Passing tissue pregnancy
Miscarriage - what you might actually see and feel
Miscarriage - what you might actually see and feel | Pregnancy Birth and Baby beginning of content7-minute read
Listen
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
A miscarriage requires prompt medical care. If you think you are having a miscarriage, call your doctor or midwife for advice and support. Go to the Emergency Department if:
- you are bleeding very heavily (soaking more than 2 pads per hour or passing clots larger than golf balls)
- you have severe pain in your tummy or shoulder
- you have a fever (a temperature above 38 degrees C)
- you are dizzy, fainting or feel like fainting
- you notice fluid coming from your vagina that smells bad
- you have diarrhoea or pain when you have a bowel motion (do a poo)
Miscarriage is a very unfortunate and sad outcome of pregnancy that takes a significant emotional and physical toll on a woman. It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
Despite close to one in 5 pregnancies ending in miscarriage, what actually happens and what a woman needs to know and do when faced with a possible miscarriage are subjects that rarely get discussed.
This article aims to give you an idea of what happens and what a woman needs to know and do at different stages in her pregnancy.
Please call Pregnancy, Birth and Baby on 1800 882 436 if you have any concerns or wish to discuss the topic further.
What might I feel during a miscarriage?
Many women have a miscarriage early in their pregnancy without even realising it. They may just think they are having a heavy period. If this happens to you, you might have cramping, heavier bleeding than normal, pain in the tummy, pelvis or back, and feel weak. If you have started spotting, remember that this is normal in many pregnancies — but talk to your doctor or midwife to be safe and for your own peace of mind.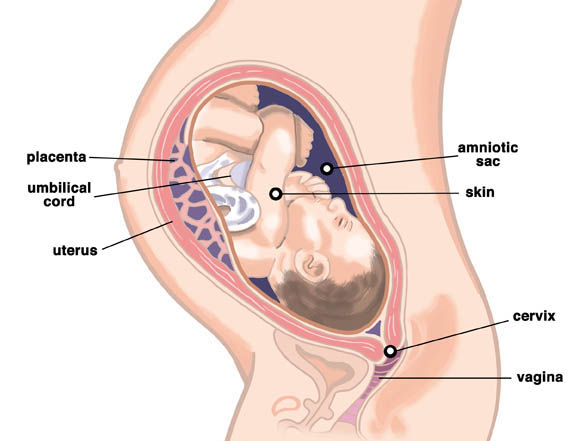
Later in your pregnancy, you might notice signs like cramping pain, bleeding or passing fluid and blood clots from your vagina. Depending on how many weeks pregnant you are, you may pass tissue that looks more like a fetus, or a fully-formed baby.
In some types of miscarriage, you might not have any symptoms at all — the miscarriage might not be discovered until your next ultrasound. Or you might just notice your morning sickness and breast tenderness have gone.
It is normal to feel very emotional and upset when you realise you’re having a miscarriage. It can take a while to process what is happening. Make sure you have someone with you, for support, and try to be kind to yourself.
What happens during a miscarriage?
Unfortunately, nothing can be done to stop a miscarriage once it has started. Any treatment is to prevent heavy bleeding or an infection.
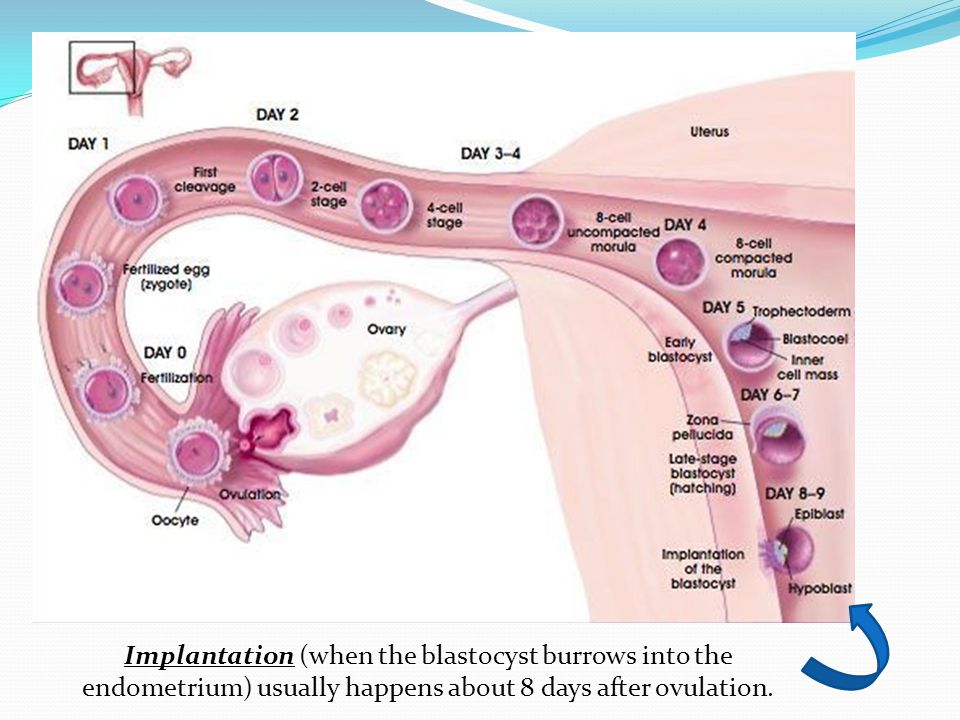
Your doctor might advise you that no treatment is necessary. This is called 'expectant management', and you just wait to see what will happen.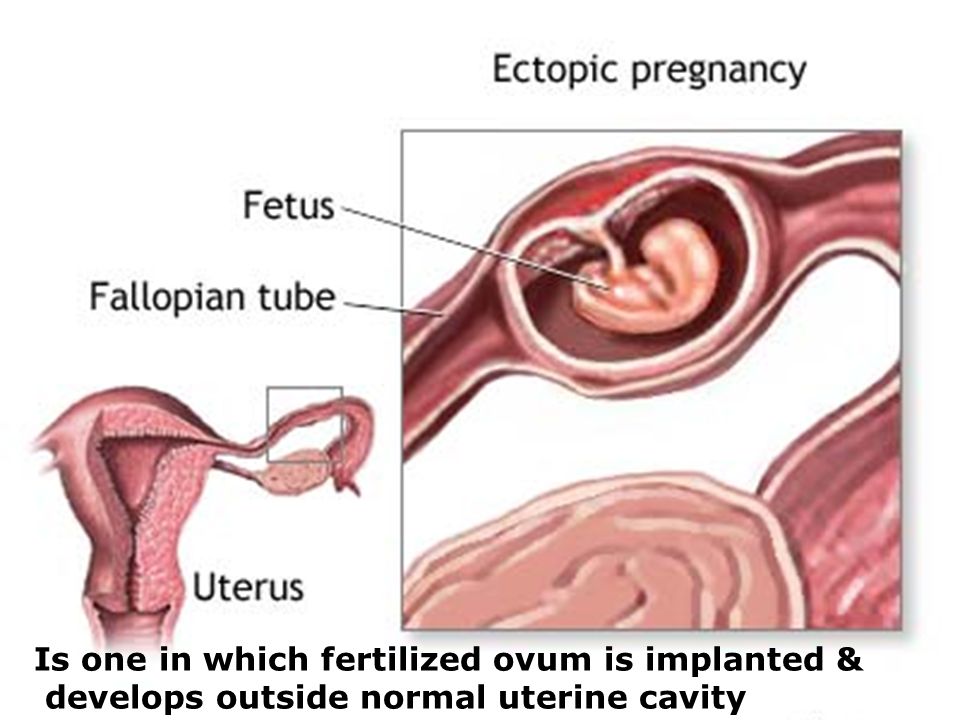 Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
It can be very hard emotionally to wait for the miscarriage because you don’t know when it will happen. When it starts, you will notice spotting and cramping and then, fairly quickly, you will start bleeding heavily. The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
Some women opt to have medicine to speed up the process. In this case, the pregnancy tissue is likely to pass within a few hours.
If not all the tissue passes naturally or you have signs of infection, you may need to have a small operation called a ‘dilatation and curettage’ (D&C). You may need to wait some time for your hospital appointment. The operation only takes 5 to 10 minutes under general anaesthetic, and you will be able to go home the same day.
While you are waiting for a miscarriage to finish, it’s best to rest at home — but you can go to work if you feel up to it. Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
What might I see during a miscarriage?
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very hard to see. You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
At 6 weeks
Most women can’t see anything recognisable when they have a miscarriage at this time. During the bleeding, you may see clots with a small sac filled with fluid. The embryo, which is about the size of the fingernail on your little finger, and a placenta might be seen inside the sac. You might also notice something that looks like an umbilical cord.
At 8 weeks
The tissue you pass may look dark red and shiny — some women describe it as looking like liver. You might find a sac with an embryo inside, about the size of a small bean. If you look closely, you might be able to see where the eyes, arms and legs were forming.
If you look closely, you might be able to see where the eyes, arms and legs were forming.
At 10 weeks
The clots that are passed are dark red and look like jelly. They might have what looks like a membrane inside, which is part of the placenta. The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
At 12 to 16 weeks
If you miscarry now, you might notice water coming out of your vagina first, followed by some bleeding and clots. The fetus will be tiny and fully formed. If you see the baby it might be outside the sac by now. It might also be attached to the umbilical cord and the placenta.
From 16 to 20 weeks
This is often called a 'late miscarriage'. You might pass large shiny red clots that look like liver as well as other pieces of tissue that look and feel like membrane. It might be painful and feel just like labour, and you might need pain relief in hospital. Your baby will be fully formed and can fit on the palm of your hand.
After the miscarriage
You will have some cramping pain and bleeding after the miscarriage, similar to a period. It will gradually get lighter and will usually stop within 2 weeks.
The signs of your pregnancy, such as nausea and tender breasts, will fade in the days after the miscarriage. If you had a late miscarriage, your breasts might produce some milk. You will probably have your next period in 4 to 6 weeks.
Remember, it’ll be normal to feel very emotional and upset at this time.
More information
Read more about miscarriage:
- What is a miscarriage?
- What happens after a miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
KidsHealth (Understanding miscarriage), The Royal Women's Hospital (Treating miscarriage), Pink Elephants Support Network (Sorry for your loss), Women’s and Children’s Health Network (Miscarriage), Patient.com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Miscarriage
- What happens after miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
What happens after miscarriage
There are a number of things you may need to consider after a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.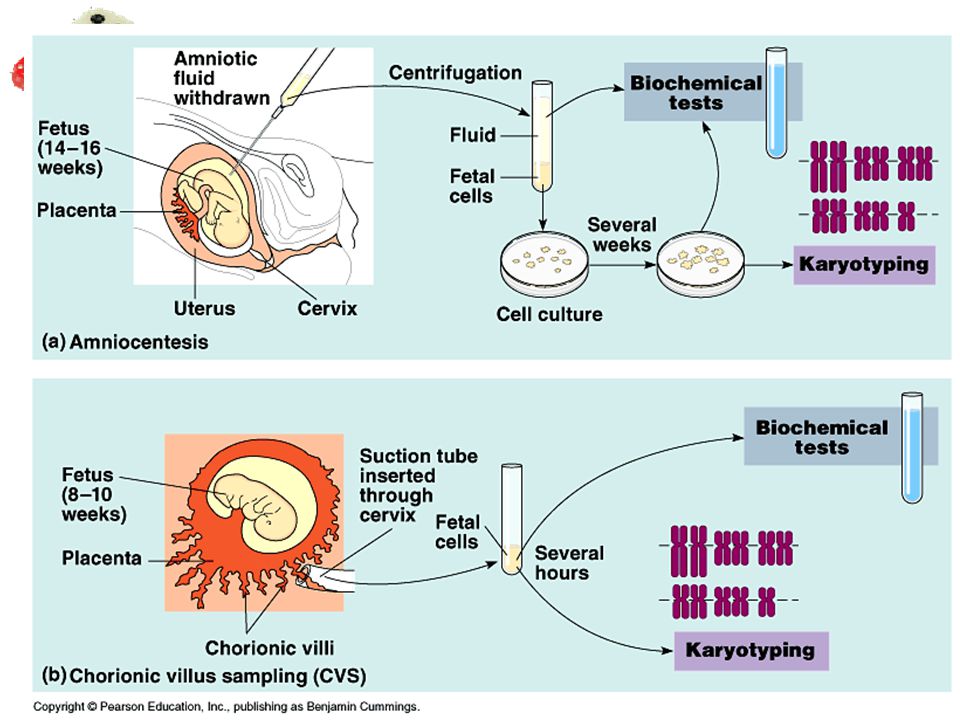
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.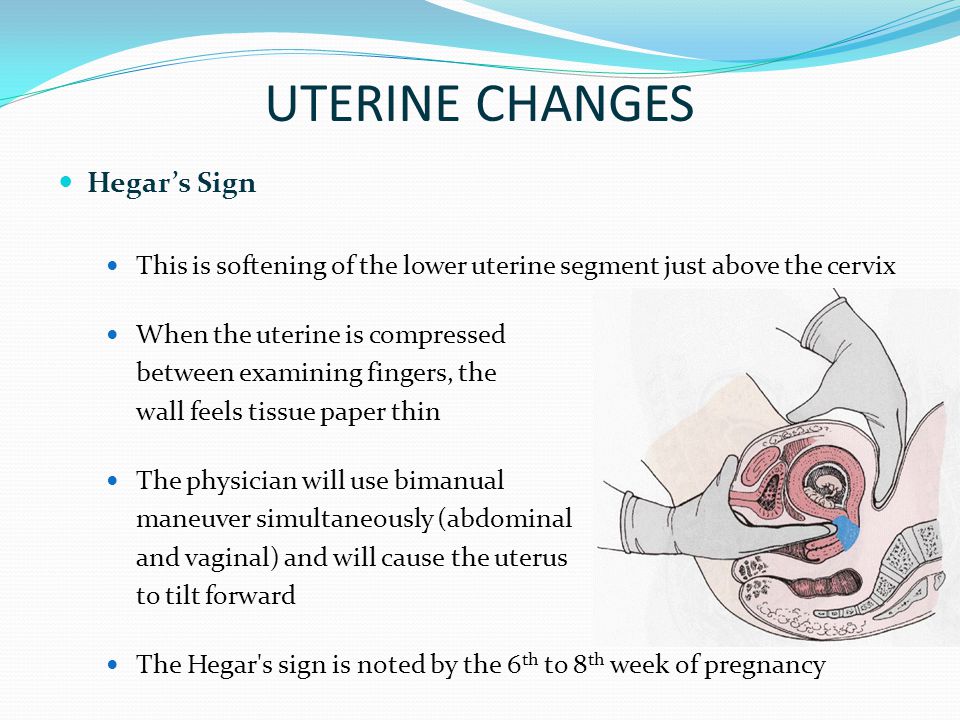 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Signs of Early Miscarriage | Obstetrics & Gynecology
Skip to main content
Department of Obstetrics and Gynecology
News | Careers | Giving | UC Davis Health
- UC Davis Health
- Obstetrics and Gynecology
- Miscarriage Management
- Signs of Early Miscarriage
Early miscarriage refers to loss of a pregnancy in the first trimester. The majority of early miscarriages occur before the pregnancy is 10 weeks gestation. Some miscarriages happen very early, even before a woman is sure she is pregnant. Still, miscarriage can be a hard and sad experience, no matter when it occurs.
The majority of early miscarriages occur before the pregnancy is 10 weeks gestation. Some miscarriages happen very early, even before a woman is sure she is pregnant. Still, miscarriage can be a hard and sad experience, no matter when it occurs.
Miscarriage is more common than many people realize. About 10 to 20% of women who learn they are pregnant will have an early miscarriage. The rates of early miscarriage are even higher when women are checking home pregnancy tests very close to the time of their period and are finding a positive test VERY early. By chance alone, 1% to 4% of women will have two miscarriages in a row. However, it is very rare to have 3 or more miscarriages in a row, which is recurrent miscarriage.
In medical terms, early miscarriage is called an early pregnancy failure. This means that the pregnancy failed to develop. Almost all early miscarriages are due to circumstances beyond anyone’s control, and were destined to happen before the woman even knows she is pregnant.
What are the symptoms of early miscarriage?
- Bleeding – light bleeding early in pregnancy is fairly common, and does not mean you will have a miscarriage.
- Brown discharge: This may look like coffee grounds. This “discharge” is actually old blood that has been in the uterus for a while and is just coming out slowly.
- Spotting, bright red bleeding or clots
- Passage of tissue through the vagina
- A gush of clear or pink vaginal fluid
- Abdominal pain or cramping
- Pregnancy symptoms, such as breast tenderness and nausea, begin to go away
- Dizziness, lightheadedness, or feeling faint
If you have any symptoms of a miscarriage, you should contact a doctor right away to have an evaluation. It will be important to have an ultrasound exam to look into the uterus to see if the pregnancy is normal or you are having a miscarriage. Even if you think you passed the entire pregnancy and are feeling better, you should see a doctor. Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
Types of early miscarriage
Early miscarriage is a non-medical term for lots of different types of events that might or might not actually result in pregnancy loss. The types of miscarriage include the following:
Spotting or bleeding in the first trimester in which the patient and the doctor are not yet sure if the pregnancy will miscarry or not. About 1/3 of all women will bleed in the first trimester, but only about half of those women will have a miscarriage.
The entire pregnancy is passed from the uterus, most commonly with bleeding and cramping, and no additional treatment or observation is needed.
The pregnancy is definitely miscarrying, but only some of the pregnancy tissue has passed. The tissue that is still in the uterus will eventually pass on its own. Some women may need emergency treatment if there is also heavy vaginal bleeding. Otherwise, women can use medicines to cause the rest of the tissue to pass or simply wait for the rest of the tissue to pass from the uterus.
Otherwise, women can use medicines to cause the rest of the tissue to pass or simply wait for the rest of the tissue to pass from the uterus.
With this type of miscarriage, the pregnancy implanted but the embryonic tissue (the part of the pregnancy that will develop into a fetus) never developed, or started to develop and then stopped.
With this type of miscarriage, the early embryo (or fetus once 10 weeks pregnant) stops developing and growing.
This is an uncommon type of miscarriage today. With a missed abortion, the pregnancy stops developing but the pregnancy tissue does not pass out of the uterus for at least 4 weeks. Sometimes, dark brown spotting or bleeding occurs, but there is no heavy bleeding.
Some miscarriages occur with an infection in the uterus. This is a serious condition that requires urgent treatment to prevent shock and death. With septic miscarriage, the patient usually develops fever and abdominal pain and may have bleeding and discharge with a foul odor. Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
What causes early miscarriage?
Almost nothing you can do will cause an early miscarriage. Avoiding sex or heavy work will not impact an early pregnancy. There are a lot of changes that need to occur with the cells and genes in a developing pregnancy, and sometimes those changes do not happen perfectly. There are some health conditions or habits that can increase the chance that an early miscarriage will occur, including:
- Heavy smoking
- Use of illicit drugs, especially cocaine
- Poorly controlled diabetes
- Hyperthyroidism or hypothyroidism
- Physical problems with the uterus, including fibroids or abnormalities of development of the uterus
Why see our specialists at UC Davis Health?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately.
We perform our own ultrasound examination in the office and can share the results with you immediately.
If we do confirm you have a miscarriage, we can discuss expectant management or treatment options with you immediately. Should you need blood testing to evaluate the pregnancy, the laboratory is in the same building as our office.
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Treatment of early miscarriage
Not all miscarriages “need” treatment. The choice of whether to wait for the pregnancy to completely pass without any treatment is up to you. Our doctors are committed to providing options for all patients, including the pros and cons of all available options when miscarriage is diagnosed. All patients with Rh-negative blood, regardless of which option they choose, need treatment with Rh-immune globulin, an injection that prevents a woman from forming substances in her blood that may attack the baby during a future pregnancy.
When a diagnosis of miscarriage is made, options include:
This means that you will not receive any treatment; just continued follow-up. In an early miscarriage, with time, most women will pass the pregnancy completely. The main issue is time – there is no way to predict exactly when this will occur. You will typically have heavy bleeding and severe abdominal cramping when the pregnancy does pass. Should you want this option, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications can be used once the pregnancy begins to pass from the uterus.
This treatment uses medicines to cause the pregnancy tissue to pass from the uterus. The medicines cause cramping and bleeding, just like what will occur with natural passing of the pregnancy tissue. Using the medicines is like expectant management, except that you know when the pregnancy is going to pass. Most women will pass the pregnancy within 24 hours of taking the medication.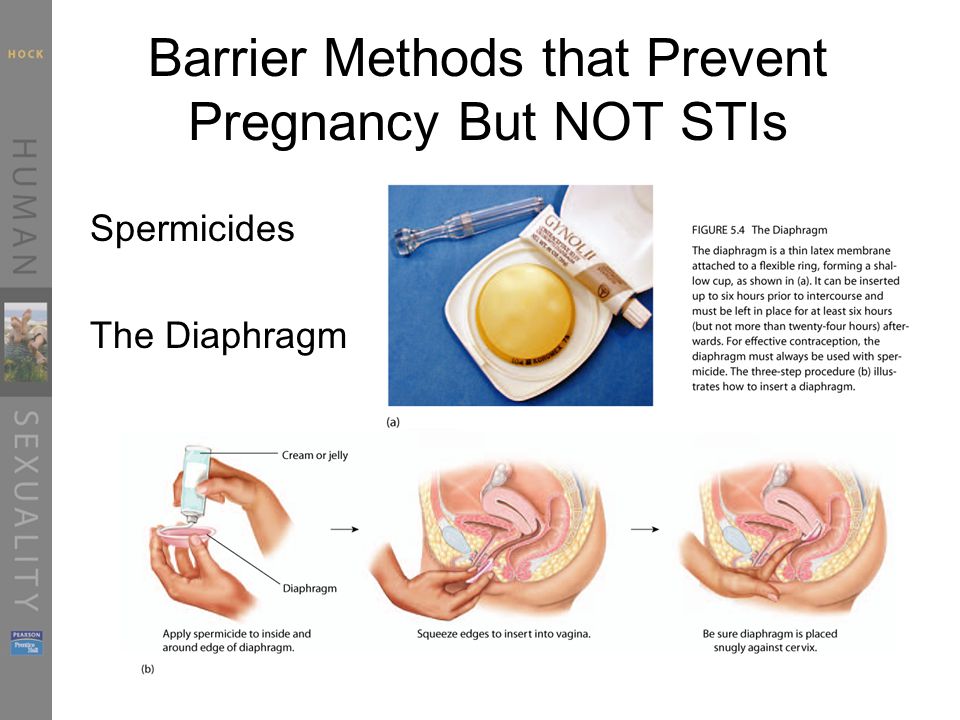 Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
- This brief procedure can be done in the office or the operating room. The following steps occur regardless of the location:
- The woman is in the same position as during a regular pelvic exam, like when a Pap test is done.
- A speculum is placed in the vagina
- A cleansing antibacterial solution is applied to the cervix and vagina
- Numbing medicine is applied to the cervix to decrease cramping
- The cervix is dilated (opened) with thin rods; with early miscarriage, the cervix does not need to be opened much to complete the procedure
- A thin straw-like tube is placed through the open cervixThe pregnancy is removed using a mechanical suction pump attached to the tube
- Everything is removed from the vagina when the procedure is done
You may choose to have the procedure in the office or operating room based on your preferences – different women have different needs.
Office procedure:
- A spouse, partner, friend or relative can be in the room with you
- If desired, oral medications can be taken before the procedure to help you feel more relaxed
- You can eat or drink anything you want before the procedure
- The suction used in the office is most commonly a syringe that creates the suction so no noisy machine is used
- You will usually goes home 15-30 minutes after the procedure and can resume relatively normal activities
- Operating room procedure
- The procedure is done in an outpatient operating suite or in the main hospital
- You will be asleep during the procedure
- You cannot eat or drink anything after midnight on the night before the procedure because you will be receiving anesthesia
- You will feel sleepy for the whole day after the procedure and will need someone to be able to drive you home and be with you for the whole day after the procedure
- The operating room is more appropriate for women with certain medical conditions
After treatment for a miscarriage
Bleeding may continue for several weeks after a miscarriage but tends to be much lighter with a suction aspiration. Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Frequently asked questions about miscarriage
Having one miscarriage does not increase your chances of having another. If you have had only one prior miscarriage, the rate of miscarriage in the next pregnancy is similar to the overall rate in the general population.
No. Working, exercise and sexual activity do not increase the risk of miscarriage.
Patients were told years ago to wait one or two menstrual cycles to wait to get pregnant.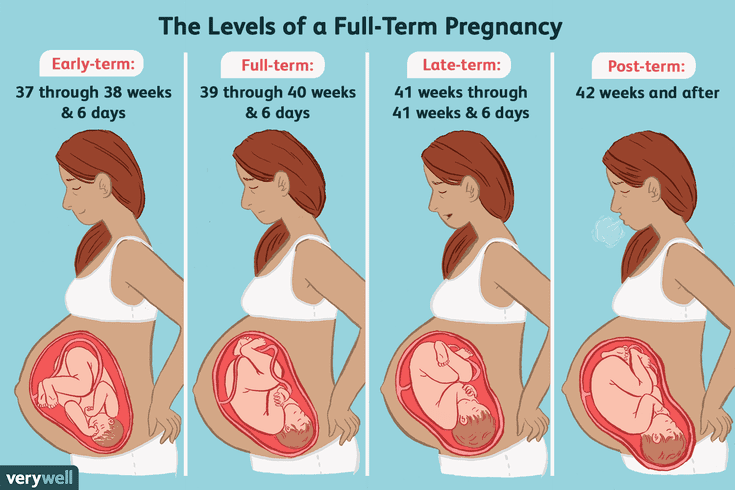 We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
Since most early miscarriages are caused by problems specific to that fertilized egg, and miscarriage overall is relatively common, most experts do not recommend special testing until you have had three early miscarriages (or two miscarriages in women 40 years and older). At that point it is termed "recurrent" miscarriage and further testing may be needed. Studies have shown that even after a woman has experienced three consecutive miscarriages, her chance of the next pregnancy being normal is still about 70%. All women who have a pregnancy loss later in pregnancy should have further testing.
Tips to help support parents after pregnancy loss
UC Davis Health social worker Brenna Rizan, who works within the Department of Obstetrics/Gynecology provides supportive tips and advice for grieving parents, family and friends after pregnancy loss.
Related stories
Miscarriages are more common than people think - KCRA (Interview with Brenna Rizan)
Facebook Live: Discussing miscarriages with Dr. Mitch Creinin
UC Davis Early Pregnancy and Miscarriage Center
404 Page not found
- University
- Manual
- Rectorate
- Appeal to the rector
- Academic Council
- University 90 years old nine0003 Telephone directory
- Documents
- Structure
- University media
- Symbols of BSMU
- Electronic Trust Box
- Comprehensive program for the development of BSMU
- Antiterror
- Information about the educational organization
- Applicant
- Appeal of citizens
- Photo gallery
- Sitemap nine0003 Video Gallery
- Available environment
- Payment by bank card
- University reorganization
- Calendar of events
- Structure and documents nine0003 Decree of the President of the Russian Federation "On the strategy of scientific and technological development of the Russian Federation"
- Clinic of BSMU
- All-Russian Center for Eye and Plastic Surgery
- Clinical dental clinic
- Clinical bases nine0003 Medical records
- About
- Project Office
- Directions of implementation
- Strategic projects
- Mission and strategy
- Digital Pulpit
- Competitions for students
- Reporting nine0003 Media publications
Angiotensin II receptor antagonists (AT1 subtype): pharmacological group
Description0269 1 receptors are one of the new groups of antihypertensive agents.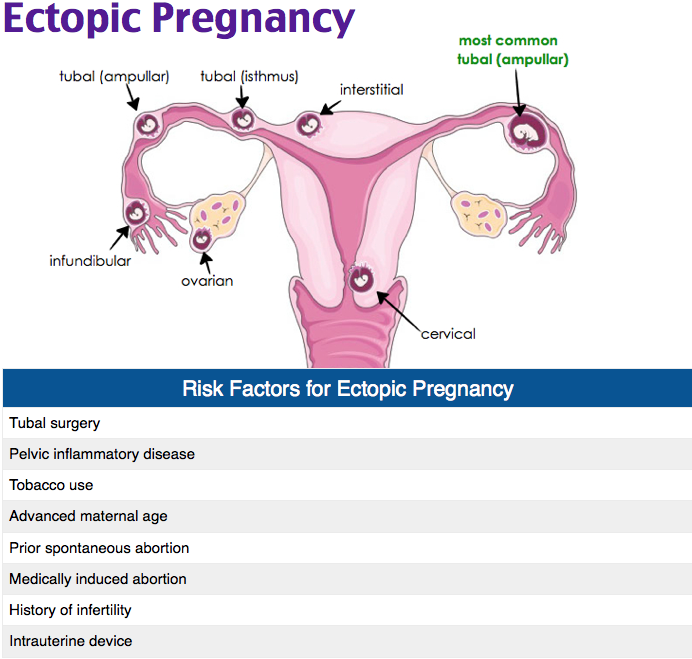 It combines drugs that modulate the functioning of the renin-angiotensin-aldosterone system (RAAS) through interaction with angiotensin receptors.
It combines drugs that modulate the functioning of the renin-angiotensin-aldosterone system (RAAS) through interaction with angiotensin receptors.
RAAS plays an important role in the regulation of blood pressure, the pathogenesis of arterial hypertension and chronic heart failure (CHF), as well as a number of other diseases. Angiotensins (from angio - vascular and tensio - tension) - peptides formed in the body from angiotensinogen, which is a glycoprotein (alpha 2 - globulin) of blood plasma, synthesized in the liver. Under the influence of renin (an enzyme formed in the juxtaglomerular apparatus of the kidneys), the angiotensinogen polypeptide, which does not have pressor activity, is hydrolyzed, forming angiotensin I, a biologically inactive decapeptide, which is easily subjected to further transformations. Under the action of angiotensin-converting enzyme (ACE), which is formed in the lungs, angiotensin I is converted into an octapeptide - angiotensin II, which is a highly active endogenous pressor compound.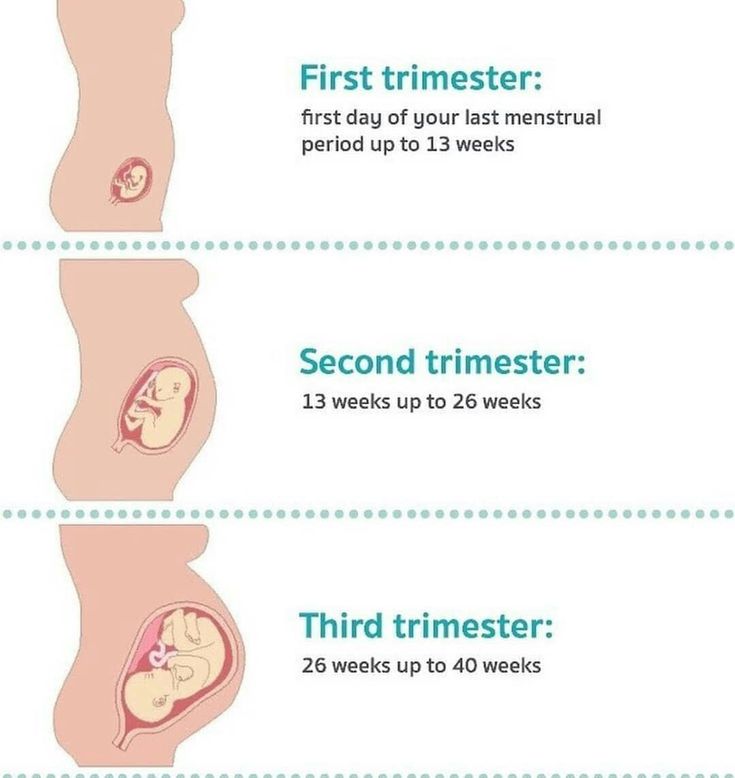 nine0267
nine0267
Angiotensin II is the main effector peptide of the RAAS. It has a strong vasoconstrictor effect, increases OPSS, causes a rapid increase in blood pressure. In addition, it stimulates the secretion of aldosterone, and in high concentrations it increases the secretion of antidiuretic hormone (increased reabsorption of sodium and water, hypervolemia) and causes sympathetic activation. All these effects contribute to the development of hypertension.
Angiotensin II is rapidly metabolized (half-life - 12 min) with the participation of aminopeptidase A with the formation of angiotensin III and then under the influence of aminopeptidase N - angiotensin IV, which have biological activity. Angiotensin III stimulates the production of aldosterone by the adrenal glands, has a positive inotropic activity. Angiotensin IV is thought to be involved in the regulation of hemostasis. nine0267
It is known that in addition to the RAAS of the systemic circulation, the activation of which leads to short-term effects (including such as vasoconstriction, increased blood pressure, aldosterone secretion), there are local (tissue) RAAS in various organs and tissues, incl.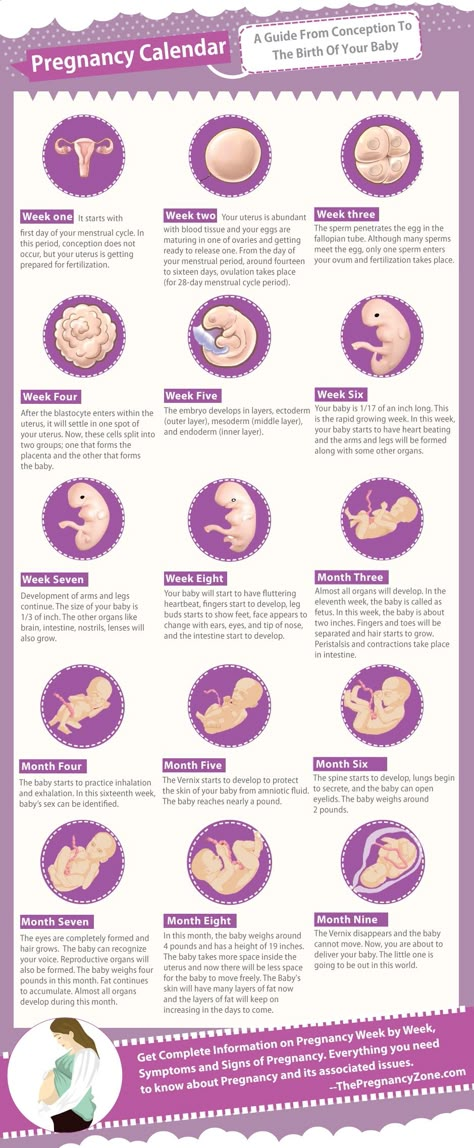 in the heart, kidneys, brain, blood vessels. Increased activity of tissue RAAS causes long-term effects of angiotensin II, which are manifested by structural and functional changes in target organs and lead to the development of such pathological processes as myocardial hypertrophy, myofibrosis, atherosclerotic damage to cerebral vessels, kidney damage, etc.
in the heart, kidneys, brain, blood vessels. Increased activity of tissue RAAS causes long-term effects of angiotensin II, which are manifested by structural and functional changes in target organs and lead to the development of such pathological processes as myocardial hypertrophy, myofibrosis, atherosclerotic damage to cerebral vessels, kidney damage, etc.
It has now been shown that in humans, in addition to the ACE-dependent pathway of converting angiotensin I to angiotensin II, there are alternative pathways involving chymases, cathepsin G, tonin, and other serine proteases. Chymases, or chymotrypsin-like proteases, are glycoproteins with a molecular weight of about 30,000. Chymases have a high specificity for angiotensin I. In various organs and tissues, either ACE-dependent or alternative pathways for the formation of angiotensin II predominate. Thus, cardiac serine protease, its DNA and mRNA were found in human myocardial tissue. The largest amount of this enzyme is found in the myocardium of the left ventricle, where the chymase pathway accounts for more than 80%. Chymase-dependent formation of angiotensin II prevails in the myocardial interstitium, adventitia, and vascular media, while ACE-dependent formation occurs in blood plasma. nine0267
Chymase-dependent formation of angiotensin II prevails in the myocardial interstitium, adventitia, and vascular media, while ACE-dependent formation occurs in blood plasma. nine0267
Angiotensin II can also be formed directly from angiotensinogen by reactions catalyzed by tissue plasminogen activator, tonin, cathepsin G, and others.
The physiological effects of angiotensin II, like other biologically active angiotensins, are realized at the cellular level through specific angiotensin receptors. nine0267
To date, the existence of several subtypes of angiotensin receptors has been established: AT 1 , AT 2 , AT 3 and AT 4 and others. - angiotensin II receptor protein - subtypes AT 1 and AT 2 .
AT 1 -receptors are localized in various organs and tissues, mainly in vascular smooth muscle, heart, liver, adrenal cortex, kidneys, lungs, and in some areas of the brain. nine0267
Most of the physiological effects of angiotensin II, including adverse ones, are mediated by AT 1 receptors:
- arterial vasoconstriction, incl. vasoconstriction of arterioles of the renal glomeruli (especially efferent), increased hydraulic pressure in the renal glomeruli,
vasoconstriction of arterioles of the renal glomeruli (especially efferent), increased hydraulic pressure in the renal glomeruli,
- increased sodium reabsorption in the proximal renal tubules,
- secretion of aldosterone by the adrenal cortex,
- secretion of vasopressin, endothelin-1,
- renin release,
- increased release of norepinephrine from sympathetic nerve endings, activation of the sympathetic-adrenal system,
- proliferation of vascular smooth muscle cells, intimal hyperplasia, cardiomyocyte hypertrophy, stimulation of vascular and heart remodeling processes.
In arterial hypertension against the background of excessive activation of the RAAS, the effects of angiotensin II directly or indirectly mediated by the AT 1 receptors contribute to an increase in blood pressure. In addition, stimulation of these receptors is accompanied by a damaging effect of angiotensin II on the cardiovascular system, including the development of myocardial hypertrophy, thickening of arterial walls, etc.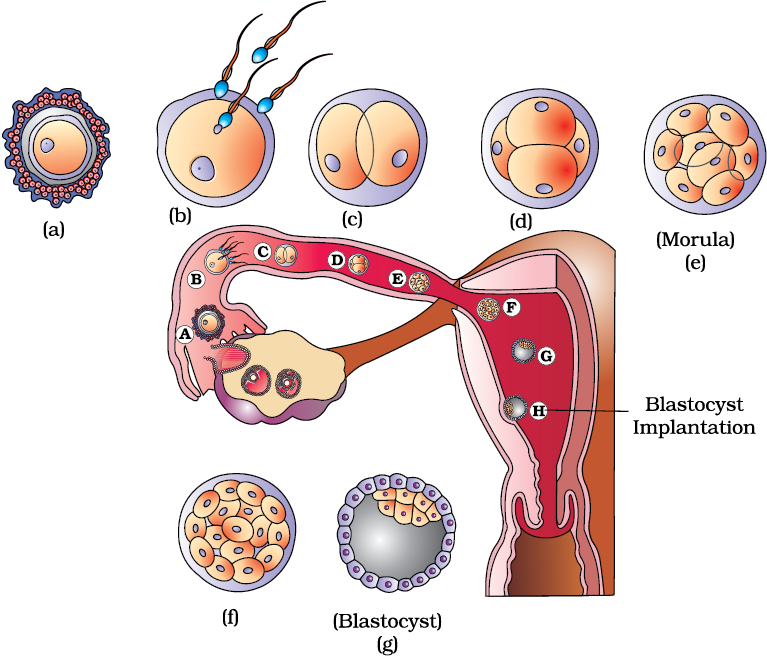
The effects of angiotensin II, mediated by AT 2 receptors, have been discovered only in recent years.
A large number of AT 2 receptors were found in fetal tissues (including the brain). In the postnatal period, the number of AT 2 receptors in human tissues decreases. Experimental studies, in particular in mice in which the gene encoding AT 2 receptors was destroyed, suggest their participation in the processes of growth and maturation, including cell proliferation and differentiation, development of embryonic tissues, and the formation of exploratory behavior. nine0267
AT 2 - receptors are found in the heart, blood vessels, adrenal glands, kidneys, some areas of the brain, reproductive organs, incl. in the uterus, atrezirovannyh ovarian follicles, as well as in skin wounds. It has been shown that the number of AT 2 receptors can increase with tissue damage (including blood vessels), myocardial infarction, and heart failure. It is suggested that these receptors may be involved in the processes of tissue regeneration and programmed cell death (apoptosis). nine0267
It is suggested that these receptors may be involved in the processes of tissue regeneration and programmed cell death (apoptosis). nine0267
Recent studies show that the cardiovascular effects of angiotensin II, mediated by AT 2 receptors, are opposite to those caused by excitation of AT 1 receptors, and are relatively weakly expressed. Stimulation of AT 2 receptors is accompanied by vasodilation, inhibition of cell growth, incl. suppression of cell proliferation (endothelial and smooth muscle cells of the vascular wall, fibroblasts, etc.), inhibition of cardiomyocyte hypertrophy. nine0267
The physiological role of angiotensin II receptors of the second type (AT 2 ) in humans and their relationship with cardiovascular homeostasis is currently not fully understood.
Highly selective AT 2 receptor antagonists (CGP 42112А, PD 123177, PD 123319) have been synthesized and used in experimental studies of RAAS.
Other angiotensin receptors and their role in humans and animals have been little studied.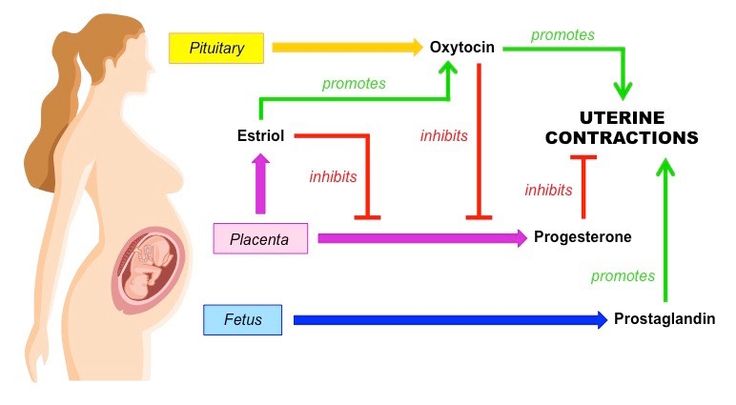
AT 9 subtypes isolated from rat mesangium cell culture0269 1 receptors - AT 1a and AT 1b , differing in affinity for angiotensin II peptide agonists (these subtypes were not found in humans). AT 1c , a subtype of receptors, whose physiological role is not yet clear, has been isolated from rat placenta.
AT 3 - receptors with affinity for angiotensin II, found on the membranes of neurons, their function is unknown. AT 4 receptors are found on endothelial cells. Interacting with these receptors, angiotensin IV stimulates the release of a type 1 plasminogen activator inhibitor from the endothelium. AT 4 receptors are also found on the membranes of neurons, incl. in the hypothalamus, presumably in the brain, they mediate cognitive functions. The affinity for AT 4 receptors has, in addition to angiotensin IV, also angiotensin III.
Long-term studies of the RAAS not only revealed the importance of this system in the regulation of homeostasis, in the development of cardiovascular pathology, influencing the functions of target organs, among which the most important are the heart, blood vessels, kidneys and brain, but also led to the creation of medicinal funds purposefully acting on individual parts of the RAAS. nine0267
nine0267
The scientific basis for the creation of drugs that act by blocking angiotensin receptors was the study of angiotensin II inhibitors. Experimental studies show that angiotensin II antagonists that can block its formation or action and thus reduce the activity of the RAAS are inhibitors of the formation of angiotensinogen, inhibitors of renin synthesis, inhibitors of the formation or activity of ACE, antibodies, angiotensin receptor antagonists, including synthetic non-peptide compounds, specifically blocking AT 1 -receptors, etc.
The first angiotensin II receptor blocker introduced into therapeutic practice in 1971 was saralazine, a peptide compound similar in structure to angiotensin II. Saralazin blocked the pressor action of angiotensin II and lowered the tone of peripheral vessels, reduced the content of aldosterone in plasma, lowered blood pressure. However, by the mid-1970s, the experience of using saralazine showed that it has the properties of a partial agonist and in some cases gives an unpredictable effect (in the form of excessive hypotension or hypertension). At the same time, a good hypotensive effect was manifested in conditions associated with a high level of renin, while against the background of a low level of angiotensin II or with a rapid injection of blood pressure increased. Due to the presence of agonistic properties, as well as due to the complexity of the synthesis and the need for parenteral administration, saralazine has not received wide practical application. nine0267
At the same time, a good hypotensive effect was manifested in conditions associated with a high level of renin, while against the background of a low level of angiotensin II or with a rapid injection of blood pressure increased. Due to the presence of agonistic properties, as well as due to the complexity of the synthesis and the need for parenteral administration, saralazine has not received wide practical application. nine0267
In the early 1990s, the first non-peptide selective AT 1 receptor antagonist, effective when taken orally, losartan was synthesized, which received practical application as an antihypertensive agent.
Currently, several synthetic non-peptide selective AT 1 -blockers - valsartan, irbesartan, candesartan, losartan, telmisartan, eprosartan, olmesartan medoxomil, azilsartan medoxomil, zolarsartan, tazosartan (zolarsartan and tazosartan not yet registered in Russia). nine0267
There are several classifications of angiotensin II receptor antagonists: by chemical structure, pharmacokinetic features, mechanism of binding to receptors, etc. : losartan, irbesartan, candesartan, valsartan, tazosartan;
: losartan, irbesartan, candesartan, valsartan, tazosartan;
- biphenyl netetrazole compounds - telmisartan;
- non-biphenyl netetrazole compounds - eprosartan. nine0267
According to the presence of pharmacological activity, AT 1 receptor blockers are divided into active dosage forms and prodrugs. Thus, valsartan, irbesartan, telmisartan, eprosartan themselves have pharmacological activity, while candesartan cilexetil and azilsartan medoxomil are prodrugs.
In addition, AT 1 -blockers differ depending on the presence or absence of active metabolites. Active metabolites are found in losartan and tazosartan. For example, the active metabolite of losartan, EXP-3174, has a stronger and longer-lasting effect than losartan (in terms of pharmacological activity, EXP-3174 exceeds losartan by 10-40 times). nine0267
According to the mechanism of binding to receptors, AT 1 receptor blockers (as well as their active metabolites) are divided into competitive and non-competitive angiotensin II antagonists.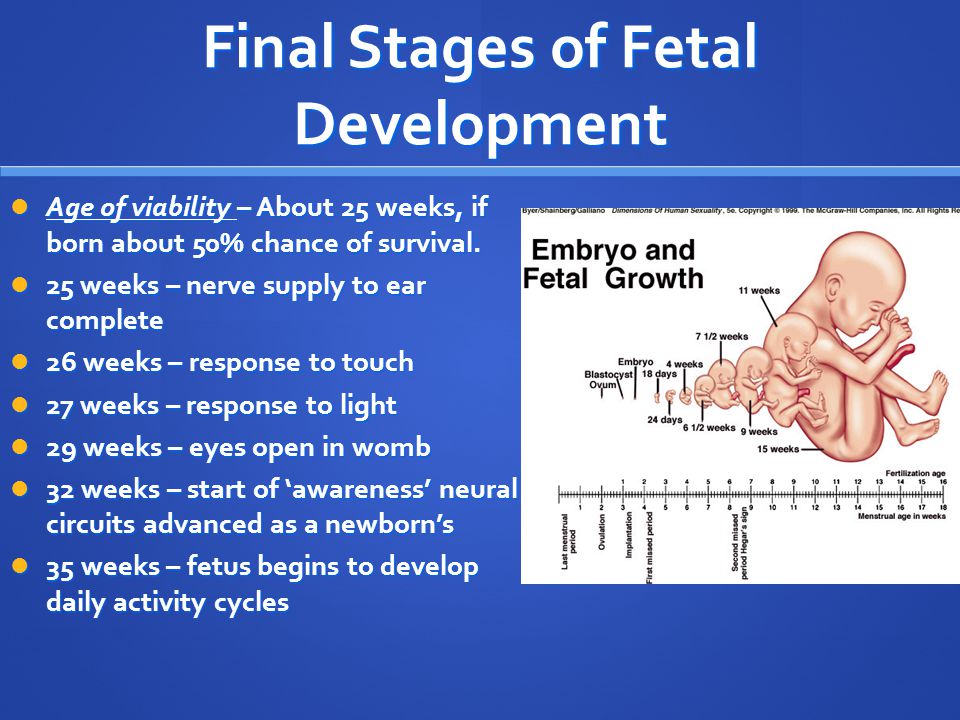 Thus, losartan and eprosartan reversibly bind to AT 1 receptors and are competitive antagonists (i.e., under certain conditions, for example, with an increase in the level of angiotensin II in response to a decrease in BCC, they can be displaced from binding sites), while valsartan , irbesartan, candesartan, telmisartan, as well as the active metabolite of losartan EXP-3174 act as non-competitive antagonists and bind to receptors irreversibly. nine0267
Thus, losartan and eprosartan reversibly bind to AT 1 receptors and are competitive antagonists (i.e., under certain conditions, for example, with an increase in the level of angiotensin II in response to a decrease in BCC, they can be displaced from binding sites), while valsartan , irbesartan, candesartan, telmisartan, as well as the active metabolite of losartan EXP-3174 act as non-competitive antagonists and bind to receptors irreversibly. nine0267
The pharmacological action of this group of drugs is due to the elimination of the cardiovascular effects of angiotensin II, incl. vasopressor.
It is believed that the antihypertensive effect and other pharmacological effects of angiotensin II receptor antagonists are realized in several ways (one direct and several indirect).
The main mechanism of action of drugs in this group is associated with the blockade of AT 1 receptors. All of them are highly selective AT9 antagonists.0269 1 -receptors.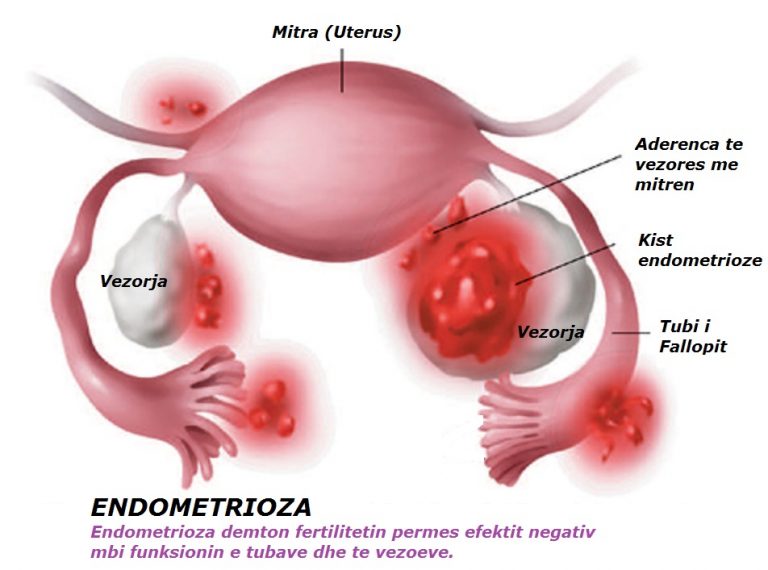 It has been shown that their affinity for AT 1 exceeds that for AT 2 receptors thousands of times: for losartan and eprosartan more than 1 thousand times, for telmisartan - more than 3 thousand, for irbesartan - 8.5 thousand. , the active metabolite of losartan EXP-3174 and candesartan - 10 thousand times, olmesartan - 12.5 thousand times, valsartan - 20 thousand times.
It has been shown that their affinity for AT 1 exceeds that for AT 2 receptors thousands of times: for losartan and eprosartan more than 1 thousand times, for telmisartan - more than 3 thousand, for irbesartan - 8.5 thousand. , the active metabolite of losartan EXP-3174 and candesartan - 10 thousand times, olmesartan - 12.5 thousand times, valsartan - 20 thousand times.
Blockade of AT 1 receptors prevents the development of the effects of angiotensin II mediated by these receptors, which prevents the adverse effect of angiotensin II on vascular tone and is accompanied by a decrease in elevated blood pressure. Long-term use of these drugs leads to a weakening of the proliferative effects of angiotensin II in relation to vascular smooth muscle cells, mesangial cells, fibroblasts, a decrease in cardiomyocyte hypertrophy, etc.
It is known that AT 1 receptors of cells of the juxtaglomerular apparatus of the kidneys are involved in the regulation of renin release (by the principle of negative feedback). Blockade of AT 1 receptors causes a compensatory increase in renin activity, an increase in the production of angiotensin I, angiotensin II, etc.
Blockade of AT 1 receptors causes a compensatory increase in renin activity, an increase in the production of angiotensin I, angiotensin II, etc.
nine0269 2 -receptors and expressed in vasodilation, slowing down of proliferative processes, etc.
In addition, against the background of an increased level of angiotensins I and II, angiotensin-(1-7) is formed. Angiotensin-(1-7) is formed from angiotensin I under the action of neutral endopeptidase and from angiotensin II under the action of prolyl endopeptidase and is another RAAS effector peptide that has a vasodilatory and natriuretic effect. The effects of angiotensin-(1-7) are mediated through the so-called, not yet identified, AT x receptors.
Recent studies of endothelial dysfunction in hypertension suggest that the cardiovascular effects of angiotensin receptor blockers may also be related to endothelial modulation and effects on nitric oxide (NO) production. The obtained experimental data and the results of individual clinical studies are rather contradictory.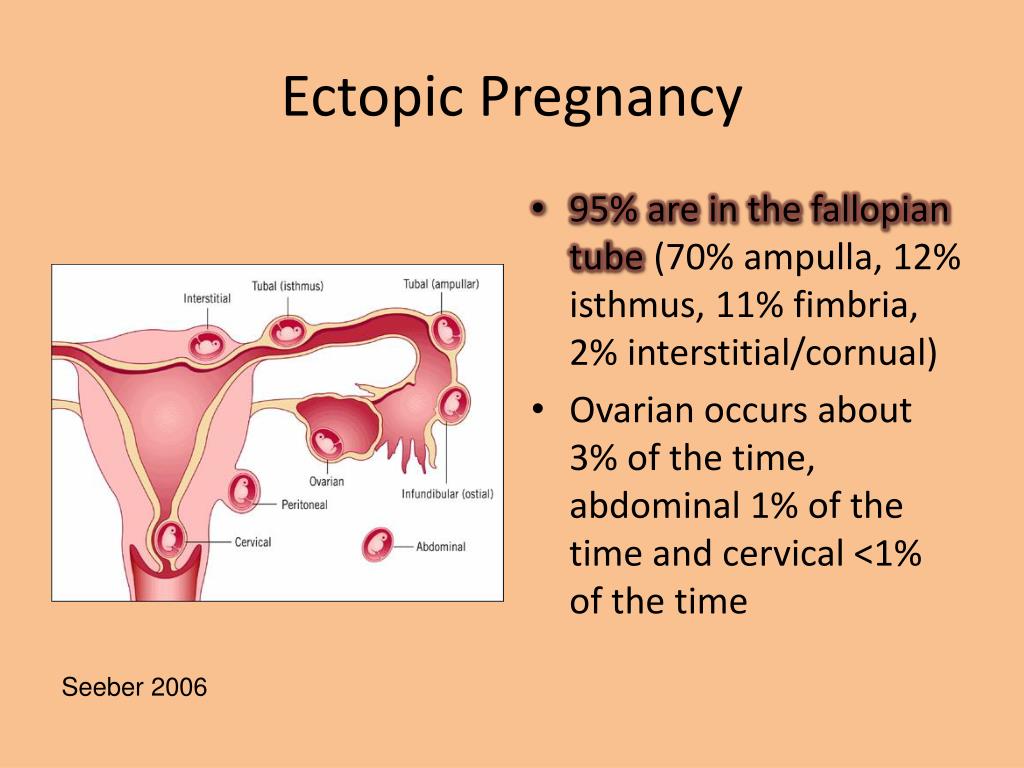 Perhaps, against the background of the blockade of AT 1 receptors, endothelium-dependent synthesis and release of nitric oxide increase, which contributes to vasodilation, a decrease in platelet aggregation and a decrease in cell proliferation. nine0267
Perhaps, against the background of the blockade of AT 1 receptors, endothelium-dependent synthesis and release of nitric oxide increase, which contributes to vasodilation, a decrease in platelet aggregation and a decrease in cell proliferation. nine0267
Thus, the specific blockade of AT 1 receptors allows for a pronounced antihypertensive and organoprotective effect. Against the background of the blockade of AT 1 receptors, the adverse effect of angiotensin II (and angiotensin III, which has affinity for angiotensin II receptors) on the cardiovascular system is inhibited and, presumably, its protective effect is manifested (by stimulating AT 2 receptors), and also develops the action of angiotensin-(1-7) by stimulating AT x -receptors. All these effects contribute to vasodilation and weakening of the proliferative action of angiotensin II in relation to vascular and heart cells.
Antagonists of AT 1 receptors can penetrate the blood-brain barrier and inhibit the activity of mediator processes in the sympathetic nervous system. By blocking the presynaptic AT 1 receptors of sympathetic neurons in the CNS, they inhibit the release of norepinephrine and reduce the stimulation of adrenoreceptors in vascular smooth muscles, which leads to vasodilation. Experimental studies show that this additional mechanism of vasodilatory action is more characteristic of eprosartan. Data on the effect of losartan, irbesartan, valsartan, etc. on the sympathetic nervous system (which manifested itself at doses exceeding therapeutic ones) are very contradictory. nine0267
By blocking the presynaptic AT 1 receptors of sympathetic neurons in the CNS, they inhibit the release of norepinephrine and reduce the stimulation of adrenoreceptors in vascular smooth muscles, which leads to vasodilation. Experimental studies show that this additional mechanism of vasodilatory action is more characteristic of eprosartan. Data on the effect of losartan, irbesartan, valsartan, etc. on the sympathetic nervous system (which manifested itself at doses exceeding therapeutic ones) are very contradictory. nine0267
All AT receptor blockers 1 act gradually, the antihypertensive effect develops smoothly, within a few hours after taking a single dose, and lasts up to 24 hours. With regular use, a pronounced therapeutic effect is usually achieved after 2-4 weeks (up to 6 weeks) treatment.
The pharmacokinetics of this group of drugs make them convenient for use by patients. These medicines can be taken with or without food. A single dose is enough to provide a good hypotensive effect during the day.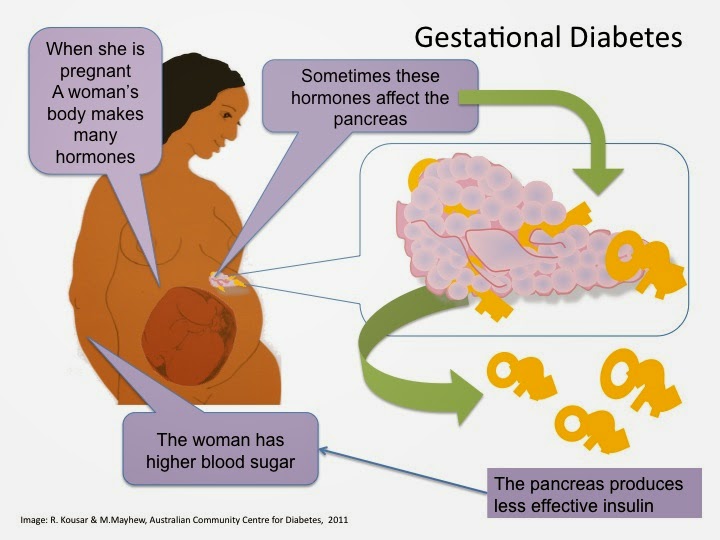 They are equally effective in patients of different sex and age, including patients over 65 years of age. nine0267
They are equally effective in patients of different sex and age, including patients over 65 years of age. nine0267
Clinical studies show that all angiotensin receptor blockers have a high antihypertensive and pronounced organoprotective effect, good tolerance. This allows them to be used, along with other antihypertensive drugs, for the treatment of patients with cardiovascular pathology.
The main indication for the clinical use of angiotensin II receptor blockers is the treatment of arterial hypertension of varying severity. Possible monotherapy (for mild arterial hypertension) or in combination with other antihypertensive drugs (for moderate and severe forms). nine0267
Combination therapy is currently preferred according to WHO/ISH (International Society of Hypertension) recommendations. The most rational for angiotensin II receptor antagonists is their combination with thiazide diuretics. The addition of a low-dose diuretic (eg, 12.5 mg hydrochlorothiazide) can improve the effectiveness of therapy, as evidenced by the results of randomized multicenter trials. Preparations have been created that include this combination - Gizaar (losartan + hydrochlorothiazide), Co-diovan (valsartan + hydrochlorothiazide), Coaprovel (irbesartan + hydrochlorothiazide), Atakand Plus (candesartan + hydrochlorothiazide), Micardis Plus (telmisartan + hydrochlorothiazide), etc. . nine0267
Preparations have been created that include this combination - Gizaar (losartan + hydrochlorothiazide), Co-diovan (valsartan + hydrochlorothiazide), Coaprovel (irbesartan + hydrochlorothiazide), Atakand Plus (candesartan + hydrochlorothiazide), Micardis Plus (telmisartan + hydrochlorothiazide), etc. . nine0267
A number of multicenter studies (ELITE, ELITE II, Val-HeFT, etc.) have shown the efficacy of some AT 1 receptor antagonists in CHF. The results of these studies are mixed, but in general they indicate high efficacy and better (compared with ACE inhibitors) tolerability.
The results of experimental and clinical studies indicate that 1 -subtype AT receptor blockers not only prevent the processes of cardiovascular remodeling, but also cause the regression of left ventricular hypertrophy (LVH). In particular, it was shown that during long-term therapy with losartan, patients showed a tendency to a decrease in the size of the left ventricle in systole and diastole, an increase in myocardial contractility.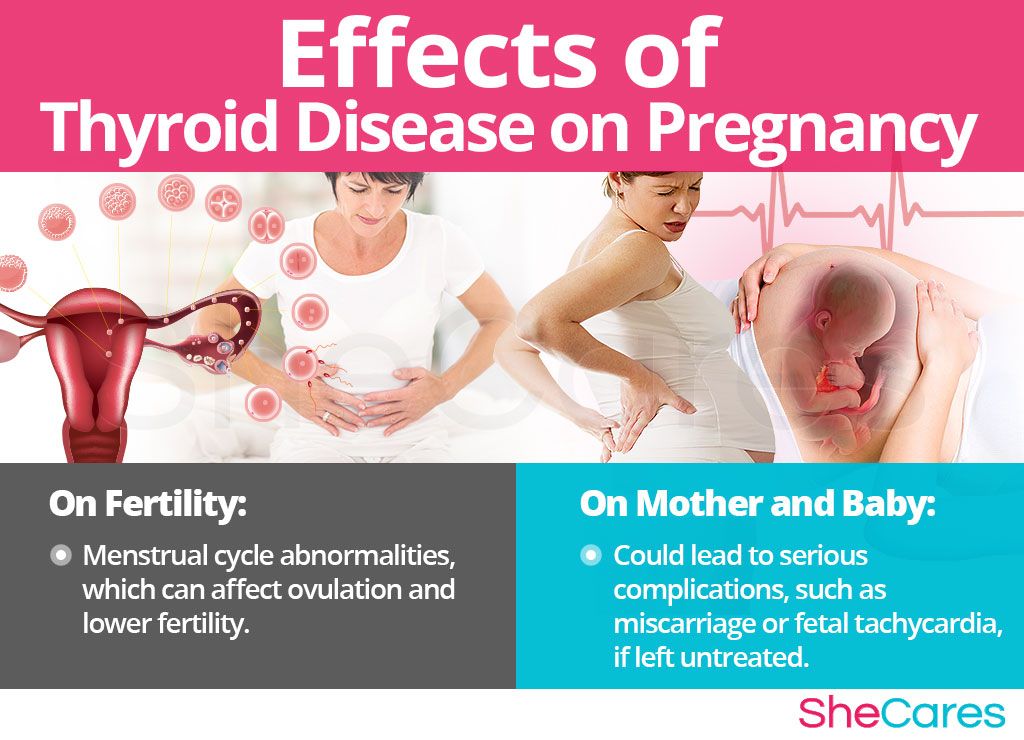 LVH regression has been noted with long-term use of valsartan and eprosartan in patients with arterial hypertension. Some AT 9 receptor blockers0269 1 has been found to improve renal function, incl. with diabetic nephropathy, as well as indicators of central hemodynamics in CHF. So far, clinical observations regarding the effect of these drugs on target organs are few, but research in this area is actively ongoing.
LVH regression has been noted with long-term use of valsartan and eprosartan in patients with arterial hypertension. Some AT 9 receptor blockers0269 1 has been found to improve renal function, incl. with diabetic nephropathy, as well as indicators of central hemodynamics in CHF. So far, clinical observations regarding the effect of these drugs on target organs are few, but research in this area is actively ongoing.
Contraindications to the use of angiotensin AT 1 receptor blockers are individual hypersensitivity, pregnancy, breast-feeding.
Animal data suggest that drugs that act directly on the RAAS can cause fetal harm, fetal and neonatal death. Especially dangerous is the effect on the fetus in the II and III trimesters of pregnancy, because. possible development of hypotension, hypoplasia of the skull, anuria, renal failure and death in the fetus. Direct indications for the development of such defects when taking AT 9 blockers0269 1 -receptors are absent, however, the funds of this group should not be used during pregnancy, and if pregnancy is detected during the treatment period, they must be discontinued.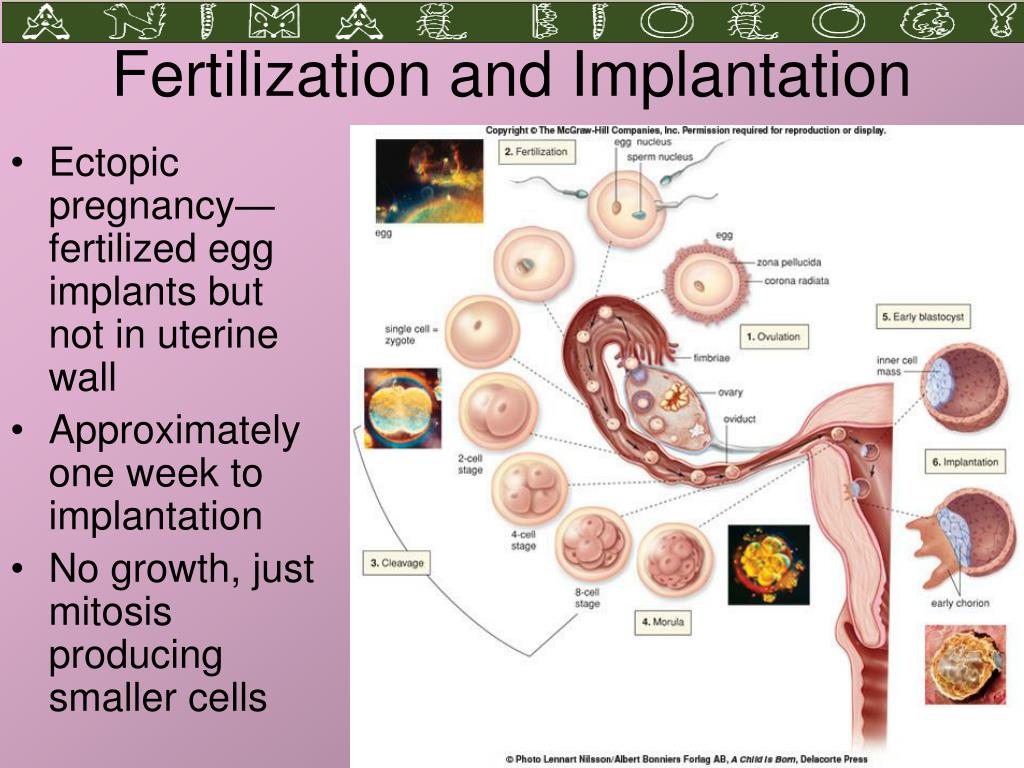
There is no information on the ability of AT 1 receptor blockers to penetrate into breast milk of women. However, in experiments on animals, it has been established that they penetrate into the milk of lactating rats (in the milk of rats, significant concentrations are found not only of the substances themselves, but also of their active metabolites). In this regard, AT 9 blockers0269 1 receptors are not used in lactating women, and if therapy is necessary for the mother, breastfeeding is stopped.
Pediatric use of these drugs should be avoided because their safety and efficacy in children have not been established.
There are a number of limitations for therapy with angiotensin receptor antagonists AT 1 . Caution should be exercised in patients with reduced BCC and / or hyponatremia (during treatment with diuretics, limiting salt intake with diet, diarrhea, vomiting), as well as in patients on hemodialysis, tk. possible development of symptomatic hypotension. An assessment of the risk / benefit ratio is necessary in patients with renovascular hypertension due to bilateral renal artery stenosis or renal artery stenosis of a single kidney, because. excessive inhibition of the RAAS in these cases increases the risk of severe hypotension and renal failure. Caution should be used in aortic or mitral stenosis, obstructive hypertrophic cardiomyopathy. Against the background of impaired renal function, it is necessary to monitor the levels of potassium and serum creatinine. Not recommended for patients with primary hyperaldosteronism, tk. in this case, drugs that inhibit the RAAS are ineffective. There are no sufficient data on the use in patients with severe liver disease (eg, cirrhosis). nine0267
An assessment of the risk / benefit ratio is necessary in patients with renovascular hypertension due to bilateral renal artery stenosis or renal artery stenosis of a single kidney, because. excessive inhibition of the RAAS in these cases increases the risk of severe hypotension and renal failure. Caution should be used in aortic or mitral stenosis, obstructive hypertrophic cardiomyopathy. Against the background of impaired renal function, it is necessary to monitor the levels of potassium and serum creatinine. Not recommended for patients with primary hyperaldosteronism, tk. in this case, drugs that inhibit the RAAS are ineffective. There are no sufficient data on the use in patients with severe liver disease (eg, cirrhosis). nine0267
Side effects reported so far from angiotensin II receptor antagonists are usually mild, transient, and rarely warrant discontinuation of therapy. The overall frequency of side effects is comparable to placebo, as evidenced by the results of placebo-controlled studies.