Neural tube defect detection
Neural tube defects | March of Dimes
Neural tube defects (NTDs) are birth defects of the brain and spinal cord. NTDs can cause serious problems for babies.
To help prevent NTDs, take a vitamin supplement that has 400 micrograms of folic acid in it every day, even if you’re not trying to get pregnant.
If you’re at high risk for NTDs, take 4,000 micrograms of folic acid every day. Talk to your provider about how to get this much safely.
Your risk for having a baby with an NTD is higher if you, your partner or your family members have an NTD, or if you’ve had a baby with an NTD.
Folic acid helps prevent NTDs only if you take it before and in the first weeks of pregnancy.
What are neural tube defects?
Neural tube defects (also called NTDs) are birth defects of the brain and spinal cord. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
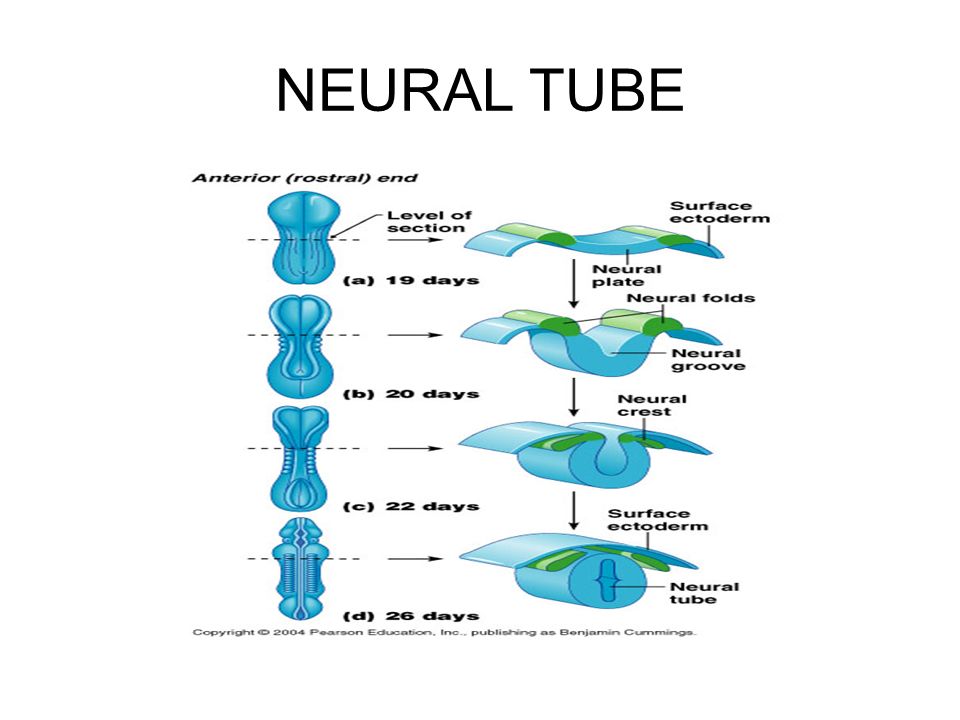
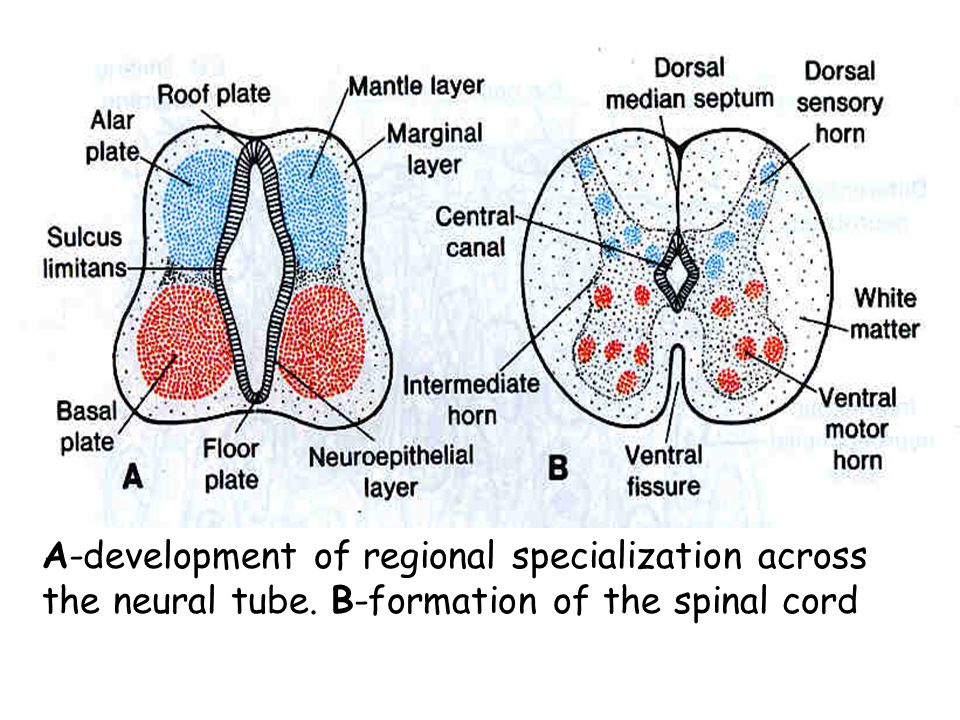
A baby’s neural tube normally starts out as a tiny, flat ribbon that turns into a tube by the end of the first month of pregnancy. If the tube doesn’t close completely, an NTD can happen. NTDs can cause serious problems for babies, including death.
NTDs happen in about 3,000 pregnancies each year in the United States. Hispanic women are more likely than non-Hispanic women to have a baby with an NTD.
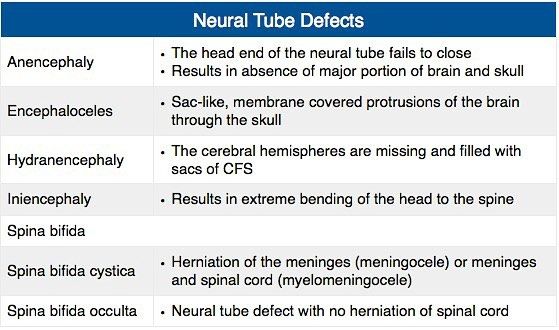
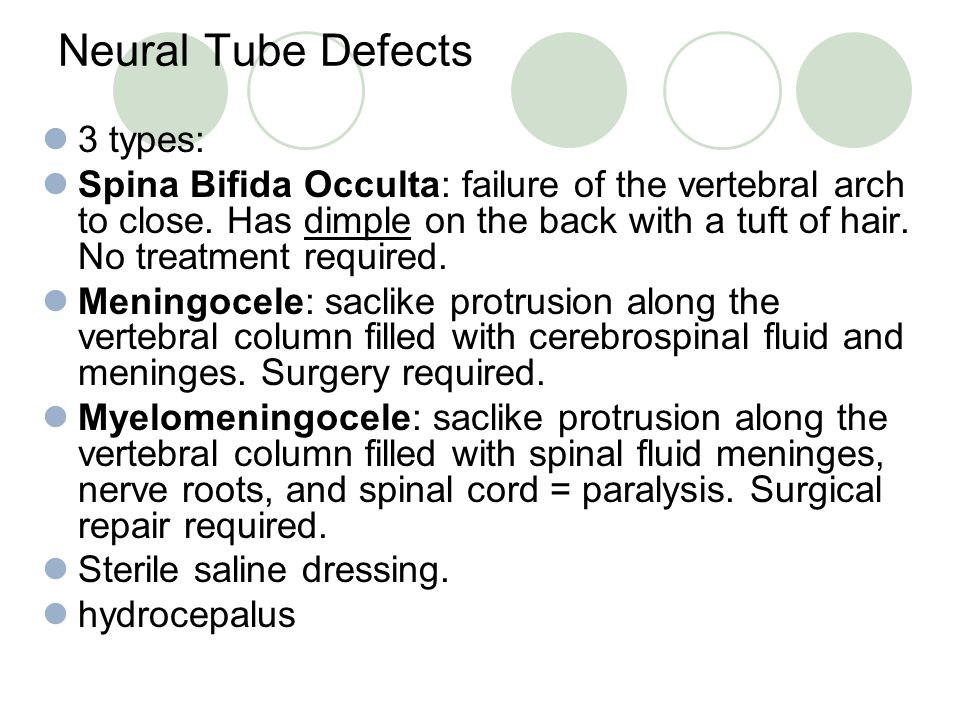
The two most common NTDs are spina bifida and anencephaly. Spina bifida affects about 1,500 babies a year in the United States. If your baby has spina bifida, the tiny bones of the spine don’t close completely, and part of the spinal cord pokes through the spine. Children with spina bifida may have paralyzed legs (not able to move) and problems controlling their bladder and bowel (going to the bathroom). Milder forms of spina bifida may cause fewer problems for children.
Anencephaly is one of the most severe NTDs. It affects about 1,000 babies each year in the United States. Anencephaly is caused when the upper part of the neural tube that forms the brain doesn’t close completely. Babies with this condition are missing major parts of the brain, skull and scalp. They do not survive long after birth, usually for just a few hours. Girls are 3 times more likely than boys to have anencephaly.
It affects about 1,000 babies each year in the United States. Anencephaly is caused when the upper part of the neural tube that forms the brain doesn’t close completely. Babies with this condition are missing major parts of the brain, skull and scalp. They do not survive long after birth, usually for just a few hours. Girls are 3 times more likely than boys to have anencephaly.
Taking folic acid before and during early pregnancy can help prevent NTDs in your baby. Folic acid is a B vitamin that every cell in your body needs for normal growth and development.
What causes NTDs?
We’re not exactly sure what causes NTDs. Experts think some may be caused by genetics. This means an NTD can be passed from parents to children through genes. Genes are part of your body’s cells that stores instructions for the way your body grows, looks and works.
NTDs also may be caused by things in your environment, which includes where you live, where you work, the kinds of foods you eat or have access to and how you like to spend your time. Some things in your environment can be harmful to a pregnancy, like certain drugs, cigarette smoke, air pollution and lead.
Some things in your environment can be harmful to a pregnancy, like certain drugs, cigarette smoke, air pollution and lead.
Are you at risk for having a baby with an NTD?
Any woman can have a baby with an NTD. But there are things that may make you more likely than other women to have a baby with an NTD. These are called risk factors.
Your risk for having a baby with an NTD is higher if:
- You’ve had a baby with an NTD. If you’ve had a baby with an NTD, there’s a 2- to 3-percent chance of having a baby with an NTD in another pregnancy. A genetic counselor can help you understand your risk for having a baby with an NTD. This is someone who is trained to help you understand medical conditions that run in families, and how they can affect your health and your baby’s health.
- You or your partner has an NTD, your partner has a child with an NTD or someone in either of your families has an NTD. This means you have a family history of NTDs.
 Use the March of Dimes Family Health History Form to keep track of health conditions, including NTDs,that may run in your family. Fill it out and share it with your health care provider or genetic counselor.
Use the March of Dimes Family Health History Form to keep track of health conditions, including NTDs,that may run in your family. Fill it out and share it with your health care provider or genetic counselor.
Other risk factors for NTDs include:
- Taking certain anti-seizure medicines. Talk to your health care provider before you get pregnant about how the medicine may affect your pregnancy.
- Obesity. Some studies show that being obese increases your risk for having a baby with an NTD. If you’re obese, you have an excess amount of body fat and your body mass index (BMI) is 30 or higher. To find out your BMI, go to cdc.gov/bmi. Talk to your provider about getting to a healthy weight before pregnancy.
- Diabetes. If your diabetes is uncontrolled, you may be at increased risk for having a baby with an NTD. Eating healthy foods and being active every day can help you keep your diabetes under control.
- Using opioids in the first 2 months of pregnancy. Opioids are highly addictive drugs. Your provider may prescribe an opioid to you as a painkiller if you’ve been injured or had surgery. Common prescription opioids include codeine, hydrocodone and oxycodone. These often are sold and used illegally. If you take any opioid during pregnancy, it can cause serious problems for your baby, like premature birth and drug withdrawal called neonatal abstinence syndrome (also called NAS). If you’re pregnant and taking any drug or medicine that may be an opioid, tell your health care provider right away.
- A high body temperature early in pregnancy. This may be caused by a fever or by spending a lot of time in a hot tub or sauna. If you’re pregnant, stay out of hot tubs and saunas. If you do use them, limit the time to less than 10 minutes.
How can you help prevent NTDs in your baby?
Taking folic acid before and during early pregnancy can help prevent NTDs in your baby.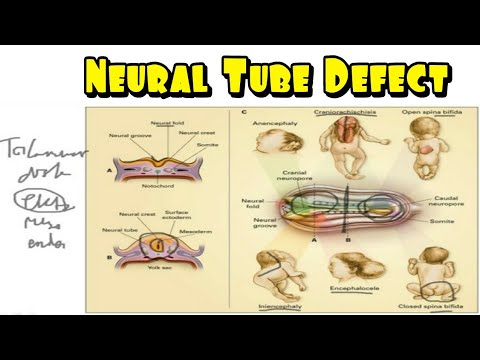 NTDs happen in the first month of pregnancy, before you may know you’re pregnant. This is why it’s important to have enough folic acid in your body before you get pregnant.
NTDs happen in the first month of pregnancy, before you may know you’re pregnant. This is why it’s important to have enough folic acid in your body before you get pregnant.
Most women
To help prevent NTDs in your baby, take a vitamin supplement with 400 mcg of folic acid every day before getting pregnant. A supplement is a product you take to make up for certain nutrients that you don’t get enough of in the foods you eat. Start taking this amount of folic acid each day at least 1 month before pregnancy and through the first 12 weeks of pregnancy. Your folic acid supplement can be:
- A multivitamin. This is a pill that contains many vitamins and other nutrients that help your body stay healthy.
- A prenatal vitamin. This is a multivitamin that has nutrients you need during pregnancy. Your health care provider may give you a prescription for prenatal vitamins, or you can get them over the counter without a prescription.
- A supplement that contains just folic acid
Take a vitamin supplement with 400 mcg of folic acid each day, even if you’re not trying to get pregnant.
Women at high risk for NTDs
If you’re at high risk for having a baby with an NTD, it’s recommended you take 4,000 mcg of folic acid each day to help prevent an NTD. Start taking 4,000 mcg 3 months before you get pregnant through 12 weeks of pregnancy. You’re at high risk if:
- You’ve had a pregnancy with an NTD in the past.
- You or your partner has an NTD.
- Your partner has a child with an NTD.
Studies show that taking 4,000 mcg of folic acid before and during early pregnancy can help reduce your risk of having another baby with an NTD by about 70 percent. Ask your provider how to safely get this much folic acid. It’s not safe to take several multivitamins or prenatal vitamins because you can get too much of other nutrients, which may be harmful to your health.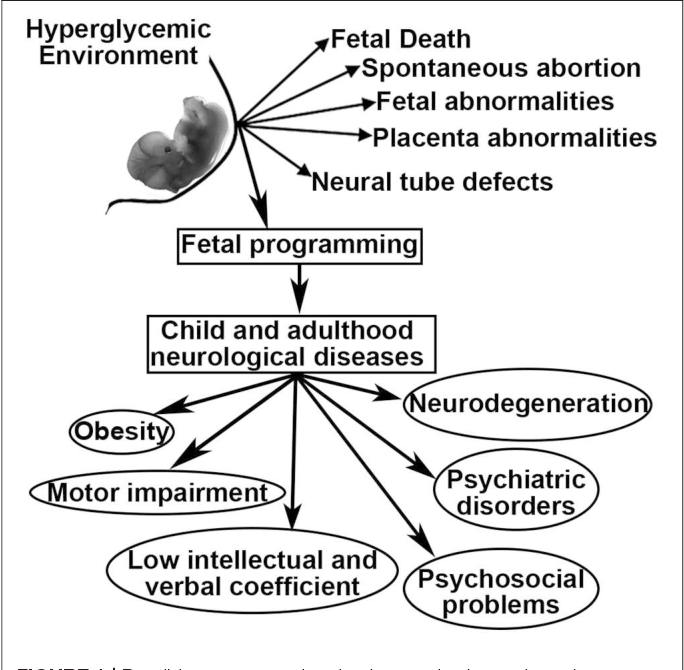 Your provider can help you figure out the best and safest way for you to get the right amount of folic acid.
Your provider can help you figure out the best and safest way for you to get the right amount of folic acid.
Can you get folic acid from food?
Yes! You can get folic acid from foods that are fortified with folic acid. Fortified means a food has folic acid added to it. Check the product label to see how much folic acid you get in each serving. Look for the word “fortified” or “enriched” on labels on foods like:
- Bread
- Breakfast cereal
- Cornmeal
- Flour
- Pasta
- Products made from a kind of flour called corn masa, like tortillas, tortilla chips, taco shells, tamales and pupusas
- White rice
Some fruits and vegetables are good sources of folic acid. When folic acid is naturally in a food, it’s called folate. Foods that are good sources of folate are:
- Beans, like lentils, pinto beans and black beans
- Leafy green vegetables, like spinach and Romaine lettuce
- Asparagus
- Broccoli
- Peanuts (But don’t eat them if you have a peanut allergy.
 )
) - Citrus fruits, like oranges and grapefruit
- Orange juice (100 percent juice is best. This means one serving of juice is equal to one serving of fruit.)
It’s hard to get all the folic acid you need from food. Even if you eat foods that have folic acid in them, take your vitamin supplement each day, too.
Can you find out if your baby has an NTD before birth?
Yes. You can get prenatal tests (medical tests you get during pregnancy) called screening tests to find out if your baby is at increased risk of having an NTD. Screening tests for NTDs include:
- Maternal blood screening (also called a quad screen). It’s called a quad screen because it measures four substances in your blood. The test is done between 15 to 22 weeks of pregnancy.
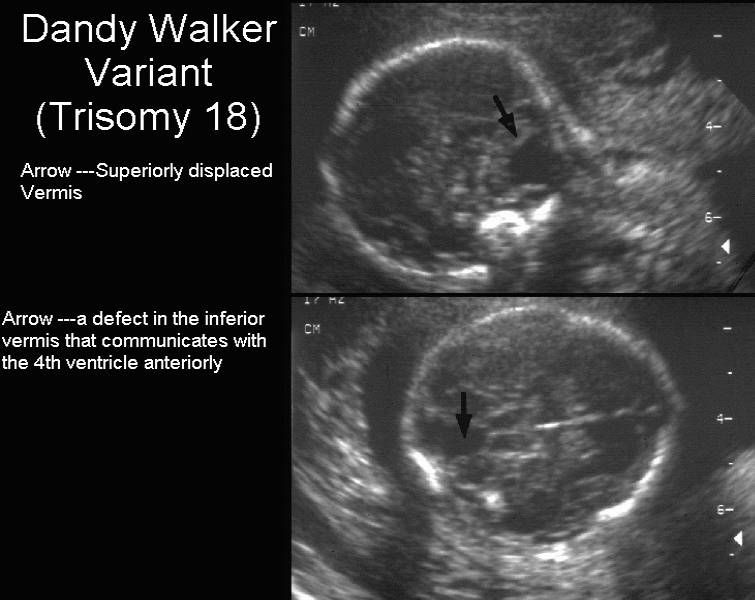
- Ultrasound. This test uses sound waves and a computer screen to show a picture of your baby inside the womb. You usually get an ultrasound at 16 to 20 weeks of pregnancy.
If a screening test shows an increased risk of NTDs, your provider may recommend a diagnostic test to find out for sure if your baby has an NTD. Diagnostic tests for NTDs include:
Diagnostic tests for NTDs include:
- Amniocentesis. In this test, your provider takes some amniotic fluid from around your baby in the uterus (womb) to check for birth defects, like NTDs, in your baby. You can get this test at 15 to 20 weeks of pregnancy.
- Detailed ultrasound of your baby’s skull and spine
If you find out that your baby has an NTD, talk to your health care provider to learn more about your baby’s condition and options for birth and treatment. For example:
- You can plan to have your baby in a hospital that specializes in caring for babies with NTDs. This way your baby can have any necessary surgery or treatment soon after birth.
- You can decide whether to have a vaginal or cesarean birth (also called c-section). During vaginal birth, the uterus contracts to help push the baby out through the vagina. A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. In some cases, a c-section may be safer for you and your baby than vaginal birth.
- If your baby has spina bifida, you can find out about surgery for your baby in the womb before birth. Surgery to repair spina bifida in the womb before birth is more effective than surgery after birth.
For more information
American Academy of Pediatrics
Spina Bifida Association
Centers for Disease Control and Prevention
Last reviewed: February, 2022
Neural tube defects | Pregnancy Birth and Baby
Neural tube defects | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Neural tube defects are abnormalities that occur in the development of the spinal cord and brain of some babies. The most common defects are spina bifida (abnormal development of part of the spine and spinal cord) and anencephaly (severely abnormal development of the brain).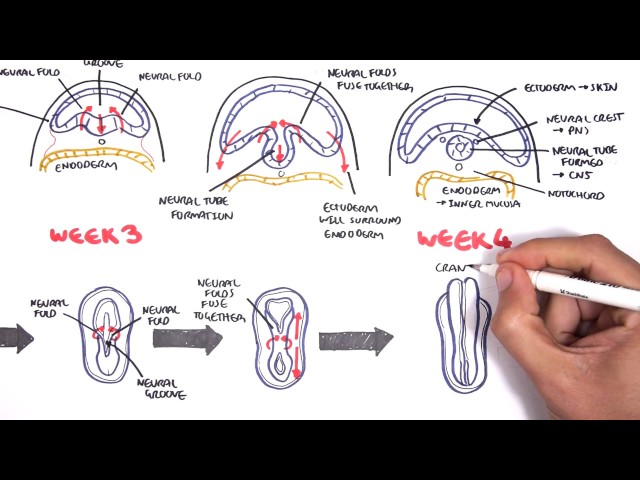
What are neural tube defects?
During the first month of life, an embryo (developing baby) grows a primitive tissue structure called the ‘neural tube’. As the embryo develops, the neural tube begins to change into a more complicated structure of bones, tissue and nerves that will eventually form the spine and nervous system.
However, in cases of spina bifida, something goes wrong with the development of the neural tube and the spinal column (the ridge of bone that surrounds and protects the nerves) does not fully close. Spina bifida is a Latin term that means ‘split spine’.
The chance that a pregnancy will be affected by a neural tube defect is less than one in 1,000.
What causes neural tube defects?
The cause of neural tube defects is not certain, but it appears to be due to a combination of genetic and environmental factors.
Women are at increased risk of having a baby with a neural tube defect if:
- they have already had a baby with a neural tube defect
- they or their partner have a close relative born with a neural tube defect
- they have type 1 (insulin dependent) diabetes (not gestational diabetes)
- they are obese, or take certain anti-epileptic medications, especially those containing sodium valproate or valproic acid
Prevention
About 2 in 3 neural tube defects can be prevented through increasing folate (folic acid) intake at least a month before pregnancy and during the first 3 months of pregnancy. Adequate folate levels are critical during the early days of the developing embryo, particularly the 3rd and 4th week, the period in which neural tube defects occur and when many women won't know they are pregnant.
Adequate folate levels are critical during the early days of the developing embryo, particularly the 3rd and 4th week, the period in which neural tube defects occur and when many women won't know they are pregnant.
You can increase your folate intake by eating folate-rich foods, including folate-fortified foods in your daily diet, or by taking a folic acid supplement. Good sources of folate include green leafy vegetables, fruit (citrus, berries and bananas), legumes and some cereals (bread and many breakfast cereals now have added folate).
Women who take medicines to control epilepsy, seizures or psychiatric disorders should talk to their doctor before taking folate because it can interfere with how their medications work.
For more information see folate and pregnancy.
Diagnosis
Neural tube defects may be diagnosed during the ultrasound scan that is carried out around week 12 of the pregnancy or, more likely, during the anomaly scan that is carried out at around weeks 18 to 20.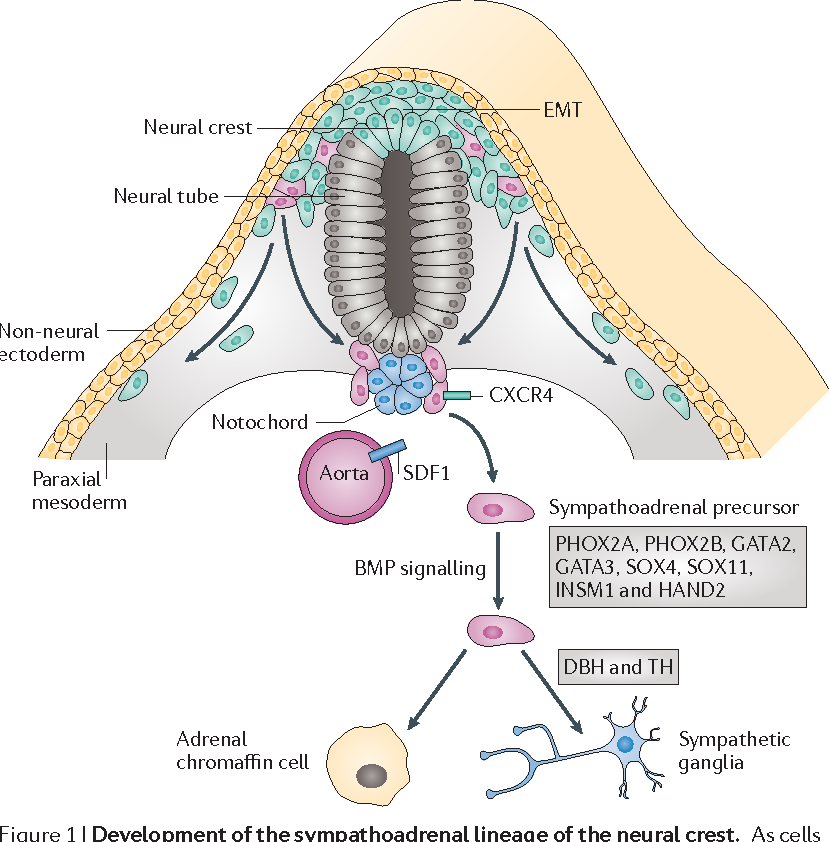
Ultrasound scans
An ultrasound scan is a safe procedure that uses sound waves to create an image of the inside of your body. Most hospitals will offer women at least 2 ultrasound scans during their pregnancy. The first is usually at around 8 to 14 weeks and is sometimes called the ‘dating scan’ because it can help to determine when the baby is due. This first scan may be able to detect problems with your baby’s spine that could indicate spina bifida if the condition is severe. If a dating scan is done earlier than 12 weeks, another ultrasound called the nuchal translucency scan is done at 12 weeks to check amongst other things for signs of Down Syndrome, and if a dating scan is not done prior to this then this scan can be used as the dating scan.
Morphology scan
The morphology or anomaly scan is an ultrasound scan that is carried out around weeks 18 to 20 of your pregnancy. This scan aims to identify any physical problems with your baby. It is usually during this scan that spina bifida is diagnosed.
Coping with the results
If tests confirm that your baby has spina bifida, the implications will be fully discussed with you. You will need to consider your options carefully. Your options are to:
- continue with your pregnancy while getting information and advice so that you are prepared for caring for your baby
- end your pregnancy
If you are considering ending your pregnancy, you should talk to your doctor or midwife. They will be able to provide you with important information and advice.
Your options for ending your pregnancy will depend on how many weeks pregnant you are when you make the decision. If you decide to end your pregnancy, you may wish to talk to a counsellor afterwards. Your doctor or midwife will be able to arrange this for you.
Call Pregnancy, Birth and Baby on 1800 882 436 to discuss your options regarding your pregnancy with a maternal child health nurse.
Sources:
Australian Institute of Health and Welfare (Neural tube defects in Australia), The Centre for Genetics Education (Neural tube defects – spina bifida and anencephaly), RANZCOG (Planning for pregnancy), Women's and Children's Health Network (Screening tests for neural tube defects), Sydney Children's Hospital Network (Factsheet: What is spina bifida?)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2020
Back To Top
Need more information?
Pregnancy checkups, screenings and scans
Knowing what check-ups, screenings and scans to have and when to have them during your pregnancy is important information for every pregnant woman.
Read more on Pregnancy, Birth & Baby website
Neural tube defects: children & teens | Raising Children Network
Neural tube defects are brain and spinal cord abnormalities, including spina bifida, encephalocele and anencephaly. Read how they affect children.
Read more on raisingchildren.net.au website
Folate and pregnancy
Folate and folic acid are important for pregnancy since they can help prevent birth defects known as neural tube defects, such as spina bifida.
Read more on Pregnancy, Birth & Baby website
Spina bifida
Spina bifida is a condition that affects the normal development of a baby’s spine early in pregnancy.
Read more on Pregnancy, Birth & Baby website
Spina Bifida | Sydney Children's Hospitals Network
Spina Bifida comes from a latin term which means “split spine”
Read more on Sydney Children's Hospitals Network website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Folic acid & iodine fortification, Summary - Australian Institute of Health and Welfare
Mandatory folic acid and iodine fortification of bread resulted in increased levels of folic acid and iodine in the food supply, increased folic acid and iodine intakes, a decreased rate of neural. ..
Read more on AIHW – Australian Institute of Health and Welfare website
Folate | Jean Hailes
Folate is a B vitamin needed for healthy growing, in particular for the nervous system.
Read more on Jean Hailes for Women's Health website
What supplements should I take during pregnancy? | Queensland Health
Find out what supplements and vitamins you need to take when trying to get pregnant, during pregnancy, after pregnancy and while breastfeeding.
Read more on Queensland Health website
Pregnancy at weeks 1 to 4
When you conceive, your body’s hormone levels change, but you may not notice any signs that you’re pregnant yet.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Fomina Clinic - a network of multidisciplinary clinics
We have already found out that when planning a pregnancy, the lifestyle of the expectant mother plays an important role, namely the rejection of bad habits, proper nutrition, hygiene and sports. Vitamins play an important role in this, namely folic acid, which is advised to start taking 1-3 months before the expected pregnancy. It is its use that prevents possible malformations that can lead to the death of the child. nine0003
This is a B vitamin that prevents fetal neural tube defects. Moreover, it is important to understand that such an effect is possible only if folic acid begins to enter the mother's body before pregnancy and continues to be taken during pregnancy. Thus, from the first days after conception, the child begins to develop in the right conditions, because by this time folic acid has time to get into your bloodstream in sufficient quantities.
Unfortunately not. The fact is that violations of the laying of the neural tube usually occur on the 18th - 30th day after conception, when a woman may still not know about her pregnancy. nine0003
Let's start with the statistics: neural tube defects (yes, there are several!) are found in about 7 out of 10,000 newborns, and it is believed that in half of these cases they are caused by a lack of folic acid in the mother's diet.
The two most common neural tube defects are:
- Spina bifida damages the spinal cord: with this defect, most children survive and reach adulthood, but they may be accompanied by central nervous system disorders throughout life, such as paralysis or inability to control urination and defecation; nine0020
- with anencephaly, the entire brain or a significant part of it is missing, in which case most children die shortly after birth.
Recommended foods include: Green vegetables, legumes (beans, peas, lentils), lettuce, berries, citrus fruits (fruits and juices), breakfast cereal, whole grain bread/bread.
This, of course, is not enough, because in most of these products the content of folic acid is less than 20% (or even 10%) of the recommended daily amount by doctors. The only exception is lentils, one glass of which contains 90%. Therefore, additionally every day when planning pregnancy and throughout its duration, you need to take vitamins that contain 400 mcg of folic acid.
Healthy women with normal pregnancy really need such a small dose, but there are preparations containing from 1 to 5 mg of folic acid. There are several "risk groups" to which they are prescribed:
- women who had a child with a neural tube defect from a previous pregnancy; nine0020
- diabetic women;
- women with elevated levels of homocysteine in the blood;
- women taking antiepileptic drugs.
If you recognize yourself in one of these groups, be sure to check with your doctor to discuss the need for higher doses of folic acid. But remember that more is not always better, and in this case, this common truth works.
Follow us
Spina bifida in children - treatment of pathology and features of the disease
On the basis of the N.N. Since 2015, G. I. Turner has been operating a specialized Center for the Treatment of Children with the Consequences of Spina bifida Spina Bifida, where an integrated approach to treatment is applied with the participation of an orthopedist, neurologist, neurosurgeon, urologist and psychologist.
We invite you to familiarize yourself with the description of the pathology and modern methods of treatment.
- What is Spina bifida? nine0020
- How does the disease develop?
- Classification and characterization of the most common forms of Spina bifida
- Clinical manifestations of the consequences of the disease Spina bifida
- Causes of Spina bifida
- Diagnostic Spina bifida
- Treatment of children with Spina bifida in Russia
Spina bifida: definition, prevalence of the disease in the world and in Russia
Spina bifida (Russian: Spina bifida, Latin: Spina bifida, English: split spine) is a congenital malformation of the spine and spinal cord, in which the arches of one or more vertebrae have not fused and, as a result, the spine remains "split". The spinal cord itself or various structures of the spinal cord and its membranes can protrude into the formed defect. The term Spina bifida was first used by N. Tulp in 1651 to describe the doubling of the spinous process of a vertebra as a manifestation of an anomaly in the development of the spine, but not the spinal cord. Despite the mere historical meaning of this term, it is still used to refer to the so-called spinal dysraphia - a group of diseases that are manifested by a violation of the formation of the spine and spinal cord. Spinal dysraphism (dys - violation + Greek rhaphē - seam), or Spina bifida, belongs to a group of diseases called neural tube defects (NTD), which also includes abnormalities in the development of the brain and skull. nine0003
In other words, Spina bifida encompasses a group of developmental defects of the spine, ranging from the rather "harmless" Spina bifida occulta (from Latin for "hidden"), which usually does not affect bodily functions, to severe myelomeningocele, which is characterized by severe impairment of motor and sensory the spheres of the lower extremities, as well as the pelvic organs - it is with this form that most people associate the concept of a spinal hernia or Spina bifida.
The incidence of the disease according to researchers in different countries is not the same and ranges from 0.1 to 5 cases per 1000 newborns. In Russia, this figure is 0.1-0.2% of all newborns. In the scientific literature there is an opinion that this malformation occurs more often in girls. nine0003
How does the disease develop?
In a normally developing human embryo, the central nervous system, which includes the brain and spinal cord, develops from a layer of cells that forms by the 2nd week of pregnancy and is called the neural plate. At the beginning of the 3rd week of embryo development, this plate thickens, forming a longitudinal groove. At week 4, the furrow deepens and folds develop on both sides of it, which eventually merge and form a closed tube. From this tube or cylinder, the brain and spinal cord subsequently develop. In parallel with this, muscles, the spine and the skull develop from the germ layers of the ecto- and mesoderm. These processes are based on complex mechanisms of cell differentiation and migration. nine0003
In Spina bifida and any neural tube defect, a certain part of the neural plate does not fuse into the cylinder and remains defective. If the neural tube has not formed correctly, then the surrounding tissues, including the skull and spine, will also be abnormal. The cavities of the brain produce cerebrospinal fluid, or cerebrospinal fluid, which washes and protects the nerve cells. This fluid normally circulates between the brain and spinal cord, passing through the foramen magnum, through which the brain passes into the spinal cord. Spina bifida is usually associated with an abnormal development of the brain and posterior cranial fossa or Arnold-Chiari type 2 anomaly. With this pathology, the structures of the brain stem, cerebellum, and fourth ventricle are displaced into the foramen magnum. In this case, a CSF circulation disorder may occur with the development of hydrocephalus and, as a result, damage to nerve cells as a result of an increase in intracranial pressure with possible complications in the form of convulsions, muscle spasticity and severe dysfunction of the brain stem, where the cardiovascular and respiratory centers are located. Such a condition often requires urgent surgical correction in the form of various shunting options in order to correct CSF flow. nine0003
Depending on the period of intrauterine development and the level of occurrence of the neural tube defect, the severity and variety of clinical manifestations will be determined. So, early damage to the upper end of the neural tube will lead to the development of anencephaly (absence of the brain), and the lower part - to myelomeningocele.
Classification and characteristics of the most common forms of Spina bifida
There are open and closed forms of Spina bifida or spinal dysraphism depending on the involvement of the skin in the pathological process and the connection of the structures of the spinal canal with the external environment. Open forms or Spina bifida include aperta/cystica when a hernial sac filled with CSF is formed in an existing skin defect. If there is only a dura mater in the hernial sac, this subtype of Spina bifida aperta is called meningocele , and if it contains the spinal cord itself, myelomeningocele , and its roots - myelomeningoradiculocele .
Closed forms of spinal dysraphism or Spina bifida occulta do not have a defect in the skin, but may be manifested by dysplastic changes on its surface in the form of nevi or local hypertrichosis. This form includes myelomeningocele . The higher the localization, the more severe the dysfunction of the organs and systems below. As a rule, this defect is most often localized in the lumbar region and leads to paresis and paralysis of the lower extremities, impaired urination and defecation. If the hernia is located in the thoracic regions, then neurological disorders are much more severe, up to complete immobility. A hernia of the cervical region is an indication for termination of pregnancy.
Meningocele occurs in 15-25 percent of cases and may not have a skin defect. At the same time, the absence of involvement of the spinal cord and its components in the defect may not lead to severe neurological deficit.
Latent forms of spinal dysraphism or Spina bifida occulta - the least severe variant of the disease. It may be asymptomatic and detected incidentally during radiological research methods. Sometimes it can give unpleasant symptoms in the form of periodic back pain, weakness in the legs or dysuric phenomena. nine0003
Clinical manifestations of the consequences of the disease Spina bifida
The variety of consequences of the disease occurs due to damage to the structures of the spinal cord and its roots, which leads to a violation of the sensitivity of the lower extremities and the inability to perform active movements due to the lack of muscle innervation below the level of the lesion with the development of flaccid or peripheral paralysis.
The level of the lesion determines the number of involved muscle groups of the lower extremities and the degree of motor disorders of the locomotor apparatus, manifested from barely noticeable gait disturbances to complete absence of movements. nine0003
Muscle imbalance or complete absence of muscle contractile activity (flaccid paralysis) causes the formation of contractures in the joints of the extremities, leads to the development of bone deformities, to dislocations and subluxations in the joints. The most common orthopedic problems are dislocations/subluxations of the hip joints, flexion contractures in the knee joints, dislocations of the bones of the lower leg, foot deformities in the form of clubfoot, plano-valgus deformity, equinus deformity, calcaneal-valgus deformity, etc.
Associated spinal malformation can cause severe deformities such as lordosis of the lumbosacral spine and kyphoscoliosis, often requiring surgical correction.
These orthopedic problems can cause gait disturbance, make it difficult to wear orthoses, and cause the development of trophic disorders of the skin of the lower extremities.
Decrease in axial load and ability to move against the background of impaired innervation of the extremities leads to the development of osteoporosis with the risk of pathological fractures of the bones of the lower extremities. nine0003
Violation of the innervation of the muscles of the pelvic organs increases the risk of urinary tract infections and the development of chronic renal failure.
Causes of the disease Spina bifida
Spina bifida is a multifactorial disease, but has no reliable cause. The following factors increase the likelihood of developing Spina bifida:
- genetic;
- alcohol;
- intoxication;
- intrauterine infection of the fetus at an early stage; nine0020
- ionizing radiation;
- folate deficiency;
- taking anticonvulsants early;
- taking cytostatics;
- obesity;
- diabetes mellitus with hyperglycemia (slightly compensated).
Diagnosis of Spina bifida
Modern diagnostic methods make it possible to detect Spina bifida in early pregnancy. Screening ultrasounds are performed for women in each trimester of pregnancy. In the first trimester, already from the 12th week, ultrasound diagnostics can reliably detect this pathology. nine0003
Comprehensive newborn screening programs are carried out at the Consultative and Diagnostic Center (Lakhtinskaya St.