Odds of spina bifida
Spina bifida | March of Dimes
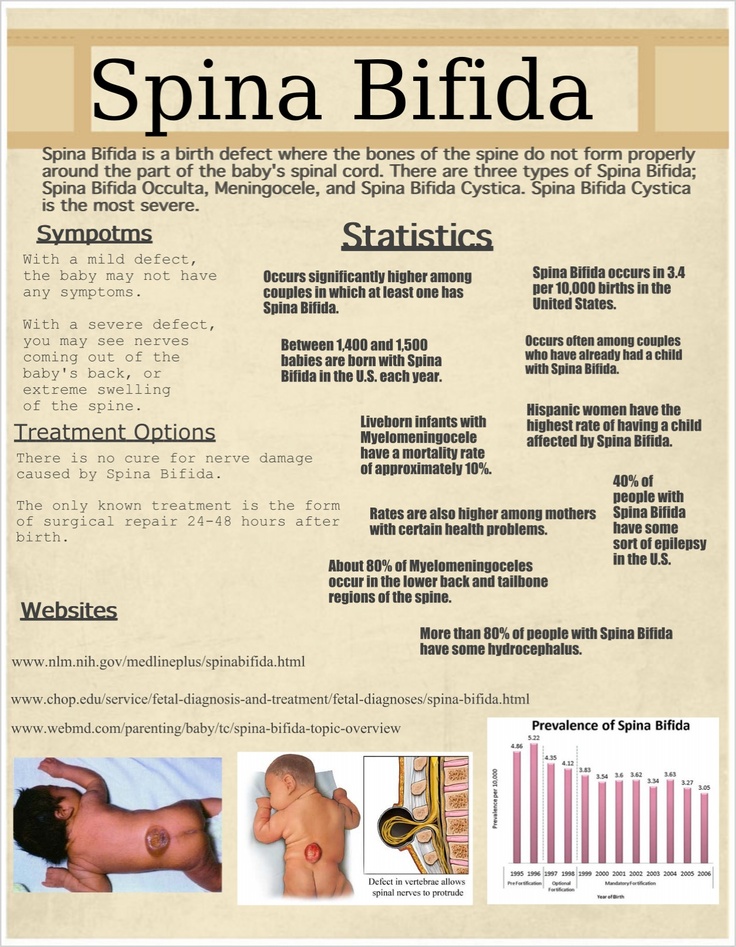
Spina bifida is the most common kind of neural tube defect. These are conditions of the brain, spine and spinal cord.
Taking folic acid every day before and in the first few weeks of pregnancy can help reduce your risk for spina bifida and other neural tube defects.
If you’ve had a baby who had a neural tube defect, your risk for having another baby who has a neural tube defect is higher.
Spina bifida can be diagnosed during pregnancy or after birth.
Spina bifida can cause health problems for your baby, such as fluid on the brain, paralysis (not being able to move parts of the body) and learning and developmental disabilities.
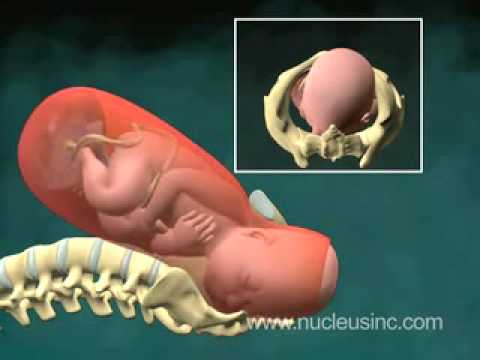
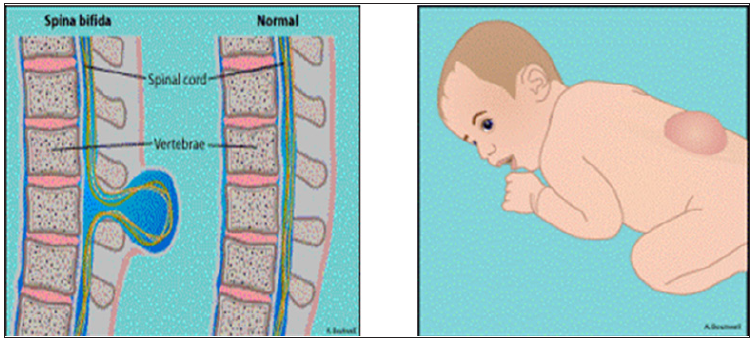
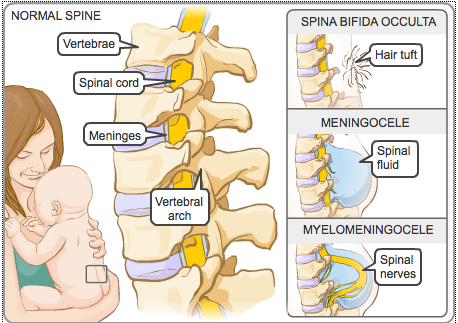
What is spina bifida?Spina bifida means “split spine” or “open spine.” The spine (backbone) protects the spinal cord, the bundle of nerves that runs down the middle of your back. The spinal cord carries signals back and forth between your body and your brain. Spina bifida happens when the spinal cord or bones in the spine don’t form correctly, leaving a gap or opening. Spina bifida can happen anywhere along the spine.
Spina bifida is the most common kind of neural tube defect. These are conditions of the brain, spine and spinal cord. Birth defects are structural changes present at birth that can affect almost any part of the body. Spina bifida can affect how your baby’s brain, spine, spinal cord and meninges develop. Meninges are the tissues that cover and protect the brain and the spinal cord.
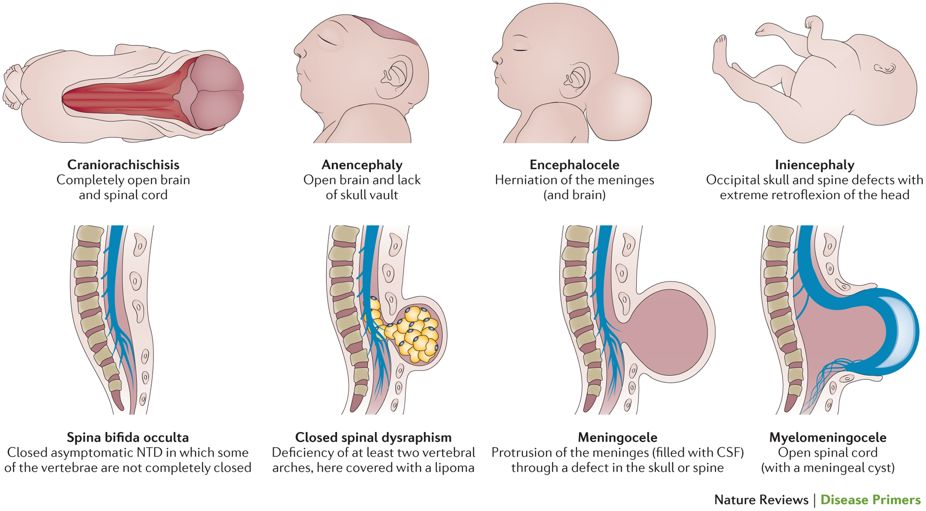
The neural tube starts out as a tiny, flat ribbon that grows into a tube. The neural tube usually closes in the first few weeks of pregnancy. In a baby who has a neural tube defect, the tube hasn’t closed completely.
About 1,400 babies are born with spina bifida in the United States each year. In this country, people who are Hispanic are more likely to have a baby who is affected by spina bifida than White or Black people.
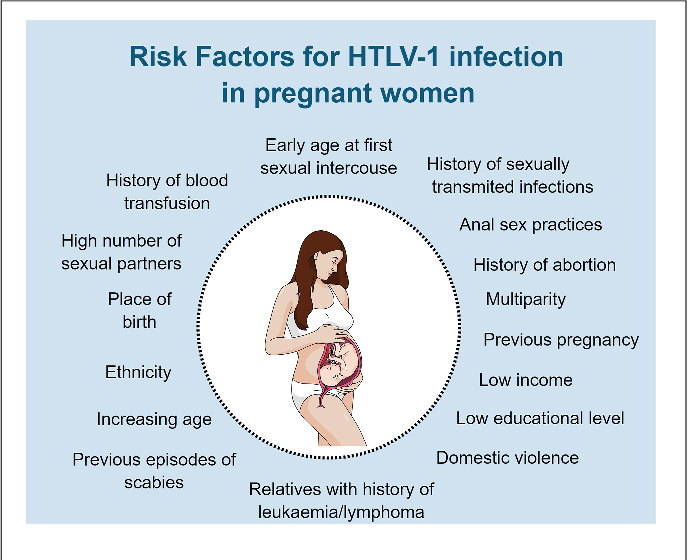
Are you at risk for having a baby with spina bifida?We don’t always know for sure what causes spina bifida, but certain things may play a role. We do know that some things may make you more likely than others to have a baby who is affected by spina bifida. These are called risk factors. Having a risk factor doesn’t mean for sure that your baby will be affected, but it may increase your chances.
We do know that some things may make you more likely than others to have a baby who is affected by spina bifida. These are called risk factors. Having a risk factor doesn’t mean for sure that your baby will be affected, but it may increase your chances.
Talk to your provider about things you can do to help reduce your risk for spina bifida:
Take folic acid. Folic acid is a B vitamin that every cell in your body needs for normal growth and development. Taking folic acid before and during early pregnancy can help prevent neural tube defects in your baby.
Learn about your genes. Genes are the part of your body’s cells that store instructions for the way your body grows and works. Genes are passed from parents to children. Sometimes changes in genes can cause spina bifida and other conditions.
- If you already have a child who is affected by a neural tube defect, you have a slightly higher risk of having another baby with the same condition.
- If you are affected by a neural tube defect yourself, you’re more likely to have a baby who has spina bifida than a person who doesn’t have a neural tube defect.
If you, your partner, your children or someone in your families has a neural tube defect, you may want to see a genetic counselor. This is a person who is trained to help you understand about genes, birth defects and other medical conditions that run in families and how they can affect your health and your baby’s health. Most often, spina bifida occurs in people who don’t have any family history of the condition.
Manage your health. Certain health conditions, such as diabetes and obesity, may play a role in spina bifida. If you have these or other health conditions:
- Talk to your provider about how your condition affects your risk for spina bifida and other neural tube defects.
- Get your health under control before you get pregnant. And get regular treatment to manage your condition during pregnancy.
- Get to a healthy weight before pregnancy. Eat healthy foods and do something active every day.
Talk with your provider about medicines you take. This includes any prescription and over-the-counter medicines, supplements and herbal products. You may need to stop taking a medicine or switch to one that’s safer during pregnancy. For example, some anti-seizure medicines may increase your risk of having a baby who is affected by a neural tube defect. Here’s how to reduce your risk:
- Tell your provider about any medicine or supplement you take before you get pregnant.
- Don’t start or stop taking any medicine before or in the first few weeks of pregnancy without talking to your health care provider first.
- Make sure any provider who prescribes you medicine knows you’re pregnant or trying to get pregnant.
Having a high body temperature (also called hyperthermia) in the first 6 weeks of pregnancy. This may be caused by fever or by spending time in a hot tub or sauna.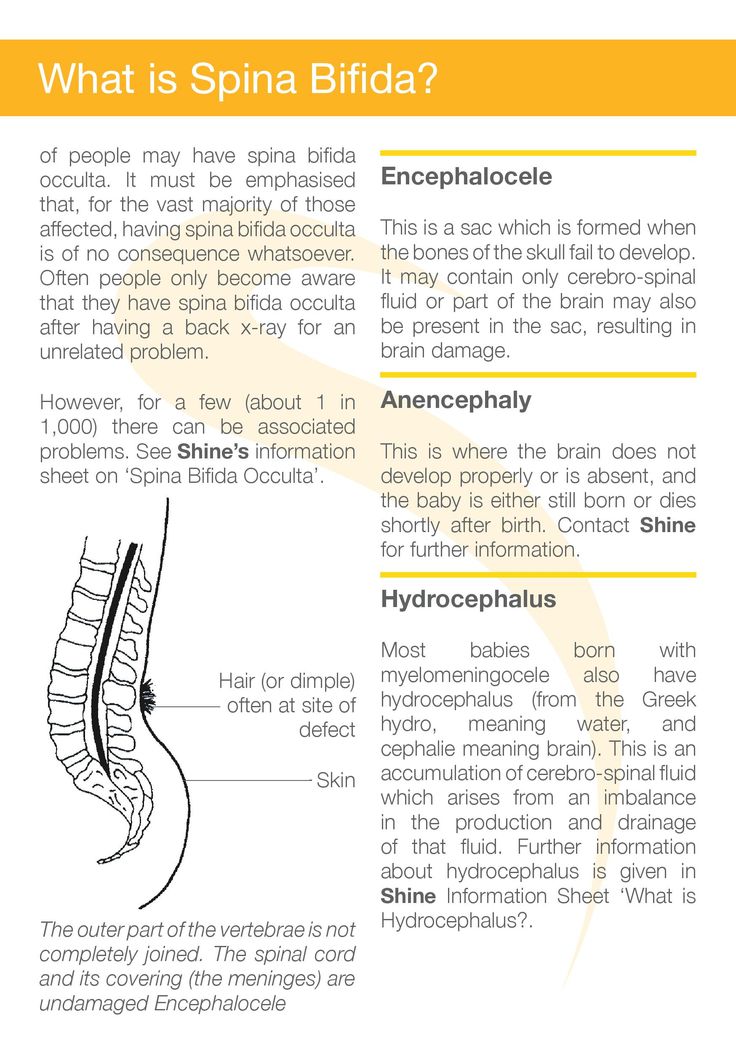 Having a high body temperature may increase your chances of having a baby who has spina bifida. Here’s what you can do to help reduce your risk:
Having a high body temperature may increase your chances of having a baby who has spina bifida. Here’s what you can do to help reduce your risk:
- If you have a fever in the first 6 weeks of pregnancy, call your provider right away.
- Don’t use hot tubs or saunas when you’re pregnant or if you’re trying to get pregnant.
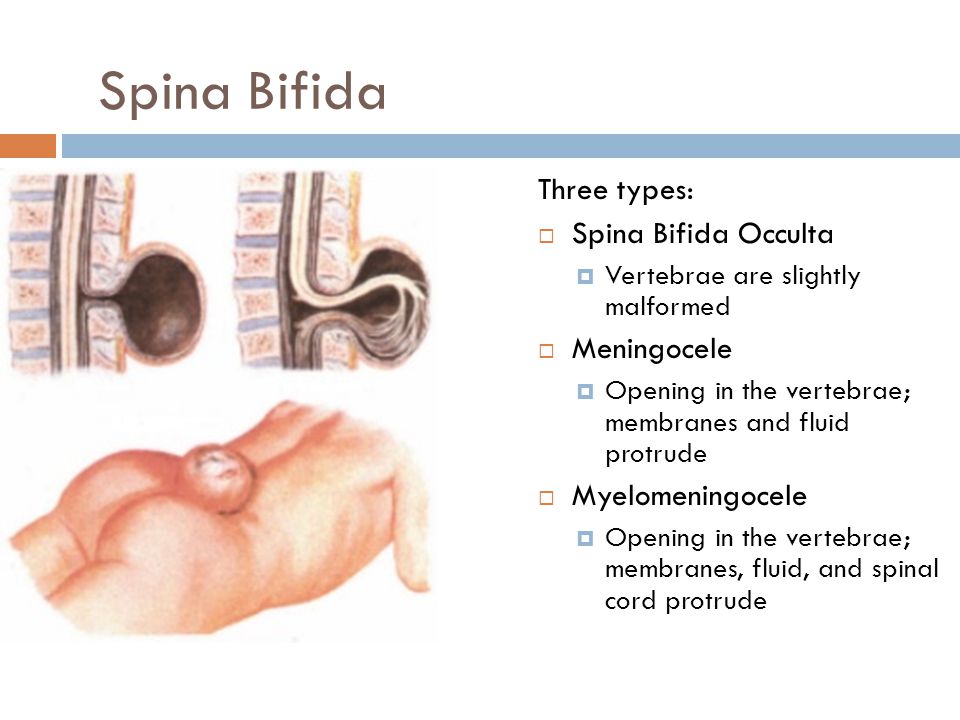
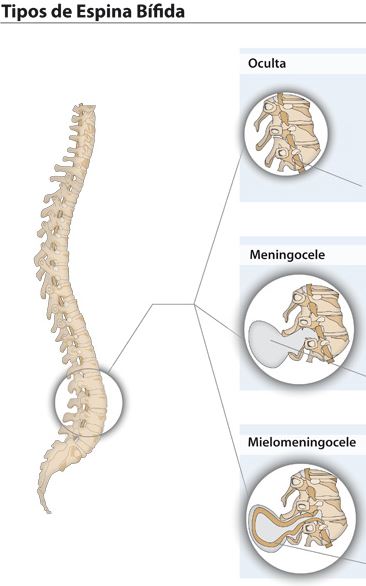
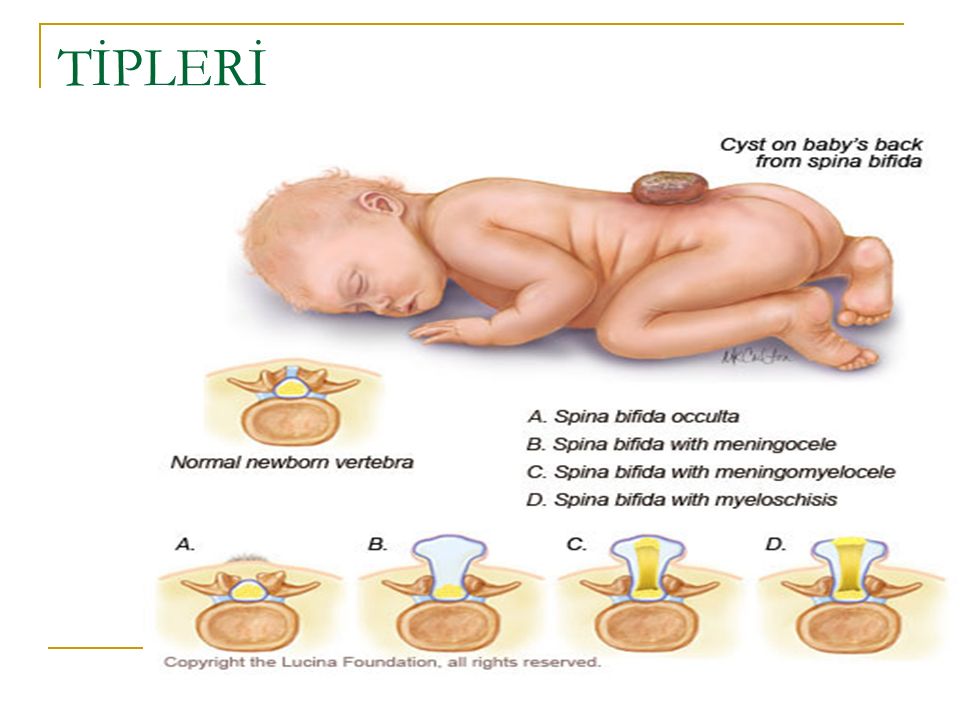
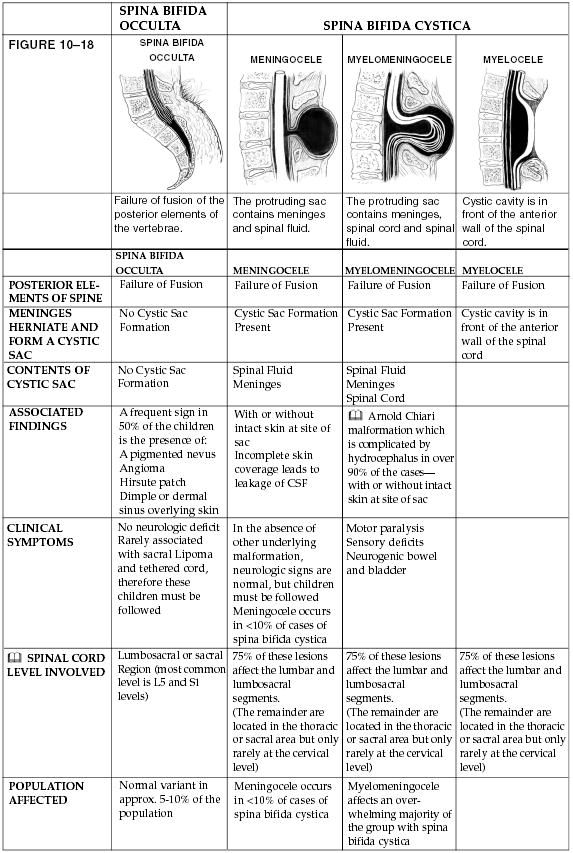
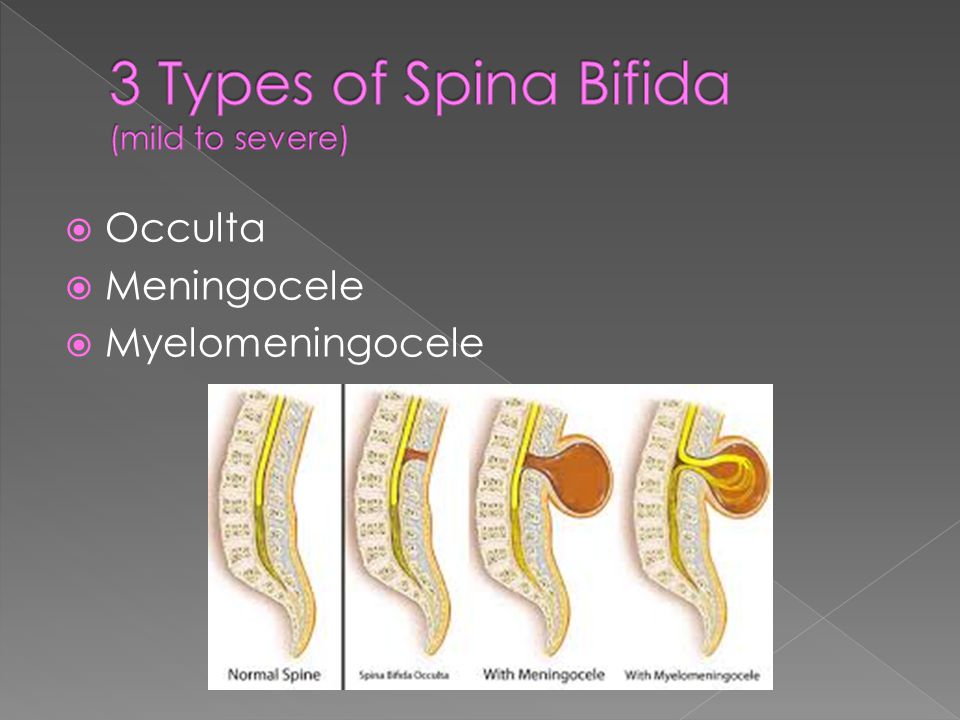
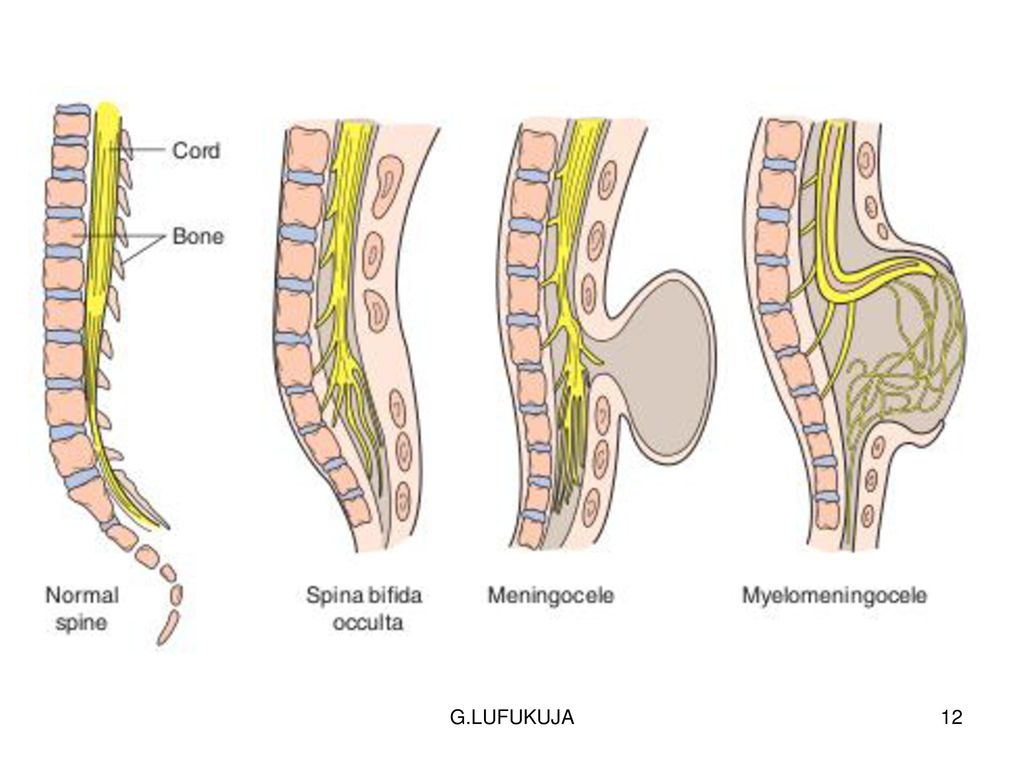
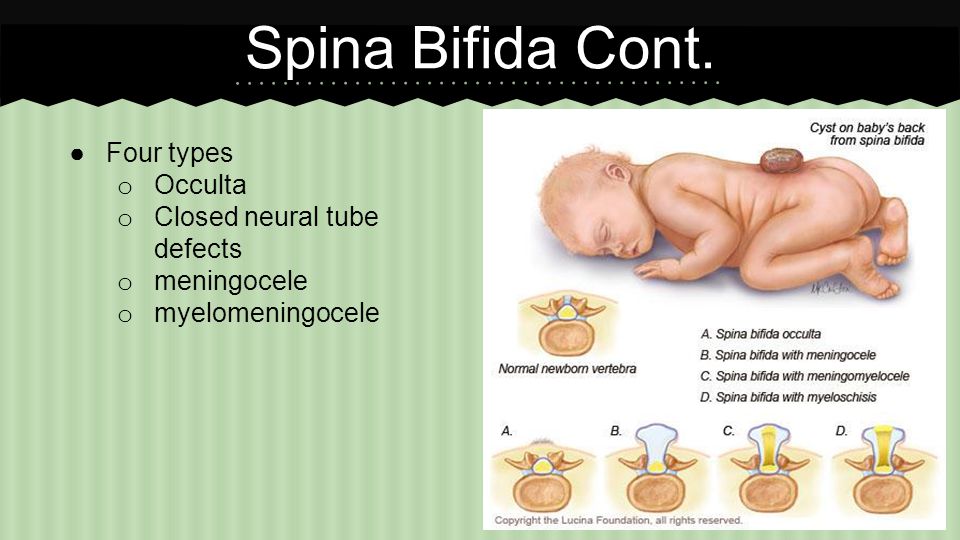
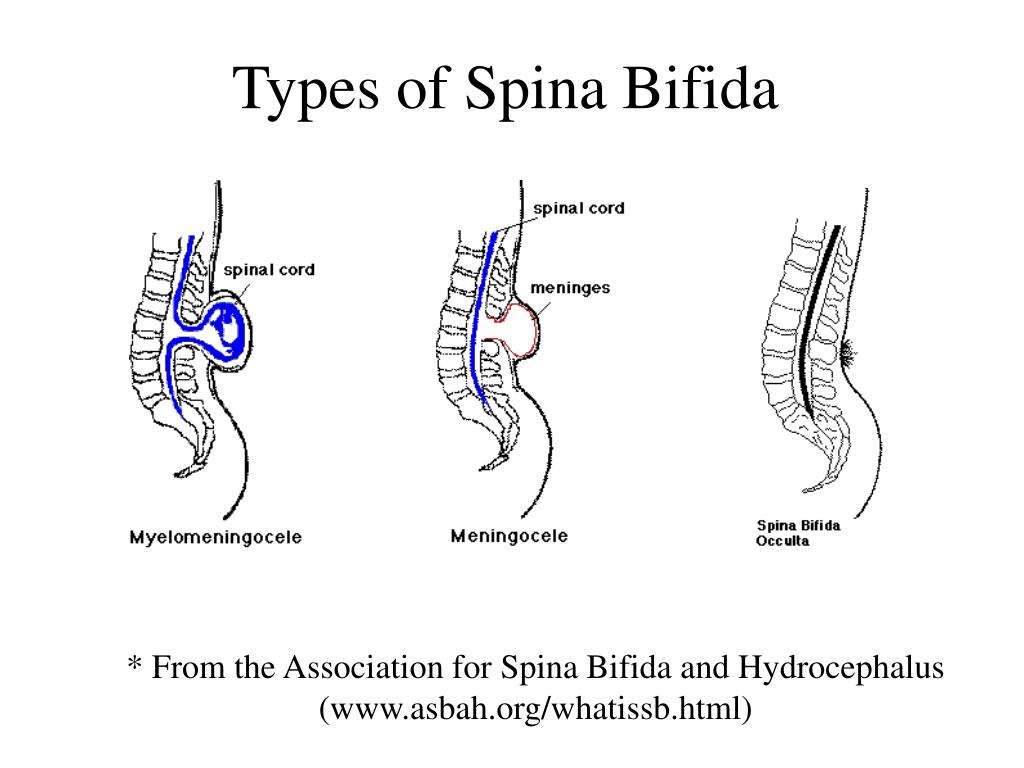
The four types of spina bifida are:
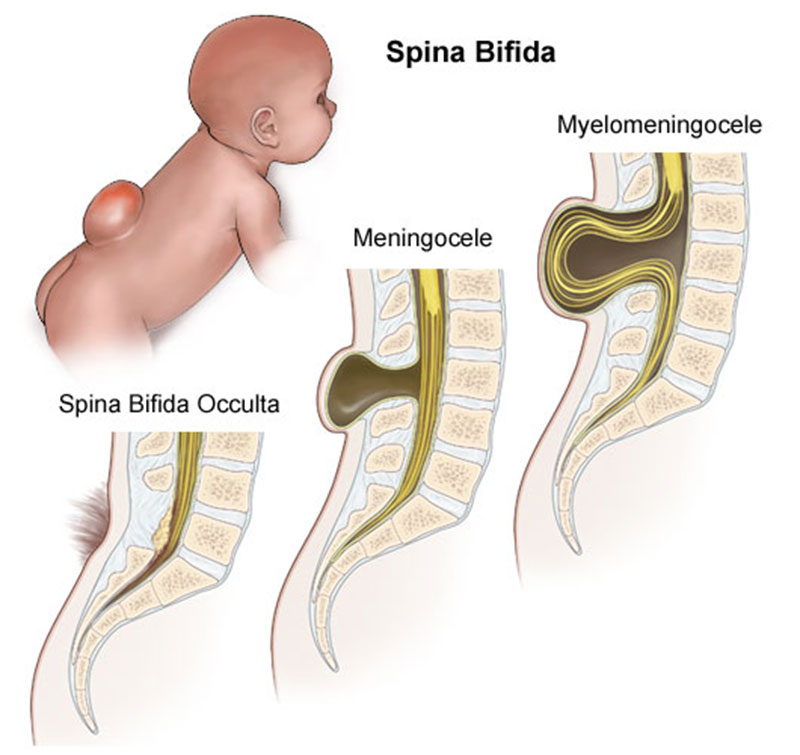
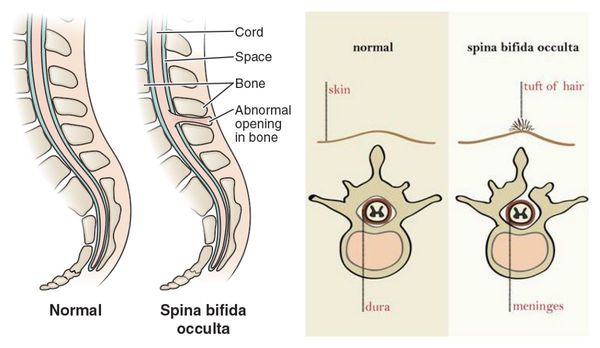
- Spina bifida occulta (also called hidden spina bifida). This is the mildest and most common form. It usually doesn’t cause health problems and you may never know your baby has it. In people who have this condition, the gap in the spine is small. The spinal cord and nerves stay in place and most often aren’t damaged. A dimple, hairy patch, dark spot or swelling may appear on the skin over the gap. If you see something like this at the bottom of your baby’s back, tell your baby’s health care provider.
- Closed neural tube defect.
 In people who have this condition, the fat, bone or meninges around the spinal cord don’t form correctly. This sometimes damages the nerves in the spinal cord. This condition often causes no symptoms, but some babies may have problems controlling their bladder and bowels.
In people who have this condition, the fat, bone or meninges around the spinal cord don’t form correctly. This sometimes damages the nerves in the spinal cord. This condition often causes no symptoms, but some babies may have problems controlling their bladder and bowels. - Meningocele. This is the rarest form of spina bifida. In this condition, the meninges push out through a gap in the spine. This creates a sac filled with fluid (called a meningocele) on the baby’s back. There’s usually little or no nerve damage, but some babies may have problems controlling their bladder and bowels. Surgery can remove the meningocele.
- Myelomeningocele (also called open spina bifida). This is the most severe form of spina bifida. In this condition, part of the spinal cord pushes out with the meninges through the opening in the spine to form a sac on the baby’s back. The spinal cord and nearby nerves are damaged. This can cause paralysis (when you can’t feel or move one or more parts of your body) and life-threatening infections.
 Babies who have this condition need surgery before birth or within the first few days of life. During surgery, a surgeon tucks the spinal cord and nerves back into the spine and covers them with muscle and skin. This can help prevent new nerve damage and infection. The surgery can’t fix any damage that’s already happened. Even with surgery, babies with this condition have lasting disabilities, such as problems walking and going to the bathroom.
Babies who have this condition need surgery before birth or within the first few days of life. During surgery, a surgeon tucks the spinal cord and nerves back into the spine and covers them with muscle and skin. This can help prevent new nerve damage and infection. The surgery can’t fix any damage that’s already happened. Even with surgery, babies with this condition have lasting disabilities, such as problems walking and going to the bathroom.
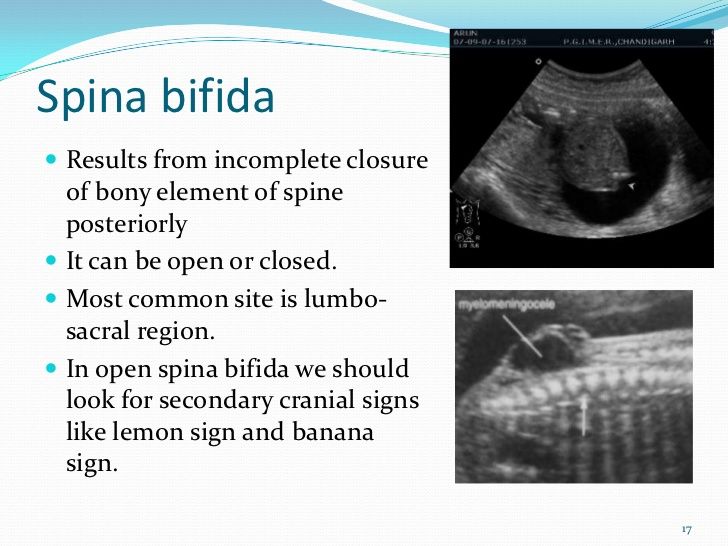
Doctors can diagnose most types of spina bifida when you’re pregnant or after your baby is born. If you baby has spina bifida occulta, it may not be diagnosed until later in your baby’s life.
Diagnosing spina bifida during pregnancyYou may have prenatal tests to check your baby for spina bifida and other birth defects. Prenatal tests used to diagnose spina bifida include:
- Maternal blood screening (also called quad screen).
 This blood test checks to see if your baby is at risk for certain birth defects, such as neural tube defects, heart defects and Down syndrome. The test is done at 15 to 22 weeks of pregnancy. If you have high levels of a substance called alpha-fetoprotein, your baby may have a neural tube defect such as spina bifida.
This blood test checks to see if your baby is at risk for certain birth defects, such as neural tube defects, heart defects and Down syndrome. The test is done at 15 to 22 weeks of pregnancy. If you have high levels of a substance called alpha-fetoprotein, your baby may have a neural tube defect such as spina bifida. - Amniocentesis. This test checks amniotic fluid taken from around your baby for birth defects such as neural tube defects. You can get this test at 15 to 20 weeks of pregnancy.
- Ultrasound. This test uses sound waves and a computer screen to show a picture of your baby. Providers may see spina bifida with this test.
Sometimes providers diagnose spina bifida after a baby is born. If your baby’s provider thinks your baby has spina bifida, they may use one of these tests to get a clearer view of your baby’s spine:
- Computed tomography (also called CT or CAT scan).
 CT scans use special X-ray equipment and powerful computers to make pictures of the inside of your baby’s body.
CT scans use special X-ray equipment and powerful computers to make pictures of the inside of your baby’s body. - Magnetic resonance imaging (also called MRI). This test uses a large magnet and radio waves to make a detailed picture of the inside of your baby’s body.
- X-ray. This test uses radiation to make a picture of your baby’s body.
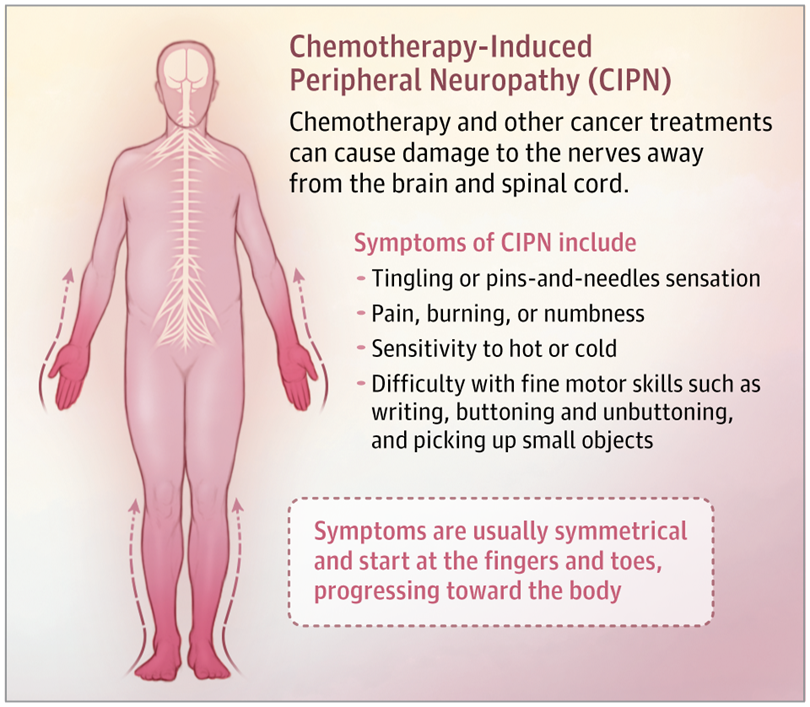
Spina bifida can cause several health problems, including:
Bowel problems. Bowel control can be a problem for people who have spina bifida. Feeding your baby certain foods to keep stools soft or giving your child foods with extra fiber may help make bowel movements more regular.
Chiari II malformation. This condition happens when the lower part of the brain sits in the upper part of the neck. Babies who have this condition usually have myelomeningocele.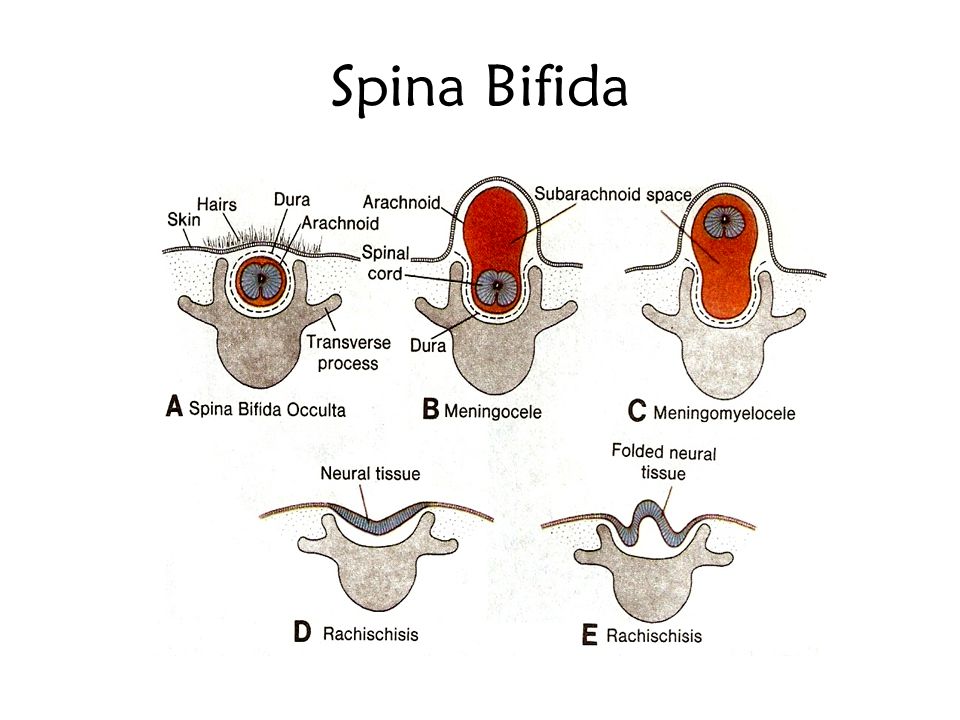 Some babies have:
Some babies have:
- Hydrocephalus. This is fluid buildup in the brain.
- Weakness or stiffness in the arms and hands
- Trouble feeding, breathing or swallowing
Hydrocephalus. Extra fluid in the head can cause it to swell and put pressure on the brain. In some cases, a surgeon needs to drain the extra fluid from a baby’s brain. The surgeon uses a shunt (a small hollow tube) that helps drain fluid and protects the brain from too much pressure. Hydrocephalus can cause intellectual and developmental disabilities.
Intellectual and developmental disabilities. These are problems with how the brain works that can cause people to have trouble or delays in physical development, learning, communicating, taking care of themselves or getting along with others. Children with spina bifida sometimes have problems with language, reading and math. They also may have trouble paying attention.
Latex allergy. Many babies who have spina bifida are allergic to latex (natural rubber).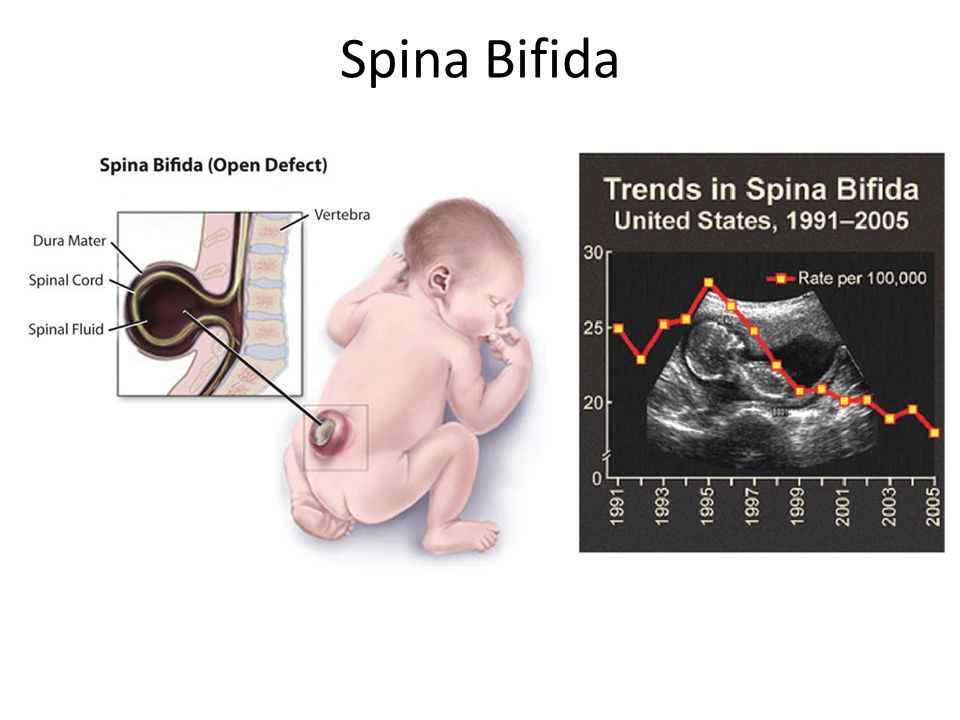 If your baby is allergic to latex, keep them away from items made of latex, such as latex bottle nipples, teething toys, changing pads, mattress covers and pacifiers. Your baby can wear a bracelet to let people know they have an allergy.
If your baby is allergic to latex, keep them away from items made of latex, such as latex bottle nipples, teething toys, changing pads, mattress covers and pacifiers. Your baby can wear a bracelet to let people know they have an allergy.
Meningitis. This is an infection that causes swelling in the brain and spinal cord. Meningitis can damage the brain and can be life-threatening. If your baby has meningitis, they may be treated with antibiotics.
Muscle weakness and joint pain. People who have spina bifida may have weak muscles and stiff joints because the nerves leading to the lower body are damaged. Surgery may help correct these conditions. Your baby may need physical therapy to help improve muscle weakness.
Paralysis. People who have spina bifida on the upper part of the spine may have paralyzed legs or feet. They may need to use wheelchairs. Those who have spina bifida lower on the spine (near the hips) may have more use of their legs.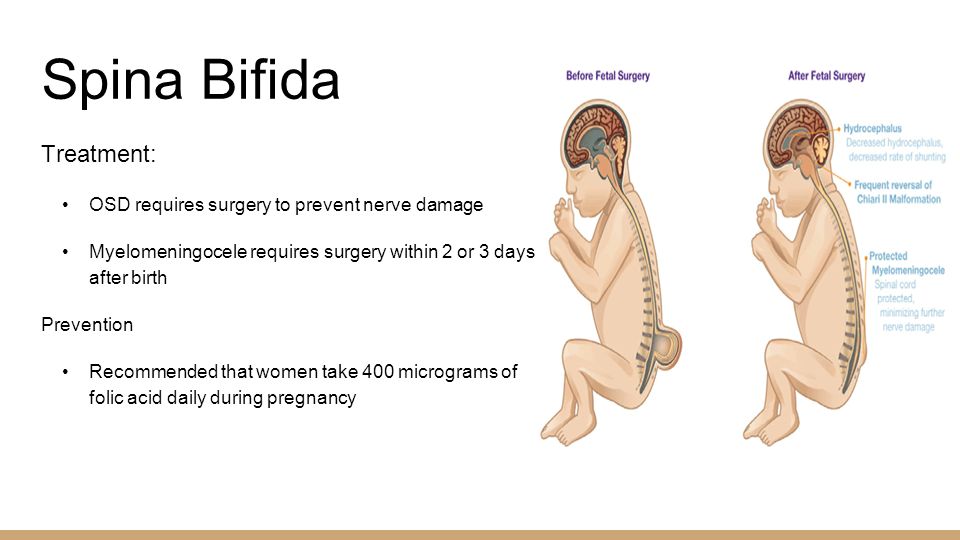 They may be able to walk on their own or use crutches, braces or walkers. Some babies can start exercises for the legs and feet to help them walk with braces or crutches when they get older.
They may be able to walk on their own or use crutches, braces or walkers. Some babies can start exercises for the legs and feet to help them walk with braces or crutches when they get older.
Skin problems. People who have spina bifida can develop sores, calluses, blisters and burns on their feet, ankles and hips. But they may not know they have these problems because they may not be able to feel certain parts of their body. Check your baby’s skin often for redness. Your baby’s health care provider can recommend ways to help prevent skin problems, such as giving cool baths and changing your baby’s position often.
Tethered spinal cord. Normally, the bottom of the spinal cord floats freely in the spinal canal (the hollow space around the spinal cord). If the cord becomes attached (also called tethered) to the spinal canal, the cord stretches as your baby grows. The stretching can cause nerve damage in the spine. The tethered spinal cord can be treated with surgery.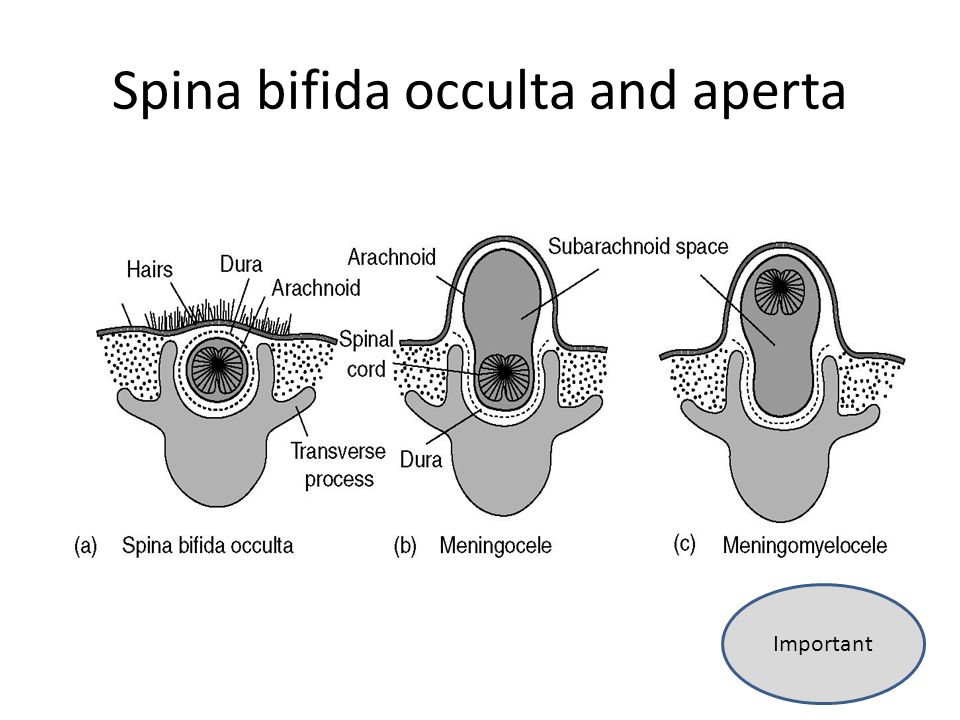 This condition affects babies who have myelomeningocele, meningocele and spina bifida occulta. Babies with a tethered spinal cord may have problems, including:
This condition affects babies who have myelomeningocele, meningocele and spina bifida occulta. Babies with a tethered spinal cord may have problems, including:
- Back pain
- Leg and foot weakness
- Bladder or bowel control problems
- A curved spine (also called scoliosis)
Urinary tract infections (also called UTIs). The urinary tract is the system of organs (including the kidneys and bladder) that helps your body get rid of waste and extra fluids in urine. Babies who have spina bifida often can’t control when they go to the bathroom because the nerves that help the bladder and bowels work are damaged. If your baby has problems emptying their bladder completely, it can cause UTIs and kidney problems. Your baby’s health care provider can teach you how to use a plastic tube called a catheter to empty your baby’s bladder.
Other conditions. Some people who have spina bifida have problems with:
- Obesity (being very overweight)
- Digestion (the process of how your body breaks down food after you eat)
- Social and mental health conditions, including depression.
- Vision
Your baby may have a team of providers who work together to treat health conditions caused by spina bifida. The team can include:
Doctors who treat your baby’s condition and related complications, including:
- A pediatrician who treats babies and children
- A neurologist who treats problems of the nervous system, including the brain, spinal cord and nerves
- An orthopedist who treats injuries and diseases of the bones, joints, ligaments, tendons, muscles and nerves
- A psychiatrist who treats people with emotional or mental health problems, like depression
- A urologist who treats problems of the urinary tract (kidneys, bladder, ureters and urethra)
Other providers, including:
- A developmental therapist who helps people develop behavior and social skills
- An occupational therapist who helps people do everyday activities, such as holding and letting go of things, getting dressed and feeding themselves
- A physical therapist who creates exercise programs to help improve strength and movement
- A psychologist who takes care of people’s emotional and mental health
More Information
- CDC videos about spina bifida
- CDC spina bifida resources
See also: Neural tube defects
Last reviewed: July, 2021
Spina bifida - Causes - NHS
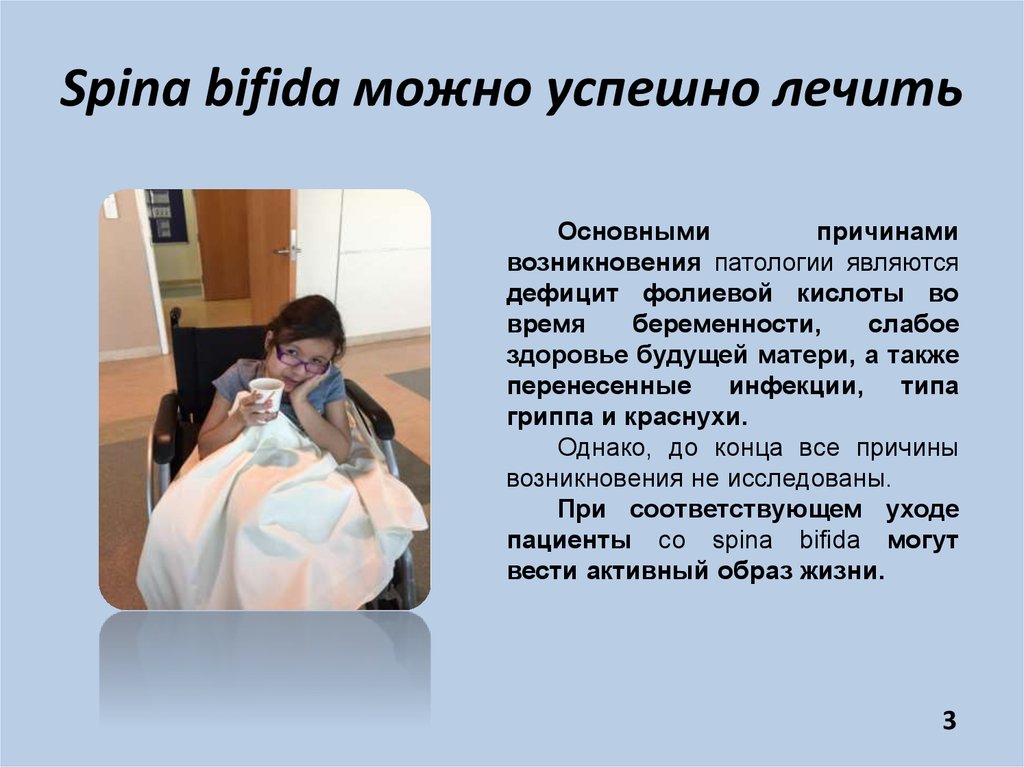
It's not known what causes spina bifida but a number of things can increase the risk of a baby developing the condition.
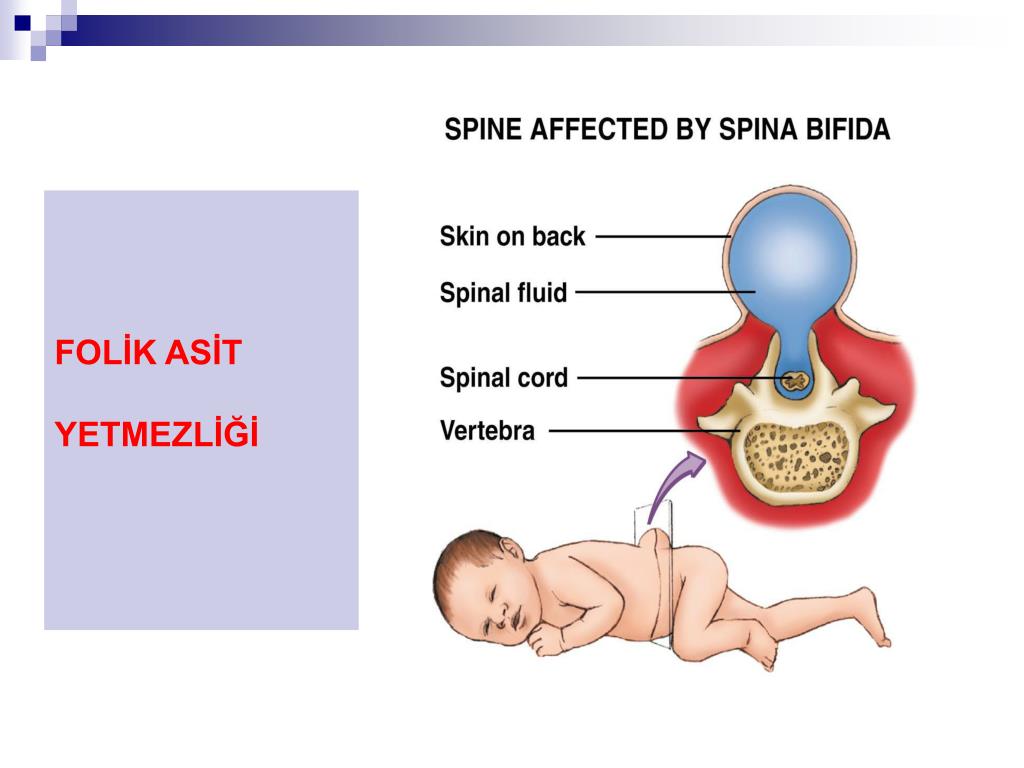
Lack of folic acid
Not having enough folic acid during pregnancy is one of the most important factors that can increase your chances of having a child with spina bifida.
Folic acid (also known as vitamin B9) occurs naturally in some foods, such as broccoli, peas and brown rice. It's also added to foods, such as some breakfast cereals. Folic acid tablets are available from pharmacies and supermarkets, or a GP may be able to prescribe them for you.
It's estimated that taking folic acid supplements before you conceive and while you're pregnant may prevent up to 7 out of 10 cases of neural tube defects, such as spina bifida.
It's not clear how folic acid helps prevent spina bifida. It's likely that folic acid is needed for important biochemical reactions in the body.
Read more about why you need folic acid in pregnancy.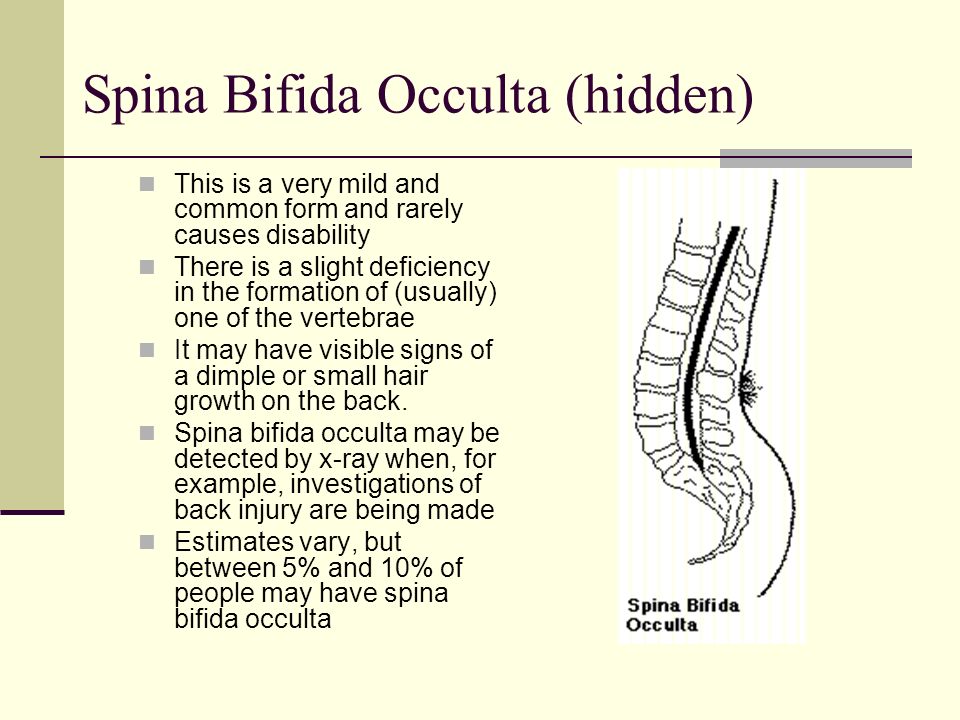
Family history
Having a family member with a neural tube defect, such as spina bifida, increases your chances of having a baby with spina bifida.
If you've previously had a child with spina bifida, your chance of having other children with the condition is increased.
If you have a family history of spina bifida, it's very important that you take high-dose folic acid, prescribed by a GP before you become pregnant, and for at least the first 12 weeks of pregnancy.
Medicine
Taking certain medicines during pregnancy has been linked to an increased risk of having a baby with spina bifida or other birth defects.
Valproate and carbamazepine are medicines linked to spina bifida. They're often used to treat epilepsy, and some mental health conditions, such as bipolar disorder.
Doctors will try to avoid prescribing these medicines if there's a chance you could get pregnant while taking them, but they may be needed if the alternatives are not effective.
It's advisable to use a reliable form of contraception if you need to take one of these medicines and are not trying to get pregnant.
Tell your doctor if you're thinking about trying for a baby and you need to take one of these medicines. They may be able to lower the dose and prescribe folic acid supplements at a higher than normal dose, to reduce the risk of problems.
If you're not sure whether a medicine could affect your pregnancy, check with your doctor, midwife or pharmacist before taking it. Never stop taking a prescribed medicine unless a GP or another healthcare professional responsible for your care advises you to.
Genetic conditions
Very rarely a baby can have spina bifida alongside a genetic condition such as Patau's syndrome, Edwards' syndrome or Down's syndrome.
If your baby is found to have spina bifida and it's thought they may also have one of these syndromes, you'll be offered a diagnostic test, such as amniocentesis or chorionic villus sampling. These tests can confirm if your baby has one of these genetic conditions.
Other risk factors
Other risk factors for spina bifida include:
- obesity – women who are obese (have a body mass index of 30 or more) are more likely to have a child with spina bifida than those of average weight
- diabetes – women with diabetes may have an increased risk of having a child with spina bifida
Page last reviewed: 20 April 2020
Next review due: 20 April 2023
Spina bifida. What is spina bifida?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment.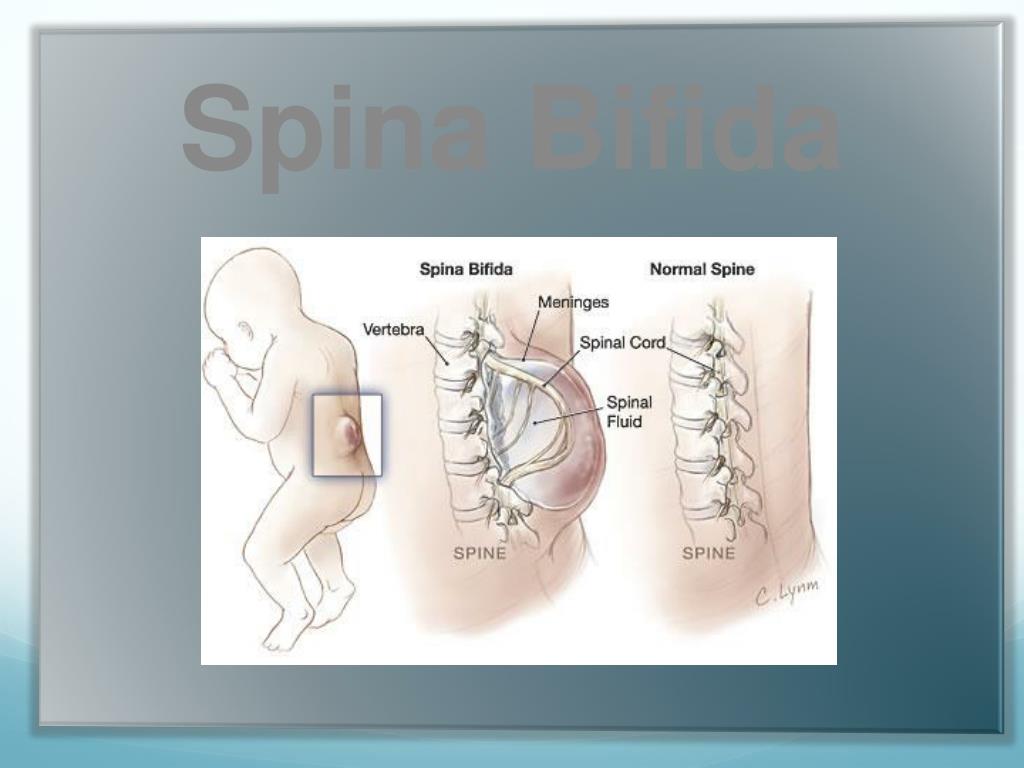 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Spina bifida is a malformation of the spinal column, which consists in the underdevelopment of the arches and / or bodies of one or more vertebrae with the formation of a defect in the wall of the spinal canal, through which the membranes and tissues of the spinal cord can prolapse with the formation of congenital spinal hernia. Clinical manifestations are observed in the formation of a hernia or compression of the spinal cord by connective tissue and fatty growths. It is diagnosed clinically, as well as with the help of radiography, CT and MRI of the spine. Treatment is surgical only. The operation is aimed at eliminating the existing defect, but in no way can affect the existing congenital pathology of the spinal cord itself.
- Causes of spina bifida
- Classification of spina bifida
- Symptoms of spina bifida
- Complications of spina bifida
- Spina bifida diagnostics
- Treatment and prognosis of spina bifida
- Prices for treatment
General
Spina bifida is a congenital anomaly of the spinal column, in which a defect in the bone tissues that form the spinal canal is formed at the level of one or more vertebrae.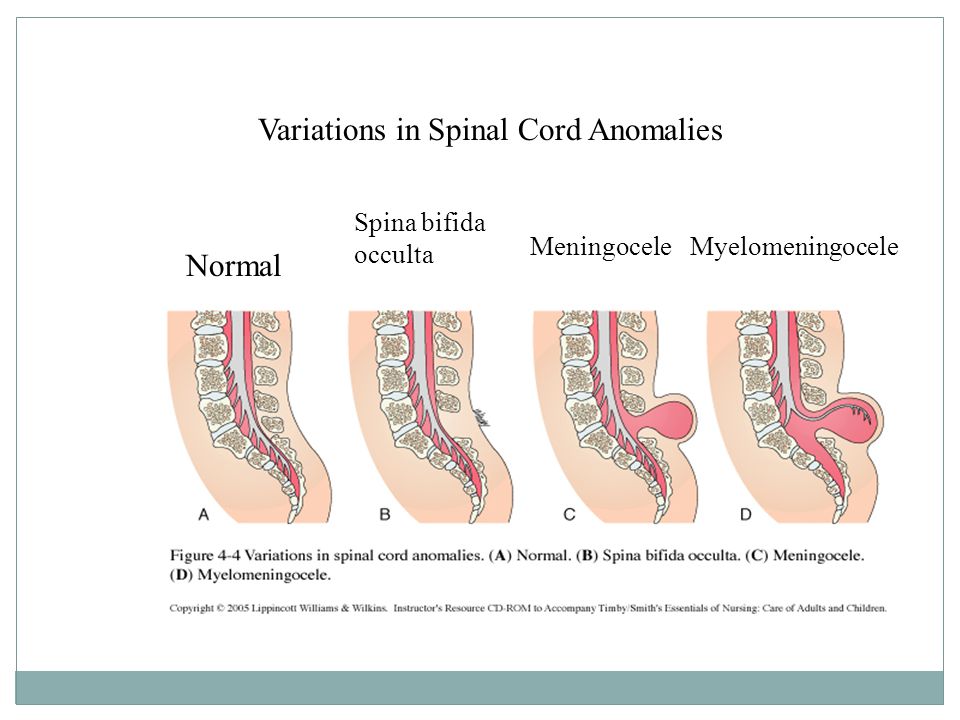 The spinal cord passes through the canal, which can prolapse at the level of the formed defect, forming a congenital spinal hernia. In modern neurology and neonatology, spina bifida is also referred to by the Latin term spina bifida. The prevalence of this anomaly in the development of the spine among the population, according to some data, is up to 20%. At the same time, the incidence of congenital spinal hernia does not exceed 1 case per 3000 newborns. Most often, the anomaly is localized in the lumbosacral spine. 99% of congenital hernias of the spinal cord are formed in the back of the spinal canal. The contents of the hernia may vary. An exit to the hernial sac of the tissues of the spinal cord is observed in 75% of cases.
The spinal cord passes through the canal, which can prolapse at the level of the formed defect, forming a congenital spinal hernia. In modern neurology and neonatology, spina bifida is also referred to by the Latin term spina bifida. The prevalence of this anomaly in the development of the spine among the population, according to some data, is up to 20%. At the same time, the incidence of congenital spinal hernia does not exceed 1 case per 3000 newborns. Most often, the anomaly is localized in the lumbosacral spine. 99% of congenital hernias of the spinal cord are formed in the back of the spinal canal. The contents of the hernia may vary. An exit to the hernial sac of the tissues of the spinal cord is observed in 75% of cases.
Spina bifida
Causes of spina bifida
Spina bifida is caused by disorders in the formation of the neural tube, which occurs at the 3rd week of pregnancy and ends by the 23rd day of gestation.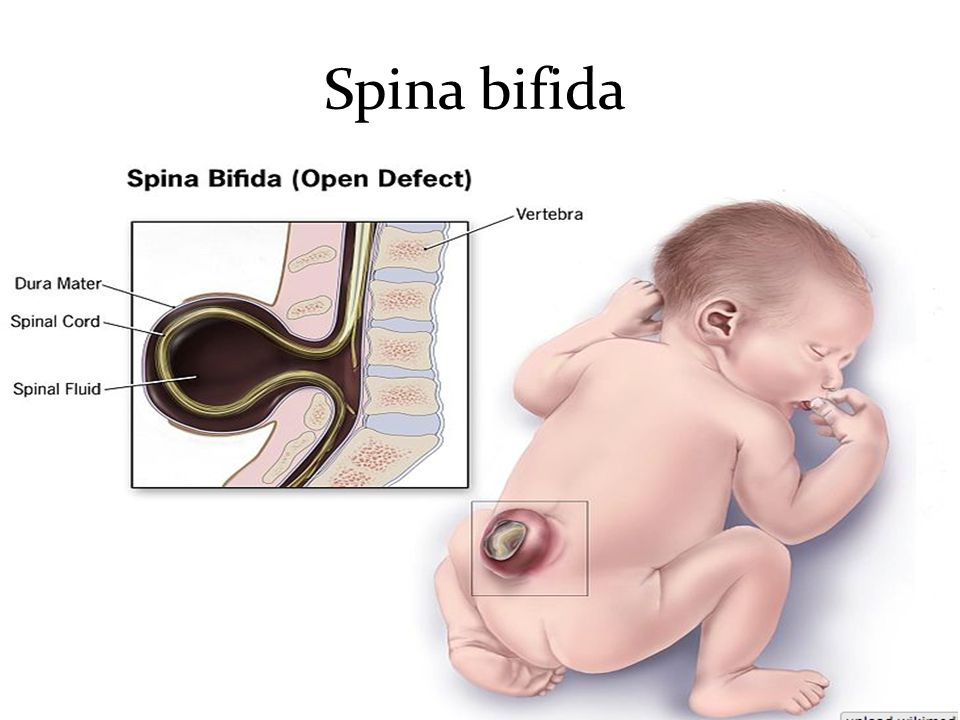 Spina bifida is a multifactorial pathology. Hereditary mechanisms, spontaneous mutations and exposure to teratogenic factors may play a role in its development.
Spina bifida is a multifactorial pathology. Hereditary mechanisms, spontaneous mutations and exposure to teratogenic factors may play a role in its development.
The latter include intrauterine infections (cytomegaly, measles, rubella, herpes), hyperglycemia in diabetes mellitus, constant overheating of the body of a pregnant woman (insolation, hot baths, sauna), taking pregnant pharmaceuticals with a teratogenic side effect (for example, antibiotics, anticonvulsants), folate deficiency acids, intoxication (drug addiction, alcoholism, substance abuse, occupational hazards), radiation. The situation is aggravated by the fact that often at such early stages of gestation, a woman does not know about her pregnancy and does not comply with the necessary protective regime aimed at excluding possible teratogenic effects as much as possible.
Classification of spina bifida
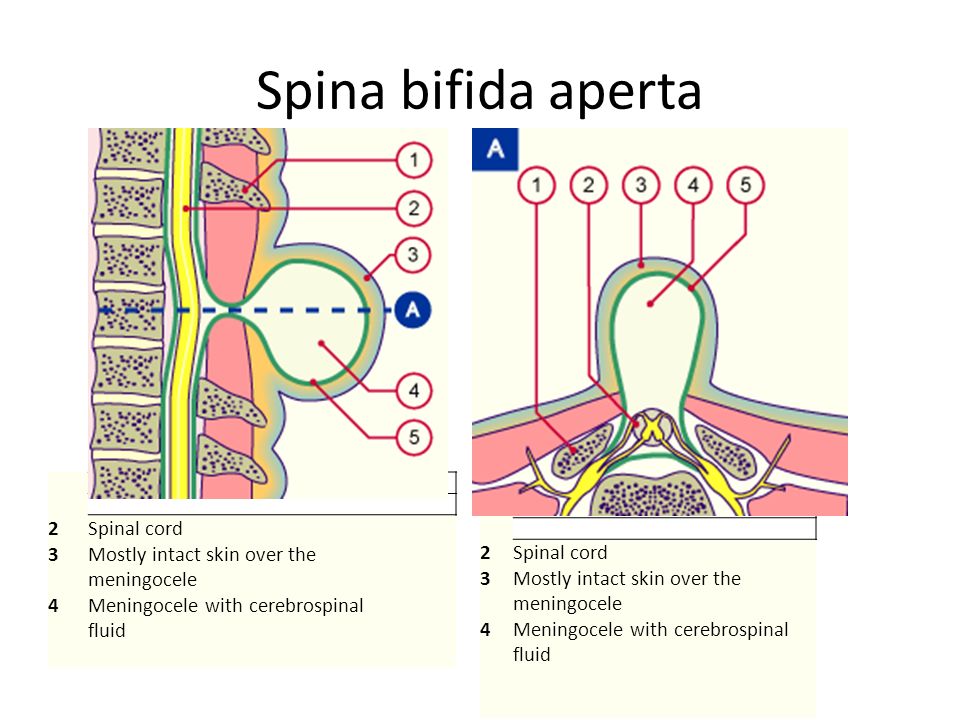
Allocate hidden and open spina bifida. Hidden (spina bifida occulta) is a small bone defects (for example, non-closure of the vertebral arches) without the formation of a spinal hernia.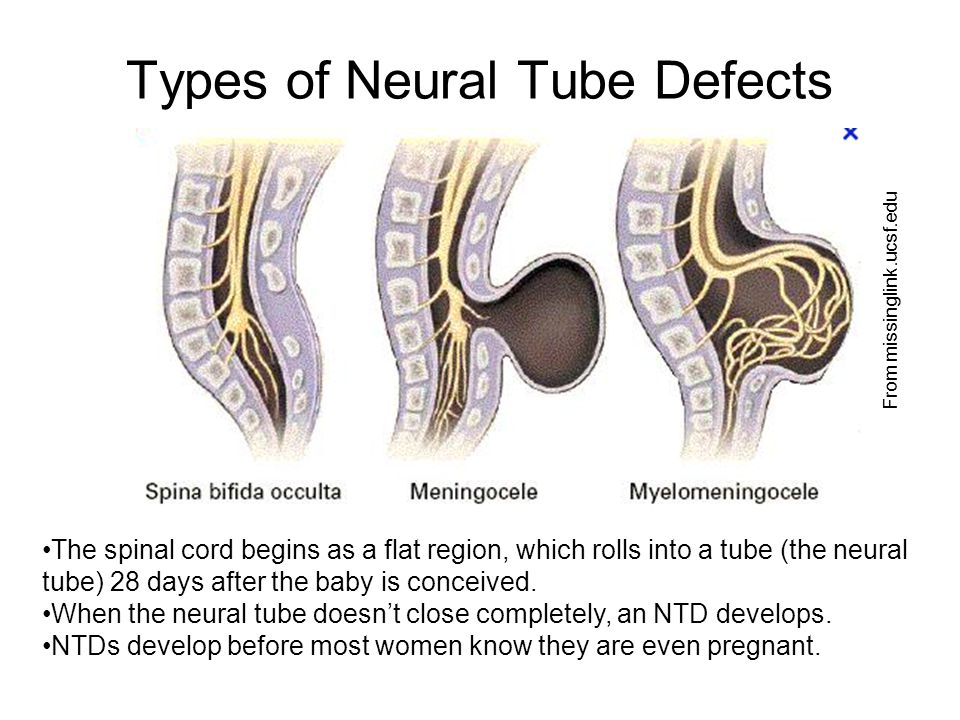 Open spina bifida (spina bifida aperta) includes rachischisis and herniated spinal cord. Any type of spina bifida can be accompanied by the growth of fibro-adipose tissue that fills bone defects, penetrates into the subarachnoid space and causes compression of the spinal cord.
Open spina bifida (spina bifida aperta) includes rachischisis and herniated spinal cord. Any type of spina bifida can be accompanied by the growth of fibro-adipose tissue that fills bone defects, penetrates into the subarachnoid space and causes compression of the spinal cord.
Depending on the contents of the hernial sac, there are 4 forms of congenital spinal hernias. With meningocele, only cerebrospinal fluid (CSF) is in the hernial sac. Meningoradiculocele, in addition to cerebrospinal fluid, contains the membranes of the spinal cord. In myelomeningocele, the hernia consists of cerebrospinal fluid, membranes, and tissues of the spinal cord. Myelocystocele is a complete prolapse of a segment of the spinal cord with membranes, accompanied by eversion and expansion of the spinal canal. Rakhishizis is a spina bifida in the most severe form, when a bone defect of great length is combined with non-fusion of the membranes of the spinal cord and skin. In this case, the spinal cord is visible through a gaping hole in the spine.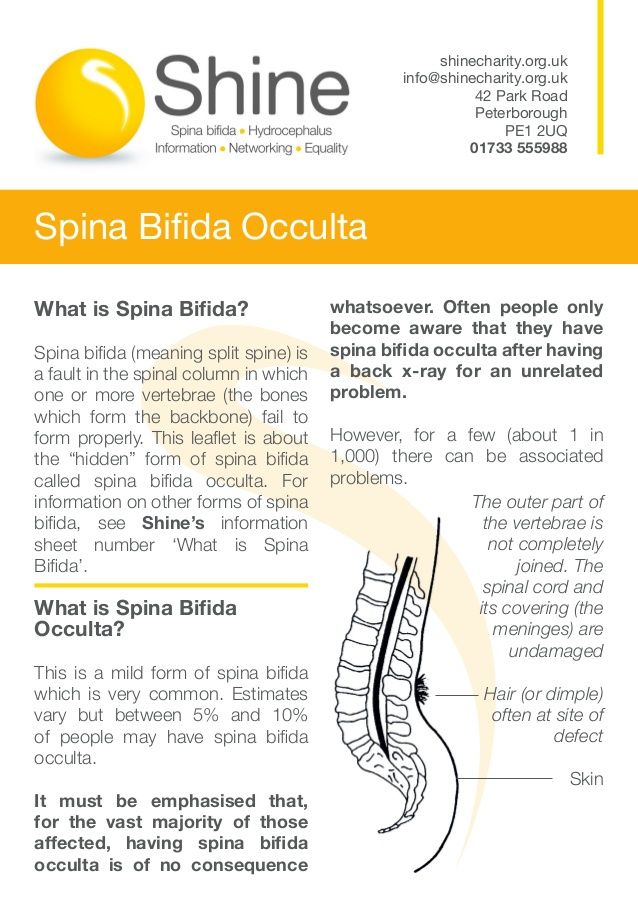 This pathology leads to death.
This pathology leads to death.
Symptoms of spina bifida
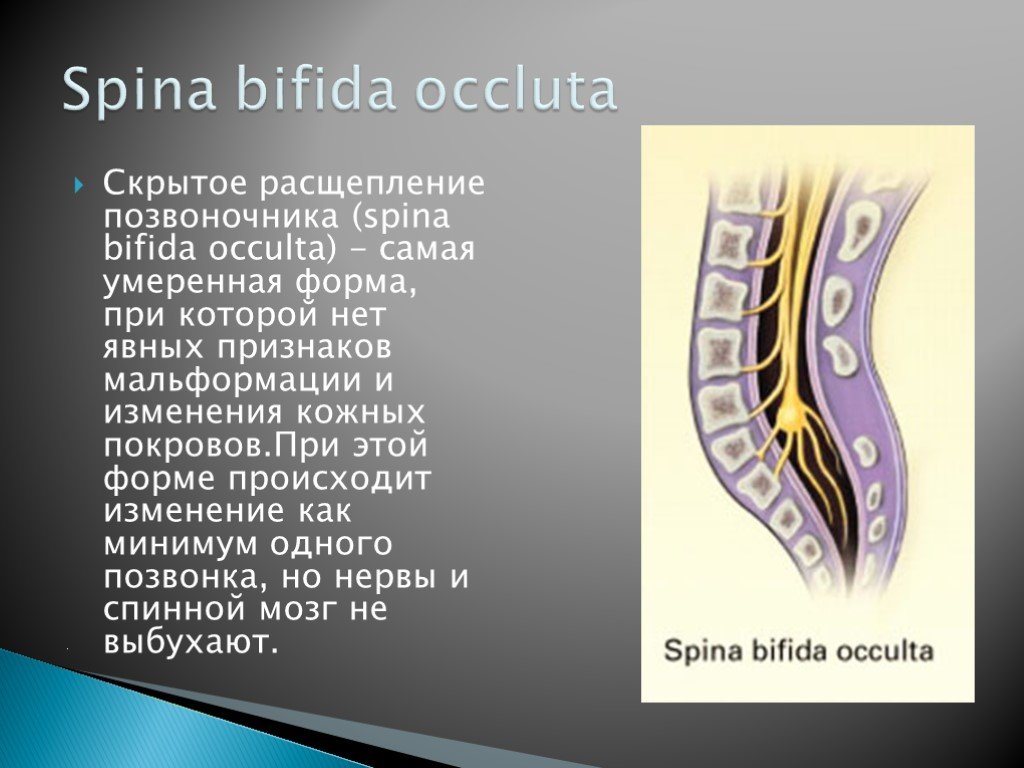
Latent spina bifida is usually asymptomatic. Clinical manifestations manifest in cases of proliferation of fibro-adipose tissue with compression of the roots and other structures of the spinal cord. Most often, the debut of the clinic falls on adolescence. Characterized by radicular pain of the type of sciatica, which the patients themselves describe as a sensation of the passage of an electric current. On the skin in the area of a bone defect, as a rule, there is a tuft of hair and / or a pigment spot, sometimes a papilloma.
A meningocele is characterized by a visible bulge on the spine covered by a thin layer of skin. Such spina bifida occurs without the development of a neurological deficit. Meningoradiculocele is a protrusion that occupies the area from 4 to 5 vertebrae. The nature of neurological disorders depends on the number of roots involved in the hernial sac and the location of the hernia.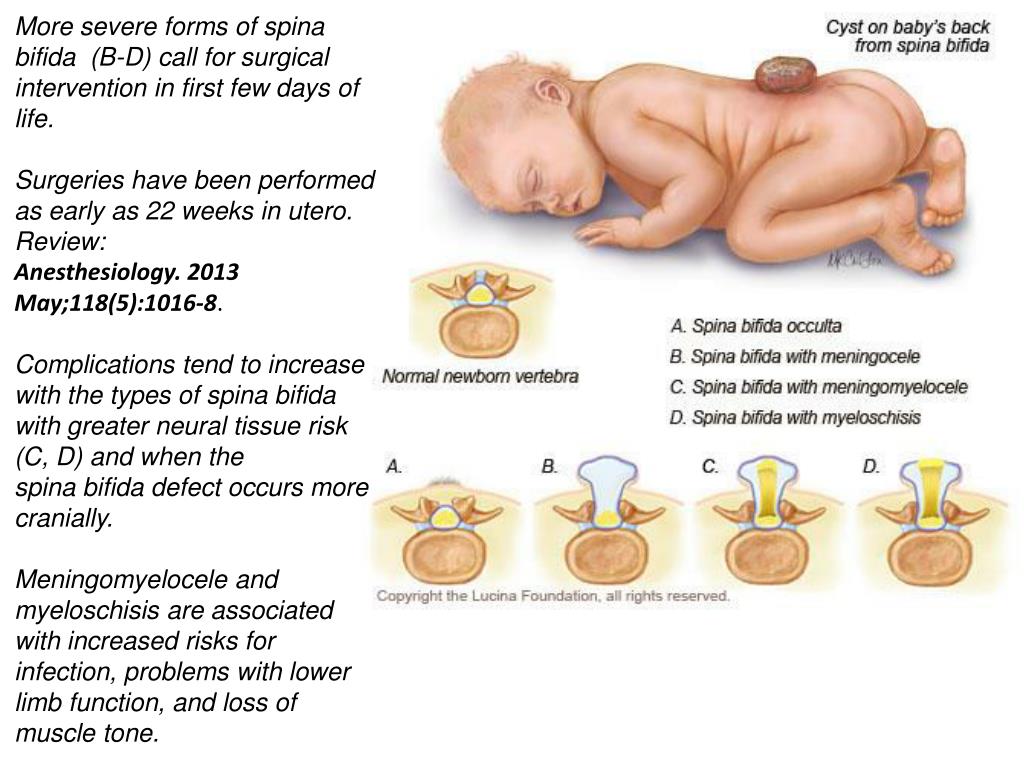 The clinic can vary from mild paresis to a pronounced decrease in muscle strength, sensory and pelvic disorders. Myelomeningocele and myelocystocele involve 6 to 8 vertebrae and are not covered by skin, characterized by severe paralysis, lack of sensation, urinary incontinence, and encopresis.
The clinic can vary from mild paresis to a pronounced decrease in muscle strength, sensory and pelvic disorders. Myelomeningocele and myelocystocele involve 6 to 8 vertebrae and are not covered by skin, characterized by severe paralysis, lack of sensation, urinary incontinence, and encopresis.
Spina bifida is often accompanied by hydrocephalus. It can be combined with other malformations: Chiari anomaly, curvature of the spine (scoliosis, kyphosis), clubfoot, congenital limb deformities, hip dysplasia, congenital heart defects, multiple dermatofibromas, lipomas, teratomas.
Complications of spina bifida
Spina bifida with the formation of a hernia is dangerous by infection of the hernial sac. As a rule, such a complication occurs in the absence of the skin over the hernial protrusion. In addition, infection can occur with ruptures and other damage to the thinned skin covering the hernia. In such cases, reddening of the tissues of the hernial sac and surrounding skin is observed.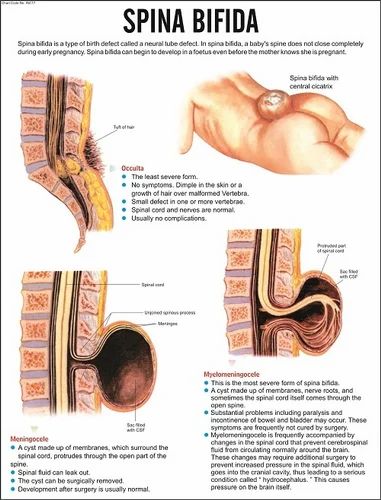 Infection is dangerous by the spread of inflammation to the meninges with the development of meningitis, the infection enters the bloodstream with the onset of sepsis.
Infection is dangerous by the spread of inflammation to the meninges with the development of meningitis, the infection enters the bloodstream with the onset of sepsis.
Another complication of congenital spinal hernias can be a rupture of the hernial sac with the outflow of cerebrospinal fluid (liquorrhea), which leads to a drop in cerebrospinal fluid pressure and also opens the gate for infection. In addition, spina bifida can be complicated by increasing compression of the spinal cord, which eventually leads to irreversible changes in the spinal tissues.
Spina bifida diagnostics
Hidden spina bifida is often not diagnosed during life. The diagnosis of congenital spinal hernia is established by a neonatologist together with a neurologist according to the clinic and the results of palpation - palpation of the bone defect of the spine. Clarification of the diagnosis is carried out using CT and MRI of the spine. CT of the spine to a greater extent allows you to identify existing bone defects and deformities, MRI - to obtain information about the state of the spinal cord and its membranes, to establish the contents of the hernial sac. In younger children, CT is not performed due to high radiation exposure. In the absence of the possibility of a tomographic examination, an X-ray of the spine is used.
In younger children, CT is not performed due to high radiation exposure. In the absence of the possibility of a tomographic examination, an X-ray of the spine is used.
CT scan of the lumbar spine. Absence of complete fusion of the L5 arch (Spina bifida)
It is mandatory to conduct a study of somatic organs to identify concomitant congenital pathology. For this purpose, a biochemical analysis of blood and urine, urography, CT scan of the kidneys, chest x-ray, ultrasound of the heart, ultrasound of the abdominal cavity, MSCT of the abdominal cavity, radiography of bones and joints are prescribed. Specialists of various profiles can be involved in the diagnosis as necessary: nephrologist, cardiologist, gastroenterologist, etc.
In some cases, prenatal diagnosis is possible. Spina bifida can be suspected according to obstetric ultrasound, amniocentesis, followed by a study of the concentration of acetylcholinesterase and α-fetoprotein in the amniotic fluid.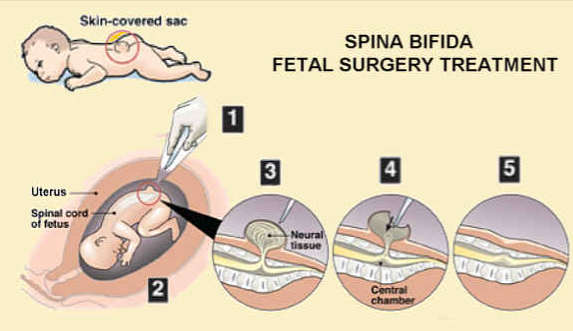 Prenatally diagnosed spina bifida is an indication for caesarean section, which helps to prevent injury to the spinal hernia during natural childbirth.
Prenatally diagnosed spina bifida is an indication for caesarean section, which helps to prevent injury to the spinal hernia during natural childbirth.
Treatment and prognosis of spina bifida
Open spina bifida needs surgical treatment. The operation is carried out by neurosurgeons in a planned manner in the first days of a newborn's life. It helps to prevent the development of complications and the growth of neurological deficit, to eliminate the existing cosmetic defect. In case of violation of the integrity of the hernial sac and liquorrhea, the operation is performed in an urgent manner. Contraindications to surgical treatment may be severe disorders of the somatic organs due to concomitant congenital pathology.
The operation is performed using general anesthesia. Its essence is to close the existing defect. An incision is made along the surface of the hernial protrusion. Nerve formations are carefully separated and retracted inside behind the spinal membranes. The membranes are sutured in layers, the skin defect is closed. Complications of surgical intervention can be increasing hydrocephalus, infection of the wound, divergence of its edges, trophic disorders in the area of the postoperative wound that interfere with its healing. A lumboperitoneal shunt may be used to prevent hydrocephalus.
The membranes are sutured in layers, the skin defect is closed. Complications of surgical intervention can be increasing hydrocephalus, infection of the wound, divergence of its edges, trophic disorders in the area of the postoperative wound that interfere with its healing. A lumboperitoneal shunt may be used to prevent hydrocephalus.
In the postoperative period, rehabilitation treatment is carried out, aimed at increasing muscle strength and range of motor activity, preventing joint contractures. Various methods of physiotherapy, physiotherapy exercises, massage are used. The outcome of the operation largely depends not on the skills of the neurosurgeon, but on the form of the spinal hernia. If spina bifida is not accompanied by the involvement of spinal cord tissues in the hernial sac, then after the operation there is a complete or significant restoration of neurological functions. With myelomeningocele and myelocystocele, the existing neurological deficit persists after surgery, since surgical intervention is not able to restore the altered tissues of the spinal cord.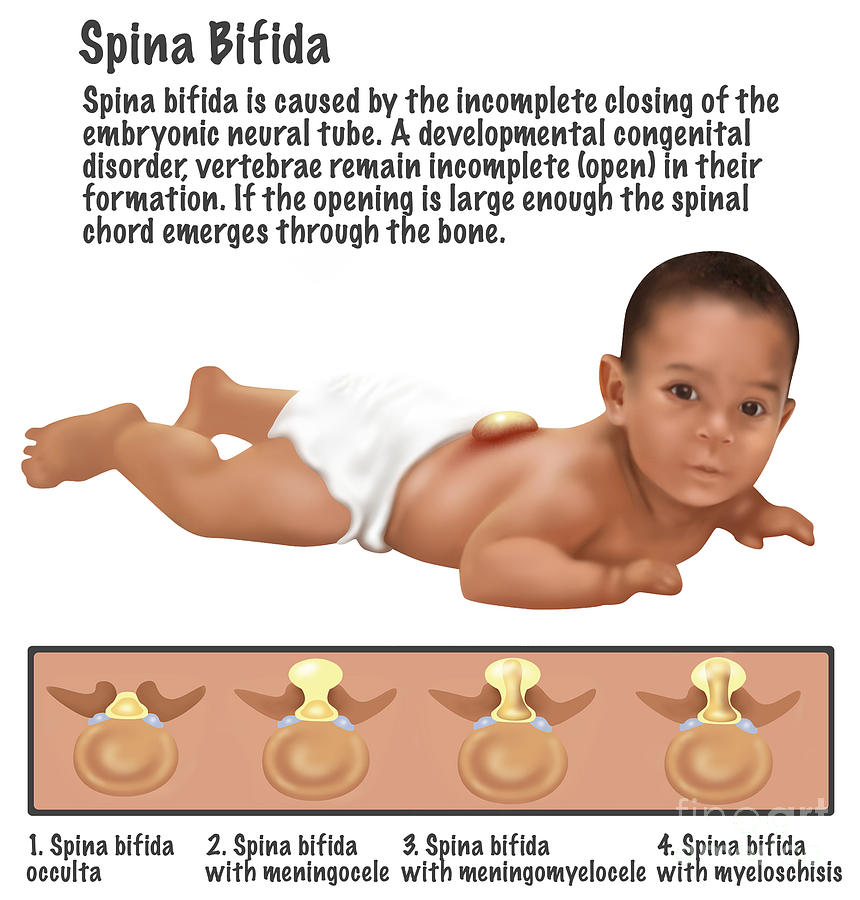
You can share your medical history, what helped you with the treatment of spina bifida.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
information from professional doctors of the Median Medical Center
The most common congenital malformation is a violation of the formation of the spine and spinal cord, united by the concept Spinal dysraphia, or defects in the development of the neural tube, have a common term Spina Bifida (Spina Bifida, in Latin - non-fusion / spina bifida), often combined with developmental disorders of the spinal cord and spinal roots in different variations, from the simplest to the most severe. Occurs during the first 28 days of pregnancy when the neural tube of the fetus is forming. The neural tube is the part of the embryo from which the brain and spinal cord are formed.
 It can be observed in various parts of the spine. It is most common in the lower thoracic, lumbar, or sacral regions and usually extends over 3–6 vertebral segments. Some children are asymptomatic, others develop severe neurological and physical dysfunction below the site of the lesion.
It can be observed in various parts of the spine. It is most common in the lower thoracic, lumbar, or sacral regions and usually extends over 3–6 vertebral segments. Some children are asymptomatic, others develop severe neurological and physical dysfunction below the site of the lesion. The vice is commonly called the "snowflake condition" because no two cases are the same.
The worldwide prevalence of Spina Bifida is estimated at 4.8 cases per 10,000 live births. The frequency of spinal hernias in different parts of the spine varies significantly: 2-5% is localized in the cervical region, 2-3% in the thoracic region, 25% in the lumbar region, and 65-70% in the lumbosacral region.
At present, the concept of "Spinal dysraphia" combines various developmental disorders of the spinal cord and spine, depending on the severity, magnitude of spina bifida, localization, level of spinal cord injury, and in accordance with the characteristics of the development of the defect, the following types of spina bifida (Spina Bifida) are distinguished :
- Spina Bifida occulta
- Spina Bifida cystica aperta - open spina bifida with the formation of cystic spinal hernia;
- Rhachischisis posterior (totalis et partialis) - spina bifida and soft tissues with spreading of the spinal cord, which occur throughout the spine or only in some part of it.
Hidden form (Spina Bifida occulta) - the simplest type of spina bifida, and at the same time, the spinal cord and spinal roots can be born in the physiological norm, the person is healthy, but even under this (Here) the pathology of the development of the spinal cord and roots can be hidden, which can cause problems for health, and more on that later.
The anatomical essence of occult spina bifida consists in incomplete fusion of the vertebral arch, caused by a violation of ossification and, as a rule, does not manifest itself clinically, does not require medical attention. Often they are an accidental "find" during X-ray examination of the spine, and people did not even know that they had this malformation. This pathology occurs in approximately 20% of Caucasians. With a hidden form, there may be no visual defects on the back. It is characterized by only a small defect or gap in the vertebrae that form the spinal column. Often this form of pathology is so moderately expressed that it does not cause any concern.
 Most often, this form of Spina Bifida - hidden spinal clefts are localized in the lumbosacral spine. The skin in the area of cleft vertebral arch is not changed.
Most often, this form of Spina Bifida - hidden spinal clefts are localized in the lumbosacral spine. The skin in the area of cleft vertebral arch is not changed. However, 1-2 out of 1000 patients with this form of defect is combined with a pathology that leads to the appearance and progression of symptoms of damage to the spinal cord, roots and cone of the spinal cord.
On the skin in the area of spinal fusion, external signs (stigmata) can very often be observed - a pigment spot, hyperpigmentation, soft tissue hemangioma, a spot in the form of a delicate scar, retraction of the dermis as a small indentation / dimple on the skin, local growth of dark hair (hypertrichosis) , subcutaneous wen (lipoma), fistulous tract (dermal sinus), teratoma.
In such cases, the congenital malformation of the latent Spina Bifida has concomitant changes that lead to muscle weakness and slow atrophy of the lower extremities, foot deformities, sensory and trophic disorders with impaired motor function of the legs, impaired posture, pain in the lumbosacral region, urinary and intestinal dysfunction, bedwetting and other manifestations.
 It is these cases of Spina Bifida occulta that require surgical care.
It is these cases of Spina Bifida occulta that require surgical care. This is how the following pathologies manifest themselves: Diastematomyelia, Spinal Lipoma, Dermal Sinus, or a combination of the latter, with the manifestation of the Fixed spinal cord clinic.
Diastematomyelia (Diastematomyelia) , the term comes from the Greek “diastematos” - gap and “myelos” - brain) - “Split spinal cord” is a hidden malformation of the development of the spine and spinal cord characterized by the formation of a bone, cartilage or fibrous septa or cord, coming from the arches, the vertebral body and partially dividing the spinal cord in the longitudinal direction into two halves (hemichords), while there is a central canal in each of them. In this place, the spinal cord is fixed, which delays its growth and upward displacement.
There are two variants of this pathology:
type I – when both the spinal cord and the dural sac are divided into two separate “sleeves”; two hemichords are located in their own dural sacs, separated by an extradural bone spine or cartilaginous bridge;
Type II - when the spinal cord itself is divided into two halves by an intradural fibrous, cartilaginous cord and they are located in a single dural sac, this is called diplomamyelia.
A feature of the anomaly of the septum is the inclusion of abnormal vessels and vestigial nerves. The vast majority of diastematomyelia is located on the lower thoracic - lumbar spine. Diastematomyelia in 40 - 50% of cases is combined with myelomeningocele, dermal sinus, thickened terminal thread. In 85%, a combination with spinal defects (vertebral segmentation, vertebral body hypoplasia) was noted. The period of absence of clinical manifestations of the disease and the manifestation of neurological symptoms depend on the anatomical features of the defect and the growth rate of the child. In most cases, primary neuroorthopedic symptoms appear between 3.5 and 7 years of age.
Lipomeningocele (Lipomeningosele) in children (lipomyeloshisis, lipomeningocele, lipoma of the cone of the spinal cord, lipoma of the spinal cord) is one of the most common variants of the latent form of spinal dysraphism, the content of which is degenerate adipose tissue and tender fat with elements of the spinal cord and usually has a fatty subcutaneous mass.
 With this type of pathology, Spina Bifida, a fatty layer (lipoma, lipomatous tissue, fibroma), which extends from the back side through a defect - a gap or hole in the spine presses on the spinal cord, which leads to disruption of the organs.
With this type of pathology, Spina Bifida, a fatty layer (lipoma, lipomatous tissue, fibroma), which extends from the back side through a defect - a gap or hole in the spine presses on the spinal cord, which leads to disruption of the organs. Depending on the anatomical relationship of lipomas with the spinal cord, the following forms are distinguished: dorsal lipoma, caudal lipoma, mixed lipoma. In relation to the dura mater and the spinal canal, they are divided into intradural, intra, and extradural.
At birth, in most cases, lipomas of the conus of the spinal cord are asymptomatic (70%) and are manifested by skin signs: subcutaneous lipoma, angioma, skin pits, asymmetry of the gluteal fold. The presence or absence of neurological symptoms depends on the degree of involvement of the cone, cauda equina roots, and terminal filament in the developmental anomaly. Periods of occurrence and progression of neurological and functional symptoms of the disease appear during periods of active growth of the child (1st - from 0 to 4 years, growth of 24 cm in the 1st year of life).
Spinal dermal (skin) sinus (Dorsal dermal sinus) is a hidden spinal malformation, represented by a fistulous tract formed by the skin ectoderm and spreading between the skin and structures of the brain and spinal cord.
Dermal sinus presents as a small dimple, skin depression, or punctate orifice, sometimes with sanious or clear discharge, which is often associated with an area of hyperpigmented, angiomatous skin or hypertrichosis and occurs in the median site or, more rarely, in the paramedian site. Soft tissue asymmetries and bone anomalies are common.
Lesions most commonly occur in the lumbosacral region, but can be seen anywhere along the midline—cervical, thoracic, cranial, and genital areas. Lateral congenital cutaneous sinuses may occur on the buttocks. The hole is not always located with a fistulous tract and may be located at the distance of several segments. Skin changes are the most common reason for seeking medical attention.
Identified dermal sinus in the first months of life, usually asymptomatic.
 In 60% of cases, the dermal sinus becomes infected, which leads to the development of intra, extramedullary abscesses, meningitis, and as a result, the appearance of a severe neurological deficit. The development of neurological symptoms is also associated with the development of the fixed spinal cord syndrome. Dermal sinus is also associated with Diastematomyelia, Teratoma, Myelomeningocele.
In 60% of cases, the dermal sinus becomes infected, which leads to the development of intra, extramedullary abscesses, meningitis, and as a result, the appearance of a severe neurological deficit. The development of neurological symptoms is also associated with the development of the fixed spinal cord syndrome. Dermal sinus is also associated with Diastematomyelia, Teratoma, Myelomeningocele. Open form (Spina Bifida aperta) spina bifida, is the least common of all types of congenital malformations of Spina Bifida (incidence is from 1 to 2 per 1,000 newborns in the world) and is a more severe degree of spinal defect, combined with dysplasia spinal cord, membranes and roots and is called spinal hernia.
Depending on the severity of spina bifida and the degree of involvement in the pathological process (the content of the hernial sac) of nerve structures, the following types of spinal hernias are divided:
- Meningocele: only the meninges protrude;
- Myelocele: only tissue of the spinal cord protrudes;
- Meningomyelocele: Tissues of the meninges and spinal cord protrude.
Thus, the protruding hernial sac in this variety of Spina Bifida as a spinal hernia may contain the meninges (Meningocele), the spinal cord (Myelocele), or both (Myelomeningocele).
Depending on the content of the hernial sac, it is a defect in any part of the back with a hernial protrusion. It occurs in various parts of the spine, more often in the lower thoracic and lumbosacral. It is combined with other developmental anomalies.
Spinal hernia is a severe malformation characterized by congenital non-closure of the posterior wall of the spinal canal with simultaneous hernial protrusion of the dura mater covered with skin and containing cerebrospinal fluid or the spinal cord and/or its roots. The complex of anatomical and functional disorders that occur with a spinal hernia is conditionally united by the term "Myelodysplasia".
Meningocele is a moderate defect in which only the spinal membranes bulge through a defect in the spine, forming a hernial sac or cyst filled with cerebral fluid (liquor), without elements of the nervous tissue (spinal cord and roots).
 This is the most benign form of spinal hernias, since the spinal cord is formed correctly in most cases. Meningocele is usually located in the lumbosacral spine, sometimes reach large sizes, have a short stalk. The spinal cord and roots are usually not changed and occupy their normal physiological position, which is typical for the cervicothoracic localization. In the lumbosacral location of the defect, the hernial sac may include the final thread, single loops of functionally intact roots, often fixed to the walls of the dome of the hernial sac and stretching the lower parts of the spinal cord. Lumbosacral Meningoceles are covered with skin and are not associated with paralysis of the lower extremities, as well as paralysis of the bladder and rectum and Hydrocephalus.
This is the most benign form of spinal hernias, since the spinal cord is formed correctly in most cases. Meningocele is usually located in the lumbosacral spine, sometimes reach large sizes, have a short stalk. The spinal cord and roots are usually not changed and occupy their normal physiological position, which is typical for the cervicothoracic localization. In the lumbosacral location of the defect, the hernial sac may include the final thread, single loops of functionally intact roots, often fixed to the walls of the dome of the hernial sac and stretching the lower parts of the spinal cord. Lumbosacral Meningoceles are covered with skin and are not associated with paralysis of the lower extremities, as well as paralysis of the bladder and rectum and Hydrocephalus. With meningocele, the severity of the patient's condition is less pronounced than in the case of myelomeningocele, but minor bladder and bowel dysfunctions are also possible, with clinical symptoms. This condition may require surgery, but it is not necessarily urgent in newborns, however, surgical treatment of this disease is still recommended for cosmetic and neonatal care reasons.
* Causes of meningocele include teratoma and Currarino syndrome. Anterior sacral meningocele is the most common presacral mass in patients with Currarino syndrome, occurring in 60% of cases. Its presence can significantly affect the surgical treatment of these patients. Other potential presacral masses include presacral teratoma and intestinal cyst.
Myelocele is a rarer defect in which a hernial sac prolapses through a defect in the spine with a partially covered membranes, spinal cord and cerebrospinal fluid (only tissues of the spinal cord protrude). This is a spinal hernia in which the hernial sac contains a partially sheathed altered spinal cord and cerebrospinal fluid. The size of the myelocele can be different: a small protrusion or an extensive defect containing spinal cord tissue. The clinical picture of this type of spinal hernia consists of neurological symptoms and local manifestations in a certain place on the back. Myelocele is associated with paralysis or paresis of the lower extremities.
 Urinary and fecal incontinence, as well as in 80% of cases with hydrocephalus. With sacral Myelocele, paresis of the lower extremities occurs in a smaller number of cases. Frequent accompanying anomalies are deformity of the legs, contractures of the lower extremities, kyphosis, anomalies in the development of the genitourinary system. Myelocele requires urgent surgical treatment, which should be carried out in the first hours after birth, because this is most likely to prevent Meningitis from ascending infection. In addition, the functioning nerve elements are preserved by repositioning the remaining parts of the nervous tissue and covering them with a dural sac, which favorably responds to maintaining mobility.
Urinary and fecal incontinence, as well as in 80% of cases with hydrocephalus. With sacral Myelocele, paresis of the lower extremities occurs in a smaller number of cases. Frequent accompanying anomalies are deformity of the legs, contractures of the lower extremities, kyphosis, anomalies in the development of the genitourinary system. Myelocele requires urgent surgical treatment, which should be carried out in the first hours after birth, because this is most likely to prevent Meningitis from ascending infection. In addition, the functioning nerve elements are preserved by repositioning the remaining parts of the nervous tissue and covering them with a dural sac, which favorably responds to maintaining mobility. Myelomeningocele (MMC), Spina Bifida cystica , Spinal hernia is the most severe type of spina bifida in Spina Bifida, which is fixed in 75% of cases and can have the most serious consequences. This malformation consists in the fact that the spinal cord, nerves, spinal cord membranes and cerebrospinal fluid are pushed out through a defect in the spine and incomplete closure of the spinal canal.
 In severe cases, there is a splitting not only of the spine, but also of the spinal cord. The bone defect captures from 3 to 6-8 vertebrae. On the back of the child, more often in the lumbar region, there is a hernial sac that is not covered with muscles and skin, its wall can be the posterior surface of the spinal cord and is often covered with thinned epidermis (thinned skin, film). The meningeal membranes that cover the spinal cord also protrude through the opening, forming a sac that encloses the spinal cord, spinal roots, and CSF. The protruding part of the spinal cord, membranes and roots can often be damaged or not developed properly. The affected area looks rough, uneven and red.
In severe cases, there is a splitting not only of the spine, but also of the spinal cord. The bone defect captures from 3 to 6-8 vertebrae. On the back of the child, more often in the lumbar region, there is a hernial sac that is not covered with muscles and skin, its wall can be the posterior surface of the spinal cord and is often covered with thinned epidermis (thinned skin, film). The meningeal membranes that cover the spinal cord also protrude through the opening, forming a sac that encloses the spinal cord, spinal roots, and CSF. The protruding part of the spinal cord, membranes and roots can often be damaged or not developed properly. The affected area looks rough, uneven and red. Often this leads to rupture of the hernial sac with the outflow of cerebrospinal fluid (liquorrhea).
The severity of the neurological deficit is determined by the level of location, size, prevalence of the anomaly, the degree of damage to the spinal cord and nerves, the number of roots involved in the pathological process, which can blindly end in the wall of the hernial sac.
Depending on this, clinical symptoms may range from mild weakness and sensory disturbances in the lower extremities below the level of damage and pelvic disorders to gross paresis and deformities of the feet and total urinary and fecal incontinence.
Myelomeningocele in 80% of cases is accompanied not only by paralysis of the legs, but also by dysfunction of the bladder and intestines.
The higher the defect is located in the spine, the more functions it can potentially affect.
Paralysis at the level of Th22 is characterized by a complete absence of movements in the legs, as the level of spinal hernia formation decreases, intact muscle groups appear corresponding to the formed innervation dermatomes (dermatome is a skin area equipped with sensory neurons that arise from the ganglion of the spinal nerve), which certainly affects the degree of disturbance in the sensitive area and control of the function of the pelvic organs.
The location of spinal hernias along the length of the spinal column in 90% of cases is limited to the lumbosacral region.
Thoracic and cervical localization of hernias are relatively rare.
The success of high social adaptation is probably higher in patients with a low spinal hernia and lower in children with a spinal hernia at the level of the thoracic spine.
Typical for all types and forms of spinal dysraphia is their posterior location with a defect in the posterior semicircle of the spinal canal. Extremely rarely (less than 1% of cases), non-closure is formed on the anterior-lateral surface of the canal, and anterior spinal hernias occur.
This CNS malformation occurs in 60-85% of patients with hydrocephalus and Arnold-Chiari malformation type II. Hydrocephalus occurs because the cerebrospinal fluid (CSF) that protects the brain and spinal cord cannot circulate properly, causing it to accumulate, causing pressure and swelling. Left untreated, this can lead to brain damage.
In 15% of cases, spinal hernia is combined with severe kyphotic deformity of the spine.
The appearance of new symptoms (pain syndrome, spinal deformity) or an increase in existing symptoms may be due to fixation of the spinal cord and spinal roots at the level of repair of spinal hernia.
Rhachischisis is a gross developmental anomaly characterized by non-closure of the skin and spinal canal, absence of neurulation (formation of the neural plate and its closure into the neural tube) of the placode. This form is an example of a severe disorder of spinal cord neurulation (the spinal cord has not closed into a tube and gapes in a split spinal canal). With this pathology, there is a complete splitting of the soft tissues, spine, membranes and spinal cord. The spinal cord, not closed into a tube, lies in the form of a velvety mass of red color, consists of dilated vessels and elements of brain tissue. Posterior rachischisis is often combined with anterior (when not only the arches, but also the bodies of the vertebrae are split) and severe deformities of the brain and other organs. Most often, rachischisis is found in the lumbar region.
The clinical picture of rachischisis is represented by gross neurological symptoms in the form of paraplegia, anesthesia, dysfunction of the pelvic organs and mental retardation.
Tethered spinal cord (“Tethered spinal cord”) the name of the pathology is often denoted by an abbreviation consisting of the first letters of the term - FSM, as well as synonyms: stiff terminal or terminal thread syndrome, tethering syndrome, which means immobility, constancy.
This condition is manifested by an abnormally low location of the cone of the spinal cord (below the L2 vertebra) and is most often associated with a short, inelastic and thick terminal filament (“Tight filum terminale”), which, as it were, stretches the spinal cord and also causes circulatory disorders in it which leads to the development of neurological and functional disorders.
Spinal Lipoma, Dermoid and Diastematomyelia (all of which are an “associated” Spina Bifida occulta complex) and Spinal Hernias can lead to a similar pathological condition.
There is also a concept as a diagnosis – “Tethered spinal cord syndrome” (SFCS) is an adaptation of the English term “the tethered spinal cord syndrome”.
The use of the word “tether” in the original name of the syndrome, meaning “tether” in literal translation, most accurately reflects the essence of the pathological process, which implies the tension of the terminal thread. It is the stretching of the spinal cord, which develops as a result of attachment and limitation of its mobility - fixation, that leads to a negative impact and the development of clinical manifestations of SFCS. In 85% of cases, tethering syndrome is observed in the lumbosacral region.
Fixed spinal cord syndrome (SFCS) is a complex of trophic, sensory and functional disorders and is found in a progressive stage with severe symptoms associated with neurological (weakness, pain in the legs, gait disturbance, development of flaccid paralysis, paresis of the lower extremities), orthopedic violations (asymmetry of the legs, musculoskeletal deformities, deformity of the feet, deformity of the spine) and dysfunction of the pelvic organs (incontinence or retention of urine and feces, urinary infections, etc.