Ovulation and cramps
Symptoms, Causes & Pain Relief
Overview
What is ovulation pain?
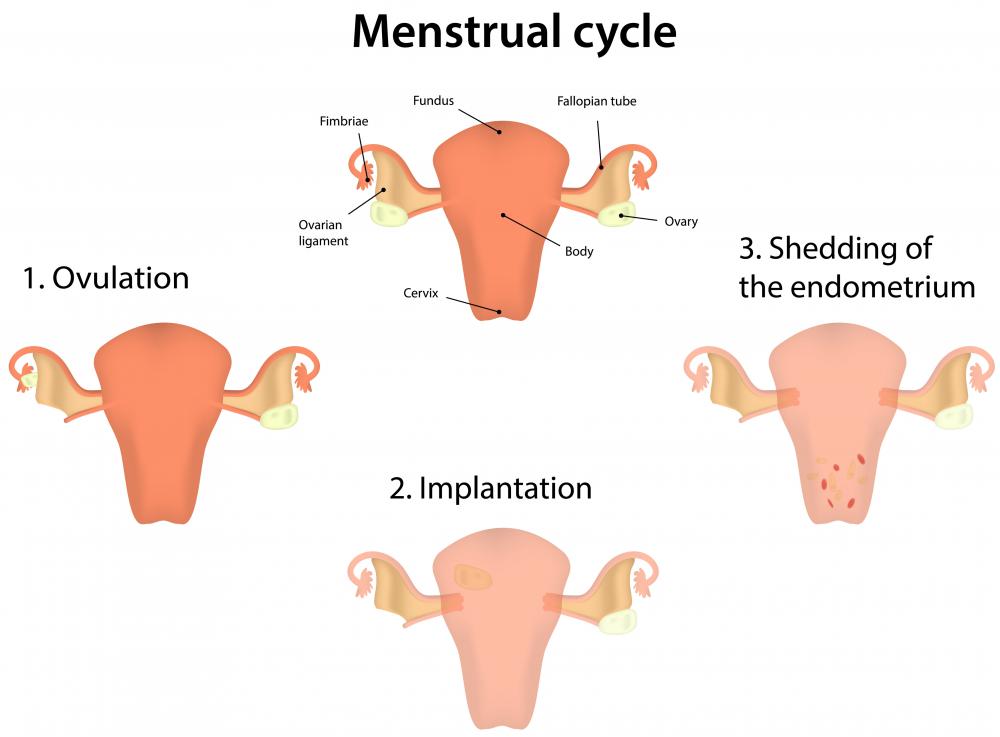
Ovulation pain is pelvic pain that some women have during ovulation. Ovulation is the part of the menstrual cycle when an ovary releases an egg. Ovulation usually happens about halfway between your periods.
Ovulation pain is also called “mittelschmerz.” The term comes from the German words for “middle” and “pain.”
Where does ovulation pain occur?
You typically feel the pain in your lower abdomen and pelvis, in the middle or on one side. You may feel it on the side where the ovary is releasing an egg. (For most people, the ovaries take turns ovulating. Each ovary releases an egg every other month.)
So if the ovary on the right side is releasing the egg, that’s where you’ll feel the pain. Some people find that the pain switches sides from one cycle to the next.
Who gets ovulation pain?
Many women never have pain at ovulation. Others have midcycle pain every month. They can often tell by the pain that they are ovulating.
Is ovulation pain the same as period pain?
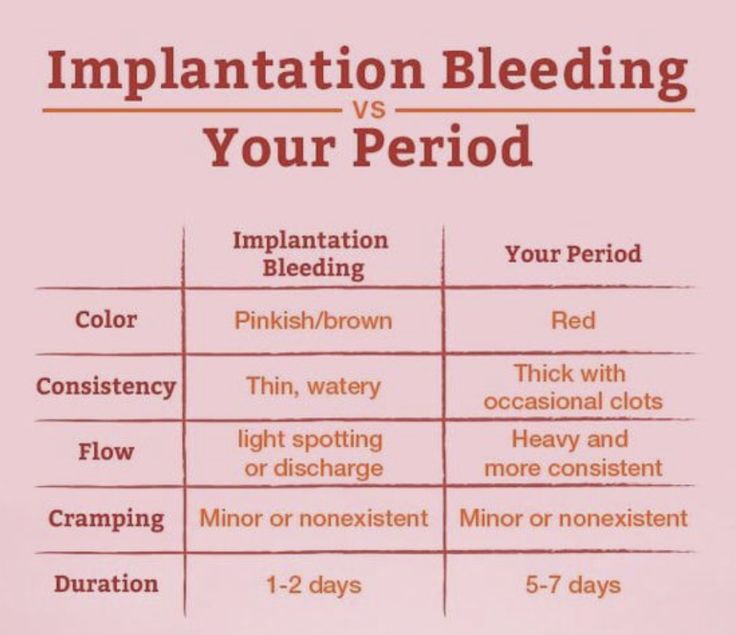
Ovulation pain may feel similar to period pain — like a cramp. But ovulation pain happens about two weeks before you get your period.
How common is ovulation pain?
Mittelschmerz may affect more than 40% of women who ovulate during their reproductive years — and it can affect them almost every month.
Symptoms and Causes
What causes ovulation pain?
The egg develops in the ovary. As it grows, follicular fluid surrounds it. During ovulation, the ovary releases the egg and fluid, along with some blood. Mittelschmerz may happen because of the egg enlarging in the ovary just before ovulation.
The pain may also be due to a ruptured follicle. The egg bursts from the follicle when it’s ready. The burst may cause some bleeding. The blood and fluid from the ruptured follicle may irritate the lining of the abdomen (peritoneum), causing pain.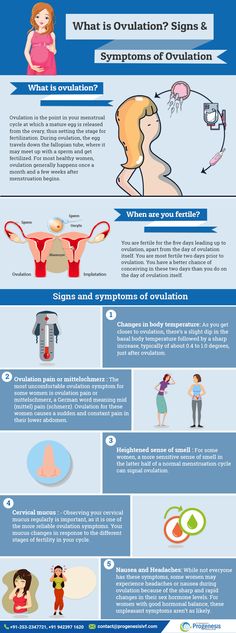
This is a normal part of the menstrual cycle.
What are the symptoms of ovulation pain?
The pain may feel like a mild twinge, or you might have severe discomfort. It often hurts on just one side. The pain can last from a few minutes to a few hours. You may also experience:
- Light vaginal bleeding.
- Vaginal discharge.
- Nausea, if the pain is bad.
Diagnosis and Tests
How is ovulation pain diagnosed?
Your healthcare provider might diagnose mittelschmerz based on the timing of the pain. Ovulation usually happens about two weeks into your menstrual cycle. So if the pain happens about midway between periods, it may be ovulation pain.
Your provider may ask you to keep a record of your menstrual cycles. Note whenever you have pain and where you feel the pain.
What tests will I need?
Your healthcare provider may perform an abdominal and pelvic examination. These tests can help rule out other causes of pain, such as endometriosis or an ovarian cyst.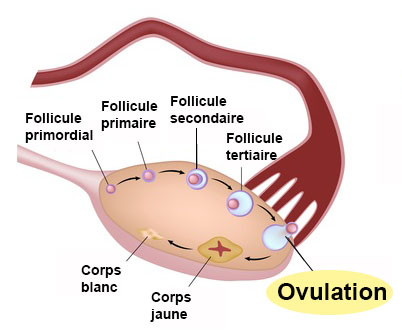 You may also need an abdominal or vaginal ultrasound.
You may also need an abdominal or vaginal ultrasound.
If your healthcare provider notices something suspicious during the exam or your pain is severe, you may need more tests to find the cause. Your healthcare provider will discuss the next steps with you.
Management and Treatment
How is ovulation pain treated?
Most people don’t need treatment for mittelschmerz. The pain typically goes away within a day. You can take medication available over the counter such as nonsteroidal anti-inflammatory medications, (ibuprofen, naproxen or Aleve) to help with the pain.
A heating pad or hot bath may also help provide pain relief.
For severe ovulation pain, talk to your healthcare provider about taking birth control pills. Hormonal birth control medications prevent ovulation. Without ovulating, you won’t have ovulation pain.
If you take birth control pills, you won’t be able to get pregnant. Talk to your healthcare provider if you wish to start or add to your family.
Prevention
Can I prevent ovulation pain?
You can prevent ovulation pain by preventing ovulation. Many hormonal contraceptives, including the pill, prevent ovulation.
Outlook / Prognosis
What is the outlook for women with ovulation pain?
Ovulation pain is normal. It’s one of the side effects of your period. It’s not dangerous or a sign of a serious health condition. Ovulation pain doesn’t affect fertility, and it can help you be more aware of when you ovulate.
It’s always a good idea to talk to your healthcare provider about any pain you’re having. A healthcare provider can rule out a more serious condition that has similar symptoms.
Should I worry about ovulation pain?
Ovulation pain itself is nothing to worry about. But talk to your healthcare provider if you have severe pain. It could be a sign of a different, more serious condition, including:
- Endometriosis, an inflammatory condition affecting the ovaries and fallopian tubes.

- Scar tissue from a cesarean section (C-section) or other abdominal surgery that caused abdominal adhesions.
- Sexually transmitted infections (STIs), such as chlamydia, which can cause inflammation that leads to painful ovulation.
- Ovarian cyst, a pouch of fluid that develops on an ovary.
- Ectopic pregnancy, when a pregnancy develops outside of the uterus, often on one of the fallopian tubes.
- Appendicitis, when the appendix is inflamed.
- Other abdominal problems, such as inflammatory bowel disease.
Can I use ovulation pain to plan a pregnancy?
Some people use ovulation pain to plan or avoid a pregnancy. Your chances of getting pregnant are higher if you have sex during the ovulation period. So, paying attention to any ovulation pain can help you know when you’re ovulating if you’re trying to get pregnant.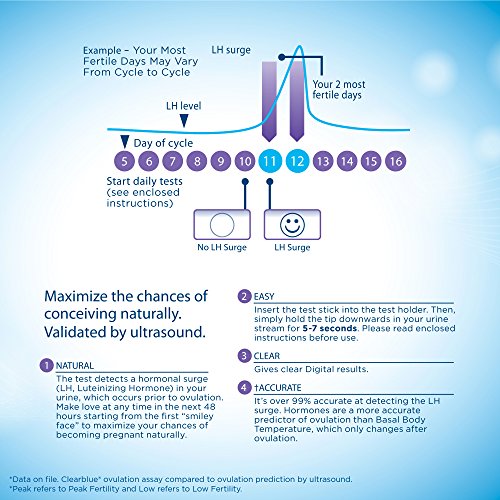
However, don’t rely on mittelschmerz as a way to avoid pregnancy. Use other, more reliable birth control methods.
Living With
How do I take care of myself?
If you have ovulation pain, try at-home treatments such as a warm bath and over-the-counter pain relief. For severe ovulation pain, talk to your healthcare provider about other treatment options.
When should I contact my healthcare provider?
Call your healthcare provider if you missed your last menstrual period or have these symptoms during ovulation:
- Fever greater than 100.4 degrees Fahrenheit.
- Pain while urinating.
- Red or burning skin where the pain is located.
- Severe nausea or vomiting.
- Severe pain in the middle of your menstrual cycle that lasts longer than a day or occurs during most months.
- Over-the-counter pain medication is not providing relief from the pain.
- Missed period.
- Heavy vaginal bleeding between periods.

What else should I ask my healthcare provider?
If you have midcycle pain, ask your healthcare provider:
- What’s causing the pain?
- What can I do to relieve the pain?
- Is there a way to prevent ovulation pain?
- Will birth control pills help control the pain?
A note from Cleveland Clinic
Ovulation pain, also called mittelschmerz, happens when people experience ovulation cramps or other pain when they ovulate. Ovulation pain is not harmful. Most of the time, you can treat it with OTC medications, rest and warm baths. But talk to your healthcare provider if you have severe ovulation pain. Your healthcare provider may recommend birth control pills to prevent ovulation.
Symptoms, Causes & Pain Relief
Overview
What is ovulation pain?
Ovulation pain is pelvic pain that some women have during ovulation. Ovulation is the part of the menstrual cycle when an ovary releases an egg. Ovulation usually happens about halfway between your periods.
Ovulation usually happens about halfway between your periods.
Ovulation pain is also called “mittelschmerz.” The term comes from the German words for “middle” and “pain.”
Where does ovulation pain occur?
You typically feel the pain in your lower abdomen and pelvis, in the middle or on one side. You may feel it on the side where the ovary is releasing an egg. (For most people, the ovaries take turns ovulating. Each ovary releases an egg every other month.)
So if the ovary on the right side is releasing the egg, that’s where you’ll feel the pain. Some people find that the pain switches sides from one cycle to the next.
Who gets ovulation pain?
Many women never have pain at ovulation. Others have midcycle pain every month. They can often tell by the pain that they are ovulating.
Is ovulation pain the same as period pain?
Ovulation pain may feel similar to period pain — like a cramp. But ovulation pain happens about two weeks before you get your period.
How common is ovulation pain?
Mittelschmerz may affect more than 40% of women who ovulate during their reproductive years — and it can affect them almost every month.
Symptoms and Causes
What causes ovulation pain?
The egg develops in the ovary. As it grows, follicular fluid surrounds it. During ovulation, the ovary releases the egg and fluid, along with some blood. Mittelschmerz may happen because of the egg enlarging in the ovary just before ovulation.
The pain may also be due to a ruptured follicle. The egg bursts from the follicle when it’s ready. The burst may cause some bleeding. The blood and fluid from the ruptured follicle may irritate the lining of the abdomen (peritoneum), causing pain.
This is a normal part of the menstrual cycle.
What are the symptoms of ovulation pain?
The pain may feel like a mild twinge, or you might have severe discomfort. It often hurts on just one side. The pain can last from a few minutes to a few hours.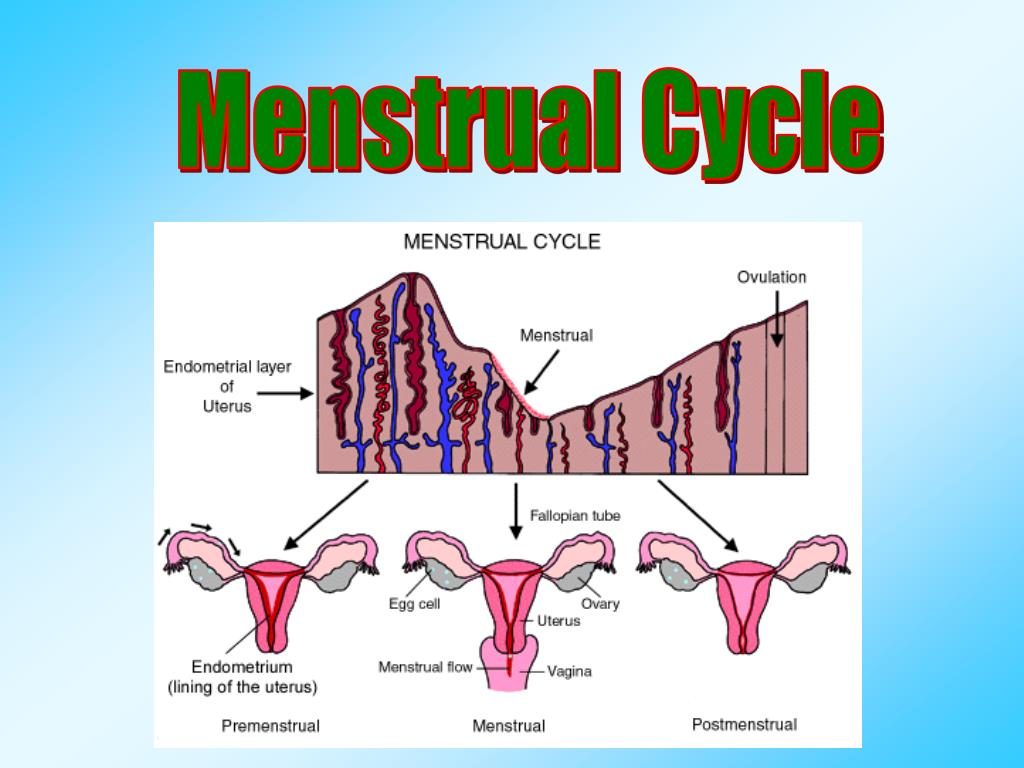 You may also experience:
You may also experience:
- Light vaginal bleeding.
- Vaginal discharge.
- Nausea, if the pain is bad.
Diagnosis and Tests
How is ovulation pain diagnosed?
Your healthcare provider might diagnose mittelschmerz based on the timing of the pain. Ovulation usually happens about two weeks into your menstrual cycle. So if the pain happens about midway between periods, it may be ovulation pain.
Your provider may ask you to keep a record of your menstrual cycles. Note whenever you have pain and where you feel the pain.
What tests will I need?
Your healthcare provider may perform an abdominal and pelvic examination. These tests can help rule out other causes of pain, such as endometriosis or an ovarian cyst. You may also need an abdominal or vaginal ultrasound.
If your healthcare provider notices something suspicious during the exam or your pain is severe, you may need more tests to find the cause. Your healthcare provider will discuss the next steps with you.
Management and Treatment
How is ovulation pain treated?
Most people don’t need treatment for mittelschmerz. The pain typically goes away within a day. You can take medication available over the counter such as nonsteroidal anti-inflammatory medications, (ibuprofen, naproxen or Aleve) to help with the pain.
A heating pad or hot bath may also help provide pain relief.
For severe ovulation pain, talk to your healthcare provider about taking birth control pills. Hormonal birth control medications prevent ovulation. Without ovulating, you won’t have ovulation pain.
If you take birth control pills, you won’t be able to get pregnant. Talk to your healthcare provider if you wish to start or add to your family.
Prevention
Can I prevent ovulation pain?
You can prevent ovulation pain by preventing ovulation. Many hormonal contraceptives, including the pill, prevent ovulation.
Outlook / Prognosis
What is the outlook for women with ovulation pain?
Ovulation pain is normal.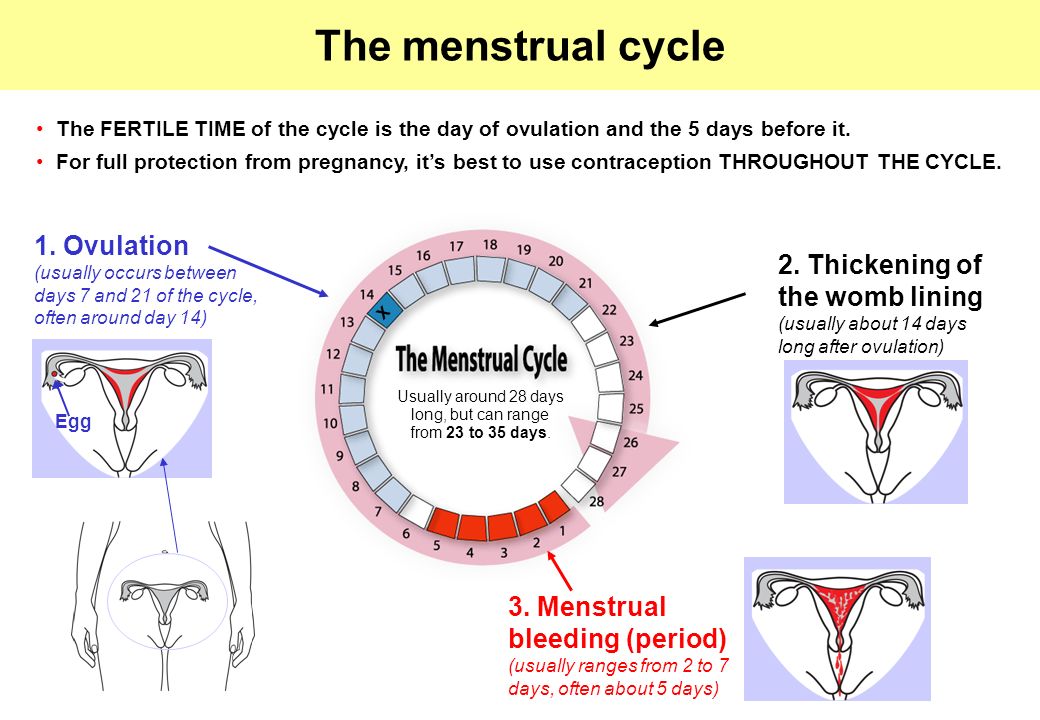 It’s one of the side effects of your period. It’s not dangerous or a sign of a serious health condition. Ovulation pain doesn’t affect fertility, and it can help you be more aware of when you ovulate.
It’s one of the side effects of your period. It’s not dangerous or a sign of a serious health condition. Ovulation pain doesn’t affect fertility, and it can help you be more aware of when you ovulate.
It’s always a good idea to talk to your healthcare provider about any pain you’re having. A healthcare provider can rule out a more serious condition that has similar symptoms.
Should I worry about ovulation pain?
Ovulation pain itself is nothing to worry about. But talk to your healthcare provider if you have severe pain. It could be a sign of a different, more serious condition, including:
- Endometriosis, an inflammatory condition affecting the ovaries and fallopian tubes.
- Scar tissue from a cesarean section (C-section) or other abdominal surgery that caused abdominal adhesions.
- Sexually transmitted infections (STIs), such as chlamydia, which can cause inflammation that leads to painful ovulation.

- Ovarian cyst, a pouch of fluid that develops on an ovary.
- Ectopic pregnancy, when a pregnancy develops outside of the uterus, often on one of the fallopian tubes.
- Appendicitis, when the appendix is inflamed.
- Other abdominal problems, such as inflammatory bowel disease.
Can I use ovulation pain to plan a pregnancy?
Some people use ovulation pain to plan or avoid a pregnancy. Your chances of getting pregnant are higher if you have sex during the ovulation period. So, paying attention to any ovulation pain can help you know when you’re ovulating if you’re trying to get pregnant.
However, don’t rely on mittelschmerz as a way to avoid pregnancy. Use other, more reliable birth control methods.
Living With
How do I take care of myself?
If you have ovulation pain, try at-home treatments such as a warm bath and over-the-counter pain relief. For severe ovulation pain, talk to your healthcare provider about other treatment options.
For severe ovulation pain, talk to your healthcare provider about other treatment options.
When should I contact my healthcare provider?
Call your healthcare provider if you missed your last menstrual period or have these symptoms during ovulation:
- Fever greater than 100.4 degrees Fahrenheit.
- Pain while urinating.
- Red or burning skin where the pain is located.
- Severe nausea or vomiting.
- Severe pain in the middle of your menstrual cycle that lasts longer than a day or occurs during most months.
- Over-the-counter pain medication is not providing relief from the pain.
- Missed period.
- Heavy vaginal bleeding between periods.
What else should I ask my healthcare provider?
If you have midcycle pain, ask your healthcare provider:
- What’s causing the pain?
- What can I do to relieve the pain?
- Is there a way to prevent ovulation pain?
- Will birth control pills help control the pain?
A note from Cleveland Clinic
Ovulation pain, also called mittelschmerz, happens when people experience ovulation cramps or other pain when they ovulate.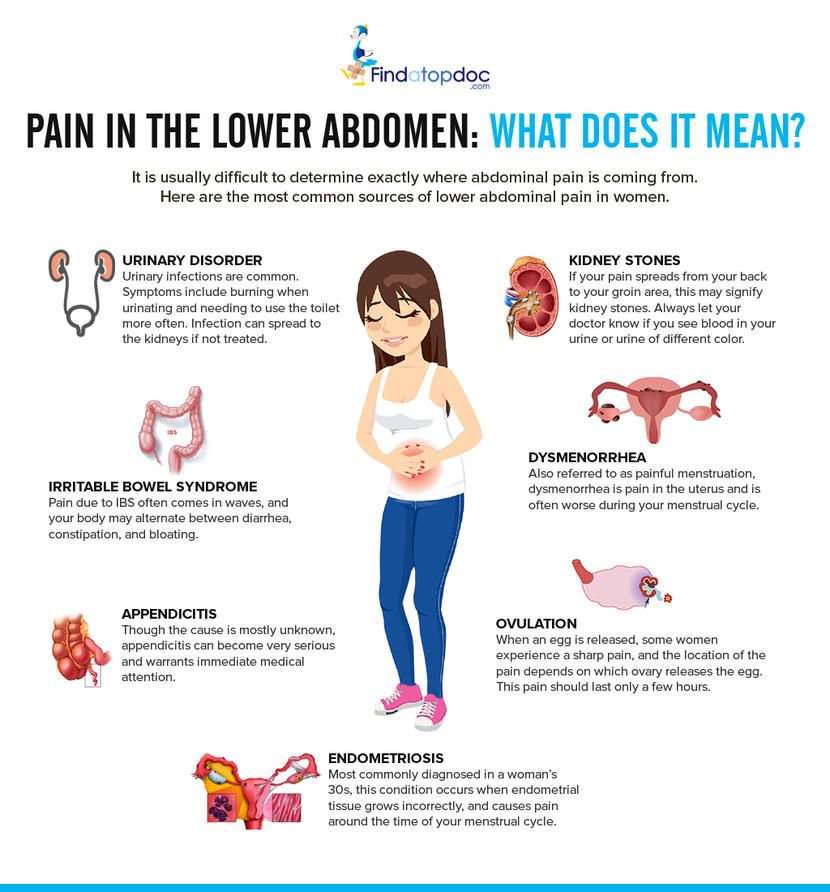 Ovulation pain is not harmful. Most of the time, you can treat it with OTC medications, rest and warm baths. But talk to your healthcare provider if you have severe ovulation pain. Your healthcare provider may recommend birth control pills to prevent ovulation.
Ovulation pain is not harmful. Most of the time, you can treat it with OTC medications, rest and warm baths. But talk to your healthcare provider if you have severe ovulation pain. Your healthcare provider may recommend birth control pills to prevent ovulation.
signs, causes, fertility tips and more
od Nov
We include products that we find useful for our readers. If you buy from links on this page, we may earn a small commission. Here is our process.
content
You may feel slight cramping or pain during ovulation. This pain is medically known as mittelschmerz. Mittelschmerz is a German word meaning "medium pain". nine0005
Not every woman will experience cramping during ovulation. Even if you regularly experience ovulation cramps, you won't necessarily experience them every month.
Pain during ovulation can last from a few minutes to several hours, but usually does not last longer than a day or two. It usually appears just before ovulation and is usually a mild, dull, aching pain on one side of the lower abdomen. For some women, the pain can be sharp and intense. nine0005
It usually appears just before ovulation and is usually a mild, dull, aching pain on one side of the lower abdomen. For some women, the pain can be sharp and intense. nine0005
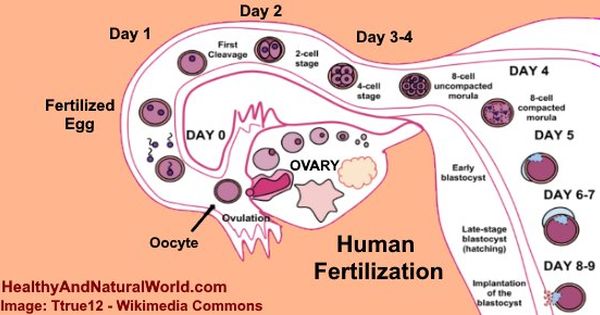
Ovulation occurs when a mature egg is released from the ovarian follicle. This usually happens around the middle of a woman's menstrual cycle. If you have a 28 day cycle, you will ovulate around day 14. The first day is the first day of bleeding.
The exact cause of ovulation pain is not fully known, but it can be caused by many factors, including:
- The rapid growth and expansion of the ovarian follicle in which the egg matures. This sprain can cause crampy pain. nine0022
- Irritation of the mucous membrane of the abdomen and pelvis with blood, fluid and other chemicals that usually accompany ovulation.
Other causes of cramps in the middle shoe
Pain in the middle of the cycle may be caused by an underlying disease. Most of these conditions are influenced by the female hormone estrogen, which is the peak of ovulation.
Other conditions that can cause mid-cycle pain include:
- Endometriosis. This condition can also cause painful periods and infertility. nine0022
- Maternal fibroids. Other symptoms of fibroids may include heavy menstrual bleeding, painful periods, and pelvic pressure.
- Ovarian cysts. Most ovarian cysts are painless, but if the cyst becomes very large, it may rupture or cause the ovary to tighten around the supporting tissues. This is called ovarian torsion and can lead to severe pain on one side.
While mittelschmerz may be a good indicator that ovulation is imminent, it is not the only sign that ovulation is imminent. nine0005
An increase in resting basal body temperature
A slight increase in resting basal body temperature may be a sign of ovulation. This is your first temperature in the morning before you get out of bed.
To schedule this little change:
- Take your temperature when you wake up before getting out of bed with a basal thermometer.
 They are available at most pharmacies or online.
They are available at most pharmacies or online. - Record your temperature every day for your entire menstrual cycle. nine0022
- Look for magnification.
Most women will see an increase from 0.4 to 0.8 at around ovulation. Temperature changes can be sudden or gradually peak during the day. You will likely ovulate within three days of this temperature change.
Changes in cervical mucus
The cervix produces mucus in response to changes in hormone levels in the body. Your cervix is the opening to your uterus.
Changes in uterine mucus during the menstrual cycle:
- After your period stops, you may not notice any mucus at all.
- After a few days, you may see cloudy, yellowish, sticky discharge on your underwear or toilet paper.
- Mucus becomes clearer, thinner and wetter as ovulation approaches. It can be stretched between two fingers. The purpose of this mucus is to help transfer the sperm to the fertilized egg.
These mucus changes may not be noticeable, so if you are using this method to detect ovulation, you will need to check and monitor your cervical mucus daily. nine0005
Other ways to recognize ovulation
You can also buy an ovulation prediction kit (OPK) to help you determine when you are ovulating. These tests measure the level of luteinizing hormone (LH) in the urine. Just before ovulation, you will have what is known as an increase in LH.
To use OPK, you will need to test your urine daily when you expect ovulation. Some tests come with a digital screen that is easy to read, although they are more expensive. nine0005
Other, more affordable kits work in a similar way to pregnancy. By dipping the strip in your urine, you will compare the control line with your LH measurement line. When the line of the left hand is the same as the line of the left hand or darker than it, this is a sign of an increase in your left hand.
If you are trying to conceive, knowing when you ovulate is the key to maximizing your chances of conceiving.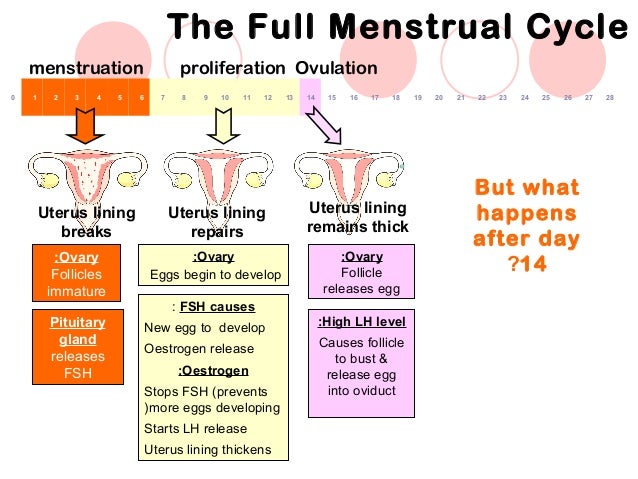 Other ways to increase your chances of conceiving include:
Other ways to increase your chances of conceiving include:
- Have sex regularly. Strive every second day to increase your chances.
- Know your fruitful window. Sperms can live in a woman's genital tract for about three to five days, while an egg can only survive up to 24 hours after hatching. having sex two days before ovulation can increase your chances of getting pregnant.
- Invest in OPK, especially if you don't have a regular menstrual cycle. An irregular cycle can make it difficult to predict ovulation. nine0022
- Forget the rumors. Use one sexual position instead of another and keep your legs elevated after intercourse. do not increase your chances of conceiving. Sperms reach the female reproductive tract in minutes, whether you are on your back or in an upright position.
- Be and stay healthy. One of the main predictors of fertility is good general health.
- Quit smoking. Cigarette smoke can damage egg quality. If you have problems with withdrawal, contact your doctor.
 It may also help you get a friend or family member involved to help you overcome the habit. nine0022
It may also help you get a friend or family member involved to help you overcome the habit. nine0022 - Get a healthy weight. Being overweight and being overweight can cause hormonal problems that affect ovulation.
- Consult an obstetrician/gynecologist. This can help detect any previously undiagnosed sexually transmitted infections or reproductive problems such as endometriosis that may affect fertility. Your doctor can also give you medically healthy ways to increase your chances of conceiving.
Cramping pain in the middle of the cycle may be a sign of ovulation. This pain should not last more than two days and will probably not require any treatment. nine0005
Talk to your doctor if your pain is severe or accompanied by heavy bleeding, fever or nausea.
You should also talk to your doctor if you have not been able to get pregnant after one year of trying if you are under 35, or after six months of trying if you are 35 or older. Your doctor may refer you to a fertility specialist.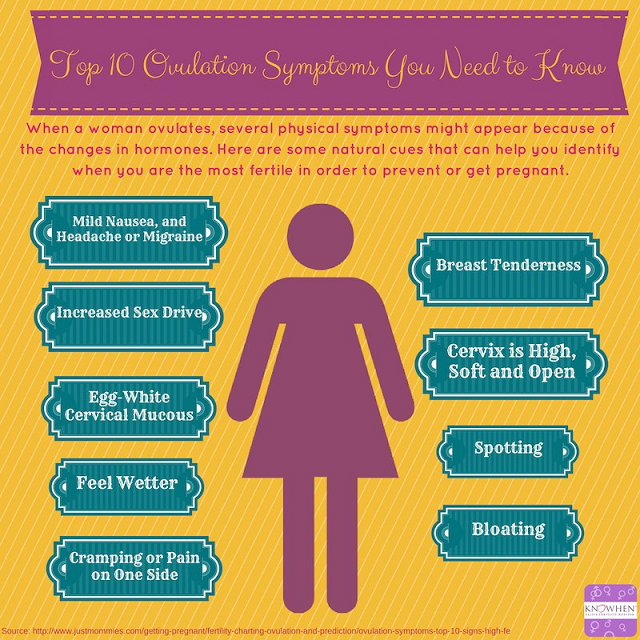
Convulsions after sex: IUD, pregnancy, menstruation and ovulation
content
Review
Most people talk about the pleasure of sex. Less commonly talked about is the pain associated with sex, which can take away a lot of your pleasure.
Cramping is just one type of pain you may experience after sex. But if you are experiencing this, you are not alone. What causes this cramp and what can be done about it? Read on to find out.
Does the IUD play a role in post-sexual seizures?
An intrauterine device (IUD) is a type of birth control. This is a small piece of T-shaped plastic that is inserted into the uterus. IUDs prevent unwanted pregnancy by preventing sperm from reaching the egg. Some also contain hormones. nine0005
A woman may have seizures for several weeks after inserting an IUD, whether she has had sex or not. Once she starts having sex, these cramps can become more intense. But that doesn't always have to be alarming.
Sex cannot replace an IUD, so don't worry if you experience convulsions within a few weeks of inserting an IUD.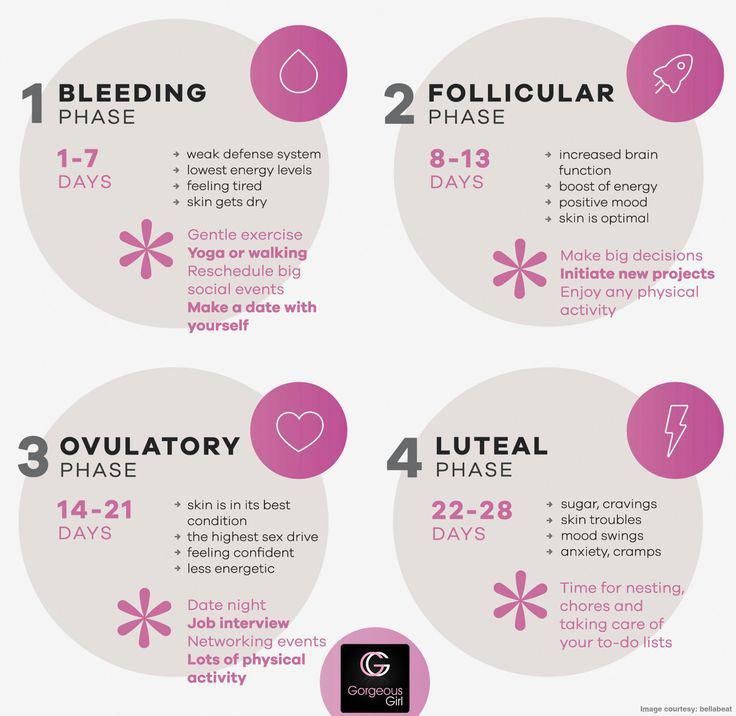 If more than a few weeks have passed since insertion and cramps are still felt, you may want to talk to your doctor about what might be causing the pain. nine0005
If more than a few weeks have passed since insertion and cramps are still felt, you may want to talk to your doctor about what might be causing the pain. nine0005
Does pregnancy play a role in post-sexual convulsions?
If you are not having a high-risk pregnancy, it is safe and healthy to have sex until your water breaks. You cannot harm your unborn child by having sex while he is in your body. However, your doctor may advise you not to have sex if you experience:
- bleeding
- abdominal pain or cramps
- broken water
- history of cervical weakness
- genital herpes
- low placenta
Pregnant women often experience cramps after sex. This is because orgasms can cause uterine contractions, leading to cramps. This is especially common when a woman is in her third trimester of pregnancy. Relaxing for a few minutes can relieve cramps.
Does menstruation or ovulation play a role in post-sexual cramps?
Many women experience menstrual pain (dysmenorrhea). This pain usually occurs in the form of abdominal cramps. It usually starts after one to two days of menstruation and can last from 12 to 72 hours. nine0005
This pain usually occurs in the form of abdominal cramps. It usually starts after one to two days of menstruation and can last from 12 to 72 hours. nine0005
Cramping can also occur during ovulation, when a woman's egg is released from the fallopian tube into the uterus. Pain during the menstrual cycle is caused by contractions of the woman's uterus.
During sex, menstrual cramps can be relieved to some extent. However, the pressure exerted by sex on the cervix can cause pain later on. Women who are ovulating and menstruating are more likely to experience cramps after sex. Orgasms can also cause contractions that cause abdominal cramps. nine0005
How to treat cramps after sex?
Seizures after sex can have many causes. Fortunately, the causes are usually not the main cause for concern. But that doesn't make cramps after sex any less painful or uncomfortable.
Taking painkillers
Painkillers are an effective way to treat post-sexual cramps. Over-the-counter pain relievers can reduce cramps by relaxing the abdominal muscles.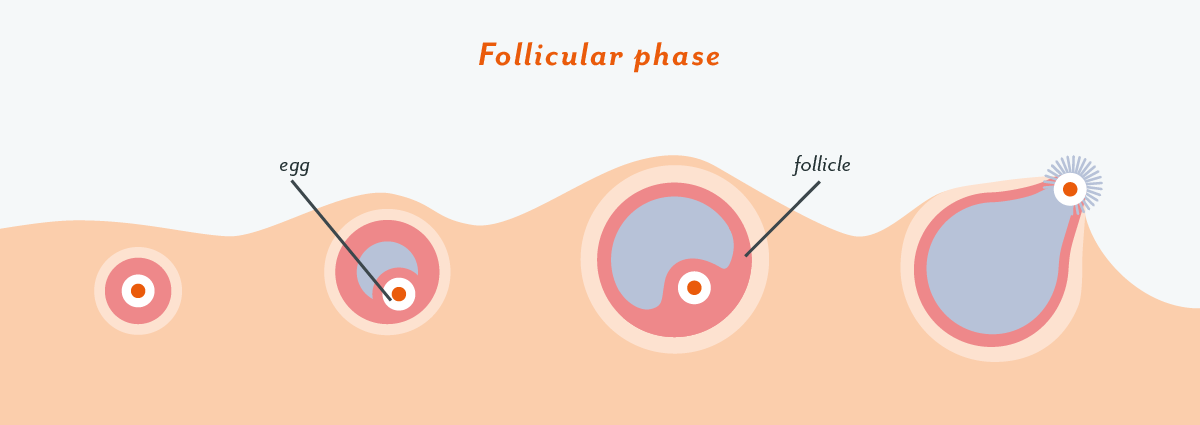 This includes:
This includes:
- ibuprofen (Advil or Motrin IB)
- naproxen sodium (Aleve)
- acetaminophen (Tylenol)
Applying heat
Applying heat to the abdomen can also help reduce abdominal cramps. You can do this with:
- hot bath
- heating pad
- hot water bottle
- thermal cloth
Heat works by increasing blood flow or circulation in a narrowed area, relieving pain.
Add additives
Try adding nutritional supplements such as:
- vitamin E
- omega-3 fatty acids
- vitamin B-1 (thiamine)
- vitamin B-6
- magnesium
Practice relaxation techniques
Sex is enjoyable, but orgasms can cause tension in the body. If you experience cramps after sex, relaxation techniques can sometimes help relieve the pain. Stretching, yoga, deep breathing and meditation can be effective.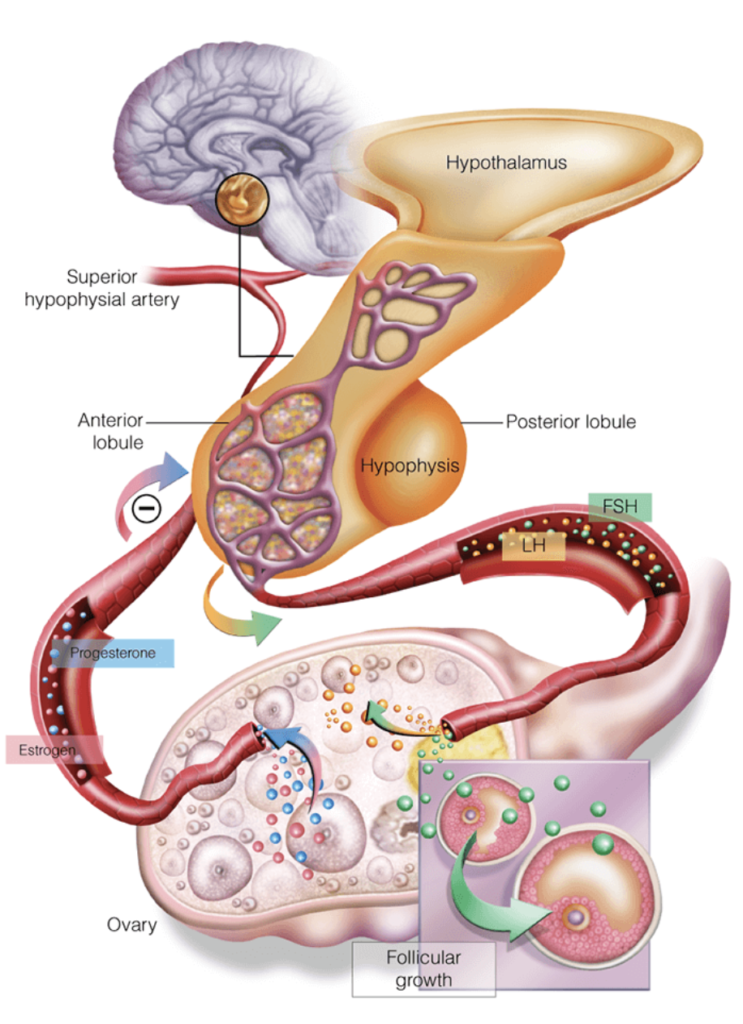 nine0005
nine0005
Adjust your lifestyle
If you experience cramps after sex, drink and smoke, you may need to rethink your habits. Drinking alcohol and smoking tobacco can often make seizures worse.
When should I see a doctor?
During pregnancy
Frequent sex during pregnancy can sometimes lead to urinary tract infections (UTIs), especially if you are prone to them. UTIs can cause complications during pregnancy if you don't seek treatment. You can have a UTI if you have experience:
- complaints
- constant urge to urinate
- burning when urinating
- cloudy urine
- reddish urine
- urine with a strong odor
Sexually transmitted infections
Some STIs can cause abdominal cramps, including:
- Chlamydia
- pelvic inflammatory disease (PID)
- hepatitis
You may notice that this cramp gets worse after sex.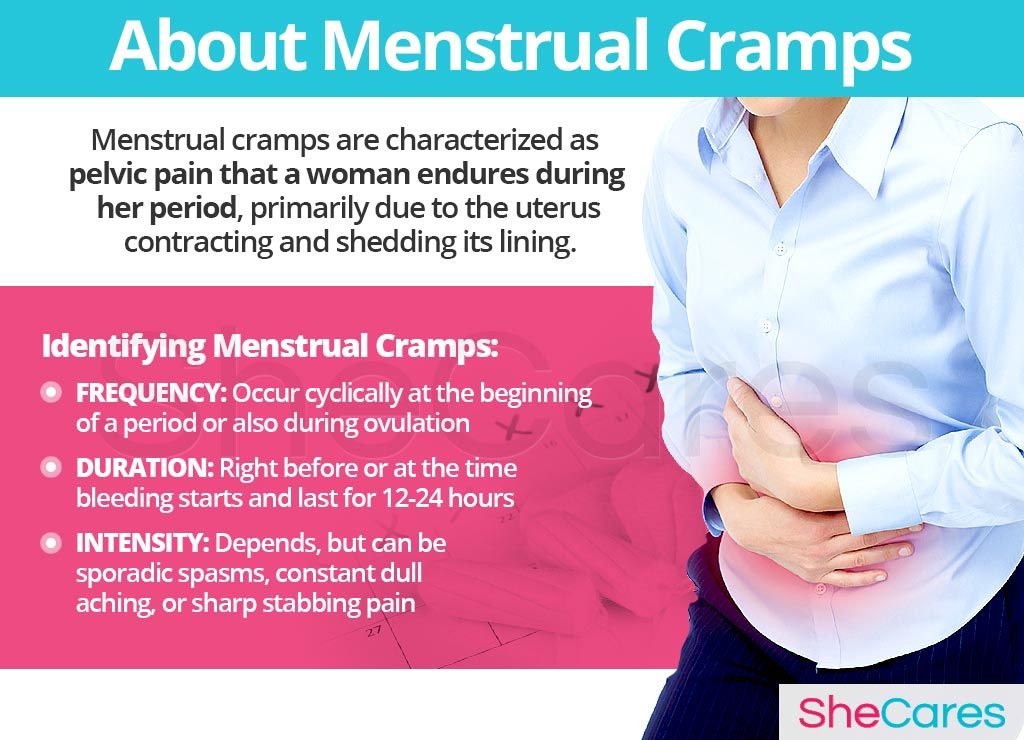 STIs often come with other symptoms, and being familiar with these symptoms can help you determine if you have an STI or not.
STIs often come with other symptoms, and being familiar with these symptoms can help you determine if you have an STI or not.
During menstruation
Usually cramps after sex during menstruation are not a cause for concern. But in some cases, menstrual cramps can be a sign of a medical problem. If menstrual pain starts earlier in your cycle and lasts longer, cramps may be due to a reproductive disorder, such as:
- endometriosis
- adenomyosis
- uterine fibroids
Call your doctor if you experience severe or prolonged menstrual cramps or cramps after sex. They will examine you for various medical problems that may be causing them.
Essence
Cramping after sex is not usually a cause for concern. And often that pain can be alleviated with a little care, whether it's over-the-counter medications or relaxation techniques. nine0005
However, if cramps after sex completely disrupt your personal or even daily life, you should contact your doctor immediately.