Twitching legs in pregnancy
What can I do about restless legs syndrome during pregnancy?
What is restless legs syndrome?
Restless legs syndrome, also known as Willis-Ekbom disease, is a common condition of the nervous system that causes an overwhelming irresistible urge to move your legs.
What are the symptoms of restless legs syndrome?
The main symptom is the overwhelming urge to move your legs. But you may also have uncomfortable and unpleasant sensations in your legs. Some people describe these as:
- tingling
- burning
- itching
- a ‘creepy-crawly’ sensation, like ants moving up and down the legs
- like fizzy water in the veins.
These sensations are often worse just below the knee and can sometimes be painful.
Your symptoms may be worse when you’re resting and may feel better when you move. They may be worse in the evening or at night.
Restless legs syndrome can be very frustrating, but it should not affect your health or pregnancy. However, it can make it more difficult to get a good night’s sleep. A lack of sleep won’t hurt your baby, but it can make your day-to-day life a bit more difficult. We have some tips that may help you sleep better.
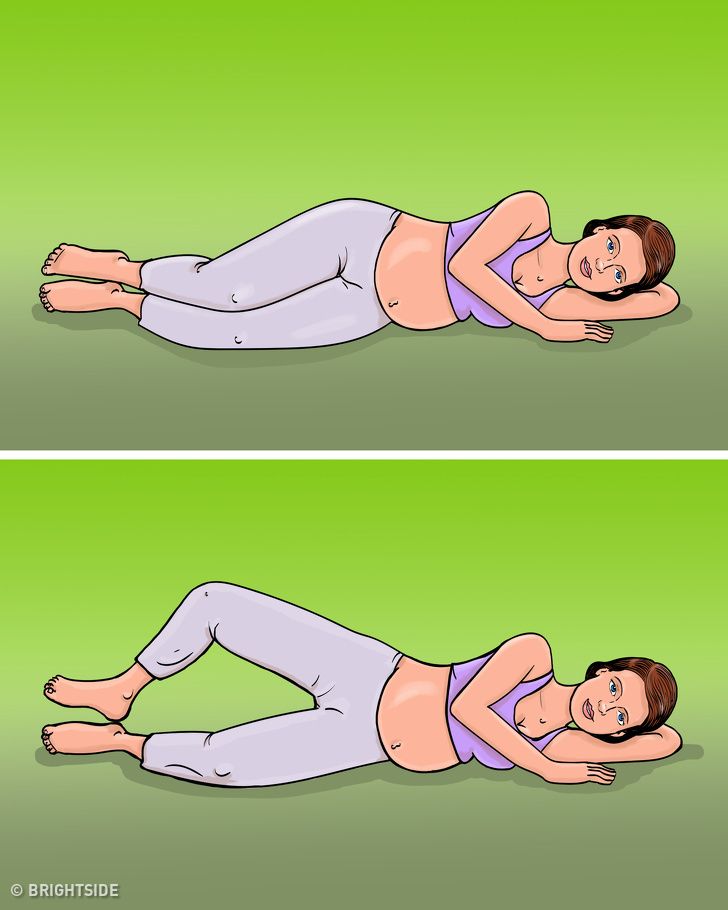
Restless legs syndrome caused by pregnancy usually develops during the third trimester (the last 3 months of pregnancy). At this point, sleeping on your side is the safest thing to do for your baby because research shows it can reduce the risk of stillbirth.
How is restless legs syndrome diagnosed?
Unfortunately, there isn’t a test that can confirm whether you have restless legs syndrome. Instead, your doctor or midwife will talk to you about your symptoms and medical history.
What causes restless legs syndrome?
Sometimes the cause for restless legs syndrome is not known. These cases are known as idiopathic.
Pregnancy
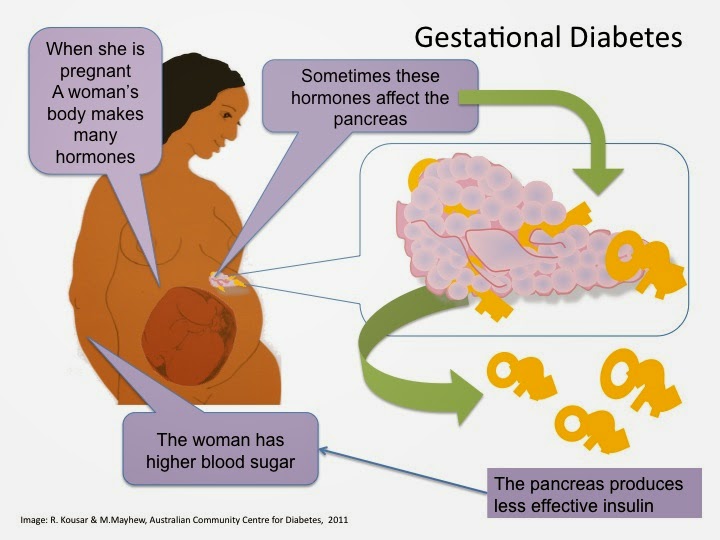
About 20% of pregnant women develop restless legs syndrome, usually in the third trimester. This is possibly caused by a change in hormones.
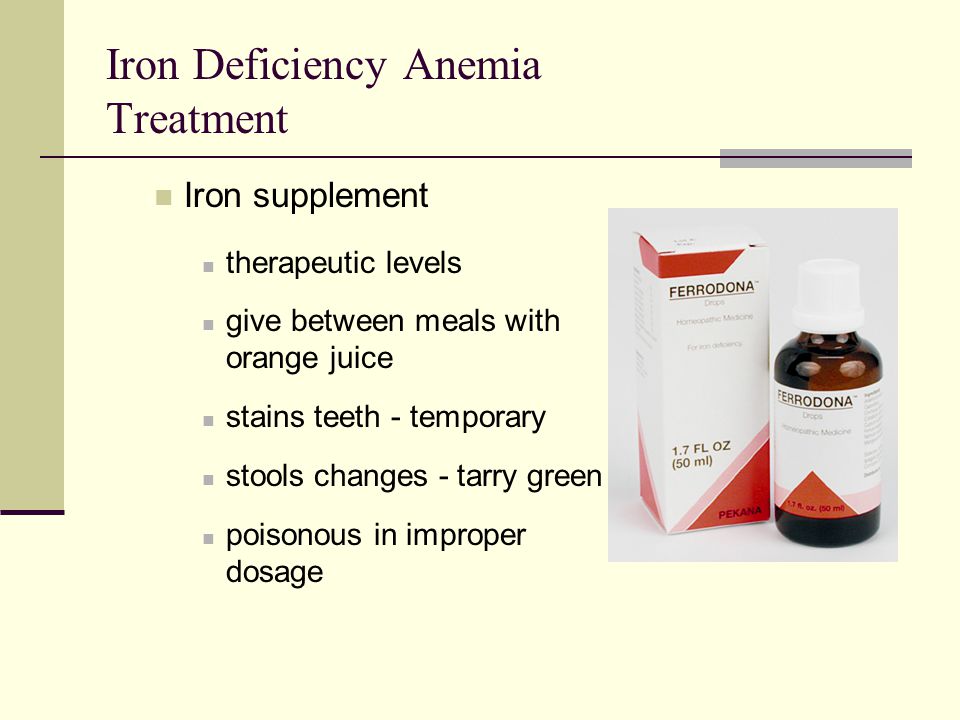
Iron-deficiency anaemia
Anaemia (a blood condition) can sometimes cause restless leg syndrome and iron-deficiency anaemia can be common in pregnancy.
You’ll be checked for anaemia as part of your routine antenatal care, but you can have a test at any time during your pregnancy if there are any concerns.
If you have anaemia, you’ll probably be prescribed iron supplements as tablets or as a liquid to take every day. Eating a healthy, balanced diet will also help you get the iron you need to either prevent anaemia or manage your symptoms if you have it.
Other conditions
There are some conditions that may cause restless legs syndrome, although the scientific research to prove this is limited. These include:
- neurological conditions, such as Parkinson’s disease and multiple sclerosis
- rheumatoid arthritis
- diabetes
- hypothyroidism
- a very high BMI (body mass index)
Some medications
Some medications can cause restless legs syndrome or make it worse, including
- antidepressants
- some antipsychotics and lithium
- some antiepileptic drugs
- antihistamines
- dopamine receptor blocking agents such as metoclopramide and prochlorperazine
- beta-blockers.
But it’s important not to stop taking any medications without speaking to your doctor first.
Diet
There is also a theory that drinking excessive amounts of alcohol, caffeine, or eating too much chocolate can cause restless legs syndrome.
There isn’t enough scientific evidence to prove this is true. But we know for certain that drinking alcohol in pregnancy can cause serious complications in pregnancy. The more you drink, the greater the risk. There is no known safe level for drinking during pregnancy, so the safest approach is not to drink at all while you're pregnant.
Caffeine is found in coffee, tea, some soft drinks, energy drinks and chocolate. Drinking a lot of caffeine in pregnancy has also been linked to miscarriage and low birth weight so the advice is to limit your intake to 200mg a day. You can check your caffeine intake with our pregnancy caffeine calculator.
What is the treatment for restless legs syndrome during pregnancy?
Medication isn’t generally recommended during pregnancy or while you are breastfeeding. But there are other things you can try. You may not be able to stop the symptoms completely, but you may be able to reduce them.
But there are other things you can try. You may not be able to stop the symptoms completely, but you may be able to reduce them.
As well as reducing your caffeine intake and not drinking alcohol, you can try:
- stopping smoking (this can also reduce the risk of serious pregnancy complications)
- doing moderate, regular exercise (such as swimming)
- walking and stretching your legs
- relaxation exercises
- using heat pads on the legs, or having a hot bath
- using distraction techniques, such as reading
- massaging the legs.
Will restless legs syndrome go away after I give birth?
Yes. If your symptoms are caused by pregnancy, it’s likely that they will go away soon after giving birth. Unfortunately, women who have restless legs syndrome during pregnancy have an increased risk of developing the syndrome in later life.
Other conditions with similar symptoms to restless legs syndrome
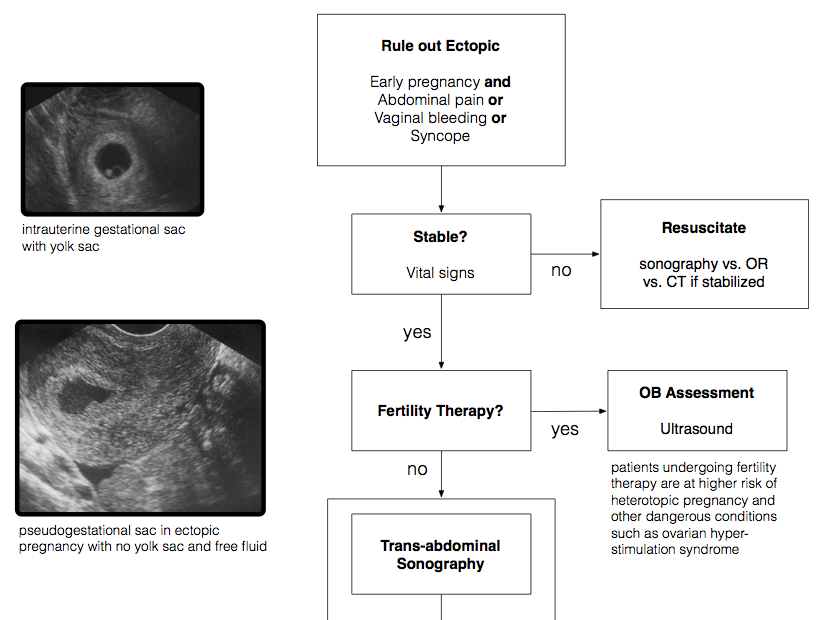
Blood clots
The symptoms of restless leg syndrome can sometimes be confused with the symptoms of blood clots (deep vein thrombosis). However, they are different problems.
However, they are different problems.
Deep vein thrombosis (DVT) can happen for no apparent reason, but you are more at risk during pregnancy and just after having your baby.
Call 111 or arrange an urgent appointment with your GP if you have these symptoms in your leg:
- throbbing or cramping pain in 1 leg (rarely both legs), usually in the calf or thigh
- swelling in 1 leg (rarely both legs)
- warm skin around the painful area
- red or darkened skin around the painful area
- swollen veins that are hard or sore when you touch them
These symptoms also happen in your arm or tummy if that's where the blood clot is.
Your risk of developing DVT during pregnancy is even greater if you:
- or a close family member have had a blood clot before
- are over 35
- have a BMI of 30 or more
- have a condition that makes clots more likely
- are carrying twins or multiple babies
- have had fertility treatment
- have had a caesarean section
- smoke
- fly for more than 4 hours.

Call 999 or go to your nearest A&E if you have any of these symptoms, with chest pain or breathlessness. This may mean that the DVT has travelled to your lungs, which can be life threatening.
Staying as active as you can during pregnancy can help reduce the risk of a DVT.
Meralgia paraesthetica
Another condition that can cause uncomfortable or painful feelings in the leg is meralgia paraesthetica. This is a common problem caused by a trapped nerve in the thigh. The most common cause for this is recent weight gain or pregnancy. This causes a painful patch of burning, numbness or pins and needles on the outer side of the thigh (although the affected area can vary from person to person). This should get better after pregnancy but talk to your GP or midwife if you have this kind of pain.
Dealing With Restless Legs Syndrome While You're Pregnant
Written by Stephanie Watson
In this Article
- Causes of Restless Legs Syndrome in Pregnancy
- Treating RLS While Pregnant
- Lifestyle Changes
Nearly a third of pregnant women have a condition called restless legs syndrome (RLS). People who have restless legs syndrome describe it as an "itchy," "pulling," "burning," "creepy-crawly" feeling that gives them an overwhelming urge to move their legs.
People who have restless legs syndrome describe it as an "itchy," "pulling," "burning," "creepy-crawly" feeling that gives them an overwhelming urge to move their legs.
Once they do move their legs, the feeling often subsides. But by then the sensation has already woken them up.
Causes of Restless Legs Syndrome in Pregnancy
Scientists don't know exactly what causes the sensations in the legs at night. But some believe it may stem from an imbalance of the brain chemical dopamine. That chemical normally helps keep muscle movements smooth and even.
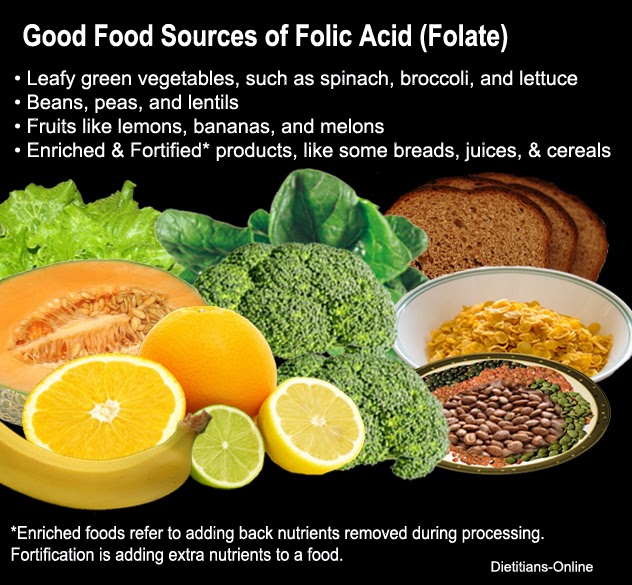
RLS in pregnancy might be triggered by a lack of enough folic acid or iron. There's also some evidence that rising estrogen levels during pregnancy may contribute to RLS.
Trying to calm your restless legs all night can make you sleepy and irritable during the day.
Having restless legs syndrome can also make you more likely to have a longer labor and to need a C-section.
Treating RLS While Pregnant
If your symptoms are severe enough to interrupt your sleep night after night, you'll probably want to see your doctor to get RLS treated. That can be challenging during pregnancy.
That can be challenging during pregnancy.
Most drugs typically used to treat restless legs syndrome, such as Requip (ropinirole) and Mirapex (pramipexole), have not been studied extensively in pregnant women. So there is not enough data to determine all potential risks for a developing fetus.
Before you take any medicine for restless legs syndrome, your doctor should check your iron levels. If you're low, you can take an iron supplement. In many cases where the supply of iron in the body is low a supplement will be enough to correct RLS.
If your RLS symptoms still don't go away after an iron deficiency has been found and treated, some doctors prescribe opioid (narcotic) medication. Because of a risk of withdrawal symptoms in a newborn, opioids are typically given for a short period of time.
Also, the FDA has approved a device for treating RLS. Relaxis is the name of the vibrating pad placed under the legs while you're in bed. It is available only by prescription.
Lifestyle Changes
If your RLS isn't that severe, try making some simple changes to your routine. These lifestyle changes have been shown to not only reduce the symptoms of restless legs syndrome, but they're also good for your pregnancy in general:
- Avoid drinking coffee, soda, and other caffeinated beverages.
- Exercise every day, but stop within a couple of hours of bedtime so you don't get too wound up to sleep.
- Get into a regular sleep routine. Go to bed and wake up at the same time every day, if you can. Before bed, relax with a warm bath or by snuggling up in bed with a good book.
- Use a heating pad
Whenever you wake up with RLS, try these tips to make the gnawing feeling go away so you can get back to sleep:
- Massage your legs.
- Apply a warm or cold compress to your leg muscles.
- Get up and walk or stretch your legs.
Restless legs syndrome can resolve after giving birth. Within a few days after your baby is born it in many cases will disappear. That's good news, because new moms will soon have much more pressing things to attend to in the middle of the night.
Within a few days after your baby is born it in many cases will disappear. That's good news, because new moms will soon have much more pressing things to attend to in the middle of the night.
Restless legs syndrome
- Home
- Restless legs syndrome
Restless legs syndrome (RLS) is a neurological disease manifested by paresthesias in the lower extremities and their excessive motor activity, mainly at rest or during sleep.
Restless legs syndrome was first described by Thomas Willis in 1672: “In some people, when they are going to sleep and lie down in bed, immediately after this there is a movement of the tendons, arms and legs, accompanied by colic and such restlessness that the patient cannot sleep like he's under torture." The modern definition of this syndrome was proposed by the Swedish scientist K. Ekbom in 1945:
Restless legs syndrome can be primary (idiopathic) and secondary.
One of the most likely causes of the development of primary restless legs syndrome is considered to be the insufficiency of dopaminergic systems in the subcortical structures of the brain involved in inhibitory processes.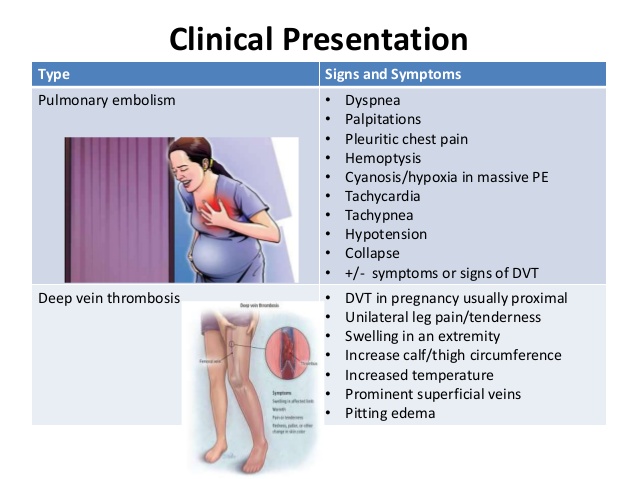
Secondary restless legs syndrome can develop during pregnancy and various pathological conditions.
The main causes of secondary restless leg syndrome are:
- Iron deficiency. Iron deficiency disrupts the production of dopamine in the brain, which in turn provokes the development of secondary RLS. A patient's iron stores may be depleted even without clinically significant anemia. Studies have shown that a decrease in iron stores, defined as a decrease in ferritin levels below 50 µg/L, can cause or exacerbate the symptoms of RLS.
- Neurological disorders. Secondary RLS is often observed in injuries of the spinal cord and peripheral nervous system, as well as peripheral neuropathies of various origins (diabetic, alcoholic, toxic). nine0004
- Pregnancy. RLS occurs in 15-20% of women during pregnancy. Symptoms can be quite severe, but usually disappear completely within a few weeks after delivery. Iron deficiency anemia, folic acid deficiency, hormonal changes, and venous congestion in the lower extremities are thought to be the causes of RLS during pregnancy.

- Uremia. Up to 50% of patients with ESRD have RLS. The frequency of RLS was shown to correlate with blood urea levels, anemia, peripheral neuropathy, and a decrease in parathyroid hormone levels in this category of patients. Especially severe symptoms are noted directly during dialysis, when the patient is forced to lie motionless for several hours. Reduction or disappearance of RLS symptoms has been shown after kidney transplantation. nine0004
- Use of medicines. Symptoms of RLS may develop or worsen with the use of various medications, such as tricyclic antidepressants (amitriptyline, azafen, etc.), selective serotonin reuptake inhibitors (trazodone, Prozac), lithium preparations, metoclopramide (raglan), calcium channel blockers (corinfar, finoptin). Caffeine also worsens the symptoms of RLS.
Clinical manifestations of RLS can be grouped into several main symptom complexes:
Discomfort in the legs. They are usually described as crawling, trembling, tingling, burning, twitching, electric shock, wiggling under the skin, etc. About 30% of patients characterize these sensations as pain. Sometimes patients cannot accurately describe the nature of the sensations, but they are always extremely unpleasant. These sensations are localized in the thighs, shins, feet and undulate every 5-30 seconds. There are significant fluctuations in the severity of these symptoms. In some patients, symptoms may occur only at the beginning of the night, in others - continuously disturb throughout the day. nine0009
About 30% of patients characterize these sensations as pain. Sometimes patients cannot accurately describe the nature of the sensations, but they are always extremely unpleasant. These sensations are localized in the thighs, shins, feet and undulate every 5-30 seconds. There are significant fluctuations in the severity of these symptoms. In some patients, symptoms may occur only at the beginning of the night, in others - continuously disturb throughout the day. nine0009
Symptoms worse at rest. The most characteristic and unusual manifestation of RLS is an increase in sensory or motor symptoms at rest. Patients usually report worsening while sitting or lying down and especially when falling asleep. Usually, before the onset of symptoms, it takes from several minutes to an hour when you are in a calm state.
Symptoms are relieved by movement. Symptoms are greatly relieved or disappear on movement. The best effect most often has a simple walk. In some cases, sipping, bending over, exercising on a stationary bike, or just standing up helps. nine0009
In some cases, sipping, bending over, exercising on a stationary bike, or just standing up helps. nine0009
Symptoms are circadian. Symptoms are significantly worse in the evening and in the first half of the night (between 6 pm and 4 am). Before dawn, the symptoms weaken and may disappear altogether in the first half of the day.
However, it should be noted that diagnostic difficulties can sometimes arise in the differential diagnosis of primary and secondary restless leg syndrome. Since there are no exact biochemical markers of primary RLS, it is not possible to say with certainty whether the above condition is the cause that caused secondary RLS, or whether it only provoked the clinical manifestations of primary RLS. nine0009
Valuable diagnostic information to confirm the presence of restless legs syndrome can be obtained by performing polysomnography, a method of long-term recording of various physiological parameters during sleep.
If you or your relatives want to fully relax while sleeping, we are waiting for you at the Department of Somnology of the Medical and Diagnostic Center of the International Institute of Biological Systems named after S. M. Berezina.
M. Berezina.
Treat yourself to a healthy sleep! nine0009
Working tips to help a pregnant woman get rid of nighttime restless legs syndrome
IN THIS ARTICLE:
Foot problems can be a problem throughout pregnancy. Initially, these are swelling, and in the second half of the term you may notice that the leg twitches at night. It's probably restless leg syndrome.
During pregnancy, this condition is often observed, but safely disappears after the birth of the baby. What the mentioned condition manifests itself in and how a pregnant woman can get rid of restless legs syndrome, read in the article. nine0009
What is restless leg syndrome during pregnancy?
Do you feel an uncontrollable urge to move your legs to relieve the crawling, tingling or burning sensation? It's probably restless leg syndrome (RLS).
You are not alone in suffering from this syndrome. A study of more than 600 pregnant women found that 16% of participants experienced RLS symptoms.
Usually, the symptoms of the syndrome appear when you are in a calm state, more often at the moment of falling asleep or when you are not moving for a long time - at work, at the cinema or on a long journey by car. Probably, with the syndrome, there will be a feeling that the legs are twitching during pregnancy. However, some pregnant women complain of strange sensations in their thighs, feet, arms, or hands. nine0009
Change the position of the limbs and there will be an immediate relief, but the symptoms described will return when you stop moving. The manifestations of the syndrome are very unpleasant and uncomfortable, especially at night. If RLS interferes for several nights in a row, you may feel tired.
But if restless legs syndrome develops during pregnancy, know that this condition is temporary. Often, the intensity of symptoms increases and reaches a peak at a period of 7-8 months, but decreases and completely ceases to disturb by the time of delivery or a month after. nine0009
nine0009
Causes of Restless Legs Syndrome
To understand how to get rid of Restless Legs Syndrome, you need to find out the cause of the phenomenon, which doctors are working on, but so far to no avail, although research continues. It has been established that the syndrome affects both pregnant women and men, children and non-pregnant women. The trend is in families. If a woman suffered from RLS before pregnancy, the problem will worsen during childbearing.
It is not known why women without RLS experience this condition during pregnancy. There are just so many theories. Iron deficiency, folate deficiency, hormonal changes (especially increased estrogen levels), and circulatory disorders are all possible culprits. nine0009
Tips on how to relieve the syndrome and improve sleep
If your leg twitches at night and prevents you from sleeping, try to avoid a number of things: Things to help get rid of nocturnal syndrome :  The safety of this substance for pregnant women has not been established. nine0004
The safety of this substance for pregnant women has not been established. nine0004