Pcos pregnancy chance
How to Get Pregnant with PCOS
Polycystic ovary syndrome, or PCOS, is a hormonal condition that tampers with more than just your fertility, but you might first receive a diagnosis when you’re trying to get pregnant. This is because it’s a common — and treatable — cause of infertility in women.
According to the Centers for Disease Control (CDC), up to 12 percent of women in the United States have difficulty getting pregnant because of untreated PCOS. In reality, this number might be bigger because almost 50 percent of women with this syndrome don’t know they have it or are not diagnosed correctly.
Having PCOS doesn’t mean you can’t get pregnant. It just might be a bit trickier and you may need extra help. There is plenty that you can do at home and with medical treatment to keep PCOS symptoms at bay and raise your chances for a healthy pregnancy.
Getting pregnant with PCOS involves some of the same steps that women without PCOS should take for a healthy pregnancy.
- Have your weight and body mass index (BMI) measured by your doctor. Your BMI shows whether you have a healthy body weight and how much of your body composition is fat. If you are carrying extra weight, talk to your doctor about how much weight you need to lose before you get pregnant.
- Start a healthy diet and exercise plan. Get into the habit of choosing healthier food choices and being more active.
- Use an ovulation calendar or app to track when you have your period. This helps you make a better guess about which days of the month you are more likely to get pregnant.
- Check your blood sugar levels. See your doctor to make sure your blood sugar levels are balanced. Your blood sugar levels are important in getting pregnant, having a healthy pregnancy, and even in your baby’s future health.
Being overweight has been linked to PCOS, but many women who have this condition are not overweight at all. Still, if you are carrying extra weight, you may improve your fertility and reduce other PCOS symptoms by losing just 5 percent of your weight.
Still, if you are carrying extra weight, you may improve your fertility and reduce other PCOS symptoms by losing just 5 percent of your weight.
Exercise daily by going for a walk and getting in your steps. Use a standing desk rather than sitting down while you’re working. Lift light weights while watching TV as building more muscle helps bring down PCOS symptoms and improves your health.
Any woman who is trying to get pregnant needs to have the right levels of nutrients. Switch out sugary foods, simple carbs, and unhealthy fats for healthier choices, including:
- fresh and cooked fruit and vegetables
- whole grains like brown rice, oats, and barley
- beans and lentils
- chicken
- fish
Certain vitamins and minerals are important for a healthy pregnancy and a growing baby. Ask your doctor about the best supplements for you. Supplements that may help fertility include:
- folic acid (vitamin B9)
- vitamin B6
- vitamin B12
- vitamin C
- vitamin D
- vitamin E
- coenzyme Q10
Your doctor will test your blood sugar levels if you’re having trouble getting pregnant. PCOS sometimes leads to high blood sugar levels or type 2 diabetes. This may cause fertility problems.
PCOS sometimes leads to high blood sugar levels or type 2 diabetes. This may cause fertility problems.
This happens because PCOS may change how your body uses insulin. This important hormone moves sugar (glucose) out of the blood and into the muscles and cells where it is burned for energy. PCOS makes your body less sensitive to insulin — making it harder for it to do its job.
Balancing your blood sugar levels may help you get pregnant. Eat a healthy diet with more fiber, protein, and healthy fats. Getting plenty of daily exercise and strength training can also help your body use insulin better.
In some cases, your doctor might recommend medications to help balance your blood sugar levels. A common type 2 diabetes drug called metformin (or Glucophage) makes your body use insulin better to help lower high blood sugar. This can also help you get pregnant with PCOS.
You might need to take metformin in low doses and only temporarily, depending on your blood sugar levels.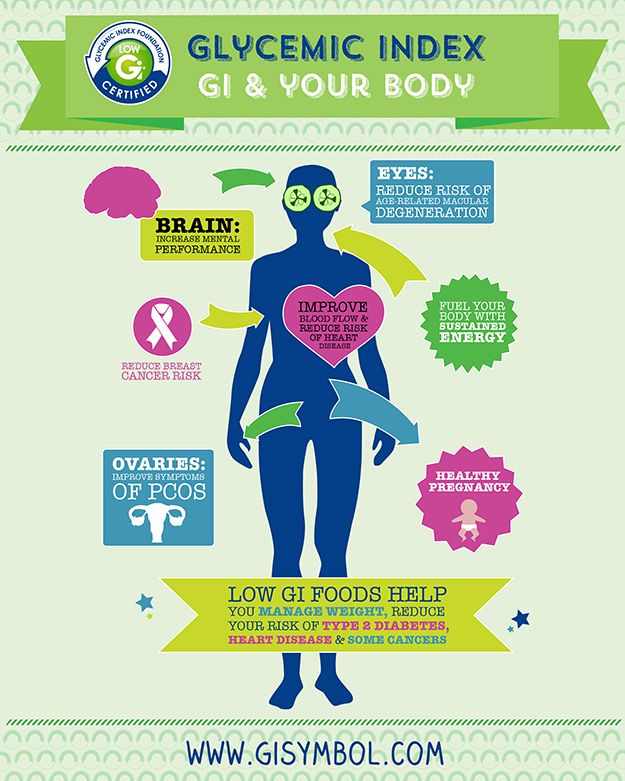 For best results, eat a healthy diet and exercise regularly along with taking any prescribed medications to help you get pregnant.
For best results, eat a healthy diet and exercise regularly along with taking any prescribed medications to help you get pregnant.
If you have high blood sugar levels or type 2 diabetes, it’s important to check your blood sugar levels with a home monitor every day.
Your doctor will check your blood sugar levels with tests, including:
- random blood sugar test
- overnight fasting blood sugar test
- oral glucose tolerance tests (after fasting and drinking a sugary drink)
- hemoglobin A1C test (checks your blood sugar levels for the last two to three months)
If you have PCOS your body might make more of both the male hormone testosterone and the female hormone estrogen. Too much (or too little) of these hormones can make it tricky to get pregnant. Your doctor might recommend prescription medications to help balance your hormones.
Medications to help you get pregnant with PCOS include:
- metformin to balance insulin levels
- clomiphene citrate (or Clomid) to help balance estrogen levels
- birth control pills to balance estrogen and testosterone levels (before beginning fertility treatment)
- fertility medications to jump-start the ovaries to send out more eggs
You may need in vitro fertilization (IVF) treatment to help you get pregnant with PCOS.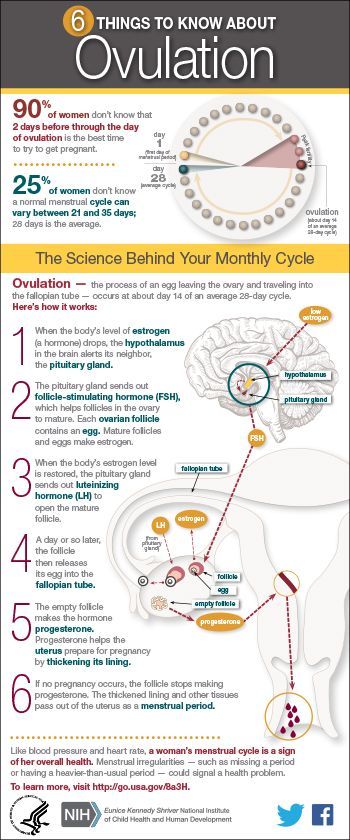 Your fertility doctor will give you a checkup that may include more blood tests, ultrasounds scans, and a physical exam.
Your fertility doctor will give you a checkup that may include more blood tests, ultrasounds scans, and a physical exam.
IVF is a process that can take months or even years whether you have PCOS or not. However, medical research shows that women with PCOS have a high success rate of getting pregnant with IVF treatment.
Some clinical studies found that women with PCOS who took birth control pills before the IVF treatment had better results. You may also need other mediations to help balance hormones and get your body ready for the IVF treatment.
For all women, the first step in IVF treatment is to eat a balanced diet and get plenty of exercise to reach a healthy weight. Women with PCOS who are a healthy weight are twice as likely to get pregnant with IVF than women with PCOS who are obese.
Before exploring IVF, your doctor might suggest a less-costly alternative called intrauterine insemination (IUI). This process increases the chance of pregnancy because it directly injects a high concentration of sperm closer to the egg.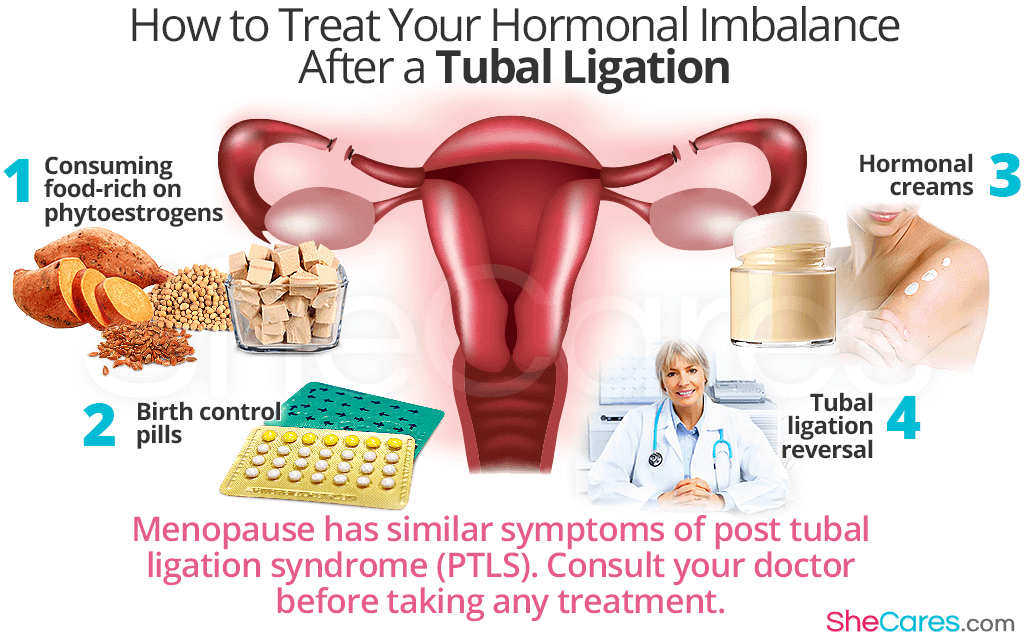
PCOS may make it harder to get pregnant because it can impact your menstruation cycle (your monthly period). Symptoms include:
- too few menstrual periods
- having your period for longer than usual
- not getting your period
- very heavy periods
- higher levels of male hormones like testosterone
- acne breakouts
- getting facial hair and extra hair in other places
- small cysts or bundles of fluid in the ovaries
- fewer eggs released from the ovaries
If you don’t get treated for PCOS, it also raises your risk for other health conditions, like:
- type 2 diabetes
- sleep apnea (snoring)
- heart disease
- high blood pressure
- high cholesterol
- stroke
No one knows why some women get PCOS. Nothing you did — or didn’t do— caused you to have this condition. But getting an early diagnosis and treatment along with making other lifestyle changes may help you get pregnant and prevent health complications from PCOS.
If you are trying to get pregnant with PCOS, you may only need treatment with medications. A medical study found that almost 80 percent of women with PCOS treated with the drug clomiphene citrate successfully ovulated. Out of these, half of the women got pregnant naturally within six period cycles.
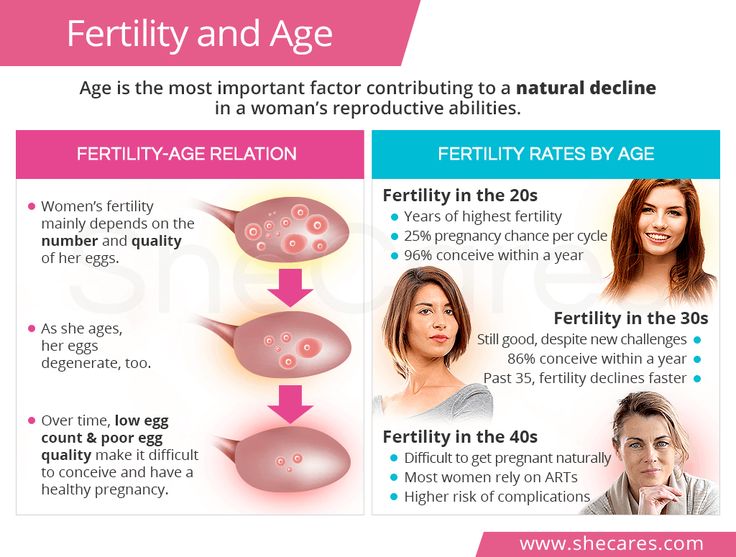
If medications don’t help you get pregnant, your doctor may recommend IVF treatments. Most women with PCOS have a 20 to 40 percent chance of getting pregnant with IVF treatment. Women who are 35 years old and older or who are overweight have a lower chance of getting pregnant.
You can get pregnant with PCOS. You will likely need to have moderate weight, balance your blood sugar levels, and treat other PCOS symptoms with healthy lifestyle changes and medications.
In some cases, fertility medications alone will help you get pregnant. If that doesn’t work, you may need IVF treatment.
But regardless of what treatment you explore, don’t lose hope. Success rates are optimistic. In time you may be smiling, positive pregnancy test in hand.
In time you may be smiling, positive pregnancy test in hand.
How to get pregnant with PCOS — Flo.Health
If you’ve been diagnosed with polycystic ovary syndrome (PCOS), one of the first things you might have heard about the condition is that it can make it harder to get pregnant. Although that can be true for some, it doesn’t make it impossible — far from it.
If you’re looking for advice on how to conceive with PCOS, you’ve come to the right place. From lifestyle changes to tried-and-tested fertility interventions, there are a range of ways you can boost your chances of getting pregnant. Let’s find out how with a little help from a professor of obstetrics, gynecology, and reproductive sciences.
Getting pregnant with PCOS: Why is it harder?
It’s true that for some people with PCOS, getting pregnant can take a little longer. That’s because PCOS — a common hormonal disorder that affects around one in ten women of reproductive age — can make some people ovulate irregularly, or not at all.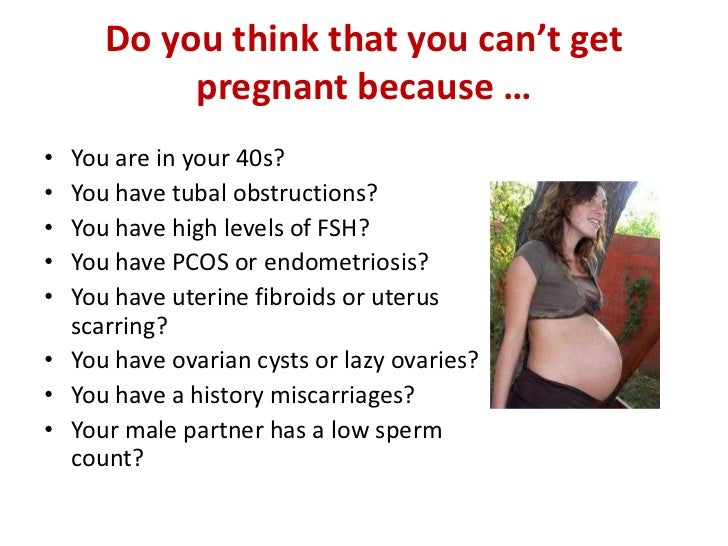 As ovulation (the monthly release of an egg) is a vital part of getting pregnant, this irregularity can make things tricky — but more on that below.
As ovulation (the monthly release of an egg) is a vital part of getting pregnant, this irregularity can make things tricky — but more on that below.
Take a quiz
Find out what you can do with our Health Assistant
Scientists still aren’t exactly sure what causes PCOS, but they believe you’re more likely to develop it if it runs in your family or if you have insulin resistance.
While it’s named polycystic ovary syndrome, confusingly, you don’t always develop polycystic ovaries if you have PCOS. Instead, you may be diagnosed with PCOS if you have two of the following three symptoms:
- Irregular or missed periods
- A high level of “male” hormones, called androgens (which can cause excessive hair growth on the body and face, as well as acne and thinning of hair on the head)
- Polycystic ovaries, which occur when small egg sacs on the ovaries become filled with fluid, known as cysts
But back to how all this can affect your chances of getting pregnant. Lubna Pal, professor of obstetrics, gynecology, and reproductive sciences at Yale School of Medicine, explains that “in order for pregnancy to happen, you need to have an egg that is released from your ovaries [once a month].”
Lubna Pal, professor of obstetrics, gynecology, and reproductive sciences at Yale School of Medicine, explains that “in order for pregnancy to happen, you need to have an egg that is released from your ovaries [once a month].”
After ovulation, an unfertilized egg stays in the uterine tubes for 12 to 24 hours before it dissolves and is shed as part of a period. If it’s fertilized by sperm before then, however, it can lead to a successful pregnancy. But if you’re not having regular periods, it means you’re probably not ovulating regularly either. As a result, Pal explains, “the probability of conception goes down.”
That’s not the only way PCOS may impact getting pregnant, however. One theory that’s been researched suggests that PCOS can cause hormonal imbalances that change the quality of your cervical fluid, making it harder for sperm to survive.
Further research shows that being overweight may play a role in hormonal disorders like PCOS, which can in turn affect fertility. For example, being overweight is linked to anovulation (when an egg isn’t released during your menstrual cycle), menstrual disorders (such as heavy bleeding and painful cramps), and difficulties with assisted reproduction (like IVF). However, it’s important to note that not everyone who has PCOS is overweight, and many people who are overweight ovulate without a problem.
For example, being overweight is linked to anovulation (when an egg isn’t released during your menstrual cycle), menstrual disorders (such as heavy bleeding and painful cramps), and difficulties with assisted reproduction (like IVF). However, it’s important to note that not everyone who has PCOS is overweight, and many people who are overweight ovulate without a problem.
There’s also the link between infertility and stress to consider. PCOS and stress are known to be associated. One Iranian study, albeit a small one, found that just over 90% of women with PCOS displayed some level of stress. As Pal explains, stress along with a fluctuation in weight (both gain and loss) can alter the signaling of an important cycle-related hormone called the gonadotropin-releasing hormone (GnRH). “There are so many factors that can mess up the GnRH, which then translates into menstrual irregularity,” Pal says. “It’s like a 1,000-piece jigsaw puzzle. ”
”
Despite the numerous ways PCOS can impact your ability to get pregnant, Pal advises that there are ways to try and work around it. “It’s about finding the right strategy that works for you,” she explains.
How much harder is it to get pregnant with PCOS? The statistics
We know that PCOS affects around one in ten women of reproductive age. Of these, 70% to 80% don’t always release an egg (ovulate) during their menstrual cycle, making conception impossible in these months. This might sound like a high figure, but it’s believed that most women with PCOS will eventually be able to get pregnant if they manage the condition with treatment.
One person who’s part of that statistic is Stephanie, 35, who says she has “always wanted to be a mum” for as long as she can remember. But following a checkup with her health care provider, after noticing a heavy and irregular cycle, stomach cramps, excessive hair growth, and weight gain, Stephanie was diagnosed with PCOS.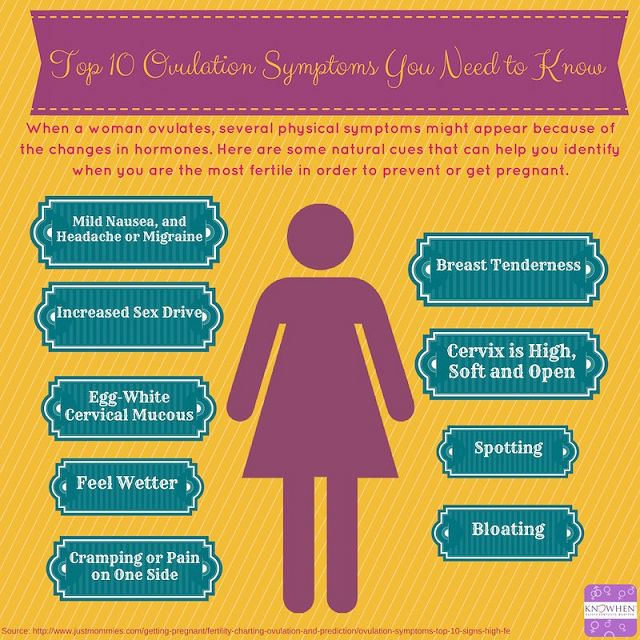 A scan later found large cysts on her ovaries, and, insensitively, she was told it was “highly unlikely” she would conceive naturally.
A scan later found large cysts on her ovaries, and, insensitively, she was told it was “highly unlikely” she would conceive naturally.
“It was gut wrenching,” she recalls. “I have always had a motherly instinct, so when you’re told that it may never happen, it sends you on a downward spiral.”
At the time, Stephanie was 27, weighed over 260 lb. (120 kg), and wasn’t actively trying to have a baby. But she still knew that one day she wanted to become a mother. After talking to her health care provider, she was placed on a contraceptive pill to help regulate her heavy and irregular cycle. She was also referred to a weight specialist, all of which eventually helped Stephanie to become pregnant when the time was right.
Is it possible to get pregnant with PCOS quickly?
When you decide you want to have a baby, it’s normal to feel like you want it to happen immediately. With a condition like PCOS, things can be a bit more complicated, but it is possible to get pregnant with PCOS quickly if you manage your health properly. Having said that, there’s no real metric for what “quick” is, apart from your own personal timeline, so try to keep that in mind if you decide you want to start trying.
Having said that, there’s no real metric for what “quick” is, apart from your own personal timeline, so try to keep that in mind if you decide you want to start trying.
“Probably 60% plus can achieve spontaneous ovulation through improved lifestyle and weight loss over a span of a few months,” says Pal. In that instance, provided you have one egg and your partner’s sperm is good quality, “success rates go back to what they are for an ovulatory woman [without PCOS].”
This was the case for Stephanie, who is now a very proud mom to her two-and-a-half-year-old son. “When I did conceive, it was a complete and utter shock. It took four pregnancy tests and a scan to make me believe [I was pregnant],” she says.
Since managing her symptoms, Stephanie now has a more regular cycle and a lighter flow, and her ovarian cysts have shrunk. Increasing the amount of exercise she did, along with steady weight loss, also had some part to play. “I looked at it like a lifestyle choice,” she says.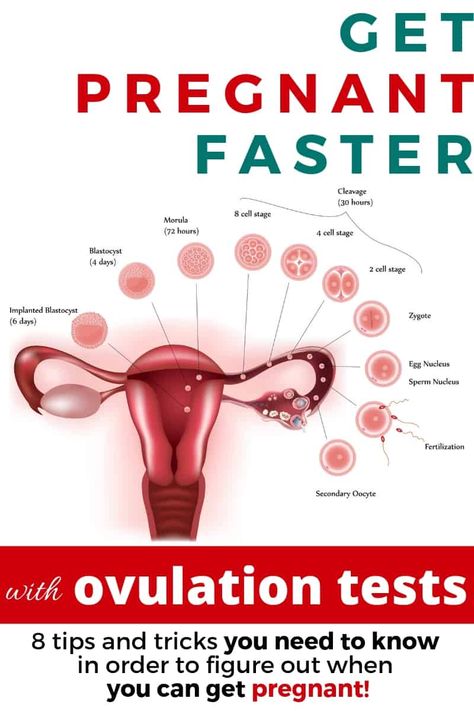 “I changed my eating habits, and they have continued to change. I do a lot of walking — I’m up to 10 km a day sometimes, and walking also helps mentally, as well as with weight loss.”
“I changed my eating habits, and they have continued to change. I do a lot of walking — I’m up to 10 km a day sometimes, and walking also helps mentally, as well as with weight loss.”
At the time of her diagnosis, Stephanie recalls that she had “given up hope of having children.” But when the time was right for her to get pregnant, and with the help of a weight specialist, it was something that fortunately happened for her. “I can’t imagine life without my son now,” she says.
We know weight loss isn’t always easy, especially if you have other factors at play, like hormonal imbalances. But the good news is that it doesn’t always require dramatic weight loss to make a difference. “All it takes is a loss of 5% of your excess weight” to improve the likelihood of getting pregnant, says Pal.
Of course, weight loss won’t be the necessary solution for everyone with PCOS who wants to have a baby. If lifestyle changes haven’t proven successful, or perhaps aren’t needed if you’re already active and maintain a balanced diet, a health care provider might recommend medication such as letrozole or clomiphene to help trigger ovulation.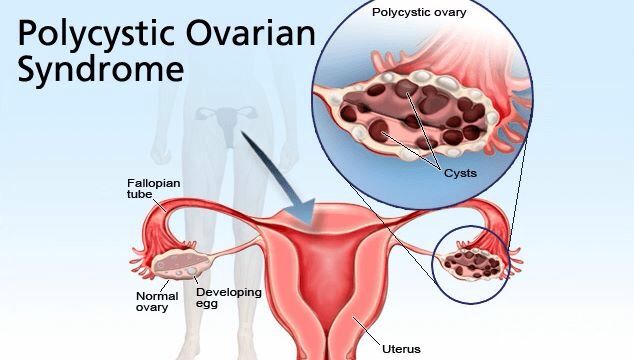 These oral pills are taken in short doses at the beginning of each menstrual cycle, usually for a number of cycles.
These oral pills are taken in short doses at the beginning of each menstrual cycle, usually for a number of cycles.
If these options don’t work, intrauterine insemination (IUI), also known as artificial insemination, may be suggested to help you conceive. This is where sperm is inserted into the uterus in an attempt to cause fertilization. Alternatively, in vitro fertilization (IVF) is another fertility treatment your health care provider may suggest next, which involves your egg being fertilized in a lab and then transferred into your uterus. You can read more on how that works here.
Tips for getting pregnant with PCOS
As we’ve seen, there are various ways to try to get pregnant with PCOS, ranging from lifestyle changes to medical help. But there are some other things you can do to boost your chances of conceiving with PCOS, such as:
1. Track your menstrual cycle
Whether you have regular periods every month or more unpredictable, irregular bleeds, it’s always worth monitoring your cycle to better understand the way your body works better. A period-tracking app like Flo can help here, improving your chances of getting pregnant by predicting when you’re likely to be ovulating — even if you have an irregular cycle. Sign up here.
A period-tracking app like Flo can help here, improving your chances of getting pregnant by predicting when you’re likely to be ovulating — even if you have an irregular cycle. Sign up here.
2. Give yourself the best possible chance
Wondering what’s the best age to get pregnant with PCOS? Generally speaking, for women under the age of 35, you have about a 25% chance of conceiving in the first month of trying and around an 85% chance in the first year.
Fertility and age go hand in hand. As we age, fertility declines because of a decrease in egg count and in egg quality. Studies have shown that for women aged 35 to 39 years old, the chances of conceiving spontaneously are about half that of women aged 19 to 26 years.
As we’ve seen, for those living with PCOS, getting pregnant can take a little bit longer, which is why it’s probably best not to delay the process if possible. “The longer you wait, the more emotional angst there is,” Pal explains. “This can cause more irregularity of periods. It becomes a catch-22.”
“This can cause more irregularity of periods. It becomes a catch-22.”
That said, having a baby is a big decision, so it’s important that you feel ready. Having open conversations with your health care provider to find out all the information you need or reaching out to support services can make a huge difference.
3. Pay attention to the preconception phase
The preconception phase is defined as the three months before you conceive — and it’s more important than you might think. In fact, Pal says, “Ideally in utopia, we’d all be paying attention to the preconception phase.”
Why? Well, a few lifestyle changes before actively trying can make all the difference to your chances, according to the Centers for Disease Control and Prevention. They recommend eating a healthy, balanced diet, drinking less alcohol, and exercising regularly to help prepare your body for getting pregnant.
Taking 400 mcg of folic acid every day is a good idea too, as studies have shown this B vitamin to be “fundamental for growth, especially in the embryonic and fetal stages.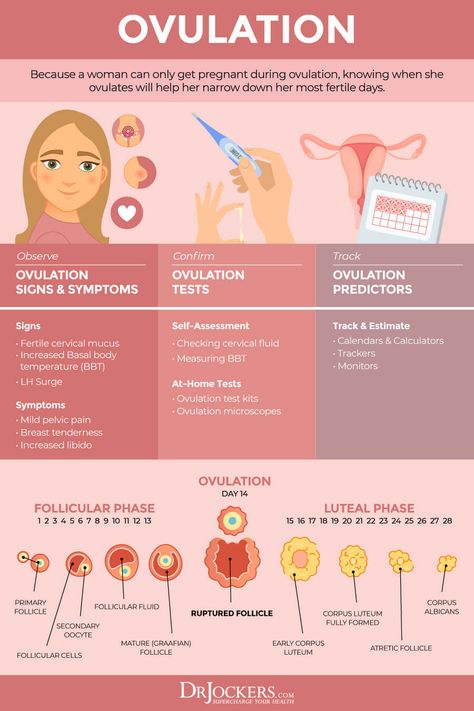 ” Prenatal vitamins that include iron, calcium, and zinc are also advisable as these minerals are crucial to support pregnancy.” Some prenatal vitamins also contain folic acid, so we’d recommend speaking with your doctor first to make sure you’re not doubling up.
” Prenatal vitamins that include iron, calcium, and zinc are also advisable as these minerals are crucial to support pregnancy.” Some prenatal vitamins also contain folic acid, so we’d recommend speaking with your doctor first to make sure you’re not doubling up.
4. Optimize your vitamin D levels
Vitamin D may well play a part in your journey to becoming a parent, too. According to Pal, a deficiency in vitamin D has been linked with “ovulatory dysfunction,” which is the word given to abnormal, irregular, or absent ovulation.
“Women with PCOS have a high prevalence of vitamin D deficiency,” says Pal, and science agrees. One study found around 67% to 85% of those living with PCOS to be vitamin D deficient. What scientists aren’t sure about just yet is whether or not you’re more likely to ovulate regularly with PCOS if you have sufficient levels of vitamin D. Regardless, the American College of Obstetricians and Gynecologists still recommends that vitamin D deficiency is treated while you’re trying to conceive and during pregnancy.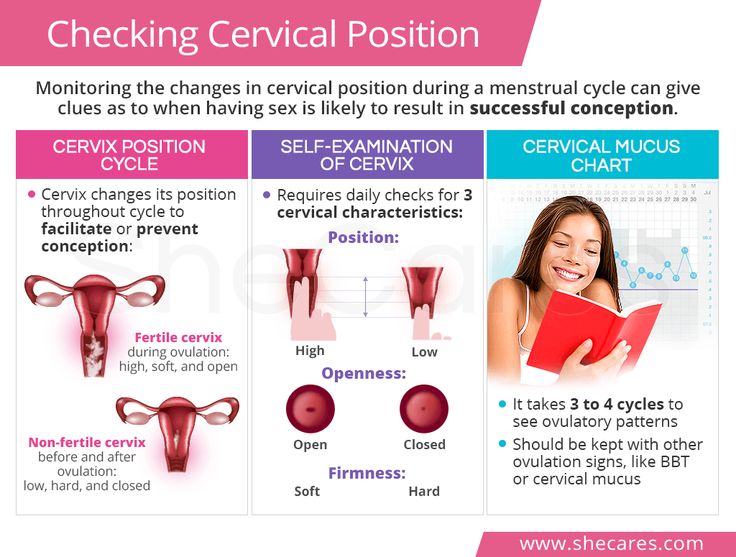
5. Get your partner checked
Pal says it’s easy to forget that “pregnancy is a team sport.” So don’t just assume PCOS is the reason it’s not happening for you. Schedule an appointment to get your partner’s sperm checked. As we’ve learned, in order for conception to happen naturally, an egg needs to be fertilized by a sperm. But if the sperm is not strong enough to meet the egg, or if your partner has a low sperm count, it “decreases the odds” that this will happen.
One-third of infertility cases are actually caused by male reproductive issues and could be related to issues including:
- Low (or no) sperm production
- Varicocele (which is an enlargement in the veins in the scrotum that results in a reduction of size and amount of sperm being produced)
- Imbalances in the “male” reproductive hormones (usually due to issues with hormone-producing glands)
How to get pregnant with PCOS: The takeaway
Remember: In many cases, having PCOS doesn’t mean you can’t start a family. Living with PCOS essentially means there are some factors that can make it harder to get pregnant. But, like with any health concern, it’s important to speak to your health care provider because everyone’s experience is different, and there are plenty of treatment options.
Living with PCOS essentially means there are some factors that can make it harder to get pregnant. But, like with any health concern, it’s important to speak to your health care provider because everyone’s experience is different, and there are plenty of treatment options.
“In some ways, PCOS is a label that acts as an alert to say, ‘Hey, be vigilant,’” Pal notes. “If infertility is your concern, use the information to maximize your well-being. Don’t be concerned about it. Just go and seek help because it’s easily, easily surmountable.”
One person who knows that to be true is mom-of-one Stephanie. Her key piece of advice? “Don’t give up hope,” she says. “Seek help and guidance from wherever possible, and don’t ignore it. I am so thankful and grateful for my little boy. It can happen for you; just don’t give up.”
Written by Rebecca Shepherd
Fomin's clinic — a network of multidisciplinary clinics
Today's world is full of information: literally with one click, each of us can open the Universe and learn everything - from string theory to concert posters for the next week.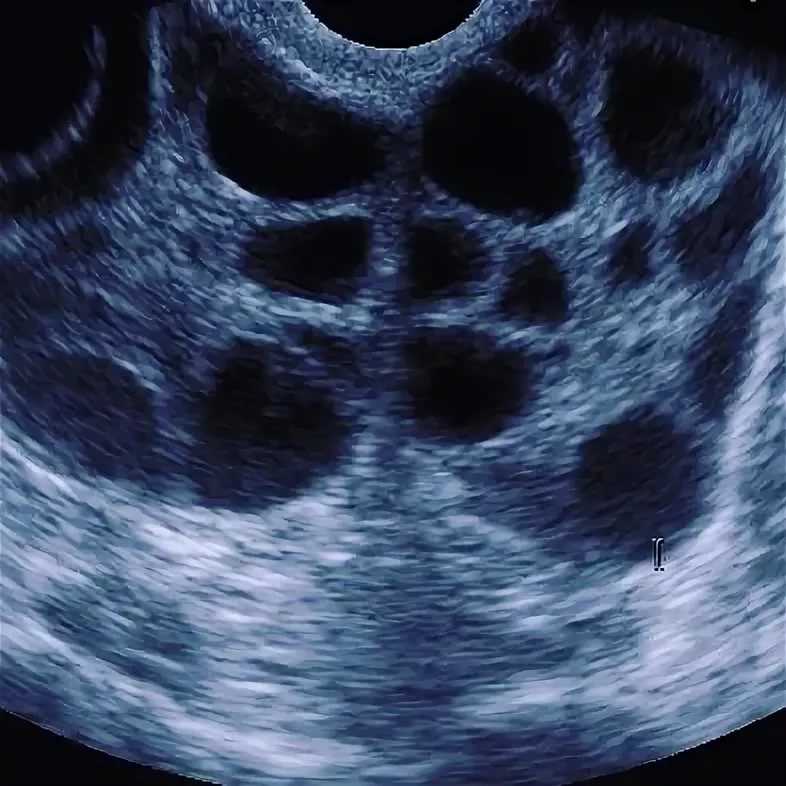 It is all the more interesting that, having unlimited access to knowledge, we still live in myths - and sometimes they arise, including thanks to the Internet, replicating untruth and absurdity.
It is all the more interesting that, having unlimited access to knowledge, we still live in myths - and sometimes they arise, including thanks to the Internet, replicating untruth and absurdity.
We have prepared for you a short “blitz” of six questions or myths about pregnancy and conception, so that you are fully equipped and do not believe the tales on the Internet.
Well... not exactly. Firstly, the idea of a “full examination” is a clear exaggeration, because there is no single list of tests that an expectant mother needs to pass. Ideally, visit a doctor three months before the end of contraception, get tested for STIs and antibodies to rubella. If additional examinations are required, you will be individually prescribed everything you need - including, probably, vaccinations that should be “updated”. As for alcohol and smoking, they are really contraindicated at the stage of pregnancy planning, so if you have these addictions, you will have to give them up.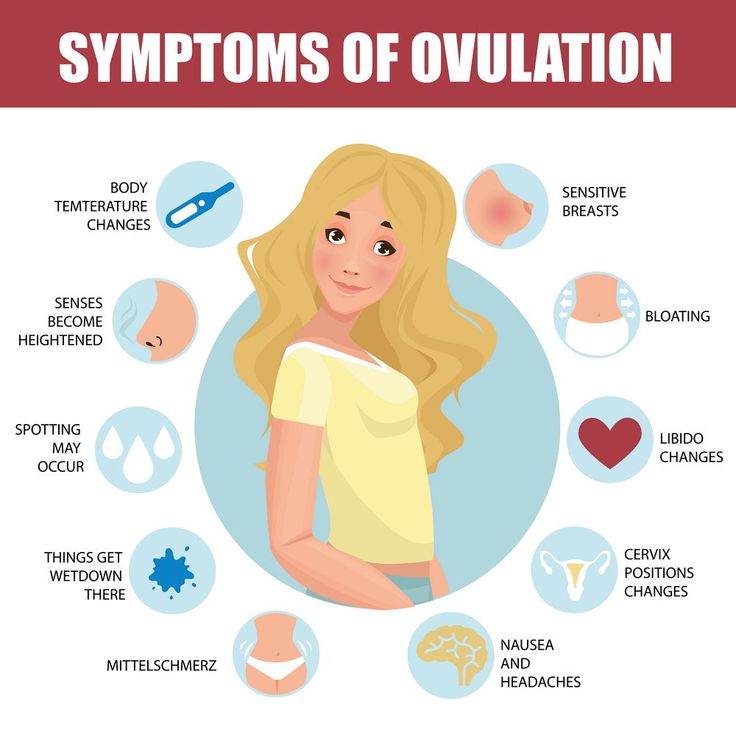 However, it should be remembered that smoking cessation applies to both electronic cigarettes and “passive smoking”, which can lead to dangerous consequences for the fetus.
However, it should be remembered that smoking cessation applies to both electronic cigarettes and “passive smoking”, which can lead to dangerous consequences for the fetus.
Spoiler: no big deal. Do not panic and blame yourself for all mortal sins because of a glass of wine. With the recognized insecurity of alcohol, scientists have proven that a woman drinking 1-2 servings a couple of times a week should not harm the unborn child. For men, the allowable figures are slightly higher - 3-4 doses of alcohol per week. The main thing is to know the measure and not to overdo it.
There is, of course, a simplified formula for calculating the estimated due date: plus 7 days and minus 3 months from the date of the last period, but to be honest, it doesn’t work like that: the fact is that it is very difficult to “program” pregnancy and make sure that the child is born when you want. If you have a plan and are going to stick to it, be prepared for the fact that things can go wrong, if only because:
- the duration of pregnancy is not 40 weeks, but 37-42 weeks, which means that you can easily fall into a five-week “loop”, which will reduce the chances of fulfilling the plan to zero;
- with regular sex, the probability of conception is not 1 time per month (exactly when you guessed it), but 1 time per year.
Nothing is impossible... However, it is worth clarifying the question a little: you can get pregnant only during ovulation (more precisely, shortly after it), but you can have sex, which will lead to a long-awaited pregnancy, on different days. Of course, on the days of menstruation, the probability is lower than on the days that precede ovulation, but on none of the days of the menstrual cycle this probability is not zero.
Let's just say that trying multiple times a day is a bad idea. Why? At least because ejaculation more than once a day worsens the quality of sperm, as a maximum - such perseverance and zeal can create tension in the relationship of partners. Doctors advise to have sex every 2-3 days throughout the cycle, and not try to guess the moment and throw all your strength into this short period.
Planning the sex of a child is an extremely prolific topic for myth-makers. Some believe that with the help of a special table that takes into account such indicators as the age of the father and mother, the month of conception, it is possible to accurately calculate the sex of the child. This "method" is anti-scientific and has nothing to do with reality.
Some believe that with the help of a special table that takes into account such indicators as the age of the father and mother, the month of conception, it is possible to accurately calculate the sex of the child. This "method" is anti-scientific and has nothing to do with reality.
Another myth is that you have to get pregnant on the day you ovulate to have a boy. Previously, scientists really believed that X and Y spermatozoa differ from each other (Y are faster), and the sex of the child is formed due to the first one that broke through the defenses of the female egg. If you want to conceive a boy, you need to have sex on the day of ovulation so that the Y-sperms responsible for the "male sex" have more time to get to the egg located farthest from the entrance to the uterus.
However, this myth does not stand up to criticism: the fact is that there is no difference between the X and Y chromosomes, which means that the sex of the child does not depend on which of the sperm reaches the egg first.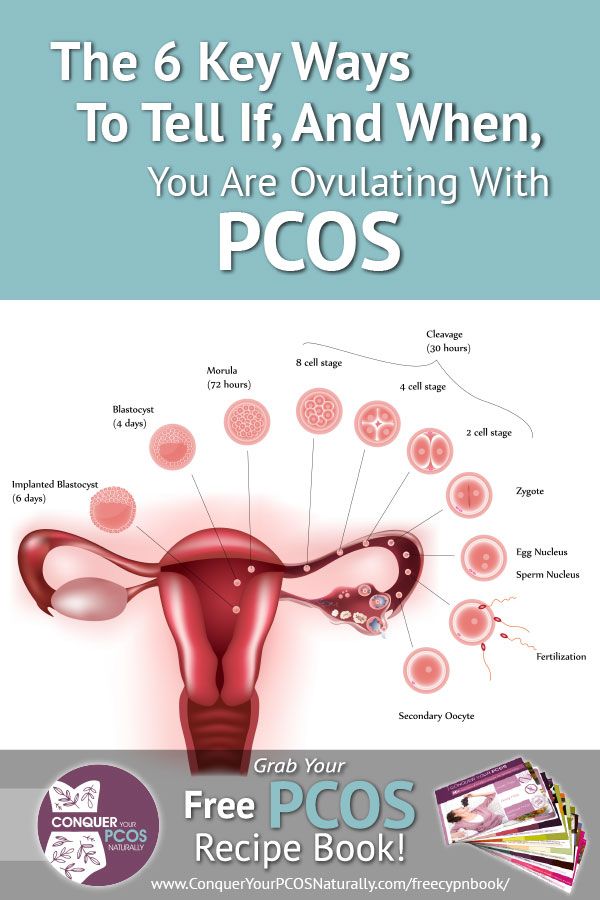 Moreover, not the fastest fertilizes the egg: thousands of spermatozoa simultaneously break its shell.
Moreover, not the fastest fertilizes the egg: thousands of spermatozoa simultaneously break its shell.
From this follows the conclusion: modern science does not know how to determine the sex of the child during natural conception, and therefore there is no universal recipe.
Follow us
ᐈ Why can't get pregnant - Reproductive medicine, gynecology, pregnancy monitoring, urology
At a certain moment in life, we feel an irresistible desire to become the parents of our baby. For some couples, this happens immediately, while others plan to continue the family for a certain period of life.
What if after a while pregnancy does not occur? Women begin to worry, and a question or even a problem arises - “I can’t get pregnant, what should I do?”. First, figure out if you are doing everything right.
First of all, it is extremely difficult to conceive the first time. To get pregnant, you need to have regular sex without using contraceptives.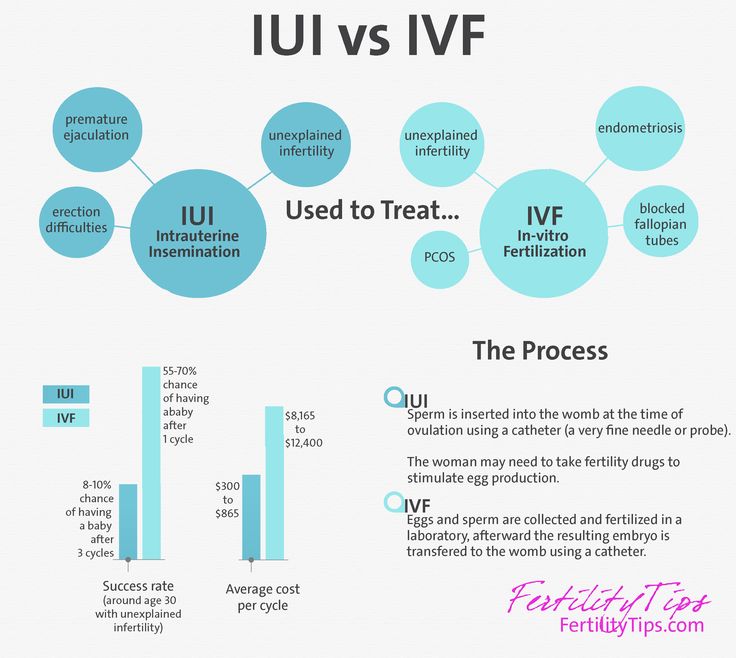 Secondly, this should be done on time, or rather, on the days of ovulation (fertile period).
Secondly, this should be done on time, or rather, on the days of ovulation (fertile period).
Reasons why you can't get pregnant
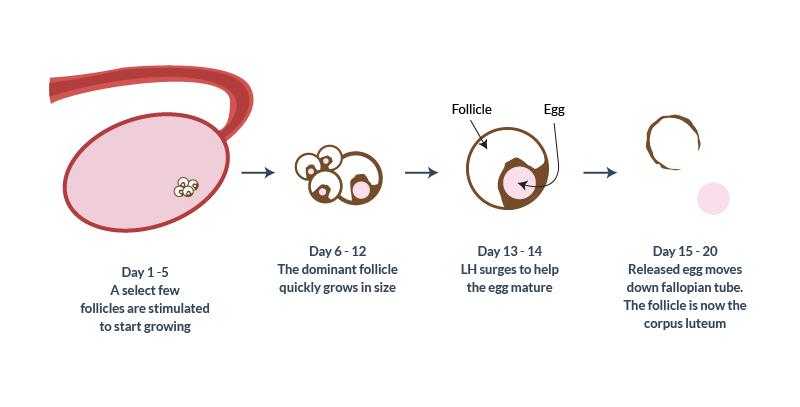
Ovulation is the process of release of an egg from the ovary. The menstrual cycle of a woman can theoretically be divided into 2 phases. In the first phase, in one of the ovaries (less often in both), the follicle grows and the egg matures in it. Around the middle of the cycle, the follicle ruptures and the egg is released - this is ovulation.
The ovum released from the follicle is ready for fertilization. Moving, she enters the fallopian tubes, where she meets with the sperm. The fertilized egg descends into the uterine cavity, where it is implanted, and pregnancy begins to develop. If fertilization does not occur or the fertilized egg is not implanted in the uterine cavity, then menstruation begins.
The probability of conception is maximum on the day of ovulation, and is approximately 33%. If we take into account that the average lifespan of a sperm cell is 2-3 days (in rare cases it reaches 5-7 days), and the egg remains viable for up to 48 hours, then the maximum duration of the "fertile period" is 7-9days (6-7 days before ovulation and 1-2 days after ovulation).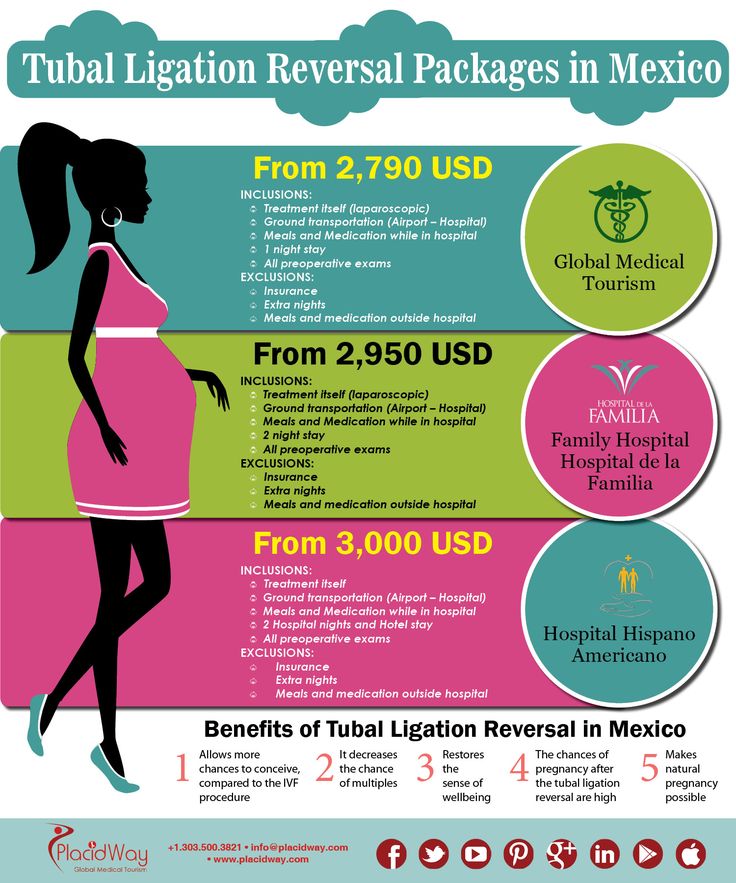
In the absence of ovulation, the egg does not mature or does not leave the follicle, which means that the spermatozoon has nothing to fertilize, and the onset of pregnancy in this case is impossible.
Lack of ovulation is a common cause of infertility in women who confess “I can’t get pregnant” at the appointment.
When planning pregnancy and simply for diagnosing women's health, determining the presence of ovulation is a top priority. There are several methods, including those that can be used at home.
How to determine ovulation?
Subjective feelings. Ovulation is usually not accompanied by any pronounced signs, and it can only be determined by carefully observing yourself. What to do and what to pay attention to?
About imminent ovulation says:
- increased vaginal discharge in the middle of the menstrual cycle;
- change in their color and consistency;
- pain in the lower abdomen on the side where ovulation occurred.
- Severe pain during ovulation occurs with a pronounced adhesive process or polycystic ovary syndrome.
Basal temperature measurement. Based on the temperature values in the rectum, a graph of basal temperature is plotted. On the days of ovulation, the temperature drops sharply, and then rises and stays at this level for 12-14 days, decreasing 1-2 days before the onset of menstruation.
An easier and more convenient method of determining ovulation at home are ovulation tests. They are similar to pregnancy tests, but are carried out approximately in the middle of the cycle and reliably show ovulation. If within three menstrual cycles, ovulation tests are negative, then you need to consult a doctor to find out the reasons for its absence.
The most reliable method for diagnosing ovulation is the ultrasound method (foliculometry). This requires repeated ultrasound monitoring. The study is safe, it can be done several times a year.
Why is there no ovulation?
There are many reasons why couples wonder why they can't get pregnant.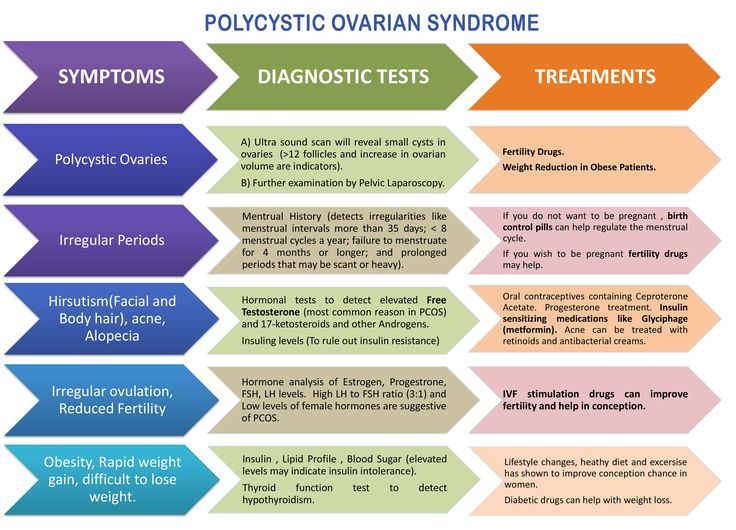 Possible reasons for the lack of ovulation:
Possible reasons for the lack of ovulation:
- diabetes mellitus;
- hyperprolactinemia;
- diseases of the thyroid gland;
- polycystic ovary syndrome;
- hypothalamic-pituitary insufficiency;
- metabolic disorders (obesity or underweight), etc.
Most often, the absence of ovulation occurs in polycystic ovary syndrome. Couples for 2 years can wait for conception, but they never will. The lack of ovulation can be corrected by hormonal stimulation of the ovaries, after which pregnancy will occur naturally.
If pregnancy does not occur in the natural cycle with ovarian stimulation, then intrauterine insemination is necessary. If, after insemination with polycystic ovary syndrome, pregnancy does not occur, then in vitro fertilization is indicated.
Obstruction of the fallopian tubes
As mentioned above, the egg and sperm meet in the fallopian tube, where fertilization takes place, and then the fertilized egg, moving through the fallopian tube, enters the uterus.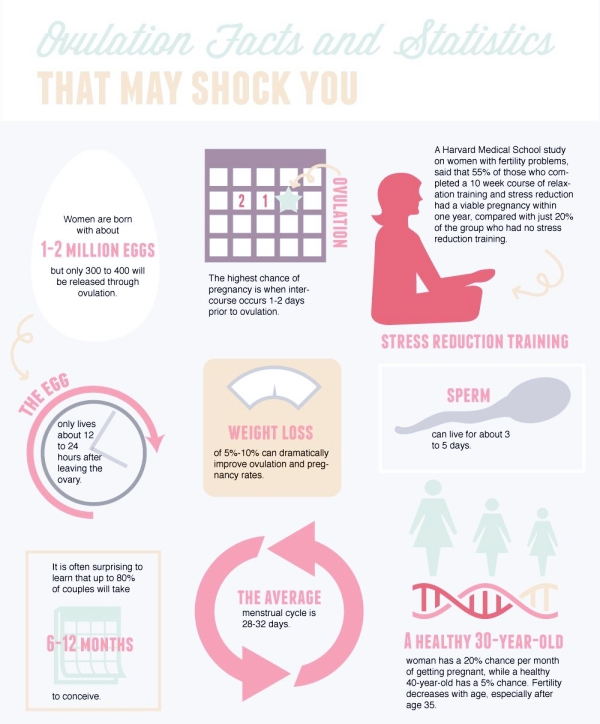 Therefore, the next reason for the absence of pregnancy may be a violation of the patency of the fallopian tubes, which occurs due to previous inflammatory diseases and adhesions formed.
Therefore, the next reason for the absence of pregnancy may be a violation of the patency of the fallopian tubes, which occurs due to previous inflammatory diseases and adhesions formed.
Tubal patency can be checked using hysterosalpingography and laparoscopy. If the obstruction of the fallopian tubes is confirmed, the patency of the tubes can be restored with the help of microsurgery. If it is not possible to restore the patency of the fallopian tubes, then the patient is recommended in vitro fertilization.
Pathology of the uterine cavity
Pathology of the uterine cavity can also be one of the reasons for the absence of pregnancy. These can be both congenital pathologies (absence or underdevelopment of the uterus, doubling, saddle uterus, septum in the uterine cavity), and acquired (scars in the uterus, intrauterine adhesions, uterine fibroids, endometrial polyp).
Methods for diagnosing uterine pathology are ultrasound and diagnostic hysteroscopy. For the treatment of uterine pathology, reconstructive surgery is sometimes necessary, and sometimes hysteroscopy is indicated.