Nursing interventions for labor and delivery
Nursing Care for a Woman in Labor: Obstetric Nursing Guide
Updated on
By Marianne Belleza, R.N.
ADVERTISEMENTS
The big day has finally arrived! Everyone must be in a state of panic and happiness, but the pregnant woman, who is the center of everything, must stay focused so the entire labor process would go by smoothly and safely.
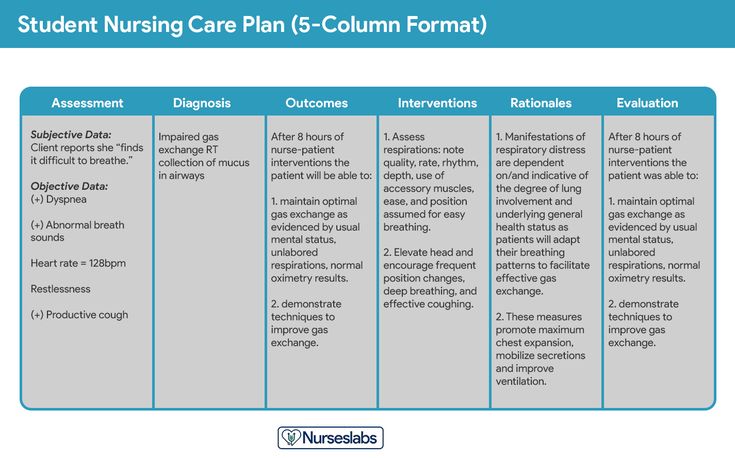
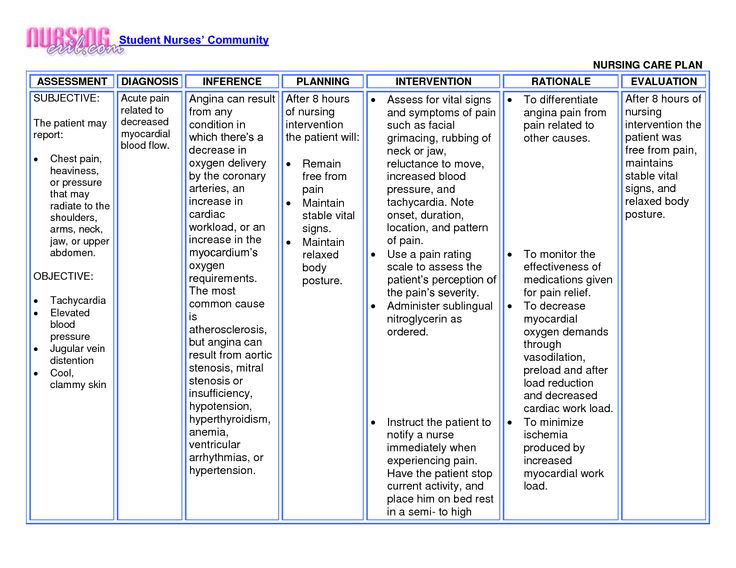
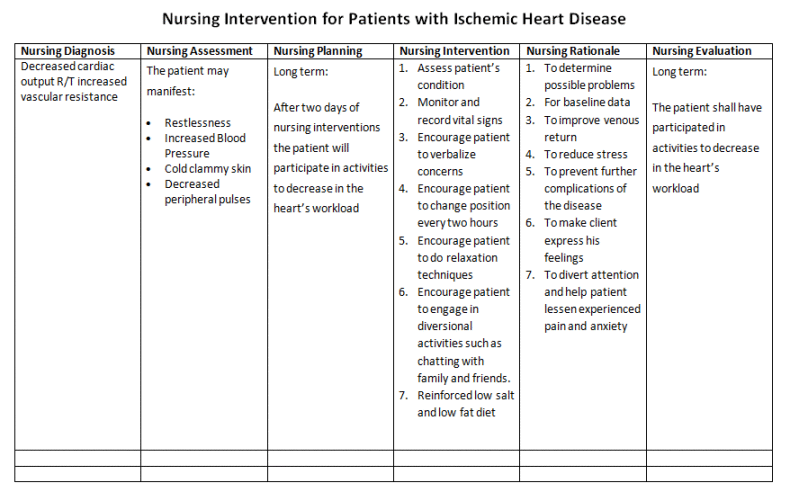
AssessmentThe key to a successful individualized care plan is the precise assessment and accurate obtaining of data. The woman would be placed under observation during labor to monitor her progress and ensure a safe delivery for her and the child.
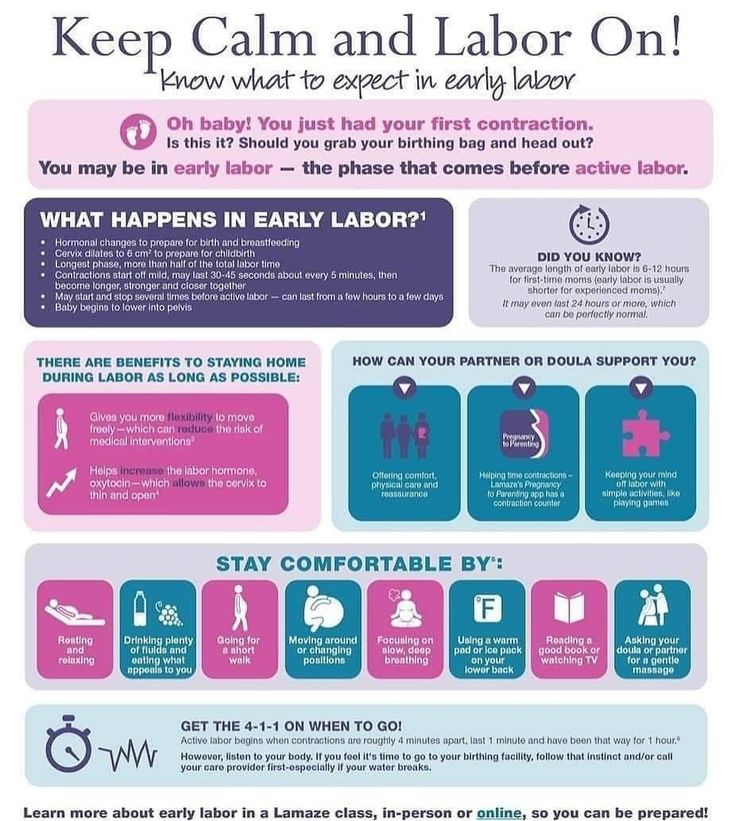
- Assess for the signs of true labor. The signs of true labor are contractions that begin irregularly but progresses regularly and predictably, the pain is felt first at the lower back and circles towards the abdomen, continues to progress no matter what the woman’s activity level is, increases in duration, frequency, and intensity and cervical dilation is already present.
- Assess for the appearance of show, which is blood mixed with mucus and would be present once the operculum or mucus plug is expelled.
- Assess for the rupture of membranes. This is the scanty or sudden gush of clear fluid from the vagina.
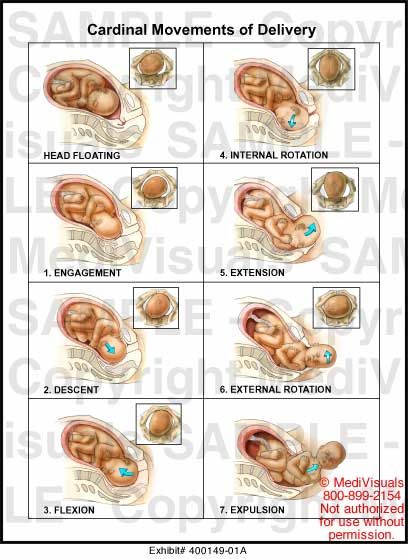
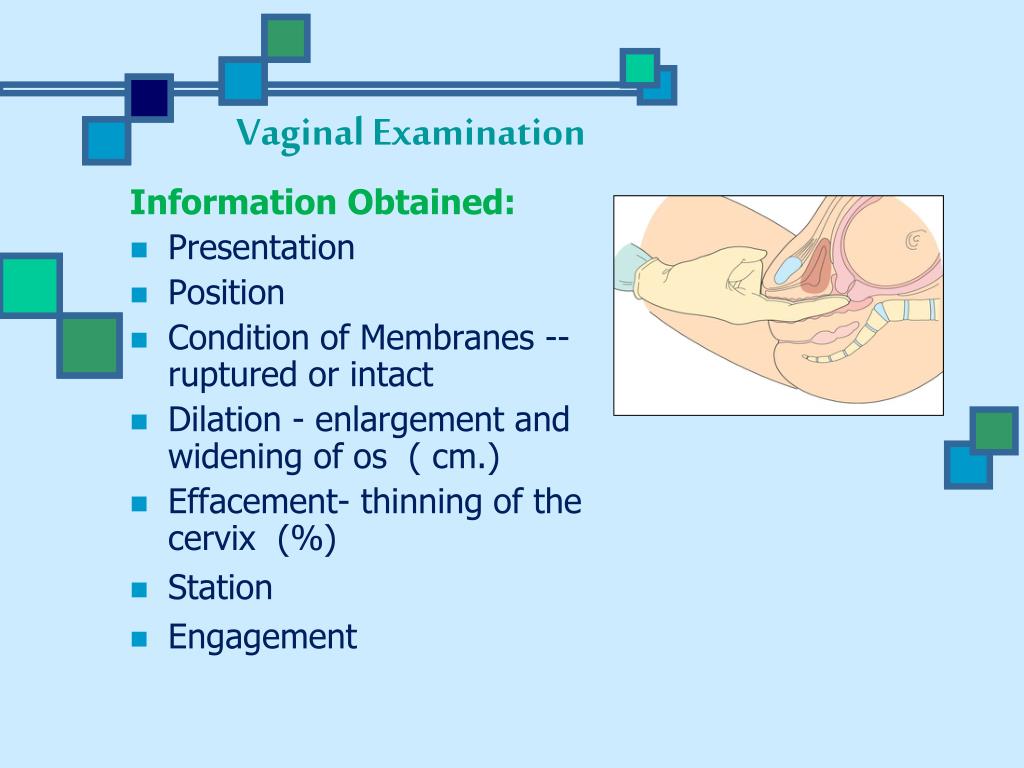
- Assess for the engagement of the fetal head. Engagement refers to the settling of the presenting part into the pelvis at the level of the ischial spines.
- Assess for the station. Station is the relationship of the presenting part to the level of the ischial spines.
- Assess for the effacement and dilatation of the cervix. Effacement is the shortening and thinning of the cervical canal. In cervical dilatation, the enlargement or widening of the cervical canal is assessed.
Main topic: Stages of Labor
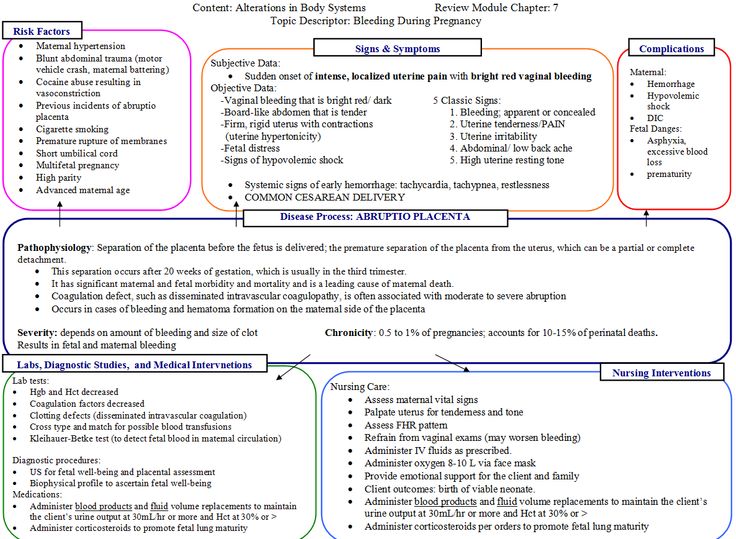
During labor, a pregnant woman might encounter difficulties that could affect her progress. These conditions should be prevented to ensure a smooth labor period and eventually, a safe delivery.
These conditions should be prevented to ensure a smooth labor period and eventually, a safe delivery.
First stage of labor
This stage of labor is divided into three phases.
- The latent phase starts during the onset of true labor contractions until cervical dilatation.
- The active phase occurs when cervical dilatation is at 4 to 7 cm and contractions last from 40 to 60 seconds with 3 to 5 minutes interval.
- The transition phase occurs when contractions reach their peak with intervals of 2 to 3 minutes and dilatation of 8 to 10 cm.
Second stage of labor
- This stage starts at full cervical dilatation until the birth of the infant.
- The woman may experience an uncontrollable urge to push and bear down with every contraction.
- Crowning or the appearance of the fetal head on the vaginal opening occurs.
Third stage of labor
- The third stage begins with the birth of the infant until the delivery of the placenta.
- The signs of placental expulsion are lengthening of the umbilical cord, sudden gush of vaginal blood, changes in the shape of the uterus and its firm contraction, and the appearance of the placenta at the vaginal opening.
With all the data gathered during assessment and through an accurate diagnosis, a care plan for the woman in labor would be made to aid her through her progress.
ADVERTISEMENTS
Care of a woman in the first stage of labor
- Labor should be allowed to start naturally, not artificially induced.
- The woman must also be allowed to move freely throughout the labor. Artificial interventions should also be prohibited.
- Allow the woman to assume a non-supine position for delivery.
- Upon delivery of the newborn, mother and child should be given unlimited opportunity for breastfeeding and bonding.
Care of a woman in the second stage of labor
- During the second stage of labor, the place of delivery of the woman must be prepared.
- The position of birth wherein the woman is most comfortable must also be determined at this stage.
- Another important part is the promotion of second stage effective pushing.
- Perineal cleaning is also an integral part of the second stage.
Care of the woman in the third stage of labor
- Placental delivery should be given focus at this stage. Once the placenta is delivered, oxytocin should be administered intramuscularly to promote uterine contractions.
- If there is episiotomy performed, perineal repair should be integrated into the care plan.
Some interventions are implemented to give comfort and safety for the mother during and after the labor period. These are essential in promoting the strength that the mother would need during delivery.
- Encourage the client to void every 2 hours.
- Observe and review the client’s breathing techniques.
- Inform the client if c interventions are necessary.
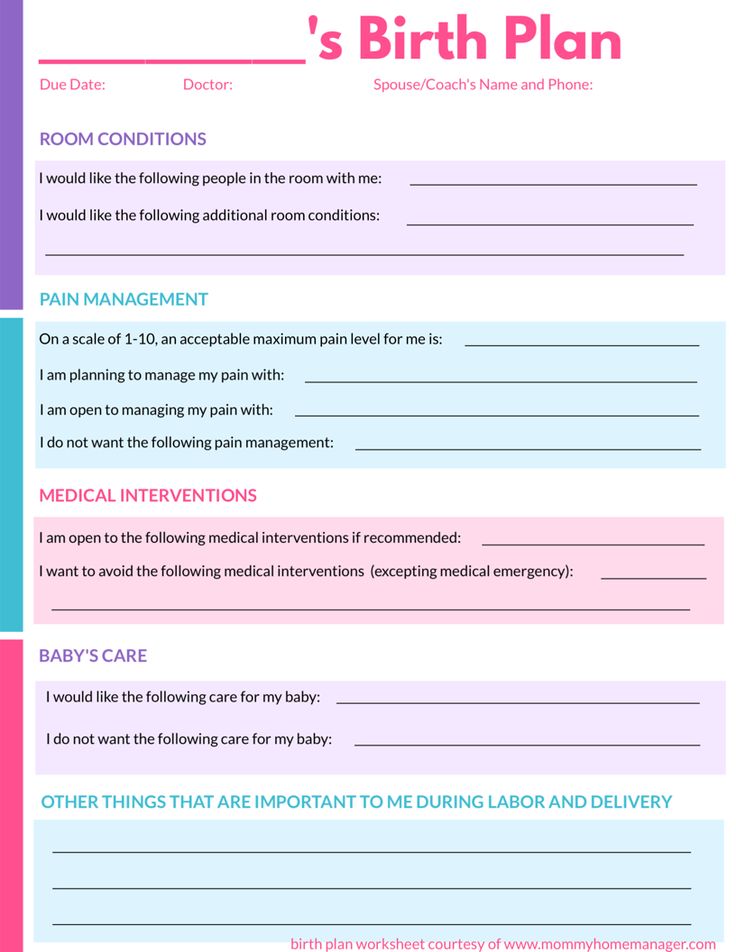
- Create a birth plan with the client so she could integrate her preferences in the care plan.
- Provide ice chips, hard candies, or fluids to relieve dry mouth.
- Provide a comfortable environment to aid in the effective coping management of the client.
- Allow the client to walk and move around freely during labor.
- Do not intervene with the client during a contraction to avoid disturbing her focus on her technique.
After the labor has passed, delivery would commence immediately. And when the labor period for the woman has gone smoothly, a great chance for a safe and healthy delivery is within reach.
- Client should exhibit no signs of bladder distention and have the ability to void every 2 hours.
- Client has a good to tolerable level of pain.
- Client can express her preferences during labor.
- Client has the ability to understand the usual process of labor.
- Client reports that her environment is comfortable and secure.
- Client would be able to verbalize her feelings about her experiences during her labor period.
- Cervical ripening must be complete during early labor.
- If there is no cervical ripening, there would be no dilatation and coordination of uterine contractions.
- To determine whether the cervix is ripe, Bishop established criteria for scoring the cervix.
- If the woman’s score is 8 or greater, the cervix is already ready or birth and would respond to induction.
- One of the ways to ripen the cervix is known as “stripping the membranes”, or separating the membranes from the lower uterine segment manually using a gloved finger in the cervix.
- Complications that may arise from this procedure include bleeding due to undetected low-lying placenta, inadvertent rupture of membranes, and infection when the membranes rupture.
- Another method that is also considered is the use of hygroscopic suppositories or suppositories of seaweed that swell upon contact with cervical secretions.
.png)
- These suppositories gradually and gently urge dilatation.
- They are held in place by gauze sponges saturated with povidone iodine or an antifungal cream.
- The number of sponges and dilators should be documented accordingly to avoid leaving behind one of them inside the cervix.
- A more common method of speeding cervical ripening is the application of a prostaglandin gel to the interior surface of the cervix by a catheter or suppository, or to the external surface by applying it to a diaphragm and then replacing it against the cervix.
- Additional doses may be applied every six hours, but two or three doses are usually enough to achieve ripening.
- Instruct the woman to remain in a side lying position to avoid leakage of the medication.
- Continuously monitor the FHR at least every 30 minutes after each complication.
- Side effects of this method include diarrhea, fever, hypertension, and vomiting.
- Oxytocin administration may also be started, but that would be 6 to 12 hours after the last prostaglandin dose.
- Use prostaglandin with caution in women with asthma, renal or cardiovascular disease, or glaucoma.
- Women who underwent cesarean birth in the past are contraindicated with prostaglandin method.
- Administration of oxytocin can initiate contractions in a uterus in pregnancy term.
- Oxytocin is administered intravenously so that when there is hyperstimulation, then it could be quickly discontinued.
- The effects happen immediately because the half-life of oxytocin is approximately 3 minutes.
- Oxytocin is usually mixed with Ringer’s lactate, 10 units of oxytocin in 1000 mL of Ringer’s lactate.
- The infusion could also be administered piggyback to a maintenance IV solution, so that if the infusion would be discontinued, the main IV line could still be maintained.
- The oxytocin solution must always be attached to the port nearest to the woman so that little solution remains in the tubing if it is discontinued.
- Use of an infusion pump is recommended to regulate the infusion rate and make sure that the rate would not change even if the woman moves.
- Do not increase the rate without any further instructions because it can cause tetanic contractions.
- Artificial rupture of membranes may be done when cervical dilatation reaches 4 cm to further induce labor.
- Be aware of peripheral vessel dilatation, a side effect of oxytocin administration, which can cause hypotension.
- Assess the woman’s pulse and blood pressure every 15 minutes to be certain of a safe induction.
- Monitor uterine contractions and FHR accordingly.
- Contractions should occur no more often than every 2 minutes, should not be longer than 70 seconds, and not stronger than 50 mmHg.
- Stop the IV infusion if the contractions become more frequent or longer in duration than the safe limits or if there are signs of fetal distress.
- Excessive stimulation of the uterus by oxytocin may lead to tonic uterine contractions with fetal death or rupture of the uterus.

- In the event that hyperstimulation is not stopped even if the infusion has been discontinued, a beta-adrenergic receptor drug or magnesium sulfate may be prescribed to decrease myometrial activity.
- A complication of oxytocin infusion is water intoxication because oxytocin has an antidiuretic effect that results in decreased urine flow.
- Symptoms of water intoxication are headache and vomiting.
- Water intoxication in its most severe form can cause seizures, coma, and even death because of the large shift in interstitial tissue fluid.
- Monitor the intake and output appropriately and assess urine specific gravity to detect fluid retention.
- Limit the amount of IV fluid to 150 mL/hr by making sure that the main line is infusing at a rate not greater than 2.5 mL/min.
- Induced labor tends to have shorter first stage than the average unassisted labor.
- Assure the woman that uterine contractions in an induced labor are basically normal so she can use her breathing techniques effectively.

- However, hyperbilirubinemia and jaundice in a newborn are possible because of induction of labor with oxytocin.
- The infant should be observed closely for these conditions during the first few days of life.
- If labor contractions begin spontaneously but become weak, irregular, and ineffective, augmentation of labor is required.
- Precautions for oxytocin administration are the same as for primary induction of labor.
- The uterus may respond effectively to oxytocin used as augmentation.
- The drug should be increased in small increments only and fetal heart sounds should be monitored during the procedure.
The labor process is the gateway towards a safe delivery. Once the woman has undergone labor, it is imminent that delivery would follow suit. It is important for the woman to have a smooth labor process for this is where she would be gathering her strength to deliver her precious bundle of joy.
ADVERTISEMENTS
Categories Maternal and Child Health Nursing, Notes Tags cervix, crowning, dilatation, effacement, engagement, labor, show, station, Vagina
Marianne Belleza, R.N.
Marianne is a staff nurse during the day and a Nurseslabs writer at night. She is a registered nurse since 2015 and is currently working in a regional tertiary hospital and is finishing her Master's in Nursing this June. As an outpatient department nurse, she is a seasoned nurse in providing health teachings to her patients making her also an excellent study guide writer for student nurses. Marianne is also a mom of a toddler going through the terrible twos and her free time is spent on reading books!
© 2023 Nurseslabs | Ut in Omnibus Glorificetur Deus!
Nursing Care Tips for Various Stages
ADVERTISEMENTS
Nursing care for pregnant women in labor proves to be a challenging task because it requires nurses to be fast in their assessment without sacrificing the quality and accuracy of rendered nursing care. Now, why should care of women in various stages of labor be taken seriously? In 2000, the United Nations Millennium Summit included the improvement of maternal health as one of the Millennium Development Goals (MDGs) to be adapted by the international community composed of over 42 countries. Promoting the health of women in labor is one active way of reducing maternal mortality and ensuring universal access to reproductive health services.
Now, why should care of women in various stages of labor be taken seriously? In 2000, the United Nations Millennium Summit included the improvement of maternal health as one of the Millennium Development Goals (MDGs) to be adapted by the international community composed of over 42 countries. Promoting the health of women in labor is one active way of reducing maternal mortality and ensuring universal access to reproductive health services.
The progression of labor is traditionally divided into three phases, and each phase deals with different concerns and considerations. Having gained mastery of this, nurses are able to implement nursing interventions to safeguard the welfare of both the mother and the baby.
Establishing Therapeutic RelationshipTo gain patient and family’s cooperation and trust, it is important that the nurse should be able to establish a therapeutic relationship with them. The nurse should introduce himself and make them feel welcome.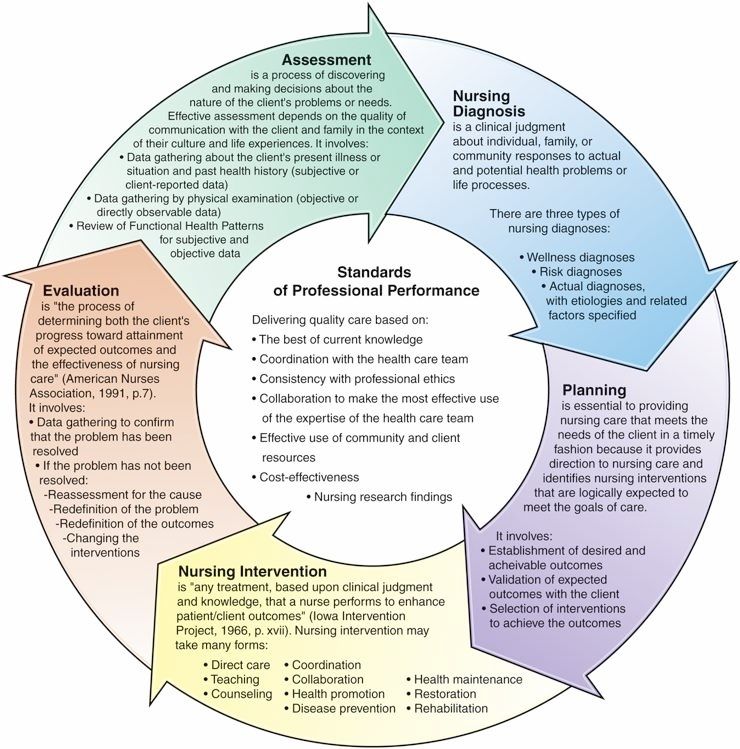 At this point, they are all anxious and it is best for the nurse to convey his message gently and confidently. Expectations of the family about birth should be determined and it is also the best time to ascertain cultural values.
At this point, they are all anxious and it is best for the nurse to convey his message gently and confidently. Expectations of the family about birth should be determined and it is also the best time to ascertain cultural values.
When a patient arrives at the labor floor, pertinent information about the pregnant woman’s health history is taken during admission. These include personal data (e.g. blood type, allergies, etc.), previous illness, pregnancy complications, preferences for labor and delivery, and childbirth preparations. Standard obstetric, medical, and social history taking is also done.
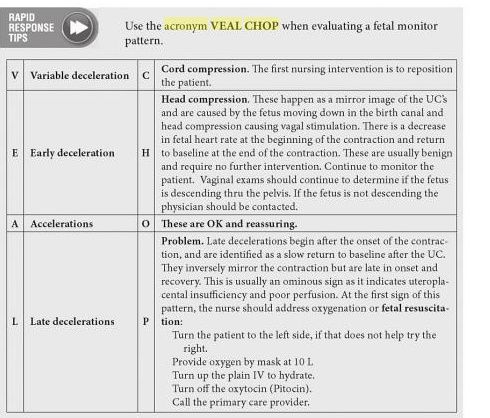
In addition, the nurse assesses the following: vital signs, physical exam, contraction pattern (frequency, interval, duration, and intensity), intactness of membranes through vaginal exam, and fetal well-being through fetal heart rate, characteristic of amniotic fluid, and contractions. The nurse performs Leopold’s maneuver to determine fetal presenting part, point of maximum impulse, fetal descent and engagement.
Admission into labor room is only done when the patient is in active labor.
Stages of LaborThe progress of cervical effacement, cervical dilatation, and descent of fetal presenting part dictate stages of labor. Here are the stages of labor and significant events that mark their beginning and end:
| Stages of Labor | Start | End | Duration | |
|---|---|---|---|---|
| Nullipara | Multipara | |||
| First Stage | True labor contractions | Full cervical dilatation | 10-12 hr but 6-20 hrs is the normal limit | 6-8 hrs but 2-12 hrs is the normal limit |
| Latent phase | Onset of regularly perceived uterine contractions (mild contractions lasting 20-40 sec) | 3 cm cervical dilatation | 6 hrs | 4.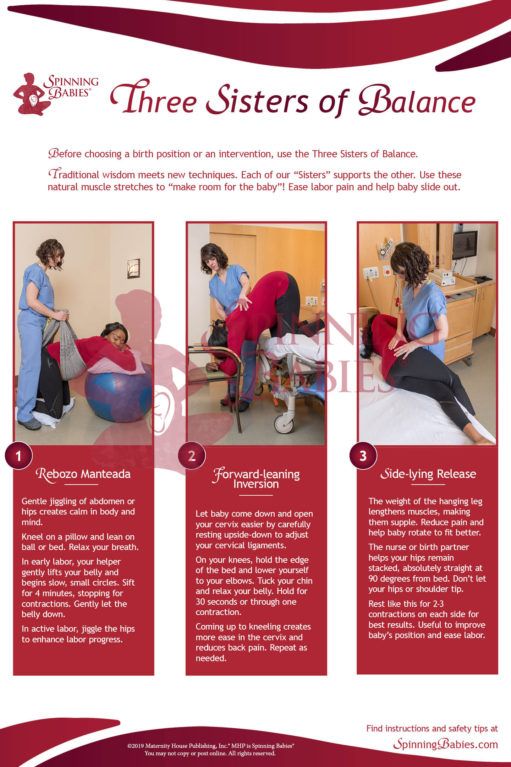 5 hrs 5 hrs |
| Active phase | Stronger uterine contractions lasting 40-60secs | 7 cm cervical dilatation | 3 hrs | 2 hrs |
| Transitional phase | Uterine contractions reaching their peak, occurring every 2-3 minutes for 60-90 s | 10 cm cervical dilatation | 3 hrs | 1.5-2 hrs |
| Second Stage | Full cervical dilatation | Infant birth | <2 hrs | 0.5-1 hrs |
| 3 hrs with epidurals | 2 hrs with epidurals | |||
| Third Stage | Infant birth | Placental delivery | Maximum of 30 min. | |
As mentioned above, the first stage of labor is divided into three sub-phases, namely: latent, active, and transitional phases.
Latent PhaseLatent (Preparatory) Phase starts from the onset of true labor contractions to 3 cm cervical dilatation. Here are nursing responsibilities during this phase:
Here are nursing responsibilities during this phase:
- Assess patient’s psychological readiness. Provide continuous maternal support (compared to usual care).
- Measure duration of latent phase. For nulliparas, it should not be more than 6 hours. On the other hand, for multiparas, it should be within 4.5 hours. Determine if patient received anesthesia because it can prolong latent phase. One of the most common cause of prolonged latent phase is cephalopelvic disproportion (CPD) and it requires cesarean birth.
- Allow patient to be continually active. Upright maternal positions are recommended for women on the first stage of labor. Patients without pregnancy complications can still walk around and make necessary birth preparations.
- Conduct interviews and filling in of forms (e.g. birth certificate) at this phase while the patient experiences minimal discomfort and has control over contraction pains.
- Conduct health teaching on breastfeeding, newborn care, and effective bearing down because during this time, patient’s anxiety is controlled and she is able to focus on nurse’s instructions.

- Educate patient on different relaxation techniques. As early as this phase, encourage patient to begin alternative therapy of pain relief.
- Ensure that the total number of internal examinations the woman receives in the entire course of labor is limited to 5 only.
- Ensure that birthing companion of choice is present all throughout the course of labor.
Active Phase starts from 4 cm cervical dilatation to 7 cm cervical dilatation. During this phase, contraction intensity is stronger, interval shortens, and duration lengthens. This is where true discomfort is first felt by the patient so she is dependent and her focus is on herself. Here are nursing responsibilities in this phase:
- Inform patient on the progress of her labor to lessen her anxiety and obtain her trust and cooperation.
- Start monitoring progress of labor with the use of WHO partograph, 2-hour action line.
- Encourage patient to be continually active to maximize the effect of uterine contractions. Upright maternal positions are recommended if tolerated.
- Assist patient in assuming her position of comfort. For those who can’t stay upright, left-side lying is recommended to avoid disruption in fetal oxygenation.
- Monitor maternal vital signs and fetal heart rate every 2 hours, or depending on the doctor’s order.
- Anticipate patient needs (e.g. sponging face with cool cloth, keeping bed clean and dry, providing ice chips or lip balm) to promote comfort.
- Determine when patient last voided because a full bladder can hinder fast labor progress.
- Institute non-pharmacological pain measures (e.g. breathing exercises, distraction method, imagery, music therapy, etc.)
Transition Phase starts from 8 cm cervical dilatation to 10 cm (full) cervical dilatation and full cervical effacement. During this time, patient may be exhausted and withdrawn or aggressive and restless. Patient’s urge to push is noticeable. Here are nursing responsibilities in this phase:
During this time, patient may be exhausted and withdrawn or aggressive and restless. Patient’s urge to push is noticeable. Here are nursing responsibilities in this phase:
- Inform patient on progress of her labor.
- Assist patient with pant-blow breathing.
- Monitor maternal vital signs and fetal heart rate every 30 minutes -1 hour, or depending on the doctor’s order. Contraction monitoring is also continued.
- When perineal bulging is noticeable, prepare for delivery. Check room temperature (25-280C and free of air drafts). The nurse should also notify staff and prepare necessary supplies and equipment, including resuscitation machine. Lastly, perform handwashing and double gloving.
WHO do not recommend the following nursing interventions during labor because they have low quality of evidence:
ADVERTISEMENTS
- Routine perineal shaving
- Routine use of enema
- Admission cardiotocography (CTG) for low-risk women
- Vaginal douching
- Routine amniotomy for patients in spontaneous labor
- Massage and reflexology
Second Stage of Labor starts when cervical dilatation reaches 10 cm and ends when the baby is delivered. At this stage, the patient feels an uncontrollable urge to push. The patient may also experience temporary nausea together with increased restlessness and shaking of extremities. The nurse at this stage must coach quality pushing and support delivery.
At this stage, the patient feels an uncontrollable urge to push. The patient may also experience temporary nausea together with increased restlessness and shaking of extremities. The nurse at this stage must coach quality pushing and support delivery.
Here are nursing care tips for this stage:
- Instruct patient on quality pushing. The abdominal muscles must aid the involuntary uterine contractions to deliver the baby out.
- Provide a quiet environment for the patient to concentrate on bearing down.
- Provide positive feedback as the patient pushes.
- Repeat doctor’s instructions. At this phase, the patient barely hears the conversation around the room because all her energy and thoughts are being directed toward giving birth.
- Take note of the time of delivery and proceed to initiate essential newborn care. Delayed cord clamping is recommended.
- Assist in restrictive episiotomy for patients who had vaginal births.
WHO do not recommend the following interventions during delivery because they provide low quality of evidence:
- Perineal massage
- Use of fundal pressure
Third Stage of Labor or the placental stage starts from birth of infant to delivery of placenta. It is divided into two separate phases: placental separation and placental expulsion. Five minutes after delivery of baby, the uterus begins to contract again, and placenta starts to separate from the contracting wall. Blood loss of 300-500 mL occurs as a normal consequence of placental separation. Placenta sinks to the lower uterine segment or upper vagina. The placenta is then expelled using gentle traction on the cord.
It is divided into two separate phases: placental separation and placental expulsion. Five minutes after delivery of baby, the uterus begins to contract again, and placenta starts to separate from the contracting wall. Blood loss of 300-500 mL occurs as a normal consequence of placental separation. Placenta sinks to the lower uterine segment or upper vagina. The placenta is then expelled using gentle traction on the cord.
Here are the signs of placental separation:
- Lengthening of umbilical cord
- Sudden gush of vaginal blood
- Change in the shape of uterus (globular in shape)
- Firm uterine contractions
- Appearance of placenta in vaginal opening
At this stage, here are the nursing care tips:
- Coach in relaxation for delivery of placenta.
- Congratulate on delivery of baby.
- Encourage skin-to-skin contact to facilitate bonding and early breastfeeding.
- Ask patient whether placenta is important to them before it is destroyed.
 For those who want to take it home, ensure that they understand and follow standard infection precautions and hospital policy.
For those who want to take it home, ensure that they understand and follow standard infection precautions and hospital policy. - Administer prophylactic oxytocin as ordered.
- Utilize controlled cord traction technique for placental expulsion.
- Utilize absorbable synthetic suture materials (over chromic catgut) for primary repair of episiotomy or perineal lacerations.
For immediate postpartum, the nurse checks the vital signs and monitors for excessive bleeding. The first four hours after birth is sometimes referred to as the fourth stage of labor because this is the most critical period for the mother. The nurse is set to perform nursing interventions that would prevent the patient from infection and hemorrhage. Also, they are being reminded of the importance of breastfeeding, ambulation, and newborn care.
Here are WHO recommendations for immediate postpartum:
- Early (<6 hours) resumption of feeding for patients who have vaginal birth
- Prophylactic antibiotics for women who sustained third to fourth degree of perineal tear during delivery
- In healthy women who delivered vaginally to term infants, early postpartum discharge is recommended.
On the other hand, here are interventions not recommended during immediate postpartum:
- Routine use of ice packs
- Oral methylergometrine for patients who delivered vaginally
Nursing care for women in labor is a routine that takes a while to fall into. After all, it is overwhelming for beginner nurses to do their responsibilities in front of a woman writhing in pain. However, the opportunity to protect women and the privilege of being a part of their positive pregnancy experience is rewarding. Read and share this to your nurse friends because women’s and children’s lives deserve only the best care.
References:
- Clinical Practice Guidelines on Intrapartum and Immediate Postpartum Care 2012 by Department of Health and Philippine Obstetrical and Gynecological Society. Retrieved from: https://www.wpro.who.int/philippines/publications/clinical_practical_guidelines_einc.pdf
- Callahan, T.
 (2013). Blueprints Obstetrics and Gynecology. (6th ed.). Baltimore, MD: Lippincott William & Wilkins.
(2013). Blueprints Obstetrics and Gynecology. (6th ed.). Baltimore, MD: Lippincott William & Wilkins. - Pillitteri, A. (2010). Maternal & Child Health Nursing: Care of the Childbearing and Childrearing Family (6th ed.). PA: Lippincott William & Wilkins.
ADVERTISEMENTS
Iris Dawn Tabangcora, RN
Iris Dawn is a nurse writer in her 20s who is on the constant lookout for latest stories about Science. Her interests include Research and Medical-Surgical Nursing. She is currently furthering her studies and is seriously considering being a student as her profession. Life is spoiling her with spaghetti, acoustic playlists, libraries, and the beach.
Sitemap
State autonomous professional
educational institution
Republic of Bashkortostan
"Salavat Medical College"
453261 Republic of Bashkortostan
Salavat, st. Furmanova, 4
Phone/fax: (3476)-38-78-83
e-mail: slv.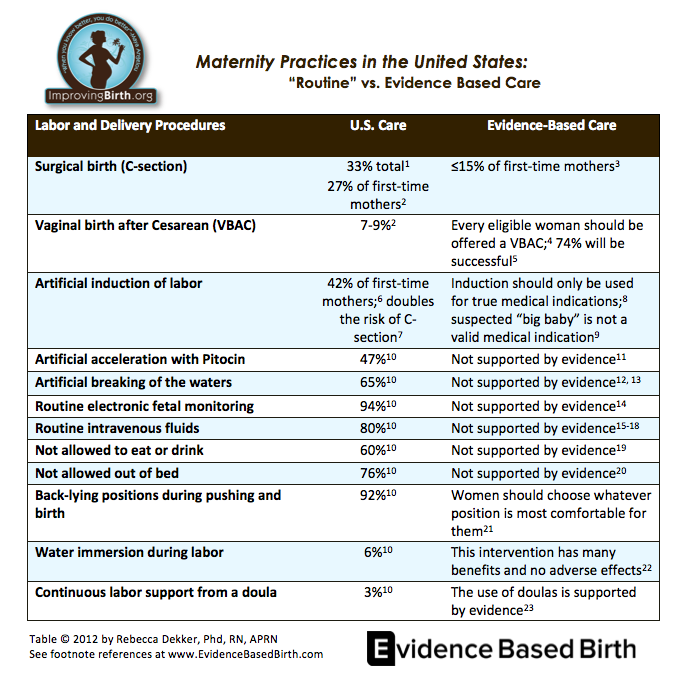 [email protected]
[email protected]
- College information
- Basic information nine0013 Structure and governing bodies of the college
- Documents
- Education
- Educational standards and requirements
- Manual. Teaching staff
- Logistics and equipment of the educational process
- Scholarships and other financial support
- Paid educational services
- Financial and business activities
- Number of students
- Vacancies for reception (transfer) nine0013 Personal data processing
- Anti-corruption
- Legal framework for combating extremism and terrorism
- Vacancies
- Information security
- Olympics nine0013 Mentoring
- Accessible environment
- International cooperation
- Employment of graduates
- Applicant nine0013 Control figures for the reception of citizens
- Fundamentals
- Regulations nine0013 Culture and sports
- Reference
- Educational and methodical work
- Additional education
- Republican information and training pedagogical seminars
This page does not exist.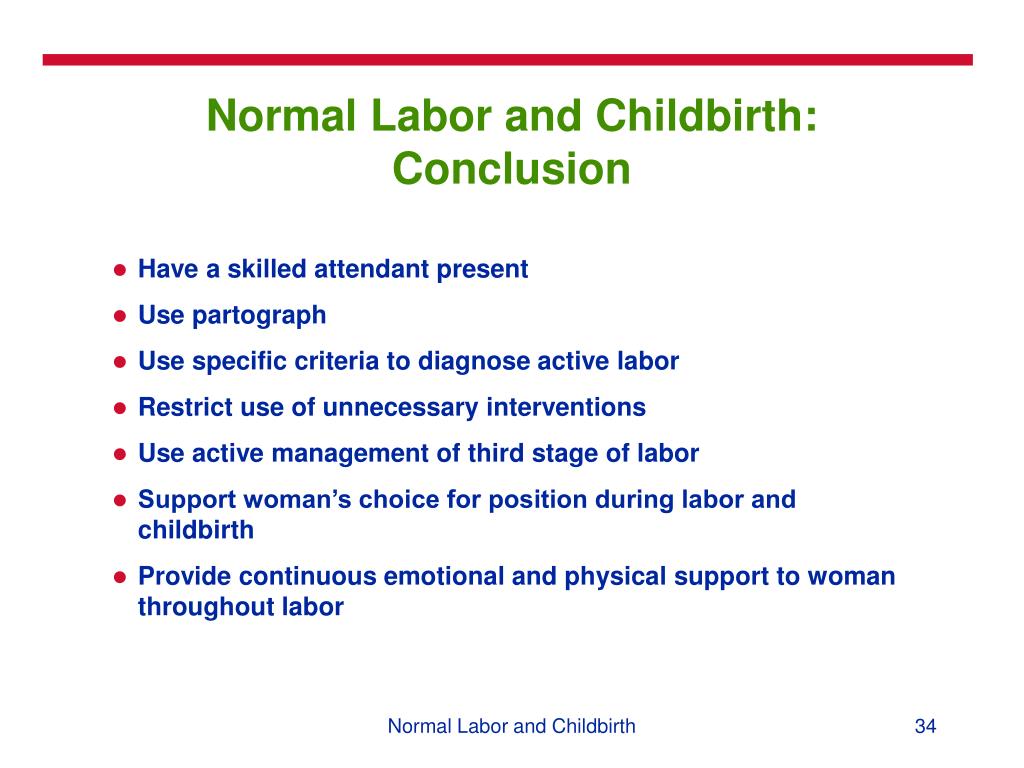
|
Contacts
Remote training
Professional retraining
Professional training
9000
Master classes 9000 9000
338
Public education
| Postal address: | 344015, Rostov-on-Don, st. | |||
| Director's office: | phone/fax: 8(863) 222-48-36, 8(863) 222-74-60, 8(863) 297-07-95 | |||
| Opening hours: | Monday-Friday from 8:45 to 17:15 (break from 12:00 to 12:30) | |||
|
| Saturday-Sunday - day off | |||
| Public VKontakte |
| |||
| E-mail: reception | This email address is being protected from spambots. You must have JavaScript enabled to view. | |||
| Director Dimitrova Lyudmila Vladimirovna | This email address is being protected from spambots. | |||
| Deputy Director for MMR Dvurechenskaya Valentina Mikhailovna | This email address is being protected from spambots. You must have JavaScript enabled to view. | |||
| Methodical room Nazarova Larisa Yurievna | This email address is being protected from spambots. You must have JavaScript enabled to view. | |||
| Chief Accountant Bobrus Olga Vladimirovna | This email address is being protected from spambots. You must have JavaScript enabled to view. | |||
|
For organization of the educational process (heads of departments): | ||||
| Voloshko Lyudmila Petrovna | 8-918-561-58-80 | This email address is being protected from spambots. | ||
| Koroleva Irina Igorevna | 8-918-561-55-25 | This email address is being protected from spambots. You must have JavaScript enabled to view. nine0006 | ||
| Parshenkova Albina Nailevna | 8-918-561-20-50 | This email address is being protected from spambots. You must have JavaScript enabled to view. | ||
| Reznikova Oksana Stanislavovna | 8-918-561-26-36 | This email address is being protected from spambots. You must have JavaScript enabled to view. nine0006 | ||
| Romanova Elena Viktorovna | 8-918-561-58-00 | This email address is being protected from spambots. | ||
| Teslitskaya Elena Vasilievna | 8-918-561-60-70 | This email address is being protected from spambots. You must have JavaScript enabled to view. nine0006 | ||
| Titarenko Irina Yurievna | 8-918-561-09-88 | This email address is being protected from spambots. You must have JavaScript enabled to view. | ||
|
For enrollment: tel/fax: 8(863) 222-28-10 | ||||
| Petrova Anastasia Vladimirovna
| 8-989-620-06-86 This email address is being protected from spambots. You must have JavaScript enabled to view. (in the subject of the letter, indicate the name of the cycle, the date of training and the student's e-mail address) 8-989-620-04-16 | |||
|
For enrollment in CME cycles: cpknmo @ yandex . Pogodina Anna Gennadievna - 8-988-540-06-37 This email address is being protected from spambots. You must have JavaScript enabled to view. Sekunova Olga Nikolaevna – 8-918-550-13-47 This email address is being protected from spambots. You must have JavaScript enabled to view. nine0007 (in the subject of the letter, indicate the name of the cycle, date of study, full name) | ||||
|
For certification: | ||||
| Kozlova Svetlana Alexandrovna | 8-918-561-05-75 | |||
|
For accreditation: head of practice Galtseva Elena Alexandrovna |
8-988-580-01-29 This email address is being protected from spambots. You must have JavaScript enabled to view. | |||
|
Human Resources: Calf Irina Valentinovna |
8-918-561-60-01 | |||
|
Accounting: Osipova Tatyana Borisovna Semernikova Tatyana Sergeevna |
8-918-561-60-01 | |||
|
Economist: Ivanova Uliana Yurievna |
8 (863) 222-48-36 This email address is being protected from spambots. You must have JavaScript enabled to view. | |||
. You must have JavaScript enabled to view. (in the subject of the letter, indicate the name of the cycle, the date of training and the student's e-mail address, and the word DISTATEGORY - if documents are sent; or the word QUESTION - if you need to ask a question)
For webinars
email address This email address is being protected from spambots.
 Blagodatnaya 170, GBOUDPORO "TsPK"
Blagodatnaya 170, GBOUDPORO "TsPK" 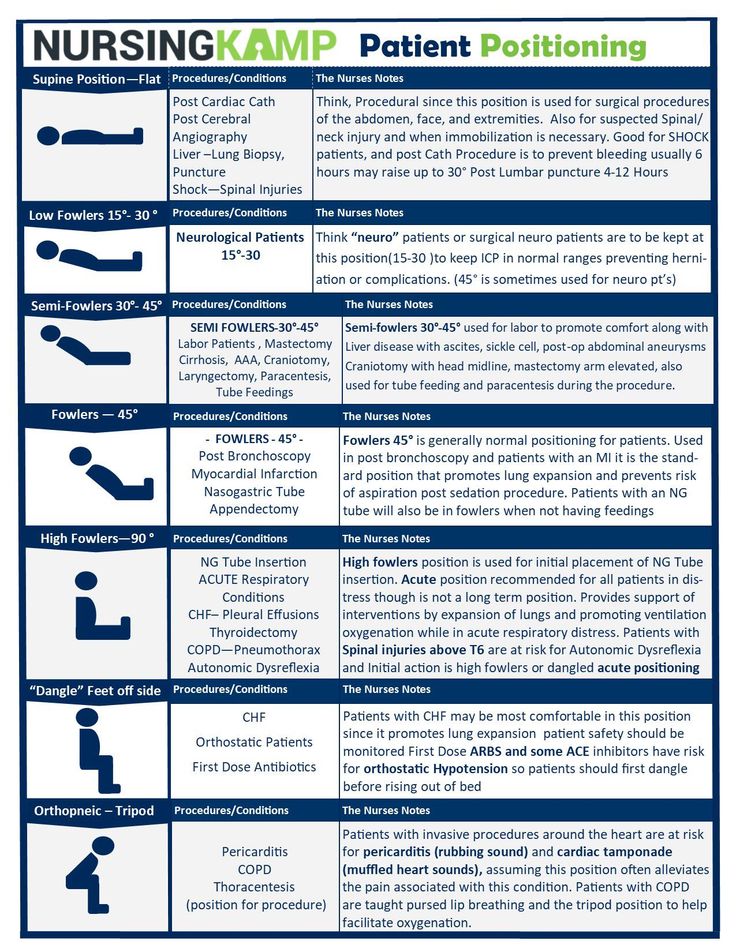 You must have JavaScript enabled to view.
You must have JavaScript enabled to view. 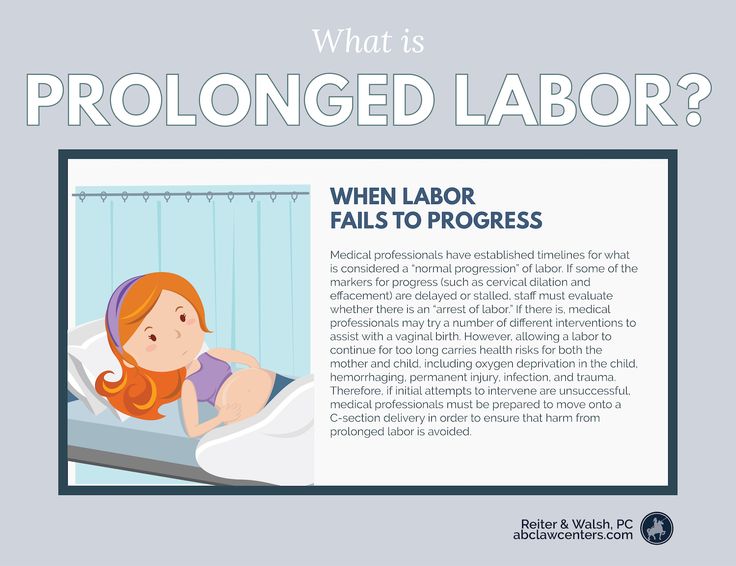 You must have JavaScript enabled to view.
You must have JavaScript enabled to view.  You must have JavaScript enabled to view.
You must have JavaScript enabled to view.  en
en