Peeing while giving birth
Surprising Things That Happen During Labor and Delivery
As the saying goes, the only thing you can predict about giving birth is that it will be unpredictable. And some of those unexpected things include bowel movements and plenty of bodily fluids. If you happen to let loose in front of a doctor, nurse or midwife, don’t give it a second thought. “Nothing surprises us. Nothing fazes us,” says Jane Martin, MD, an OB with Midtown Ob/Gyn who practices at Rose Medical Center in Denver. “Childbirth is the most natural thing your body can do, and whatever your body does in the process is nothing to feel embarrassed about.” Besides, as you’ll see here, you’re not alone: Plenty of others have gone through exactly the same thing.
Pooping
“When I was close to delivery, I was on my hands and knees, sort of pushing to see if baby was ready to move down yet. Every time I would do that, I would poop. My midwife wiped my crack every time.” —MamaB
This is some women’s biggest fear, but pooping during labor is no big deal. With all that pushing—you’re expelling a whole human being from your body—it’s almost inevitable. Plus, says Martin, “When you poop when you push, it means you’re using the right muscles. When you’re pushing from elsewhere, it’s not as effective.”
Losing the Mucus Plug
“I was induced, and my doctor checked me after a dose of Cervidil. When she pulled her hand out, my mucus plug was hanging from her finger. The nurse finally said, ‘You’ve got a dangler!’” —MaryF
The mucus plug has an important purpose. The thick membrane builds up at your cervix and covers the opening to your uterus to block bacteria. As your cervix starts to efface or dilate, it gets pushed out. Sometimes it happens before labor and other times during it. Sometimes it’s a small discharge; sometimes it’s bigger. It’s all part of the process. Don’t worry about it.
Peeing on Yourself
“After I gave birth, the nurses told me to hit the call button when I had to pee and they’d help me. They came in and stood me up—I was still numb from the epidural—and I heard all this fluid hitting the floor. I was peeing all over the place!” —KrystalD
They came in and stood me up—I was still numb from the epidural—and I heard all this fluid hitting the floor. I was peeing all over the place!” —KrystalD
It’s not uncommon at all to temporarily lose bladder control post-baby. That’s because during a vaginal delivery, the pelvic floor muscles get stretched out. Until they start to tighten up again—a process you can speed along with Kegel exercises—you might have some leaks. In addition, with an epidural, you can temporarily not be able to feel that your bladder is full.
Water Breaking
“My water didn’t just break—it exploded! It kept coming in gushes, and when we got to the hospital, I was soaked right down to my shoes. I gushed and squished all the way down the hall.” —BeckyM
About 10 percent of women experience a rupturing of the amniotic sac before labor. For everyone else, it happens during labor, either naturally or with some help from the doctors. If your water breaks on its own, it could be a trickle or a huge gush. “Some women will carry a towel with them to the office,” says Martin. “It will definitely freak out some of your colleagues, but if your water breaks, you’ll be glad you have it.”
“Some women will carry a towel with them to the office,” says Martin. “It will definitely freak out some of your colleagues, but if your water breaks, you’ll be glad you have it.”
Vomiting
“After my c-section, I was so nauseated from the meds. I was on a liquid diet that day and was only able to keep down some grape juice. I was holding my new son and puked all over the place. My mom, mother-in-law, husband and friend were all in the room. The vomit was bright purple.” —KateB
For some moms, pain meds can make you queasy, and it’s especially common when you take them after a c-section. Vomiting can also happen when you progress really quickly in labor. “It’s just a stimulus response to baby moving quickly through the birth canal,” says Martin. Nausea can also happen with blood pressure fluctuations. Don’t be shy—ask the nurse to keep something close by for you to throw up in. Remember, they really are used to all this.
Passing Gas
“After I got my epidural, I had zero control from the waist down, so two nurses were trying to help me roll over to my other side to help speed things along. I totally farted in one of the nurses’ faces.” —DianeS
I totally farted in one of the nurses’ faces.” —DianeS
Some people notice they have more gas when they’re pregnant or when they get close to delivery, says Martin. “It’s all part of the baby pushing on everything,” she explains. “Lots of people do it and it is nothing to be embarrassed about.”
Postbirth Bleeding
“When I went to visit the babies in the NICU, I had bled through my pad and mesh undies and had a stain the size of a dinner plate on my behind while walking around. I didn’t know until I got back to my room.” —JennaB
Bleeding is natural. The uterus bleeds from where the placenta used to be attached, explains Martin. It can be a very heavy period, except it’s not predictable. You can think it’s over, but then it might pick up again. It’s normal for it to last as much as six weeks. In the meantime, avoid tampons (it’s an infection risk) and stock up on really thick, absorbent pads.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Surprise! Good Things Happen During Labor, Too
Biggest Labor and Delivery Fears
8 Surprising Things That Happen After Labor and Delivery
Signs You Are Going Into Labor
Not every woman will experience labor and delivery in the exact same way. This can make it difficult to explain when a person will know that they are in labor if they have never experienced such an occurrence before. Thankfully, there are a few signs and symptoms that all women can consistently look for in the first few days prior to going into labor.
If you are experiencing the early signs of labor call All About Women OB/GYN to discuss your symptoms with your obstetrician. Your obstetrician will evaluate your symptoms and recommend the best course of action.
Book Your Appointment Online
Call us at (703) 437-0001
Your Cervix Begins to Thin
As your uterus prepares for delivery, it will start to stretch in order to create a thinner cervix that will dilate more easily. This process is known as effacement, and will gradually occur during the last few weeks of pregnancy.
This process is known as effacement, and will gradually occur during the last few weeks of pregnancy.
You’re No Longer Short of Breath
While your baby is growing larger, it is perfectly normal for them to press on nearby internal organs and bodily structures, including your diaphragm. Contractions of the diaphragm are what allow all of us to breathe in and out. Naturally, when a growing fetus begins to push against the diaphragm, the muscle is no longer able to expand quite as far as it used to, leaving many expectant mothers out of breath.
If you notice that your breaths are suddenly able to be much deeper and longer, it most likely means that the baby has dropped. This happens when the fetus is getting close to making their way through the birth canal, meaning that labor is getting closer.
It is also common for women to experience more intense pressure on their bladder once their baby drops, so you may also notice increased discomfort in this area along with more frequent urges to urinate.
You Have So Much More Energy
Lots of friends and family members have probably been asking if you have begun to nest yet. All of these questions are related to this one particular symptom.
When the nesting stage takes hold, many women will experience a sudden burst of energy. This often motivates them to complete a whole slew of tasks such as cleaning, buying needed supplies and baby clothes, and any other preparation that still has to get done before baby arrives.
All of this is happening because your body intrinsically knows that your baby will soon be on the way, so it’s instinct to want to run around and take advantage of this newfound energy. Try to remind yourself that the biggest hurdle has yet to come, and you will need all the extra energy that you can get once you actually start to go into labor. Rather than taking on your to-do list all at once, start with just a few simple tasks at a time to make it easier on yourself in the long run.
Your Mucus Plug Pops
Once the baby is ready to make their exit, the thick plug of mucus that protects the opening of the cervix will start to break down. This allows the cervix to begin opening freely so that the baby will be able to make their way out of the uterus during delivery.
This allows the cervix to begin opening freely so that the baby will be able to make their way out of the uterus during delivery.
Technically, to say that this plug “pops” is not entirely correct. Instead, this symptom will appear as a clear, pink, or slightly bloody discharge. Not all women will notice the loss of their mucus plug, so don’t worry if this particular sign of labor seems to pass you by.
Your Water Breaks
Perhaps the most noticeable sign of labor, the breaking or leaking of the amniotic sac is a symptom that all women look for when questioning whether or not they may be about to go into labor. Unfortunately, even this sign is not always crystal clear as only 10% of pregnant women will experience the kind of dramatic scenario we often see in movies.
More often, women will notice a small trickle of fluid that is similar to urination. It is also not uncommon for urine to actually leak from the bladder due to the pressure being placed on it during the last few days leading up to labor. In order to differentiate between amniotic fluid and urine, you will need to determine if the fluid has an odor. If there is no smell, then it is likely that your amniotic membranes have ruptured slightly, meaning your water has broken.
In order to differentiate between amniotic fluid and urine, you will need to determine if the fluid has an odor. If there is no smell, then it is likely that your amniotic membranes have ruptured slightly, meaning your water has broken.
You’re Starting to Dilate
Before the baby is able to pass through the birth canal, the cervix must open further and further until it is wide enough to allow a child through. This process is called dilation, which is measured in centimeters. Once a woman’s cervix has dilated to 10 centimeters she is considered fully dilated and ready to give birth.
It is important to remember that you cannot measure the dilation of your cervix on your own. This will need to be evaluated by your obstetrician.
You Experience Consistent Contractions
No matter what signs of labor you have or have not noticed up to this point, you will definitely know that you are in labor once your uterus begins to contract in a persistent pattern. It is important to track how close together your contractions are, as their duration and spacing will help determine just how close you actually are to delivering.
It is important to track how close together your contractions are, as their duration and spacing will help determine just how close you actually are to delivering.
Many women’s contractions will begin by being 20-30 minutes apart. This time between contractions will gradually shorten, and once she has reached 5 minutes or less between contractions it is time to call the hospital and prepare for the baby’s birth.
Urination in newborns - how it should be | Mamovediya
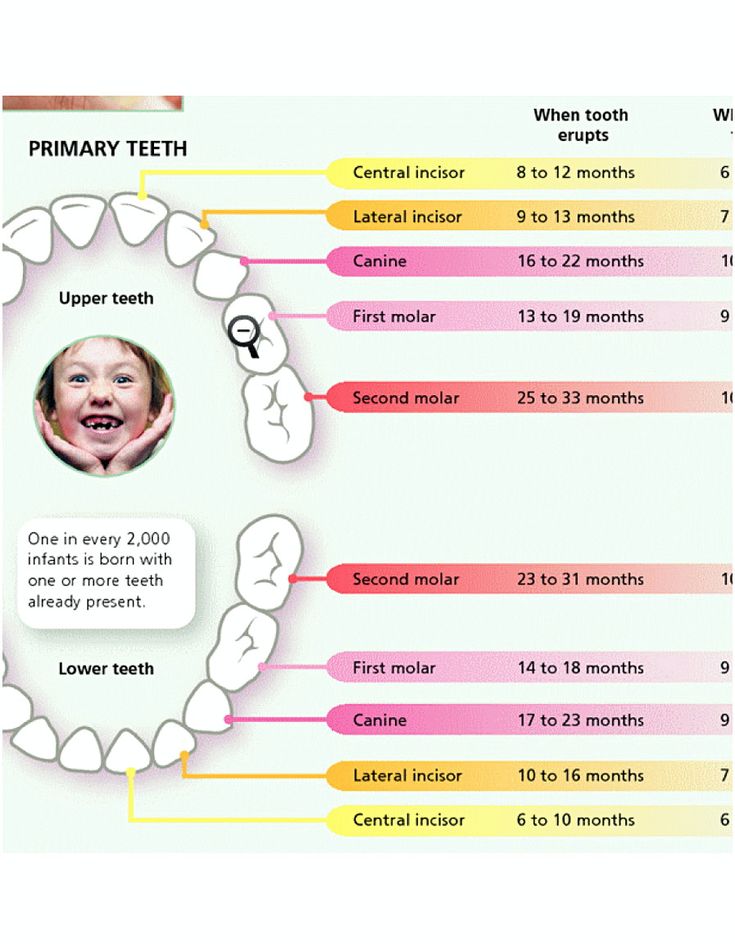
For the first time, a child urinates sometimes during childbirth, and sometimes immediately after them. In general, the first urination in newborns occurs in the first 12 hours of life. However, in every 10th child, it can occur only on the 2nd and even on the 3rd day.
Therefore, if you gave birth at home and it so happened that the baby does not pee, wait 2-3 days after giving birth. If the situation has not changed during this time, invite a doctor. nine0003
Newborns produce little urine in the first 3 days of life, although their urinary system is well formed. What is the matter here has not been definitively established. But, of course, a certain role is played by the fact that the child outside the womb excretes water with the entire surface of the body, and so far receives little liquid.
What is the matter here has not been definitively established. But, of course, a certain role is played by the fact that the child outside the womb excretes water with the entire surface of the body, and so far receives little liquid.
Reduced urine output in newborns in the 1st week of life is called transient oliguria (Greek oligos - few, insignificant).
In the same week, all newborns develop another transitional state - uric acid infarction, which externally manifests itself as an unusual yellow-brick color of urine. It is cloudy and leaves a correspondingly colored stain on the diaper. By the end of the week, urine acquires its natural color and transparency.
The frequency of urination in full-term newborns in the 1st week of life is 4–5, and in preterm infants 8–13 times a day.
Usually, in healthy children, by the end of the 1st week, the daily urine output reaches an average of 209±26 ml. If by this time it is significantly less than the age norm (for example, it is only a third of it), you should observe the baby.
Reduced urine output is not always associated with kidney, bladder or ureter disease.
A child may develop a high temperature (38-39°C) if they are dressed too warmly, lying next to a radiator, or the room is very hot, all of which can lead to decreased urine output.
The same result occurs with a disorder of the stool - diarrhea, which is accompanied by large losses of fluid. nine0003
However, if the child is not overheated and his stools are normal, you should see a doctor.
The unusual color of urine should also alert you. It can be concentrated - very yellow. At the same time, diapers are also painted yellow, and the skin of the child in the place where the urine has got turns pink. An increased concentration of urine can be caused by the fact that the baby is not getting enough liquid. In this case, he needs to give more to drink.
If he drinks a lot and his urine is still concentrated, you should consult your doctor. nine0003
Newborns rarely experience acute urinary retention in the first days. At the same time, the bladder is full of it, stretched and clearly visible above the womb. Sometimes it even reaches the level of the navel.
At the same time, the bladder is full of it, stretched and clearly visible above the womb. Sometimes it even reaches the level of the navel.
The reasons for this may vary, but in any case, the baby will need urgent medical attention.
A combination of two symptoms may serve as a reason for an urgent visit to a doctor: 1) the child has not urinated for 2-3 days and 2) his bladder is empty. nine0016
Anuria, a severe disease characterized by such a combination of symptoms, can soon lead to a sharp deterioration in the child's condition. He will turn pale, become drowsy and lethargic, and will refuse to eat. Further, convulsions, coma are possible. Anuria is treated exclusively in a hospital.
In some pathologies of the urinary system, blood is found in the urine of a newborn. This symptom may also be associated with other diseases, such as hemorrhagic disease of the newborn. nine0003
However, the urine may turn reddish after taking certain drugs. Therefore, after consulting a doctor, you can not give the child medicine for some time to find out if it is to blame.
Therefore, after consulting a doctor, you can not give the child medicine for some time to find out if it is to blame.
Quite rarely, in children in the first days of life, signs of hereditary metabolic pathologies may appear. At birth, the baby looks quite healthy, but after a few days (and more often months) he becomes drowsy and lethargic, he has vomiting, convulsions. And at the same time, an unusual smell of urine and body appears. It is associated with the smell of mice, sweaty feet, mustiness, maple syrup, rotting fish
You should consult a doctor without delay, because the treatment of hereditary fermentopathies, in order to be effective, must be started in the neonatal period, and the sooner the better. Otherwise, as a rule, the mental development of the baby suffers. And often the course of the disease acquires a life-threatening character.
Sometimes it happens that the diaper on which the child urinates, when dry, turns black as pitch. Urine acquires the same color when standing. This is a sign of another hereditary fermentopathy - alkaptonuria. Often the disease does not give other symptoms. However, over time, alkapton (black pigment) can accumulate in the cartilage of the nose and ears, and then in the joints, the mobility of which will decrease because of this. nine0003
Urine acquires the same color when standing. This is a sign of another hereditary fermentopathy - alkaptonuria. Often the disease does not give other symptoms. However, over time, alkapton (black pigment) can accumulate in the cartilage of the nose and ears, and then in the joints, the mobility of which will decrease because of this. nine0003
The disease is treatable if treated early.
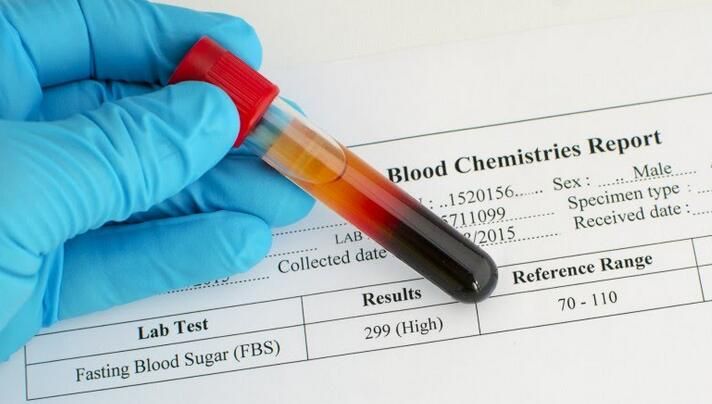
Congenital diabetes mellitus, which is extremely rare in newborns, is characterized by characteristic signs. The child sucks a lot and greedily, urinates often and profusely, the diaper, having dried, becomes hard, as if starched.
The child may quickly develop a diabetic coma. Therefore, with such symptoms, you need to urgently consult a doctor.
It is important to pay attention to the color, consistency and turbidity of the baby's urine. It should be fairly clear and light, not cloudy, not orange or red. nine0003
Postpartum hygiene
Congratulations! You have become a mother!
The postpartum period is no less important and responsible stage in the life of a family than pregnancy.
The postpartum period lasts 6-8 weeks (begins after the birth of the placenta and ends when the organs and systems that have changed during pregnancy return to their original state).
In the process of healing the inner surface of the uterus, postpartum discharge appears - lochia, which is a wound secret. Their character during the postpartum period changes: in the first days, lochia has a bloody character; from the 4th day, their color changes to reddish-brown; by the 10th day they become light, liquid, without blood, and after 3 weeks there is practically no discharge. There may be discomfort due to uterine contractions. To relieve discomfort, bend forward and gently massage your belly. If discomfort in the uterine area occurs during feeding, try choosing a different position. It is convenient to feed lying on your side. The stomach may ache for another reason. It hurts the abdominal muscles that were actively involved during childbirth, try to relax or do a light massage. nine0077 In most non-nursing women, menstruation occurs on the 6-8th week after childbirth, more often it comes without the release of an egg from the ovary. However, ovulation and pregnancy may occur during the first months after childbirth. In lactating women, the time of the onset of the first menstruation after childbirth can be delayed for many months.
nine0077 In most non-nursing women, menstruation occurs on the 6-8th week after childbirth, more often it comes without the release of an egg from the ovary. However, ovulation and pregnancy may occur during the first months after childbirth. In lactating women, the time of the onset of the first menstruation after childbirth can be delayed for many months.
The normal postpartum period is characterized by a good general condition of the woman, normal temperature, sufficient lactation. For the prevention of infectious complications, strict adherence to sanitary and epidemiological requirements and personal hygiene rules is important. nine0003
POSTPARTUM HYGIENE
Strict cleanliness is essential.
- The mother should take a shower twice a day (in the morning and in the evening), then wash the mammary gland with soap and brush her teeth.
- Particular attention should be paid to the cleanliness of hands. Nails should be cut short, hands should be washed more often with soap and be sure before each feeding of the child (if the hands are dirty, you can infect the child, infect the nipples).
 nine0089
nine0089 - Among the hygienic measures of particular importance in the postpartum period is the maintenance of cleanliness of the external genitalia and the surrounding skin.
- Should be washed with warm water and soap (liquid with a dispenser, because microbes feel great on lumps) with a fluid stream, washing the genitals should be from front to back (from the pubis to the anus) after each visit to the toilet at least 4-5 times a day (you need to go to the toilet exactly at such a frequency that the filled bladder does not interfere with uterine contraction). nine0077 Wash hands cleanly before washing.
- Keep the pads clean, change them every 3-4 hours, regardless of fullness. Remove pads from front to back to prevent microorganisms from entering the vagina from the anus. If there are seams on the perineum, they should be washed thoroughly enough - you can simply direct a jet of water at it. After washing, you need to dry the perineum and the seam area by blotting the towel from front to back.
 nine0089
nine0089 - Do not take a bath for the first 6 weeks after giving birth. This is due to the fact that the entrance to the vagina is not yet closed enough and pathogenic microbes can penetrate into it along with water. It is clear that at this time you can not swim in the pool, river, lake, sea.
- The use of tight underwear is strictly excluded, as it puts significant pressure on the perineum, which disrupts blood circulation, preventing healing.
- If there are stitches on the perineum, a woman should not sit down for 7-14 days (depending on the degree of damage). At the same time, you can sit on the toilet already on the first day after childbirth. By the way, about the toilet. Many women are afraid of severe pain and try to skip bowel movements, as a result, the load on the muscles of the perineum increases and the pain intensifies. nine0089
To avoid constipation after childbirth, do not eat foods that have a fixative effect. If the problem of constipation is not new to you, drink a tablespoon of vegetable oil before each meal. The stool will be soft and will not affect the healing process of the stitches.
The stool will be soft and will not affect the healing process of the stitches.
- Underwear and bed linen must be cotton. We change underwear daily, bedding - at least once every three to five days.
- Stitches after caesarean section do not require special care. After the stitches and bandage are removed, you can take a shower. Do not scrub the seam area with a washcloth. With painful sensations in the anterior abdominal wall, a postpartum or postoperative bandage, which must be worn for 4 months, will help to cope. Young mothers are often interested in: will the seams come apart if you carry a baby in your arms? For the first 2-3 months after surgery, it is recommended to lift no more than your child's weight. nine0089
It happens that redness, irritation, bloody or purulent discharge occurs at the suture site. This indicates suppuration or divergence of the seams. Then you should immediately consult a doctor in a antenatal clinic.
Sexual life after childbirth can be resumed after 6-8 weeks. By this time, the woman's body is already completely back to normal. Your doctor will advise you on contraceptives.
By this time, the woman's body is already completely back to normal. Your doctor will advise you on contraceptives.
To fully recover from childbirth, at least two years must pass before the next pregnancy. nine0003
BREASTFEEDING
Feeding the baby should not go by the clock, but on demand, incl. at night time. At one feeding, put the baby on one breast so that he suckles for a long time and receives later milk, which contains brain and intelligence development factors, growth factors and immunoglobulins. Later, the milk comes in droplets like colostrum, the child sucks it intermittently. Sometimes the mother at this moment thinks that the child is indulging and tearing him off the breast. You don't need to do this. Let him let her go. nine0077 Breast milk is the best food for a baby!
- After the baby has had enough, the mother should carefully feel the mammary gland. If the breast is soft and there is no soreness and seals anywhere, then pumping is not necessary.
 If necessary, you can wash the mammary glands with warm water after feeding, starting from the nipple and ending with the armpit, and dry with a clean towel.
If necessary, you can wash the mammary glands with warm water after feeding, starting from the nipple and ending with the armpit, and dry with a clean towel.
Very useful for the breasts after childbirth and air baths, which are best taken after feeding, to give the breast a chance to rest, "breathe". The duration of such an air bath may not exceed 15-20 minutes, but the benefits of it are enormous. nine0003
- The nipple should be carefully inspected daily, the surface of which should not be cracked, and as a preventive measure, leave a drop of milk on the nipple and let it dry in the open air.
Only breast milk should be used as the main and only product for feeding a newborn. The use of nipples, horns and "pacifiers" is unacceptable, as this leads to a weakening of sucking in newborns and, accordingly, to incomplete emptying of the mammary gland, a decrease in prolactin production. nine0077 Are you worried about the question - do I have enough milk?
To resolve this issue, you need to observe the child, if he urinates more than 6 times a day, then he receives a sufficient amount of milk. The reason for the decrease in the amount of milk can be:
The reason for the decrease in the amount of milk can be:
- rare feeding break (3 or more hours)
- if you do not feed at night
- short feedings or by the hour
To increase the amount of milk, you need to rearrange the feeding regimen, feed often and for as long as you want child. Try to feed with one breast so that the baby sucks out milk later, you can strain the empty breast for 10 minutes, thereby increasing the flow of milk. It is necessary to improve the mother's nutrition or use herbal teas to increase lactation. nine0003
NUTRITION
Nutrition of a nursing mother should be high in calories (3200 kcal), balanced with the proper amount of proteins, fats, carbohydrates, vitamins and microelements. This diet will be dominated by lactic acid, protein foods, fresh fruits and vegetables. Food should be rich in vitamins and minerals. Spicy, fatty, fried, smoked foods, canned food, sausages, alcohol and potential allergens for the child (chocolate, citrus fruits, coffee) should be excluded from the diet. nine0077 The food of the puerperal should be 5-6 times a day. It is necessary to distribute products in the daily menu in such a way that those that are rich in protein and are much more difficult to digest in the gastrointestinal tract (meat, fish, cereals) would be used during the first half of the day, and in the second half it is advisable to give preference to milk. - vegetable food.
nine0077 The food of the puerperal should be 5-6 times a day. It is necessary to distribute products in the daily menu in such a way that those that are rich in protein and are much more difficult to digest in the gastrointestinal tract (meat, fish, cereals) would be used during the first half of the day, and in the second half it is advisable to give preference to milk. - vegetable food.
Conditions requiring special attention
Unfortunately, the first month after childbirth does not always go smoothly. Situations may arise, when medical attention is needed . Monitor your well-being, regularly measure your body temperature, as fever is most often the first sign of complications in the postpartum period.
All complications of the postpartum period can be divided into several groups:
1. Complications of the uterus.
Subinvolution of the uterus - a decrease in the rate of contraction of the uterus, due to a delay in the uterus of postpartum discharge. The disease often occurs 5-7 days after childbirth, due to the closure of the cervical canal with a blood clot or a piece of membranes, as well as the inflection of the uterus due to relaxation of the ligamentous apparatus. nine0077 Infection of the contents of the uterus can lead to inflammation of the uterine mucosa - endometritis. Predisposing factors for the occurrence of endometritis are difficult childbirth, violations of the separation of the placenta during childbirth, infections of the genital tract during pregnancy, impaired immunity, abortion. Symptoms of the disease are: fever, unpleasant odor in lochia, aching pain in the lower abdomen. If these symptoms appear, you should consult an obstetrician-gynecologist at the place of residence. To clarify the diagnosis, an ultrasound examination is performed and, if necessary, surgery, during which the contents are removed from the uterine cavity (washing or curettage of the uterus). After surgery, antibiotics must be prescribed. nine0003
The disease often occurs 5-7 days after childbirth, due to the closure of the cervical canal with a blood clot or a piece of membranes, as well as the inflection of the uterus due to relaxation of the ligamentous apparatus. nine0077 Infection of the contents of the uterus can lead to inflammation of the uterine mucosa - endometritis. Predisposing factors for the occurrence of endometritis are difficult childbirth, violations of the separation of the placenta during childbirth, infections of the genital tract during pregnancy, impaired immunity, abortion. Symptoms of the disease are: fever, unpleasant odor in lochia, aching pain in the lower abdomen. If these symptoms appear, you should consult an obstetrician-gynecologist at the place of residence. To clarify the diagnosis, an ultrasound examination is performed and, if necessary, surgery, during which the contents are removed from the uterine cavity (washing or curettage of the uterus). After surgery, antibiotics must be prescribed. nine0003
2. Breast complications.
Breast complications.
Laktostasis - stagnation of milk in the mammary gland. At the same time, the chest swells and becomes painful, foci of seals appear, a short-term rise in body temperature is possible. In itself, lactostasis is not a disease, requiring only gentle pumping of the breast, restriction of fluid intake, and frequent feeding of painful breasts. However, when an infection joins, it turns into lactational mastitis, requiring immediate medical attention , antibiotic therapy, and sometimes surgery. The question of the possibility of breastfeeding with mastitis is decided individually, depending on the stage of the disease.
Another complication of the breast is the appearance of cracks in the nipples. The main reason for their appearance is improper attachment of the baby to the breast, when the baby captures only the nipple, and not the entire areola. Such a seizure is very painful for the mother - and this is the main danger signal. Breastfeeding doesn't have to be painful. Good advisory and practical help for lactostasis and cracked nipples is provided by breastfeeding consultants. Treatment of cracks consists in treating the nipple with wound healing drugs. nine0077 Hypogalactia - insufficient milk production. In order to increase the amount of milk, a mother needs to increase the frequency of feedings, not skip night feedings, offer her baby both breasts in one feeding, drink more, eat well and sleep a lot.
Breastfeeding doesn't have to be painful. Good advisory and practical help for lactostasis and cracked nipples is provided by breastfeeding consultants. Treatment of cracks consists in treating the nipple with wound healing drugs. nine0077 Hypogalactia - insufficient milk production. In order to increase the amount of milk, a mother needs to increase the frequency of feedings, not skip night feedings, offer her baby both breasts in one feeding, drink more, eat well and sleep a lot.
3. Complications from the tissues of the cervix, vagina and skin.
Inflamed wounds of these tissues are called postpartum ulcers. When an infection is attached, these wounds swell, become covered with a purulent coating, and their edges are painful. For the purpose of treatment, they are treated with various antiseptics, sometimes they require surgical treatment. nine0003
4. Complications of the venous system.
Hemorrhoids (varicose veins of the rectum) also cause pain. When infringed, they increase, become swollen, tense and painful. Thorough hygiene helps to reduce pain (shower after each visit to the toilet), applying ice to the perineum. Certain medications can be used as prescribed by a doctor.
When infringed, they increase, become swollen, tense and painful. Thorough hygiene helps to reduce pain (shower after each visit to the toilet), applying ice to the perineum. Certain medications can be used as prescribed by a doctor.
Thrombophlebitis is a disease of the veins characterized by inflammation of the venous wall and thrombosis of the vein. After childbirth, thrombophlebitis of the pelvic veins most often occurs. Usually this disease occurs in the third week after childbirth. In terms of symptoms, it is very similar to endometritis, but requires a different treatment. Surgeons are involved in the treatment of complications from the venous system. nine0077 Complications after childbirth require immediate treatment, as they can lead to a generalization of the process - postpartum peritonitis or sepsis. Therefore, if something bothers you in your condition, be sure to consult a doctor.
You must come to the antenatal clinic for the first time 10 days after discharge from the maternity hospital.