Placenta scab bleeding
Postpartum symptoms: when to call us - Oula
Go Back
As you enter your “4th trimester,” you may notice changes in your body as you heal. We’ll be checking in with you a week after your birth, and again a few weeks later. Though you will be busy caring for your new baby, we encourage you to check in with yourself and monitor how you are feeling physically and emotionally. We are here to help you navigate this phase and answer your questions and, in particular, please reach out to if you are experiencing any of the below warning signs.
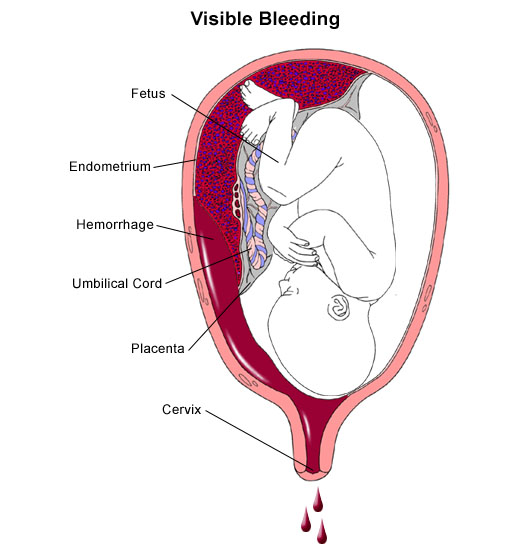
Postpartum bleeding
You can expect to have vaginal bleeding for about six weeks after the birth of your baby. The bleeding will taper from dark red to brown to yellow. In the first few days after the birth, you might notice that you pass some small blood clots. As you recover, you will notice that the bleeding might get heavier if you’ve had a busy day. This is normal. This bleeding is called “lochia. ” Lochia has an earthy smell.
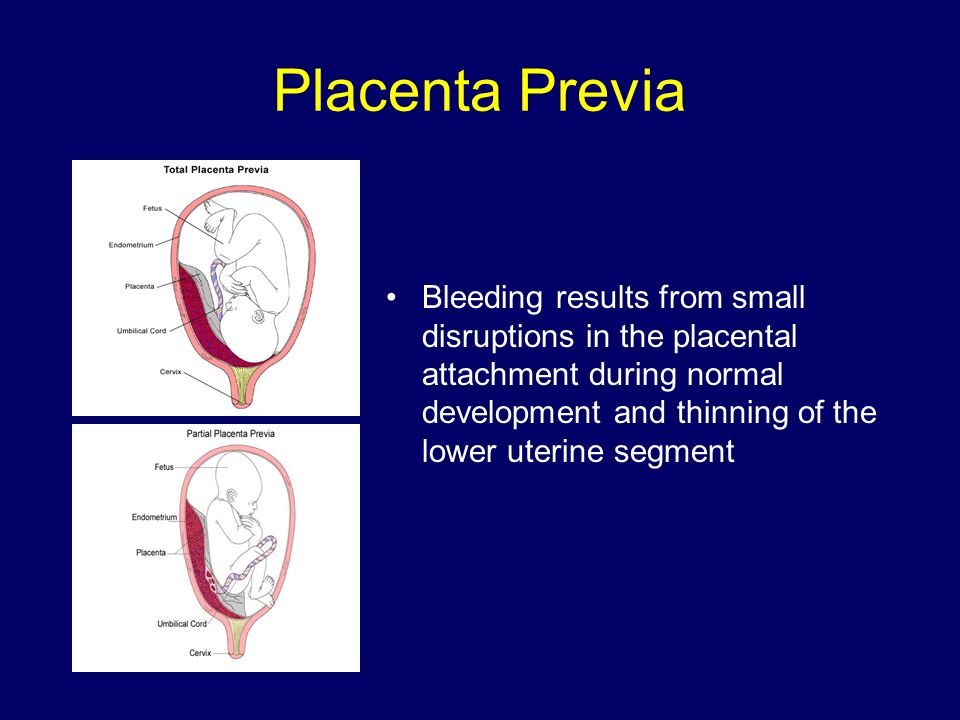
It is also normal to notice a return to bright red bleeding at about 7 to 10 days after the birth, this is called eschar. Eschar happens when the scab over the placental site breaks down – in much the same way that a scab on your knee might bleed if you disrupted it, the scab in your placenta can cause a day or two of red bleeding a week or two after the birth.
When to call us: If you notice that your bleeding is heavy, bright red, and soaking through more than two pads per hour, or if you are passing clots the size of a lemon or larger.
Fever or Infection
Fever can be a sign of infection. Other signs of uterine infection include severe abdominal pain or foul-smelling discharge.
When to call us: If you have a fever higher than 100.4F, or severe pain and foul-smelling discharge.
Cramping
Cramping in your uterus is normal after birth. You might notice that the cramping is more intense when you are breast/chest feeding, especially if this is not your first baby. You can take Tylenol or Ibuprofen to help with the cramping.
You can take Tylenol or Ibuprofen to help with the cramping.
When to call us: If you have pain that is severe or that does not respond to medication.
Symptoms of Postpartum Preeclampsia / Headache
As your hormones fluctuate postpartum, headaches can be common. The lack of sleep can contribute as well! Make sure you are well hydrated.
However, a headache (especially a headache that does not resolve with ibuprofen or tylenol) can be a symptom of preeclampsia. Other signs of preeclampsia include swelling (you might notice it in your hands, your feet, or your face), visual changes such as flashing lights or blank spots in your field of vision, nausea/vomiting, or pain on the upper right side of your abdomen.
When to call us: If you have a headache that does not respond to Ibuprofen or Tylenol or any other signs of postpartum preeclampsia.
Breast Changes
Your body will make milk regardless of whether you are breast/chest feeding. Your breasts are likely to become engorged (full of milk) three or four days after the birth. Engorgement can also cause you to have a low-grade fever (less than 100.4F).
Your breasts are likely to become engorged (full of milk) three or four days after the birth. Engorgement can also cause you to have a low-grade fever (less than 100.4F).
If you are breastfeeding, it is important to put the baby to the breast, or otherwise drain the breast (pump, hand-express) every 2-4 hours, round the clock. This will give your body signals to make milk in the right amount for your baby.
It is possible to develop plugged milk ducts, and plugged ducts can lead to infection, also known as mastitis. If you notice that you have any lumps in your breast, you need to get that milk moving – stand in the shower and let the warm water run on the breast while you massage the lump. You can also try feeding the baby in alternative positions like the football hold or dangle feeds. Some women who are prone to plugged ducts also benefit from soy lecithin supplements (take one 1200 mg capsule 3-4 times per day, reduce dosage by one capsule per day when the blockage has resolved for one week).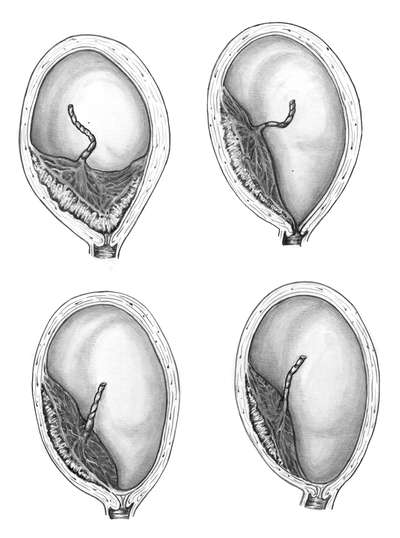
If you have hard, painful areas in the breast that look red & feel warm to the touch, you may be developing mastitis. It is important to stay very well hydrated, take Ibuprofen for its anti-inflammatory properties, and drain the breast completely.
When to call us: If you develop symptoms of mastitis along with fever over 100.4F and malaise (you feel unwell), as you may need antibiotics.
Blood Clots
If you notice that you have one leg that is more swollen than the other, especially if the affected leg is dusky or grey/purple colored, or if you have pain in your calf or the back of your thigh, you might have developed a blood clot.
Go to the emergency room: If you have these symptoms and are also experiencing shortness of breath.
Mood Changes
Mood changes are very common in the first few weeks postpartum. About 85% of women experience the “baby blues” after birth. You might notice that you are laughing one moment and crying the next.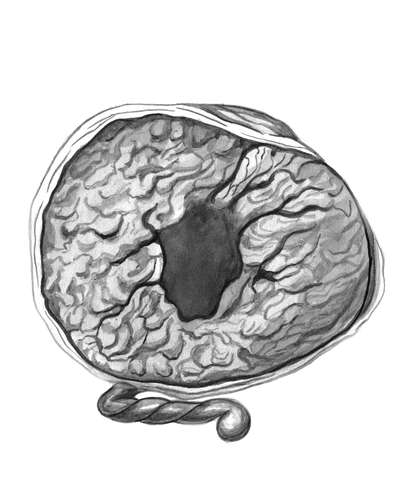 These mood swings are caused by hormone changes combined with the sleep deprivation and role changes that you experience as the parent of a newborn. Your mood should feel more stable by the time the baby is one month old.
These mood swings are caused by hormone changes combined with the sleep deprivation and role changes that you experience as the parent of a newborn. Your mood should feel more stable by the time the baby is one month old.
Postpartum depression and anxiety are less common than the baby blues, but can cause mood changes up to a year after your birth. Please don’t discount mood changes that are causing issues for you, these issues are real and treatable.
When to call us: if you’d like to discuss what you’re feeling or if you’d like a referral to mental health therapist that specializes in postpartum. But if you have any thoughts of doing harm to yourself or the baby, you need emergency attention.
Wounds that aren’t healing
If you have an abdominal incision or perineal wound, you will need to keep those areas clean & dry as they heal. Let soapy water run over them in the shower and pat to dry. Be sure to expose the incision to good air-flow (don’t keep it covered all day).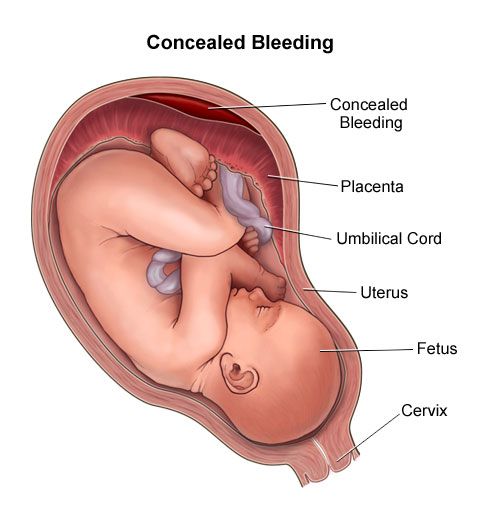
Our c-section patients will come to the office two weeks after the birth so we can look at your incision and remove any remaining dressings.
If you have a perineal or vaginal laceration, the stitches will dissolve and do not need to be removed. You might notice pieces of the stitch material on your toilet paper about a week after the birth. Use the peri-bottle to spray the area to clean it and pat dry with toilet paper. You can keep ice on the area for the first 24 hours, and do warm sitz baths (shallow baths that dunk your perineum in warm water) 2-3 times per day until the area feels better. Sitz baths provide cleaning and improved circulation to this delicate area. They are soothing and therapeutic — don’t skip them! You can add healing herbs or epsom salts to the water in the sitz bath, but even plain warm water has the desired effect.
When to call us: If you notice that the incision is bleeding, opening, leaking pus, if areas of redness on the edges are getting larger, or if you are not able to manage your pain with the medications you were given.
Healing your placenta scab self care to Keep You Alive
Here are some handy postpartum recovery tips from a L&D nurse. Your uterus is now healing from a “placenta scab” left from the baby making their exit. This post includes info on pads, pain medicine, and the timeline you’ll likely follow.
Having a baby is hard work! Sometimes you don’t think about all that your body is going through (or WILL go through AFTER you go through labor). I know I was guilty of thinking I’d be 100% back to normal when I got out of the hospital. Wow, was I in for a surprise!
First off, hello! I’m Hilary — many people know me as The Pregnancy Nurse 👩⚕️. I have been a nurse since 1997 and I have 20 years of OB nursing experience. I am also the curly head behind this website Pulling Curls and The Online Prenatal Class for Couples. 🩺 I have had 3 babies of my own, I have seen THOUSANDS of moms deliver, and taught them what to watch for when bleeding is problematic. Grab my hospital packing list here:
Grab my hospital packing list here:
Table of contents
- Placenta Scab
- Get the Best Postpartum Pads
- Postpartum Pain Management
- Postpartum Blood Clots
- Postpartum recovery timeline
- Postpartum Swelling
- Postpartum Depression
If you’re looking to learn more about your postpartum recovery, I love this class for it. Instead of glazing over it like many prenatal classes, that one really teaches you what to expect!
This is a topic I am so passionate about I actually just did a podcast on it. I think it will help you know even more what to expect!
And, I must admit that taking care of your bottom after baby was a BIG eye-opener to me (and lots of ladies) — so I did a full video on it:
Ok, let’s dive in:
Your Placenta Scab
I know, super gross right.
But I think a lot of time women wonder why they need to to go slow those first few weeks after having their baby.
Yes, your bottom has had a big change, but you also need to realize what your uterus has gone through as well!
When the baby exits, within a few minutes the placenta comes off. That leaves a big wound on your uterus where the placenta site was.
It slowly applies “direct pressure” (think back to first aid class) by cramping back down to its normal size. The uterus contracts and causes this.
It helps to visualize that if you got a cut on your hand, if you made a fist, it would help put pressure on that area and stop the bleeding.
So, when your uterus cramps down (or goes back to a “fist”) it helps that area not bleed out. If for some reason, your uterus stop cramping down and becomes loose (or, boggy – -that’s what we call it) it can be a real problem.
After you have your baby, the nurse will push on your uterus to make sure that it cramping back down, to prevent a postpartum hemorrhage (which can be REALLY bad).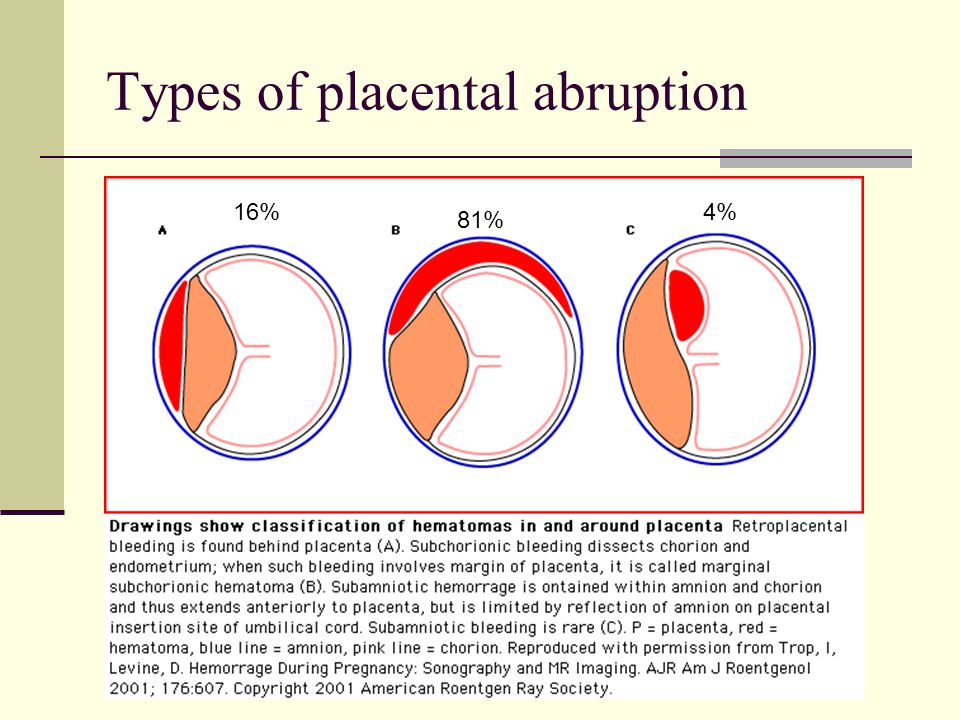 It is a good idea to just breathe when they do it — and yes, I do talk a LOT about this here.
It is a good idea to just breathe when they do it — and yes, I do talk a LOT about this here.
Keep in mind the uterus has a TON of blood flow right after delivery, because it was just growing a human. Your body needs to slow that down as well as stop the bleeding from the scab. Every delivery is very similar to major surgery (even though you won’t have scars on the outside).
This is all just the normal process of the placental site scab (but not fun). But if there’s ever a question about your bleeding, be sure to seek medical help.
Placental Scab FAQ’s
How long does Placenta Scab Bleeding Last?
It varies for each person. And it lengthens with each pregnancy. Most new moms stop around 3 weeks postpartum but some go shorter and many bleed up into their 5th week. Most people stop by 6 weeks.
It is often like a very heavy period once you go home from the hospital, and then tapers from there.
With each baby, women likely bleed more and longer.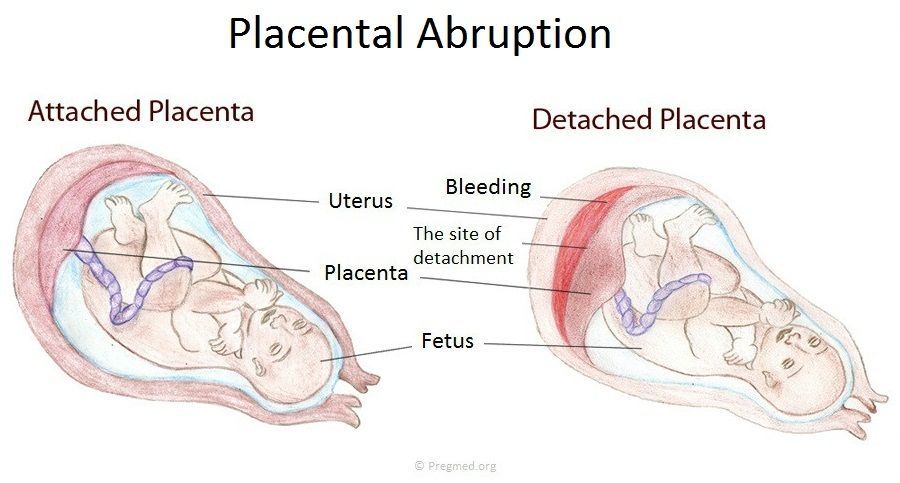 Your uterus is just getting more tired and doesn’t cramp down as well. It is not unusual to have more prolonged heavy bleeding when you’ve had several babies.
Your uterus is just getting more tired and doesn’t cramp down as well. It is not unusual to have more prolonged heavy bleeding when you’ve had several babies.
Why is there a scab?
It is from where your placenta attached to your uterus so that your body could feed your baby as it grew.
What is retained placenta?
If a part of the placenta stays attached, it’s called retained placenta. It can cause increased bleeding and possibly even infection.
When you deliver, your healthcare provider will check your placenta to make sure that it is intact. If there is a question, they may go into your uterus to check (using their hand). And if they think there is retained placenta, you may go to the OR to get it removed.
Do you recommend making pills out of your placenta
I do not — I have a post on placentophagy which shares why I don’t recommend it.
Will I still bleed with a cesarean section?
Yes, as the placental scab is still there, you will still bleed, just like a vaginal birth (most of the bleeding with a vaginal birth is from the placenta, not the birth canal).
Wait, what is the placenta?
It is the tissue that grows next to your uterus to give your baby nutrients and take away waste through the umbilical cord.
How much is excessive bleeding?
Your nurse will assess your bleeding in the hospital and you should get a good idea of what’s normal for you (because it REALLY varies). When you go home, if that increases, you need to call your provider.
What about a sudden gush of blood?
Again, you’re doing too much. Unless it’s enough to soak through your pads and panties I’d clean up, put a new pad on, rest with my feet up and see if it keeps happening — or, contact your provider with any questions.
Also, take note of the type of blood. If it’s brown, that’s older blood (not as worry-some). If it’s a sudden gush of bright red blood, that’s more problematic.
What is the problem if I’m bleeding too much?
Most often it’s because you are doing too much (and not allowing your uterus to cramp back down). However, sometimes pieces of the placenta can be left behind (even if your provider looks to make sure it’s intact). That requires medical treatment.
Am I going to bleed like this forever?
That first week can be a doozy, but it should get a little better — bit by bit. It can seem like a long time though.
In my first prenatal class I took, they acted like it would all be unicorns and rainbows after the baby came home. When I created my own class I knew I wanted it to be different. I wanted to let you know exactly what to expect.
Postpartum Recovery
Feeling overwhelmed — grab my postpartum recovery checklist:
Get the Best Postpartum Pads
Your uterus has a giant placenta-sized scab.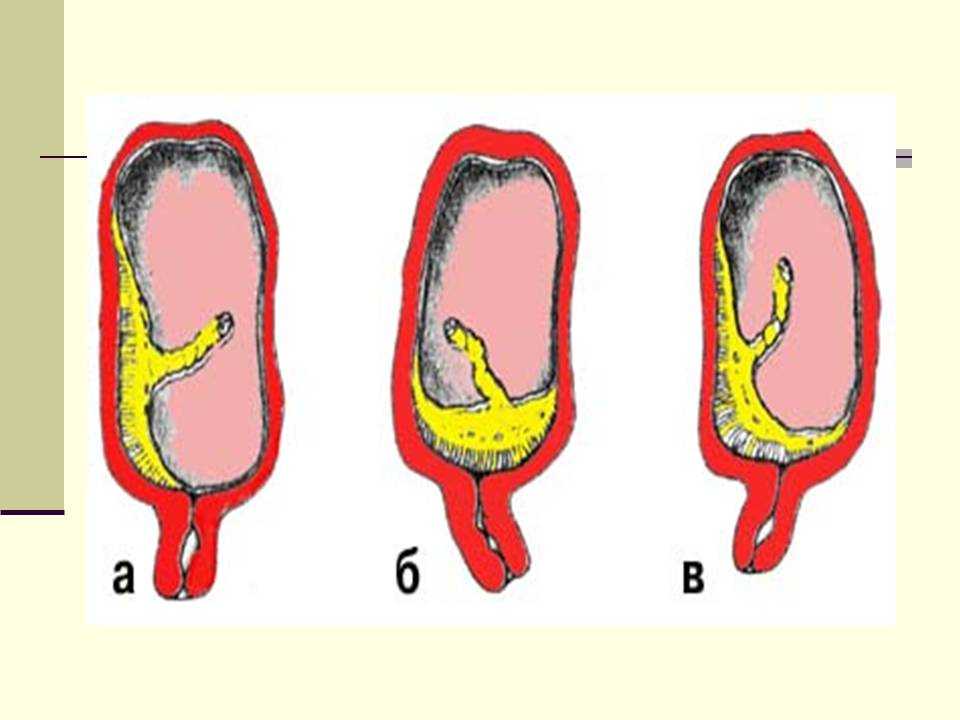 Your placenta peels off after your baby is born and you are left with a big wound inside you that has to heal. That means you can’t move your household the week after you have a baby {guilty!}.
Your placenta peels off after your baby is born and you are left with a big wound inside you that has to heal. That means you can’t move your household the week after you have a baby {guilty!}.
If your bleeding starts back to bright red or increases you need to SLOW DOWN.
Let me say it again (because I get a LOT of emails about it)…
If your bleeding picks back up after it has slowed down — you NEED TO SLOW DOWN. It is mother nature’s tip that you’re doing too much!
Your uterus will thank you for it! BTW, it’s smart to have some GOOD sanitary pads at home, so you don’t have to worry about leakage — something like these are nice (it seems like overkill, but it’s not), and I’ve also heard of people really liking these.
Postpartum Pain Management
For cramping pain — most people take ibuprofen. Ibuprofen needs to be taken with a meal. I was guilty of popping ibuprofen like it was candy on #3. Those after-birth cramps weren’t pretty. I would have taken an epidural with some of them if they had offered it. I ended-up ripping up my stomach lining and it hasn’t been the same since. {sad face}. Ibuprofen is GREAT for cramps — just take it with food {and, FYI — with each baby the cramps get worse, hooray!}
I would have taken an epidural with some of them if they had offered it. I ended-up ripping up my stomach lining and it hasn’t been the same since. {sad face}. Ibuprofen is GREAT for cramps — just take it with food {and, FYI — with each baby the cramps get worse, hooray!}
In my postpartum comforts I go over some of the things to keep you comfortable — but I hear SO many good things about this stuff — I’d definitely check it out!
Some doctors will also provide you a prescription medication that you might take for further pain. Please remember that you shouldn’t drive when you’re on prescription pain killers.
This just in: I just did a Tushy Review. Cliffnotes: It’s amazing. Check it out! {save 10% with code CURLS too!} It sprays water on your bum. It’s not hard to install and I may have had a love affair with it postpartum if I’d had it back then!
Postpartum Blood Clots
You shouldn’t be passing clots larger then a golf ball. If you are, you need to call your doctor.
If you are, you need to call your doctor.
Be sure that you have a BIG pad for when you get home. I recommend these for the first few days home, and this pack for after that. I’ve also heard a lot of people loving these undies.
A word on the…
Postpartum recovery timeline
In general you should be bleeding less and less each day. If you notice a lot more bleeding suddenly, that’s mother nature’s sign that you’re working too hard. Even if you think you’re not — do less. Your body needs that!
Every person’s timeline will be different… just know it should be a little better each day….
Pro Tip: Bright red bleeding is new blood and darker brown’ish blood is older.
What to do if your bleeding is slowing down and suddenly is more?
This is a sign that you’re doing too much.
You might not FEEL like you’re doing a lot — but that really is what it is.
Do less, drink more water. Put your feet up more. Less walking and less carrying things (besides the baby).
Postpartum Swelling
Likely, after the hospital you’ll be swollen. BUT, in your postpartum recovery you will pee. A lot. You will sweat, a lot. Your blood volume increase like CRAZY when you are pregnant — your blood’s just going back to normal. Free weight loss, enjoy!
Postpartum Depression – how to know?
If you have been more crying then happy and you’re on day 3 of that — you need to call someone. It’s not a perfect rule of thumb — but it’s a good start. It really helps you know the difference between baby blues (which are totally normal) and when it’s a problem. Emotional swings are totally normal, but living on one end of that swing set isn’t good for you. There are a lot of ways to get help, and talking to someone about it is the first start. If your OB is worth their paycheck, they should be concerned about you and want to know.
I love this podcast I did on postpartum mental health with a social worker.
Whatever you do. Be kind to yourself. There’s just a lot going on with your body. Rest, love, and give yourself time to adjust to the change. Make sure family members are checking on you (and not just the baby).
There’s just a lot going on with your body. Rest, love, and give yourself time to adjust to the change. Make sure family members are checking on you (and not just the baby).
Postpartum Discharge
It’s normal for the bleeding to taper (like we’ve talked about previously), and then maybe just have some different vaginal discharge for a bit as your uterus fully heals. If it smells (a foul odor) or looks foul, call your provider.
Related Post: Postpartum Comforts & What to do before baby
Ok, if you are still pregnant, NOW is the time to get prepared for all this kind of stuff with a high quality prenatal class. After 20 years in the delivery room I know SO many families just can’t fit it in — which is why I created the solution just for you.
- Use Hilary’s 20 years at the bedside to help you know what you NEED to know.
- Can be done in just 3 hours.
- 3 price points to fit all the budgets.
If you’re not quite sure you’re ready for the full class, check out my free birth toolkit — you can sign up right here:
Diathermoelectrocoagulation (DEC) of the cervix in Kirzhach, make an appointment with a gynecologist
Our license
Our Doctors
Prices
Diathermoelectrocoagulation is a method for the treatment of diseases of the cervix , based on the use of high frequency current, which destroys pathologically affected tissues without harming healthy tissues.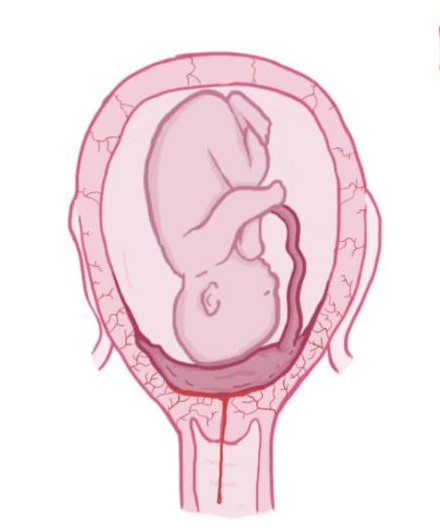 At the same time, the current coagulates the vessels, which helps prevent or stop bleeding during surgery. After 1.5-2 months, a completely new tissue is formed at the site of the electric shock. A very important factor is the appointment of this kind of operation only after the completion of the menstrual cycle.
At the same time, the current coagulates the vessels, which helps prevent or stop bleeding during surgery. After 1.5-2 months, a completely new tissue is formed at the site of the electric shock. A very important factor is the appointment of this kind of operation only after the completion of the menstrual cycle.
When is diathermocoagulation (DEC) used?
Indications for this procedure are :
- Mild or moderate dysplasia
- DEC cervical erosion
- Ectopia (no gross changes)
- Condylomas of the cervix and vagina
- Endometriosis of the cervix.
Contraindications for diathermocoagulation (DEC)
Before performing diathermocoagulation, the doctor must make sure that there are no contraindications for this woman. This method cannot be used in the following situations:
- In inflammatory processes of the female genital organs (colpitis, cervicitis, acute salpingo-oophoritis and endometritis).
 Before the procedure, an infectious pathology must be treated and control tests for its presence must be passed.
Before the procedure, an infectious pathology must be treated and control tests for its presence must be passed. - For cervical cancer. The use of this method in this case can cause the progression of the process and a significant deterioration in the condition.
- During pregnancy. This is fraught with abortion.
- In the early postpartum period.
DEC cervical erosion
One of the most common reasons for this procedure is cervical erosion. By itself, the disease may not manifest itself. Unless during sexual intercourse there may be minor bleeding. But you should know that this disease is very dangerous and can lead to cancer. If, while viewing, the gynecologist of the medical center "Health", Kirzhach noticed any changes, he is obliged to carry out the procedure of colposcopy and biopsy.
Read more about cervical erosion here.
How to prepare for diathermocoagulation (DEC)?
To prescribe a procedure for the treatment of pathologies of the cervix (erosions, dysplasia), it is necessary to undergo an examination, identify the nature of ectopia, the causes of its occurrence.
It is advisable to undergo the following examinations:
- Bacteriological examination - smear on the flora to identify the inflammatory process, infections;
- Cytological examination - the study of structural features of the cells of the cervix;
- Biopsy - to determine the nature of the pathology;
- Blood for RW, HIV, hepatitis B and -C;
- Colposcopy - to determine the nature and extent of damage to the cervix.
How is diathermocoagulation (DEC) performed?
Before manipulation, all inflammatory diseases of the cervix and vagina are cured, achieving 1-2 degrees of purity. The procedure is prescribed for a time after the end of menstruation, this is very important. At the same time, before the procedure, the patient must refrain from sexual intercourse. The operation is performed under local anesthesia. After the anesthesia begins to act, the doctor gently cauterizes the desired area.
Within a month after the intervention, the patient is advised to have sexual rest, it is forbidden to lift weights, visit pools, baths, swim in open water, take hot baths, use vaginal tampons.
Possible complications after diathermocoagulation (DEC)
Since the invention of the method, it has been indicated that it causes a large number of complications. These adverse effects are well studied:
- One of the frequent complications is bleeding. It can occur immediately during the procedure or when the resulting scab is rejected. Sometimes severe bleeding requires surgery.
- Diathermocoagulation can lead to narrowing and even fusion of the cervical canal.
- Often after it, hematomas and vascular dilations (telangiectasias) appear.
- One of the most serious complications of manipulation is endometriosis, which occurs due to the deposition of endometrial cells on the wound surface. These cells are deposited on the surface of the cervix during menstrual bleeding.
- As a result of a change in the shape of the cervix, infertility is likely.
- Diathermocoagulation leads to the development of isthmic-cervical insufficiency, which increases the likelihood of miscarriage.
 Premature birth or violation of the disclosure of the cervix during childbirth is not excluded.
Premature birth or violation of the disclosure of the cervix during childbirth is not excluded.
In general, the incidence of pregnancy complications in patients after this procedure reaches 80%. Diathermocoagulation should not be used to treat young women planning pregnancy and childbirth. In women of mature age, cauterization of erosion by current is used to treat cervical intraepithelial neoplasia, that is, precancerous conditions.
Where to do diathermocoagulation (DEC) in the city of Kirzhach?
To find out the cost of diathermocoagulation (DEC), make an appointment with a doctor and for a procedure at Medical Center "Health", Kirzhach, please call: 8 (49237) 2-95-56, 8 (915) 776-29- 66.
Reviews of doctors of the Health Medical Center are available at the link.
404 Page not found
Size:
AAA
Images On Off
Regular version of the site
Unfortunately, the requested page was not found.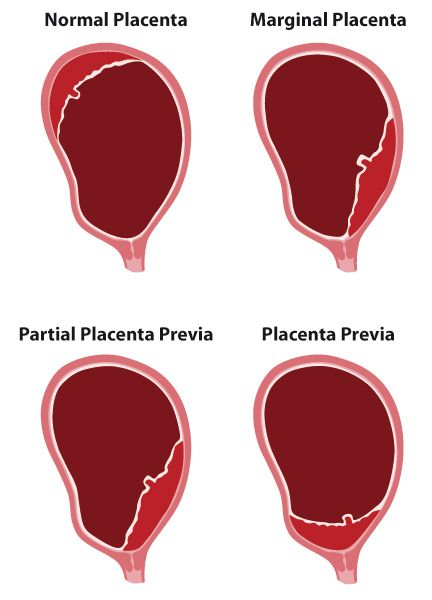
But you can use the search or the sitemap below
|