Nitrous oxide for childbirth
Laughing gas for childbirth: 5 FAQ
Speaking of Health
Topics in this Post
- Obstetrics and Gynecology
When you think of laughing gas, the first image that comes to mind likely is someone hysterically laughing. Nitrous oxide, also known as laughing gas, has been making a comeback as a pain-relief option for women during childbirth. While the option is safe for most women, many rumors surround its use.
Here are the answers to 5 common questions about nitrous oxide as a pain relief option for labor:
1. Why are more women turning to laughing gas for managing childbirth pain?
Women want more options for managing pain during labor and delivery. Nitrous oxide is self-administered, so you feel more control over pain relief.
Nitrous oxide does not limit mobility, slow labor or cause significant risk to the baby. It has a quick onset after it is inhaled and leaves the system quickly once its use is discontinued.
Nitrous oxide will not eliminate pain, but it can dull pain and lessen anxiety. It's a good option for women who are prone to anxiety or want the ability to move around during labor.
2. Does laughing gas make you laugh like crazy?
Contrary to its name, laughing gas does not make you laugh like crazy. The gas slows the nervous system, which makes you feel less inhibited. It also can create a sense of well-being or euphoria. This combination can make you feel gigglier than usually, but most don't laugh hysterically.
Nitrous oxide may make you feel groggy or nauseous, but those potential side effects usually go away within a few minutes.
3. What are some of the benefits of using laughing gas over other pain relief methods?
Laughing gas is the least expensive pain relief option available and has little effect on the baby. It can be used continuously, and it allows you to walk during labor.
Laughing gas also is less invasive than an epidural. If you choose a different pain management option, nitrous oxide can be stopped at any time.
You can safely breastfeed after delivery even if you used laughing gas.
4. Who benefits from using laughing gas?
Laughing gas is a good option if you tend to feel anxious. If you have been diagnosed with anxiety, are nervous around needles, scared of being in hospitals or have a hard time relaxing and releasing tension, it may be for you.
It also is an option to consider if you wanted to avoid an epidural and narcotic pain medication, or it's too early or late for an epidural.
5. How is laughing gas administered?
You give yourself laughing gas by holding a small mask to your mouth to inhale the gas. It takes effect within a minute. Once the mask is removed, the effects of nitrous oxide quickly wear off. Some women prefer to use nitrous oxide during contractions, and others prefer to use it to help relax between contractions. Your health care team will teach you how to use it.
Nitrous oxide is a good option if you are looking for a noninvasive pain reliever that you can control. Knowing the available options will help you choose an effective pain relief method for labor and delivery.
Knowing the available options will help you choose an effective pain relief method for labor and delivery.
Learn more about easing pain with nitrous oxide and the importance of having a birth plan.
Christina Spencer, D.O., is an OB-GYN in Eau Claire, Wisconsin.
For the safety of our patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a non-patient care area where social distancing and other safety protocols were followed.
Topics in this Post
- Obstetrics and Gynecology
Pain management options with midwifery
Menopause transition: What's normal?
Essential oils and pregnancy
Laughing gas helpful for labor pain, safe for baby, but ultimately most women switched to an epidural, study shows
ORLANDO, Fla. – Women report being very satisfied with nitrous oxide (laughing gas) to manage labor pain, experiencing no adverse side effects to the baby, although over half of the women ultimately opted for an epidural or other pain management technique, suggests a study being presented at the ANESTHESIOLOGY® 2019 annual meeting.
– Women report being very satisfied with nitrous oxide (laughing gas) to manage labor pain, experiencing no adverse side effects to the baby, although over half of the women ultimately opted for an epidural or other pain management technique, suggests a study being presented at the ANESTHESIOLOGY® 2019 annual meeting.
“Our research is one of the first large retrospective studies done in the U.S., in five large university hospitals, on the use of nitrous oxide in the labor and delivery unit,” said Barbara Orlando, M.D, one of the lead authors of the study and assistant professor of anesthesiology, perioperative and pain medicine at the Icahn School of Medicine at Mount Sinai, New York. “Although nitrous oxide did not prevent women in labor from requesting other pain management options like an epidural, we received positive feedback from patients who said they like laughing gas as an option to manage their pain.”
There are a variety of options available for women to manage labor pain, ranging from epidurals and medications delivered intravenously, to complementary methods including massage, deep breathing and nitrous oxide.
Nitrous oxide is more commonly used in Europe and Australia to manage labor pain, but has recently gained popularity in the U.S. It is an inhaled anesthetic gas that may help reduce anxiety and make patients less aware of pain, but does not eliminate it. Conversely, epidural anesthesia is the most common type of pain relief used during labor and blocks pain in the lower part of the body, allowing the laboring mother to be awake and alert throughout delivery.
Researchers reviewed the medical records of 1,958 women who used nitrous oxide during labor between March 2016 and March 2018. The average age of the patients was 28 years old. Researchers collected: patient demographics; patient satisfaction; conversion rate to alternate pain management options, including epidurals; and Apgar score, which ranges from 0 to 10 (7 to 10 is considered reassuring) and is used to assess a newborn’s overall condition and health 1 minute and 5 minutes after birth. The authors note only 850 patients included in the study had patient satisfaction information available.
The mean patient satisfaction rate for nitrous oxide use was 7.4 (on a scale from 0 to 10, with 10 being high). Ultimately, 68.9% of women who used nitrous oxide switched to another pain management technique, with the majority (92%) opting for an epidural. Nitrous oxide was found to be safe for the newborns, whose Apgar scores averaged 8 and 9 at 1 and 5 minutes, respectively.
“Nitrous oxide is easy for patients to use, relatively inexpensive, and will attract more patients looking for a birthing center, or more homelike type of delivery experience,” said Dr. Orlando. “The high patient satisfaction rate and safety profile that we found should motivate other institutions nationwide to offer nitrous oxide as a pain management option to women in labor.”
THE AMERICAN SOCIETY OF ANESTHESIOLOGISTS
Founded in 1905, the American Society of Anesthesiologists (ASA) is an educational, research and scientific society with more than 53,000 members organized to raise and maintain the standards of the medical practice of anesthesiology. ASA is committed to ensuring physician anesthesiologists evaluate and supervise the medical care of patients before, during and after surgery to provide the highest quality and safest care every patient deserves.
ASA is committed to ensuring physician anesthesiologists evaluate and supervise the medical care of patients before, during and after surgery to provide the highest quality and safest care every patient deserves.
For more information on the field of anesthesiology, visit the American Society of Anesthesiologists online at asahq.org. To learn more about the role physician anesthesiologists play in ensuring patient safety, visit asahq.org/WhenSecondsCount. Join the ANESTHESIOLOGY® 2019 social conversation today. Like ASA on Facebook, follow ASALifeline on Twitter and use the hashtag #ANES19.
# # #
Childbirth pain relief
Since ancient times, people have perceived pain during childbirth as an evil, attributed it to punishment coming from supernatural forces. To appease these forces, amulets were used or special rituals were performed. Already in the Middle Ages, decoctions of herbs, poppy heads or alcohol were tried to anesthetize childbirth.
However, the use of these drinks brought only minor relief, accompanied by serious adverse events, primarily drowsiness. In 1847, the English professor Simpson first used ether anesthesia to anesthetize childbirth.
Physiological basis of labor pain. Typically, contractions are accompanied by pain of varying severity. Many factors affect the pain in childbirth, their intensity, truly painless childbirth are rare.
Pain during contractions due to:
- 1. Cervical dilatation.
- 2. Contraction of the uterus and tension of the uterine ligaments
- 3. Irritation of the peritoneum, the inner surface of the sacrum due to mechanical compression of this area during the passage of the fetus.
- 4. Pelvic floor muscle resistance.
- 5. Accumulation of products of tissue metabolism, formed during prolonged uterine contraction and temporary violation of the blood supply to the uterus.
The strength of the pain sensation depends on the individual characteristics of the threshold of pain sensitivity, the emotional mood of the woman and her attitude to the birth of the child. It is important not to be afraid of childbirth and labor pain. Nature has taken care to supply the woman with the painkillers she needs for childbirth. Among the hormones produced during childbirth, a woman's body secretes a large number of hormones of joy and pleasure - endorphins. These hormones help a woman to relax, relieve pain, give a feeling of emotional uplift. However, the mechanism for the production of these hormones is very fragile. If a woman experiences fear during childbirth, then a reflex suppression of the production of endorphins occurs and a significant amount of adrenaline (a stress hormone produced in the adrenal glands) is released into the blood. In response to the release of adrenaline, convulsive muscle tension occurs (as an adaptive form of response to fear), which leads to squeezing of muscle vessels and impaired blood supply to the muscles. Violation of the blood supply and muscle tension irritates the receptors of the uterus, which we feel as pain.
It is important not to be afraid of childbirth and labor pain. Nature has taken care to supply the woman with the painkillers she needs for childbirth. Among the hormones produced during childbirth, a woman's body secretes a large number of hormones of joy and pleasure - endorphins. These hormones help a woman to relax, relieve pain, give a feeling of emotional uplift. However, the mechanism for the production of these hormones is very fragile. If a woman experiences fear during childbirth, then a reflex suppression of the production of endorphins occurs and a significant amount of adrenaline (a stress hormone produced in the adrenal glands) is released into the blood. In response to the release of adrenaline, convulsive muscle tension occurs (as an adaptive form of response to fear), which leads to squeezing of muscle vessels and impaired blood supply to the muscles. Violation of the blood supply and muscle tension irritates the receptors of the uterus, which we feel as pain.
Effect of pain on the course of labor.
The uterus has a complex system of receptors. There is a relationship between painful stimulation of the uterine receptors and the accumulation of the hormone of labor (oxytocin) in the pituitary gland. The facts of reflex influences of various painful stimuli on the motor function of the uterus have been established.
Feelings during childbirth largely depend on the mental state of the woman. If all the attention of a woman in labor is concentrated only on pain sensations, a violation of homeostatic mechanisms may occur, a violation of normal labor activity. Pain, fear and excitement during childbirth stimulate that part of the nerve fibers that irritate the circular fibers of the uterine muscle, thereby resisting the pushing forces of the longitudinal fibers of the uterus and disrupt the opening of the cervix. Two powerful muscles begin to oppose each other, this brings the muscles of the uterus into great tension. The tension is of an average level and is perceived as pain. Overvoltage causes a violation of the blood supply to the child through the placenta. If this phenomenon is short-term, then the condition of the fetus does not suffer, since much less oxygen saturation of the blood is necessary for its life support than for an adult. But if this situation persists for a long time, then due to the lack of oxygen, irreversible damage to the tissues and organs of the fetus, primarily its brain, as the organ most dependent on oxygen, can occur.
Overvoltage causes a violation of the blood supply to the child through the placenta. If this phenomenon is short-term, then the condition of the fetus does not suffer, since much less oxygen saturation of the blood is necessary for its life support than for an adult. But if this situation persists for a long time, then due to the lack of oxygen, irreversible damage to the tissues and organs of the fetus, primarily its brain, as the organ most dependent on oxygen, can occur.
The main task of pain relief in childbirth is an attempt to break this vicious circle and not bring the muscles of the uterus to overexertion. Many women prepared for childbirth manage to cope with this task on their own, without resorting to medication due to psychological stability and various psychotherapeutic techniques (relaxation, breathing, massage, water procedures). Other women simply need to provide appropriate medical attention, reducing the feeling of pain or blunting the nervous system's response to pain. If this is not done on time, then the overstressing of the uterus muscles can lead to negative consequences for the mother and fetus.
If this is not done on time, then the overstressing of the uterus muscles can lead to negative consequences for the mother and fetus.
Medications used for labor pain relief must meet the following requirements:
- Have a fairly strong and fast-acting analgesic effect.
- Suppress negative emotions, a sense of fear, while not disturbing the consciousness of the woman in labor for a long period.
- Do not have a negative effect on the body of the mother and fetus, slightly penetrate the placenta and into the brain of the fetus.
- Do not adversely affect labor, the woman's ability to participate in childbirth and the postpartum period.
- Do not cause drug dependence at the required course of drug administration.
- Be available for use in any maternity facility.
The following groups of medicines are used to relieve childbirth:
1. Antispasmodics - drugs that reduce the tone and contractile activity of smooth muscles and blood vessels. Back in 1923, Academician A.P. Nikolaev suggested using an antispasmodic for pain relief during childbirth. The following drugs are usually used: DROTAVERIN (NO-SHPA), PAPAVERIN, BUSCOPAN. Appointment of antispasmodics shown:
Back in 1923, Academician A.P. Nikolaev suggested using an antispasmodic for pain relief during childbirth. The following drugs are usually used: DROTAVERIN (NO-SHPA), PAPAVERIN, BUSCOPAN. Appointment of antispasmodics shown:
- women in childbirth who have not undergone sufficient psychoprophylactic training, showing signs of weakness, imbalance of the nervous system, too young and old women. In such cases, antispasmodics are used at the beginning of the active phase of the first stage of labor (at 2-3 cm of cervical dilatation) in order to prevent labor pains and only partially to eliminate them. It is important to wait for regular steady contractions, otherwise this process of childbirth may stop.
- for women in labor, as an independent analgesic for already developed pains, or in combination with other drugs, when the cervix is dilated by 4 cm or more.
In case of developed labor activity, antispasmodics do not affect the strength and frequency of contractions, do not disturb the consciousness of the woman in labor and her ability to act. Antispasmodics well help to cope with the opening of the cervix, relieve spasm of smooth muscles, reduce the duration of the first stage of labor. They do not have a negative effect on the fetus. Of the side effects, there is a drop in blood pressure, nausea, dizziness, weakness. However, these drugs have an analgesic effect is not pronounced.
Antispasmodics well help to cope with the opening of the cervix, relieve spasm of smooth muscles, reduce the duration of the first stage of labor. They do not have a negative effect on the fetus. Of the side effects, there is a drop in blood pressure, nausea, dizziness, weakness. However, these drugs have an analgesic effect is not pronounced.
2. Non-narcotic analgesics: ANALGIN, TRAMAL, TRAMADOL. The use of drugs of this group, despite the good analgesic effect, in childbirth has some limitations.
In particular, analgin, when prescribed at the very beginning of labor, can weaken uterine contractions and lead to the development of weakness in labor. This is due to the fact that analgin suppresses the production of prostaglandins, which accumulate in the wall of the uterus in order to ensure the proper functioning of the muscles of the uterus during childbirth. At the same time, when labor activity is expressed, analgin does not affect uterine contractility. In addition, analgin affects blood clotting, which can increase blood loss during childbirth. And the use of a combination of analgesics with antispasmodics shortens the duration of the first stage of labor. Contraindications for the use of analgin in childbirth are impaired renal or hepatic function, blood diseases, bronchial asthma.
In addition, analgin affects blood clotting, which can increase blood loss during childbirth. And the use of a combination of analgesics with antispasmodics shortens the duration of the first stage of labor. Contraindications for the use of analgin in childbirth are impaired renal or hepatic function, blood diseases, bronchial asthma.
In addition to pain relief, tramadol has a sedative effect, which is useful in case of a pronounced emotional component of labor pain. However, the sedative effect of tramadol allows it to be attributed to an intermediate position between analgesics and drugs. Respiratory depression in parturient women with the use of tramadol, as a rule, does not occur, rarely causes short-term dizziness, blurred vision, impaired perception, nausea, vomiting and itching. It is forbidden to use these drugs in late toxicosis of pregnancy (preeclampsia). However, the use of these drugs is limited, since with repeated injections they affect the nervous system of the fetus, cause a slowdown in the breathing of the newborn, and disrupt his heart rhythm. Premature newborns are especially sensitive to these drugs.
Premature newborns are especially sensitive to these drugs.
3. Sedatives - sedatives that relieve irritability, nervousness, and stress. These include DIAZEPAM, HEXENAL, THIOPENTAL, DROPERIDOL Hexenal and thiopental are used in childbirth as components of drug anesthesia to relieve agitation, as well as to reduce nausea and vomiting. Side effects of these drugs include hypotension and respiratory depression. They quickly penetrate the placental barrier, but at low doses do not cause severe depression in mature full-term newborns. During childbirth, these drugs are rarely prescribed. The main indication for their use is to obtain a rapid sedative and anticonvulsant effect in pregnant women with severe forms of preeclampsia.
Diazepam has no analgesic effect, so it is prescribed in combination with narcotic or non-narcotic analgesics. Diazepam is able to accelerate the opening of the cervix, helps to relieve anxiety in a number of women in labor. However, it easily penetrates into the blood of the fetus, therefore, it causes respiratory failure, a decrease in blood pressure and body temperature, and sometimes signs of neurological depression in newborns.
Droperidol causes a state of neurolepsy (calmness, indifference and aloofness), has a strong antiemetic effect. In obstetric practice has received significant distribution. However, one should be aware of the side effects of droperidol: it causes incoordination and weakness in the mother, respiratory depression and pressure drop in the newborn. With high blood pressure in a woman in labor, droperidol is combined with analgesics.
4. Narcotic analgesics: PROMEDOL, FENTANIL, OMNOPON, GHB
The mechanism of action of these drugs is based on interaction with opiate receptors. They are believed to be safe for both mother and child. They act soothingly, relaxes, while maintaining consciousness. They have an analgesic, antispasmodic effect, promote the opening of the cervix, contribute to the correction of uncoordinated uterine contractions.
However, all narcotic drugs have a number of disadvantages, the main of which is that in high doses they depress breathing and cause drug dependence, state of stupor, nausea, vomiting, constipation, depression, lowering blood pressure. The drugs easily cross the placenta, and the more time passes from the moment the drug is administered, the higher its concentration in the blood of the newborn. The maximum concentration of promedol in the blood plasma of a newborn was noted 2-3 hours after its administration to the mother. If the birth occurs at this time, then the drug causes temporary respiratory depression of the child.
The drugs easily cross the placenta, and the more time passes from the moment the drug is administered, the higher its concentration in the blood of the newborn. The maximum concentration of promedol in the blood plasma of a newborn was noted 2-3 hours after its administration to the mother. If the birth occurs at this time, then the drug causes temporary respiratory depression of the child.
Sodium oxybutyrate (GHB) is used when a woman in labor needs to rest. As a rule, when the drug is administered, sleep occurs after 10-15 minutes and lasts 2-5 hours. Ether is not currently used for labor pain relief, since it significantly weakens labor activity, can increase blood pressure, and adversely affect the fetus.
Inhalation anesthesia of childbirth by inhalation of painkillers is still widely used in obstetric practice. Inhalation anesthetics are used in the active phase of labor with the opening of the cervix by at least 3-4 cm and in the presence of severe pain in contractions.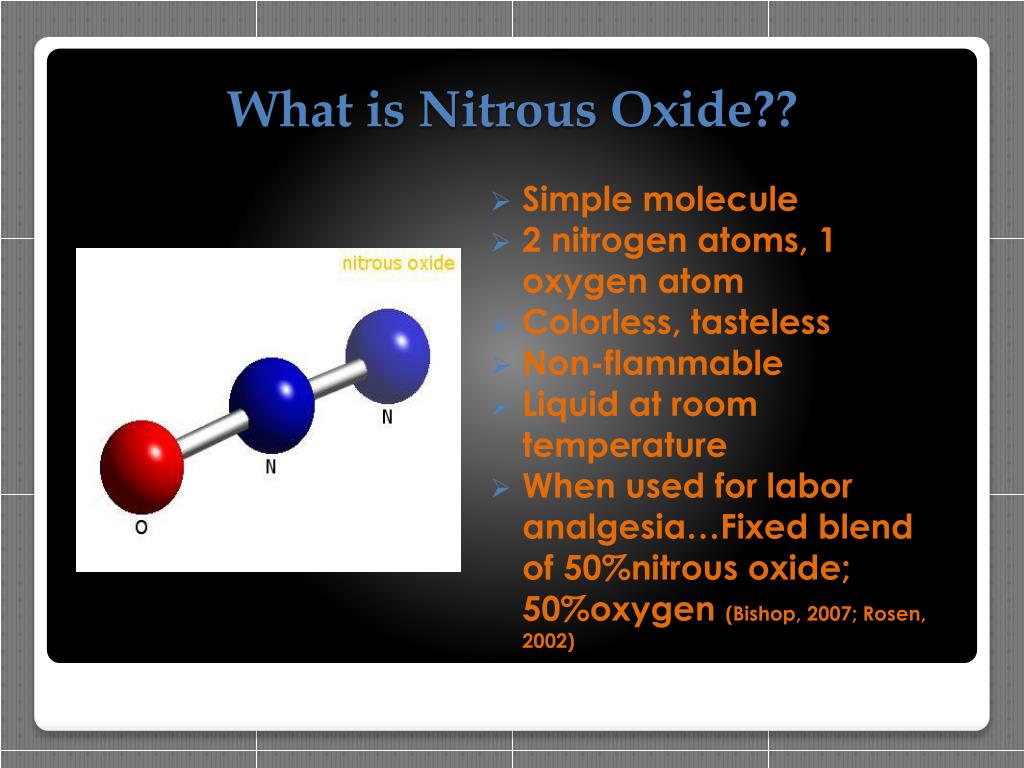
Nitrous oxide is the primary inhalant used for both obstetric and labor pain relief. The advantage of nitrous oxide is safety for the mother and fetus, the rapid onset of action and its rapid end, as well as the absence of a negative effect on contractile activity, and a pungent odor. They give nitrous oxide through a special apparatus using a mask. The woman in labor is introduced to the technique of using the mask and she herself applies the mask and inhales nitrous oxide with oxygen as needed. When inhaling it, a woman feels dizzy or nauseous. The action of the gas is manifested in half a minute, so at the beginning of the contraction, you need to take a few deep breaths
Trilene is a clear liquid with a pungent odor. It has an analgesic effect even in small concentrations and with the preservation of consciousness. Does not suppress labor activity. It is a well-administered fast-acting agent - after the cessation of inhalation, it quickly ceases to have an effect on the body. The downside is the bad smell.
The downside is the bad smell.
6. Epidural anesthesia during childbirth and caesarean section
Epidural analgesia is performed by blocking pain impulses from the uterus along the nerve pathways entering the spinal cord at a certain level by injecting a local anesthetic into the space around the spinal cord membrane.
Performed by an experienced anesthesiologist. The time to start epidural analgesia is determined by the obstetrician and anesthesiologist, depending on the needs of the woman in labor and the child during childbirth. It is usually performed with established regular labor and at least 3-4 cm dilatation of the cervix.
Epidural lumbar anesthesia is performed in the lower back with the mother sitting or lying on her side. After treating the skin in the area of the lumbar spine, the anesthesiologist makes a puncture between the vertebrae and enters the epidural space of the spine. First, a trial dose of anesthetic is administered, then, if there are no side effects, a catheter is inserted and the desired dose is administered. Sometimes the catheter can touch a nerve, causing a shooting sensation in the leg. The catheter is attached to the back, if it is necessary to increase the dose, subsequent injections will no longer require a second puncture, but are made through the catheter.
Sometimes the catheter can touch a nerve, causing a shooting sensation in the leg. The catheter is attached to the back, if it is necessary to increase the dose, subsequent injections will no longer require a second puncture, but are made through the catheter.
Pain relief usually develops 10-20 minutes after the epidural and can be continued until the end of labor and is usually very effective. Epidural anesthesia is safe for mother and child. Of the side effects, there is a decrease in blood pressure, back pain, weakness in the legs, headaches. More severe complications are a toxic reaction to local anesthetics, respiratory arrest, and neurological disorders. They are extremely rare.
Sometimes the use of epidural anesthesia leads to a weakening of labor. At the same time, a woman cannot effectively push, and thus the percentage of surgical interventions (obstetrical forceps) increases.
Contraindications to the use of epidural anesthesia are: violation of blood clotting, infected wounds, scars and tumors at the puncture site, bleeding, diseases of the nervous system and spine.
Epidural anesthesia can be safely used for caesarean section. If an epidural catheter is already in place at the time of delivery and it becomes necessary to perform a caesarean section, it is usually sufficient to inject an additional dose of anesthetic through the same catheter. A higher concentration of the drug can cause a feeling of "numbness" in the abdominal cavity, sufficient for surgery
7. General anesthesia.
Indications for the use of general anesthesia in childbirth are emergency situations, such as a sharp deterioration in the condition of the child and maternal bleeding. This anesthesia can be started immediately and causes a rapid loss of consciousness, allowing for an immediate caesarean section. In these cases, general anesthesia is relatively safe for the child.
The use of any painkillers during childbirth is carried out only by obstetrician-gynecologists and anesthesiologists-resuscitators. Nurses, anesthetists and midwives follow the doctor's orders, monitor the condition of the woman in labor and note possible side effects that require a change in treatment.
Midwife billed 00 for using laughing gas in her own labor
Nurse midwife billed $5,000 for using laughing gas to manage pain during labor.
Carly-Rae Kerrschneider (32) of Baldwin, Wisconsin used an epidural when she gave birth to her first child, daughter Eleanor, in 2016, but she didn't like the way the drug hindered her movements during labor. So she decided to use nitrous oxide, or laughing gas, which allowed her to walk around the ward during the delivery of her second child, son Leviathan, in December 2018.
Nitrous oxide is inhaled through a mask and helps women cope with pain without becoming numb. Recently, there has been an increase in hospitals that offer women during childbirth not to use epidural anesthesia, which hinders movement, but laughing gas.
During the 11-hour labor, the woman inhaled laughing gas about 10-15 times per hour, according to Kaiser Health News. And the woman was shocked when she and her husband Christopher received a $12,000 hospital bill, including $4,836 for nitric oxide alone.
Midwife, 32, hit with $5,000 medical bill for using laughing gas for pain during her own labor: Karli-Rae Kerrschneider, 32, from Baldwin, Wisconsin, was charged nearly $12,000 for her hospital stay when she gave birth in December 2018, including $5,000… https://t.co/fNm57iQRrR pic.twitter.com/ijQSu61UYx
— RushReads (@RushReads) May 29, 2019
The woman says her water birth at Hudson Hospital was uneventful. “It was amazing. I would do it again,” , she told Kaiser Health News. She and her son spent 2 days in the hospital before they were released. Kerrschneider says she was not given any other painkillers other than laughing gas.
When Kerrschneider received the bill, she called the hospital, suggesting that she had been inadvertently sent a bill for an epidural. At the Western Wisconsin Health hospital in St. Croy County, where she works herself, nitrous oxide costs as little as $100, according to Kaiser Health News.