Pcos and trying to conceive
Polycystic ovary syndrome | Office on Women's Health
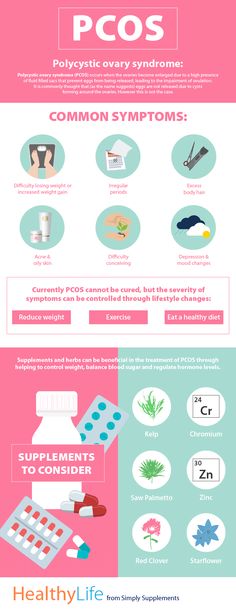
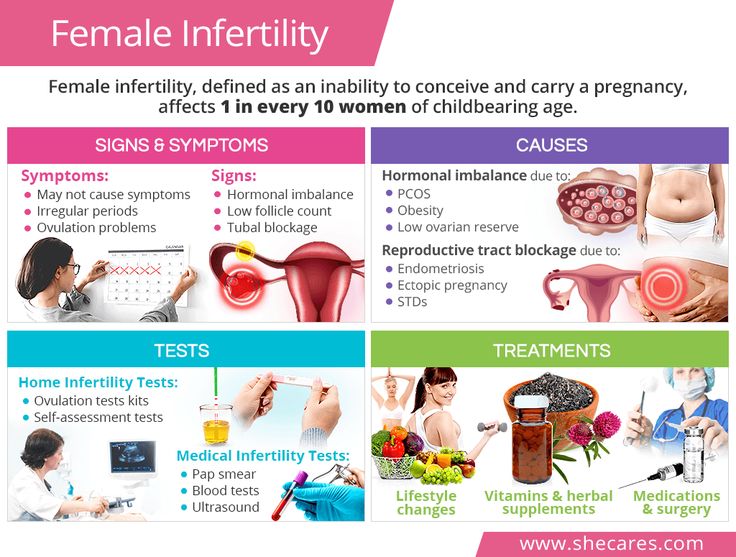
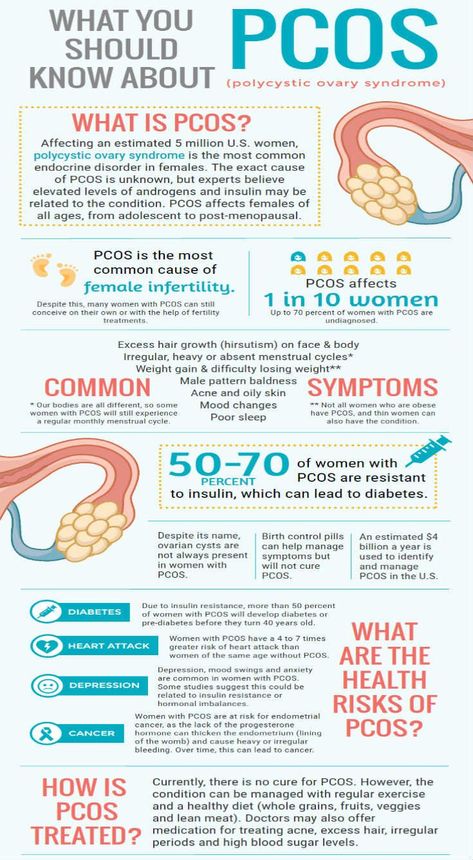
Polycystic ovary syndrome (PCOS) is a health problem that affects 1 in 10 women of childbearing age. Women with PCOS have a hormonal imbalance and metabolism problems that may affect their overall health and appearance. PCOS is also a common and treatable cause of infertility.
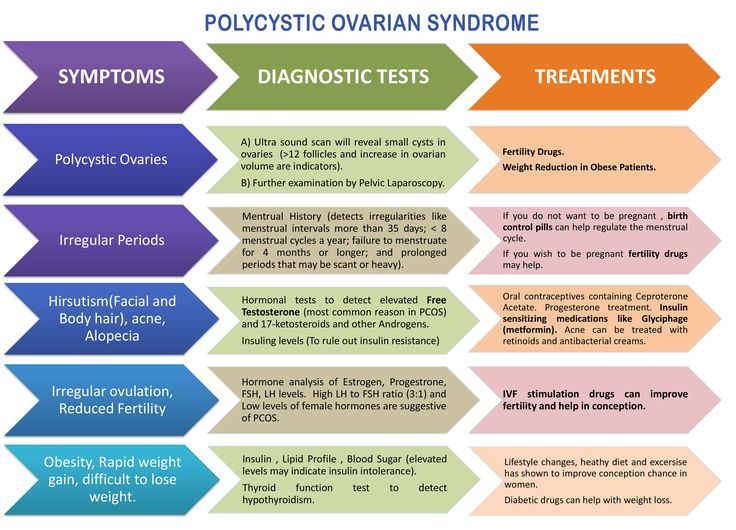
What is polycystic ovary syndrome (PCOS)?
Polycystic ovary syndrome (PCOS), also known as polycystic ovarian syndrome, is a common health problem caused by an imbalance of reproductive hormones. The hormonal imbalance creates problems in the ovaries. The ovaries make the egg that is released each month as part of a healthy menstrual cycle. With PCOS, the egg may not develop as it should or it may not be released during ovulation as it should be.
PCOS can cause missed or irregular menstrual periods. Irregular periods can lead to:
- Infertility (inability to get pregnant). In fact, PCOS is one of the most common causes of infertility in women.
- Development of cysts (small fluid-filled sacs) in the ovaries
Who gets PCOS?
Between 5% and 10% of women between 15 and 44, or during the years you can have children, have PCOS.1 Most women find out they have PCOS in their 20s and 30s, when they have problems getting pregnant and see their doctor. But PCOS can happen at any age after puberty.2
Women of all races and ethnicities are at risk of PCOS. Your risk of PCOS may be higher if you have obesity or if you have a mother, sister, or aunt with PCOS.
What are the symptoms of PCOS?
Some of the symptoms of PCOS include:
- Irregular menstrual cycle. Women with PCOS may miss periods or have fewer periods (fewer than eight in a year). Or, their periods may come every 21 days or more often. Some women with PCOS stop having menstrual periods.
- Too much hair on the face, chin, or parts of the body where men usually have hair.
 This is called "hirsutism." Hirsutism affects up to 70% of women with PCOS.3
This is called "hirsutism." Hirsutism affects up to 70% of women with PCOS.3 - Acne on the face, chest, and upper back
- Thinning hair or hair loss on the scalp; male-pattern baldness
- Weight gain or difficulty losing weight
- Darkening of skin, particularly along neck creases, in the groin, and underneath breasts
- Skin tags, which are small excess flaps of skin in the armpits or neck area
What causes PCOS?
The exact cause of PCOS is not known. Most experts think that several factors, including genetics, play a role:
- High levels of androgens. Androgens are sometimes called "male hormones," although all women make small amounts of androgens. Androgens control the development of male traits, such as male-pattern baldness. Women with PCOS have more androgens than normal. Higher than normal androgen levels in women can prevent the ovaries from releasing an egg (ovulation) during each menstrual cycle, and can cause extra hair growth and acne, two signs of PCOS.
- High levels of insulin. Insulin is a hormone that controls how the food you eat is changed into energy. Insulin resistance is when the body's cells do not respond normally to insulin. As a result, your insulin blood levels become higher than normal. Many women with PCOS have insulin resistance, especially those who have overweight or obesity, have unhealthy eating habits, do not get enough physical activity, and have a family history of diabetes (usually type 2 diabetes). Over time, insulin resistance can lead to type 2 diabetes.
Can I still get pregnant if I have PCOS?
Yes. Having PCOS does not mean you can't get pregnant. PCOS is one of the most common, but treatable, causes of infertility in women. In women with PCOS, the hormonal imbalance interferes with the growth and release of eggs from the ovaries (ovulation). If you don't ovulate, you can't get pregnant.
Your doctor can talk with you about ways to help you ovulate and to raise your chance of getting pregnant.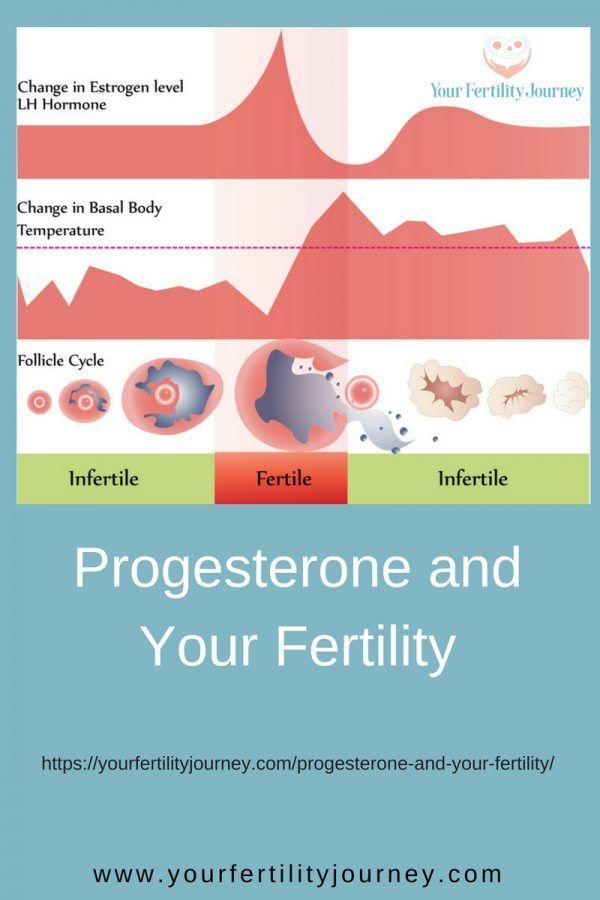 You can also use our Ovulation Calculator to see which days in your menstrual cycle you are most likely to be fertile.
You can also use our Ovulation Calculator to see which days in your menstrual cycle you are most likely to be fertile.
Is PCOS linked to other health problems?
Yes, studies have found links between PCOS and other health problems, including:
- Diabetes. More than half of women with PCOS will have diabetes or prediabetes (glucose intolerance) before the age of 40.4 Learn more about diabetes on our Diabetes page.
- High blood pressure. Women with PCOS are at greater risk of having high blood pressure compared with women of the same age without PCOS. High blood pressure is a leading cause of heart disease and stroke. Learn more about heart disease and stroke.
- Unhealthy cholesterol. Women with PCOS often have higher levels of LDL (bad) cholesterol and low levels of HDL (good) cholesterol. High cholesterol raises your risk of heart disease and stroke.
- Sleep apnea. This is when momentary and repeated stops in breathing interrupt sleep.
 Many women with PCOS have overweight or obesity, which can cause sleep apnea. Sleep apnea raises your risk of heart disease and diabetes.
Many women with PCOS have overweight or obesity, which can cause sleep apnea. Sleep apnea raises your risk of heart disease and diabetes. - Depression and anxiety. Depression and anxiety are common among women with PCOS.
- Endometrial cancer. Problems with ovulation, obesity, insulin resistance, and diabetes (all common in women with PCOS) increase the risk of developing cancer of the endometrium (lining of the uterus or womb).
Researchers do not know if PCOS causes some of these problems, if these problems cause PCOS, or if there are other conditions that cause PCOS and other health problems.
Will my PCOS symptoms go away at menopause?
Yes and no. PCOS affects many systems in the body. Many women with PCOS find that their menstrual cycles become more regular as they get closer to menopause. However, their PCOS hormonal imbalance does not change with age, so they may continue to have symptoms of PCOS.
Also, the risks of PCOS-related health problems, such as diabetes, stroke, and heart attack, increase with age.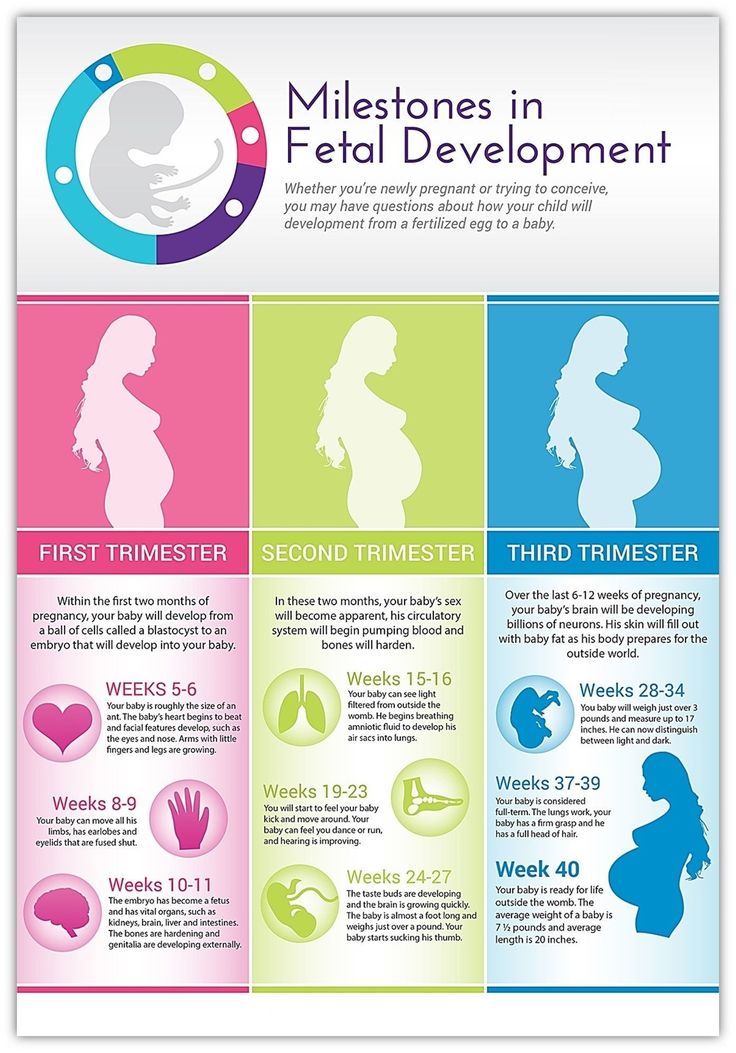 These risks may be higher in women with PCOS than those without.
These risks may be higher in women with PCOS than those without.
How is PCOS diagnosed?
There is no single test to diagnose PCOS. To help diagnose PCOS and rule out other causes of your symptoms, your doctor may talk to you about your medical history and do a physical exam and different tests:
- Physical exam. Your doctor will measure your blood pressure, body mass index (BMI), and waist size. They will also look at your skin for extra hair on your face, chest or back, acne, or skin discoloration. Your doctor may look for any hair loss or signs of other health conditions (such as an enlarged thyroid gland).
- Pelvic exam. Your doctor may do a pelvic exam for signs of extra male hormones (for example, an enlarged clitoris) and check to see if your ovaries are enlarged or swollen.
- Pelvic ultrasound (sonogram). This test uses sound waves to examine your ovaries for cysts and check the endometrium (lining of the uterus or womb).

- Blood tests. Blood tests check your androgen hormone levels, sometimes called "male hormones." Your doctor will also check for other hormones related to other common health problems that can be mistaken for PCOS, such as thyroid disease. Your doctor may also test your cholesterol levels and test you for diabetes.
Once other conditions are ruled out, you may be diagnosed with PCOS if you have at least two of the following symptoms:5
- Irregular periods, including periods that come too often, not often enough, or not at all
- Signs that you have high levels of androgens:
- Extra hair growth on your face, chin, and body (hirsutism)
- Acne
- Thinning of scalp hair
- Higher than normal blood levels of androgens
- Multiple cysts on one or both ovaries
How is PCOS treated?
There is no cure for PCOS, but you can manage the symptoms of PCOS. You and your doctor will work on a treatment plan based on your symptoms, your plans for having children, and your risk of long-term health problems such as diabetes and heart disease.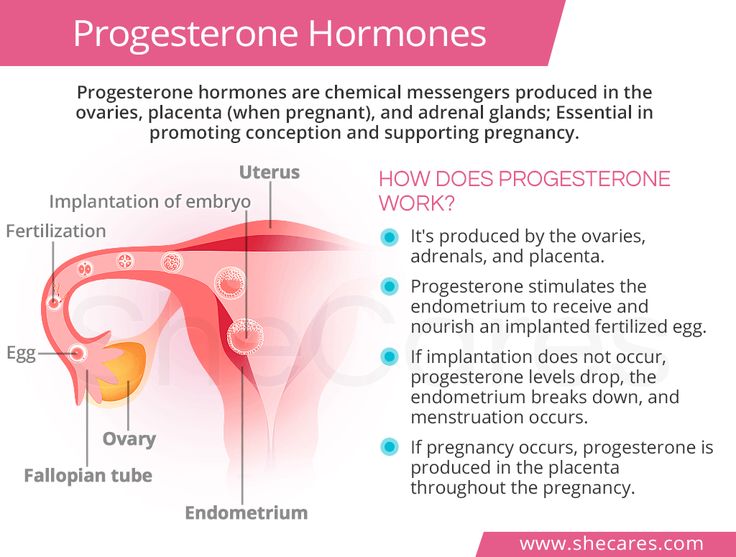 Many women will need a combination of treatments, including:
Many women will need a combination of treatments, including:
- Steps you can take at home to help relieve your symptoms
- Medicines
What steps can I take at home to improve my PCOS symptoms?
You can take steps at home to help your PCOS symptoms, including:
- Losing weight. Healthy eating habits and regular physical activity can help relieve PCOS-related symptoms. Losing weight may help to lower your blood glucose levels, improve the way your body uses insulin, and help your hormones reach normal levels. Even a 10% loss in body weight (for example, a 150-pound woman losing 15 pounds) can help make your menstrual cycle more regular and improve your chances of getting pregnant.3 Learn more about healthy weight.
- Removing hair. You can try facial hair removal creams, laser hair removal, or electrolysis to remove excess hair. You can find hair removal creams and products at drugstores. Procedures like laser hair removal or electrolysis must be done by a doctor and may not be covered by health insurance.

- Slowing hair growth. A prescription skin treatment (eflornithine HCl cream) can help slow down the growth rate of new hair in unwanted places.
What types of medicines treat PCOS?
The types of medicines that treat PCOS and its symptoms include:
- Hormonal birth control, including the pill, patch, shot, vaginal ring, and hormone intrauterine device (IUD). For women who don't want to get pregnant, hormonal birth control can:
- Make your menstrual cycle more regular
- Lower your risk of endometrial cancer
- Help improve acne and reduce extra hair on the face and body (Ask your doctor about birth control with both estrogen and progesterone.)
- Anti-androgen medicines. These medicines block the effect of androgens and can help reduce scalp hair loss, facial and body hair growth, and acne. They are not approved by the Food and Drug Administration (FDA) to treat PCOS symptoms.
 These medicines can also cause problems during pregnancy.
These medicines can also cause problems during pregnancy. - Metformin. Metformin is often used to treat type 2 diabetes and may help some women with PCOS symptoms. It is not approved by the FDA to treat PCOS symptoms. Metformin improves insulin's ability to lower your blood sugar and can lower both insulin and androgen levels. After a few months of use, metformin may help restart ovulation, but it usually has little effect on acne and extra hair on the face or body. Recent research shows that metformin may have other positive effects, including lowering body mass and improving cholesterol levels.
What are my treatment options for PCOS if I want to get pregnant?
You have several options to help your chances of getting pregnant if you have PCOS:
- Losing weight. If you have overweight or obesity, losing weight through healthy eating and regular physical activity can help make your menstrual cycle more regular and improve your fertility.
 Find a personalized healthy eating plan using the MyPlate Plan tool.
Find a personalized healthy eating plan using the MyPlate Plan tool. - Medicine. After ruling out other causes of infertility in you and your partner, your doctor might prescribe medicine to help you ovulate, such as clomiphene (Clomid).
- In vitro fertilization (IVF). IVF may be an option if medicine does not work. In IVF, your egg is fertilized with your partner's sperm in a laboratory and then placed in your uterus to implant and develop. Compared to medicine alone, IVF has higher pregnancy rates and better control over your risk of having twins and triplets (by allowing your doctor to transfer a single fertilized egg into your uterus).
- Surgery. Surgery is also an option, usually only if the other options do not work. The outer shell (called the cortex) of ovaries is thickened in women with PCOS and thought to play a role in preventing spontaneous ovulation. Ovarian drilling is a surgery in which the doctor makes a few holes in the surface of your ovary using lasers or a fine needle heated with electricity.
 Surgery usually restores ovulation, but only for 6 to 8 months.
Surgery usually restores ovulation, but only for 6 to 8 months.
Read more about treating infertility in PCOS.
How does PCOS affect pregnancy?
PCOS can cause problems during pregnancy for you and for your baby. Women with PCOS have higher rates of:6
- Miscarriage
- Gestational diabetes
- Preeclampsia
- Cesarean section (C-section)
Your baby also has a higher risk of being heavy (macrosomia) and of spending more time in a neonatal intensive care unit (NICU).
How can I prevent problems from PCOS during pregnancy?
You can lower your risk of problems during pregnancy by:
- Reaching a healthy weight before you get pregnant. Use this interactive tool to see your healthy weight before pregnancy and what to gain during pregnancy.
- Reaching healthy blood sugar levels before you get pregnant. You can do this through a combination of healthy eating habits, regular physical activity, weight loss, and medicines such as metformin.
- Taking folic acid. Talk to your doctor about how much folic acid you need.
What is the latest research on PCOS?
Researchers continue to search for new ways to treat PCOS. Some current studies focus on:
- Genetics and PCOS
- Environmental exposure and PCOS risk
- Ethnic and racial differences in PCOS symptoms
- Medicines and supplements to restart ovulation
- Obesity and its link to PCOS
- Health risks for children of women with PCOS
To learn more about current PCOS treatment studies, visit ClinicalTrials.gov.
Did we answer your question about PCOS?
For more information on PCOS, call the OWH Helpline at 1-800-994-9662 or contact the following organizations:
- Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), NIH, HHS
Phone Number: 1-800-370-2943 - American Association of Clinical Endocrinologists
Phone Number: 904-353-7878 - American College of Obstetricians and Gynecologists
Phone Number: 1-800-673-8444 - American Society for Reproductive Medicine
Phone Number: 205-978-5000 - InterNational Council on Infertility Information Dissemination, Inc.

Phone Number: 703-379-9178 - PCOS Foundation
Phone Number: 713-487-7267 - PCOS Awareness Association
- PCOS Challenge
Sources
- Trivax, B., & Azziz, R. (2007). Diagnosis of polycystic ovary syndrome. Clinical Obstetrics and Gynecology, 50(1), 168–177.
- Bremer, A. A. (2010). Polycystic ovary syndrome in the pediatric population. Metabolic Syndrome and Related Disorders, 8(5), 375–394.
- American College of Obstetricians and Gynecologists. (2015). Polycystic ovary syndrome.
- Lorenz, L. B., & Wild, R. A. (2007). Polycystic ovarian syndrome: an evidence-based approach to evaluation and management of diabetes and cardiovascular risks for today's clinician. Clinical Obstetrics and Gynecology, 50, 226–243.
- Goodman, N. F., Cobin, R. H., Futterweit, W., Glueck, J. S., Legro, R. S., & Carmina, E. (2015). American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome - part 1.
 Endocrine Practice, 11, 1291–300.
Endocrine Practice, 11, 1291–300. - Boomsma, C. M., Fauser, B. C., & Macklon, N.S. (2008). Pregnancy complications in women with polycystic ovary syndrome. Seminars in Reproductive Medicine, 26, 72–84.
The Office on Women's Health is grateful for the medical review by:
- Violanda Grigorescu, M.D., M.S.P.H., Chief, Partnerships and Evaluation Branch, Division of Health Informatics and Surveillance, Center for Surveillance, Epidemiology and Laboratory Services, Centers for Disease Control and Prevention
- Torie Comeaux Plowden, M.D., M.P.H., Fellow, Reproductive Endocrinology and Infertility, Eunice Kennedy Shriver National Institute of Child Health and Human Development
- Lubna Pal, M.B.B.S., M.R.C.O.G., M.S., F.A.C.O.G., Associate Professor, Director of the Polycystic Ovary Syndrome (PCOS) Program, Department of Obstetrics, Gynecology & Reproductive Sciences, Yale School of Medicine
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.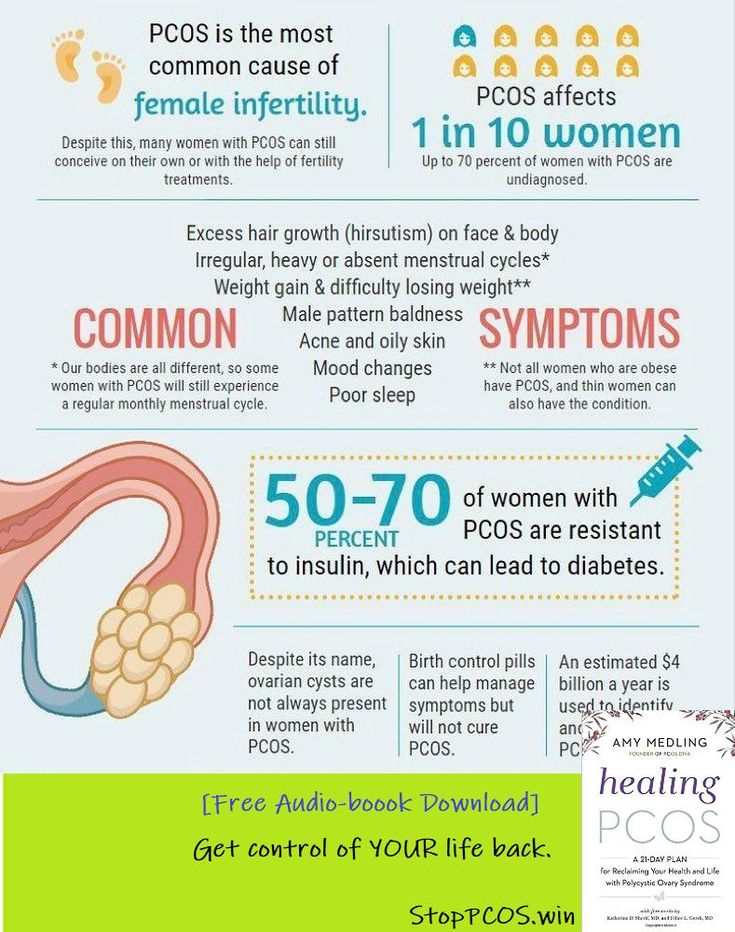 S. Department of Health and Human Services. Citation of the source is appreciated.
S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
I have PCOS and I want to have a baby, what do I need to know?
This article is republished from The Conversation under a Creative Commons license.
Sara Holton, Deakin University and Karin Hammarberg, Monash University
Most women want and expect to have children. But women who have a chronic health condition such as polycystic ovary syndrome (PCOS) often have concerns about childbearing, including whether they can become pregnant.
PCOS is a complex hormonal condition which affects up to one in five women of reproductive age. Most women with PCOS have elevated levels of a type of hormone called luteinising hormone, which brings about ovulation, and reduced levels of a hormone called “follicle stimulating hormone”, which is essential for pubertal development and the function of women’s ovaries and men’s testes.
Women with PCOS also have an underproduction of oestrogen (“female” hormones) and an overproduction of androgens (“male” hormones). This causes tiny cysts on the surface of the ovaries.
Due to these hormonal imbalances, women with PCOS often have irregular menstrual cycles because they don’t ovulate or ovulate only occasionally. So women with PCOS are more likely to have trouble conceiving than other women.
While most women who have PCOS become pregnant, they often take longer to fall pregnant and are more likely to need fertility treatment than women without PCOS.
In a recent study by Monash University, women with PCOS took part in an online discussion group. They talked about their concerns about pregnancy and what they could do to improve their chances of falling pregnant, the sort of information they would like about fertility and PCOS, and when they would like to receive this information.
Their greatest worry was about whether they would be able to get pregnant. They also wanted to know how best to prepare for pregnancy and what they should do before trying to conceive. They had trouble finding up-to-date, relevant and reliable information.
They also wanted to know how best to prepare for pregnancy and what they should do before trying to conceive. They had trouble finding up-to-date, relevant and reliable information.
Read more: Explainer: what is polycystic ovary syndrome?
How to increase chance of pregnancy
As for all women, being in the best possible health before trying for a baby increases the chance of pregnancy and gives the baby the best start in life.
According to the international evidence-based guideline for the assessment and management of PCOS, adopting a healthy lifestyle – including being in the healthy weight range, not smoking, cutting back on alcohol, eating a healthy diet, getting plenty of regular exercise and enough sleep – is the first thing to do to improve a woman’s chances of becoming pregnant and having a healthy baby.
To get the right kind of advice and support, women planning to get pregnant should have a preconception health check with their GP. This is also an opportunity to discuss a plan of action in case the PCOS causes fertility difficulties.
This is also an opportunity to discuss a plan of action in case the PCOS causes fertility difficulties.
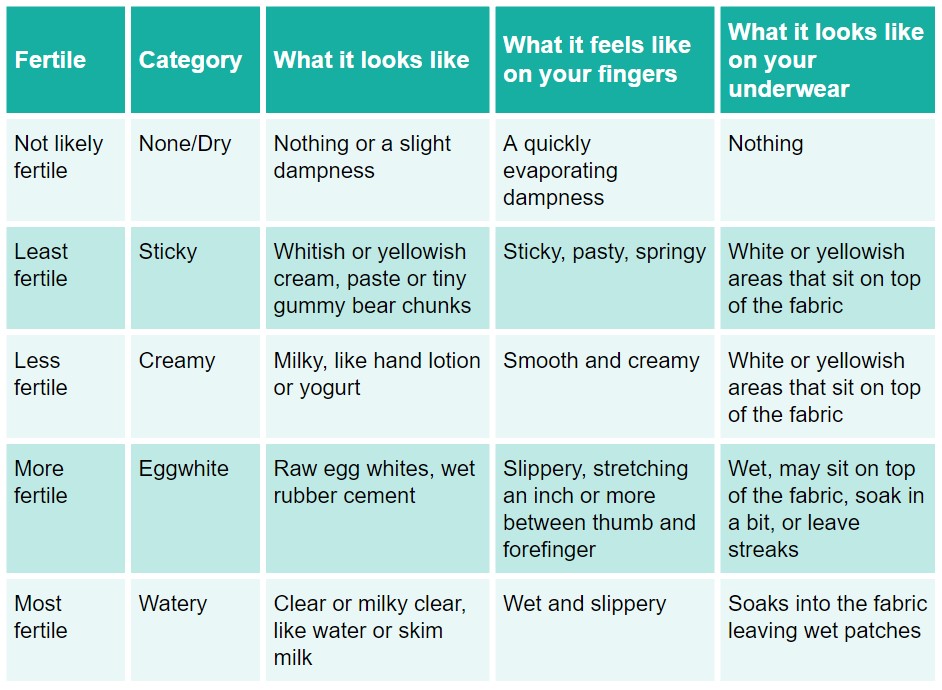
For women with PCOS who are overweight or obese, a modest weight loss sometimes results in more regular ovulation, which increases the chance of pregnancy. For those who know they ovulate, having sex during the “fertile window” (the five days leading up to and including ovulation) boosts the chance of conception.
Overall, women with and without PCOS have a similar number of children. john looy unsplash
Read more: Women's fertility: does 'egg timer' testing work, and what are the other options?
What are my options?
If you have tried for a baby for 12 months without success (or six months if you are aged 35 or over) it’s time to seek medical advice. Your GP is your first port of call, but she might refer you to a fertility specialist.
If you have very irregular or only sporadic periods, this is an indication you are not ovulating and need medical help to have a baby.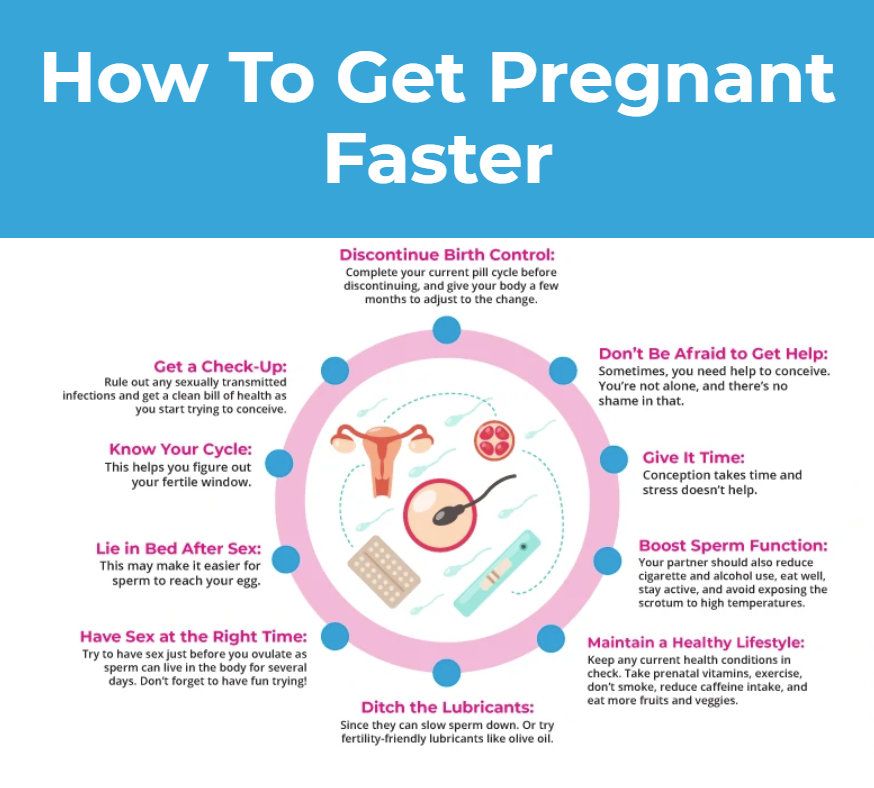 The first line of medical treatment is ovulation induction. This involves a course of tablets or injections to stimulate the ovaries to release an egg that can be fertilised, either during intercourse or through intra-uterine insemination (IUI).
The first line of medical treatment is ovulation induction. This involves a course of tablets or injections to stimulate the ovaries to release an egg that can be fertilised, either during intercourse or through intra-uterine insemination (IUI).
If this doesn’t work, there may be other reasons why pregnancy can’t be achieved and more invasive treatments such as IVF may be needed.
IVF involves a course of injections to stimulate the ovaries to produce multiple eggs. When they’re mature the eggs are retrieved in an ultrasound-guided procedure under light anaesthetic. Sperm are added to the eggs in the laboratory for embryos to form.
A few days later, an embryo is placed in the uterus where it may implant and grow into a baby. If there is more than one embryo, these can be frozen for later use if there is no pregnancy.
While IVF is safe in the hands of specialists, there are some possible health effects to be aware of, including ovarian hyperstimulation syndrome. This is an over-response to the fertility drugs that are used to stimulate the ovaries to produce multiple eggs.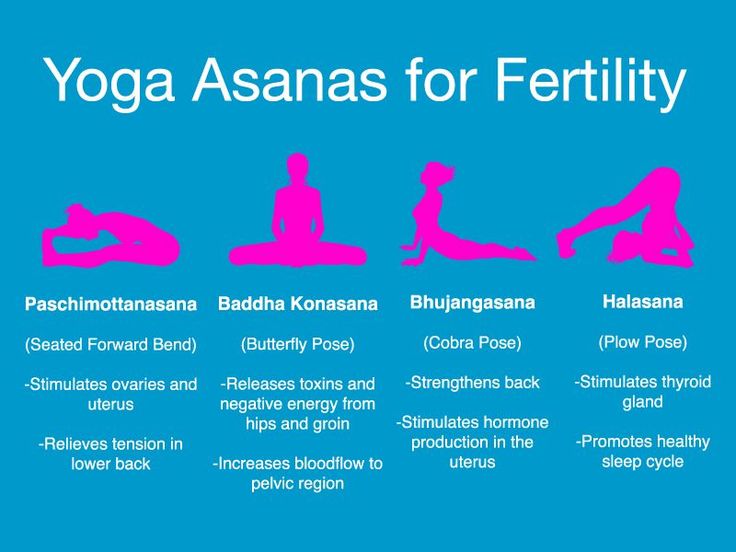 This can lead to abdominal pain, nausea and vomiting, rapid weight gain and blood clots.
This can lead to abdominal pain, nausea and vomiting, rapid weight gain and blood clots.
Read more: Better health and diet well before conception results in healthier pregnancies
For more information
The Your Fertility website has more information on PCOS and fertility. The Centre for Research Excellence in Polycystic Ovary Syndrome has also produced a list of questions for women with PCOS to use in conversations with their healthcare provider and a fact sheet about PCOS, fertility and pregnancy.
While fertility problems are common among women with PCOS, it’s reassuring that, overall, women with PCOS and women without PCOS have similar numbers of children. And, although PCOS is associated with fertility difficulties, women with PCOS should also be aware conception is possible and effective contraception is needed to avoid pregnancy when it’s not wanted.
This article was co-authored by Louise Johnson, CEO of the Victorian Assisted Reproductive Treatment Authority (VARTA).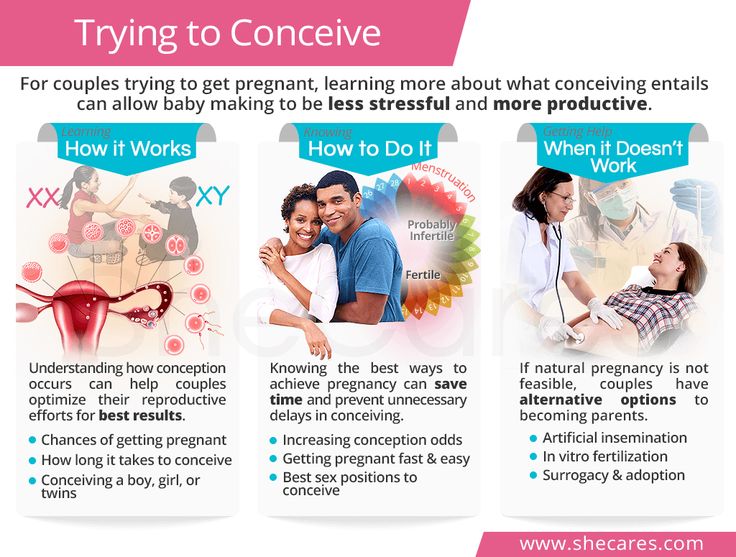 Louise has no conflicts of interest to note.
Louise has no conflicts of interest to note.
Sara Holton, Research Fellow, Deakin University and Karin Hammarberg, Senior Research Fellow, Jean Hailes Research Unit, School of Public Health & Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
PCOS Fertility Pregnancy
How to get pregnant with polycystic ovaries?
Polycystic disease is a common hormonal disease that affects the functioning of a woman's ovaries. The dangers of PCOS include irregular menstrual periods, excessive hair growth, acne, weight gain, and other problems. Left untreated, PCOS can even lead to infertility. In this article, we will tell you more about causes of polycystic , polycystic ovaries and pregnancy , and also give an answer to the question: “ Is it possible to give birth with polycystic ovaries? ".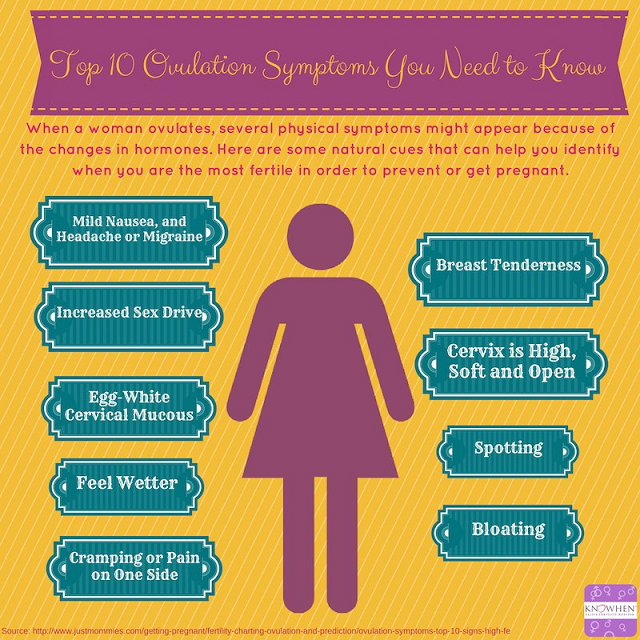
What is polycystic ovary syndrome?
Polycystic ovary syndrome (PCOS) is a hormonal disorder common among women of reproductive age. Women with PCOS may have menstrual irregularities and elevated levels of male hormones (androgens). Numerous small collections of fluid (follicles) may form in the ovaries, and an egg may not be released regularly. This condition should not be confused with multifollicular ovaries, because with multifollicular ovaries, ovulation and a normal menstrual cycle can persist, unlike polycystic disease.
50-75% of cases of endocrine infertility. 20-22% of marital infertility. It is detected in 5-16% of women of reproductive age. These are the figures for the diagnosis of "Polycystic Ovary".
Symptoms of polycystic ovary syndrome
Polycystic ovary syndrome is accompanied by characteristic symptoms, upon noticing which it is necessary to seek advice from an endocrinologist or gynecologist. For some women, symptoms begin around the time of their first menstrual period. Others discover symptoms of PCOS only after they have gained a lot of weight or have problems getting pregnant. In some cases, PCOS may be asymptomatic.
Others discover symptoms of PCOS only after they have gained a lot of weight or have problems getting pregnant. In some cases, PCOS may be asymptomatic.
The most common symptoms of PCOS:
- Irregular periods. Lack of ovulation prevents the lining of the uterus from falling off every month. Some women with PCOS have fewer than eight periods a year, or none at all.
- Severe bleeding. The lining of the uterus builds up over a longer period of time, so menstruation may be heavier than usual.
- Hair growth . More than 70 percent of women with this condition grow hair on their face and body, including on their back, abdomen, and chest. Excess hair growth is called hirsutism.
- Acne . Male hormones can make the skin more oily than normal and cause breakouts on areas such as the face, chest, and upper back.
- Weight gain. Up to 80 percent of women with PCOS are overweight or obese.
- Male pattern baldness. The hair on the scalp becomes thinner and may fall out.
- Darkening of the skin. Dark patches of skin may develop in body folds, such as the neck, groin area, and under the breasts.
- Headaches. Hormonal changes may cause headaches in some women.
Irregular periods
Infrequent, irregular periods, long or no periods are the most common symptom of PCOS. For example, with PCOS, you may have fewer than nine periods a year, more than 35 days between periods, and abnormally heavy periods.
Hyperandrogenism
Hyperandrogenism is a disease characterized by high levels of androgens. It is more common in women than in men. Symptoms of hyperandrogenism may include acne, seborrhea (inflammation of the skin), hair loss on the scalp, increased body or facial hair, and infrequent or absent periods.
Hyperandrogenism is a defining feature of women and young girls with PCOS. Polycystic disease causes a malfunction of the ovaries or adrenal glands, which leads to the production of excess androgens (male sex hormones).
Polycystic disease causes a malfunction of the ovaries or adrenal glands, which leads to the production of excess androgens (male sex hormones).
Anovulation
Anovulation occurs when an egg is not released from the ovary during the menstrual cycle. The egg is essential for pregnancy. Since several hormones are involved in ovulation, there are many causes of anovulation, one of which is PCOS. Chronic anovulation is a common cause of infertility.
Diagnosis
There is no test to definitively diagnose polycystic ovary syndrome (PCOS). The doctor will likely begin by discussing your medical history, including menstrual periods and weight changes. A physical exam will include checking for signs of excessive hair growth, acne, and weight gain.
Your doctor may recommend:
- Gynecological examination. A physician visually and manually examines the reproductive organs for growths or other abnormalities.
- Blood tests.
 A blood test is given to determine the level of hormones. This will help rule out possible causes of menstrual irregularities or excess androgens that mimic PCOS. An additional blood test may also be needed to measure insulin resistance as well as fasting cholesterol and triglyceride levels.
A blood test is given to determine the level of hormones. This will help rule out possible causes of menstrual irregularities or excess androgens that mimic PCOS. An additional blood test may also be needed to measure insulin resistance as well as fasting cholesterol and triglyceride levels. - Ultrasound examination (ultrasound). The doctor will check the appearance of the ovaries and the thickness of the lining of the uterus. A rod-shaped device (sensor) (transvaginal ultrasound) is inserted into the vagina, which emits sound waves and converts them into images on a computer screen.
Is it possible to get pregnant with PCOS
How to get pregnant with PCOS? Getting pregnant with PCOS can be difficult, but that doesn't mean it's impossible. While PCOS can affect your hormones and therefore your fertility, there are medical treatments and lifestyle changes you can make to improve your chances of pregnancy.
Is it possible to get pregnant with polycystic ovaries? To get pregnant, you must ovulate, which PCOS most often prevents.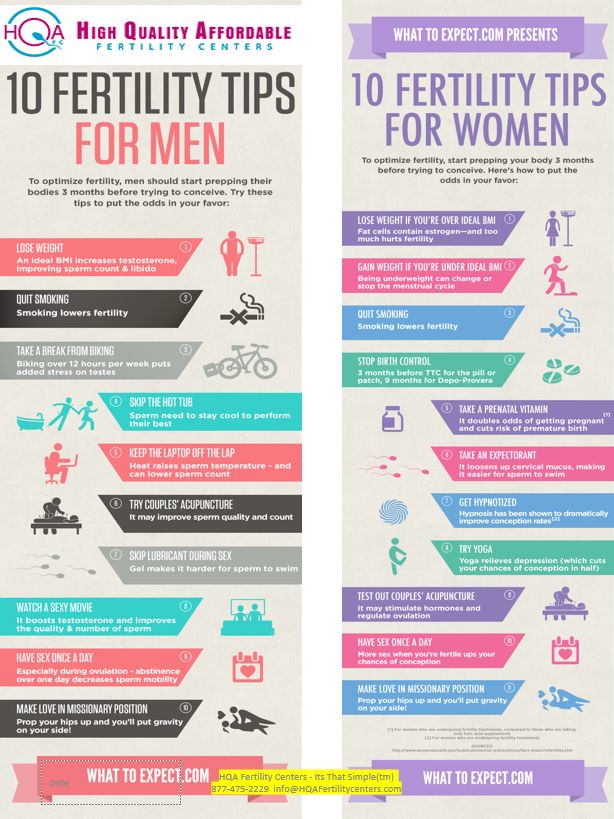 Women who do not ovulate regularly with PCOS do not release enough eggs for fertilization. Pregnancy with PCOS is further complicated by the fact that PCOS causes a hormonal imbalance that changes the quality of cervical fluid, making it difficult for sperm to survive.
Women who do not ovulate regularly with PCOS do not release enough eggs for fertilization. Pregnancy with PCOS is further complicated by the fact that PCOS causes a hormonal imbalance that changes the quality of cervical fluid, making it difficult for sperm to survive.
It is impossible to say categorically that PCOS is infertility, but PCOS is one of the main causes of infertility in women.
Is it possible to get pregnant with PCOS? And although there are no exact statistics on the chances of pregnancy, 70 to 80 percent of women with PCOS have fertility problems. PCOS disrupts the normal menstrual cycle and makes it difficult to conceive.
Is it possible to get pregnant with PCOS? Polycystic ovary syndrome is not a sentence and it is possible to get pregnant, albeit problematic. However, if PCOS is left untreated, the chances of getting pregnant decrease with age.
It is possible to get pregnant with polycystic disease, but most often pregnancy with polycystic disease is difficult. This condition can increase the risk of pregnancy complications. Women with PCOS are twice as likely to have a preterm birth than women without. They are also at greater risk of miscarriage, high blood pressure, and gestational diabetes. However, by managing the symptoms, many women with PCOS can become pregnant and have a healthy baby.
This condition can increase the risk of pregnancy complications. Women with PCOS are twice as likely to have a preterm birth than women without. They are also at greater risk of miscarriage, high blood pressure, and gestational diabetes. However, by managing the symptoms, many women with PCOS can become pregnant and have a healthy baby.
How to get pregnant with PCOS? Women with PCOS can become pregnant using fertility treatments that improve ovulation. Losing weight and lowering your blood sugar can increase your chances of a healthy pregnancy.
Pregnancy planning for PCOS
How to get pregnant with PCOS? While your chances of getting pregnant with PCOS may be lower, there are a few things you can do to increase those chances.
- Call your doctor. How to get pregnant with polycystic ovaries? Normalization of hormones and menstruation is the first step. Your doctor may prescribe medications to help your body deal with insulin better and regulate your menstrual cycle.
- Maintain a healthy weight. Is it possible to get pregnant with PCOS? Weight loss can lower insulin levels, androgen levels, and restore ovulation. Ask your doctor about a weight management program and meet with a nutritionist regularly for help with your weight loss goals.
- Eat right. Polycystic Ovarian Diet includes sugary foods, simple carbohydrates and unhealthy fats. Add to your menu: fresh and cooked fruits and vegetables, whole grains such as brown rice, oats and barley, beans and lentils, chicken, fish.
- Be active. Exercise helps lower blood sugar levels. How to get pregnant with insulin resistance? If you have PCOS, increasing daily activity such as walking, exercising, walking can help treat or even prevent insulin resistance, control your weight, and avoid developing diabetes.
- Lead a healthy lifestyle. Follow a healthy lifestyle with PCOS, give up bad habits, unhealthy diet, lack of sports and irregular sleep.

Treatment for PCOS
Treatment for PCOS focuses on your individual problems such as infertility, acne or obesity. Also, the direction of PCOS treatment largely depends on whether a woman is planning a pregnancy or not. Specific treatment may include lifestyle changes or medications.
How to treat PCOS?
Lifestyle changes
Your doctor may recommend weight loss through a low-calorie diet combined with moderate exercise. Even small weight loss - like losing 5 percent of your body weight - can improve your condition. Can you get pregnant with PCOS? Losing weight can also increase the effectiveness of medications your doctor recommends to treat PCOS and help with infertility.
Treatment with drugs for polycystic ovaries
To regulate the menstrual cycle, the doctor may recommend:
Combination birth control pills. Estrogen and progestin tablets reduce androgen production and regulate estrogen.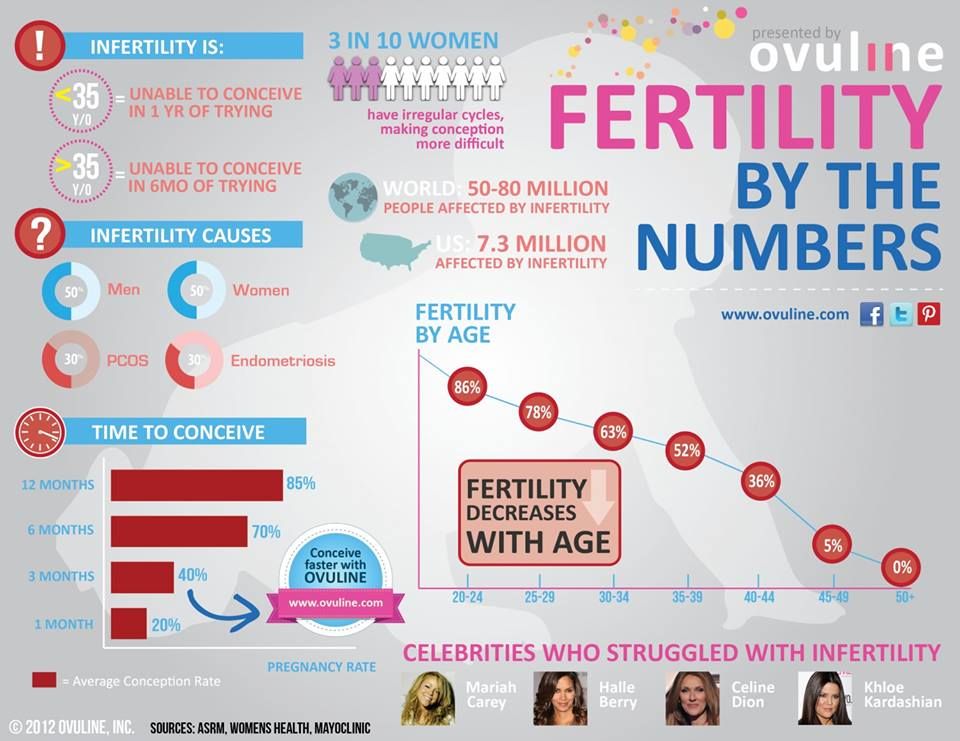 Hormone regulation can reduce the risk of endometrial cancer and correct abnormal bleeding, excess hair growth, and acne. Instead of pills, you can use a skin patch or vaginal ring containing a combination of estrogen and progestin.
Hormone regulation can reduce the risk of endometrial cancer and correct abnormal bleeding, excess hair growth, and acne. Instead of pills, you can use a skin patch or vaginal ring containing a combination of estrogen and progestin.
Progestin therapy. Daily progestin may: restore normal hormonal balance, regulate ovulation, stop excessive hair growth, protect against endometrial cancer, and help get pregnant with sleep deprivation.
How to induce ovulation in PCOS? To help induce ovulation in PCOS, your doctor may recommend:
Clomiphene is a fertility medication that can help women with PCOS get pregnant.
Metformin is a drug used to treat type 2 diabetes. It also treats PCOS by increasing insulin levels.
Operation
How to get pregnant with PCOS? Surgery may be an option to improve fertility if other treatments don't work. Ovarian drilling is a procedure in which tiny holes are made in the ovary using a laser or a thin, heated needle to restore normal ovulation and the possibility of pregnancy with PCOS.
Important! To determine the right treatment and choose the right drug, you need to consult a doctor!
Help Doc.ua: you can make an appointment with a gynecologist-endocrinologist on the website.
Polycystic ovaries and pregnancy (is it possible to get pregnant with polycystic ovaries?) - Medical Reproduction Clinic MAMA (www.ma-ma.ru).
"I have polycystic ovaries. How can I get pregnant?"0019
"How to get pregnant?"
“I have polycystic ovaries. How can I get pregnant? Aida, Moscow
The Chief Physician of the MAMA Clinic Victoria Viktorovna Zaletova answers the letter.
This issue can only be resolved after an examination and an accurate determination of the cause of the disease. Polycystic ovary syndrome is associated with an excess of androgens in the blood of a woman - male sex hormones. As a result, the mechanism of ovulation is disrupted, the maturation of a full-fledged egg does not occur, which means that pregnancy is impossible. Polycystic ovaries and pregnancy require a special medical approach.
Polycystic ovaries and pregnancy require a special medical approach.
Since the 1930s, polycystic ovary syndrome, which was called Stein-Leventhal syndrome, later renamed polycystic ovary syndrome, has been successfully treated surgically. Modern technologies make it possible to replace abdominal operations with laparoscopic ones, after which the scars on the skin are practically invisible. Laparoscopy is possible with any volume of surgery from wedge-shaped resection of the ovary to electrocauterization (burning tissue with electric current).
In the last 30 years, after the appearance of hormonal drugs, attempts have been made to oppose surgical treatment with conservative, that is, hormonal therapy. The use of estrogens and gestagens in a cyclic mode gave some patients a positive effect in the treatment of polycystic ovaries, which made it possible to prepare for pregnancy. Later, progesterone preparations appeared, with the help of which it was also possible to achieve certain positive results.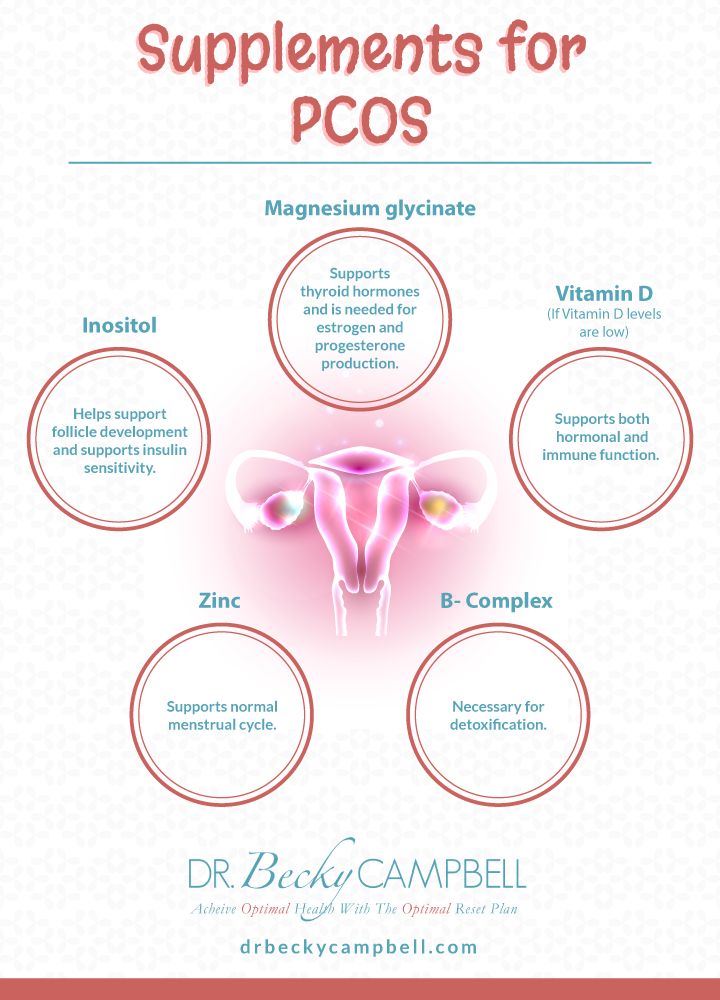 Later, synthetic estrogen-progestin oral contraceptives began to be used. Treatment with these drugs in 20 percent of cases gave a positive effect in terms of eliminating infertility, but, in the end, due to relapses, ended with surgery.
Later, synthetic estrogen-progestin oral contraceptives began to be used. Treatment with these drugs in 20 percent of cases gave a positive effect in terms of eliminating infertility, but, in the end, due to relapses, ended with surgery.
A revolution in the hormonal treatment of polycystic ovaries and pregnancy was made by a drug with the international name clomiphene. Clomiphene is an antiestrogen, which is quite capable, by occupying all estrogen-sensitive receptors, to lead to the restoration of ovulation in about 70 percent of patients. But, as is already well known, the ability to become pregnant was restored only in 40 percent of patients. The search for new drugs continued. Ovulation-stimulating gonadotropic drugs have appeared. The most famous and widely used drugs are metrodin, menagon, horagon. The most modern studies make it possible to achieve a reduction in the size of the ovary with the help of hypothalamic hormones that regulate the functioning of the pituitary gland (For example, Decapeptyl-Depot or Zoladex) and with the subsequent appointment of the same gonadotropins (Metrodin, Menogon, Horagon).