Night sickness not pregnant
Nausea at Night: Causes, Treatment, Prevention
Nausea can happen at any time of the day. But some conditions may be more likely to make you feel nauseous at night.
Sometimes you can be nauseous without an underlying cause, but it’s most often a symptom of another condition.
Read on to learn more about what can cause nighttime nausea, when to see a doctor, the treatment options, and how to help ease your nausea at home.
The possible causes of nausea at night include the conditions outlined below.
Anxiety
Anxiety includes feelings of nervousness and worry. It’s common to have these feelings from time to time. Almost everyone experiences anxiety at some time or another.
If, however, you have these feelings often, or if your anxiety seems out of proportion to your current situation, you may have a condition called generalized anxiety disorder.
Whether you have everyday worries or an anxiety disorder, anxiety can get worse at night. This may be because you have fewer distractions at night, compared to the daytime when you’re occupied with work, school, or family matters.
When your mind isn’t focused on something else, you may be more likely to dwell on your worries or problems.
All types of anxiety can cause gastrointestinal issues, including nausea. Since anxiety may be worse at night, you may be more likely to have nausea at night, too.
Other symptoms of anxiety include:
- restlessness
- trouble concentrating
- increased heart rate
- panic attacks
- sweating
- trouble falling asleep
- trouble thinking about anything except what’s causing your anxiety
GERD
Gastroesophageal reflux disease (GERD) is a condition in which stomach acid flows back up through your esophagus. It’s also called acid reflux.
It occurs when the band of muscle between your esophagus and stomach doesn’t properly close or tighten. This allows the digestive juices in your stomach to move up into your esophagus.
The most common symptom of GERD or acid reflux is heartburn — an uncomfortable burning sensation in your chest. You might also notice a bitter taste at the back of your mouth. Nausea may accompany these symptoms, too.
You might also notice a bitter taste at the back of your mouth. Nausea may accompany these symptoms, too.
Other symptoms of GERD include:
- trouble swallowing
- feeling like something is stuck in your throat
- dry cough
- pain in your chest or upper abdomen
- vomiting
- asthma
Eating late at night can increase symptoms of GERD, including nausea. This is because lying down, especially after eating a big meal, makes it easier for acid to flow up into your esophagus.
Medication side effects
Nausea is a common side effect of medications, especially:
- antibiotics
- aspirin
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- some types of blood pressure medication
If you take your medication at night, you might notice more nausea at night.
Other symptoms or side effects depend on the medication.
Peptic ulcers
Peptic ulcers are sores on the lining of your stomach or small intestine. The bacteria H. pylori can cause it.
The bacteria H. pylori can cause it.
The most common symptom is pain between your ribs and belly button. Other symptoms include:
- nausea
- burping
- feeling full after eating a small amount of food
- vomiting
- black or bloody stool
- unexplained weight loss
These symptoms often get worse after meals and at night.
Pregnancy
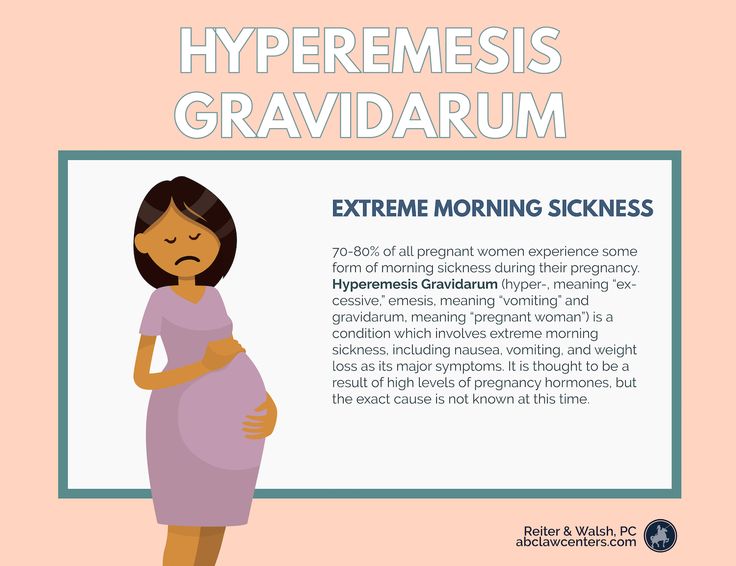
Nausea is a very common pregnancy symptom. While nausea during pregnancy is often called morning sickness, it can happen at any time of the day.
An increase in hormones causes nausea during pregnancy. It usually begins around week 6 and ends around week 12 of pregnancy. It’s not dangerous to you or baby, unless you can’t keep food down.
Gastroparesis
Another possible cause of nausea at night is gastroparesis. This is a disease in which the stomach can’t normally empty itself of food.
It’s most common in people with diabetes. Other causes include:
- infections
- surgery
- scleroderma
- narcotics
- some antidepressants
Gastroparesis can also occur from an injury to the vagus nerve, which helps your stomach muscles contract to move food.
Symptoms may be worse at night, as the food you eat during the day builds up in your stomach.
Symptoms of gastroparesis include:
- nausea
- heartburn
- vomiting
- feeling full after eating a small amount of food
- bloating
- weight loss
Cyclic vomiting
Although less common, cyclic vomiting syndrome is another possible cause of nausea at night that can affect both adults and children. It’s a rare disorder that causes recurrent episodes of severe nausea and vomiting.
These episodes can last for a few hours or a few days. Most people have episodes about the same length each time. In between the vomiting and nausea you feel healthy.
Besides nausea and vomiting, symptoms may include:
- pale skin
- lethargy
- dizziness
- headaches
- abdominal pain
- dry heaving
Exhaustion and anxiety are both triggers for cyclic vomiting syndrome, and both are more common at night. This can make cyclic vomiting syndrome more likely to start at night.
This can make cyclic vomiting syndrome more likely to start at night.
In many cases, nausea is temporary and will go away on its own. But it can also be a sign of a more serious problem. See your doctor if:
- your nausea lasts longer than a week
- you consistently feel nauseous after eating
- your nausea leads to severe headaches with vomiting
- you have unexplained weight loss
- nausea and vomiting keep coming back over the course of at least 1 month
- you can’t keep food down, especially if you’re pregnant
- you’re experiencing:
- confusion
- blurred vision
- severe abdominal pain
Treatment for nausea at night will depend on the underlying cause.
Anxiety
One of the most effective treatments for anxiety is psychotherapy, especially cognitive behavioral therapy, also known as CBT.
This type of therapy helps you identify negative or destructive thought patterns. Once you notice these patterns, you can start learning how to reframe your thoughts in a more positive way.
Other possible treatment options for anxiety include:
- anti-anxiety medication
- lifestyle changes, such as exercise and reducing caffeine and alcohol consumption
GERD
The most common treatment options for GERD include:
- antacids
- medications called h3 blockers, which reduce acid production (available over the counter or by prescription)
- medications called proton pump inhibitors, which are stronger acid reducers (available OTC and by prescription)
- surgery, if medications don’t help
- lifestyle changes, such as avoiding spicy food, not eating at night, eating smaller meals, and limiting alcohol and caffeine
Medication side effects
If a prescription medication is causing your nausea, talk to your doctor about switching medications or taking them at a different time of day to alleviate nausea and other side effects. You may also need to take your medication with food or water.
It’s important that you don’t stop taking your medication on your own. Always talk to your doctor about the best way to change your medication or the way you take it.
Always talk to your doctor about the best way to change your medication or the way you take it.
If an OTC medication is making you nauseous, try taking a different kind, like ibuprofen instead of naproxen.
Peptic ulcers
The most common treatment options for peptic ulcers include:
- antibiotics to get rid of H. pylori bacteria
- antacids, h3 blockers, or proton pump inhibitors to reduce stomach acid
- medications to protect your stomach’s lining
- lifestyle changes, such as quitting smoking and avoiding foods that make your symptoms worse
Gastroparesis
Treatment for gastroparesis typically includes:
- medications that help your stomach muscles move normally
- surgery
- lifestyle changes, such as eating smaller meals and eating food that’s easy to digest
Cyclic vomiting syndrome
Treatment for cyclic vomiting syndrome may include:
- anticonvulsants
- anti-nausea medication
- anti-migraine treatment
- treatment for dehydration; if it’s severe, you may need to be treated in the hospital with IV fluids
- avoiding triggers
There are steps you can take to help reduce the severity of your nausea at home. If your nausea persists for longer than a week, or if it gets worse, it’s important that you see your doctor.
If your nausea persists for longer than a week, or if it gets worse, it’s important that you see your doctor.
The following self-care measures may help your nausea:
- Prop your head up so you’re not lying flat in bed. If it’s comfortable for you, try to sleep with your head about 12 inches above your feet. This can help keep acid or food from moving up into your esophagus.
- Drink a small amount of a slightly sweet liquid, like fruit juice, but avoid citrus. Drink slowly. Increase the amount as you start to feel better.
- Drink ginger or peppermint tea.
- Suck on a peppermint.
- Eat a small amount of light, bland food, like plain crackers or bread.
- Avoid physical activity until you feel better, but try to avoid lying down.
Nausea at night is usually a symptom of an underlying condition. Some of the most common causes include acid reflux, anxiety, medication side effects, peptic ulcers, or pregnancy.
Nausea at night is usually treatable, either with self-care remedies or by a doctor.
If your nausea is severe or long lasting, or if you have bad headaches or unexplained weight loss together with nighttime nausea, see your doctor. They can diagnose the cause of your nausea and work with you to find the right type of treatment.
Not Pregnant, Early Pregnancy, and More
Overview
Nausea is one of the most common medical symptoms and it can be related to many different conditions. Usually, nausea is not a sign of a serious problem and passes on its own. But in other cases, nausea may be a sign of a health condition that needs attention, such as stomach flu, pregnancy, or a side effect from medication.
Nausea is defined as having discomfort in the stomach usually accompanied by an urge to vomit. Discomfort might include heaviness, tightness, and a feeling of indigestion that doesn’t go away.
Vomiting is what happens when your body empties its stomach contents through your mouth. Not all cases of nausea cause vomiting.
Nausea can affect all people of all ages. Your nausea might be caused by something as simple as eating a food that doesn’t agree with your stomach. But in other cases, nausea has more serious causes.
Your nausea might be caused by something as simple as eating a food that doesn’t agree with your stomach. But in other cases, nausea has more serious causes.
Common causes of nausea include:
- anesthetics
- chemotherapy from cancer treatment
- digestive problems such as gastroparesis
- inner ear infections
- migraine headache
- motion sickness
- obstruction in the intestines
- stomach flu (viral gastroenteritis)
- viruses
Morning sickness is a common symptom of pregnancy. It’s described as nausea experienced during pregnancy, usually in the mornings after waking up. It’s most common during a woman’s first trimester. Sometimes, it begins as early as two weeks after conception.
Morning sickness is an uncomfortable condition that can occur with or without vomiting. But the main difference between nausea caused by morning sickness and nausea caused by other conditions is morning sickness is accompanied by other symptoms of early pregnancy. These symptoms include:
These symptoms include:
- A delayed or missed period. Some people may experience bleeding after they become pregnant but this bleeding is very light and is much shorter than a typical period. A missed period can also be caused by excessive weight loss or gain, fatigue, stress, change in birth control use, illness, high activity level, and breastfeeding.
- A change in breasts. Usually pregnancy causes swollen or sensitive breasts that feel tender to the touch. It can also cause darkening of the areas around the nipples (areolas). These changes in breasts can be caused by hormonal imbalances, changes in birth control, and PMS.
- Tiredness or fatigue. This symptom can also be caused by stress, overworking, mental health problems such as depression, the cold, the flu, a virus, allergies, insomnia, and poor nutrition.
- Lower backaches. These can also be caused by PMS, poor form when exercising, injury, poor sleeping habits, poor footwear, being overweight, and stress.
- Headaches. Headaches are commonly caused by dehydration and caffeine. They can also be caused by PMS, withdrawals from drugs or alcohol, eye strain, and stress.
- Mood swings caused by hormonal changes. You might feel happy one moment and depressed another. Mood swings can also be caused by poor nutrition, hormonal imbalances, or underlying mental health issues.
- Frequent urination. This can also be caused by urinary tract infections and diabetes, as well as an increase in liquid intake, or consumption of diuretics such as coffee.
- Food cravings or food aversions. You might feel like eating foods you normally don’t like eating or avoiding foods you normally like to eat. These symptoms can also be caused by a poor diet, lack of proper nutrition, anxiety and stress, depression, PMS, or illness.
You should consider taking a pregnancy test if you experience nausea with a few of these symptoms, especially if you’ve missed a period.
The only way to know for certain whether or not you’re pregnant is to take a pregnancy test. You can get early detection tests at most drug stores. If you want a certain result, your doctor can do a blood test to check for pregnancy.
Both morning sickness and nausea can greatly impact your quality of life.
If you’re not pregnant and you’ve been nauseous for more than a month, especially with weight loss, schedule an appointment with your doctor. In the meantime, try to relax and stay hydrated.
Keep away from strong odors such as perfume and food and other triggers like heat that could make your nausea worse. Stick to eating bland foods such as crackers and rice, and take over-the-counter motion sickness medication.
Eating small meals and snacks, staying hydrated, avoiding nausea triggers, and taking vitamin B-6 supplements and antihistamines can ease most cases of morning sickness.
If you’re pregnant and experiencing morning sickness that’s getting in the way of your daily activities, schedule a visit to your doctor. They can prescribe anti-nausea medication that will make you feel better and able to eat so you can nourish your pregnant body.
They can prescribe anti-nausea medication that will make you feel better and able to eat so you can nourish your pregnant body.
Again, in most cases, nausea and morning sickness are not a cause for concern. But it’s important to see a doctor if you’re concerned or if your symptoms are getting in the way of your daily activities, so you can be happy and healthy.
Night sweats
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Night sweats - the causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
According to statistics, more than a third of patients complain of periodic sweating that occurs during the day. Far from always, this condition is a sign of a disease, but if such a symptom occurs regularly for no apparent reason and at night, this should be paid attention to.
Types of episodes of sweating
When talking to a doctor about the occurrence of episodes of sweating at night, many people mean different manifestations by this. In some cases, this refers to perspiration on the forehead, and in others, so much sweat that you have to change clothes, and sometimes bed linen. In addition, the number of episodes of increased sweating, or hyperhidrosis, per night and the accompanying symptoms (snoring, holding your breath, fever, fear, insomnia, frequent urination) are important.
Possible causes
Increased heat production and sweating can be caused by various reasons, including those not related to the disease.
First of all, you should pay attention to the microclimate of the room and bedding.
Too warm blankets, synthetic clothes, elevated temperature in the bedroom will inevitably cause bouts of night sweats. If the above is excluded from the list of causes of excessive sweating, then other possible factors should be considered.
Excessive sweating can occur as a result of infectious diseases with alternating periods of increase and sharp decrease in temperature. A sharp decrease in temperature in viral infections (flu, SARS, mononucleosis), bacterial diseases (pneumonia, tuberculosis, endocarditis, lung abscess), septic fevers is always accompanied by profuse sweating. A number of tumors also give such a symptom as increased sweating. Pheochromocytoma (a tumor of the adrenal glands that secretes the catecholamines adrenaline and norepinephrine) causes hyperproduction of sweat due to increased production of hormones.
With lymphoma, along with the general signs of intoxication, night sweats can be profuse (profuse). Excessive sweating is accompanied by some endocrine diseases.
Excessive sweating is accompanied by some endocrine diseases.
In women, increased heat production, leading to hyperhidrosis, occurs during hormonal changes: during pregnancy and perimenopause. Against the background of a decrease in the level of estrogens and an increase in the content of follicle-stimulating hormone, a change in the distribution of blood in the vessels of the skin occurs. This explains the sudden reddening of the skin and sweating during hot flashes. Men can also experience night sweats during andropause, an age-related decrease in the production of the sex hormone testosterone.
Increased sweating can be a symptom of thyrotoxicosis - a disorder of endocrine regulation due to dysfunction of the thyroid gland.
In this disease, there is an increased metabolism and an increase in body temperature, which causes hyperproduction of sweat. Nervousness and psychological instability, characteristic of patients with thyrotoxicosis, also contribute to the increase in sweating.
Hypoglycemia in diabetics leads to episodes of night sweats.
Acromegaly, in which the production of somatotropin growth hormone is increased, is almost always accompanied by increased sweat production in the evening and at night.
Be sure to mention obesity, which also increases sweating. This process can be associated not only with the activity of the endocrine glands, but also with the use of products that stimulate the sweat glands.
At night, sweat can come out with a sudden cessation of breathing - apnea. As a rule, in this case, perspiration appears mainly on the face. Episodes of transient cerebrovascular accident, hypertensive crisis, encephalitis, and volumetric brain tumors can lead to sweating disorders. All these diseases can be accompanied not only by increased sweating, but also by other signs of autonomic dysfunction: chills, fear, irritability. Sweat on the face often occurs with Parkinson's disease. Panic attacks are among the neurological conditions associated with excessive night sweats. They are characterized by an unexpected and inexplicable attack of feeling unwell, accompanied by fear or anxiety. Panic attacks can occur either in certain uncomfortable situations, such as when riding the subway, or develop for no apparent reason (at night) and be accompanied by a feeling of fear, palpitations and sweating.
They are characterized by an unexpected and inexplicable attack of feeling unwell, accompanied by fear or anxiety. Panic attacks can occur either in certain uncomfortable situations, such as when riding the subway, or develop for no apparent reason (at night) and be accompanied by a feeling of fear, palpitations and sweating.
Increased sweating is often provoked by taking medications (cytostatics, aspirin, insulin, prozerin), alcohol, drugs, sometimes this phenomenon is observed with withdrawal reactions (occurring when psychoactive substances are stopped).
Diagnostics and examinations
First of all, you need to make sure that sweating does not serve as a reaction to elevated room temperature, excessively warm bedding and clothes. It is necessary to exclude the infectious nature of sweating, in particular, tuberculosis. At the same time, it is important to establish the patient's belonging to risk groups for tuberculosis (migrants; persons released from prison; persons in whose families there is a patient with tuberculosis; frequently ill patients; HIV-infected; patients with diabetes mellitus people receiving corticosteroids and immunosuppressive therapy, as well as chemotherapy and radiation therapy for cancer). Long-term respiratory symptoms dictate the need for chest x-ray, clinical blood test, sputum examination for acid-resistant mycobacteria by microscopy (three times) and immunodiagnosis of tuberculosis infection.
Long-term respiratory symptoms dictate the need for chest x-ray, clinical blood test, sputum examination for acid-resistant mycobacteria by microscopy (three times) and immunodiagnosis of tuberculosis infection.
In the absence of data confirming the infectious or endocrine nature of sweating, an examination for the presence of oncological diseases is necessary.
Which doctors should I contact?
First of all, you need to visit a therapist who, after a survey and an initial examination, can give directions for tests and additional examinations. With hormonal disorders, further treatment is endocrinologist. In the case of infectious diseases, either the therapist or the infectious disease specialist will continue the treatment. When tuberculosis is confirmed, the patient is sent to the anti-tuberculosis dispensary. In the presence of tumor diseases, they turn to an oncologist.
What should I do if I'm sweating?
If sweating is associated with a natural restructuring of the hormonal background, you need to take it calmly - experiences and nervous breakdowns will only exacerbate the problem.
Treatment
Increased sweating, if it is not caused by uncomfortable temperature conditions and a genetic predisposition, is only a symptom of a pathological condition.
Therefore, the main task is the treatment of the causative disease.
Sources:
- Clinical guidelines "Tuberculosis in adults". Developed by: Russian Society of Phthisiologists, Association of Phthisiologists. – 2022.
- Clinical guidelines "Tuberculosis in children". Developed by: Russian society of phthisiatricians. – 2020.
- Clinical guidelines "Menopause and menopause in women." Developed by: Russian Society of Obstetricians and Gynecologists. – 2021.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
False pregnancy - causes, symptoms, diagnosis and treatment
I confirm More
- INVITRO
- Library
- Disease Handbook
- False pregnancy
Pseudocyesis
Pseudo-pregnancy
Amenorrhea
Toxicosis
25812 February 17
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes over time, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
False pregnancy, or pseudocyesis: causes, symptoms, diagnosis and treatment.
Definition
False pregnancy is a psychophysiological disorder characterized by a woman's erroneous belief that she is pregnant based on her neuroendocrine symptoms, which resemble those of a true pregnancy.
Pseudo-pregnancy occurs in one in 22,000 pregnancies.
Causes of false pregnancy
The development of this pathology is based on mental, psychological and emotional factors that provoke endocrine, vegetative and somatic disorders. Experts note that women who experience a false pregnancy are very eager to experience the state of pregnancy and become mothers.
Experts note that women who experience a false pregnancy are very eager to experience the state of pregnancy and become mothers.
At the heart of mental causes development of false pregnancy are functional neurological disorders: neurosis, anxiety, personality disorders, schizophrenia, dementia praecox, manic-depressive psychosis, hysteria, frontotemporal degeneration.
Psychological reasons often go in addition to mental ones. False pregnancy is more likely in women with an unstable nervous system, in the presence of psychopathic character traits and traumatic situations.
The risk group is women over 35 years old, especially suspicious and impressionable.
The psychological reasons for the development of a false pregnancy are the desire to have a child, a large number of abortions or spontaneous abortion at different stages of gestation, fear of bearing a child, the death of an already born child, envy towards people who have children, the desire to keep a husband in the family, approaching menopause . In young women, pseudopregnancy can develop as a result of amenorrhea, anxiety associated with unprotected intercourse, tubal ligation (surgical sterilization), and hysterectomy (removal of the uterus).
In young women, pseudopregnancy can develop as a result of amenorrhea, anxiety associated with unprotected intercourse, tubal ligation (surgical sterilization), and hysterectomy (removal of the uterus).
Stress, emotional experiences and increased anxiety are accompanied by increased production of pituitary hormones. Against the background of hormonal imbalance, a woman has a partial or full range of manifestations of pregnancy, with the exception of the presence of a fetus.
It is assumed that the disease can be caused by trauma (physical or mental), hormone imbalance and some diseases. The appearance of symptoms of false pregnancy is noted with hormone-secreting tumors (ovarian cyst, uterine myoma, etc.), hypothyroidism (a disease caused by a decrease in thyroid function and insufficient hormone production), alcoholic liver disease, cholecystitis (including gallstones), infections urinary tract (complicated by urinary retention), tumors of the abdominal cavity, hyperprolactinemia, esophageal achalasia.
There are a number of studies that focus on the neuroendocrine mechanism underlying false pregnancy. Changes in plasma levels of prolactin, follicle-stimulating hormone, luteinizing hormone, growth hormone, estradiol, progesterone, and testosterone can cause amenorrhea, galactorrhea (milk production outside the breastfeeding period), and diurnal and/or nocturnal hyperprolactinemia, which are found in most women with false pregnancies .
I.P. Pavlov in the development of false pregnancy attached great importance to cortical impulses under the influence of self-hypnosis. He believed that an ultraparadoxical phase state develops in the cerebral cortex.
Somatic changes are probably also explained by endocrine disorders (hypothalamic-pituitary, ovarian, adrenal).
Increased activity of the sympathetic nervous system causes apparent fetal movements and contractions on the day of expected delivery. The sympathetic system increases the contractility of the diaphragm, chronic contraction of the diaphragmatic muscle pushes the intestines down in the abdominal cavity, the intestines are stretched, constipation, pain and a characteristic lordotic posture occur (the head is pushed forward, the chest is flat, turning into a protruding abdomen, the shoulders are pushed forward, and the legs are spread apart in knee joints).
False pregnancy syndrome can also be experienced by men (Couvade syndrome, or sympathetic pregnancy) whose partners are currently carrying a child. Such a disorder can develop in men of an infantile-hysterical psychotype against the background of strong empathy for the condition of a woman. At the same time, men feel many of the symptoms that characterize the course of pregnancy in a partner.
Disease classification
In the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), false pregnancy is a disorder with somatic symptoms. The disease is listed as "not elsewhere classified", meaning that it is in a separate category from other somatic symptom disorders such as functional neurological symptomatic disorder.
Symptoms of a false pregnancy
In pseudopregnancy, a woman does not pretend her condition, but is really convinced that she is pregnant, experiences and feels its signs.
False pregnancy is accompanied by vegetative and endocrine symptoms that mimic the changes that occur in the female body after fertilization.
In women with pseudopregnancy, there may be slight discharge during menstruation or amenorrhea, signs of toxicosis (nausea, increased salivation, vomiting, fatigue, drowsiness, mood swings, perversion of food addictions, etc.) may appear.
In case of false pregnancy, the mammary glands increase, breast milk is secreted, nipples are hyperpigmented, in rare cases, changes in the external genitalia and cervix are noted, the stomach enlarges as a result of excessive development of subcutaneous tissue on the anterior abdominal wall and flatulence, weight is added. The woman feels the movement of the "fetus" associated with increased peristalsis.
Diagnosis of false pregnancy
An objective examination of the patient can provide a number of valuable data, such as the degree of protrusion of the navel, the degree of development of subcutaneous fat. The diagnosis is usually made during a gynecological examination. In patients with false pregnancy, objective changes in the genital organs, such as cyanosis of the cervix and vagina, enlargement and softening of the uterus, are not detected.
Modern possibilities of pregnancy detection make it possible to reliably exclude a true pregnancy. To confirm the diagnosis, a woman is prescribed:
- ultrasound examination;
Fetal ultrasound according to indications (before the 20th week)
Additional ultrasound, which is prescribed in the presence of concomitant pathologies to monitor the condition of the fetus.
RUB 2,540 Sign up
Human chorionic gonadotropin (hCG, beta-hCG, b-hCG, Human Chorionic)
Synonyms: Beta-hCG general. Human Chorionic Gonadotropin; hCG; Pregnancy Quantitative hCG; Beta hCG; Total beta hCG. Brief description of the analyte Human Chorionic Gonadotropin. ..
..
Up to 1 business day
Available with home visit
RUB 685
Add to cart
Plain X-ray of the abdominal organs
X-ray examination that allows to detect pathological changes in the abdominal cavity, including foreign bodies and neoplasms.
RUB 2,440 Sign up
Differential diagnosis in pseudopregnancy is carried out with simulated pregnancy, missed pregnancy, ectopic pregnancy, tumor processes in the pelvic region.
Which doctors to contact
To confirm pregnancy, a woman usually goes to gynecologist. If endocrine disorders are suspected in a patient with a false pregnancy, a gynecologist-endocrinologist or endocrinologist.
If endocrine disorders are suspected in a patient with a false pregnancy, a gynecologist-endocrinologist or endocrinologist.
In the event that a woman stubbornly refuses to believe in a false pregnancy and inadequately perceives reality, she needs the help of a psychologist or psychotherapist.
Treatment of false pregnancy
As a rule, the condition of false pregnancy does not require special treatment. In most cases, to eliminate imaginary sensations, a competent and sympathetic explanation of the situation by a gynecologist, as well as understanding and support from close people, is sufficient. In the absence of self-hypnosis, the woman's menstrual cycle is restored, and the symptoms of toxicosis and other signs of pregnancy also disappear.
If a woman is diagnosed with a depressive disorder, drugs are prescribed that increase the formation and release of dopamine. Normalization of dopamine levels leads to adequate work of the adrenal glands, a decrease in the excessive activity of the sympathetic nervous system.
If a false pregnancy manifested itself in hormone-secreting tumors, hypothyroidism, alcoholic liver disease, cholecystitis, urinary tract infections, etc., then these pathologies are treated. It is necessary to identify the causes of psychogenic and neuroendocrine disorders, possible mental illnesses. In this case, the woman needs psychiatric treatment. Psychotherapy, pharmacotherapy with antidepressants or antipsychotics, hormonal therapy, and uterine curettage are sometimes needed as treatment. As a rule, after treatment, the state of false pregnancy in women no longer occurs.
It happens that a false pregnancy is caused on purpose - for example, if the uterus or mammary glands are underdeveloped. In this case, the woman is prescribed a certain dose of estrogens and progestins for 8-12 weeks. In order for the therapeutic effect to persist for a long time, an ointment is used, which includes progesterone and estradiol.
Complications
False pregnancy syndrome can lead to pathological hyperprolactinemia. It has been shown that the symptoms of false pregnancy are caused by the secretion of prolactin with a simultaneous decrease in the secretion of luteinizing hormone and an increase in follicle-stimulating hormone. Perhaps hormonal disorders in some women can serve as a background for the development of mental disorders.
It has been shown that the symptoms of false pregnancy are caused by the secretion of prolactin with a simultaneous decrease in the secretion of luteinizing hormone and an increase in follicle-stimulating hormone. Perhaps hormonal disorders in some women can serve as a background for the development of mental disorders.
Sometimes it is extremely difficult to convince a woman that she is not pregnant. Psychopathic personalities can live in this delusion for years. In women with neurosis-like reactions and mental disorders, the news of a false pregnancy can cause depression and suicidal thoughts.
Prevention of false pregnancy
Due to the fact that the causes of false pregnancy are not well understood, it is not possible to prevent its development.
Sources:
- Clinical guidelines "Hyperprolactinemia". Developed by: Russian Association of Endocrinologists. – 2016.
- Sholokhova V.R. Pathology of pseudocyesis as a psychosomatic disorder / V.
 R. Sholokhova, O.V. Minaev. // Medicine: today's challenges: materials of the IV Intern. scientific conf. (Moscow, November 2017). - Moscow: Buki-Vedi, 2017. - S. 64-68.
R. Sholokhova, O.V. Minaev. // Medicine: today's challenges: materials of the IV Intern. scientific conf. (Moscow, November 2017). - Moscow: Buki-Vedi, 2017. - S. 64-68. - Tarin et al. Endocrinology and physiology of pseudocyesis (Review). Reproductive Biology and Endocrinology 2013, 11:39.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
Allergies
4480 November 16
-
Kaposi's sarcoma
23128 15th of November
-
Symptoms of coronavirus disease: what has changed?
1911 November 14
Show more
Hypervitaminosis D
Hypervitaminosis A
Anemia
Dysbacteriosis
Malabsorption syndrome
Celiac disease
Lactase deficiency
Cystic fibrosis
Toxicosis
Preeclampsia
Fetal hypoxia
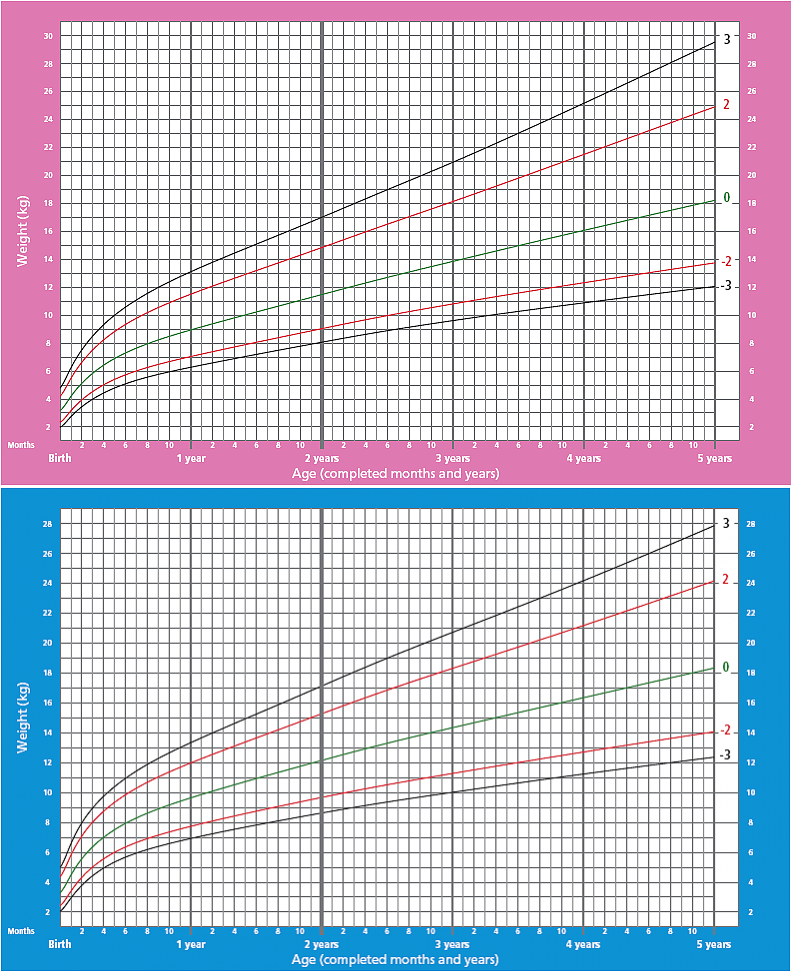
Underweight
Hypotrophy (protein-energy malnutrition (PEM))
Hypotrophy: causes, symptoms, diagnosis and treatment.
More
Diabetes mellitus
Pancreatitis
Hypercholesterolemia
Diabetes mellitus type II (Insulin-dependent DM, Type 2 Diabetes)
Diabetes mellitus type II: causes, symptoms, diagnosis and treatment.
More
Omphalocele
Embryonic hernia
Umbilical hernia
Umbilical hernia: causes, symptoms, diagnosis and treatment.
More
Allergy
Worms
Vomiting
Jaundice
Hepatitis
Iron deficiency
Helminthiasis
Helminthiasis (worm infestation): causes, symptoms, diagnosis and treatment.