanks to several high-quality studies in Sweden since the beginning of the 21st century, proving its safety.
Also, according to the current recommendations of the American Academy of Allergology and Immunology (AAAAI), ICS are considered safe and effective in the treatment of rhinitis and rhinosinusitis during pregnancy. But at the same time, there is no indication of specific drugs. Other competent medical associations also do not give any recommendations in terms of choosing a drug. Therefore, summing up all of the above, and also according to the latest review, mometasone, fluticasone, budesonide can be considered as safe and effective agents in the treatment of RB. It should also be noted that an experienced ENT doctor should be involved in prescribing the drug and managing the patient, since these drugs are sold without a prescription in the Russian Federation; we strongly recommend not to self-medicate. nine0007
But at the same time, there is no indication of specific drugs. Other competent medical associations also do not give any recommendations in terms of choosing a drug. Therefore, summing up all of the above, and also according to the latest review, mometasone, fluticasone, budesonide can be considered as safe and effective agents in the treatment of RB. It should also be noted that an experienced ENT doctor should be involved in prescribing the drug and managing the patient, since these drugs are sold without a prescription in the Russian Federation; we strongly recommend not to self-medicate. nine0007
Yes, I will not take these hormones!
In some situations, acute respiratory viral infections during pregnancy may be accompanied (largely due to concomitant RB or AR, or their combination) with a prolonged runny nose, nasal congestion and heaviness in the face - classic symptoms of rhinosinusitis. This disease, if not adequately treated, can lead to serious complications, so the correct diagnosis of this disease is extremely important.