Neural tube closure week
Closing of the neural tube
As you enter week 5 of your pregnancy you can be assured that although your baby is only fractionally larger than a sesame seed, its growth and development are taking place at an incredibly rapid rate.
Important landmarks at this stage include the emergence of the child’s facial features, the first pumping of the tiny heart, and the “budding” of your child’s arms and legs. Soon your child will begin to look less like a tadpole and more like what it is – a miniature, emerging human.
The importance of the neural tube
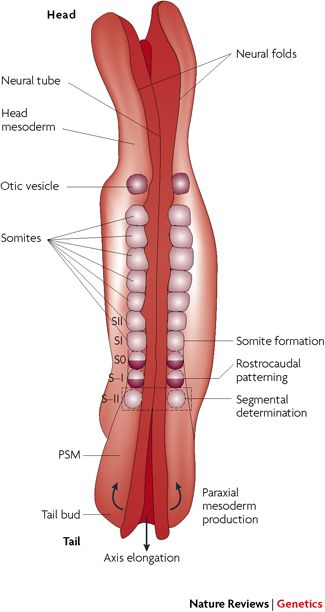
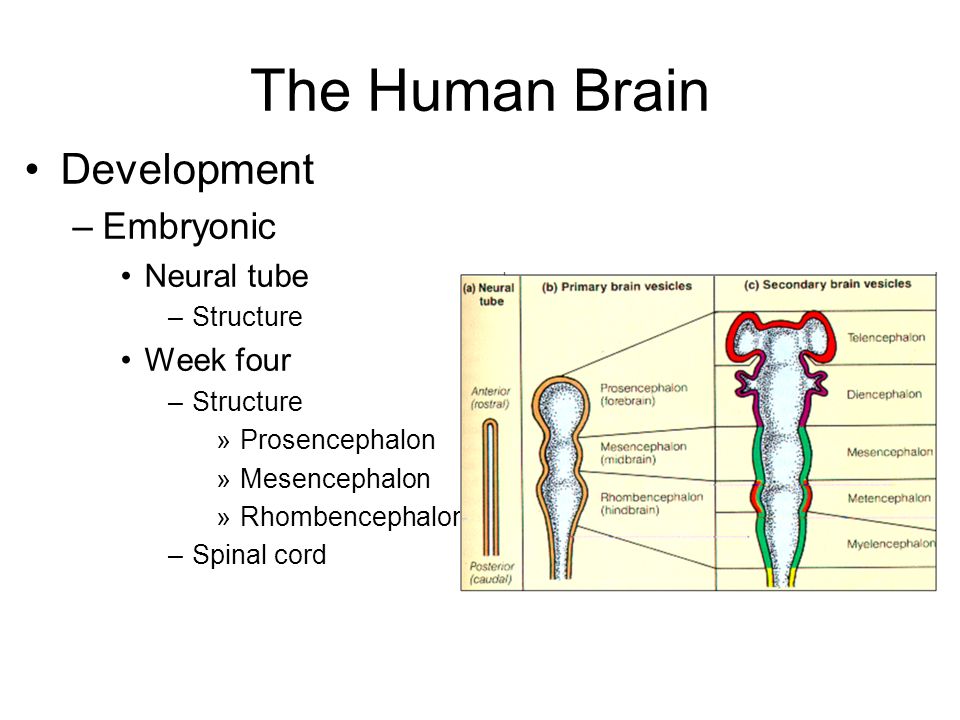
The neural tube is a hollow structure of tissue which later develops into the brain, spinal cord and nervous system. At week 5, the neural tube begins to close, forging the way for communication between spine and brain. There are four stages of neural tube subdivisions that occur in the creation of the nervous system. These take place in the prosencephalon, the mesencephalon, the rhombencephalon, and the spinal cord. Once these have all been achieved your baby will have a brain, a spine, and a spinal cord.
Neural tube defects
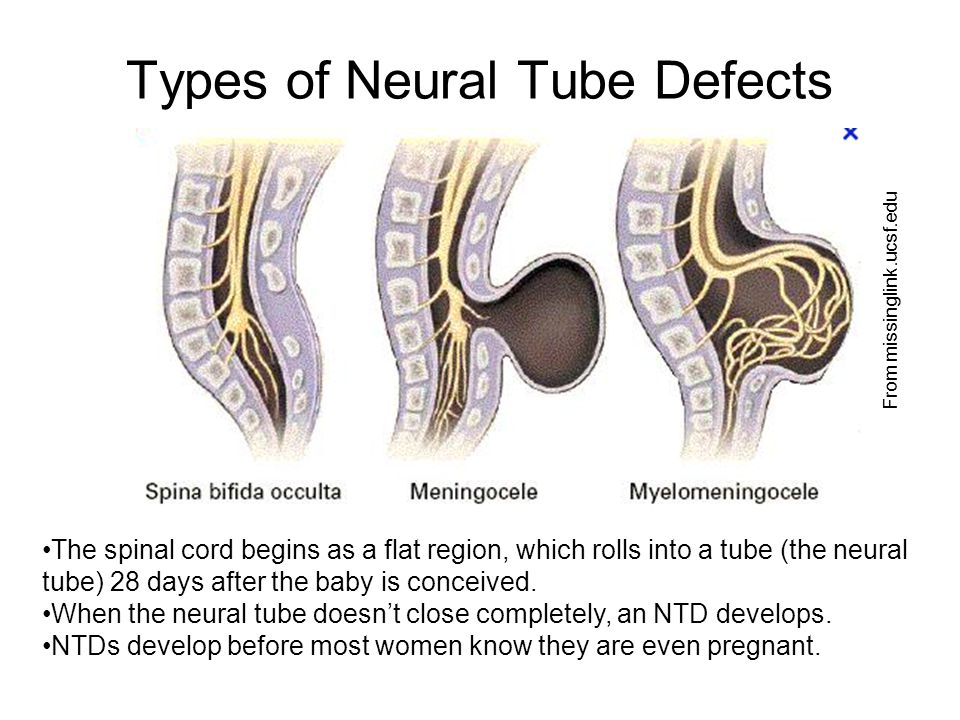
If there are problems with the development of the neural tube, this can result in defects affecting the brain, spine, or spinal cord. The majority of these occur during the first four or five weeks of pregnancy and may be very serious or even life-threatening. The following are the most common neural tube defects:
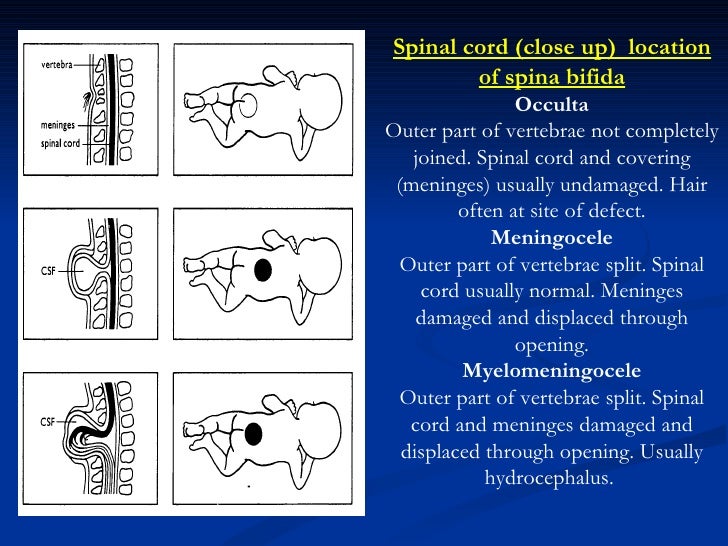
- Spina bifida – occurs as a result of a fault in the spinal cord and surrounding bones leaving a gap in the spine. Spina bifida literally means “split spine”.
- Anencephaly – a defect in which the baby is born with portions missing from its brain and/or skull
- Occult spinal dysraphism – describes a group of congenital and pathological changes affecting the development of the spine and spinal cord
- Encephalocele – also known as cranium bifidum, this condition results in protrusions of the brain and its membranes through openings in the skull
Risk
If you, your partner, or a member of either of your families has a neural defect, you are likely to be at increased risk of having a child with the same or a related condition.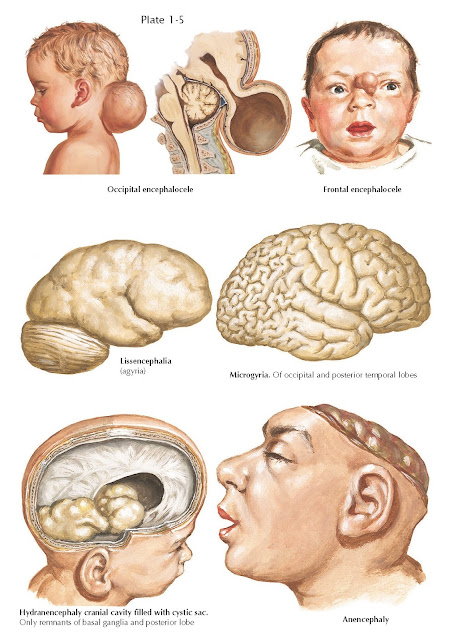 Additionally, you are at increased risk if you have previously had a child with a neural defect, are obese, or if you suffer from insulin dependent diabetes. Another notable risk factor is if you take anti-epileptic medications, particularly those that contain valproic acid or sodium valproate.
Additionally, you are at increased risk if you have previously had a child with a neural defect, are obese, or if you suffer from insulin dependent diabetes. Another notable risk factor is if you take anti-epileptic medications, particularly those that contain valproic acid or sodium valproate.
However, even if you have a family history of neural tube defects or are affected by other risk factors, the chance of having a child with some form of neural tube defect remains relatively low, while for general members of the population, the risk of such a defect stands at less than one in 1,000.
About two-thirds of neural tube defects can be prevented if you eat enough folate (folic acid) before and during the first three months of pregnancy.
Detection
In some cases neural tube defects may be detected during your routine ultrasound scan at around 12 weeks. However, they are more likely to be evident later on in your pregnancy, so are more likely to be detected during your mid-pregnancy anomaly scan which typically takes place between week 18 and week 21 of your pregnancy.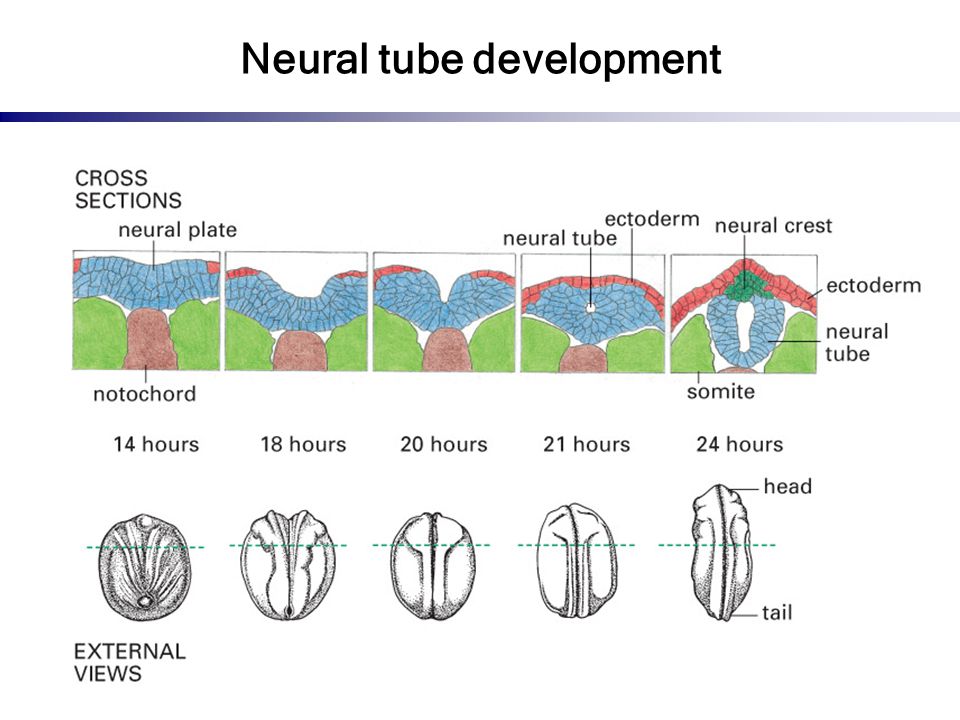 Although not all neural tube defects are detected by the anomaly scan, most are – for example, around 9 in 10 cases of spina bifida are detected.
Although not all neural tube defects are detected by the anomaly scan, most are – for example, around 9 in 10 cases of spina bifida are detected.
Occasionally you may need the anomaly scan to be repeated, either because the scan does not present a clear enough picture of your baby’s health or because the sonographer believes it is in your best interests to be referred to a specialist.
The benefits of folic acid
It is accepted by most agencies that folic acid (also called vitamin B9 as well as “folate” when in its non-synthesised state) can significantly reduce a woman’s chances of having a child with a neural tube defect.
In fact, the Department of Health recommends that women who are trying to become pregnant should take a daily supplement of 400 micrograms of folic acid and, once pregnant, should continue on this dosage for 12 weeks.
Women at increased risk of having a child with a neural tube defect should take a slightly higher dose of folic acid: 500 micrograms daily.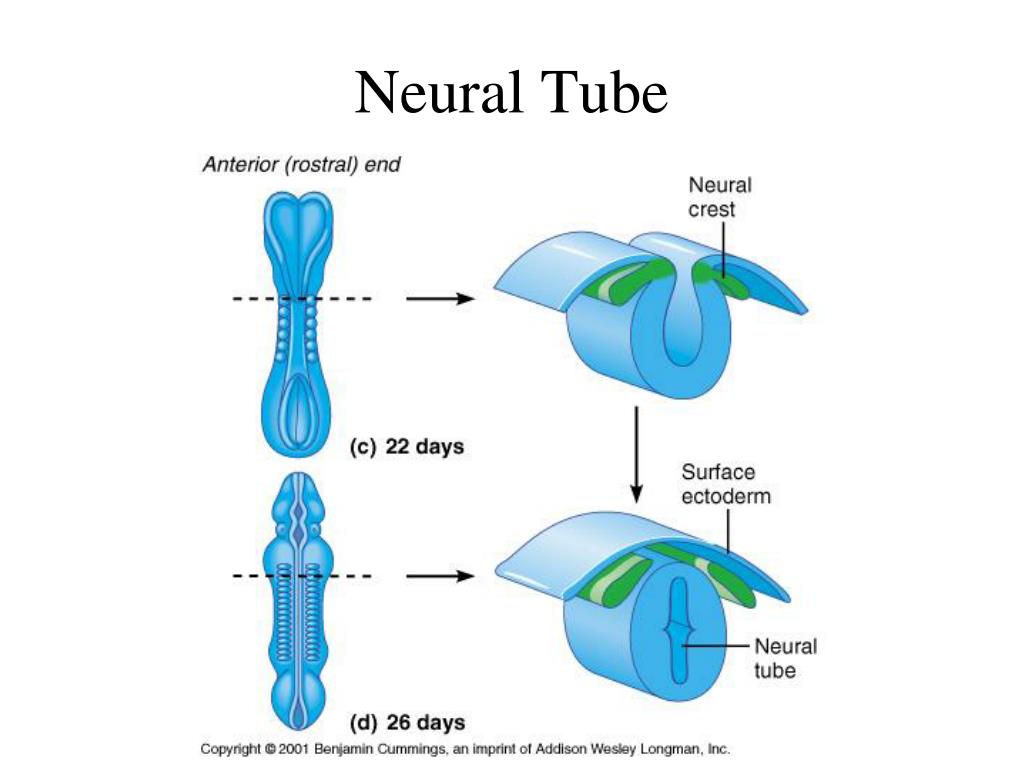
It is fine if you have become pregnant without taking folic acid in the pre-conception period – just begin to take it once you are pregnant.
Although there are no official guidelines recommending that mothers-to-be continue to take folic acid, throughout the whole pregnancy, there is not thought to be any harm in continuing to take a B9 supplement.
It is advisable that all women of child-bearing age take a folic acid supplement just in case they become unexpectedly pregnant.
Important – If you or your child are unwell you should seek medical advice from a professional – contact your GP or visit an A&E department in an emergency. While My BabyManual strives to provide dependable and trusted information on pregnancy and childcare 24/7 via our website pages, we cannot provide individual answers to specific healthcare questions.
What They Are, Causes & Prevention
Overview
Neural tube defects (NTDs) happen to developing fetuses within the first month of pregnancy.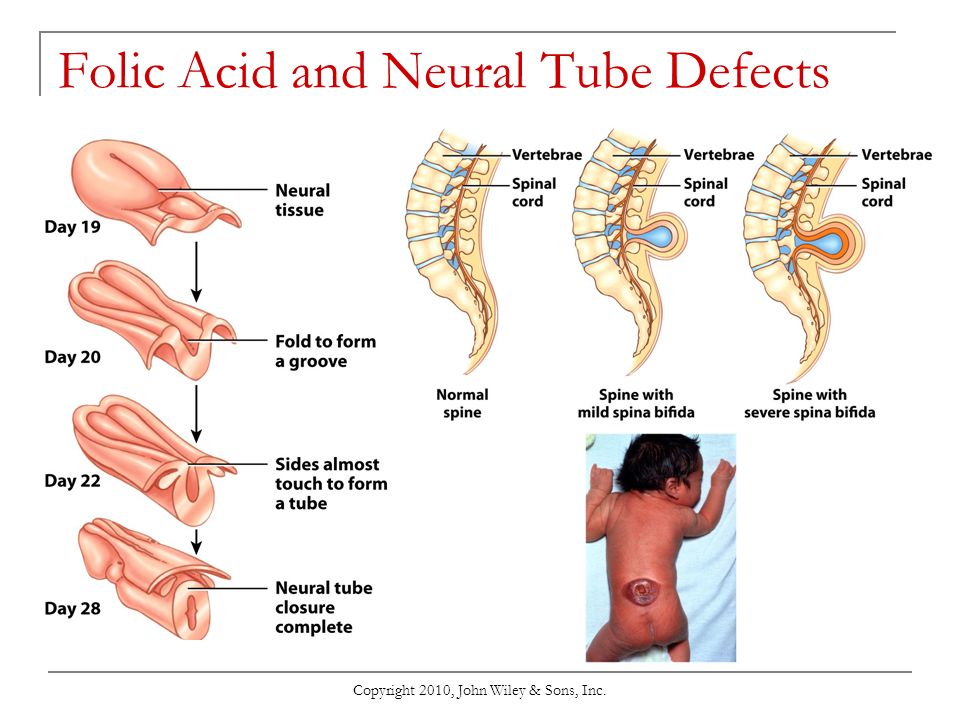 An NTD happens when the neural tube doesn’t close completely somewhere along its length.
An NTD happens when the neural tube doesn’t close completely somewhere along its length.What is a neural tube defect?
Neural tube defects (NTDs) are birth defects (congenital conditions) of the brain, spine or spinal cord. They happen to developing fetuses within the first month of pregnancy — often before you even know you’re pregnant. The two most common neural tube defects are spina bifida and anencephaly.
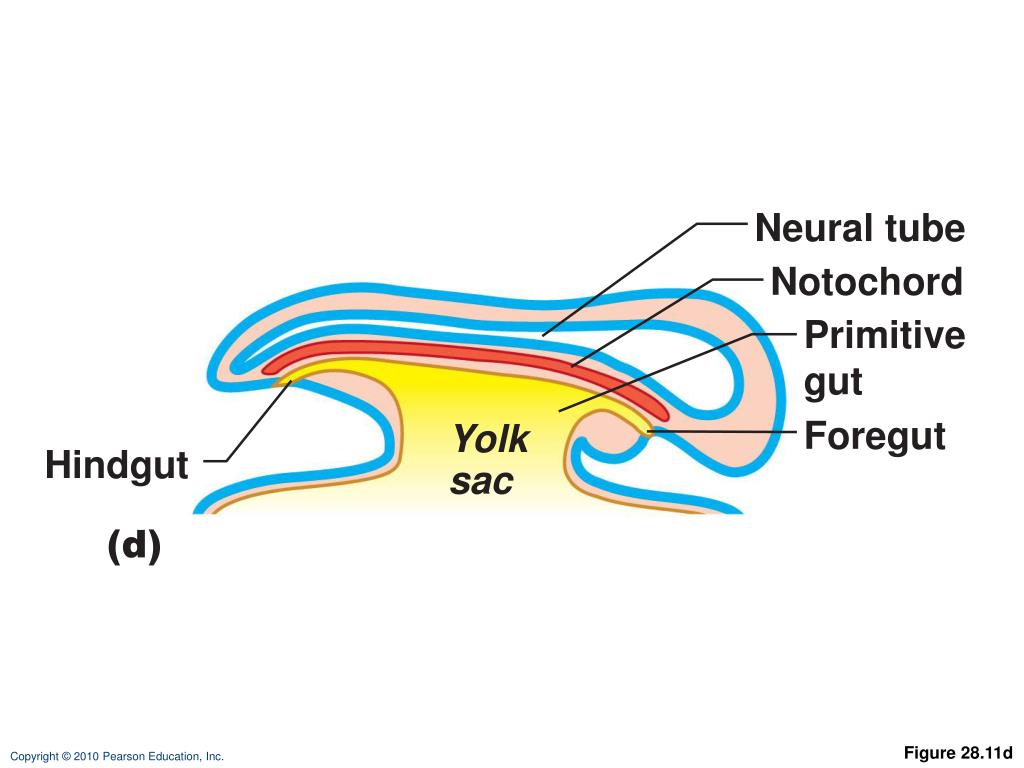
Normally, during your first month of pregnancy, the two sides of the fetus's spine (backbone) join together to cover and protect the spinal cord, spinal nerves and meninges (the tissues covering the spinal cord). At this point, the developing brain and spine are called the neural tube.
As development progresses, the top of the neural tube becomes the brain, and the rest of the tube becomes the spinal cord. An NTD happens when this tube doesn’t close completely somewhere along its length.
What are the types of neural tube defects (NTDs)?
There are several types of neural tube defects, including:
- Spina bifida.
- Anencephaly.
- Encephalocele.
- Iniencephaly.
Spina bifida
Spina bifida is the most common type of neural tube defect (NTD). It happens when the neural tube doesn’t close completely somewhere along the spine during fetal development.
There are a few different types of spina bifida, including:
- Myelomeningocele (open spina bifida): This NTD is characterized by incomplete neural tube closure and a fluid-filled sac that protrudes (sticks out) from your baby’s back. The sac contains part of their spinal cord, meninges, nerves and cerebrospinal fluid (CSF). Myelomeningocele is the most severe and the most common form of spina bifida.
- Meningocele: This NTD is characterized by a sac of fluid that protrudes through an opening in your baby’s back, but their spinal cord is not involved or damaged.
- Spina bifida occulta: This NTD is characterized by a small gap in your baby’s spine, but there isn’t an opening or sac on their back.
 Their nerves and spinal cord aren’t damaged, and the condition usually doesn’t cause any disability. This is the mildest form of spina bifida.
Their nerves and spinal cord aren’t damaged, and the condition usually doesn’t cause any disability. This is the mildest form of spina bifida.
Anencephaly
Anencephaly happens when the fetus's neural tube doesn’t close at the top during fetal development. This causes the skull, scalp and brain not to develop properly, and portions of the brain and skull are missing. The brain tissue that does form is usually exposed because there isn’t enough skin and bone to cover it. Infants with anencephaly are either stillborn or die soon after birth.
Encephalocele
Encephalocele happens when the neural tube doesn’t close near the brain, and there’s an opening in the skull. The fetus's brain and the membranes that cover it can protrude through the skull, forming a sac-like bulge. In some cases, there’s only a small opening in the nasal cavity or forehead area that’s not noticeable.
Iniencephaly
Iniencephaly happens when the spine is severely malformed (misshapen). It often causes a lack of a neck, and your baby’s head is bent severely backward. The skin of your baby’s face is connected to their chest, and their scalp is connected to their back. Babies with iniencephaly are usually stillborn.
It often causes a lack of a neck, and your baby’s head is bent severely backward. The skin of your baby’s face is connected to their chest, and their scalp is connected to their back. Babies with iniencephaly are usually stillborn.
Who do neural tube defects affect?
Neural tube defects (NTDs) are birth defects (congenital conditions), so they develop in fetuses. NTDs develop within the first month of pregnancy.
How common are neural tube defects?
Neural tube defects (NTDs) occur in about 3,000 pregnancies each year in the United States. To put that into perspective, there were approximately 3,605,000 births in the U.S. in 2020.
The two most common NTDs are spina bifida and anencephaly. Spina bifida affects about 1,500 babies a year in the U.S., with myelomeningocele being the most common form. Anencephaly affects about 1,000 babies each year in the U.S.
Encephalocele and iniencephaly are both rare NTDs.
Symptoms and Causes
What causes neural tube defects (NTDs)?
Healthcare providers and scientists don’t yet know the exact cause of neural tube defects (NTDs), but they believe it’s a complex combination of genetic, nutritional and environmental factors.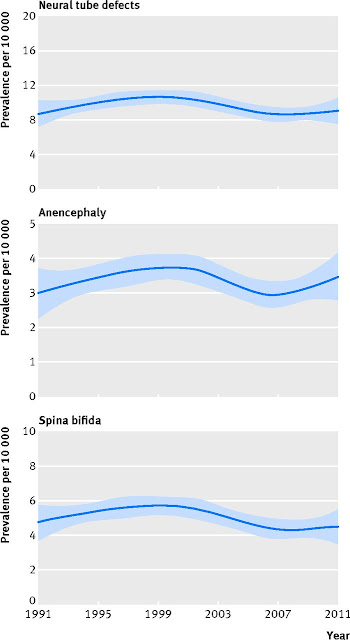
In particular, low levels of folic acid in a person’s body before and during early pregnancy appear to play a part in this type of congenital condition. Folic acid (or folate) is important for the fetal development of the brain and spinal cord.
What are the symptoms of neural tube defects (NTDs)?
Each type of neural tube defect (NTD) has different symptoms.
Some babies with NTDs have no symptoms, while others experience serious disabilities. Babies with iniencephaly and anencephaly are typically stillborn or die shortly after birth due to complications from the defect.
General symptoms of NTDs can include:
- Physical problems, such as paralysis and urinary and bowel control issues.
- Blindness.
- Deafness.
- Intellectual disability.
- Lack of consciousness and, in some cases, death.
If your healthcare provider suspects that the fetus you're carrying has a neural tube defect, your medical team will be able to provide more information about what to expect.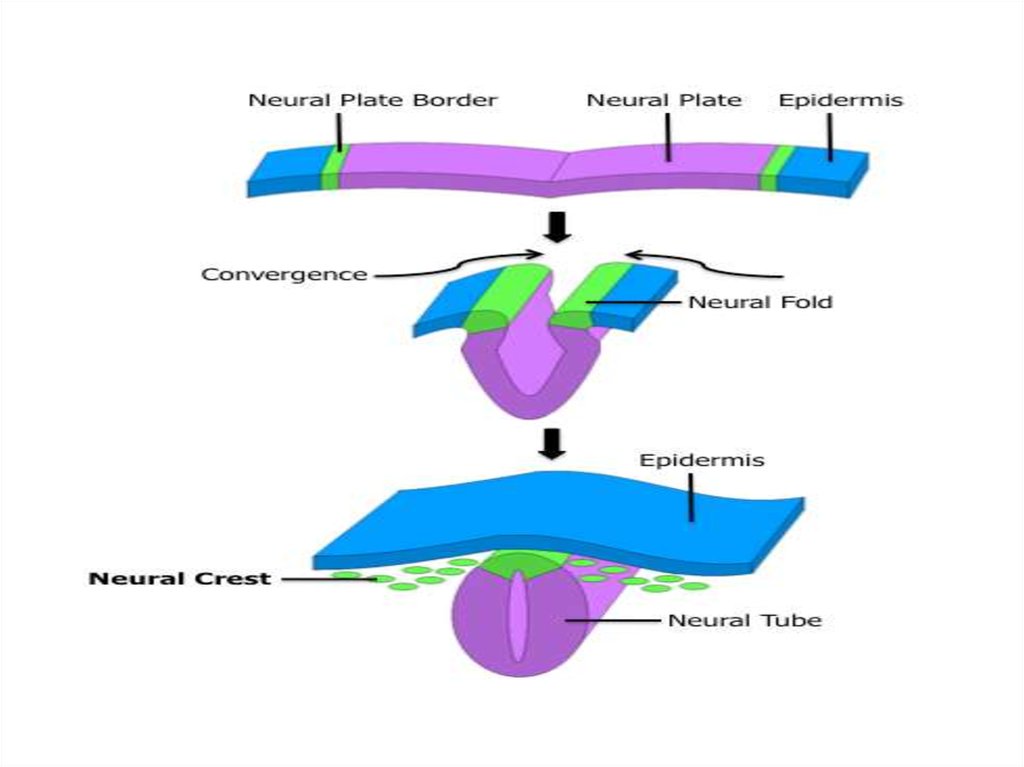 NTDs affect each baby differently.
NTDs affect each baby differently.
What are the signs of neural tube defects (NTDs) during pregnancy?
If you’re pregnant with a fetus that has a neural tube defect (NTD), you won’t experience any symptoms directly related to it.
When you undergo a fetal ultrasound, your healthcare provider will look for certain signs of the fetus's health and development depending on its fetal age, including looking for signs of NTDs in the spine and head. Healthcare providers can usually diagnose NTDs with an ultrasound.
Diagnosis and Tests
How are neural tube defects (NTDs) diagnosed?
Healthcare providers typically diagnose neural tube defects (NTDs) during pregnancy through prenatal tests, such as ultrasound.
What tests will be done to diagnose neural tube defects (NTDs)?
Healthcare providers use the following tests to help diagnose neural tube defects (NTDs) before birth:
- Blood test: Your healthcare provider will order a screening test that measures the amount of alpha-fetoprotein (AFP) in your blood during the 16th to 18th week of pregnancy.
 The amount is higher than normal in about 75% to 80% of pregnant people who are carrying a fetus with an NTD. If your level is elevated, your healthcare provider will order other tests, such as an ultrasound, to better evaluate the growing fetus.
The amount is higher than normal in about 75% to 80% of pregnant people who are carrying a fetus with an NTD. If your level is elevated, your healthcare provider will order other tests, such as an ultrasound, to better evaluate the growing fetus. - Fetal (prenatal) ultrasound: An ultrasound during pregnancy is the most accurate method to diagnose several NTDs. Healthcare providers typically recommend ultrasounds during the first trimester (11 to 14 weeks of pregnancy) and second trimester (18 to 22 weeks of pregnancy).
- Amniocentesis: Healthcare providers use this test to check for NTDs and other birth defects. During amniocentesis, they use a needle to remove a sample of fluid from the amniotic sac that surrounds te fetus. You can get this test at 15 to 20 weeks of pregnancy. This test carries certain risks. Be sure to talk to your healthcare provider about the process.
Healthcare providers also use imaging tests, such as an MRI (magnetic resonance imaging) or CT (computed tomography) scan, to diagnose some NTDs after birth.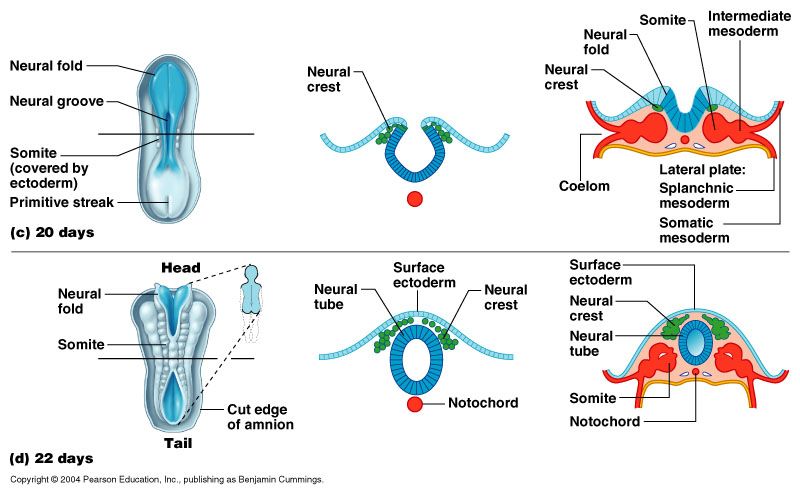
Management and Treatment
How are neural tube defects (NTDs) treated?
There are several treatment options for spina bifida and encephalocele depending on the severity of the condition.
There isn’t a treatment for anencephaly or iniencephaly. Infants with these conditions are typically stillborn or die shortly after birth.
Treatment for spina bifida and encephalocele
Treatment for both spina bifida and encephalocele depends on the severity of the condition and if your baby has other complications. Surgery is a common option for both conditions.
Healthcare providers typically treat encephalocele with surgery to place the protruding part of your baby’s brain and the membranes covering it back into their skull. They then close the opening in your baby’s skull.
Treatment for myelomeningocele, the most common form of spina bifida, typically involves surgery to repair the opening in your baby’s spine. Healthcare providers can perform surgery before birth (fetal surgery) or shortly after birth (postnatal surgery).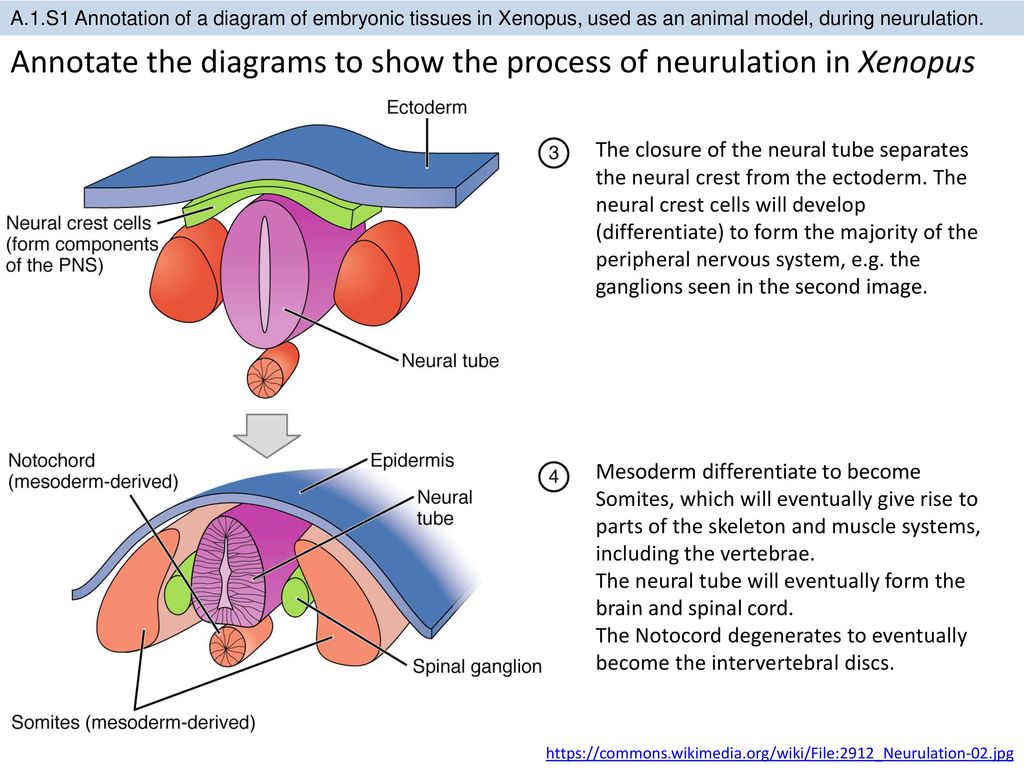
Long-term treatment for both conditions depends on your child’s condition. They may need multiple surgeries over time and other treatments related to complications, such as a shunt to treat hydrocephalus (excess fluid surrounding their brain).
Prevention
What are the risk factors for developing a neural tube defect (NTD)?
Any person can have a baby with a neural tube defect (NTD). But certain factors make you more likely to have a baby with an NTD, including:
- Folate (folic acid) deficiency: Folate, the natural form of vitamin B-9, is important for healthy fetal development. A folate deficiency before and during pregnancy increases the risk of having a baby with spina bifida and other NTDs. If you’re pregnant or thinking of becoming pregnant, it’s important to take prenatal vitamins to ensure you’re getting enough folate (folic acid) and other nutrients to support a healthy pregnancy. The Centers for Disease Control and Prevention (CDC) recommends all people who can become pregnant take 400 micrograms (mcg) of folic acid every day, in addition to eating food with folate, to help prevent NTDs.

- Family history of neural tube defects: People who’ve had one baby with an NTD have a 2% to 3% increased risk of having a second baby with an NTD. To learn more about your risk of having a baby with an NTD, consider seeing a genetic counselor.
- Certain antiseizure medications: These medications are linked to neural tube defects when taken during pregnancy. If you take medicine to prevent seizures, talk to your healthcare provider before you get pregnant about how the medicine may affect your pregnancy.
- Diabetes: People with poorly managed diabetes who are pregnant have a higher risk of having a baby with an NTD.
- Obesity: People who have obesity before pregnancy have an increased risk of having a baby with an NTD.
- Increased body temperature in early pregnancy: Increases in core body temperature (hyperthermia) in the early weeks of pregnancy due to a prolonged fever or use of a sauna or hot tub have been associated with a slightly increased risk of NTDs.
- Opioid use in early pregnancy: Opioids are a class of very powerful and highly addictive drugs that reduce pain. People who are pregnant and who’ve taken opioids in the first two months of pregnancy have an increased chance of having a baby with an NTD, in addition to other complications. If you’re pregnant and taking any drugs or medications that may be an opioid, tell your healthcare provider right away.
Outlook / Prognosis
Can a baby live with a neural tube defect?
Yes, your baby can live with certain neural tube defects, including spina bifida and encephalocele.
Babies with anencephaly and iniencephaly are typically stillborn or die shortly after birth, however.
What is the prognosis (outlook) for neural tube defects (NTDs)?
For babies with spina bifida, especially myelomeningocele, or encephalocele, there’s a high likelihood of nerve damage, which can cause paralysis and other issues. The nerve damage and loss of function that are present at birth are usually permanent.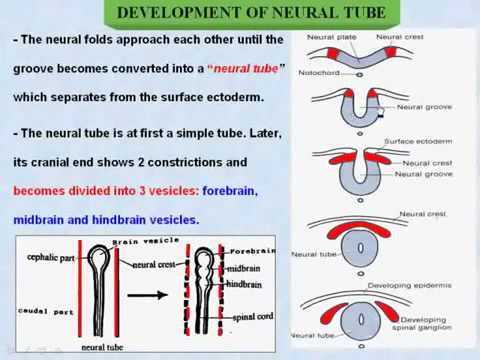 But there are a number of treatments that can sometimes prevent further damage and help with complications.
But there are a number of treatments that can sometimes prevent further damage and help with complications.
Some babies with spina bifida have no or minimal complications.
Living With
How do I take care of my baby with a neural tube defect?
It’s important to remember that no two people with a neural tube defect (NTD), especially spina bifida and encephalocele, are affected in the same way. It’s impossible to predict how your baby will be affected. The best way you can prepare is to talk to healthcare providers who specialize in researching and treating your baby’s condition.
As they grow, your child may benefit from a team of healthcare providers who can care for their needs. It’s important to advocate for your child and to arrange the best medical care possible.
When should I see my healthcare provider about neural tube defects (NTDs)?
If your child was born with a neural tube defect (NTD), they’ll likely need to see their healthcare provider — or team of healthcare providers — regularly throughout their life.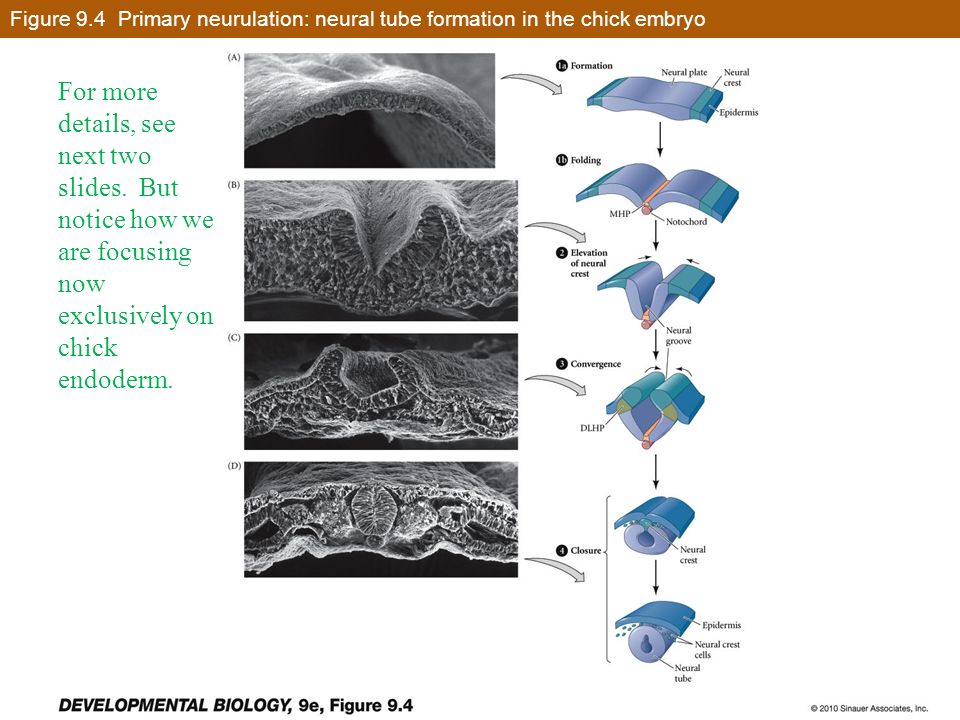
If you take antiseizure medication or opioids, it’s important to talk to your healthcare provider before becoming pregnant about how these medications could affect your pregnancy and the likelihood of having a child with an NTD.
A note from Cleveland Clinic
Learning that the fetus you're carrying has a neural tube defect (NTD) is scary and overwhelming. But know that you’re not alone — many resources are available to help you and your family. It’s important that you speak with a healthcare provider who’s very familiar with neural tube defects so you can learn more about how your baby will be affected and how to prepare.
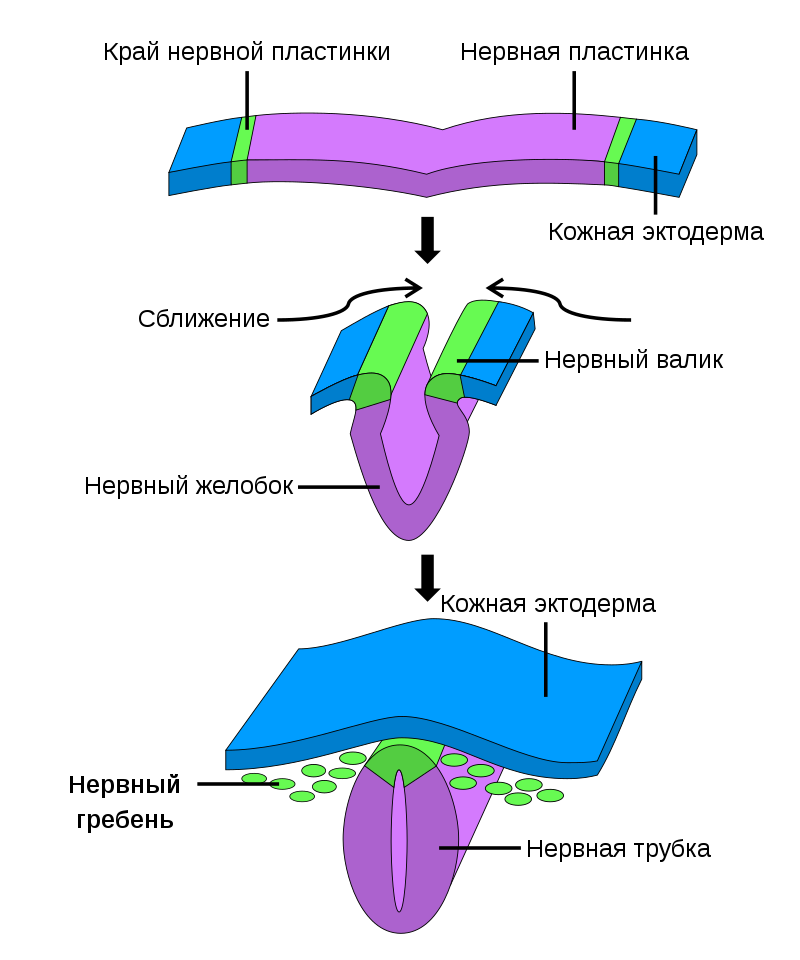
Neural tube formation process and malformations
The process of neural tube formation is called neurulation. Neurulation of begins with the appearance of the neural plate, which invaginates into the spine to form a neural network with neural grooves on either side of the spine.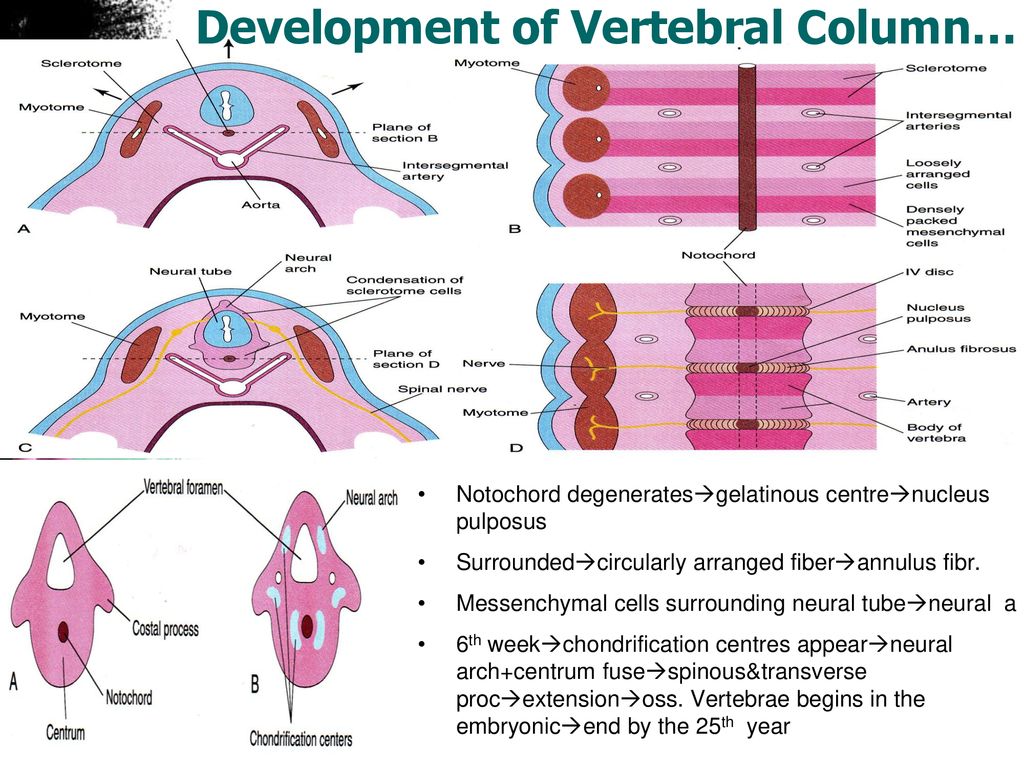 Gradually, the neural grooves approach each other along the midline of the spine and merge, thus transforming the neural grooves into a neural tube.
Gradually, the neural grooves approach each other along the midline of the spine and merge, thus transforming the neural grooves into a neural tube.
Formation of the neural tube begins in the region of the future neck at the level of the 4th somite (4 segments of the cervical spine). Neurulation begins 16 days after fertilization and ends on days 21-22. Neurulation in humans occurs in several stages. First, the dorsal section of the spine closes, then the closure occurs in the area from the forehead to the parietal tubercles, the third stage closes the facial section of the skull, then the section from the occipital lobes to the cervical spine, and the last stage closes the sacral section.
When neurulation is disturbed , congenital malformations are detected at the stages of neural tube closure, such as:
- anencephaly (congenital absence or underdevelopment of the brain and cerebellum),
- spina bifida - Spina Bifida,
- exencephaly (absence of skull bones)
and other defects of the central nervous system.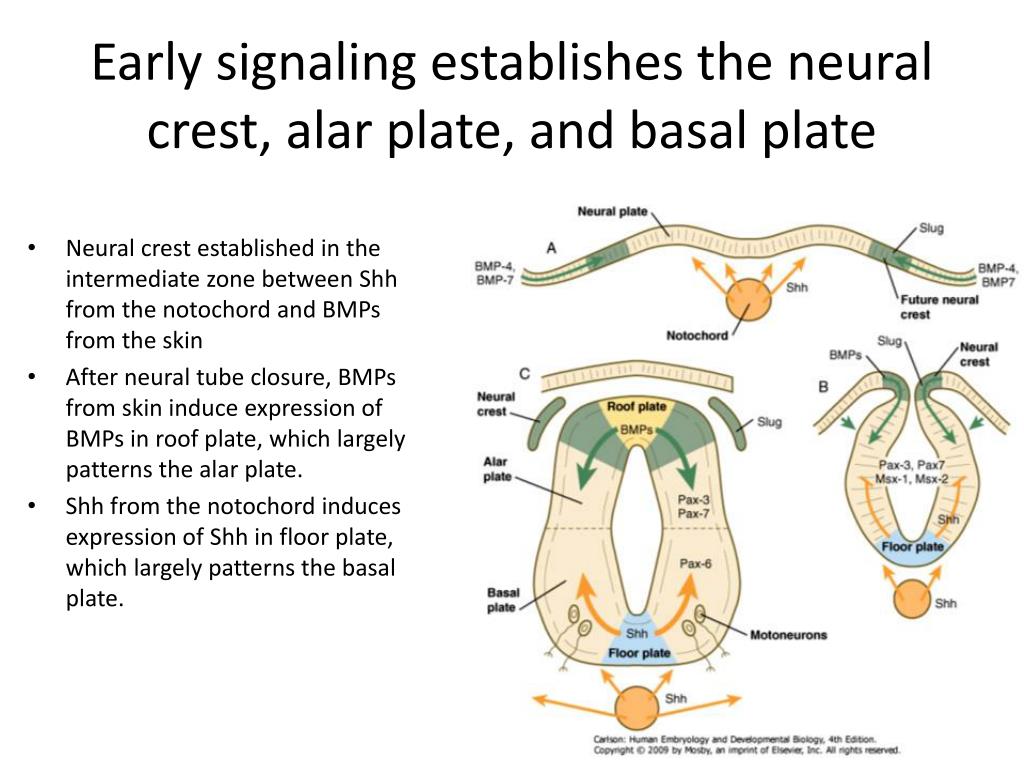 Neural tube closure defects are quite rare. With severe defects in the development of the neural tube, such as anencephaly, spina bifida, the fetus dies in the womb or is born non-viable and dies in the coming days after birth. Modern equipment helps to detect neural tube malformations at regular check-ups during pregnancy. With early diagnosis of malformations of the neural tube, termination of pregnancy is indicated.
Neural tube closure defects are quite rare. With severe defects in the development of the neural tube, such as anencephaly, spina bifida, the fetus dies in the womb or is born non-viable and dies in the coming days after birth. Modern equipment helps to detect neural tube malformations at regular check-ups during pregnancy. With early diagnosis of malformations of the neural tube, termination of pregnancy is indicated.
The formation of the human neural tube is a complex interaction between genetic and environmental factors. Some genes are important for neural tube formation, but dietary factors such as cholesterol and folic acid levels are also important for proper neural tube formation. Scientists have calculated that 50% of neural tube defects in the fetus can be prevented by prescribing folic acid and vitamin B12 to the pregnant woman.
WHO recommends that all women planning pregnancy and pregnant women take 400 micrograms of folic acid daily to reduce the risk of neural tube defects.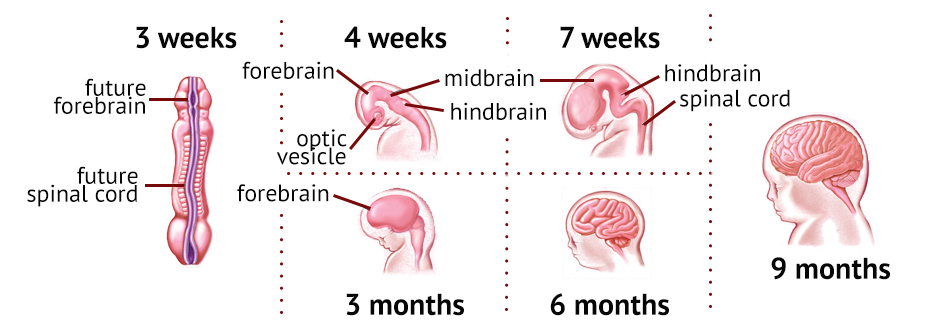
All information is for informational purposes only. If you have any health problems, you need to consult a specialist.
Read also
What is a genetic passport?
Importance of the HLA system in the management of couples in IVF programs
Quality of embryos in IVF
Genetic factors of miscarriage
How does the neural tube defect of the fetus manifest itself. Treatment of neural tube defects
Na 19 -22 day from conception starts take shape nervous a tube fetus - primary the form development nervous systems , including head and dorsal brain . open nervous a tube - this is platform for formation front , medium and rear bubble . If a violated process closing top department , develops anencephaly - absence head brain at fetus . If a there is violations in closing bottom parts nervous tubes , arises spinal hernia . Pathology incompatible With life , but to fortunately meet very rarely , y one fetus from thousands .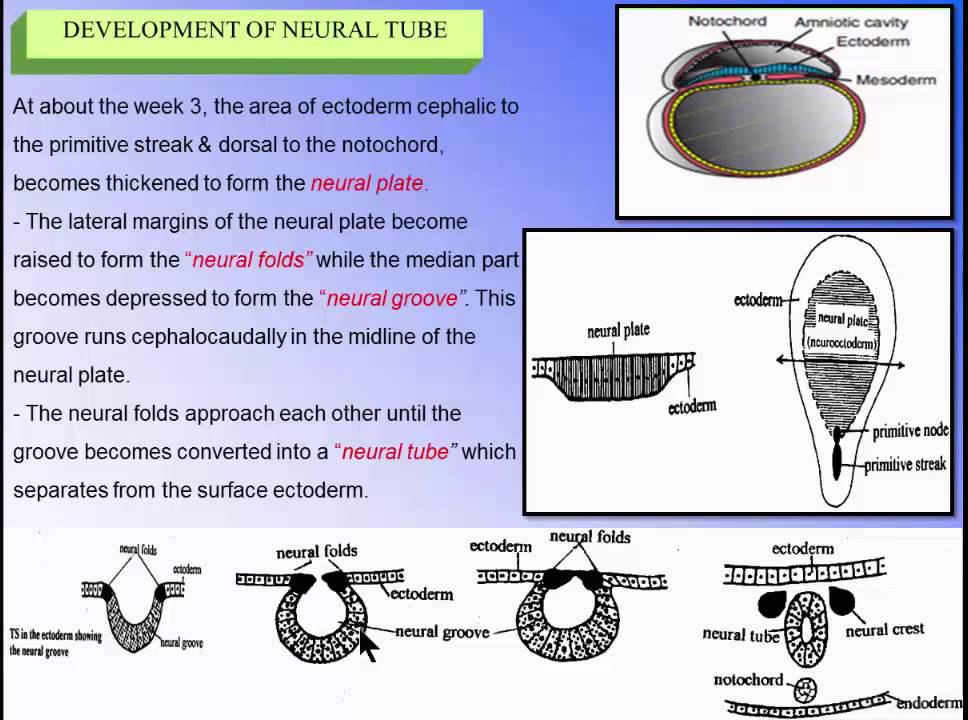
Pathologies nervous tubes not are diseases modernity provoked current conditions life . By records paleontologists defects development dorsal and head brain (wrong development skulls and spine ) were fixed at of people , which lived more 7000 years back .
First intelligence , from which on essence start develop neurosurgery , were marked in writings Hippocrates . Italian anatomist Morgagni batista one from first did approximate description similar pathologies . Of course , treatment defects not were subject to , because what the medicine was on the low level development .
Most widespread reasons vices development nervous tubes considered viral infections , irradiation received future mom in time treatment oncological diseases , other factors external environments (pesticides , oil products , synthetic fertilizer , GMO and t .d .). More often Total similar deviations meet at pregnant women , also have had like defect in history , then there is high risk provokes genetic predisposition .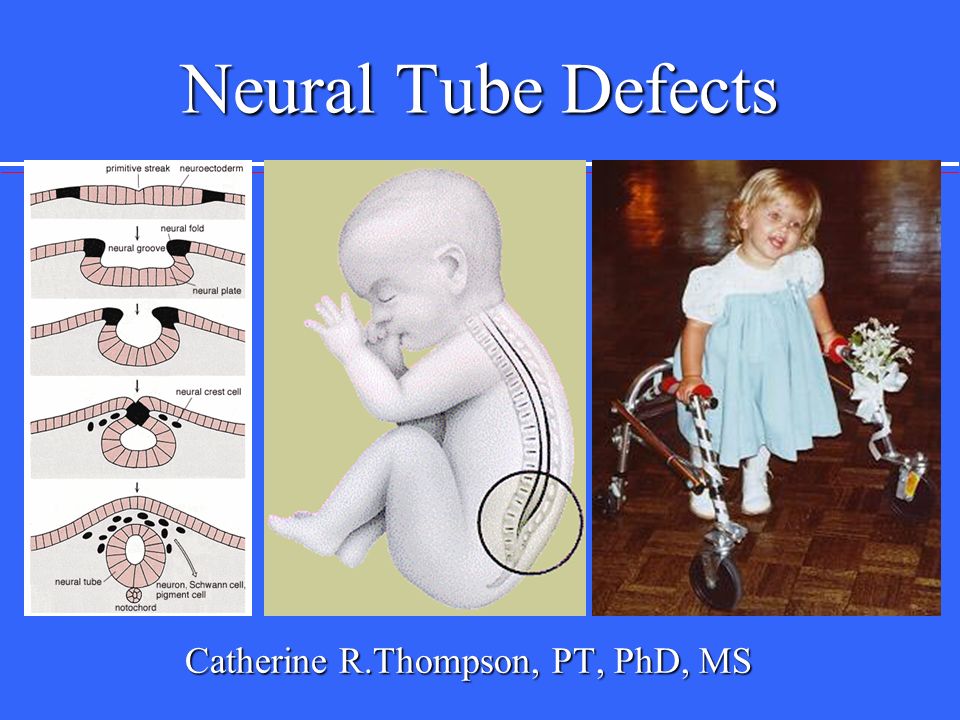
According to new research It was confirmed interesting fact - at women With excess weight body risk development defect nervous tubes at fetus in two times above , how at women With normal or lowered index masses body . Data formed on the basis stories diseases women California per period With 1989 on 1991 G .., AT which was discovered flaw nervous tubes fetus . At women With redundant weighing risk was promoted in 2 ,one times . Interesting , what on the received results no one way not influenced increase doses use folic acids , flaw which counts one from reasons development pathology . Gynecologists advise in period planning and before 12 –ty weeks pregnancy use daily 5 mg folic acids .
B progress embryogenesis on the first week formed germinal nodes . On the second week actively develop extra-embryonic parts . On the third week formed nervous a tube from special plates , then there is first 3 weeks is period primary neurulation .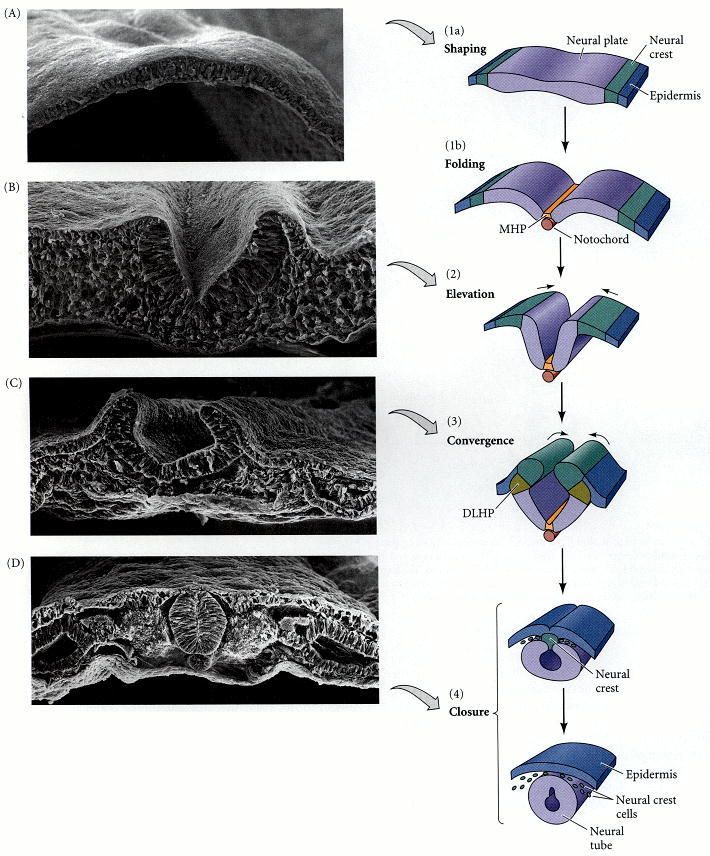 Secondary neurulation account for on the four -7 week pregnancy , in this period may arise violations – spinal dysraphia more often Total in form hernia lumbar -coccygeal department future spine . Exactly that's why preventive therapy must start off more before offensive pregnancy and continue in flow first trimester .
Secondary neurulation account for on the four -7 week pregnancy , in this period may arise violations – spinal dysraphia more often Total in form hernia lumbar -coccygeal department future spine . Exactly that's why preventive therapy must start off more before offensive pregnancy and continue in flow first trimester .
Diagnose problem can thanks to holding ultrasound , after confirmation diagnosis accepted solution about interruption pregnancy or , if degree violations allows , about bearing pregnancy and holding surgical intervention after childbirth . If a in time spend operation , then in most cases succeed fully reestablish integrity cerebral shells , then there is child after operations will be fine develop and live complete life .
Most frequent complication after removal hernia is purulently -inflammatory processes , they meet at 78 % small patients . Should Mark , what already through day after operations condition child normalizes and only 5 % of children all same remain under threat .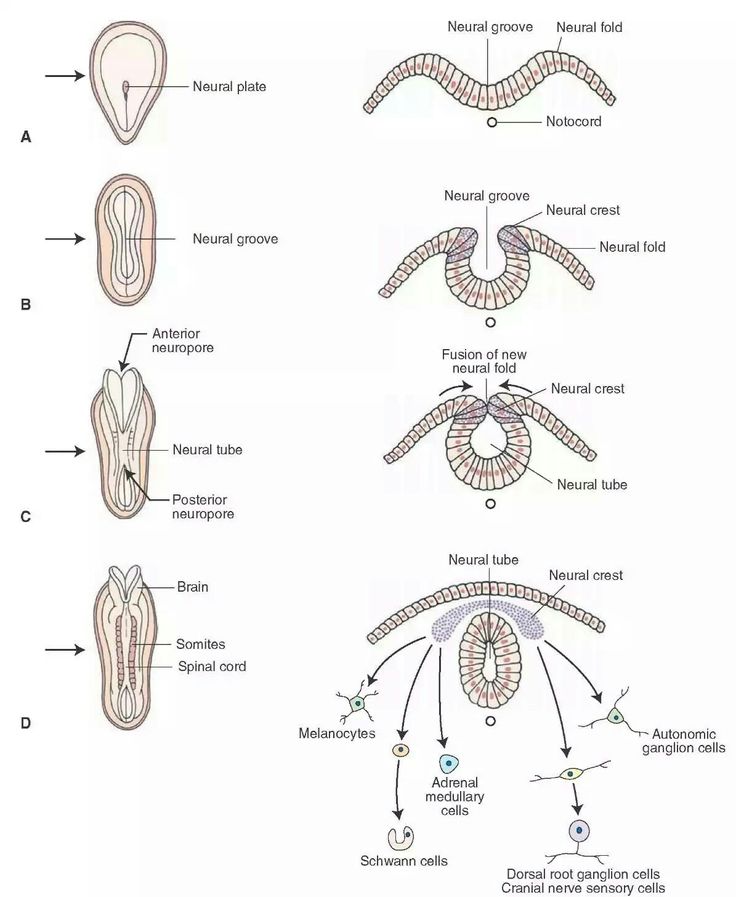
Based on extensive research, scientists have concluded that women who consume folic acid during the first 6-12 weeks of pregnancy, and ideally 1-2 months before conception, significantly reduce the likelihood of a number of fetal abnormalities. In particular, the probability of having a child with a neural tube defect is reduced by 70%.
Neural tube defects are referred to as problems with the development of the baby's brain, skull, and spinal cord, usually during the first 6 weeks of pregnancy.
At the very beginning of pregnancy, nature lays the foundation for the baby's spinal cord and brain. Cells of a certain type form along the back of the embryo at first something like a long groove, which then transforms into a hollow tube (the so-called "neural tube"). The neural tube closes between 21 and 28 days (or 3 to 4 weeks) after conception.
Normally, the brain and spinal cord grow and develop inside the neural tube. However, if the neural tube does not close completely, the previously mentioned defect or hole in the neural tube occurs.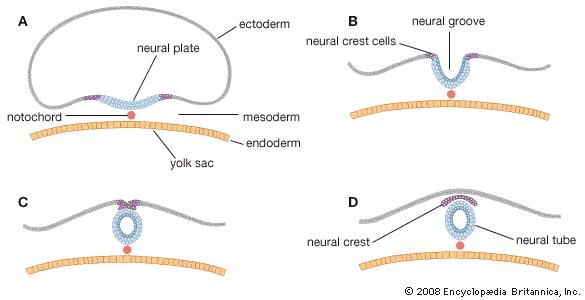 For some reason that is not fully understood, a low level of folic acid in a woman's body stimulates the onset of pathology, while sufficient can in most cases prevent it. Taking folic acid during the first weeks of pregnancy also helps prevent some other intrauterine anomalies, such as cleft lip or palate.
For some reason that is not fully understood, a low level of folic acid in a woman's body stimulates the onset of pathology, while sufficient can in most cases prevent it. Taking folic acid during the first weeks of pregnancy also helps prevent some other intrauterine anomalies, such as cleft lip or palate.
The causes of neural tube defects are not fully understood. However, the cases studied suggest that they are caused by a combination of genetic predispositions and environmental factors (eg folic acid deficiency in the mother's diet). Doctors pay close attention to this particular problem, because. it is widespread in many countries, and there is no direct dependence on geographical location or standard of living. For example, neural tube defects are more common in Northern Ireland and Scotland (4-6 per 1000) than in the south of England (less than 1 per 1000) in the UK, and are 6 times more common in the northern provinces of China (6 per 1000), according to compared with the southern provinces (1 per 1000). The United States recorded a relatively low rate - from 1 to 1.5 per 1000, as in Japan - less than 1 per 1000 births . New Zealand reports about 1.7 cases per 1000 (and much lower among the Maori people ). In Australia, the sad statistics is about 1.6-2 pathologies per 1000 births.
The United States recorded a relatively low rate - from 1 to 1.5 per 1000, as in Japan - less than 1 per 1000 births . New Zealand reports about 1.7 cases per 1000 (and much lower among the Maori people ). In Australia, the sad statistics is about 1.6-2 pathologies per 1000 births.
For a woman whose previous child had a neural tube defect, the chance of a subsequent child having a neural tube defect is 5%. The risk also increases for the expectant mother, among whose relatives there were similar cases.
The risk of having a baby with a neural tube defect is also serious for insulin-dependent diabetic women and for women taking certain medications that interfere with folic acid absorption. These drugs include drugs that control epileptic seizures and prevent malaria. If you are planning a pregnancy and are taking these drugs, you may need to consult a geneticist.
The following information describes rare serious illnesses and may sound alarming. It is not necessary to read this section, but, on common sense, it is useful.
There are two main types of neural tube defects:
spina bifida;
anencephaly.
The frequency of fixation of pathologies of both types is approximately 50/50.
Spina bifida
Condition in which a child is born with a split in the spine. In some cases, the spinal cord may "protrude" from this fissure. The split can be small or large, and can occur anywhere along a child's spine.
Spina bifida is often life-threatening, with about a third of children surviving. In the future, they are waiting for permanent health problems. The severity of the consequences will generally depend on where along the spine the opening occurs, the size of the opening, and the degree of injury to the protruding spinal cord.
Anencephaly
This is a medical term that literally means "no brain". In fact, while the embryo develops in the uterus, with anencephaly, the skull and brain do not form at all. The baby usually remains alive while in the mother's uterus, but is not viable after birth. Unfortunately, children with anencephaly cannot be saved.
Unfortunately, children with anencephaly cannot be saved.
What if you have one of the risk factors?
1. Take folic acid (preferably in advance) after consulting your doctor.
2. There is a blood test that a pregnant woman can take to check for neural tube defects in the fetus. This test is called maternal serum alpha-fetoprotein (or AFP). ) and is usually performed between 16 and 18 weeks of gestation. Accurate to 80%, when in doubt, AFR will help to dot the "i".
3. In addition, ultrasound performed between 17 and 20 weeks of gestation reveals up to 90% of neural tube defects.
4. And, of course, genetic testing.
It is advisable to review all options and test results with a gynecologist and/or genetic laboratory specialist.
Classification
There are different classifications; we present Lemire's classification55 (with modifications).
1. neurulation defects: abnormal closure of the neural tube leads to open defects
A.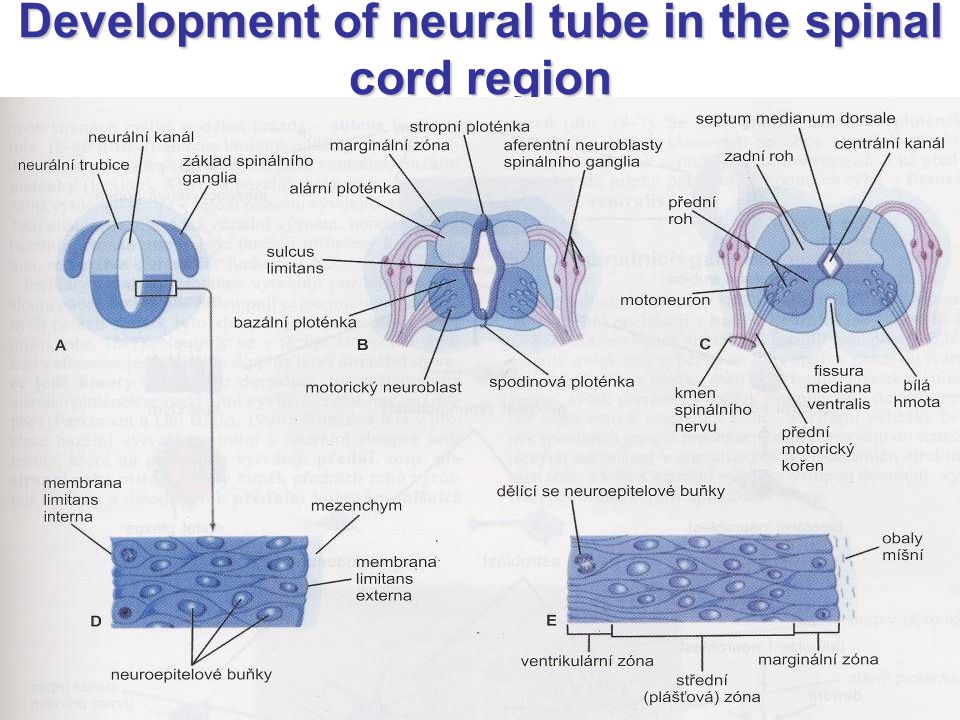 craniorachischisis: complete dysraphism. The fetus may die as a result of spontaneous miscarriage
craniorachischisis: complete dysraphism. The fetus may die as a result of spontaneous miscarriage
B. anencephaly: so-called. exencephaly. Occurs as a result of a violation of the closure of the anterior neuropore. This partially damaged brain is neither skull nor skin covered. In all cases, it ends in death. Risk of recurrence in the following pregnancies: 3%
C. meningomyelocele: most common in the lumbar region
1. myelomeningocele: see p.153
2. myelocele
2. post-neurulatory defects: leading to defects covered by skin (so-called closed) (some may be considered "migration abnormalities", see below)
A. cranial:
1. microcephaly: see below
2. hydrancephaly: the absence of a significant part of the cerebral hemispheres, which are replaced by CSF. To be distinguished from maximum GCF (see p. 174)
3. holoprosencephaly: see below
4. lissencephaly: see below
5. proencephaly: see below for schizencephaly
6. agenesis of the corpus callosum: see below
agenesis of the corpus callosum: see below
7. cerebellar hypoplasia/Dandy-Walker syndrome: see p.
1. diastematomyelia, diplomamyelia: see split spinal cord, p.160
2. hydromyelia/syringomyelia: see p.338
Migration anomalies
According to a slightly different classification, they are considered anomalies of neuronal migration (some consider them to be post-neurulatory defects, see above):
1. lissencephaly: the most severe form of migration anomaly. Violation of the development of the cerebral convolutions (it is possible to stop the formation of the cortex at an early stage of fetal development). Infants have severe mental retardation and usually live less than 2 years
A. agyria: perfectly flat surface
B. pachygyria: several wide and flat convolutions with shallow furrows
C. polymicrogyria: small convolutions with shallow furrows. Diagnosis by CT/MRI can be difficult; may be difficult unlike pachygyria
2. heterotopia: abnormal areas of gray matter that can be located anywhere from the subcortical white matter to the subependymal lining of the ventricles
heterotopia: abnormal areas of gray matter that can be located anywhere from the subcortical white matter to the subependymal lining of the ventricles
3. schizencephaly:
A. cleft that communicates with the ventricles (may be detected by CT/cisternography)
B. lined with cortical gray matter. This is the main difference from porencephaly, a cystic mass lined with connective or glial tissue that may communicate with the ventricular system. The latter is often due to vascular infarcts or develops as a result of ICH or penetrating trauma (including repeated ventricular punctures)
C. fusion of pia and arachnoid membranes
D. 2 forms: open (large cleft into the ventricle) or closed (walls touching)
Holoprosencephaly
T.S. archinencephaly. Lack of division of the telencephalic bladder into two cerebral hemispheres. The degree of lack of separation varies from severe alobar (one ventricle, no interhemispheric fissure) to semi-lobar and lobar (less severe forms of anomalies).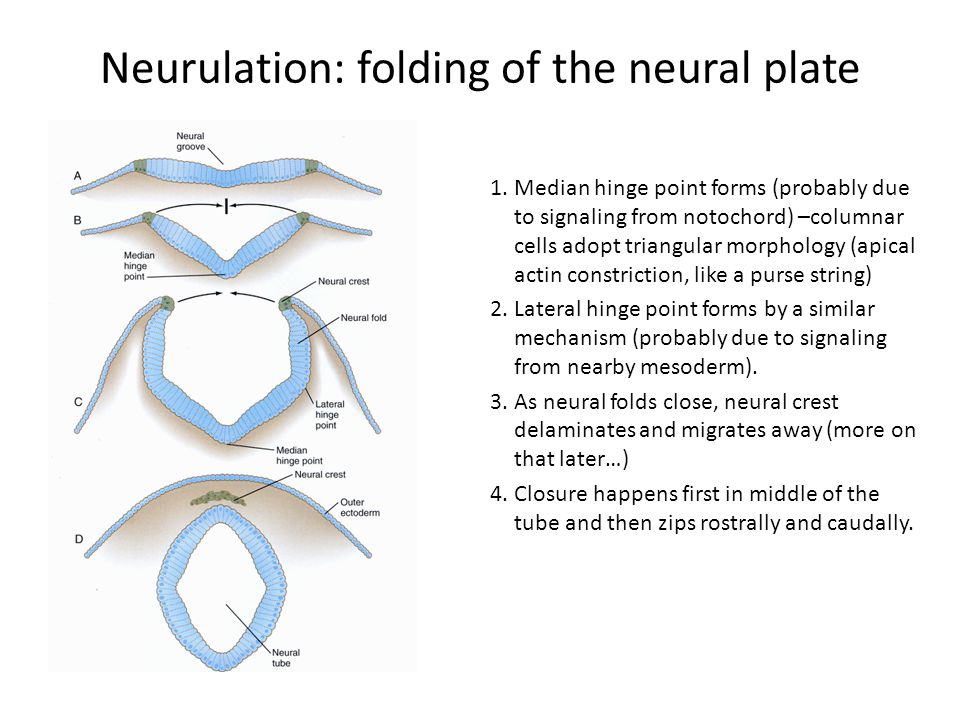 The olfactory bulbs are usually small; the cingulate gyrus usually remains connected. Often there is median cerebrofacial dysplasia, the degree of which corresponds to the degree of impairment of division into hemispheres (see Tables 6-13). The cause of these anomalies is often trisomy, however, normal karyotypes are also common. Survival beyond infancy is rare. Most survivors have severe mental retardation; only a small proportion of patients can participate in public life. The risk of holoprosencephaly is increased in some families with repeated pregnancies.
The olfactory bulbs are usually small; the cingulate gyrus usually remains connected. Often there is median cerebrofacial dysplasia, the degree of which corresponds to the degree of impairment of division into hemispheres (see Tables 6-13). The cause of these anomalies is often trisomy, however, normal karyotypes are also common. Survival beyond infancy is rare. Most survivors have severe mental retardation; only a small proportion of patients can participate in public life. The risk of holoprosencephaly is increased in some families with repeated pregnancies.
Tab. 6-13.
Microcephaly
Definition: LZO
Macroencephaly30 (p.109)
T.S. macroncephaly, megalencephaly (not to be confused with macrocephaly, which is an enlargement of the skull, see p. 880). It is not a strictly defined pathology. Enlargement of the brain is possible as a result of: hypertrophy of only gray matter, gray and white matter, the presence of additional structures (proliferation of glia, diffuse gliomas, heterotopia, metabolic accumulation diseases, etc.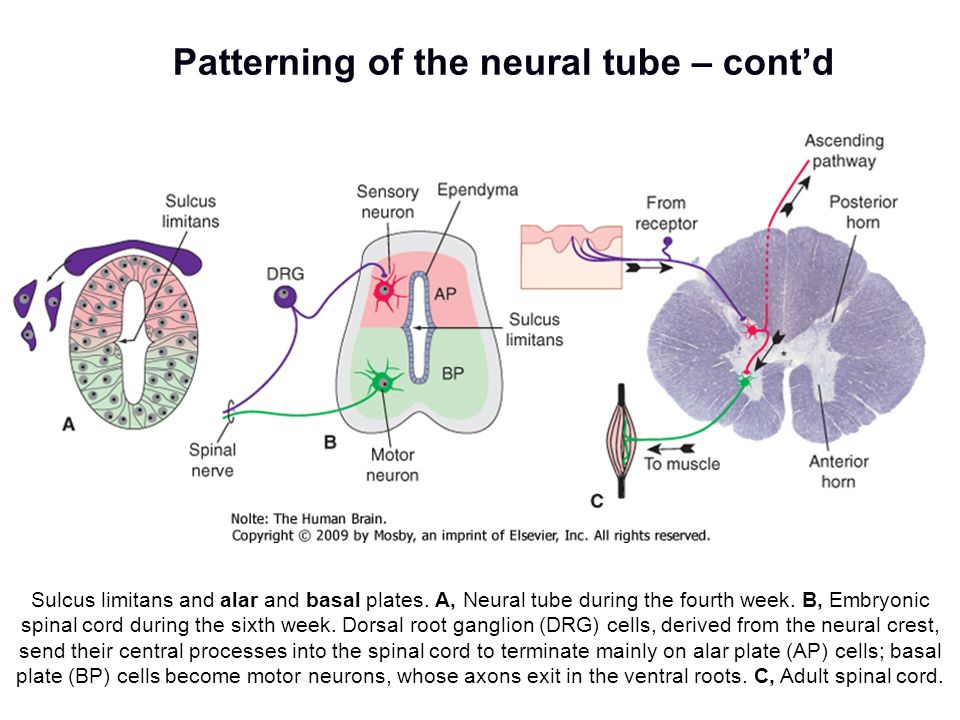 ). It can be observed in neurocutaneous syndromes (especially in NFM).
). It can be observed in neurocutaneous syndromes (especially in NFM).
The brain can weigh up to 1.600-2.850 g. IQ may be normal, but there may be mental retardation, spasticity, and hypotension. LZO > average by 4-7 cm. There are no usual signs of HCP (protruding forehead, protrusion of fontanelles, a symptom of the "setting sun", enlarged veins of the head). On CT and MRI, the ventricles are of normal size; these studies allow to exclude the presence of extracerebral accumulations of fluid.
Risk factors
1. early administration of vitamins (especially 0.4 mg/d folic acid) may reduce the incidence of neural tube defects (NTDs) (make sure vitamin B12 levels are normal, see p. 866)
2. maternal exposure heat in the form of hot baths, saunas or fever (but not electric blankets) during the first trimester is associated with an increased risk of NTDs61
3. Use of valproic acid (Depakene®) during pregnancy is associated with a 1-2% risk of NTDs
4. obesity (before and during pregnancy) increases the risk of NTD63,64
obesity (before and during pregnancy) increases the risk of NTD63,64
5. maternal cocaine use may increase the risk of microcephaly, disorders of nerve migration, neuronal differentiation and myelination57
Prenatal detection of neural tube defects
Plasma alpha-fetoprotein (AFP)
For basic information, see Alpha-fetoprotein, p.476. A high plasma AFP level (more than 2-fold increase in mean week of gestation) at 15–20 weeks gestation corresponds to a relative risk of NTD of about 224. An abnormal level (high or low) is associated with 34% of significant birth defects65. The sensitivity of maternal plasma AFP for spina bifida was 91% (10 cases out of 11) and 100% for 9 cases of anencephaly. However, other series of observations showed less sensitivity. Plasma AFP screening will probably fail to detect closed defects of the lumbosacral spine, which account for ?20% of spina bifida cases66. They also, apparently, cannot be detected by ultrasound. Because maternal plasma AFP levels are elevated during normal pregnancy, overestimation of gestational age may cause an elevated AFP to be considered normal, and an underestimation, conversely, to a normal AFP as elevated67.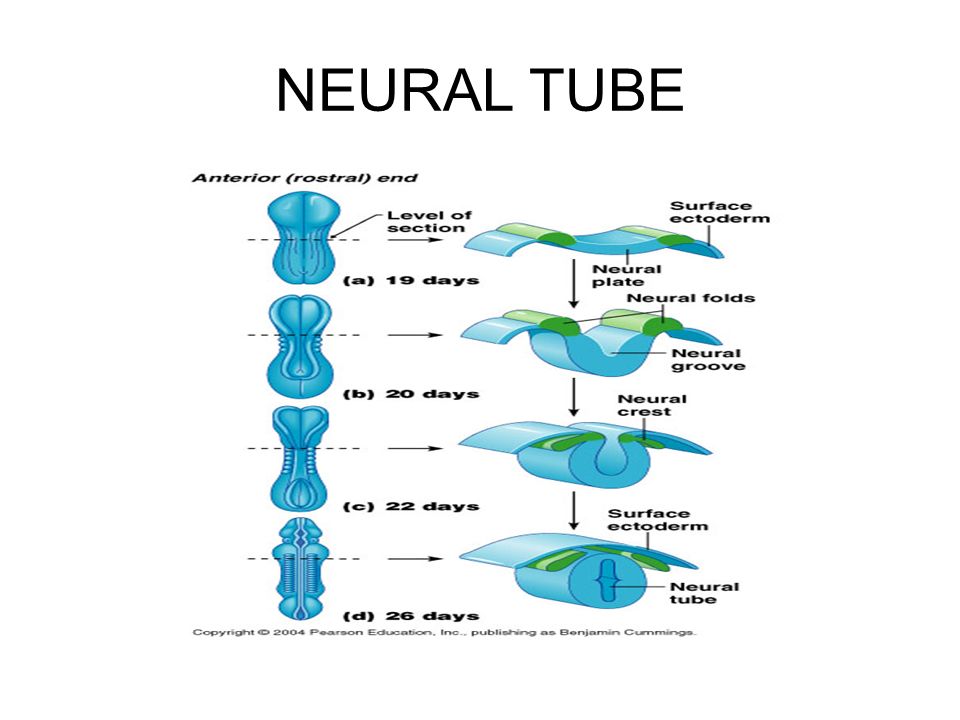
Ultrasound
Prenatal ultrasound can detect spina bifida in 90-95% of cases. In a situation of elevated AFP, it can help differentiate between non-neurological causes of elevated AFP (eg, omphalocele). It can also help to more accurately determine the duration of pregnancy.
Amniocentesis
In postnatal pregnancy with MMC, if prenatal ultrasonography does not show spinal dysraphism, amniocentesis is indicated (even if abortion is not contemplated, this may help provide optimal care if MMC is diagnosed). The AFP index in the amniotic fluid is increased with open NTDs. Its peak occurs at 13-15 weeks of pregnancy. In this group of patients, amniocentesis is associated with a ?6% risk of fetal loss.
Identification of groups of pregnant women with high and low risk of having a child with a neural tube defect. Pathology of the neural tube of the fetus, which turns into malformations of the lumbosacral spine of the future spine, can occur only during the period of secondary neurulation.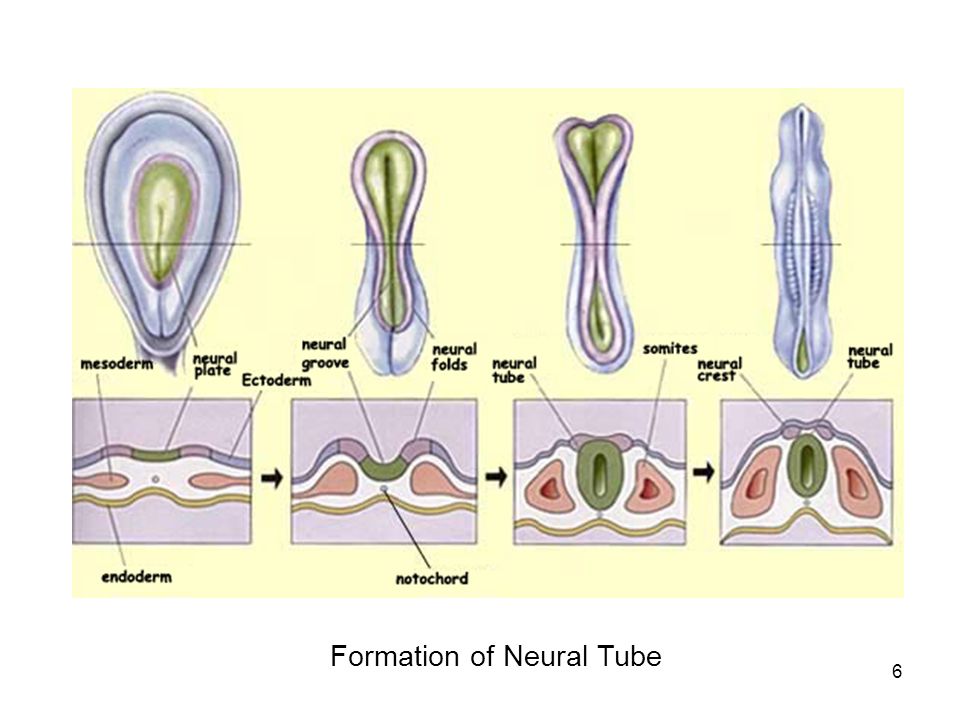 Doctors also refer to unbalanced nutrition of the mother as one of the root causes of the development of a neural tube defect.
Doctors also refer to unbalanced nutrition of the mother as one of the root causes of the development of a neural tube defect.
The first thing a woman should do is to register with a good specialist whom she trusts in order to be sure of the normal course of pregnancy. Gather all your will into a fist and do everything possible so that the child is born healthy. It is important to understand that the pathology of the neural tube of the fetus is not a modern disease that is caused by the current conditions of human life.
What are neural tube defects?
The Italian anatomist Morgagni Batista was perhaps one of the first to give approximate descriptions of neural tube defects. Of course, such pathologies were not subject to treatment at that time, because medicine was still at a very low level of development. So, on the 19-20th day after conception, a specific plate is formed in each fetus - the very first form of development of the human nervous system. If, on the 23rd day from conception, the neural plate has not closed completely into a tube, the fetus will develop problems with the spine.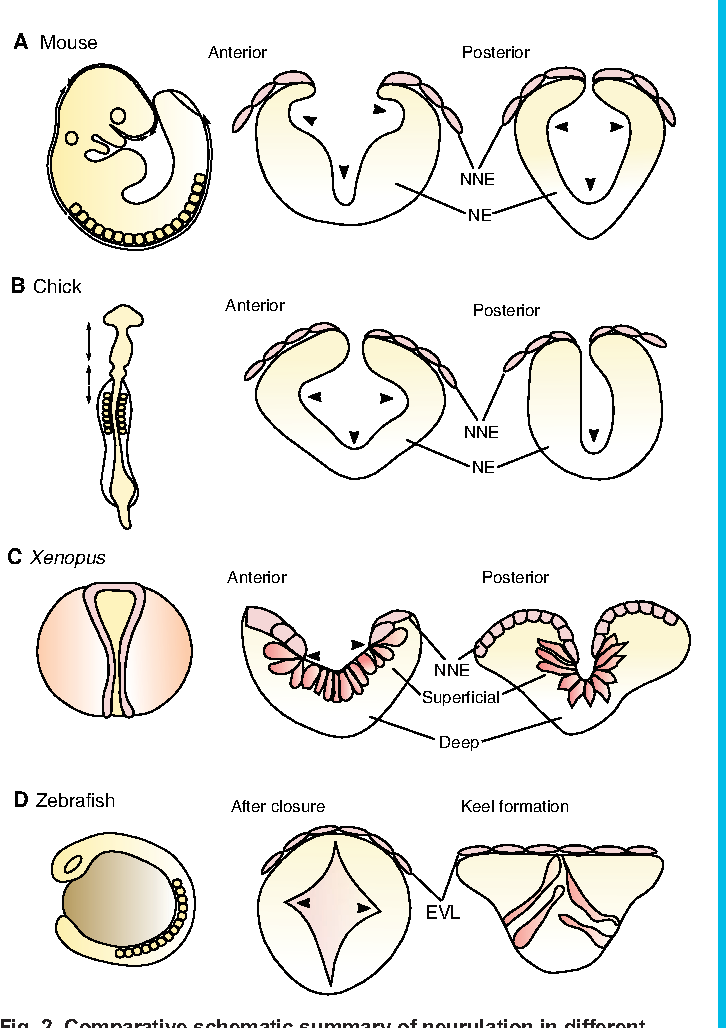
Yes, a genetic predisposition to such a defect greatly increases the risk of its occurrence. Even a hot bath taken by a woman at the beginning of pregnancy can provoke the occurrence of such a defect. Already during this period of time, violations may occur, that is, spinal dysraphia.
As with any disease or disorder of normal development, the defective formation of the neural tube in the fetus has its own symptoms. Hidden spinal cleft: a similar defect is most often located in the lumbosacral region. Such a disease has a number of consequences, which include bedwetting, a significant violation of the correct posture, leg muscle weakness, pain in the lumbar region, and even foot deformity.
How to diagnose a neural tube defect or pathology?
This is a very severe form of the defect, which often results in rupture of the hernial sac and leakage of cerebrospinal fluid. The extreme degree of deformity is considered to be non-fusion of the spine and soft tissues, which is accompanied by an inferior formation of the spinal cord.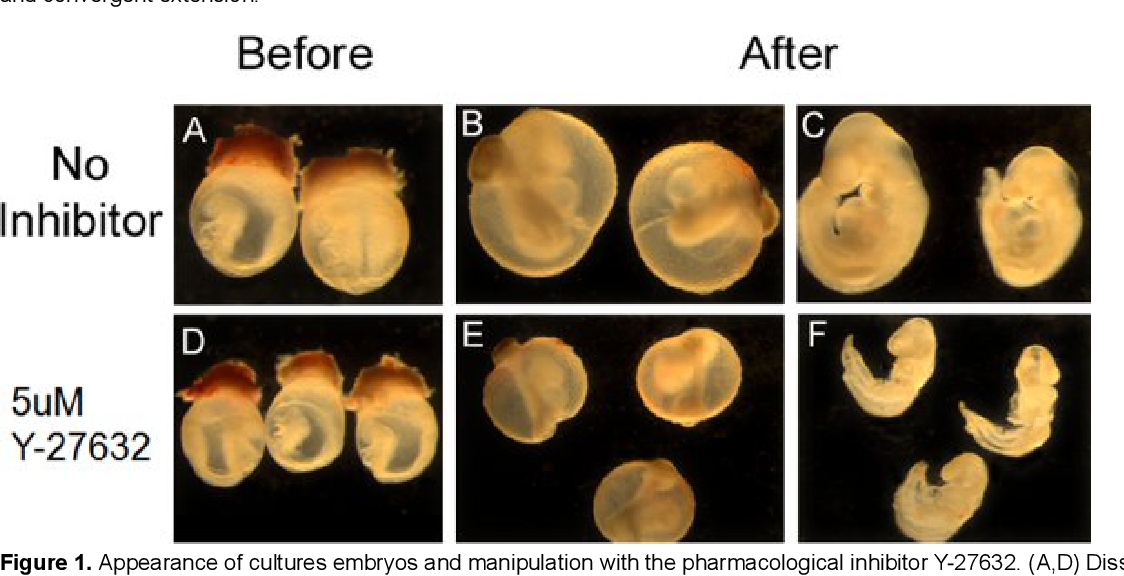 Such a defect is practically incompatible with life.
Such a defect is practically incompatible with life.
This state of affairs is explained by the fact that if the defect develops in the fetus, then the pregnancy is most often completed by spontaneous abortion (miscarriage). This will help you understand what the fetal neural tube is, and will also allow you to study all the recommendations of specialists that will be useful to you in the future. In the third trimester, it is already possible to see, through ultrasound, a congenital malformation of the fetus, which arose as a result of the fact that the neural tube was not formed correctly.
Treatment of problems that have arisen due to the fact that the formation of the neural tube has been disturbed can be started immediately after the birth of the child. Congenital malformations of development are one of the main causes of infant mortality and disability. Therefore, the social and medical aspects of gross defects in the development of the neural tube are reduced to the prevention of the formation of a defect, its early diagnosis and timely termination of pregnancy.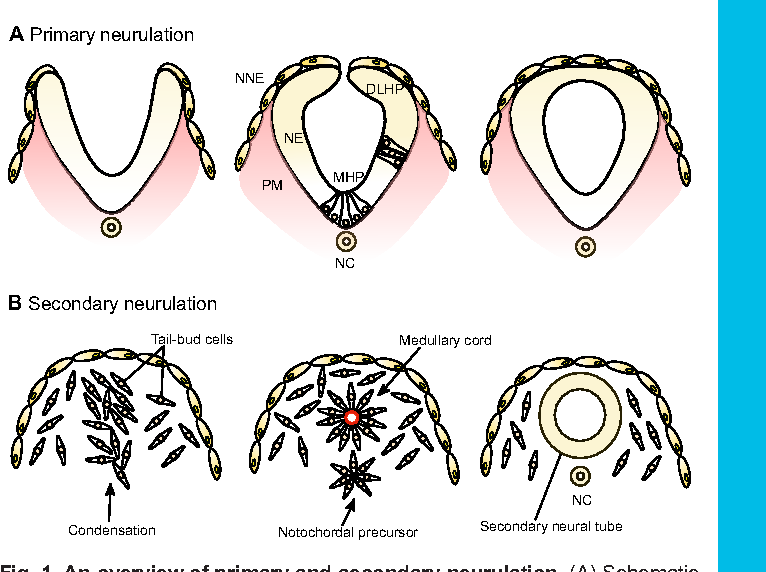
He also proved the possibility of hidden anomalies in the formation of the neural tube. A more effective method of treatment was proposed by Dr. Wauer in 1889.year, which “closed” the bone defect with a muscle-aponeurotic flap cut from the underlying tissues. Paresis of the extremities, deformities of the spine and feet, urinary incontinence, delayed physical and mental development were often found in children, which required specific treatment.
In the embryo on the 20th day after conception, the neural plate is formed on the dorsal side, the edges of which later begin to close, forming the neural tube. Around the 23rd day, this tube should close completely, leaving only the holes at its ends open. First, a genetic defect inherited from one of the parents.
To understand the essence of the formation of malformations of the spine and spinal cord, it is necessary, at least in general terms, to imagine the process of embryogenesis of these structures.