Symptoms of retained tissue after miscarriage
Hysteroscopy and Retained Products of Conception: An Update
1. Capmas P, Lobersztajn A, Duminil L, Barral T, Pourcelot AG, Fernandez H. Operative hysteroscopy for retained products of conception: Efficacy and subsequent fertility. J Gynecol Obstet Hum Reprod. 2019;48:151–4. [PubMed] [Google Scholar]
2. Smorgick N, Barel O, Fuchs N, Ben-Ami I, Pansky M, Vaknin Z. Hysteroscopic management of retained products of conception: Meta-analysis and literature review. Eur J Obstet Gynecol Reprod Biol. 2014;173:19–22. [PubMed] [Google Scholar]
3. Hooker AB, Aydin H, Brölmann HA, Huirne JA. Long-term complications and reproductive outcome after the management of retained products of conception: A systematic review. Fertil Steril. 2016;105:156–64. e1-2. [PubMed] [Google Scholar]
4. Kamaya A, Petrovitch I, Chen B, Frederick CE, Jeffrey RB. Retained products of conception: Spectrum of color Doppler findings. J Ultrasound Med. 2009;28:1031–41. [PubMed] [Google Scholar]
5. Tinelli AP, Haimovich S. Hysteroscopy. New York, NY: Springer Berlin Heidelberg; 2017. [Google Scholar]
6. Alonso Pacheco L, Timmons D, Saad Naguib M, Carugno J. Hysteroscopic management of retained products of conception: A single center observational study. Facts Views Vis Obgyn. 2019;11:217–22. [PMC free article] [PubMed] [Google Scholar]
7. Scribner D, Fraser R. Diagnosis of acquired uterine arteriovenous malformation by Doppler ultrasound. J Emerg Med. 2016;51:168–71. [PubMed] [Google Scholar]
8. Sellmyer MA, Desser TS, Maturen KE, Jeffrey RB, Jr, Kamaya A. Physiologic, histologic, and imaging features of retained products of conception. Radiographics. 2013;33:781–96. [PubMed] [Google Scholar]
9. De Winter J, De Raedemaecker H, Muys J, Jacquemyn Y. The value of postpartum ultrasound for the diagnosis of retained products of conception: A systematic review. Facts Views Vis Obgyn. 2017;9:207–16. [PMC free article] [PubMed] [Google Scholar]
10. Munros J, Gracia M, Nonell R, Cardona M, Lavilla P, Garcia A, et al. Delayed hysteroscopic removal of retained products of conception is associated with spontaneous expulsion. SRL Reprod Med Gynecol. 2017;3:24–8. [Google Scholar]
Delayed hysteroscopic removal of retained products of conception is associated with spontaneous expulsion. SRL Reprod Med Gynecol. 2017;3:24–8. [Google Scholar]
11. Hooker AB, Thurkow A. Asherman's syndrome after removal of placenta remnants: A serious clinical problem. Gynecol Surg. 2011;8:449–53. [Google Scholar]
12. Nanda K, Lopez LM, Grimes DA, Peloggia A, Nanda G. Expectant care versus surgical treatment for miscarriage. Cochrane Database Syst Rev. 2012;2012:CD003518. [PMC free article] [PubMed] [Google Scholar]
13. Klement AH, Frederic M, Bentov Y, Chang P, Nayot D, Haas J, et al. Oral contraceptive pills as an option for non- surgical management of retained products of conception – A preliminary study. Gynecol Endocrinol Gynecol Endocrinol. 2018;34:609–11. [PubMed] [Google Scholar]
14. Stewart KT, Lee JS, Pan K, Albert AY, Fisher S. Outcome of using vaginal misoprostol for treatment of retained products of conception after first trimester miscarriage: A retrospective cohort study. Euro J Contracept Reproduct Health Care. 2020;25:474–9. [PubMed] [Google Scholar]
Euro J Contracept Reproduct Health Care. 2020;25:474–9. [PubMed] [Google Scholar]
15. Akazawa M, Yokoyama M, Minami C, Takeuchi T, Kawamoto Y. Hysteroscopic resection of retained products of conception after temporal laparoscopic uterine artery ligation. Gynecol Mini Invasive Ther. 2016;5:81–3. [Google Scholar]
16. Pather S, Ford M, Reid R, Sykes P. Postpartum curettage: An audit of 200 cases. Aust N Z J Obstet Gynaecol. 2005;45:368–71. [PubMed] [Google Scholar]
17. Friedler S, Margalioth EJ, Kafka I, Yaffe H. Incidence of post-abortion intrauterine adhesions evaluated by hysteroscopy – A prospective study. Hum Reprod. 1993;8:442–4. [PubMed] [Google Scholar]
18. Rein DT, Schmidt T, Hess AP, Volkmer A, Schöndorf T, Breidenbac M. Hysteroscopic management of residual trophoblastic tissue is superior to ultrasound-guided curettage. J Minim Invasive Gynecol. 2011;18:774–8. [PubMed] [Google Scholar]
19. Cohen SB, Kalter-Ferber A, Weisz BS, Zalel Y, Seidman DS, Mashiach S, et al. Hysteroscopy may be the method of choice for management of residual trophoblastic tissue. J Am Assoc Gynecol Laparosc. 2001;8:199–202. [PubMed] [Google Scholar]
Hysteroscopy may be the method of choice for management of residual trophoblastic tissue. J Am Assoc Gynecol Laparosc. 2001;8:199–202. [PubMed] [Google Scholar]
20. Jimenez JS, Gonzalez C, Alvarez C, Munoz L, Perez C, Munoz JL, et al. Conservative management of retained trophoblastic tissue and placental polyp with diagnostic ambulatory hysteroscopy. Euro J Obstet Gynecol Reproduct Biol. 2009;145:89–92. [PubMed] [Google Scholar]
21. Perez-Medina T, Sancho-Sauco J, Rıos M, Pereira A, Argila N, Cabezas E, et al. Hysteroscopy in pregnancy-related conditions: Descriptive analysis in 273 patients. J Minim Invasive Gynecol. 2014;21:417–25. [PubMed] [Google Scholar]
22. Maček KJ, Blaganje M, Šuster NK, Starič KD, Kobal B. Office hysteroscopy in removing retained products of conception – A highly successful approach with minimal complications. J Obstet Gynaecol. 2020;40:1122–6. [PubMed] [Google Scholar]
23. Nappi C, Di Spiezio Sardo A. State-of-the-art: hysteroscopic approaches to pathologies of the genital tract. Endo: Press Tuttlingen; 2014. [Google Scholar]
Endo: Press Tuttlingen; 2014. [Google Scholar]
24. Goldenberg M, Schiff E, Achiron R, Lipitz S, Mashiach S. Managing residual trophoblastic tissue.Hysteroscopy for directing curettage. J Reprod Med. 1997;42:26–8. [PubMed] [Google Scholar]
25. Faivre E, Deffieux X, Mrazguia C, Gervaise A, Chauveaud-Lambling A, Frydman R, et al. Hysteroscopic management of residual trophoblastic tissue and reproductive outcome: A pilot study. J Minim Invasive Gynecol. 2009;16:487–90. [PubMed] [Google Scholar]
26. Golan A, Dishi M, Shalev A, Keidar R, Ginath S, Sagiv R. Operative hysteroscopy to remove retained products of conception: Novel treatment of an old problem. J Minim Invasive Gynecol. 2011;18:100–3. [PubMed] [Google Scholar]
27. Hamerlynck TW, Blikkendaal MD, Schoot BC, Hanstede MM, Jansen FW. An alternative approach for removal of placental remnants: Hysteroscopic morcellation. J Minim Invasive Gynecol. 2013;20:796–802. [PubMed] [Google Scholar]
28. Mallick R, Middleton B. The use of hysteroscopic morcellation in the outpatient management of retained products of conception. Res Rep Gynecol Obstet. 2017;1:12–5. [Google Scholar]
The use of hysteroscopic morcellation in the outpatient management of retained products of conception. Res Rep Gynecol Obstet. 2017;1:12–5. [Google Scholar]
29. Sutherland NSV, Rajesh H. The Intrauterine Bigatti Shaver System: An alternative option for focal retained products of conception. Case Rep Obstet Gynecol. 2018;2018:1536801. [PMC free article] [PubMed] [Google Scholar]
30. Ansari SH, Bigatti G, Aghssa MM. Operative hysteroscopy with the Bigatti shaver (IBS®) for the removal of placental remnants. Facts Views Vis Obgyn. 2018;10:153–9. [PMC free article] [PubMed] [Google Scholar]
31. Capote S, Cubo-Abert M, Casellas-Caro M, Sánchez-Iglesias JL, Gomez-Cabeza JJ, Gil-Moreno A. Role of office hysteroscopic morcellation and 3-dimensional transvaginal ultrasound in conservative management of retained placenta accreta. Eur J Obstet Gynecol Reprod Biol. 2018;230:199–200. [PubMed] [Google Scholar]
32. Emanuel MH, Wamsteker K. The Intra Uterine Morcellator: A new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62–6. [PubMed] [Google Scholar]
J Minim Invasive Gynecol. 2005;12:62–6. [PubMed] [Google Scholar]
33. Marques K, Looney C, Hayslip C, Gavrilova-Jordan L. Modern management of hypervascular placental polypoid mass following spontaneous abortion: A case report and literature review. Am J Obstet Gynecol. 2011;205:e9–11. [PubMed] [Google Scholar]
34. Takeda A, Koyama K, Imoto S, Mori M, Sakai K, Nakamura H. Placental polyp with prominent neovascularization. Fertil Steril. 2010;93:1324–6. [PubMed] [Google Scholar]
35. Bettocchi S, Di Spiezio Sardo A, Ceci O, Nappi L, Guida M, Greco E, et al. A new hysteroscopic technique for the preparation of partially intramural myomas in office setting (OPPIuM technique): A pilot study. J Minim Invasive Gynecol. 2009;16:748–54. [PubMed] [Google Scholar]
36. Capmas P, Levaillant JM, Fernandez H. Surgical techniques and outcome in the management of submucous fibroids. Curr Opin Obstet Gynecol. 2013;25:332–8. [PubMed] [Google Scholar]
37. Smorgick N, Rabinovitch I, Levinsohn-Tavor O, Maymon R, Vaknin Z, Pansky M. Two-step hysteroscopy for management of morbidly adherent retained products of conception. Arch Gynecol Obstet. 2019;300:669–74. [PubMed] [Google Scholar]
Two-step hysteroscopy for management of morbidly adherent retained products of conception. Arch Gynecol Obstet. 2019;300:669–74. [PubMed] [Google Scholar]
38. Legendre G, Zoulovits FJ, Kinn J, Senthiles L, Fernandez H. Conservative management of placenta accreta: Hysteroscopic resection of retained tissues. J Minim Invasive Gynecol. 2014;21:910–13. [PubMed] [Google Scholar]
39. Bagratee JS, Khullar V, Regan L, Moodley J, Kagoro H. A randomized controlled trial comparing medical and expectant management of first trimester miscarriage. Hum Reprod. 2004;19:266–71. [PubMed] [Google Scholar]
40. Lin YH, Cheng YY, Ding DC. Hysteroscopic management of retained products of conception. Gynecol Minim Invasive Ther. 2018;7:133–5. [PMC free article] [PubMed] [Google Scholar]
41. Goldenberg M, Schiff E, Achiron R, Lipitz S, Mashiach S. Managing residual trophoblastic tissue.Hysteroscopy for directing curettage. J Reprod Med. 1997;42:26–8. [PubMed] [Google Scholar]
42. Hamerlynck TW, van Vliet HA, Beerens AS, Weyers S, Schoot BC. Hysteroscopic morcellation versus loop resection for removal of placental remnants: A randomized trial. J Minim Invasive Gynecol. 2016;23:1172–80. [PubMed] [Google Scholar]
Hysteroscopic morcellation versus loop resection for removal of placental remnants: A randomized trial. J Minim Invasive Gynecol. 2016;23:1172–80. [PubMed] [Google Scholar]
43. Hrazdirová L, Kuzel D, Zizka Z. Is the hysteroscopy the right choice for therapy of placental remnants? Ceska Gynekol. 2012;77:35–8. [PubMed] [Google Scholar]
44. Fox H. Placenta accreta, 1945–1969. Obstet Gynecol. 1972;27:475–49. [Google Scholar]
45. Di Spiezio Sardo A, Calagna G, Scognamiglio M, O'Donovan P, Campo R, De Wilde RL. Prevention of intrauterine post-surgical adhesions in hysteroscopy.A systematic review. Euro J Obstet Gynecol Reproduct Biol. 2016;203:182–92. [PubMed] [Google Scholar]
46. van Wessel S, Coryn N, van Vliet H, Schoot B, Weyers S, Hamerlynck T. Reproductive and obstetric outcomes after hysteroscopic removal of retained products of conception. J Minim Invasive Gynecol. 2020;27:840–6. [PubMed] [Google Scholar]
Conservative and timely treatment in retained products of conception: a case report of placenta accreta ritention
Int J Clin Exp Pathol.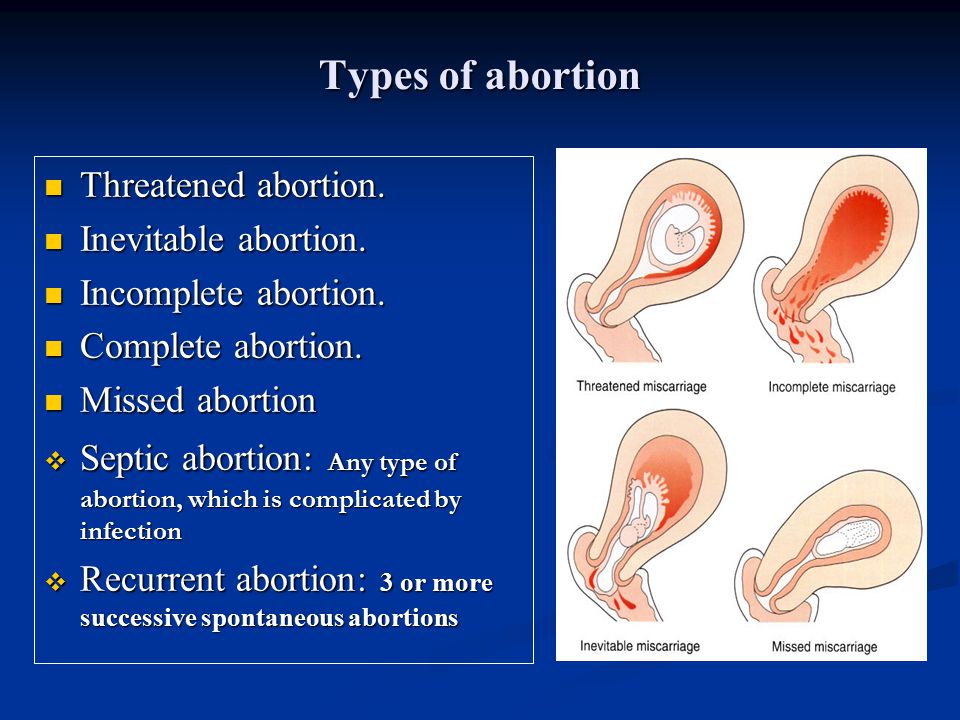 2015; 8(10): 13625–13629.
2015; 8(10): 13625–13629.
Published online 2015 Oct 1.
Author information Article notes Copyright and License information Disclaimer
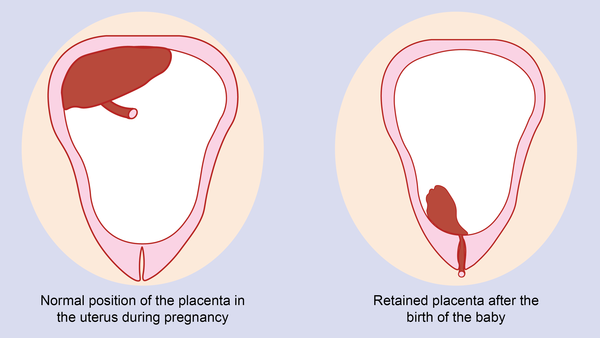
The term retained products of conception (RPOC) refers to intrauterine tissue that develops after conception and persists after medical and surgical pregnancy termination, miscarriage, and vaginal or cesarean delivery. One of the most important factor risk for RPOC is placenta accreta, defined as “the abnormal adherence, either in whole or in part, of the afterbirth to the underlying uterine wall”. We report a case of a 37 years old woman referred to our gynecologic department with irregular vaginal bleeding. On her medical history, she had a cesarean occurred 3 months before. Ultrasonography revealed in the uterine cavity hyperechoic mass, treated with curettage. Two weeks later the curettage, patient complained still vaginal bleeding. On the transvaginal ultrasound, the uterine cavity was occupied again by a hyperechoic mass. She underwent to hysteroscopic resection and histological diagnosis was compatible with placenta accreta residual.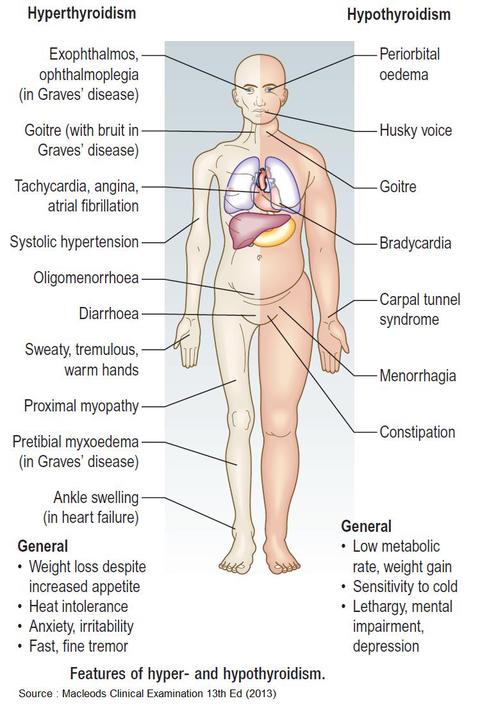 In the follow up she had not complications. Early diagnosis, prompt evaluation of bleeding is important for timely treatment and for preventing immediate complications and demolitive approach. A careful follow up is necessary to prevent late consequences. The purpose of this study is to report our experience in timely diagnosis and conservative management.
In the follow up she had not complications. Early diagnosis, prompt evaluation of bleeding is important for timely treatment and for preventing immediate complications and demolitive approach. A careful follow up is necessary to prevent late consequences. The purpose of this study is to report our experience in timely diagnosis and conservative management.
Keywords: Retained products of conception, placenta accreta, postpartum bleeding
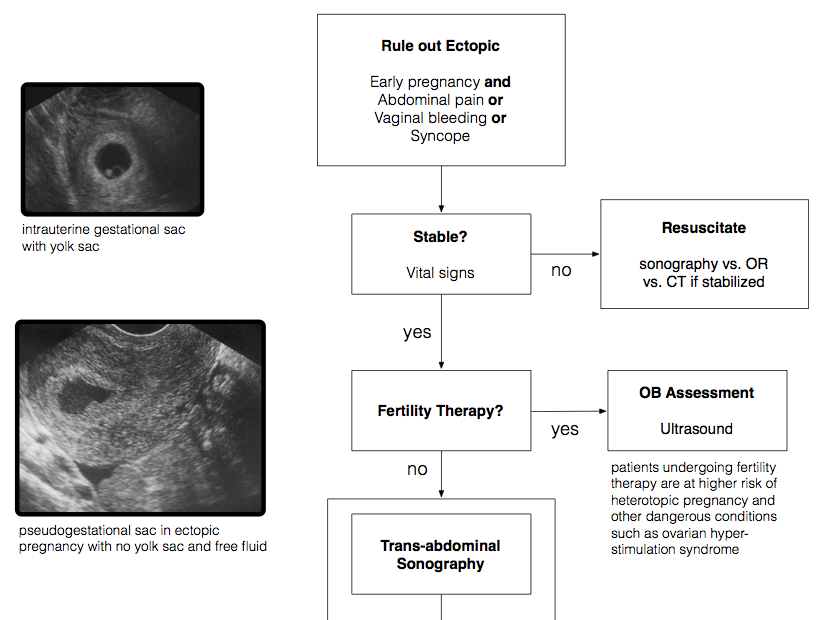
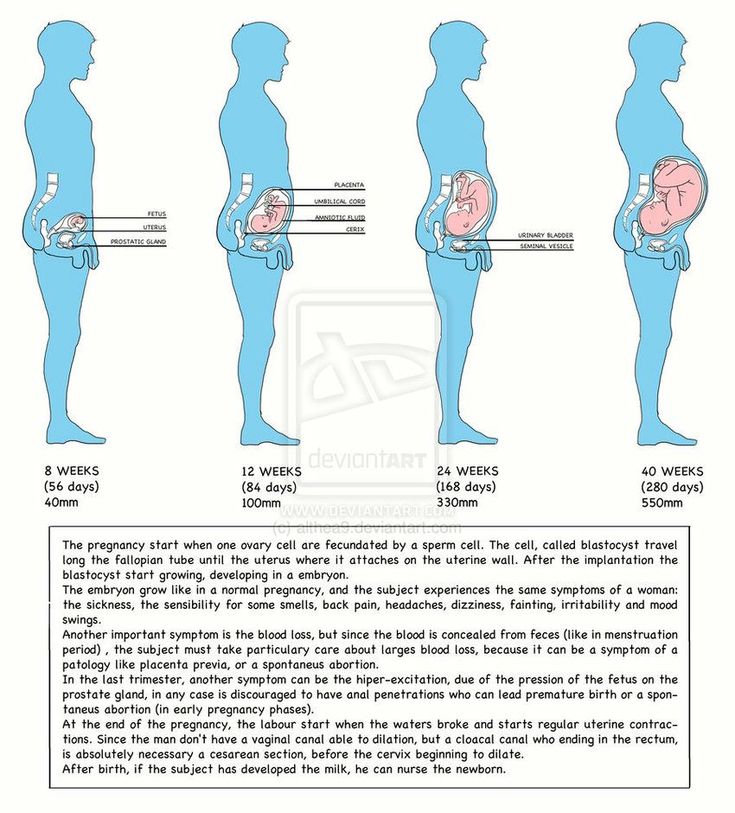
The term retained products of conception (RPOC) refers to intrauterine tissue that develops after conception and persists after medical and surgical pregnancy termination, miscarriage, and vaginal or cesarean delivery. This intrauterine tissue is often of placental origin [1]. RPOC is one of the most common causes of postpartum bleeding, but the clinical presentation can be also characterized by pain or fever. The incidence of RPOC seems to related on the gestational age of the pregnancy, most frequently after second-trimester delivery or termination of pregnancy. RPOC are estimated approximately 1% of term pregnancies [2]. The main risk factors are failure to progress during delivery, placenta accreta, and instrument delivery. The diagnosis presents a major clinical challenge. The association between clinical features and ultrasonographic characteristic is essential for diagnosis; however color Doppler US increases the positive predictive value for the diagnosis of RPOC. Serum beta human chorionic gonadotropin (B-hCG) levels also may be checked, but they may not be helpful because they can be elevated in the postpartum period [2]. The histological diagnosis is based on the presence of chorionic villi, which indicates persistent placental or trophoblastic tissue, can invade uterine endometrium [1].
RPOC are estimated approximately 1% of term pregnancies [2]. The main risk factors are failure to progress during delivery, placenta accreta, and instrument delivery. The diagnosis presents a major clinical challenge. The association between clinical features and ultrasonographic characteristic is essential for diagnosis; however color Doppler US increases the positive predictive value for the diagnosis of RPOC. Serum beta human chorionic gonadotropin (B-hCG) levels also may be checked, but they may not be helpful because they can be elevated in the postpartum period [2]. The histological diagnosis is based on the presence of chorionic villi, which indicates persistent placental or trophoblastic tissue, can invade uterine endometrium [1].
We report a case of a 37 years old woman, G1P1, referred to our gynecologic department with irregular vaginal bleeding since her cesarean section occurred 3 months before. In the last few days she had also pelvic pain. On her medical history, she had a cesarean section and no postpartum complications. During her cesarean section, at macroscopic examination, placenta appeared to be accrete, with scleroialina degeneration, so the histological examination was done, with the result of term placenta, without cellular atypie.
During her cesarean section, at macroscopic examination, placenta appeared to be accrete, with scleroialina degeneration, so the histological examination was done, with the result of term placenta, without cellular atypie.
During our observation serum levels of beta-human chorionic gonadotrophin (β-hCG) were always negative. Ultrasonography revealed in the uterine cavity hyperechoic mass, measuring 22×31 mm in diameter (). Both annexes were normal. She underwent dilatation and curettage and so much material was removed (FIG). The histopathological description was of shadows tissue compatible with placental villi in degeneration scleroialina. There were also some trophoblastic cells still vital. Two weeks later the curettage, the patient complained still vaginal bleeding. On the transvaginal ultrasound, the uterine cavity was occupied again by a hyperechoic mass (32×30 mm) (). Sonohysterography demonstrated that it was strictly adherent to uterine walls and color Doppler US excluded a vascularization of the neoformation.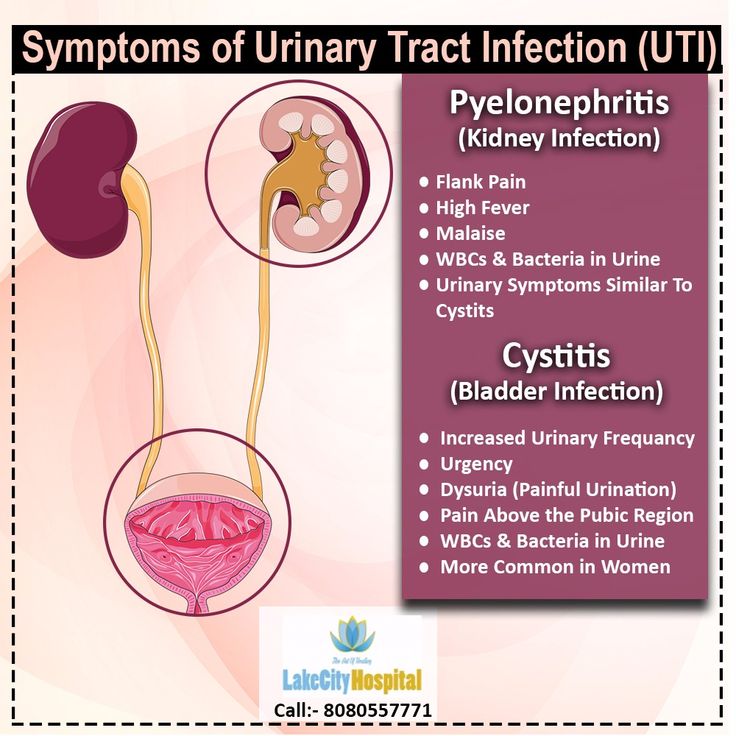 Serum level of β-hCG was still negative. We programmed a new access to our gynecology department, for hysteroscopic resection and at the end of the surgical procedure the cavity appeared to be empty. The removed material was sent to histological examination and the first histological report was confirmed. In the follow up she hasn’t got complications.
Serum level of β-hCG was still negative. We programmed a new access to our gynecology department, for hysteroscopic resection and at the end of the surgical procedure the cavity appeared to be empty. The removed material was sent to histological examination and the first histological report was confirmed. In the follow up she hasn’t got complications.
Open in a separate window
Hyperechoic mass (22×31 mm in diameter) in the uterine cavity, three months after cesarean delivery.
Open in a separate window
Two weeks later the curettage, the uterine cavity was occupied again by a hyperechoic mass (32×30 mm).
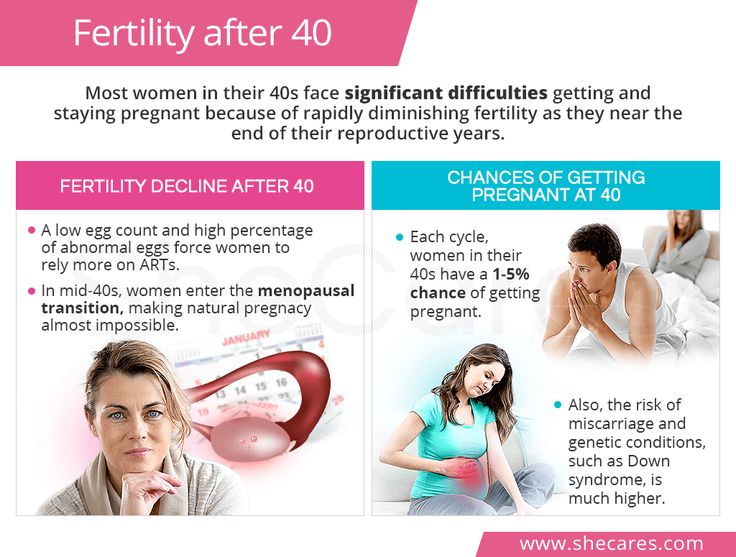
After medical and surgical pregnancy termination, vaginal or cesarean delivery there may be partial or complete retention of parts of the placenta or other decidual tissues within the uterus. This condition is defined RPOC. It is one of the most common causes of both primary and secondary post partum hemorrhage [1]. One of the most important factor risk for RPOC is placenta accreta, defined as “the abnormal adherence, either in whole or in part, of the afterbirth to the underlying uterine wall” [3]. Placenta accreta is a severe pregnancy complication. It is a major cause of obstetric hemorrhage, a situation that remains the most significant cause of maternal morbidity and mortality worldwide [4]. It is caused by a defect in decidua basalis resulting in an abnormally invasive placental implantation [5]. This condition is often related to previous uterine scars (cesarean sections and prior uterine curettage), and other risk factors associated with placenta accreta are multiparity, placenta previa, prior intrauterine infections, elevated maternal serum a-fetoprotein, and maternal age >35 years [6]. The incidence of placenta accreta approximates about 1 in 1000 deliveries and, has increased 10-fold in the last 50 years, primarily because of the rise in cesarean section rates [5]. Patients with RPOC usually presented abdominal pain, bleeding, fever: these clinical symptmos aren’t specific, but the early diagnosis is critical for directing clinical management of bleeding and for preventing associated consequences [1].
Placenta accreta is a severe pregnancy complication. It is a major cause of obstetric hemorrhage, a situation that remains the most significant cause of maternal morbidity and mortality worldwide [4]. It is caused by a defect in decidua basalis resulting in an abnormally invasive placental implantation [5]. This condition is often related to previous uterine scars (cesarean sections and prior uterine curettage), and other risk factors associated with placenta accreta are multiparity, placenta previa, prior intrauterine infections, elevated maternal serum a-fetoprotein, and maternal age >35 years [6]. The incidence of placenta accreta approximates about 1 in 1000 deliveries and, has increased 10-fold in the last 50 years, primarily because of the rise in cesarean section rates [5]. Patients with RPOC usually presented abdominal pain, bleeding, fever: these clinical symptmos aren’t specific, but the early diagnosis is critical for directing clinical management of bleeding and for preventing associated consequences [1]. Ultrasonography (US) is useful in the evaluation of RPOC and the diagnosis is supposed on the sonographic appearance of intrauterine echogenic material. Although transvaginal sonographic enhances evaluation for RPOC, the diagnosis is sometimes difficult because necrotic decidua and blood clots may be very difficult to differentiate from RPOC [7]. For this reason combined gray scale and color Doppler US can improve the valuation of suspected RPOC, allows realtime assessment of the uterine structures and blood flow, whereas magnetic resonance (MR) imaging can be helpful imaging modality in complicated cases [1]. The most sensitive finding of RPOC at gray-scale US is a thickened endometrial echo complex (EEC). The exact definition of “thickened” varies in the literature, ranging from 8 to 13 mm. The degree of vascularity in a thickened EEC or endometrial mass can help improve diagnostic assessment of RPOC. To better describe the typical color Doppler US findings of RPOC, the degree of vascularity of the endometrial component can be compared with the myometrial vascularity in the same image section and graded [7].
Ultrasonography (US) is useful in the evaluation of RPOC and the diagnosis is supposed on the sonographic appearance of intrauterine echogenic material. Although transvaginal sonographic enhances evaluation for RPOC, the diagnosis is sometimes difficult because necrotic decidua and blood clots may be very difficult to differentiate from RPOC [7]. For this reason combined gray scale and color Doppler US can improve the valuation of suspected RPOC, allows realtime assessment of the uterine structures and blood flow, whereas magnetic resonance (MR) imaging can be helpful imaging modality in complicated cases [1]. The most sensitive finding of RPOC at gray-scale US is a thickened endometrial echo complex (EEC). The exact definition of “thickened” varies in the literature, ranging from 8 to 13 mm. The degree of vascularity in a thickened EEC or endometrial mass can help improve diagnostic assessment of RPOC. To better describe the typical color Doppler US findings of RPOC, the degree of vascularity of the endometrial component can be compared with the myometrial vascularity in the same image section and graded [7].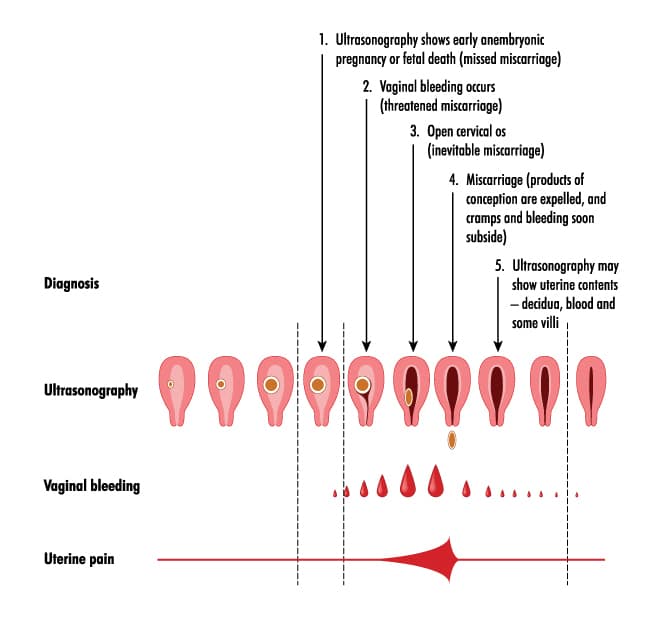 Transvaginal sonohysterography has also been shown to be an useful method. Combining these tecniques, color Doppler sonography and sonohysterography, may increase the accuracy of the diagnosis of RPOC over that from conventional sonography [8]. The majority of women with placenta accreta have no symptoms during pregnancy [9]. However Prenatal diagnosis of MAP and its variants can help reduce maternal/fetal morbidity and mortality by allowing us to choose the best time and place of birth. Calì et al. have to identify ultrasonographic criteria for morbidly adherent placent (MAP): loss/irregularity of the echolucent area between uterus and placenta, termed ‘clear space’; thinning or interruption of the hyperechoic interface between uterine serosa and bladder wall, termed ‘bladder line’; presence of turbulent placental lacunae13,14 with high-velocity flow (>15 cm/s). Transabdominal 3D powerDoppler was used to map the vascularization of the intraplacental and uterine serosa-bladder interface.
Transvaginal sonohysterography has also been shown to be an useful method. Combining these tecniques, color Doppler sonography and sonohysterography, may increase the accuracy of the diagnosis of RPOC over that from conventional sonography [8]. The majority of women with placenta accreta have no symptoms during pregnancy [9]. However Prenatal diagnosis of MAP and its variants can help reduce maternal/fetal morbidity and mortality by allowing us to choose the best time and place of birth. Calì et al. have to identify ultrasonographic criteria for morbidly adherent placent (MAP): loss/irregularity of the echolucent area between uterus and placenta, termed ‘clear space’; thinning or interruption of the hyperechoic interface between uterine serosa and bladder wall, termed ‘bladder line’; presence of turbulent placental lacunae13,14 with high-velocity flow (>15 cm/s). Transabdominal 3D powerDoppler was used to map the vascularization of the intraplacental and uterine serosa-bladder interface. In particular, the sagittal sections were used to assess the depth of placental tissue neovascularization and whether this was limited to the basal layer or if it affected the entire remaining placental parenchyma.
In particular, the sagittal sections were used to assess the depth of placental tissue neovascularization and whether this was limited to the basal layer or if it affected the entire remaining placental parenchyma.
Coronal sections were used to assess the extent of the serosa-bladder wall interface neovascularization and to determine if the process involved the whole area or only a portion [10].
In our case Doppler US excluded vascularization of the neoformation and sonohysterography demonstrated that the mass was strictly adherent to uterine walls. Once RPOC is diagnosed on the basis of clinical, laboratory, and US findings, several treatment are available, including expectant management, use of uterotonic medications such as prostaglandin E1 analogs, and surgical interventions such as dilation and curettage and hysteroscopic removal. Actually there aren’t clear guidelines for optimal treatment of retained products of conception with high risks of the complications in these women [11]. Short term consequences of RPOC include bleeding and infections, while long term consequences include formation of intrauterine adhesions, also defined Asherman’s syndrome. Historically the curettage with a large curette was the standard of care. Therefore a more conservative management included awaiting spontaneous expulsion of the placental tissue with the aid of prostaglandins; but a new approach is reported by Goldenberg et al. that introduced the use of hysteroscopy [12]. The goal of this procedure is decrease thermal damage to the endometrium, preserve the integrity of the uterine cavity minimizing rates of intrauterine adhesions and fertility problems. Additional advantages may be complete removal of RPOC without the need for a second procedure, and identification and treatment of uterine cavity anomalies, which are sometime the underlying cause of RPOC [12]. However this technique may be problematic in the immediate postpartum period due to heavy vaginal bleeding and it has been suggested that hysteroscopic selective resection of the retained products of conception should be considered in patients with secondary (delayed) postpartum bleeding [1].
Short term consequences of RPOC include bleeding and infections, while long term consequences include formation of intrauterine adhesions, also defined Asherman’s syndrome. Historically the curettage with a large curette was the standard of care. Therefore a more conservative management included awaiting spontaneous expulsion of the placental tissue with the aid of prostaglandins; but a new approach is reported by Goldenberg et al. that introduced the use of hysteroscopy [12]. The goal of this procedure is decrease thermal damage to the endometrium, preserve the integrity of the uterine cavity minimizing rates of intrauterine adhesions and fertility problems. Additional advantages may be complete removal of RPOC without the need for a second procedure, and identification and treatment of uterine cavity anomalies, which are sometime the underlying cause of RPOC [12]. However this technique may be problematic in the immediate postpartum period due to heavy vaginal bleeding and it has been suggested that hysteroscopic selective resection of the retained products of conception should be considered in patients with secondary (delayed) postpartum bleeding [1].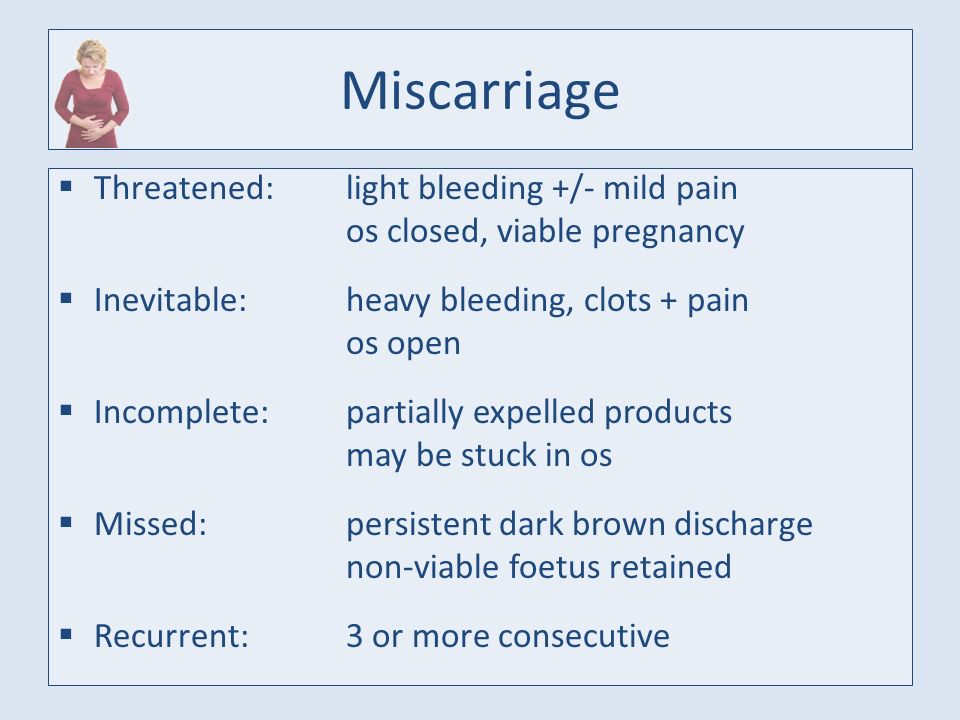 Although hysteroscopy is theoretically less traumatic to the endometrium than curettage, the recent available literature points out that lack scientific evidence to prove that the hysteroscopic technique is superior to the traditional suction and curettage in terms of intrauterine adhesions rates and future pregnancies [13]. Retained placental tissue following birth, and retained products of conception following curettage, are not uncommon consequences. In most cases, secondary evacuation of the retained tissue ends without any sequelae. However, in a minority of cases the formation of intrauterine adhesions may significantly affect future reproductive outcomes due to infertility or miscarriages. Although histopathological examination of tissue is required to ascertain diagnosis, our experience shows the importance of an accurate diagnosis grounded on clinical presentation in association with imaging features [1]. Our experience shows that the first step in all bleeding cases was to evaluate the uterine cavity by ultrasound, but sometimes it was difficult to distinguish between placental tissue and blood clots, however ultrasonography combined gray scale-color Doppler and sonohysterography is the best predictor in women with a suspicion of RPOC.
Although hysteroscopy is theoretically less traumatic to the endometrium than curettage, the recent available literature points out that lack scientific evidence to prove that the hysteroscopic technique is superior to the traditional suction and curettage in terms of intrauterine adhesions rates and future pregnancies [13]. Retained placental tissue following birth, and retained products of conception following curettage, are not uncommon consequences. In most cases, secondary evacuation of the retained tissue ends without any sequelae. However, in a minority of cases the formation of intrauterine adhesions may significantly affect future reproductive outcomes due to infertility or miscarriages. Although histopathological examination of tissue is required to ascertain diagnosis, our experience shows the importance of an accurate diagnosis grounded on clinical presentation in association with imaging features [1]. Our experience shows that the first step in all bleeding cases was to evaluate the uterine cavity by ultrasound, but sometimes it was difficult to distinguish between placental tissue and blood clots, however ultrasonography combined gray scale-color Doppler and sonohysterography is the best predictor in women with a suspicion of RPOC. This approach represents a useful diagnostic tool for prompt evaluation for timely treatment and for preserve fertility of these women. Further studies may be necessary to confirm the benefit of hysteroscopy over traditional suction and curettage for treatment of RPOC [14]. So a careful investigation, a management with efficient planning and an accurate follow up are required in patients with retained products of conception to lessen morbidity and to preserve their obstetric outcome. In our study, we have presented a conservative approach for placenta accreta case. Planned cesarean hysterectomy at the time of cesarean is the standard recommended treatment in the United States, but over the last years interest in conservative management has most resurged [15]. Conservative management should be the preferred approach for reduce the morbility of peripartum hysterectomy and especially for save fertility in young women. Our surgical procedure seems to be useful in the conservative treatment of placenta accreta.
This approach represents a useful diagnostic tool for prompt evaluation for timely treatment and for preserve fertility of these women. Further studies may be necessary to confirm the benefit of hysteroscopy over traditional suction and curettage for treatment of RPOC [14]. So a careful investigation, a management with efficient planning and an accurate follow up are required in patients with retained products of conception to lessen morbidity and to preserve their obstetric outcome. In our study, we have presented a conservative approach for placenta accreta case. Planned cesarean hysterectomy at the time of cesarean is the standard recommended treatment in the United States, but over the last years interest in conservative management has most resurged [15]. Conservative management should be the preferred approach for reduce the morbility of peripartum hysterectomy and especially for save fertility in young women. Our surgical procedure seems to be useful in the conservative treatment of placenta accreta. The patient presented any septic complication or secondary vaginal bleeding. However subsequent pregnancies after conservative treatment for placenta accreta were mostly successful, a history of placenta accreta is an independent risk factor for recurrent placenta accrete and postpartum hemorrhage [16]. This should be taken into account in order to ensure future safety pregnancies and deliveries to patients. In fact in these patients the site and time of delivery, as well as the surgical approach, can be planned ahead and blood loss minimized.
The patient presented any septic complication or secondary vaginal bleeding. However subsequent pregnancies after conservative treatment for placenta accreta were mostly successful, a history of placenta accreta is an independent risk factor for recurrent placenta accrete and postpartum hemorrhage [16]. This should be taken into account in order to ensure future safety pregnancies and deliveries to patients. In fact in these patients the site and time of delivery, as well as the surgical approach, can be planned ahead and blood loss minimized.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
1. Sellmyer MA, Desser TS, Maturen KE, Jeffrey RB Jr, Kamaya A. Physiologic, histologic, and imaging features of retained products of conception. Radiographics. 2013;33:781–96. [PubMed] [Google Scholar]
2. Wolman I, Altman E, Faith G, Har-Toov J, Amster R, Gull I, Jaffa AJ. Combined clinical and ultrasonographic work-up for the diagnosis of retained products of conception. Fertil Steril. 2009;92:1162–4. [PubMed] [Google Scholar]
Combined clinical and ultrasonographic work-up for the diagnosis of retained products of conception. Fertil Steril. 2009;92:1162–4. [PubMed] [Google Scholar]
3. Chaudhary P, Sharma S, Yadav R, Dhaubhadel P. B-Lynch brace suture: an effective method of conservative surgical management for placenta increta. Kathmandu Univ Med J (KUMJ) 2004;2:149–51. [PubMed] [Google Scholar]
4. Humphrey J. Primary cesarean delivery results in emergency hysterectomy due to placenta accreta: a case study. AANA J. 2015;83:28–34. [PubMed] [Google Scholar]
5. Kelekci S, Ekmekci E, Aydogmus S, Gencdal S. A Comprehensive Surgical Procedure in Conservative Management of Placenta Acc-reta: A Case Series. Medicine (Baltimore) 2015;94:e529. [PMC free article] [PubMed] [Google Scholar]
6. Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005;192:1458–1461. [PubMed] [Google Scholar]
7. Ustunyurt E, Kaymak O, Iskender C, Ustunyurt OB, Celik C, Danisman N.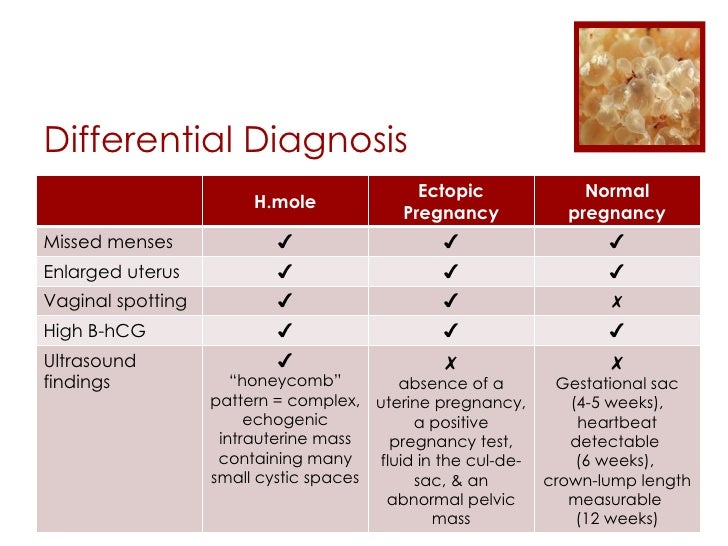 Role of transvaginal sonography in the diagnosis of retained products of conception. Arch Gynecol Obstet. 2008;277:151–4. [PubMed] [Google Scholar]
Role of transvaginal sonography in the diagnosis of retained products of conception. Arch Gynecol Obstet. 2008;277:151–4. [PubMed] [Google Scholar]
8. Wolman I, Altman E, Fait G, Har-Toov J, Gull I, Amster R, Jaffa A. Transvaginal Sonohysterography for the Evaluation and Treatment of Retained Products of Conception. Gynecol Obstet Invest. 2000;50:73–6. [PubMed] [Google Scholar]
9. Snegovskikh D, Clebone A, Norwitz E. Anesthetic management of patients with placenta accreta and resuscitation strategies for associated massive hemorrhage. Curr Opin Anaesthesiol. 2011;24:274–281. [PubMed] [Google Scholar]
10. Cali G, Giambanco L, Puccio G, Forlani F. Morbidly adherent placenta: evaluation of ultrasound diagnostic criteria and differentiation of placenta accreta from percreta. Ultrasound Obstet Gynecol. 2013;41:406–412. [PubMed] [Google Scholar]
11. Fejgin MD, Shvit TY, Gershtansky Y, Biron-Shental T. Retained placentalt issue as an emerging cause for malpractice claims. Isr Med Assoc J. 2014;16:502–5. [PubMed] [Google Scholar]
Isr Med Assoc J. 2014;16:502–5. [PubMed] [Google Scholar]
12. Smorgick N, Barel O, Fuchs N, Ben-Ami I, Pansky M, Vaknin Z. Hysteroscopic management of retainedproducts of conception: meta-analysis and literaturereview. Eur J Obstet Gynecol Reprod Biol. 2014;173:19–22. [PubMed] [Google Scholar]
13. Barel O, Krakov A, Pansky M, Vaknin Z, Halperin R, Smorgick N. Intrauterine adhesions after hysteroscopic treatment for retained products of conception: what are the riskfactors? Fertil Steril. 2015;103:775–9. [PubMed] [Google Scholar]
14. Golan A, Dishi M, Shalev A, Keidar R, Ginath S, Sagiv R. Operative Hysteroscopy to Remove Retained Products of Conception: Novel Treatment of an Old Problem. J Minim Invasive Gynecol. 2011;18:100–3. [PubMed] [Google Scholar]
15. Fox KA, Shamshirsaz AA, Carusi D, Secord AA, Lee P, Turan OM, Huls C, Abuhamad A, Simhan H, Barton J, Wright J, Silver R, Belfort MA. Conservative management of morbidly adherent placenta: expert review. Am J Obstet Gynecol. 2015 [Epub ahead of print] [PubMed] [Google Scholar]
2015 [Epub ahead of print] [PubMed] [Google Scholar]
16. Vinograd A, Wainstock T, Mazor M, Mastrolia SA, Beer-Weisel R, Klaitman V, Dukler D, Hamou B, Benshalom-Tirosh N, Vinograd O, Erez O. A prior placenta accreta is an independent risk factor for post-partum hemorrhage in subsequent gestations. Eur J Obstet Gynecol Reprod Biol. 2015;187:20–24. [PubMed] [Google Scholar]
Miscarriage, symptoms - Health Clinic 365 Yekaterinburg
Causes of miscarriage
Questions to the doctor about miscarriage
Diagnosis of miscarriage
Treatment and prevention of miscarriage
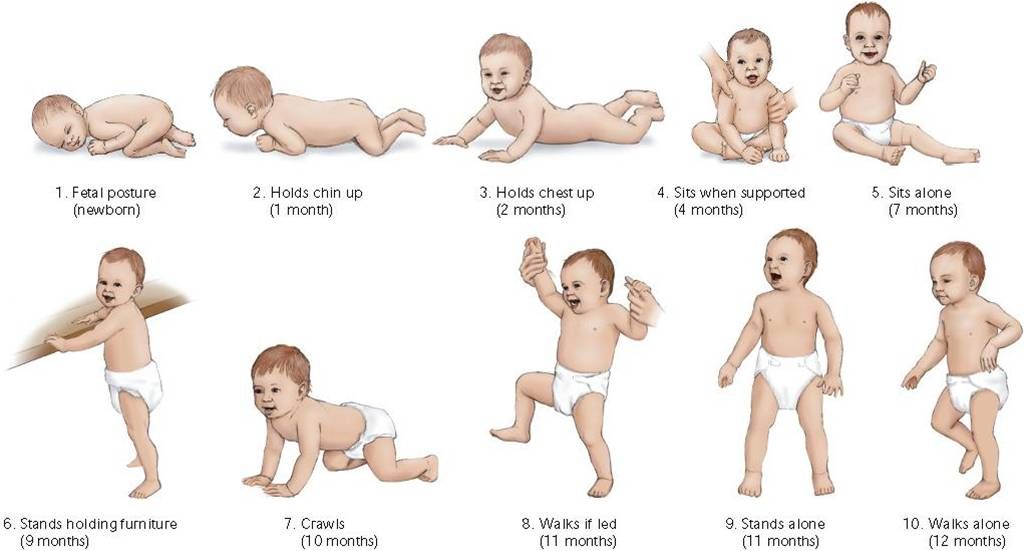
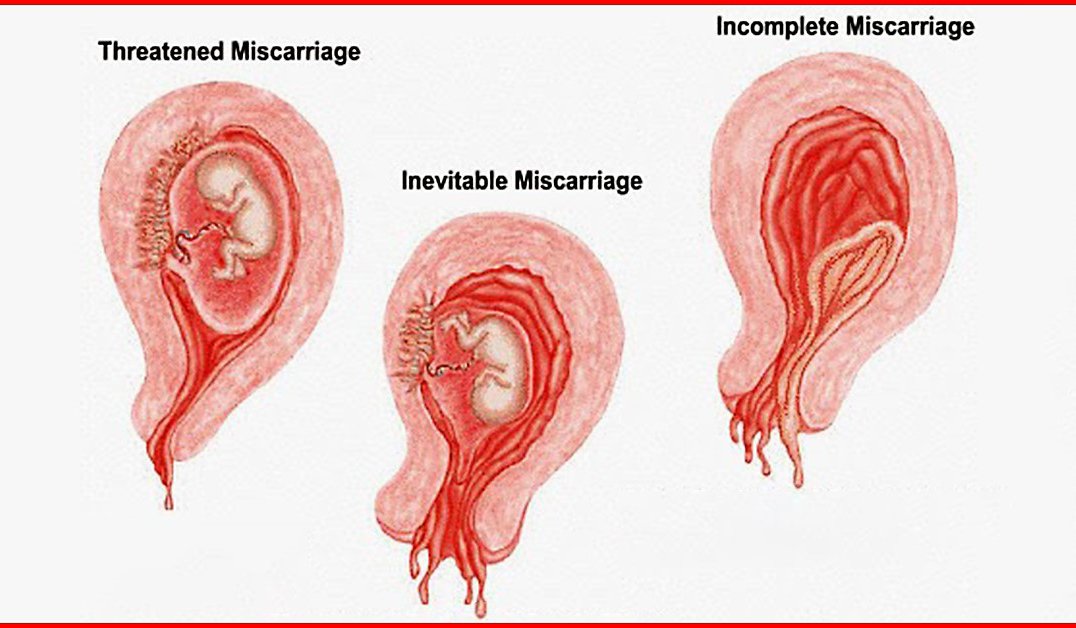
According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus. nine0003 Miscarriage is quite common, but this fact does not make things any easier. Miscarriage symptoms . Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include: It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage. nine0003 Some women who have a miscarriage develop an infection in the uterus. When to see a doctor. Call your doctor if: You can put a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy. nine0003 You can get more detailed information about miscarriage from the gynecologists of the Health 365 clinic in Yekaterinburg. Gynecologist, initial appointment 2300 i When a woman finds out about her pregnancy, she changes her rhythm of life, especially if the pregnancy is desired. However, depending on many circumstances, miscarriage , that is, a natural termination of pregnancy, may occur. Statistics say that up to 20 percent of pregnancies end in pathological abortions. Often a woman may not know that she was pregnant, as a miscarriage sometimes occurs at a very early stage and seems to be just a normal delay in menstruation followed by heavy discharge. nine0003 If a woman finds out that she is pregnant and wants to become a mother, she should be very attentive to her condition. The threat of miscarriage often occurs in the early stages of pregnancy and therefore it is necessary to know what symptoms and signs precede a sudden miscarriage. Signs The main sign of a suspected miscarriage is bleeding from the uterus. They happen not abundant, pale scarlet or gray-brown. The discharge most often gradually increases and is characterized by sudden spasms or pulling pains in the lower abdomen. These symptoms may last for some time. nine0003 The pains are often so mild that the woman simply does not pay attention to them. They are able to be interrupted, and the woman simply forgets about them, especially if the discharge also stopped, and before that they were insignificant. Meanwhile, the very first symptoms should alert you and you should urgently go to the gynecologist for examination and consultation. Even if the process has stopped, after a few days you can feel a sharp deterioration in health, and then you can no longer save the life of the unborn child. Be sure to pay attention to what exactly comes out with the discharge, if there are tissue fragments, it means that miscarriage has already occurred. Terms of miscarriages A miscarriage is classified as early if it occurred before twelve weeks from the onset of pregnancy. Starting from the 22nd week, if a spontaneous miscarriage has occurred, it is considered late. If the termination of pregnancy occurred before thirty-seven weeks, then this is already called premature birth. All subsequent fetal rejections are called term births and are generally considered normal, since during this period, mostly able-to-survive children are born. In modern medicine, children born after 22 weeks are nursed and subsequently do not differ from those born at term with normal weight. nine0003 Types of miscarriages Specialists have identified several types of miscarriages. Causes of spontaneous abortion The vast majority of women, having learned about their pregnancy, want to give birth to a healthy baby. And if a spontaneous miscarriage occurs, then for a failed mother this is a real tragedy. There are several reasons for this: This is the most common cause of miscarriage. This is not due to heredity, it is a consequence of the mutation of parent germ cells, which accidentally ended up in unfavorable conditions. This is also the influence of radiation, poisoning, viruses, that is, temporary situations that affected the quality of germ cells. The body thus gets rid of a weak non-viable fetus. It is impossible and unnecessary to prevent such spontaneous abortion. It is only necessary, having decided to become pregnant, to try to cleanse your body of possible harmful influences. nine0003 The cause of a miscarriage at a very early stage also lies in the lack of the hormone progesterone, or in the fact that a woman has an excess of male sex hormones that suppress the production of estrogen and progesterone in her body. In this case, the vitality of the fetus is directly affected by the Rh conflict. The embryo will inherit the positive Rh of the man, and if the partner has a negative Rh, then her body simply rejects cells that are foreign to him. A similar situation can be prevented by injecting the expectant mother with a variety of progesterone, a process called immunomodulation. Sexually transmitted infections such as toxoplasmosis, syphilis, trichomoniasis, chlamydia and others are of great danger. External infection: bacteria and viruses infect the fetal membranes, and the body will inevitably reject the embryo. Therefore, before becoming pregnant, you should be examined to know for sure that there are no infections, and if the result is positive, undergo treatment. In addition, all inflammatory processes, various diseases of the internal organs, which are accompanied by a persistent high temperature, can also lead to unexpected rejection of the fetus. Rubella is especially dangerous, and viral hepatitis is common. But even a sore throat, mild pneumonia, appendicitis sometimes play a key role and lead to a miscarriage, so the expectant mother must undergo a thorough examination even before the child is conceived, and then beware of all kinds of infections and weakening of the body. nine0003 If a woman had an abortion in a hospital and then became pregnant and decided to give birth, there is a risk that she will have a miscarriage. Abortion is a stress factor for the body, ovarian dysfunction is often observed, inflammatory processes in the female genital organs can begin, and all this will lead, at best, to miscarriage and subsequent repeated miscarriages, and at worst, to infertility. Pregnant women should not take any medication at all, especially during the first three calendar months. Medicines and herbs can cause various defects in the fetus, which in turn will lead to its rejection. Analgesics and uncontrolled hormonal contraceptives are especially dangerous. Parsley and nettle should be eaten with caution - they cause a high tone of the uterus, which in turn can reject the fetus. nine0003 It is no coincidence that in ancient times, pregnant women were protected from unrest, they were created comfortable conditions, they tried to give as many positive emotions as possible. Now the direct dependence of the health of the unborn baby on the mental state during pregnancy has already been proven. Any stress, fear and overstrain can cause an unexpected termination of pregnancy. Of course, the intake of alcoholic beverages, an unhealthy lifestyle, smoking, even coffee consumption in large quantities, improper diet - all this can lead to a transient miscarriage. Therefore, the expectant mother should prioritize and change her rhythm of life in advance in order to give birth to a healthy child. All of these factors can affect the fetus, so you should protect yourself and your baby by avoiding these activities. What to do after a miscarriage? Having experienced the tragedy of losing a child, parents often intend to immediately conceive a new baby, but they are afraid that everything will happen again. If no obvious cause is found, the fetus most likely has a chromosomal abnormality. In this case, you should not worry, since the next conception will occur with a different set of chromosomes, which means that there will be no repeated miscarriage. If the miscarriage was repeated, it is necessary to contact a geneticist and conduct a study of the set of chromosomes of both parents. If it turns out that the cause was an infection, then it is necessary to fully recover. If we are talking about sexual infections, then both parents need to undergo therapy. It is necessary to take tests for hormonal studies, hemostasis systems and determine the immune status. nine0003 After a miscarriage, should be treated, if necessary, and pause between conceptions. The first week after a miscarriage women often experience pain in the lower abdomen, heavy bleeding, so you should refrain from sexual intercourse with a man. If there is severe bleeding, acute pain in the lower abdomen, convulsions, high fever, palpitations, nausea, vomiting, then you should immediately consult a doctor to identify the cause of this condition. It is necessary to plan a subsequent pregnancy not earlier than three months after this situation, but preferably six months later. It is very important during this recovery period to have a positive attitude and confidence that the next attempt will be successful. This is harder to do than to say, because after a miscarriage the woman is depressed and afraid of a repeat of the situation. You can’t get hung up on your problem, during this period it’s better to do some favorite thing, relax, change the situation, travel, visit the city more often. The modern ecological situation in cities has a bad effect on women's health, so private trips to nature, a trip to the sea, to friends in another city can distract from painful thoughts. An important role in this case is played by the woman's relatives and, above all, the husband, who can surround her with care and attention, creating peace of mind.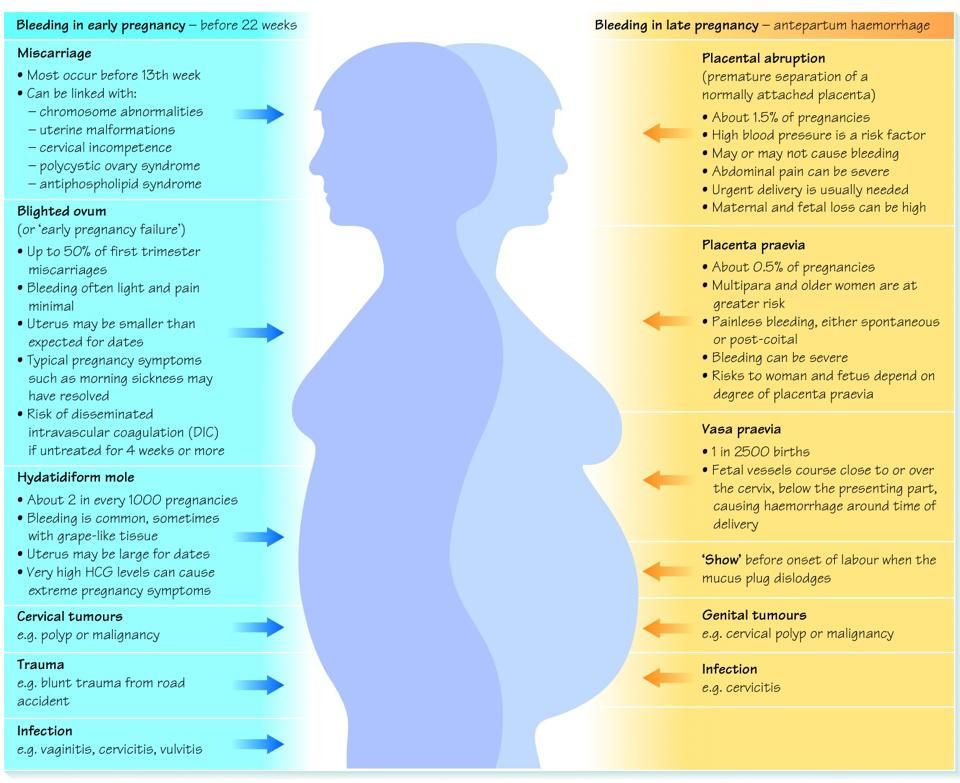 It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
 This infection, also called septic miscarriage, can cause:
This infection, also called septic miscarriage, can cause:
Prices
Miscarriage. What to do after a miscarriage?
 Therefore, one should not hesitate to go to the doctor, the fetus may come out, in whole or in parts, there may be white particles or a round gray bubble. When the body is completely cleansed, the pain will subside, but before that it may continue for some time.
Therefore, one should not hesitate to go to the doctor, the fetus may come out, in whole or in parts, there may be white particles or a round gray bubble. When the body is completely cleansed, the pain will subside, but before that it may continue for some time. 
 Many, having experienced an abortion, try to conceive a child faster again, but first you need to know the reasons for what happened in order to save the fetus in the future. According to statistics, the largest number of miscarriages occurs precisely in the early stages. nine0003
Many, having experienced an abortion, try to conceive a child faster again, but first you need to know the reasons for what happened in order to save the fetus in the future. According to statistics, the largest number of miscarriages occurs precisely in the early stages. nine0003
 In this case, the fetus can be saved medically by administering the necessary medicines to the woman. The work of the adrenal glands, as well as the thyroid gland, affects the production of hormones, so a lot depends on the work of these glands throughout the pregnancy process. nine0003
In this case, the fetus can be saved medically by administering the necessary medicines to the woman. The work of the adrenal glands, as well as the thyroid gland, affects the production of hormones, so a lot depends on the work of these glands throughout the pregnancy process. nine0003
 nine0003
nine0003
 Therefore, you need to think very seriously before going for an abortion. nine0003
Therefore, you need to think very seriously before going for an abortion. nine0003
 If you have a problem (death of a loved one, divorce, etc.), you need to find sedatives with the help of a doctor, they will help you cope with this period. nine0003
If you have a problem (death of a loved one, divorce, etc.), you need to find sedatives with the help of a doctor, they will help you cope with this period. nine0003
 In this case, you do not need to make independent decisions, but consult a doctor. And first of all, it is necessary to identify the cause that led to the miscarriage. For this, the expectant mother needs to undergo as thorough an examination as possible. nine0003
In this case, you do not need to make independent decisions, but consult a doctor. And first of all, it is necessary to identify the cause that led to the miscarriage. For this, the expectant mother needs to undergo as thorough an examination as possible. nine0003 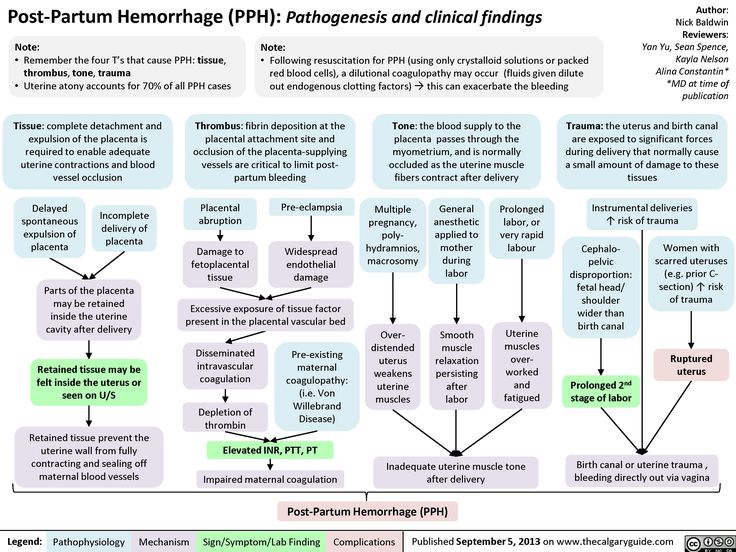 During pregnancy, you should not take medications to prevent re-spontaneous pathological termination of pregnancy. Therefore, you can become pregnant only after the end of the course of treatment. If the cause was hormonal abnormalities, then the expectant mother should take special drugs to stabilize the background, and at this time she should never become pregnant. During the pause, you need to choose contraceptives with the help of a doctor. You can go to a specialized clinic where you will be prescribed a full course of rehabilitation. nine0003
During pregnancy, you should not take medications to prevent re-spontaneous pathological termination of pregnancy. Therefore, you can become pregnant only after the end of the course of treatment. If the cause was hormonal abnormalities, then the expectant mother should take special drugs to stabilize the background, and at this time she should never become pregnant. During the pause, you need to choose contraceptives with the help of a doctor. You can go to a specialized clinic where you will be prescribed a full course of rehabilitation. nine0003  Until that time, it is worth reconsidering your outlook on life, giving up hard work, eating right and wisely, taking vitamins, exercising, losing weight if you are overweight, stop smoking, drinking alcohol, think over your daily routine. nine0003
Until that time, it is worth reconsidering your outlook on life, giving up hard work, eating right and wisely, taking vitamins, exercising, losing weight if you are overweight, stop smoking, drinking alcohol, think over your daily routine. nine0003