Passing clots during pregnancy
Blood clots during pregnancy: Symptoms and prevention
There is nothing quite like the feeling of not being able to catch your breath. When I was 22 years old, I had trouble breathing. I eventually went to the hospital where they diagnosed me with a pulmonary embolism—a blood clot in the lung, a rare condition for a person of my age. I later learned that I had a genetic condition that increased my likelihood of developing a blood clot.
My clot was broken up and I was treated for some time afterward with blood thinners, but I knew that in the future I would need to take proactive measures if I were to become pregnant or have surgery. Blood clots during pregnancy are a concern for many expectant mothers, but as I learned, it is possible to manage your high risk.
What is a blood clot?
Blood clotting is a natural process that occurs when blood clumps together to form a gelatinous mass. This process protects your body from bleeding too much when you’ve been injured, as clotting can seal off the wound. Blood clotting (called thrombosis) can also cause complications, especially when it happens internally in your blood vessels.
This can happen in any blood vessel in the body. However, the most common place for abnormal blood clots to occur is in the deep veins of your legs. This is called deep vein thrombosis (DVT). The major concern is that the clot can break free and travel to other parts of the body (lungs are most common), which can lead to serious complications or even death.
Why are pregnant women at greater risk of blood clots?
In pregnancy, the body is primed to clot to prevent blood loss during delivery. While this is important, it also increases the risk of clotting problematically.
It is estimated that pregnant women may be up to five times more likely to experience blood clots than non-pregnant women. There are several reasons for this uptick. Higher-than-normal levels of estrogen during pregnancy are known to increase clotting risk, although the exact mechanism by which this happens is unknown.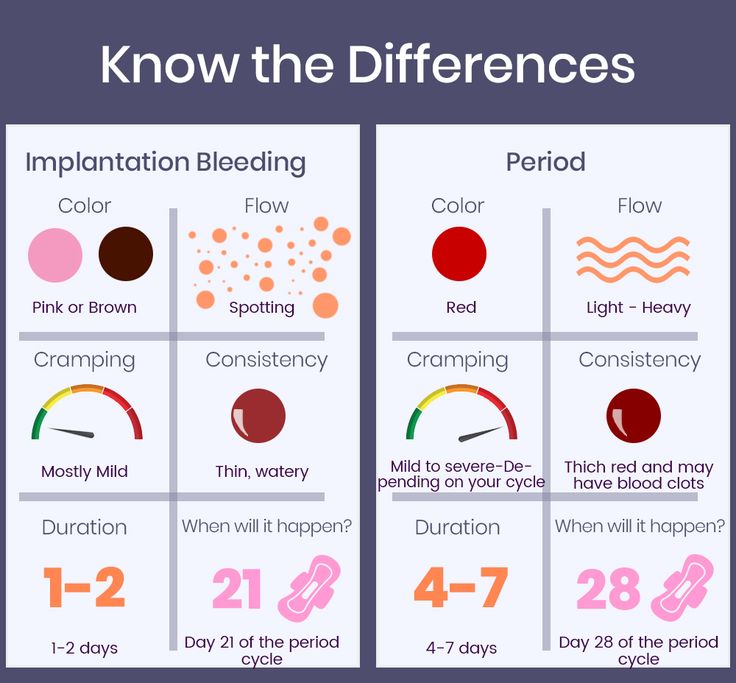 Also, a woman’s blood clots more easily in preparation for childbirth in order to reduce blood loss at delivery. Restricted blood flow may also raise the likelihood of blood clots. As the baby gets larger during pregnancy, it places more pressure on the blood vessels in the pelvic region, resulting in a restriction of blood flow that can also cause blood clots. If bed rest is required, lack of movement can decrease blood flow to the arms and legs, also increasing risk.
Also, a woman’s blood clots more easily in preparation for childbirth in order to reduce blood loss at delivery. Restricted blood flow may also raise the likelihood of blood clots. As the baby gets larger during pregnancy, it places more pressure on the blood vessels in the pelvic region, resulting in a restriction of blood flow that can also cause blood clots. If bed rest is required, lack of movement can decrease blood flow to the arms and legs, also increasing risk.
A blood clot in the lung, also known as a pulmonary embolism, is a leading cause of maternal death for pregnant women in the U.S., according to the CDC. And the risk of developing blood clots isn’t just during the pregnancy—it continues to be a concern for approximately three months after giving birth. Delivery by cesarean section (C-section) nearly doubles your risk after birth.
“Pregnant women are at a higher risk of DVT for several reasons,” says Nisha Bunke, MD, a vein specialist and diplomate of the American Board of Venous and Lymphatic Medicine, “a hypercoagulable state (proteins in the blood make it thicker, and more likely to form clots), an enlarged uterus may put pressure on the veins in the lower abdomen, and the hormones decrease venous tone.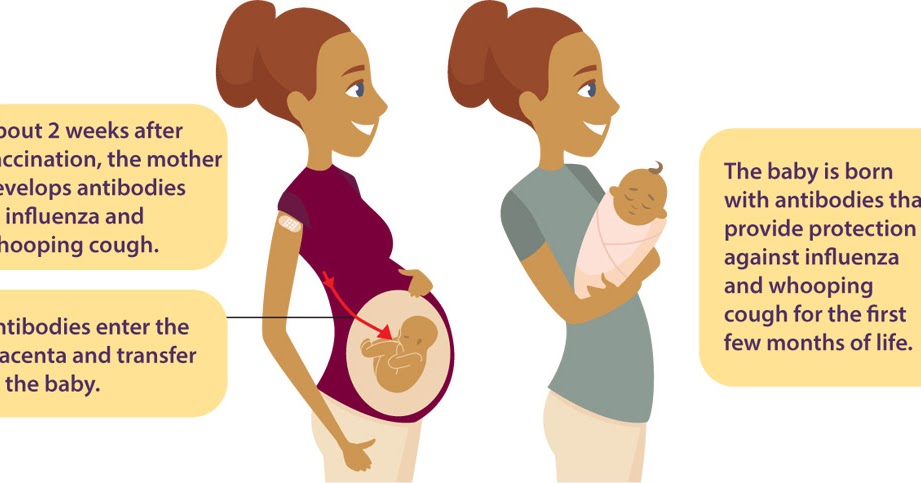 ”
”
Anyone can develop a blood clot during pregnancy, however it is more likely under certain conditions, or for those who already have some risk factors. Dr. Bunke adds that “some women have risk factors that increase their risk of DVT even more during pregnancy, like inherited blood clotting disorders, medical conditions such as lupus and sickle cell disease, obesity, immobility and age over 35.”
Other factors that may increase the risk of clotting during pregnancy are:
- Family history of blood clots
- Multifetal gestation (twins or more)
- Being dehydrated
- Traveling long distances (sitting for long time periods)
- Prolonged stillness, like bed rest during pregnancy
- Other medical conditions
- Transfusion at delivery
- Peripartum cardiomyopathy
- Postpartum hemorrhage
- Pre-eclampsia
What are other risk factors for blood clots?
In addition to pregnancy, the following risk factors can increase your risk of developing a blood clot.
Acquired:
- Smoking
- Being overweight or obese (a BMI of 30 or greater)
- Having a surgery, hospitalization or illness that necessitates prolonged bed rest
- Traveling for long stretches by car or plane with little movement
- Being on estrogen-containing contraceptives or hormone replacement therapy
- Having cancer
Genetic:
- Having a family member who’s had a blood clot
- Having a personal history of blood clots
- Having a personal history of unexplained miscarriages
Condition-related:
- Atherosclerosis
- Diabetes
- High blood pressure
- Vasculitis
- Heart failure
- Irregular heartbeat
- Metabolic syndrome
Additionally, some people may be predisposed to getting blood clots if they have thrombophilias, a group of disorders that increase a person’s risk of thrombosis (abnormal blood clotting). This was my case, with a condition known as Protein C Deficiency.
This was my case, with a condition known as Protein C Deficiency.
Symptoms of blood clots during pregnancy
“The most obvious symptom of DVT is swelling and heavy pain or extreme tenderness in one of your legs,” says Kendra Segura, MD, a board-certified OB-GYN in Southern California. Other symptoms include:
- Swelling
- Pain in the legs while in motion
- Skin feels warm or tender
- Redness, usually behind the knee
- A heavy, painful sensation
Dr. Segura says if you are experiencing these symptoms you must seek medical attention immediately. Your healthcare provider may require further testing because “it’s not always easy to diagnose DVT in pregnancy from symptoms alone,” she says.
What problems are associated with blood clots during pregnancy?
Blood clots during pregnancy can increase your risk of complications including:
- Blood clots in the placenta that can inhibit blood flow to your baby, causing damage to a developing fetus.

- Heart attack can occur if a blood clot blocks blood flow to the heart.
- Intrauterine growth restriction (IUGR), or when your baby does not grow as expected, may occur.
- Miscarriage can occur before week 20 of your pregnancy.
- Placental insufficiency may occur, reducing the supply of necessary food and oxygen to your baby.
- Preeclampsia, a dangerous condition marked by high blood pressure and high levels of protein in the urine, may occur after week 20 in your pregnancy or immediately after childbirth. This can be fatal if not treated.
- Premature birth, in which your baby is born prior to week 37 of pregnancy, may occur.
- Pulmonary embolism, or a blood clot that moves to the lung, can potentially lower your blood oxygen levels and damage your organs, even leading to death.
- Stillbirth, or death of a baby after week 20 of pregnancy, may occur.

- Stroke can occur if a blood clot blocks one of the blood vessels that supplies blood to the brain or causes a blood vessel in the brain to burst.
- Sudden death
- Thrombosis occurs when a blood clot inside of a blood vessel impedes blood flow. Central vein thrombosis (CVT) occurs in the brain, and deep vein thrombosis usually occurs in the leg.
- Venous thromboembolism occurs if a blood clot travels to the brain, lungs, or heart.
Bleeding during early pregnancy
Sometimes during pregnancy, women pass blood clots vaginally, which is an understandable cause of concern.
In the first trimester of pregnancy (first three months), women may bleed as a result of implantation (where the fertilized egg attaches to the uterine wall) or due to early pregnancy loss (miscarriage). Implantation bleeding is usually light and not enough to soak a pantiliner. While not all cases of passing clots within the first 12 weeks of pregnancy are indicative of a loss, vaginal bleeding during pregnancy can be indicative of a complication.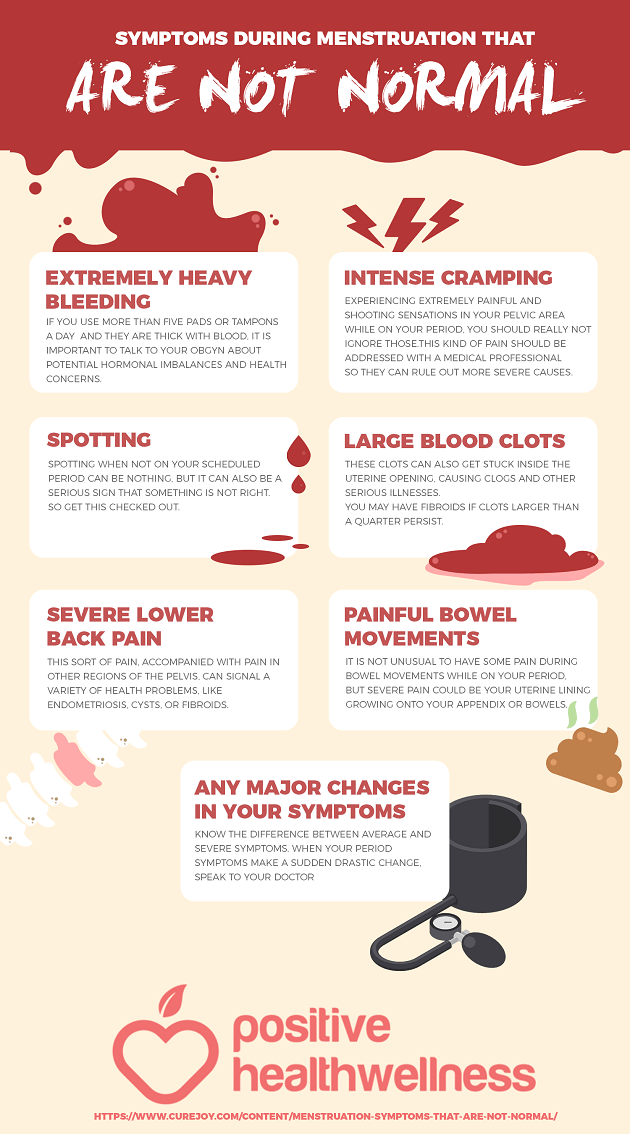
For example, bleeding during the first trimester of pregnancy may be caused by a cervical infection, subchorionic hematoma (bleeding from the membranes surrounding the fetus), cervical polyps, ectopic pregnancy, or molar pregnancy (in which a fertilized egg develops into abnormal tissue). That’s why if you experience bleeding of any kind–including blood clots, it’s best to follow up with your obstetrician, gynecologist, or another healthcare professional.
Blood clots that develop in the body can increase the risk of miscarriage, or loss of a fetus prior to 20 weeks of pregnancy. Signs of a miscarriage include vaginal spotting or bleeding, abdominal cramping, back pain, and passing fluid, tissue or blood clots from the vagina. Light vaginal bleeding often occurs during the first trimester, but if you are bleeding or passing blood clots or tissue, seek immediate medical attention and bring the discharge to your provider.
Bleeding in the second and third trimesters
In the second and third trimesters, bleeding could be caused by a variety of factors. These may include miscarriage, preterm labor, or obstetric abnormalities including placenta previa, or placental abruption. Bleeding and especially passing clots during pregnancy can be a sign of miscarriage, preterm labor, or other complications, so make sure to contact your healthcare provider if you experience bleeding.
These may include miscarriage, preterm labor, or obstetric abnormalities including placenta previa, or placental abruption. Bleeding and especially passing clots during pregnancy can be a sign of miscarriage, preterm labor, or other complications, so make sure to contact your healthcare provider if you experience bleeding.
How to prevent and treat blood clots in pregnancy
When it comes to DVT in pregnancy, prevention is key. In my own case, I was known to have a higher risk due to a thrombophilic disorder, as well as a history of previous clots. This meant that I was given an injectable low-molecular-weight Heparin (LMWH) drug (Fragmin coupons | Fragmin details) for the duration of my pregnancy as a preventive measure.
There are also other preventative measures that can help lower your risk of clots, Dr. Segura says, including:
- Wearing compression stockings
- Keeping well-hydrated
- Staying active (“Regular exercise improves circulation,” Dr.
 Segura notes.)
Segura notes.) - Avoid prolonged sitting or bed rest, travel can also be considered prolonged bed rest
- Avoiding smoking
- Communicating any other medical conditions to your doctor
- Keep your blood pressure normal
Although the development of blood clots during pregnancy can be dangerous, they are still fairly uncommon—and treatable. Due to associated risks to you and your developing baby, getting diagnosed and treated as soon as possible is crucial.
Anticoagulant medications (also known as blood thinners) can be prescribed to help to break up the clot and get the blood moving again. Dr. Segura says that both Heparin and low-molecular-weight Heparin are safe in pregnancy for mother and baby. The main side effect of taking blood thinners is an increased risk of bleeding, so your doctor will monitor you as the pregnancy progresses.
Blood clots and pregnancy | March of Dimes
Anyone can develop a blood clot but pregnant women are at higher risk during pregnancy and after giving birth.
Blood clots can cause other health problems in pregnancy but there are ways to prevent and protect you and your baby.
It is important to know the signs of a blood clot and factors that may increase your risk for a blood clot.
Tell your health care provider if you or someone in your family has had problems with blood clots.
A blood clot (also called a thrombosis) is a mass or clump of blood that forms when blood changes from a liquid to a solid. The body normally makes blood clots to stop the bleeding after a scrape or cut. But sometimes blood clots can partly or completely block the flow of blood in a blood vessel, like a vein or artery.
Anyone can develop a blood clot, but you are at higher risk for a blood clot during pregnancy and up to 3 months after giving birth to your baby. Most women with blood clotting conditions have healthy pregnancies. But these conditions may cause problems for some pregnant women. In severe cases, they can cause death for both mom and baby. But testing and treatment can help protect and save both you and your baby.
But testing and treatment can help protect and save both you and your baby.
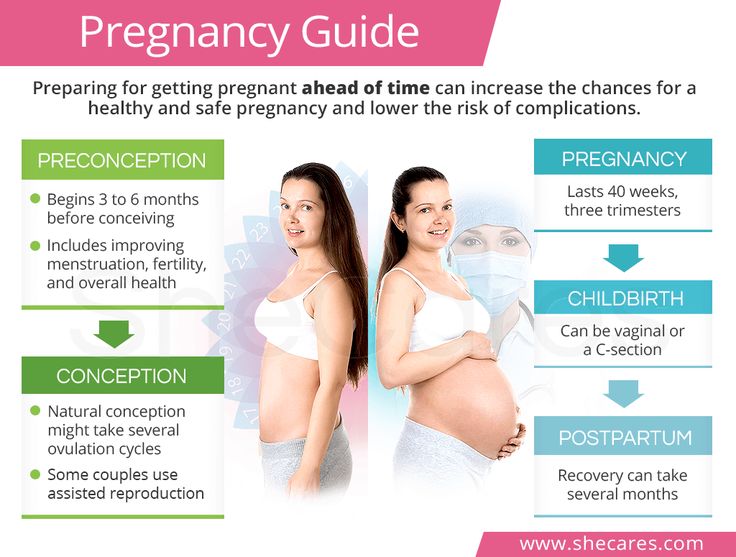
If you’re pregnant or trying to get pregnant and have had problems with blood clots in the past, tell your health care provider at a preconception checkup (before pregnancy) or at your first prenatal care checkup.
If you or someone in your family like your parent, brother or sister has had problems with blood clots, talk to your provider. Blood clots may run in your family. You may also talk to your provider about getting a blood test to see if you have a thrombophilia. This is a health condition that increases your chances of making abnormal blood clots. Some pregnant women with thrombophilias need treatment with medicines called blood thinners. They stop clots from getting bigger and prevent new clots from forming.
Why are pregnant women at greater risk for blood clots?
Pregnant women are 5 times more likely to experience a blood clot compared to women who are not pregnant. This may be because:
This may be because:
- When you’re pregnant, your blood clots more easily to lessen blood loss during labor and delivery.
- In pregnant women, the blood may flow less to the legs later in pregnancy because the growing baby presses upon blood vessels around your pelvis.
- When you’re pregnant you may experience less movement or immobility (not moving a lot) like when you’re on bed rest or recovering from giving birth.
What are other reasons people may be at risk for having blood clots?
Certain things make you more likely than others to have a blood clot. These are called risk factors. Having a risk factor doesn’t mean for sure that you’ll have a blood clot. But it may increase your chances. Talk to your provider about what you can do to help reduce your risk.
Risk factors for blood clots include:
- Having certain health conditions, like a thrombophilia, high blood pressure, diabetes or being overweight or obese.
 A family history of blood clotting problems also increases your chances of blood clots.
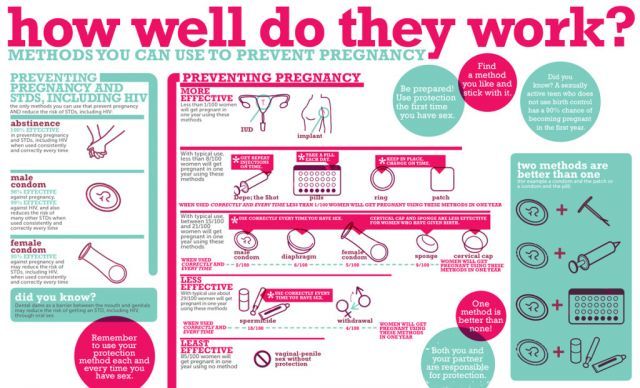
A family history of blood clotting problems also increases your chances of blood clots. - Taking certain medicines, like birth control pills or estrogen hormones. These medicines can increase the risk of clotting. If you’ve had problems with blood clots or thrombophilias or have a family history of these conditions, birth control pills may not be safe for you to use. Talk to your provider about other birth control options.
- Smoking. Smoking damages the lining of blood vessels, which can cause blood clots to form.
- Having surgery, like a cesarean section (also called c-section). A c-section is a surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. The American College of Obstetricians and Gynecologists (ACOG) recommends that doctors help prevent blood clots in women during a c-section.
 This may include using compression devices that put pressure on your legs to help keep your blood flowing during the c-section.
This may include using compression devices that put pressure on your legs to help keep your blood flowing during the c-section. - Being dehydrated. This means you don’t have enough water in your body. Dehydration causes blood vessels to narrow and your blood to thicken, which makes you more likely to have blood clots.
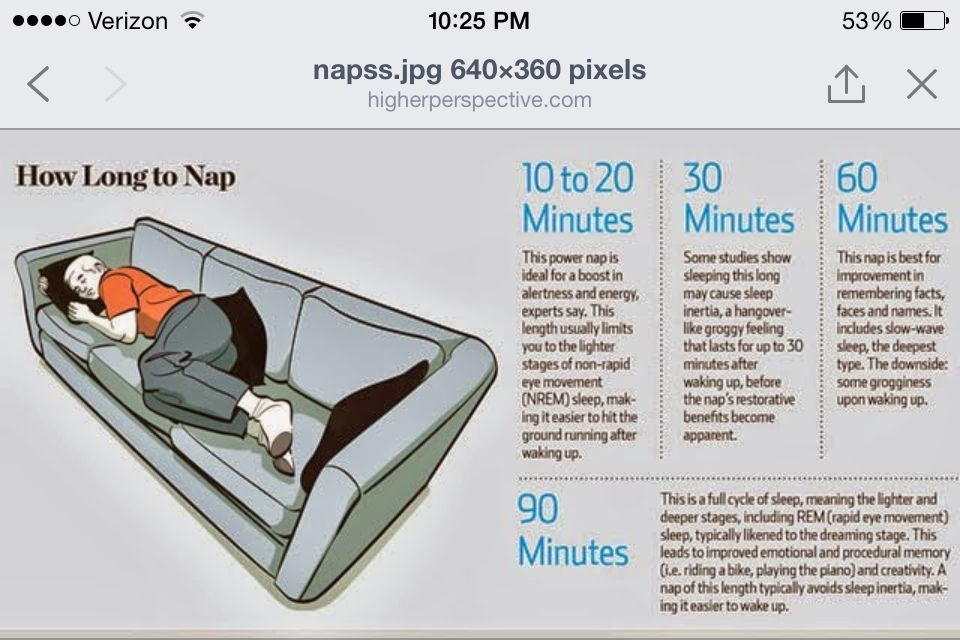
- Not moving around much. This may be because you’re on bed rest during pregnancy or recovering from surgery or an accident. Being still for long periods of time can lead to poor blood flow, which makes you more likely to have blood clots. Even sitting for long periods of time, like when traveling by car or plane for 4 hours or more, can increase your chances of having a blood clot.
- Having a baby. You’re more likely to have a blood clot in the first 6 weeks after birth than women who haven’t given birth recently.
What problems can blood clots cause during pregnancy?
If you have a blood clot or a kind of thrombophilia called antiphospholipid syndrome (also called APS), you may be more likely to have complications that can affect your health and your baby’s health, including:
Blood clots in the placenta. The placenta grows in your uterus (womb) and supplies the baby with food and oxygen through the umbilical cord. A blood clot in the placenta can stop blood flow to your baby and harm your baby.
The placenta grows in your uterus (womb) and supplies the baby with food and oxygen through the umbilical cord. A blood clot in the placenta can stop blood flow to your baby and harm your baby.
Heart attack. This usually happens when a blood clot blocks blood and oxygen flow to the heart. Without blood and oxygen, the heart can’t pump blood well, and the affected heart muscle can die. A heart attack can lead to lasting heart damage or death.
Intauterine growth restriction (also called IUGR). This is when your baby grows poorly in the womb.
Miscarriage. A miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
Placental insufficiency. This is when the placenta doesn’t work as well as it should so your baby gets less food and oxygen.
Preeclampsia. This condition that usually happens after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has both protein in her urine and high blood pressure.
It’s when a pregnant woman has both protein in her urine and high blood pressure.
Premature birth. This is when your baby is born before 37 weeks of pregnancy.
Pulmonary embolism (also called PE). An embolism is a blood clot that moves from where it formed to another place in the body. When the clot moves to a lung, it’s a PE. PE can cause low oxygen levels in your blood and damage your body organs. It’s an emergency and a leading cause of death during pregnancy. Signs and symptoms of PE may include:
- Trouble breathing
- Fast or irregular heartbeat
- Chest pain
- Fainting
- Coughing up blood
Stillbirth. This is when a baby dies in the womb before birth but after 20 weeks of pregnancy.
Stroke. This happens when a blood clot blocks a blood vessel that brings blood to the brain, or when a blood vessel in the brain bursts open. Pregnancy and childbirth cause strokes in about 8 in 100,000 women. Stroke can cause lasting damage to the body or death.
Pregnancy and childbirth cause strokes in about 8 in 100,000 women. Stroke can cause lasting damage to the body or death.
Thrombosis. This happens when a blood clot forms in a blood vessel and blocks blood flow. It most often happens in the deep veins of the legs but can be in other places of the body:
- Cerebral vein thrombosis (also called CVT). This happens when a blood clot forms in a vein in the brain. CVT can lead to stroke. Signs and symptoms include headache, vision problems and seizures.
- Deep vein thrombosis (also called DVT). This happens when a blood clot forms in a vein deep in the body, usually in the lower leg or thigh. DVT can be diagnosed with ultrasound or other imaging tests. Signs and symptoms may include warmth and tenderness over the vein and pain, swelling or skin redness in the affected area.
Venous thromboembolism (also called VTE). This happens when a blood clot breaks off and travels through blood to vital organs, like the brain, lungs or heart. This condition includes DVT and PE. VTEs that block blood vessels in the brain or heart can cause stroke or heart attack.
This happens when a blood clot breaks off and travels through blood to vital organs, like the brain, lungs or heart. This condition includes DVT and PE. VTEs that block blood vessels in the brain or heart can cause stroke or heart attack.
How are these conditions treated?
Your provider may use tests like ultrasound or magnetic resonance imaging (also called MRI) to find out if you have a blot clot or clotting conditions. Ultrasound uses sound waves and a computer screen to make a picture of a baby in the womb. MRI uses magnets and computers to make a clear picture of the inside of the body. These tests are painless and safe for you and your baby.
If you’re pregnant and have a clotting condition, you may need to go for prenatal care checkups more often than women who don’t have these blood clot conditions. At these visits, your provider checks your blood pressure and can use other tests, like blood tests, to monitor your health.
Your provider also checks your baby’s health in the womb using tests like:
- Ultrasound to check your baby’s growth and development.
 She may use a special kind of ultrasound called Doppler to check your baby’s blood flow in the umbilical artery, a blood vessel in the umbilical cord. The umbilical cord connects your baby to the placenta. It carries food and oxygen from the placenta to the baby.
She may use a special kind of ultrasound called Doppler to check your baby’s blood flow in the umbilical artery, a blood vessel in the umbilical cord. The umbilical cord connects your baby to the placenta. It carries food and oxygen from the placenta to the baby. - Fetal heart rate monitoring (also called a nonstress test or NST). This test checks your baby’s heart rate in the womb and sees how the heart rate changes when your baby moves. Your provider uses this test to make sure your baby’s getting enough oxygen.
During pregnancy your provider may give you a blood thinner called heparin (low-molecular weight heparin or unfractionated heparin). If you have APS, your provider may instruct you to take heparin along with low-dose aspirin. Your provider also may refer you to a hematologist. This is a doctor who treats blood conditions.
After you give birth, your provider may continue to treat you with heparin. Or she may treat you with a blood thinner called warfarin. Warfarin is safe to take after pregnancy, even if you’re breastfeeding. Warfarin is not safe to take during pregnancy because it may cause birth defects.
Warfarin is safe to take after pregnancy, even if you’re breastfeeding. Warfarin is not safe to take during pregnancy because it may cause birth defects.
Don’t take combined hormonal methods of birth control during the first 21-42 days after delivery. The risk of DVT is highest in the first 21 days.
How can I safely keep up with my prenatal care appointments during the COVID-19 pandemic?
During the coronavirus disease 2019 pandemic (COVID-19) your prenatal care visits may change. Ask your provider how he will monitor your health and do the tests you need while keeping you and your baby safe from COVID-19.
Providers are taking steps to prevent the spreading of COVID-19 by using telehealth or telemedicine. Telehealth or telemedicine are health visits where you talk to your provider by phone or by videocall, instead of going to his office. You will need either a phone, tablet or computer for a telehealth visit and in some cases you may need access to the internet. Let your provider know if you are unable to have telehealth visits due to lack equipment or any other reason. Ask any questions you may have about keeping up with your ultrasounds and other tests while avoiding getting COVID-19.
Let your provider know if you are unable to have telehealth visits due to lack equipment or any other reason. Ask any questions you may have about keeping up with your ultrasounds and other tests while avoiding getting COVID-19.
What can I do to reduce my risk of blood clots?
- Know the signs and symptoms of a blood clot. On an affected limb like a leg or arm, you may notice swelling, pain or tenderness that was not caused by an injury, warm skin when you touch it or redness and discoloration. Contact your provider if you experience any of these symptoms.
- Talk to your provider about your risk. If you or a family member like a parent, brother or sister have had blood clots before, tell your provider.
- Move or stretch on long trips. If you sit for more than 4 hours on a trip, try to move your legs often. If you can walk around, you may do so. If you can’t, you may try seated leg stretches like extending your legs straight out and moving your ankles to move your toes toward and away from you.
 You may also pull your knee to your chest and hold it there with your hands for 15 seconds.
You may also pull your knee to your chest and hold it there with your hands for 15 seconds. - Follow other travel tips for reducing risk of blood clots. These include drinking lots of fluids like water, wearing loose-fitted clothing or wearing special stockings that compress your legs below the knee. Talk to your provider before trying these stockings.
- Follow your provider’s instructions during pregnancy and after giving birth. Your provider may give you medications like blood thinners or ask you to come in for additional prenatal care checkups.
Last reviewed September 2022
More information
- Shane Foundation
- Stop The Clot, Spread the Word™ campaign
Uterine bleeding: description of the disease, causes, symptoms, cost of treatment in Moscow
Uterine bleeding is the discharge of blood from the uterine cavity. Unlike the normal menstrual cycle of a woman, it is characterized by abundance, intensity, and duration. Bleeding is due to a serious disease or pathology. In any case, the manifestation of this disease should not proceed without medical attention. Girls of any age are at risk. Even in the first days after uterine life, bloody discharge from the genitals can be observed. nine0003
Bleeding is due to a serious disease or pathology. In any case, the manifestation of this disease should not proceed without medical attention. Girls of any age are at risk. Even in the first days after uterine life, bloody discharge from the genitals can be observed. nine0003
Every woman should know her cycle. It is considered normal if it is regular, occurs monthly and lasts, on average, 5 days. They start out sparsely, gain in abundance towards the middle, and just as slowly go down. A healthy woman has no pain syndromes during menstruation. Everything else is a deviation or congenital pathology of the uterus. It can also mean a serious gynecological disease, hormonal failure. If menstruation occurs with pain, dizziness and weakness, contact your gynecologist immediately. nine0003
It should be understood that the onset of early menstruation in girls under the age of 11, as well as the resumption of bloody discharge in women after menopause (after 55 years), is a serious pathological abnormality, and should not proceed without medical supervision. There is no menstruation during pregnancy.
There is no menstruation during pregnancy.
Sometimes, within the normal range, there may be small blood discharge that occurs during periods of menstruation. The cause may be a hormonal failure as a result of ovulation. The walls of the vessels thin out a little, so blood blotches can come out along with the secretions. Duration 1 to 2 days maximum. Also, colds and inflammatory processes can have such a side effect. nine0003
This pathology has the first and main symptom - this is the discharge of blood from the vagina. The amount of blood loss in a woman increases dramatically. This can be noticed when changing special hygiene products too often. The cycle lasts more than 7 days. Its interval changes. After sexual intercourse, bleeding is observed. Bleeding after menopause, when the cycle has been stopped for a long time.
Cause. Types of bleeding.
The cause of uterine bleeding is ovarian dysfunction. There is a failure in the system of work of the hypothalamus, pituitary gland and ovaries. The release of the pituitary hormone is disrupted, which provokes the immaturity of the follicle. Ovulation and the menstrual cycle are disturbed. The follicle does not mature in the ovary and the corpus luteum does not mature. The production of estrogen and progesterone stops. The endometrium is shed, resulting in uterine bleeding. It stands out for a long time and plentifully. nine0003
The release of the pituitary hormone is disrupted, which provokes the immaturity of the follicle. Ovulation and the menstrual cycle are disturbed. The follicle does not mature in the ovary and the corpus luteum does not mature. The production of estrogen and progesterone stops. The endometrium is shed, resulting in uterine bleeding. It stands out for a long time and plentifully. nine0003
During bleeding, the risk of developing diseases of the uterus and adnexal system, cancer, mastopathy, and adenoma carcinoma increases.
There are many reasons that can cause uterine bleeding. It is necessary to determine the type of blood loss, and understand what caused it. The cause can be both a disease of the genital organs and a failure in their functions.
Non-genital disorders include the following:
- nine0002 Some infectious diseases (measles, influenza).
-
Cirrhosis of the liver.
-
Hypertension.
-
Atherosclerosis.
-
Urinary disorders.
-
Changes in the thyroid gland.
-
Blood diseases. nine0003
Bleeding may begin during gestation. This can carry a number of reasons, for example, an ectopic pregnancy, as well as:
-
scar on the uterus;
-
endometritis;
-
fibroids;
-
chorionepitheloma;
-
birth canal injuries; nine0003
-
ovarian pathology;
-
uterine rupture;
-
destruction of uterine tissue;
-
departed placenta;
-
placental abruption or previa.
Bleeding during pregnancy
Bleeding can also occur in a woman who is not carrying a child. Can be called: nine0003
-
gross sexual activity;
-
taking contraceptives;
-
trauma to the external part of the genitals;
-
any injury to the uterus;
-
inflammatory processes such as vaginitis, erosion, cervicitis;
-
cyst and its rupture; nine0003
-
ovarian rupture;
-
intrusion of mucosa into uterus;
-
benign and malignant tumors, such as fibroids;
-
menopausal, juvenile and reproductive bleeding.
Menopausal bleeding
With menopause, women may experience uterine bleeding. They are of a different nature. This comes from the frequency of ovulation and the production of hormones. A fairly common occurrence, but you should consult a specialist. They may also indicate tumors. The reason for the urgent visit to the doctor is: nine0003
-
Abundant discharge that special hygiene products cannot cope with.
-
Discharge with clots.
-
Exceeding the duration of menstruation by more than 3 days.
-
Severe pain syndrome.
-
Remember that they can indicate polyps, fibroids, imbalances, tumors and other serious diseases of the female reproductive system. nine0003
Bleeding due to hormonal imbalance
With a change or violation of the hormonal system, a woman may experience uterine bleeding. Women of all ages are prone to this problem.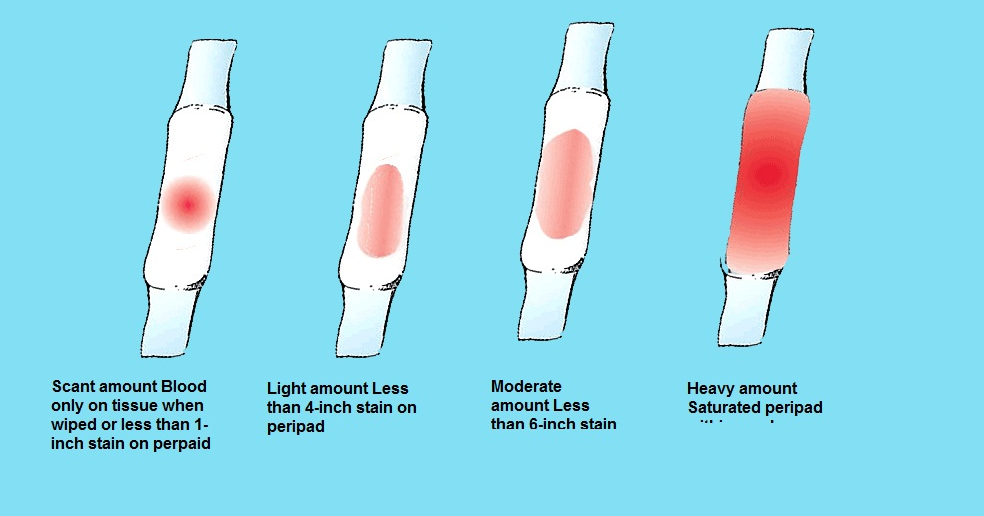 With improper brain function, the level and production of the hormone is not controlled. An example of such a disease is the pathology of the pituitary gland.
With improper brain function, the level and production of the hormone is not controlled. An example of such a disease is the pathology of the pituitary gland.
Lethargy and chronic fatigue, malnutrition and exhaustion of the body can cause this problem. Violations of this type occur in the girl's body during the first menstrual cycle, as well as after abortion, childbirth and during pregnancy. Prolonged bleeding caused by medical abortion is gaining popularity. The use of hormonal drugs and heredity are attributed to a number of causes. nine0003
Treatment should be selected individually, it is necessary to determine the cause that caused the disease.
Bleeding during pregnancy
Uterine bleeding during pregnancy most often indicates a miscarriage, an ectopic pregnancy, or damage to the placenta. These causes are accompanied by severe pain in the lower abdomen, nausea, vomiting, and malaise. The blood is bright red or dark scarlet in color, most often with clots.
It is possible to damage the cervix during pregnancy during a gynecological examination or sexual intercourse. This bleeding is usually not prolonged or heavy. In the second or third trimester, bleeding may begin due to damage or placenta previa. nine0003
Bleeding poses a serious threat to the health and life of the mother and child. It should be understood that uterine bleeding is very dangerous for pregnant women. The woman should immediately call an ambulance.
Bleeding due to caesarean section
The cause of this bleeding is hemostasis. To do this, a medical intervention is carried out, in which the walls of the uterus are thoroughly cleaned. A caesarean section leaves behind a scar on the uterus, which prevents it from contracting normally. A caesarean section takes a long time to heal and can cause uterine bleeding. A woman should be under medical supervision, and after healing, when the first signs appear, immediately seek help. nine0003
Hypotonic bleeding is very difficult to stop, because it occurs at the moment after the contraction of the uterus. Hypotensive shock may occur. In this case, doctors must immediately proceed to rescue, and have a supply of blood for recovery.
Hypotensive shock may occur. In this case, doctors must immediately proceed to rescue, and have a supply of blood for recovery.
The last degree of severity of uterine bleeding after cesarean is the removal of the uterus. It is used in cases where the salvation of the patient directly depends on stopping the bleeding, and other methods are powerless. nine0003
Gynecologists classify bleeding according to various criteria. The most common are:
Hypotonic. The fertilized egg lingers in the myometrium of the uterus. The reason is hypotension. The contraction of the muscle tissue of the uterus after childbirth occurs spontaneously. A critical state occurs when it is completely absent. The bleeding should be stopped immediately. Replenish the volume of circulating blood. Continuous measurement of blood pressure and pulse. Treatment is aimed at the speedy restoration of the motor function of the uterus. nine0003
Hypotonic occurrence after childbirth requires removal of the placenta. It is this action that helps to restore the healthy functioning of the walls of the uterus. Massage if needed. Apply ice or irritate the uterus with a swab dipped in ether. If hypotension does not stop, the therapy of atony is started.
It is this action that helps to restore the healthy functioning of the walls of the uterus. Massage if needed. Apply ice or irritate the uterus with a swab dipped in ether. If hypotension does not stop, the therapy of atony is started.
Atonic. Atonic appear when the uterus is not able to contract. In gynecology, non-contractility of the uterus is called the uterus of Kuveler. Zero tone of the uterus does not make it possible to stop bleeding with the help of special injections and drugs. To clamp the uterine artery, a thick suture is placed on the lip of the uterus, secured with additional clamps. The inefficiency of the method is considered as preparation for the removal of the uterus. Critical blood loss is considered from 1.2 liters. Electrical stimulation makes attempts to reduce blood vessels. Constantly infuse blood to avoid fainting. nine0003
Juvenile. Occur during puberty. The main cause is ovarian dysfunction. Infection, psychological trauma, excessive physical activity, colds, malnutrition can cause juvenile bleeding.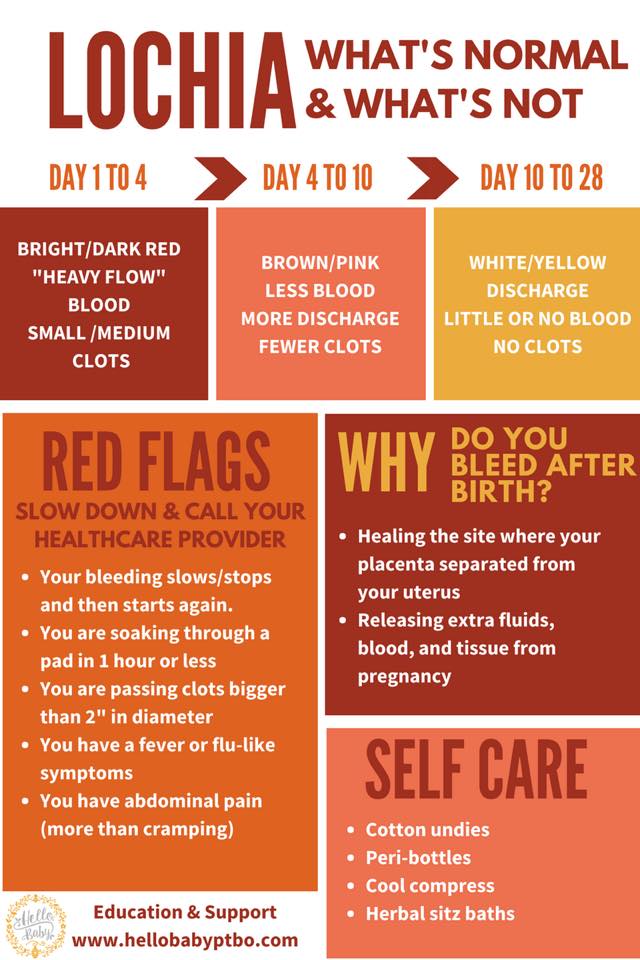 Climatic conditions are reflected. Treatment is carried out only in a hospital. Depending on the severity, this can lead to anemia. At the first detection, you should immediately call an ambulance, take a horizontal position, apply cold to the groin area and take a hemostatic drug. nine0003
Climatic conditions are reflected. Treatment is carried out only in a hospital. Depending on the severity, this can lead to anemia. At the first detection, you should immediately call an ambulance, take a horizontal position, apply cold to the groin area and take a hemostatic drug. nine0003
Dysfunctional. Occurs when the ovaries fail. The absence of menstruation for a long time and copious discharge are characteristic of this species.
Anuvulatory. Women undergo bleeding during menopause and adolescents. It is caused by a violation of the follicles and progesterone, during the absence of ovulation. It is also called single-phase, during bleeding, the corpus luteum does not form. A dangerous type of bleeding can cause the development of malignant tumors. Duration lasts more than 10 days. Bleeding is observed during a malfunction of the pituitary gland, after infections, poisoning and stress. nine0003
Profuse. Not accompanied by pain. The amount of fluid lost can vary. The reasons can be different, from a miscarriage to taking hormonal drugs.
The reasons can be different, from a miscarriage to taking hormonal drugs.
Clots in uterine bleeding
There are cases when a woman observes the presence of clots during bleeding. Doctors explain this with an anomaly that was transferred by the uterus in utero. The uterine cavity holds blood, forming clots. Such menstruation brings a lot of discomfort to a woman, especially during a hormonal crisis. This anomaly sometimes causes the appearance of a large number of clots. The anomaly can also be acquired. They are associated with lifestyle, profession and addiction to bad habits. nine0003
Menstruation with clots causes severe pain. To exclude an anomaly, you should apply for a gynecological consultation. To exclude the possibility of the appearance of clots on a hormonal background, take an analysis for hormones and check the thyroid gland. The presence of clots and pain indicate endometriosis. If the diagnosis is confirmed, then the disease requires urgent special treatment.
Stopping uterine bleeding
Upon arrival of the ambulance, the following actions are carried out: nine0003
-
apply cold to the abdomen;
-
with heavy bleeding, the woman is carried in a horizontal position;
-
urgent hospitalization;
-
specialist assistance;
-
the introduction of the desired solution, depending on the type of uterine bleeding.
nine0051
If the patient has not given birth, and she does not have tumors, treatment in the hospital is carried out with the help of hormonal drugs. Treatment begins with an increased dose, gradually increasing from 6 tablets per day to 1 piece. In the absence of anemia, gestogens are used. Prescribe hemostatic drugs, such as Vikasol, Dicinon, Ascorutin.
During puberty, girls are prescribed drugs that strengthen blood vessels and stop the blood. It is recommended to take vitamins. Phytotherapy and hormonal preparations for regulating the menstrual cycle.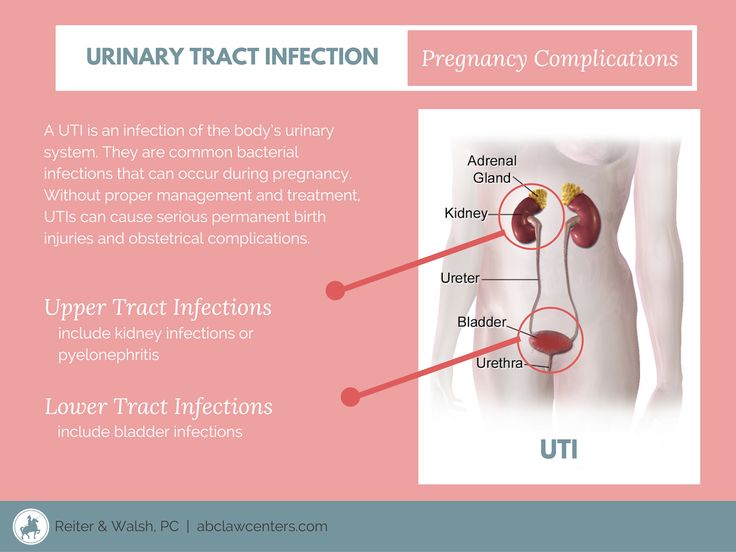 Women of childbearing age undergo surgery for endometriosis, fibroids. Pathology of the uterus and ovaries, oncological diseases, after menopause, requires only surgical intervention, removal of the appendages and uterus. nine0003
Women of childbearing age undergo surgery for endometriosis, fibroids. Pathology of the uterus and ovaries, oncological diseases, after menopause, requires only surgical intervention, removal of the appendages and uterus. nine0003
It is very important for proper treatment to undergo an examination in time and establish the cause that caused the bleeding. Women experiencing this pathology should immediately seek medical help.
First aid
An ambulance should be called immediately. During pregnancy, the woman's condition deteriorates sharply, because blood loss is plentiful. Every minute counts. If it is not possible to contact the medical team, you should take the woman to the hospital yourself. The reaction should be quick, with uterine bleeding a serious threat to life looms. In case of dysfunctional bleeding, do not apply any warm heating pads to the stomach, do not use drugs, douching, taking a bath. nine0003
Before the ambulance arrives, a woman can be helped independently by the following actions:
1. We put the woman to bed. In a horizontal position, it is desirable to raise the legs above the head. Place a pillow or roll up a blanket. With impressive bleeding, this will help the patient not to lose consciousness.
We put the woman to bed. In a horizontal position, it is desirable to raise the legs above the head. Place a pillow or roll up a blanket. With impressive bleeding, this will help the patient not to lose consciousness.
2. Apply cold to the stomach. If there is no heating pad or ice, replace it with any item from the refrigerator, after wrapping it in a cloth. A plastic cold water bottle will do. It is possible to achieve vasoconstriction and reduce bleeding with the help of cold for no more than 15 minutes. Take 5 minute breaks. nine0003
3. A woman is given plenty to drink. This will replace the drip at home. Make sweet tea or water.
4. When carrying a child, take medication seriously. If it is not possible to consult a doctor, it is necessary to read the insert and find out the minimum dose. Be sure to read the side effects. Upon the arrival of medical workers, tell the name of the drug that the woman took and its dosage.
Diagnosis
At the first sign of uterine bleeding, contact your gynecologist immediately.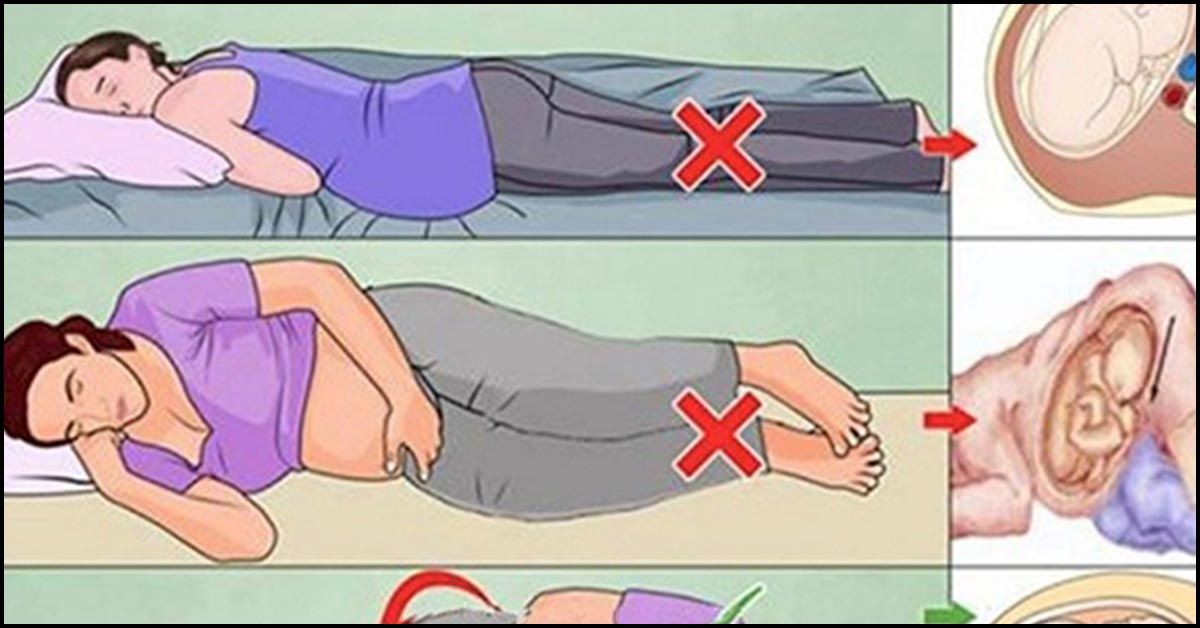 Women should keep a calendar where the nature, symptoms, well-being and duration of the menstrual cycle are noted. This will help the gynecologist prescribe the correct treatment and complete the course of therapy faster. Performing ultrasound diagnostics, taking smears of the cervix for the presence of cancer. Blood tests are performed to determine the level of hormones. A biopsy is done to examine the endometrium under a microscope. Proper diagnosis is the key to optimal rehabilitation. nine0003
Women should keep a calendar where the nature, symptoms, well-being and duration of the menstrual cycle are noted. This will help the gynecologist prescribe the correct treatment and complete the course of therapy faster. Performing ultrasound diagnostics, taking smears of the cervix for the presence of cancer. Blood tests are performed to determine the level of hormones. A biopsy is done to examine the endometrium under a microscope. Proper diagnosis is the key to optimal rehabilitation. nine0003
Bacteriuria, cystitis and pyelonephritis during pregnancy
The human urinary system consists of two kidneys that filter the blood plasma and remove part of the liquid and some substances dissolved in it into the urine, two ureters that conduct urine from the kidneys to the bladder, the bladder that serves as a reservoir for urine, and the urethra through which urine is excreted from the body.
During pregnancy, several changes occur in the urinary system that increase the risk of urinary tract infection. The acidity of urine changes, urine becomes more alkaline (its pH rises), and this creates a more favorable environment for the development of bacteria, slows down the passage of urine and creates conditions for reflux (reverse reflux) of urine, so that bacteria can be transported with urine from the underlying sections to the overlying ones. , to the renal pelvis. In addition, perfectly normal during pregnancy changes in the functioning of the immune system also reduce the body's ability to fight infection.
The acidity of urine changes, urine becomes more alkaline (its pH rises), and this creates a more favorable environment for the development of bacteria, slows down the passage of urine and creates conditions for reflux (reverse reflux) of urine, so that bacteria can be transported with urine from the underlying sections to the overlying ones. , to the renal pelvis. In addition, perfectly normal during pregnancy changes in the functioning of the immune system also reduce the body's ability to fight infection.
Thus, we see that pregnant women are more predisposed to developing urinary tract infections than their non-pregnant peers.
Asymptomatic bacteriuria
Asymptomatic bacteriuria is the presence of bacteria in the urine without signs of inflammation.
Normally, our urine is sterile, and bacteria, even if they pass from the rectum to the bladder through the urethra, are washed out with the urine stream the next time we urinate.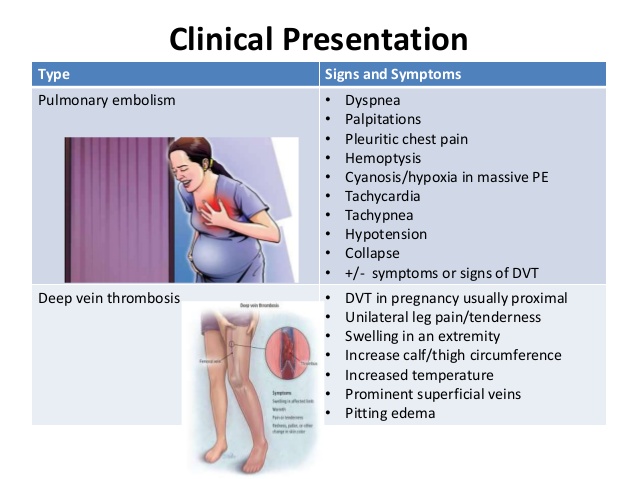 During pregnancy, very comfortable conditions are created for bacteria, and they can linger in the bladder, multiply, attach to the walls of the urinary tract, causing inflammation, and even throw into the renal pelvis. nine0003
During pregnancy, very comfortable conditions are created for bacteria, and they can linger in the bladder, multiply, attach to the walls of the urinary tract, causing inflammation, and even throw into the renal pelvis. nine0003
If bacteria and, in particular, nitrites, a product of the decomposition of urine urea by bacteria living in it, are detected in a general urine test during pregnancy, a urine culture is required to determine the pathogen, its amount (titer) and antibiotics to which it is sensitive.
Approximately thirty percent, that is, one in three pregnant women with asymptomatic bacteriuria without treatment, develop gestational (pregnancy-related) pyelonephritis during the same pregnancy. Therefore, asymptomatic bacteriuria during pregnancy always requires treatment. All urinary tract infections during pregnancy are treated antibacterial drugs.
Select drugs that are compatible with pregnancy and are safe enough for the fetus to be used at that time. The sensitivity of the pathogen to the antibiotic is also taken into account. Phytotherapeutic drugs for the treatment of urinary tract infections during pregnancy should not be used.
The sensitivity of the pathogen to the antibiotic is also taken into account. Phytotherapeutic drugs for the treatment of urinary tract infections during pregnancy should not be used.
Cystitis
Cystitis (inflammation of the bladder wall) during pregnancy usually manifests itself in a more erased form than outside it, less often there is very severe pain, less often cystitis is hemorrhagic - that is, blood in the urine is less often detected. Cystitis can also serve as the first step to the subsequent development of pyelonephritis, so cystitis during pregnancy also requires treatment with antibacterial drugs, herbal medicine in this case should not be used. nine0003
Gestational pyelonephritis
Gestational pyelonephritis, in which the inflammatory process is localized in the pelvis of the kidney or both kidneys, is a rather formidable disease that can lead to abortion, stillbirth and even threaten the life of the pregnant woman herself.