Placenta previa birth
Placenta previa | March of Dimes
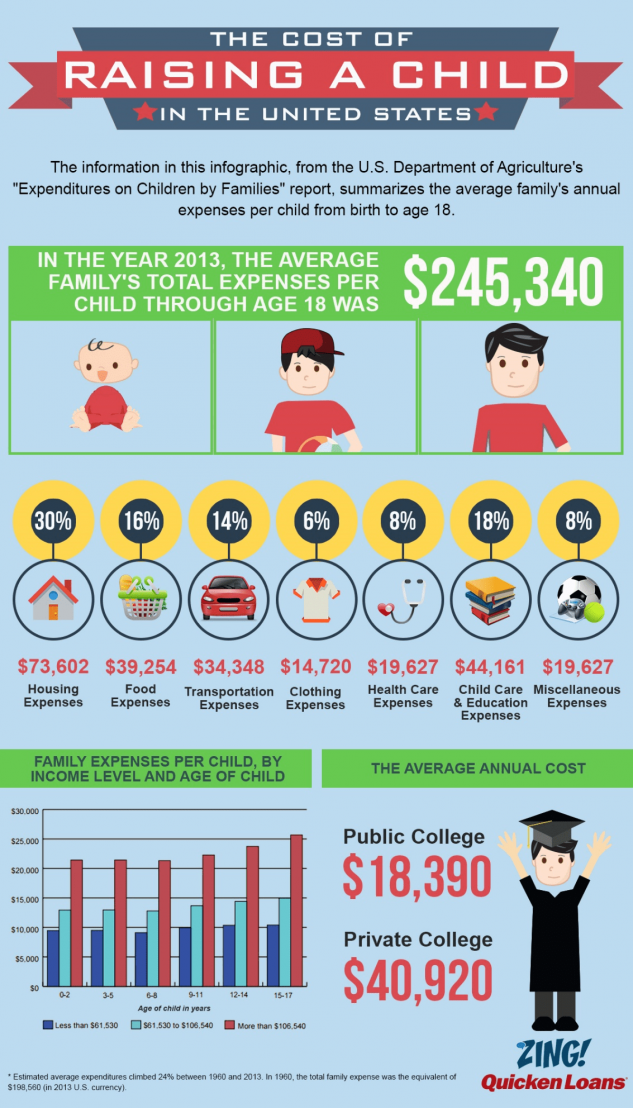
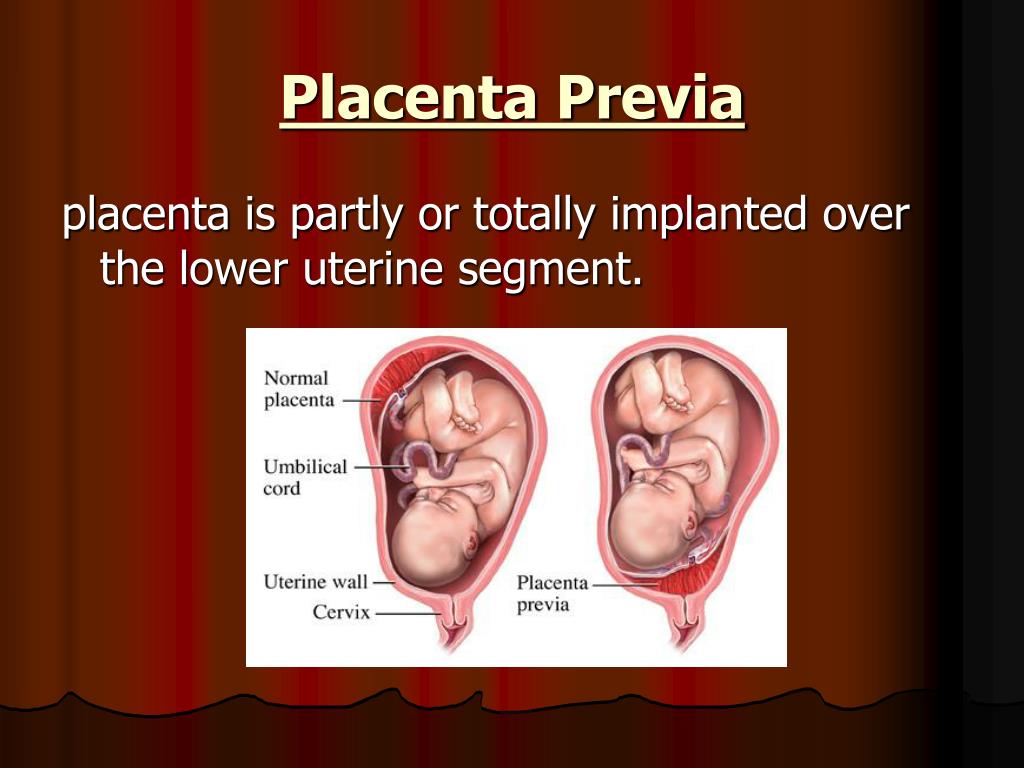
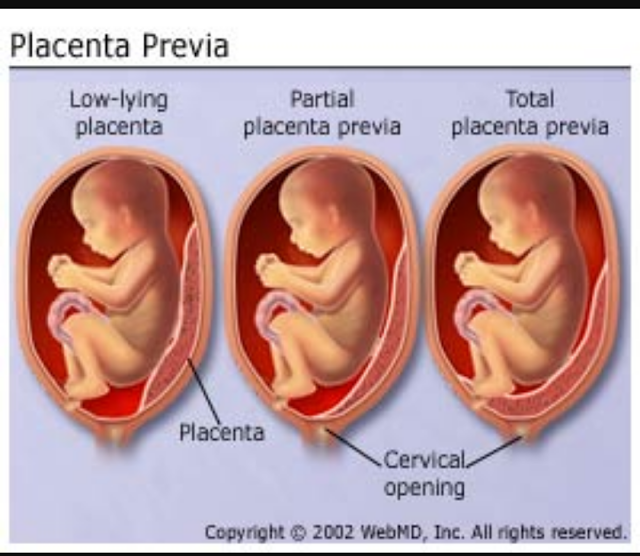
Placenta previa happens when the placenta lies low in the uterus and covers all or part of the opening to the vagina.
If you develop the condition early in your pregnancy, it usually isn’t a problem since the placenta grows upward with the uterus during pregnancy.
If you develop the condition later in pregnancy and the birth canal is blocked it can cause serious bleeding and may prevent vaginal delivery.
Talk with your providers about ways to deal with placenta previa, which could include having a planned c-section (caesarean birth).
The placenta attaches to the wall of the womb (uterus) and supplies the baby with food and oxygen through the umbilical cord.
Placenta previa is a condition in which the placenta lies very low in the uterus and covers all or part of the opening to the cervical opening that sits at the top of the vagina.
Placenta previa happens in about 1 in 200 pregnancies. If you have placenta previa early in pregnancy, it usually isn’t a problem because it may resolve as the pregnancy grows. However, if it persists it can cause serious bleeding and other complications later in pregnancy.
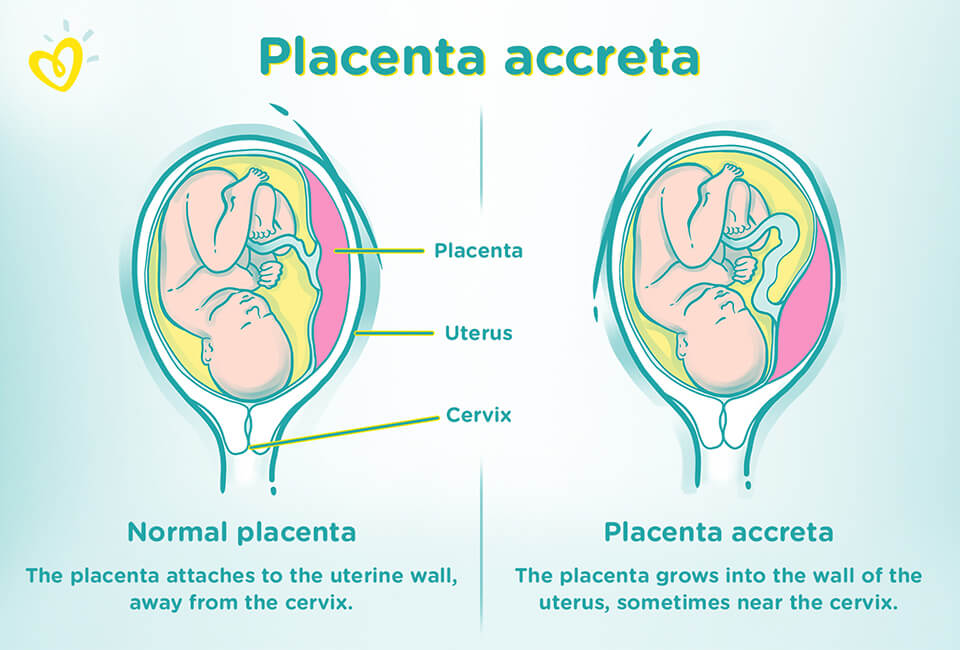
Normally, the placenta grows into the upper part of the uterus wall, away from the cervix. It stays there until your baby is born. During the last stage of labor, after the baby is born the placenta separates from the wall, and your contractions help push it into the birth canal (vagina). This is also called the afterbirth.
During labor, your baby passes through the cervix into the birth canal. If you have placenta previa, when the cervix begins to thin out (efface) and open up (dilate), blood vessels connecting the placenta to the uterus may tear. This can cause severe bleeding during labor and birth, putting you and your baby in danger.
If a placenta previa is identified by ultrasound and appears to block the cervix, no vaginal exams are performed and an elective c-section is planned.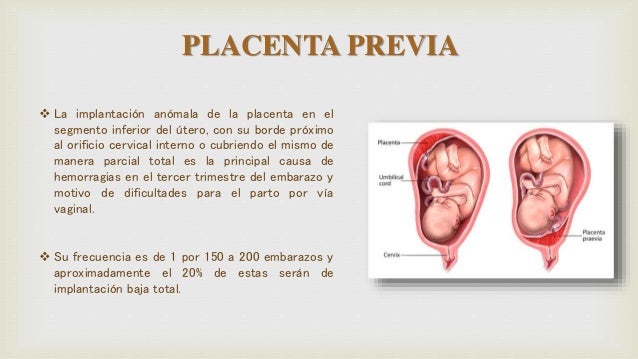
What causes placenta previa?
No one knows what causes placenta previa. However, you may be at higher risk for placenta previa if you:
- Have had a c-section in the past.
- Have had in vitro fertilization for infertility.
- Smoke cigarettes.
- Use cocaine.
- Are 35 or older.
- Have been pregnant before.
- Are pregnant with twins, triplets or more.
- Have had placenta previa in an earlier pregnancy.
- Have had surgery on your internal reproductive organs, such as myomectomy or tissue removal from the lining of your uterus (this is also called dilation and curettage or D&C). Some people have a D&C after miscarriage.
If you’ve had placenta previa before, what are your chances of having it again?
If you’ve had placenta previa in a past pregnancy, you have a 2 to 3 in 100 (2 to 3 percent) chance of having it again.
What are the symptoms of placenta previa?
Most of the time, placenta previa has no symptoms; it is often found during a routine ultrasound test.
For those who do have symptoms, the most common is painless bleeding from the vagina during the second half of pregnancy. You also may have contractions. Call your health care provider right away if you have vaginal bleeding anytime during your pregnancy. If the bleeding is severe, go to the hospital.
Not everyone who has placenta previa has vaginal bleeding. In fact, about one-third of people with placenta previa don’t have this symptom.
How is placenta previa diagnosed?
A prenatal test that uses sound waves to show a picture of your baby in the womb (ultrasound) usually can find placenta previa and determine the placenta’s location. In some cases, your provider may do an ultrasound through the birth canal (transvaginal ultrasound) or a translabial ultrasound instead. In places where it’s available, three-dimensional ultrasound may be used.
Even if you don’t have vaginal bleeding, a routine, second trimester ultrasound may show that you have placenta previa.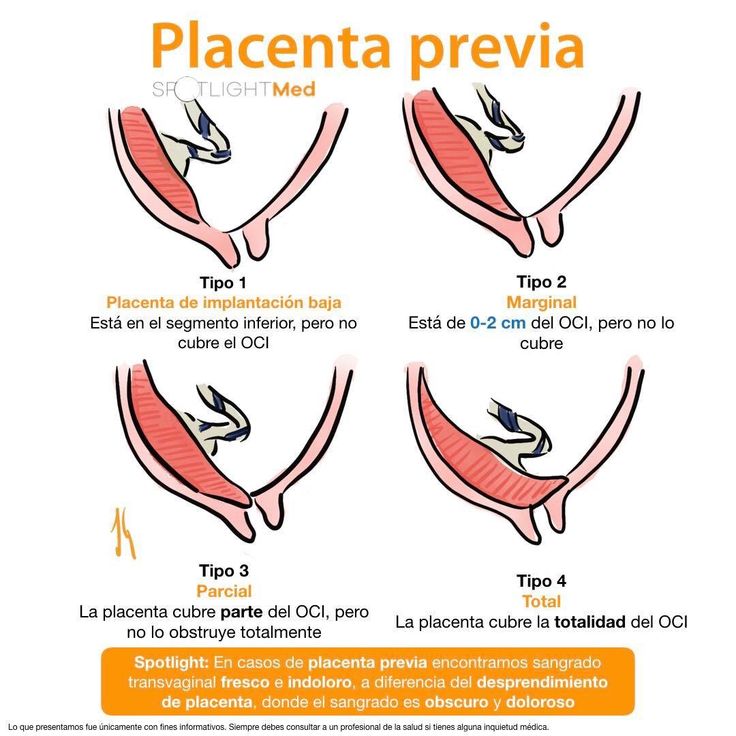 Don’t be too worried if this happens. Placenta previa found in the second trimester requires repeat follow-up ultrasounds to assure that the cervix is no longer blocked. If the placenta is no longer covering the cervical opening, you can usually have a vaginal delivery.
Don’t be too worried if this happens. Placenta previa found in the second trimester requires repeat follow-up ultrasounds to assure that the cervix is no longer blocked. If the placenta is no longer covering the cervical opening, you can usually have a vaginal delivery.
How is placenta previa treated?
Treatment depends on how far along you are in your pregnancy, the seriousness of your bleeding and the health of you and your baby. The goal is to keep you pregnant as long as possible. Your provider may recommend no vaginal exams or sex to prevent damage to the placenta and bleeding. Providers recommend c-section for nearly everyone with placenta previa to prevent severe bleeding.
If you are early in your pregnancy and have no symptoms, your provider will probably recommend no treatment, but will schedule follow-up ultrasounds to make sure everything is normal.
If you are bleeding as a result of placenta previa, you need to be closely monitored in the hospital.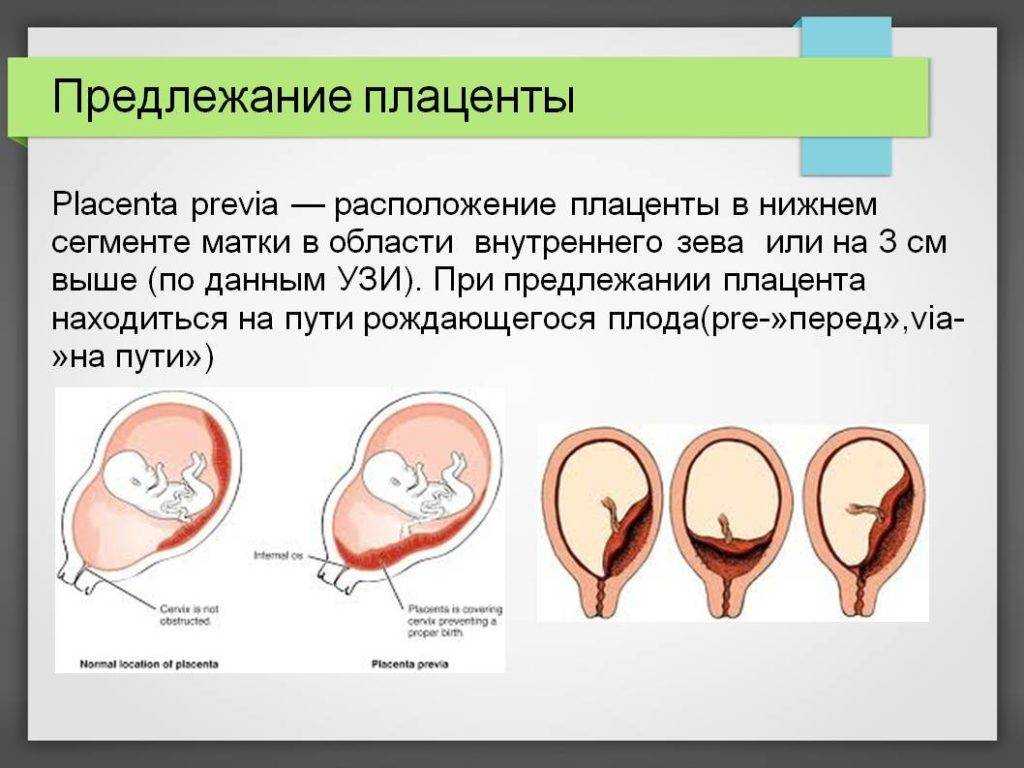 If tests show that you and your baby are doing well, your provider may give you treatment to try to keep you pregnant for as long as possible.
If tests show that you and your baby are doing well, your provider may give you treatment to try to keep you pregnant for as long as possible.
If you have a lot of bleeding, you may be treated by having new blood put into your body (blood transfusions). Your provider also may give you medicines called corticosteroids to help speed up development of your baby’s lungs and other organs in case a preterm delivery is needed.
Your provider may want you to stay in the hospital until you give birth. If the bleeding stops, you may be able to go home. If you have severe bleeding due to placenta previa at about 34 to 36 weeks of pregnancy, your provider may recommend an immediate c-section.
At 36 to 37 weeks, your provider may suggest an amniocentesis to test the amniotic fluid around your baby to see if the lungs are fully developed. If they are, your provider may recommend an immediate c-section to avoid risks of future bleeding. Nowadays, providers may use corticosteroids to help the baby lung development while you are pregnant and to help avoid an immediate c-section.
At any stage of pregnancy, an emergency c-section may be necessary if you have dangerously heavy bleeding or if you and your baby are having problems.
Is there anything you should avoid if you have placenta previa?
If you have placenta previa that doesn’t require immediate treatment right away, your provider may recommend that you avoid doing the following:
- Having sex that leads to orgasm
- Vaginal penetration or vaginal examinations
- Moderate and strenuous exercise
- Lifting more than 20 pounds
- Standing for more than four hours
All of these activities could lead to contractions that could lead to bleeding.
How can you reduce your risk for complications if you have placenta previa?
Have an ultrasound in the second trimester to identify location of the placenta. You may need follow up ultrasounds to help plan for a safe birth and delivery.
Follow your providers precaution instructions to prevent bleeding or complications.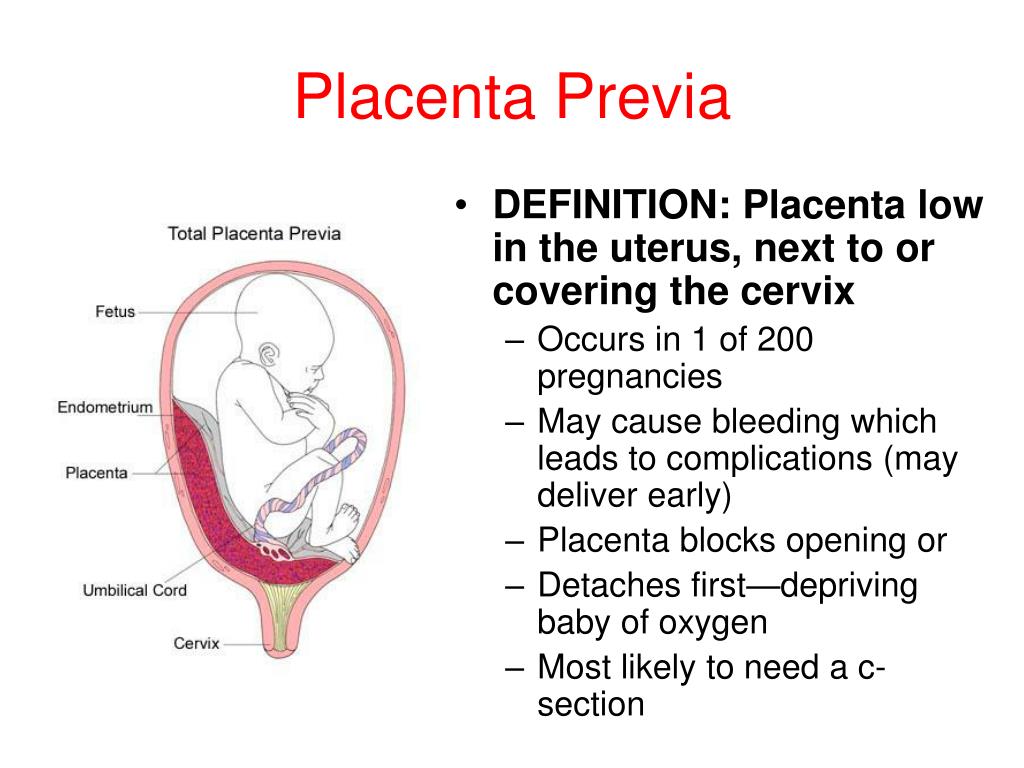 Contact your provider and go to the hospital if you have bleeding at any time during your pregnancy.
Contact your provider and go to the hospital if you have bleeding at any time during your pregnancy.
We don’t know how to prevent placenta previa, but you may be able to reduce your risk by not smoking and not using cocaine.
You also may be able to lower your chances of having placenta previa in future pregnancies by having a c-section only if it’s medically necessary. If your pregnancy is healthy and there are no medical reasons for you to have a c-section, it’s best to let labor begin on its own.
Last reviewed: January, 2022
Placenta Previa: Symptoms, Causes & Treatments
Overview
With placenta previa, the placenta covers all or part of the cervix.What is placenta previa?
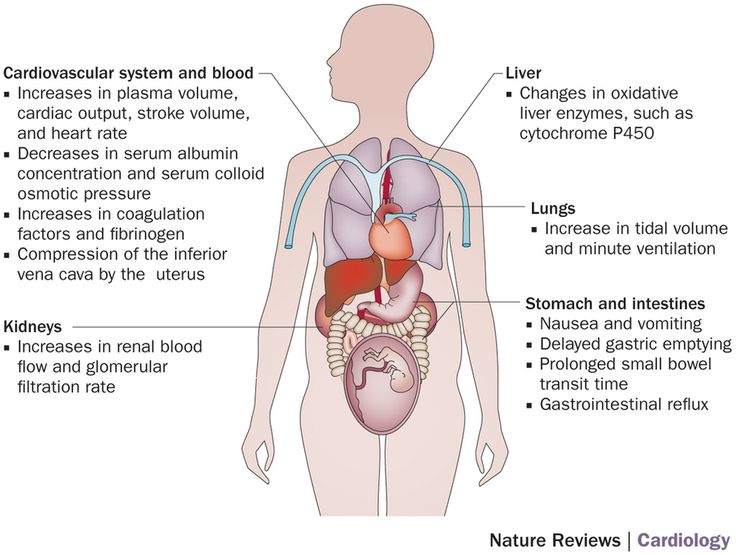
Placenta previa is a condition when the placenta blocks all or part of your cervix in the last months of pregnancy. The placenta develops in your uterus during pregnancy. It’s a sac-like organ that supplies oxygen and nutrients to the fetus through the umbilical cord.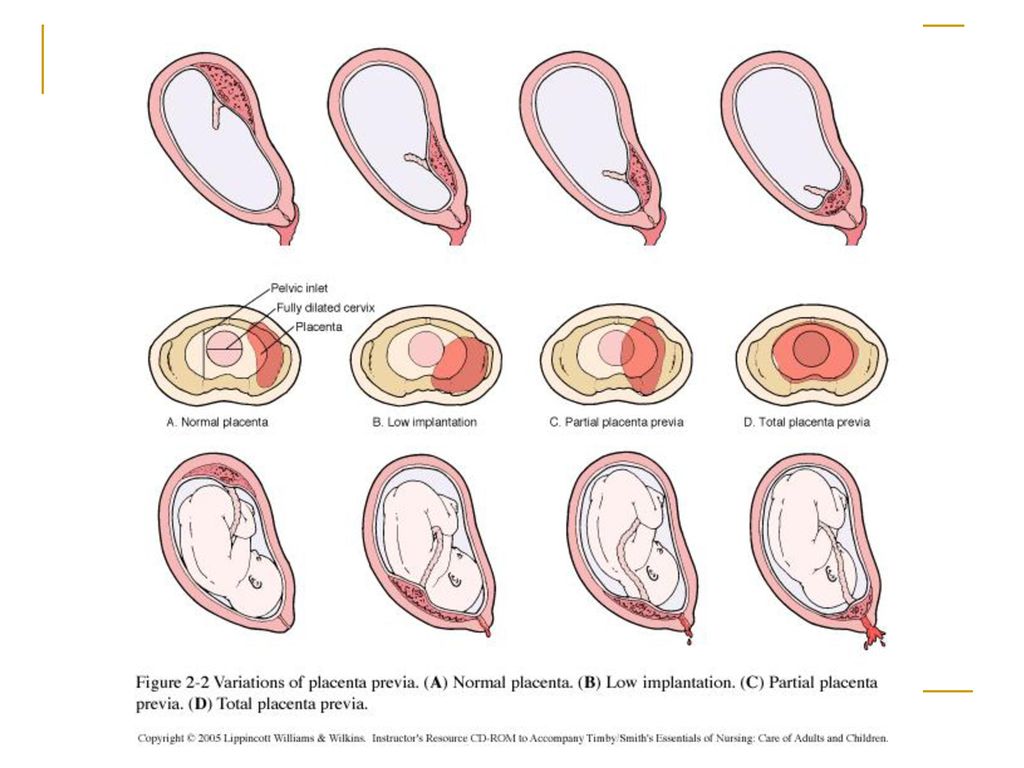
The placenta stretches and grows through pregnancy. It’s common for it to be low in your uterus in early pregnancy. In the third trimester (weeks 28 to 40 of pregnancy), the placenta should move to the top of your uterus. This happens so your baby has a clear path to the vagina for delivery. Placenta previa occurs when the placenta doesn’t move to the top of your uterus. This means the placenta is blocking your baby’s exit from your vagina.
What are the types of placenta previa?
There are several types of placenta previa:
- Marginal placenta previa: The placenta is positioned at the edge of your cervix. It’s touching your cervix, but not covering it. This type of placenta previa is more likely to resolve on its own before your baby’s due date.
- Partial placenta previa: The placenta partially covers your cervix.
- Complete or total placenta previa: The placenta is completely covering your cervix, blocking your vagina.
 This type of placenta previa is less likely to correct itself.
This type of placenta previa is less likely to correct itself.
Each type of placenta previa can cause vaginal bleeding during pregnancy and labor. Due to the high risk of bleeding, most people will require a Caesarean (C-section) delivery.
How common is placenta previa?
Placenta previa occurs in about 1 in 200 pregnancies. Pregnancy care providers usually diagnose it in the second trimester during an ultrasound.
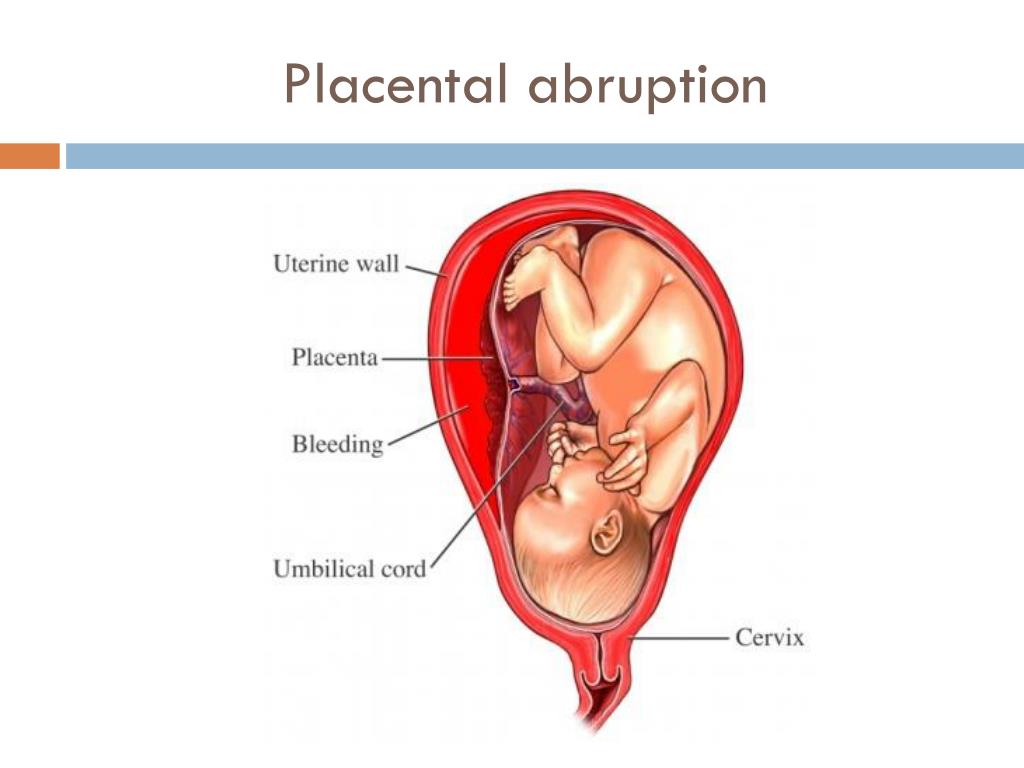
What is the difference between placenta previa and placental abruption?
In placenta previa, the placenta is covering all or part of your cervix. Even though the placenta is in a complicated position, it’s still attached to your uterus. A placental abruption is when the placenta detaches from your uterus. Both conditions can cause vaginal bleeding during pregnancy and labor.
Is placenta previa the same as anterior placenta?
Placenta previa isn’t the same as anterior placenta. Your placenta can grow anywhere in your uterus. An anterior placement of the placenta means the placenta has implanted in the front of your body. Think of anterior placenta as a pillow between your baby and your stomach.
An anterior placement of the placenta means the placenta has implanted in the front of your body. Think of anterior placenta as a pillow between your baby and your stomach.
Symptoms and Causes
What are the symptoms of placenta previa?
The most common symptoms of placenta previa are:
- Bright red bleeding from your vagina. The bleeding often starts near the second half of pregnancy. It can also start, stop, then start again a few days later.
- Mild cramping or contractions in your abdomen, belly or back.
The amount of vaginal bleeding can vary and is often not accompanied by any pain.
What causes placenta previa?
There isn’t a known cause of placenta previa. There are some factors that can increase your risk of developing placenta previa, including your medical history and certain lifestyle habits.
What are the risk factors for developing placenta previa?
There are several factors that increase your risk for placenta previa during pregnancy:
- You smoke cigarettes or use cocaine.
- You’re 35 or older.
- You’ve been pregnant several times before.
- You’re pregnant with twins, triplets or more.
- You’ve had surgery on your uterus, including a C-section or a D&C (dilation and curettage).
- You have a history of uterine fibroids.
What are possible complications of placenta previa?
If you have placenta previa, there are risks for both you and your baby. Complications from placenta previa include:
For you:
- Bleeding: Severe bleeding can occur during pregnancy, labor or delivery.
- Early birth: If you’re bleeding severely, your healthcare provider may perform an emergency C-section before your baby is full term (40 weeks).
- Blood loss: Anemia, low blood pressure, pale skin or shortness of breath are all side effects of losing too much blood.
- Placenta accreta: The placenta grows too deeply in the wall of your uterus.
 This can cause severe bleeding after delivery.
This can cause severe bleeding after delivery. - Placental abruption: The placenta separates from your uterus before your baby is born. This decreases your baby’s supply of oxygen and nutrients.
For baby:
- Premature birth: If your bleeding is severe and you need an emergency C-section, your baby may be born too early.
- Low birth weight: Trouble staying warm and poor weight gain are potential side effects of low birth weight.
- Respiratory issues: Underdeveloped lungs could make breathing more difficult.
Can you have placenta previa without bleeding?
Yes, it’s possible to have placenta previa and not experience vaginal bleeding. You could have mild cramping or pain in your pelvic region or back. It’s best to discuss any bleeding or pelvic pain you have with your healthcare provider.
Why do you bleed when you have placenta previa?
There are two main reasons you bleed if you have placenta previa.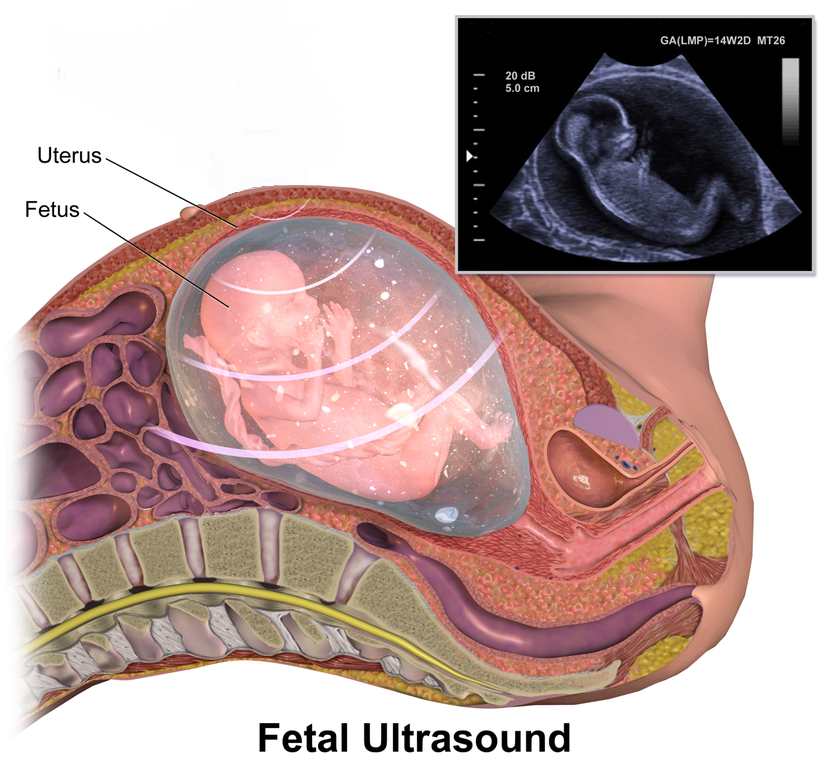 They have to do with how your body prepares for labor.
They have to do with how your body prepares for labor.
- Your cervix is the opening from uterus to your vagina. As pregnancy progresses in the third trimester, your cervix thins (effaces) and spreads to prepare for birth. If your placenta is touching or covering your cervix, this thinning will cause you to bleed.
- During labor, your cervix opens (dilates) in order to allow the baby to exit your uterus and descend down your vagina. When your cervix opens, the blood vessels connecting the placenta to your uterus are torn and can cause bleeding.
Can placenta previa cause a miscarriage?
Miscarriage occurs when you experience a loss of pregnancy before 20 weeks. Pregnancy care providers don’t typically diagnose placenta previa until around or after the 20th week of pregnancy. It’s uncommon that placenta previa would be the cause of a miscarriage.
Diagnosis and Tests
How is placenta previa diagnosed?
Pregnancy care providers usually identify placenta previa in a routine ultrasound around 20 weeks of pregnancy.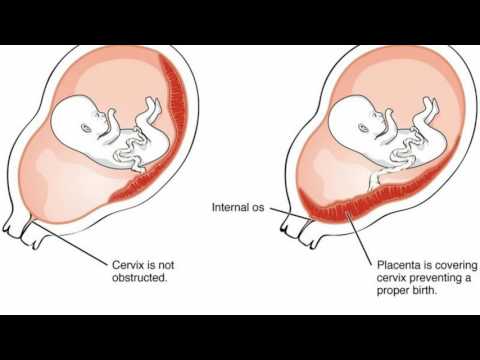 It’s sometimes found when a person experiences symptoms of placenta previa like vaginal bleeding. Your provider will recommend ultrasounds to monitor the placement of the placenta for the remainder of your pregnancy.
It’s sometimes found when a person experiences symptoms of placenta previa like vaginal bleeding. Your provider will recommend ultrasounds to monitor the placement of the placenta for the remainder of your pregnancy.
What tests are used to diagnose placenta previa?
Your healthcare provider will diagnose placenta previa using ultrasounds that show the inside of the female reproductive system:
- Vaginal ultrasound (or transvaginal ultrasound): Your provider places a wand-like device (a transducer) into your vagina to check the position of your baby, the placenta and your cervix.
- Abdominal ultrasound: Your provider places gel on your abdomen, then moves a handheld device (the transducer) around the outside of your belly. This can also show the position of your baby, the placenta and your cervix.
Both types of ultrasound show the images on a monitor or screen. Your pregnancy care provider will determine how much of your cervix is covered by the placenta and recommend treatment.
Management and Treatment
How is placenta previa treated?
The goal is to get you as close to your due date as possible. Delivering via C-section is often the safest treatment if bleeding continues. Treatment of placenta previa depends on:
- How severely you’re bleeding.
- The gestational age of your baby.
- The position of the placenta and your baby.
- The health of you and your baby.
If your provider finds placenta previa early in your second trimester, it can get better on its own. The position of the placenta can change as your uterus expands to accommodate the growing baby. There is often less of a chance that the placenta will move higher in your uterus if your provider diagnoses you with the condition later in pregnancy.
If the placenta is near or covering just part of the cervix and you’re not bleeding, your healthcare provider may recommend:
- Reducing strenuous activities like running, lifting and exercising.
- Bed rest at home.
- No sexual intercourse, tampons or douching.
- More frequent prenatal appointments and ultrasounds.
For moderate to severe cases of placenta previa or frequent bleeding, other treatments could include:
- Bed rest in the hospital.
- Medicine to prevent early labor.
- Steroid shots to help the baby's lungs develop faster.
- Blood transfusions if you experience heavy bleeding.
- An emergency C-section for heavy, uncontrolled bleeding.
Does placenta previa go away?
Placenta previa can go away on its own if it’s found in the second trimester. Going away on its own means the placenta shifts upwards to the top of your uterus. As your uterus expands in the third trimester, the placenta may still move. The later in the pregnancy it remains covering the cervix, the less likely it is to go away. Your healthcare provider will monitor the position of the placenta to see if the condition has resolved before delivery.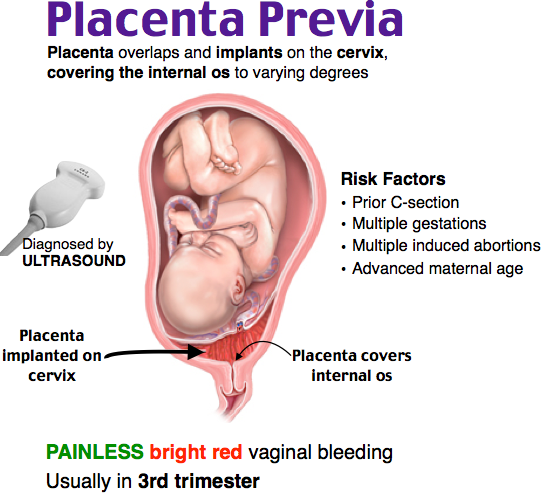
Prevention
Can I reduce my risk for placenta previa?
There is nothing you can do to prevent placenta previa and no surgical or medical procedure can correct it. There are certain risk factors for placenta previa that are within your control, like not smoking or using cocaine. Once your provider diagnoses the condition, there are ways to reduce the amount of vaginal bleeding.
Outlook / Prognosis
What can I expect if I have placenta previa?
Your treatment will be unique to your condition. Most people can expect:
- Frequent monitoring through the second and third trimester. Your provider does this to check the position of the placenta and watch for any changes in symptoms.
- Modified or restricted physical activities like exercise and sex.
- Blood tests post-delivery to check your blood counts.
Will my baby be born early if I have placenta previa?
Maybe. Your healthcare provider will consider the amount of bleeding, the position of the placenta and the baby’s gestational age before deciding if an early delivery is necessary.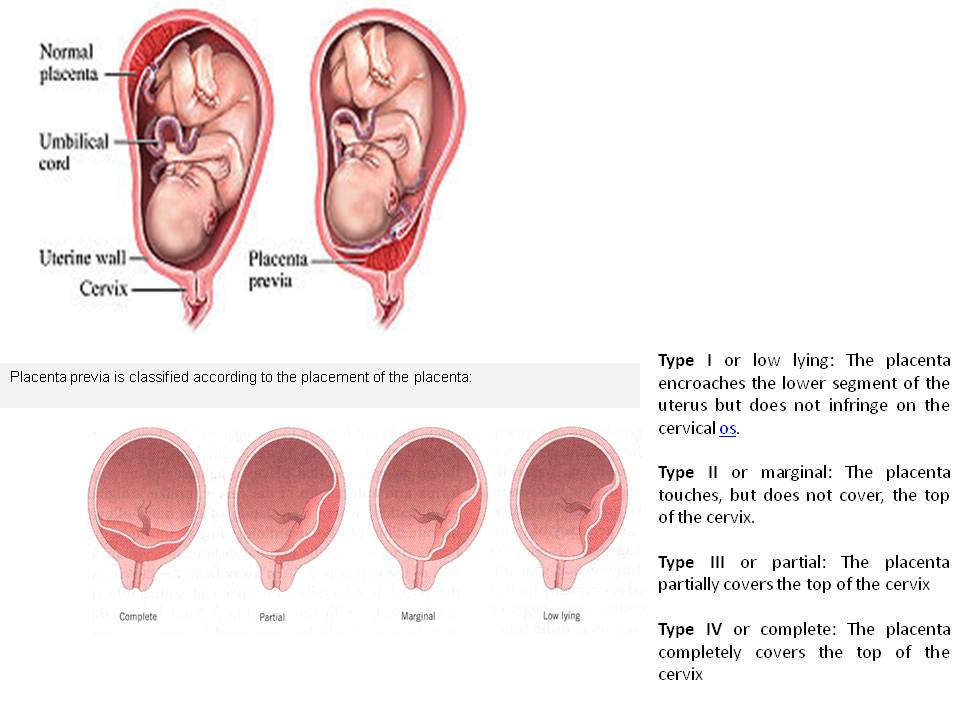 Around 36 weeks of pregnancy, the best option for the health of you and your baby could be an early delivery. Other times a person reaches full term or 40 weeks of pregnancy.
Around 36 weeks of pregnancy, the best option for the health of you and your baby could be an early delivery. Other times a person reaches full term or 40 weeks of pregnancy.
Can I still have a vaginal delivery with placenta previa?
If you have a marginal placenta previa (the placenta is close to your cervix, but not covering it), your healthcare provider may be able to deliver your baby vaginally. This carries a risk of bleeding and may be too dangerous. Your provider will discuss the safest way to deliver your baby.
Will I need a C-section if I’m diagnosed with placenta previa?
A C-section is usually the safest delivery option if you have placenta previa. If the placenta covers even a part of your cervix, a vaginal delivery can cause severe bleeding. Your provider will typically schedule your C-section in advance, but if your bleeding is too severe at any time, you may need an emergency C-section.
Can placenta previa cause birth defects?
It’s uncommon for placenta previa to cause birth defects. Your baby may be born premature if your healthcare provider feels it’s the safest time to deliver. Premature birth carries some complications such as low birth weight and respiratory problems.
Your baby may be born premature if your healthcare provider feels it’s the safest time to deliver. Premature birth carries some complications such as low birth weight and respiratory problems.
Will I get placenta previa again?
If you’ve had placenta previa in a past pregnancy, your chances of having it again are around 2%. If you become pregnant, let your healthcare provider know so that they’re aware of your medical history.
Will placenta previa affect my fertility?
Placenta previa doesn’t impact your chances of getting pregnant again. You’ll have a small risk of getting placenta previa again if you become pregnant.
What questions should I ask my doctor?
Your healthcare provider should be able to answer your questions and prepare you for treatment of placenta previa. Here are some questions you might ask:
- Is the baby’s life in danger? Is mine?
- What are my treatment options?
- How will I know if my placenta previa goes away?
- Should I limit certain activities?
- Can the baby be born now?
- What are potential complications?
- Will I need additional ultrasounds or tests?
- What are the signs that I need to go to the hospital?
What questions will my doctor ask me?
- When did you first notice bleeding?
- How heavy is the bleeding?
- Is bleeding constant or does it come and go?
- Do you have any pelvic pain?
- Have you had pregnancy complications before?
- Have you had uterine surgeries?
- Do you smoke or use cocaine?
- Is there someone to care for you if bed rest is required?
Living With
When should I see my healthcare provider?
Call your healthcare provider immediately if you’re bleeding, cramping or experiencing pelvic pain during your pregnancy, especially in the second half of pregnancy.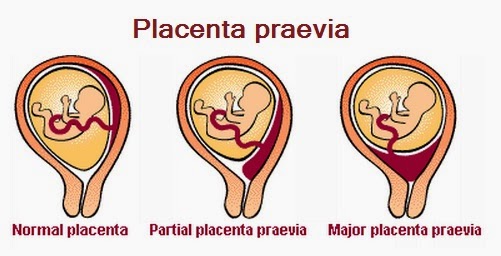
When should I go to the ER?
If you’re experiencing severe blood loss, you should seek emergency medical care immediately. Major blood loss carries several serious side effects to both you and your baby.
Can I exercise with placenta previa?
Your healthcare provider will likely advise you to limit certain activities like exercise, squatting, jumping and lifting. These activities could cause bleeding. It's best to discuss your day-to-day activities with your provider so they can suggest modifications as necessary.
Can I have sex if I have placenta previa?
Most healthcare providers will advise against having sexual intercourse if you have placenta previa. It’s best to avoid any activities that can trigger bleeding or contractions, like using tampons, douching or inserting anything into your vagina.
A note from Cleveland Clinic:
Placenta previa is a treatable condition where most people go on to deliver healthy babies. You’re likely to have a safe delivery if you follow the guidance of your pregnancy care provider. Don’t be afraid to speak up if you experience any bleeding or discomfort during your pregnancy.
Don’t be afraid to speak up if you experience any bleeding or discomfort during your pregnancy.
Save the future - articles from the specialists of the clinic "Mother and Child"
SAVE THE FUTURE
PREGNANCY COMPLICATIONS ARE NOT SO RARE. IF A WOMAN DOES NOT UNDERSTAND WHAT IS HAPPENING TO HER, THEN STARTS TO PANIC AND THEREFORE ONLY aggravates the SERIOUS SITUATION. WHEN THE FUTURE MOTHER HAS A CLEAR VIEW OF THE CURRENT SITUATION, AND SHE REALIZES WHAT AND WHY DOCTORS DO, AND STRICTLY FOLLOWS THEIR RECOMMENDATIONS, IT IS EASIER FOR DOCTORS TO ACHIEVE SUCCESS AND SAVE THE PREGNANCY. nine0005
Pregnancy is a significant and very important period in the life of every woman. It can be divided into three trimesters, in each of which an “abnormal” situation may arise, that is, a complication of pregnancy. In such circumstances, the main thing is not to panic, but to immediately seek medical help.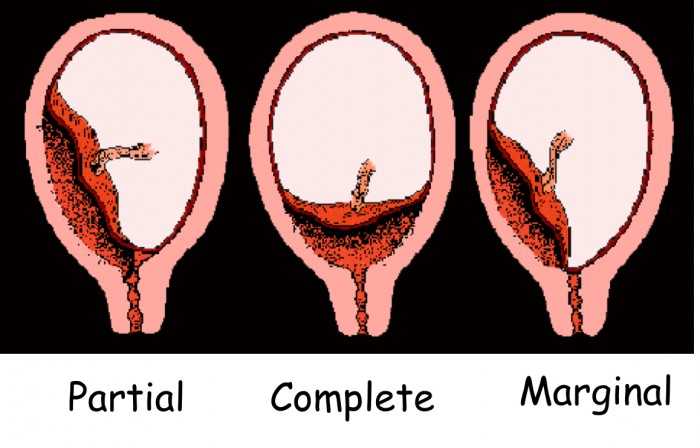 In order not to miss the moment and notice the first signs of trouble in time, the expectant mother should know what complications can occur in each of the trimesters and their symptoms. nine0006
In order not to miss the moment and notice the first signs of trouble in time, the expectant mother should know what complications can occur in each of the trimesters and their symptoms. nine0006
I TRIMESTR
ERROR IS OUT
For the first time, a woman is suspected of being pregnant when her period is delayed. To make sure that this is really the case, a blood test for human chorionic gonadotropin, a hormone whose level rises sharply during pregnancy, helps. And here it is necessary, without delay, to visit an obstetrician-gynecologist and do an ultrasound. It should confirm that the fetal egg is in the uterine cavity. Sometimes (recently, according to the literature, the percentage is growing), a fetal egg can also attach outside the uterine cavity. nine0006
In this case, one speaks of an ectopic pregnancy. Its most common form is tubal, when the fetal egg begins to develop in the fallopian tube. It happens that it is attached in the ovary, abdominal cavity or in the cervix. This condition is life-threatening and requires urgent surgical intervention. The risk is that no organ other than the uterus itself is fit for carrying a baby. A pipe, for example, has a very small volume and, under the “onslaught” of a growing embryo, it will burst sooner or later. The resulting bleeding poses a serious threat to a woman's life. nine0006
This condition is life-threatening and requires urgent surgical intervention. The risk is that no organ other than the uterus itself is fit for carrying a baby. A pipe, for example, has a very small volume and, under the “onslaught” of a growing embryo, it will burst sooner or later. The resulting bleeding poses a serious threat to a woman's life. nine0006
Against the background of a delay in menstruation, paroxysmal pains, often accompanied by weakness, dizziness, nausea, and bloody discharge from the genital tract, should cause anxiety. It is urgent to go to the doctor, since it is possible to accurately determine an ectopic pregnancy only with the help of ultrasound. When an ectopic pregnancy is detected, laparoscopic surgery is most often performed. After restorative treatment, a normal pregnancy often occurs.
EXPECTED COMPLICATION - TOXICOSIS
Everyone has heard about it, everyone is waiting with horror when it comes. What's this? That's right - toxicosis.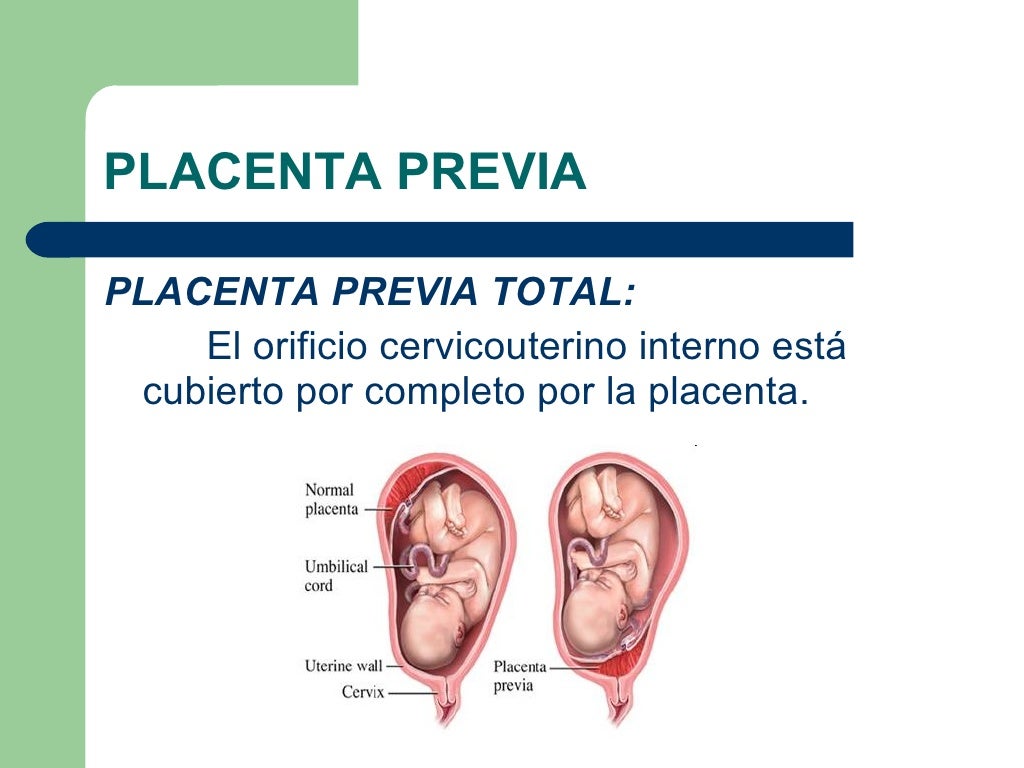 The most anticipated and most common complication of early pregnancy. Mild nausea, intolerance to certain odors, sometimes dizziness - these are the symptoms of early toxicosis, which, not without reason, are also considered indirect signs of pregnancy.
The most anticipated and most common complication of early pregnancy. Mild nausea, intolerance to certain odors, sometimes dizziness - these are the symptoms of early toxicosis, which, not without reason, are also considered indirect signs of pregnancy.
If vomiting is repeated no more than 3-5 times a day and the expectant mother generally feels fine, there is no need to change her usual lifestyle. But when nausea and vomiting occur 10 or even 20 times a day and any food and even a sip of water do not go for the future, a woman needs hospitalization. Lack of food and dehydration - that's what will worry doctors the most. After all, the expectant mother is losing weight, heart palpitations begin, blood pressure drops, but she needs strength to carry the baby. In the hospital, the fluid deficiency will be replenished with the help of droppers, vomiting will be eliminated with the help of special medications approved for pregnant women, and a full examination of the expectant mother will be carried out.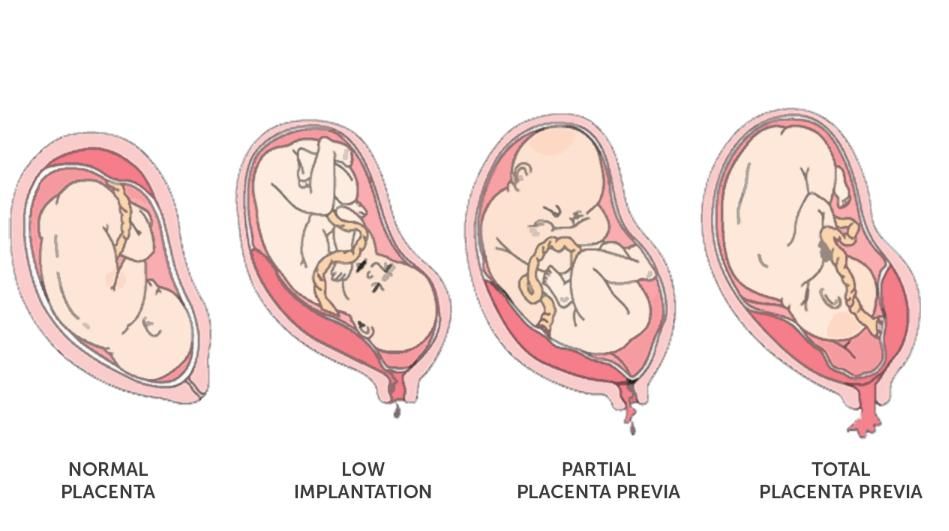 Thanks to this, the unborn child and his expectant mother will feel much better and return to their normal lifestyle again. nine0006
Thanks to this, the unborn child and his expectant mother will feel much better and return to their normal lifestyle again. nine0006
I-II TRIMESTER
THREAT OF TERMINATION OF PREGNANCY
At the beginning of pregnancy, this condition is associated with a hormonal imbalance. For some reason, the hormones that support pregnancy begin to be produced in smaller quantities. Genetic malformations of the embryo can also provoke such a complication. This will seem strange to many, but in Western Europe, doctors do not seek to keep the pregnancy at any cost in the early stages. It is believed that in this way nature conducts natural selection. nine0006
No matter how you feel about this problem and whatever the causes of the complication, the expectant mother should be alerted by pulling pains in the lower abdomen and lower back, bloody discharge from the genital tract. Any of these symptoms may indicate a threatened miscarriage. Moreover, if there is a discharge, the doctors diagnose "a miscarriage that has begun", but this does not mean that the situation cannot be reversed and the situation normalized.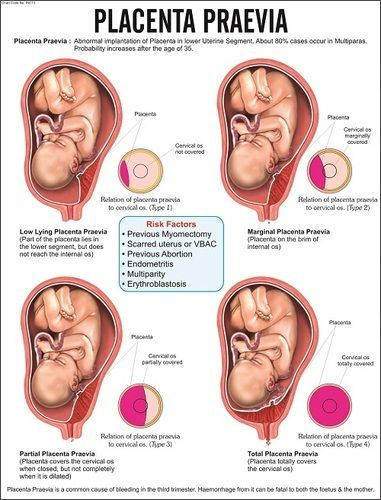 So, when you see such a record in medical documents, do not be alarmed. Doctors will make every effort to still save the pregnancy. nine0006
So, when you see such a record in medical documents, do not be alarmed. Doctors will make every effort to still save the pregnancy. nine0006
And in order for the efforts of doctors to be successful, you should visit a doctor as soon as possible and have an ultrasound scan done. With it, you can find out how the pregnancy develops, but if a woman is concerned about the discharge, then find out their cause: for example, malformations of the uterus or too low location of the placenta, as well as premature opening of the cervix caused by its shortening (isthmic-cervical insufficiency - ICI ). Another mandatory study is the level of hormones in the urine and blood.
In any case, bleeding, too much pain in the lower abdomen, increased uterine tension are a good reason for hospitalization. If hormonal deficiency is detected, hormonal therapy is prescribed to maintain the pregnancy. With a low location of the placenta, a woman will be advised to lead a calm lifestyle and take drugs that relieve tension in the uterus.
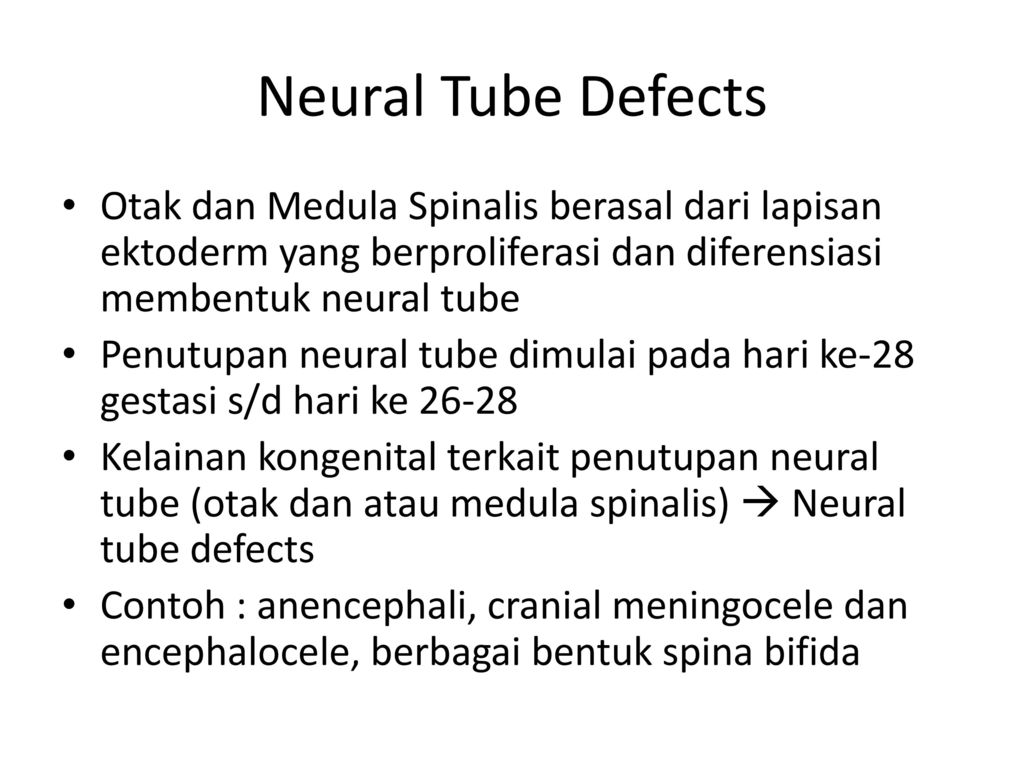
When signs of CCI are detected, the cervix is sutured. All these measures help to prolong the pregnancy to full term - 37 weeks. If the baby is still born earlier, modern equipment and advances in medicine make it possible to nurse babies even with low body weight (from 500 g). nine0006
III TRIMESTER
PLACENTA PRESENTATION
The placenta is formed during pregnancy and is excreted from the body after childbirth. Normally, it should be located in the upper and middle third of the uterus so that the child can be safely born at the time appointed by nature. If the placenta occupies a place near the exit from the uterus, is attached at least partially to the cervix, they speak of placenta previa. The reasons for this situation may be malformations of the internal genital organs, chronic inflammation of the uterus and others. nine0006
A characteristic symptom is bloody discharge from the genital tract, most often after 7 months of pregnancy. To determine this complication, it is enough to do an ultrasound. The woman is recommended hospitalization and bed rest, as well as drug therapy. If placenta previa persists at the time of delivery, the baby can only be born by caesarean section. The expectant mother is hospitalized at the 37-38th week of pregnancy (at this time the pregnancy is considered full-term) in order to prepare for the operation. But if a woman has heavy bleeding, a caesarean section will have to be done on an emergency basis. nine0006
To determine this complication, it is enough to do an ultrasound. The woman is recommended hospitalization and bed rest, as well as drug therapy. If placenta previa persists at the time of delivery, the baby can only be born by caesarean section. The expectant mother is hospitalized at the 37-38th week of pregnancy (at this time the pregnancy is considered full-term) in order to prepare for the operation. But if a woman has heavy bleeding, a caesarean section will have to be done on an emergency basis. nine0006
PLACENTAL DETECTION
This complication occurs when the placenta separates from the uterine wall before the baby is born. Most often this occurs at the end of the third trimester or during childbirth. Women with high blood pressure are most at risk, which is why doctors strongly recommend expectant mothers to carefully monitor their blood pressure levels and strictly follow the doctor's recommendations when it rises.
An expectant mother should be alerted by prolonged abdominal pain, increased activity of the uterus, bleeding from the genital tract. This situation is risky both for the woman herself and for her unborn child. The woman is threatened with blood loss, and the baby is in danger of hypoxia: extensive placental abruption in the truest sense of the word cuts off oxygen to him. The actions of doctors depend on how strong the labor activity is and how great the woman's blood loss is. If the bleeding is weak, the contractions continue, the baby's heartbeat is normal, the baby feels good, the doctors allow the birth to go naturally, but closely monitor the well-being of the mother and baby. With heavy bleeding and the appearance of signs of hypoxia in crumbs, an emergency caesarean section is performed. nine0006
This situation is risky both for the woman herself and for her unborn child. The woman is threatened with blood loss, and the baby is in danger of hypoxia: extensive placental abruption in the truest sense of the word cuts off oxygen to him. The actions of doctors depend on how strong the labor activity is and how great the woman's blood loss is. If the bleeding is weak, the contractions continue, the baby's heartbeat is normal, the baby feels good, the doctors allow the birth to go naturally, but closely monitor the well-being of the mother and baby. With heavy bleeding and the appearance of signs of hypoxia in crumbs, an emergency caesarean section is performed. nine0006
PREMATURE ROUTING OF WATER
This complication is said to occur when the amniotic fluid breaks before contractions begin. There can be many reasons for this development of events, but the main one is infection. That is why doctors carefully monitor expectant mothers and during pregnancy several times do bacteriological culture of flora from the cervical canal.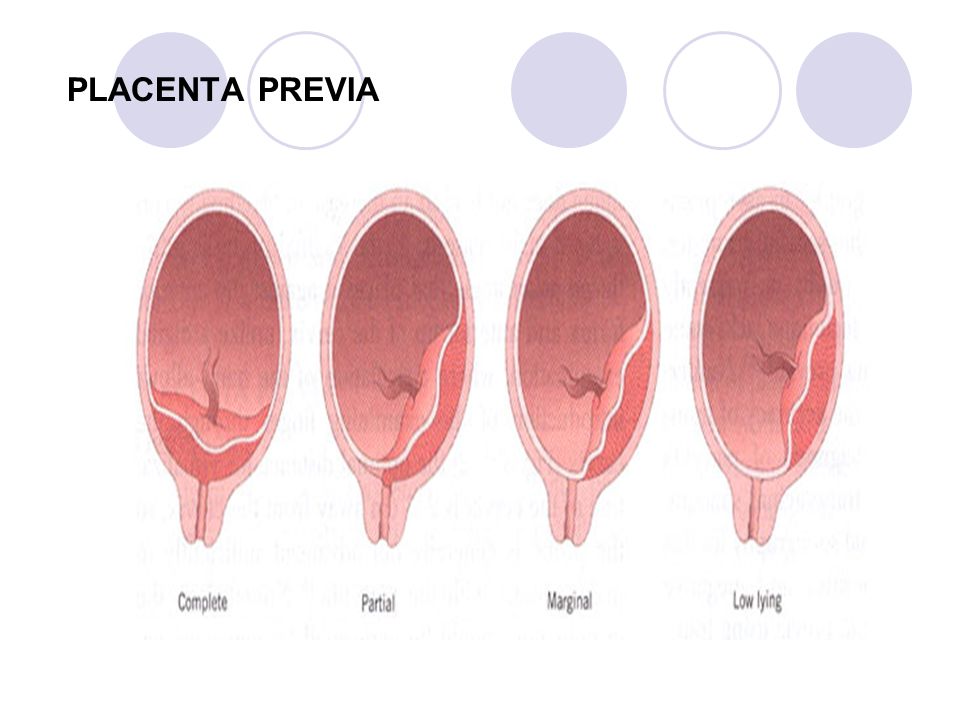 According to modern international recommendations, it is also desirable to take a smear for group B streptococci before childbirth at about 36-37 weeks. If an infection is detected during childbirth, a woman is given antibiotic therapy. nine0006
According to modern international recommendations, it is also desirable to take a smear for group B streptococci before childbirth at about 36-37 weeks. If an infection is detected during childbirth, a woman is given antibiotic therapy. nine0006
If the amniotic fluid is shed, regardless of the gestational age, call an ambulance or go to the maternity hospital. Making sure that this is really amniotic fluid is quite simple. If the flow of urine can be stopped by tensing the muscles, then the amniotic fluid will continue to flow even if the muscles are tensed. In addition, you can use the amniotest (test for amniotic fluid). If amniotic fluid is expelled, the test strip will change color. There are also special pads that are much easier to use. The principle of their action is the same: if amniotic fluid gets on them, the pads change color. nine0006
You should also see a doctor if the amniotic fluid starts to leak a little. Only a doctor can clarify the situation. Don't refuse hospitalization. If the leakage intensifies, medical attention is indispensable. In most cases, after the outflow of amniotic fluid, a woman and her unborn child begin to prepare for childbirth. If this happened before the 34th week of pregnancy, the baby is given medication to help his lungs open up. But when the waters have not completely poured out, it is possible to prolong the pregnancy. And the efforts of doctors will be directed precisely at this. nine0006
If the leakage intensifies, medical attention is indispensable. In most cases, after the outflow of amniotic fluid, a woman and her unborn child begin to prepare for childbirth. If this happened before the 34th week of pregnancy, the baby is given medication to help his lungs open up. But when the waters have not completely poured out, it is possible to prolong the pregnancy. And the efforts of doctors will be directed precisely at this. nine0006
PRE-ECLAMPSIA
Another insidious complication in late pregnancy is preeclampsia, or, as it used to be called, preeclampsia. Another name for this complication is late toxicosis of pregnant women. Its main symptom is the presence of protein in the urine. It is for this reason that during pregnancy it is necessary to take this analysis so often. In addition, preeclampsia is manifested by an increase in blood pressure up to 130/90 mm Hg. and above, internal and external edema, due to which the expectant mother gains excess weight. DO NOT refuse hospitalization: adverse symptoms may increase, due to which the well-being of the unborn baby may deteriorate sharply. Complex therapy prescribed by the attending physician, as a rule, leads to a positive result. If the symptoms increase, you have to resort to emergency delivery - depending on the situation, induce labor or do a caesarean section. nine0006
DO NOT refuse hospitalization: adverse symptoms may increase, due to which the well-being of the unborn baby may deteriorate sharply. Complex therapy prescribed by the attending physician, as a rule, leads to a positive result. If the symptoms increase, you have to resort to emergency delivery - depending on the situation, induce labor or do a caesarean section. nine0006
To avoid trouble, doctors advise expectant mothers not to abuse salt, but rather to stop consuming it, lead a healthy lifestyle, drink 2 liters of fluid a day and observe a sleep and rest regimen.
Placenta previa. What is placenta previa?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0006
Placenta previa is an anomaly of the period of pregnancy, characterized by attachment of the placenta to the lower segment of the uterus with partial or complete overlap of the internal uterine os. Clinically, placenta previa is manifested by recurrent bleeding from the genital tract, anemia of the pregnant woman, the threat of miscarriage, and fetal placental insufficiency. Placenta previa is diagnosed during a vaginal examination, ultrasound. Identification of placenta previa requires the prevention of spontaneous abortion, correction of anemia and fetal hypoxia, the choice of optimal delivery tactics (more often - caesarean section). nine0006
Clinically, placenta previa is manifested by recurrent bleeding from the genital tract, anemia of the pregnant woman, the threat of miscarriage, and fetal placental insufficiency. Placenta previa is diagnosed during a vaginal examination, ultrasound. Identification of placenta previa requires the prevention of spontaneous abortion, correction of anemia and fetal hypoxia, the choice of optimal delivery tactics (more often - caesarean section). nine0006
ICD-10
O44 Placenta previa
- Causes of placenta previa
- Symptoms of placenta previa
- Diagnosis of placenta previa
- Treatment for placenta previa
- Prophylaxis
- Prices for treatment
General
The placenta (afterbirth, child's place) is an important embryonic structure that fits snugly against the inner wall of the uterus and provides contact between the organisms of the mother and fetus. During pregnancy, the placenta performs nutritional, gas exchange, protective, immune, hormonal functions necessary for the full development of the embryo and fetus.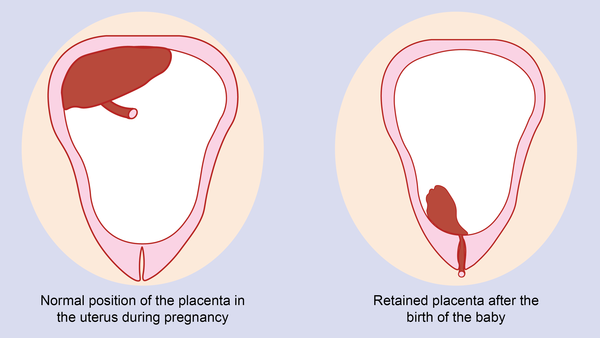 The location of the placenta in the region of the posterior and lateral walls of the body or the bottom of the uterus, i.e., in the zones of the best vascularization of the myometrium, is considered to be physiological. Attachment of the placenta to the posterior wall is optimal because it protects this embryonic structure from accidental damage. The location of the placenta on the anterior surface of the uterus is rare. nine0006
The location of the placenta in the region of the posterior and lateral walls of the body or the bottom of the uterus, i.e., in the zones of the best vascularization of the myometrium, is considered to be physiological. Attachment of the placenta to the posterior wall is optimal because it protects this embryonic structure from accidental damage. The location of the placenta on the anterior surface of the uterus is rare. nine0006
In the event that the placenta is attached so low that it overlaps the internal os to a certain extent, they speak of placenta previa. In obstetrics and gynecology, placenta previa occurs in 0.1-1% of all births. With the total closure of the internal pharynx by the placenta, there is a variant of complete placenta previa. This type of pathology occurs in 20-30% of cases of the number of presentations. With partial overlap of the internal pharynx, the condition is regarded as incomplete placenta previa (frequency 35-55%). With the localization of the lower edge of the placenta in the III trimester at a distance of less than 5 cm from the internal pharynx, a low location of the placenta is diagnosed.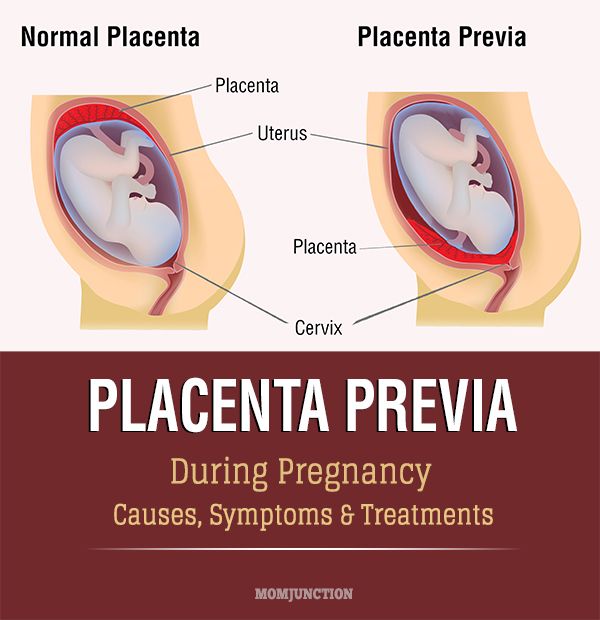 nine0006
nine0006
Placenta previa creates conditions for prematurity and fetal hypoxia, incorrect position and presentation of the fetus, premature birth. The proportion of perinatal mortality in placenta previa reaches 7-25%, and maternal mortality due to bleeding and hemorrhagic shock is 3%.
placenta previa
Causes of placenta previa
Placenta previa is more often due to pathological changes in the endometrium that disrupt the course of the decidual reaction of the stroma. Such changes can be caused by inflammation (cervicitis, endometritis), surgical interventions (diagnostic curettage, surgical termination of pregnancy, conservative myomectomy, caesarean section, uterine perforation), multiple complicated births. nine0006
Among the etiological factors of placenta previa are endometriosis, uterine fibroids, uterine anomalies (hypoplasia, bicornuity), multiple pregnancy, cervical canal polyps. In connection with these factors, the timeliness of implantation of the fetal egg in the upper sections of the uterine cavity is disrupted, and its attachment occurs in the lower segments. Placenta previa is more likely to develop in re-pregnant women (75%) than in nulliparous women.
In connection with these factors, the timeliness of implantation of the fetal egg in the upper sections of the uterine cavity is disrupted, and its attachment occurs in the lower segments. Placenta previa is more likely to develop in re-pregnant women (75%) than in nulliparous women.
Symptoms of placenta previa
In the clinic of placenta previa, the leading manifestations are repeated uterine bleeding of varying severity. During pregnancy, bleeding due to placenta previa is recorded in 34% of women, during childbirth - in 66%. Bleeding can develop at different stages of pregnancy - from the first trimester to the very birth, but more often - after the 30th week of gestation. On the eve of childbirth, bleeding usually increases due to periodic uterine contractions.
The cause of bleeding is the repetitive detachment of the presenting part of the placenta, which occurs due to the inability of the placenta to stretch after the uterine wall during the development of pregnancy or labor.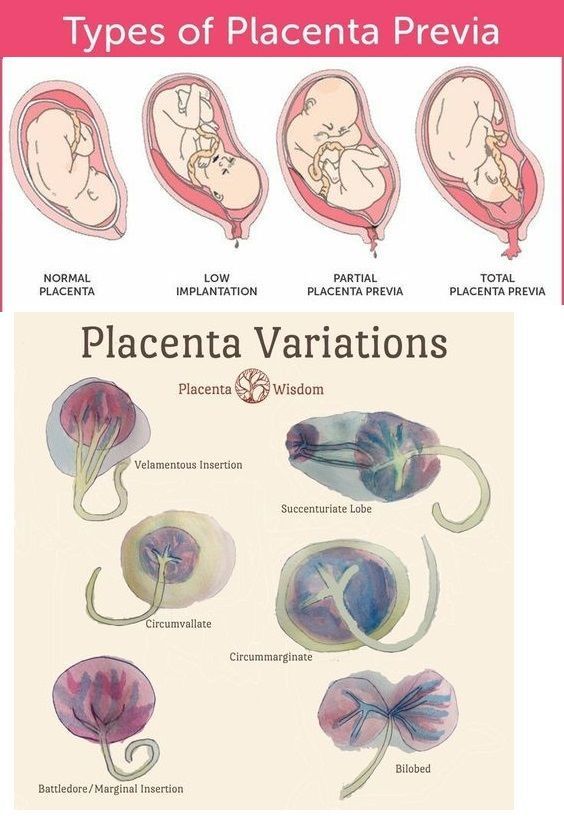 With detachment, a partial opening of the intervillous space occurs, which is accompanied by bleeding from the vessels of the uterus. The fetus at the same time begins to experience hypoxia, since the exfoliated area of the placenta ceases to participate in gas exchange. With placenta previa, bleeding can be provoked by physical activity, coughing, sexual intercourse, straining during bowel movements, vaginal examination, thermal procedures (hot bath, sauna). nine0006
With detachment, a partial opening of the intervillous space occurs, which is accompanied by bleeding from the vessels of the uterus. The fetus at the same time begins to experience hypoxia, since the exfoliated area of the placenta ceases to participate in gas exchange. With placenta previa, bleeding can be provoked by physical activity, coughing, sexual intercourse, straining during bowel movements, vaginal examination, thermal procedures (hot bath, sauna). nine0006
The intensity and nature of bleeding is usually due to the degree of placenta previa. Complete placenta previa is characterized by the sudden development of bleeding, the absence of pain, and the abundance of blood loss. In the case of incomplete placenta previa, bleeding, as a rule, develops closer to the term of labor, especially often at the beginning of labor, during the period of smoothing and opening of the pharynx. The greater the degree of placenta previa, the earlier and more intense the bleeding. Thus, bleeding during placenta previa is characterized by an external character, a sudden onset without visible external causes (often at night), the release of scarlet blood, painlessness, and mandatory repetition. nine0006
Thus, bleeding during placenta previa is characterized by an external character, a sudden onset without visible external causes (often at night), the release of scarlet blood, painlessness, and mandatory repetition. nine0006
Recurrent blood loss quickly leads to anemia of the pregnant woman. A decrease in BCC and the number of red blood cells can cause DIC and the development of hypovolemic shock, even in the case of minor blood loss. Pregnancy complicated by placenta previa often occurs with the threat of spontaneous abortion, arterial hypotension, preeclampsia. Preterm birth occurs more often with complete placenta previa.
The pathology of the location of the placenta most adversely affects the development of the fetus: it causes fetal-placental insufficiency, hypoxia and delayed fetal maturation. With placenta previa, the pelvic, oblique or transverse position of the fetus is often observed. In the II-III trimesters of pregnancy, the localization of the placenta may change due to the transformation of the lower uterine segment and changes in the growth of the placenta in the direction of better blood-supplying areas of the myometrium. This process in obstetrics is called "migration of the placenta" and is completed by the 34-35th week of pregnancy. nine0006
This process in obstetrics is called "migration of the placenta" and is completed by the 34-35th week of pregnancy. nine0006
Diagnosis of placenta previa
When recognizing placenta previa, the presence of risk factors in the anamnesis of the pregnant woman, episodes of recurrent external uterine bleeding, and objective examination data are taken into account. An external obstetric examination reveals a high standing of the uterine fundus, due to the location of the presenting part of the fetus, often a transverse or oblique position of the fetus. During auscultation, placental vascular noise is heard in the lower segment of the uterus, at the location of the placenta. nine0006
In the course of a gynecological examination, the cervix is examined in the mirrors to exclude its injuries and pathologies. With a closed external pharynx, the presenting part of the fetus cannot be established. With complete placenta previa, a massive soft formation is palpated, occupying all the vaults of the vagina; with incomplete - the anterior or one of the lateral arches.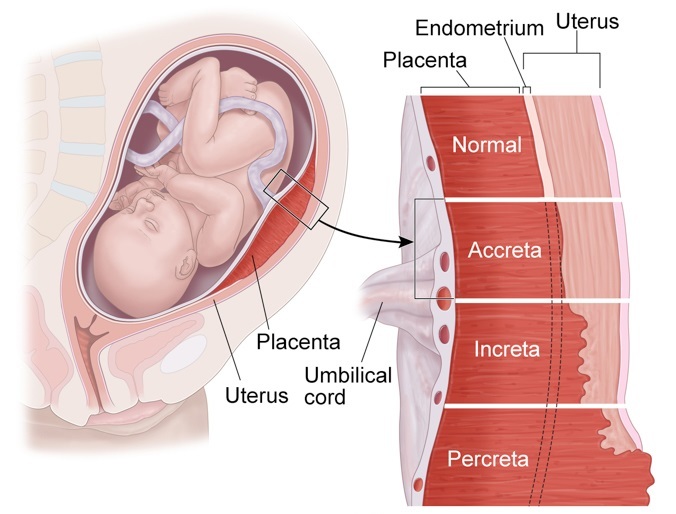
With the patency of the cervical canal in the case of complete presentation, the placenta closes the entire opening of the internal pharynx, and its palpation leads to increased bleeding. If fetal membranes and placental tissue are found in the lumen of the uterine os, an incomplete placenta previa is diagnosed. Vaginal examination with placenta previa is performed very carefully, in conditions of readiness for emergency assistance in the development of massive bleeding. nine0006
The safest objective method for detecting placenta previa, which is widely used in obstetrics and gynecology, is ultrasound. In the course of echography, a variant (incomplete, complete) of placenta previa, the size, structure and area of the presenting surface, the degree of detachment during bleeding, the presence of retroplacental hematomas, the threat of miscarriage, is determined, "migration of the placenta" is determined in the process of dynamic studies.
Treatment for placenta previa
The tactics of conducting pregnancy with placenta previa is determined by the severity of bleeding and the degree of blood loss. In the I-II trimester, in the absence of spotting, a pregnant woman with placenta previa can be under outpatient supervision of an obstetrician-gynecologist. At the same time, a protective regimen is recommended, which excludes factors provoking bleeding (physical activity, sexual life, stressful situations, etc.).
In the I-II trimester, in the absence of spotting, a pregnant woman with placenta previa can be under outpatient supervision of an obstetrician-gynecologist. At the same time, a protective regimen is recommended, which excludes factors provoking bleeding (physical activity, sexual life, stressful situations, etc.).
At a gestational age of more than 24 weeks or bleeding that has begun, pregnancy is monitored in an obstetric hospital. Therapeutic tactics for placenta previa is aimed at maximizing the prolongation of pregnancy. Bed rest is prescribed, drugs with antispasmodic (drotaverine) and tocolytic (fenoterol, hexoprenaline) action, iron deficiency anemia is corrected (iron preparations). In order to improve fetoplacental and uteroplacental blood flow, the administration of pentoxifylline, dipyridamole, ascorbic acid, thiamine pyrophosphate is used. With the threat of the onset of preterm labor at a period of 28 to 36 weeks of pregnancy, glucocorticoids (dexamethasone, prednisolone) are prescribed for the prevention of respiratory disorders in a newborn.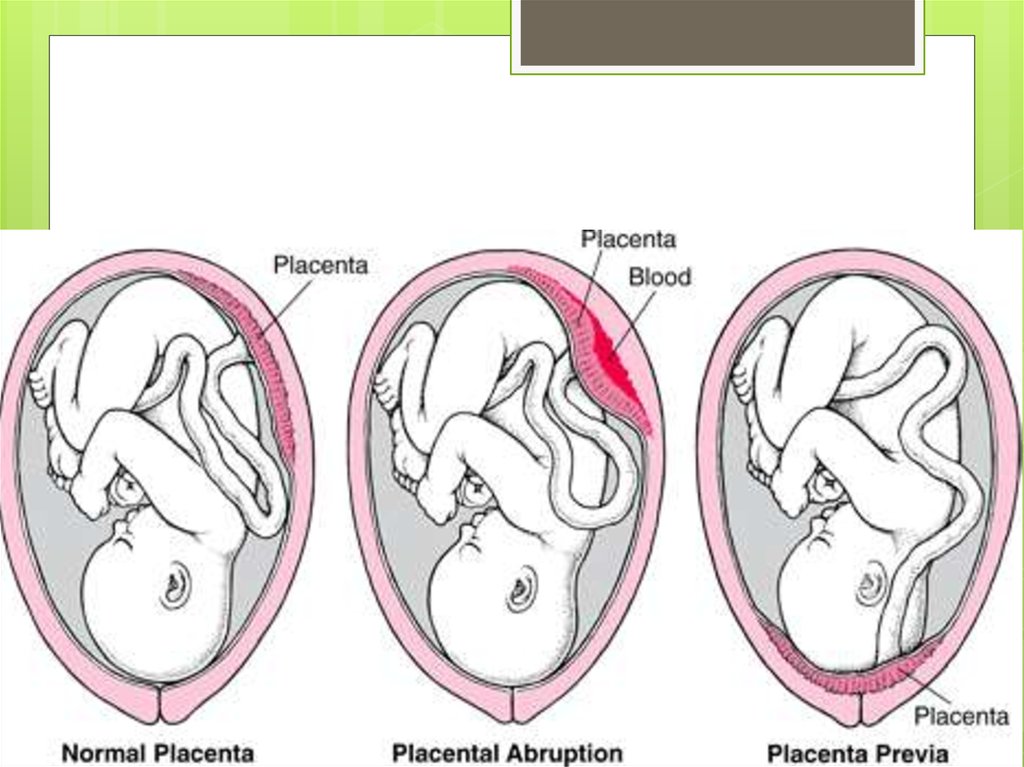 nine0006
nine0006
Indications for emergency early delivery are repeated bleeding of more than 200 ml, severe anemia and hypotension, bleeding with a simultaneous blood loss of 250 ml, bleeding with complete placenta previa. Caesarean section in these cases is performed to save the mother, regardless of the gestational age and viability of the fetus.
With successful prolongation of pregnancy to a period of 37-38 weeks, the optimal method of delivery is selected. Cesarean section is shown in absolutely all cases of complete placenta previa, as well as with incomplete presentation, combined with a transverse position or pelvic presentation of the fetus; aggravated obstetric and gynecological history; the presence of a scar on the uterus, multiple pregnancy, polyhydramnios, narrow pelvis. nine0006
Natural childbirth is possible only with incomplete placenta previa, subject to the maturity of the cervix, good labor activity, head presentation of the fetus.