Nerve damage from breastfeeding
A Breastfeeding Mom's Symptoms Are as Important as the Baby's — DrGhaheri.com
by Bobby Ghaheri
My last post detailed how tongue-tie and lip-tie can have significant adverse effects on the baby trying to nurse. This post will detail how a poor latch from tongue-tie or lip-tie can harm mom.
I often hear from moms that they feel like they're being selfish for putting their children through a procedure, particularly if that child is not experiencing any significant negative effects from breastfeeding. The argument against this sentiment is quite easy: anything that jeopardizes a mom's ability to breastfeed obviously puts the baby in harm's way. I maintain that babies should nurse for as long as possible without having some external situation forcing them to wean. Sometimes, that means focusing on the mom's symptoms instead of the baby's if her symptoms are worse.
What are some of the consequences for mom when the baby has a poor latch from tongue-tie or lip-tie?
- Nipple damage - These are among the most obvious consequences of a baby's poor latch from tongue or lip restrictions.
If the baby cannot flange out their lip appropriately, the lip will roll inwards, making the latch more shallow. Additionally, if the tongue is restricted, it cannot appropriately cup and lift the breast within the oral cavity, and the lower gumline is exposed. When the lower gum and the upper lip are what is being used to hold on to the breast, nipple damage can occur. Early signs include a change in the nipple shape following breastfeeding. Nipples can be creased or flattened, or can come out white (blanching) from compression and restriction of blood flow. If trauma is persistent or severe, mom can experience cracking, bruising or blistering. When it is most severe, mom can experience bleeding and scabbing. Even after the latch does improve with treatment, some moms have experienced long term nerve damage that may not improve with time.
- Pain - This is one of the most common symptoms a mom experiences. Unfortunately, it's one of the most commonly dismissed symptoms by healthcare providers.
 Too many are quick to propagate the myth that painful breastfeeding is normal. Painful breastfeeding is common, but that does not mean that it is normal. Is there a sensitivity at the beginning of breastfeeding? Sure, but that isn't what I am describing here. The often toe-curling pain that accompanies breastfeeding a tongue-tied baby can be severe enough that mom will begin to dread it. Even when the pain isn't as bad, but is still present, the persistence of the discomfort can most definitely lead to premature weaning.
Too many are quick to propagate the myth that painful breastfeeding is normal. Painful breastfeeding is common, but that does not mean that it is normal. Is there a sensitivity at the beginning of breastfeeding? Sure, but that isn't what I am describing here. The often toe-curling pain that accompanies breastfeeding a tongue-tied baby can be severe enough that mom will begin to dread it. Even when the pain isn't as bad, but is still present, the persistence of the discomfort can most definitely lead to premature weaning. - Poor or incomplete breast drainage - There are numerous reasons why a baby won't empty a breast. These include prematurely falling asleep at the breast, being unable to form an appropriate seal or being unable to use the tongue appropriately to draw enough negative intraoral pressure to nurse. Whatever the reason, stagnant milk can be indicative of future problems with lessening milk supply. Additionally, it can be a precursor to mastitis.

- Breast disease - Ultimately, if anything threatens the health of the breasts, milk supply becomes jeopardized. In the setting of a traumatic latch, mom's nipples can become infected from cracking. This can lead to breast abscesses. Surface trauma can lead to inoculation with thrush, which can be transferred to and from the baby. Superficial bacterial infections, blebs, or plugged ducts can also result. One of the more miserable results from a poor latch is mastitis, often recurrent. If a mom has recurrent episodes of mastitis, I always look for a restriction in the mouth as a primary potential cause. Mastitis can lead to hospitalization and a sudden drop in milk supply, so it must be taken seriously.
It is critical that we look at breastfeeding as a tag-team effort if we are going to achieve long term success in babies who are otherwise anatomically unable to latch appropriately. If a baby is completely healthy and growing well but mom is persistently sick or too traumatized to frequently breastfeed, we have failed to treat the dyad in a supportive fashion.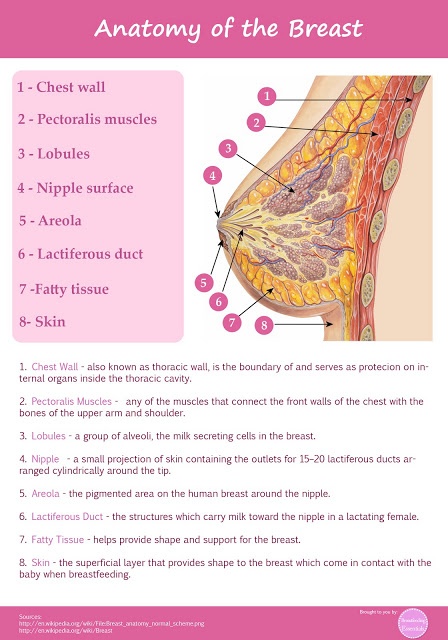 We must stop dismissing mom's symptoms and we must stop propagating a culture where it is somehow ok to ignore the needs of the mom.
We must stop dismissing mom's symptoms and we must stop propagating a culture where it is somehow ok to ignore the needs of the mom.
Nipple Vasospasm and Breastfeeding - Breastfeeding Support
A vasospasm is a sudden narrowing (or constriction) of blood vessels. If the blood vessels in the nipple have a vasospasm this can cause nipple pain and sometimes deeper breast pain. A breastfeeding baby can trigger a nipple vasospasm if they are not attached (latched) to the breast comfortably ie with a big mouthful of breast tissue as well as the nipple. A nipple vasospasm can also be connected with Raynaud’s phenomenon (a condition affecting blood supply). This article looks at the symptoms, causes and possible treatments for easing nipple vasospasm.
Nipple vasospasm and breastfeeding
If a nipple is flattened or compressed because a baby is pinching the nipple during a breastfeed, this may trigger a nipple vasospasm. The nipple may look pointed or slanted like the top of a new lipstick straight after a feed and, since the blood vessels in the nipple are narrowed, less blood can flow and the nipple can temporarily turn white. When the blood flows back to the nipple after each breastfeed, mothers may feel a painful burning or throbbing sensation.
When the blood flows back to the nipple after each breastfeed, mothers may feel a painful burning or throbbing sensation.
What are the symptoms of nipple vasospasm?
Symptoms of nipple vasospasm include:
- Painful nipples—the pain is often described as burning, stabbing or itching and may be felt a short time after breastfeeding and/or in between feeds.
- Sore nipples—nipple vasospasm is associated with misshapen nipples and sore nipples or previously damaged nipples that are healing.1
- White nipples—nipple tips may look white (blanched) after a feed or mothers may notice other colour changes in their nipples e.g. blue or dark red (also associated with Raynaud’s Phenomenon—see below)
- Deep breast pain—some mothers may feel deep breast pain or shooting pains deep in the breast sometimes referred to as Mammary Constriction Syndrome.

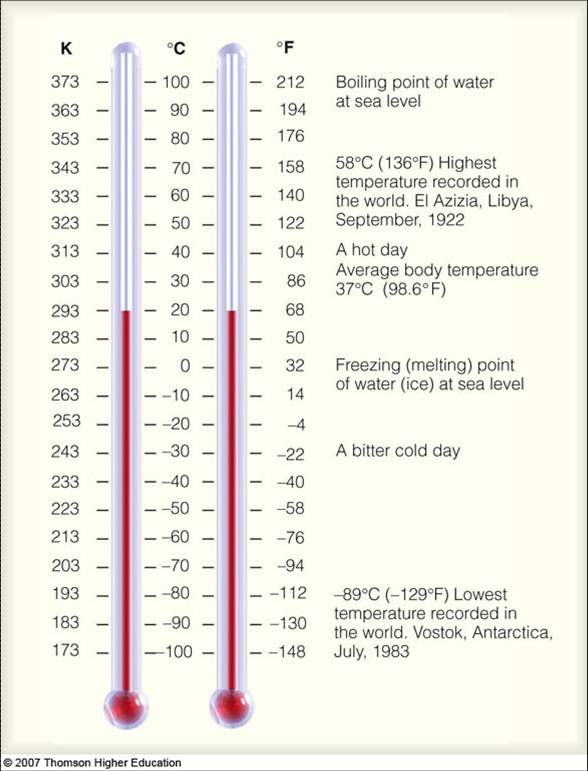
- Cold temperatures and stress may worsen the pain or trigger it.
Not vasospasm? Other causes of pain
There are many causes of sore nipples or pain during breastfeeding and for a complete overview see Causes of Sore Nipples and Why Does Breastfeeding Hurt? Vasospasm symptoms such as burning pain and soreness can be very similar to those of a bacterial infection (e.g. a Staph infection) or a fungal infection (e.g. thrush). Note that a misdiagnosis of thrush and resulting unnecessary prescription medication, may make vasospasm symptoms worse.2
What causes nipple vasospasm?
There are a number of risk factors that seem to make nipple vasospasm more likely:
- A shallow latch. In breastfeeding mothers, the main trigger for nipple vasospasm is likely to be a poor latch (the way a baby attaches to the breast).
 If a baby breastfeeds with mostly only the nipple in their mouth and not a good deep mouthful of breast tissue as well, this is often called a shallow latch. In a shallow latch the nipple is more likely to get pinched between baby’s tongue and the roof of their mouth and trigger the vasospasm. Some babies also learn that pinching the nipples is a good way to slow the milk flow in a fast let-down.
If a baby breastfeeds with mostly only the nipple in their mouth and not a good deep mouthful of breast tissue as well, this is often called a shallow latch. In a shallow latch the nipple is more likely to get pinched between baby’s tongue and the roof of their mouth and trigger the vasospasm. Some babies also learn that pinching the nipples is a good way to slow the milk flow in a fast let-down. - Sore nipples. Sore nipples, damaged or cracked nipples, and nipples that are healing are associated with poor positioning at the breast and are risk factors for vasospasm (Thomas, 2013).
- Cold temperatures. Exposure to cold temperatures and climates, or the sudden drop in temperature when a baby lets go of the nipple is a risk factor for a nipple vasospasm.3
- Severe stress. Severe emotional stress is a risk factor for nipple vasospasm and a history of migraines may be a risk factor (Goldfarb, 2019).

- Medical conditions. An existing history of autoimmune disease eg lupus, rheumatoid arthritis, thyroid dysfunction, scleroderma, or previous diagnosis of Raynaud’s syndrome increases the likelihood of nipple vasospasm.4
- Cigarette smoking. Exposure to cigarette smoke, second-hand smoke or nicotine can be triggers for nipple vasospasm (Goldfarb, 2013).5
- Medications. Certain medications including fluconazole (prescribed for thrush), some decongestants, or birth control medication are risk factors for nipple vasospasm (Goldfarb, 2019; Breastfeeding Network, 2019) also beta-blockers, or vasoconstrictor medications which narrow blood vessels (Douglas, Vol 18: 1–29 2022).
- Caffeine may be a trigger for vasospasm (Goldfarb, 2019; Breastfeeding Network, 2019) however Douglas says there is no clear evidence linking caffeine intake to secondary Raynaud’s syndrome (vasospasm without existing Raynaud’s) (Douglas, Vol 18: 1–29 2022).

How can I avoid vasospasm symptoms?
Minimising the risk factors can work very well to help prevent symptoms of nipple vasospasm, namely:
- Get help with positioning from an International Board Certified Lactation Consultant so that your baby’s latch is not triggering vasospasm. A poorly latched baby, an ineffective suck or the baby clamping on the nipple can all cause nipple blanching. Babies with high muscle tone or those with tummy ache (e.g. from a food allergy) may seem to “bite” at the breast and can cause a nipple vasospasm. A baby needs to attach to the breast deeply with a big mouthful of breast as well as the nipple. See Breastfeeding Positioning for Newborns, Latching Tips and Why Does Breastfeeding Hurt? for more information and see your breastfeeding specialist for one to one help.
- Check pumping equipment. A poorly fitted pump flange could cause nipple damage and vasospasm symptoms, conversely pumping with a well fitted pump may offer relief to symptoms compared to breastfeeding for some women until they can get help with positioning.
- Keep warm; breastfeed in a warm room and cover the nipple as soon as a breastfeed ends. Don’t leave nipples to air dry as they will get colder that way. Keep breastpads dry, some mothers use woollen or fleecy breastpads for warmth. Try to avoid sudden temperature changes.6
- Avoid latching a baby while the nipple is having a vasospasm, as this may cause damage to the nipple, try warming the breast and repeatedly squeezing the nipple to help blood flow back into this area before latching (Hills, accessed Oct 2022).
- Gentle massage. Try massaging the nipples with warm olive oil after a breastfeed to stop a nipple vasospasm.78 Repeatedly squeezing the nipple during a vasospasm helps blood flow return to the nipple and can improve recovery time.
 9
9 - Rule out a bacterial infection or thrush—check with your health professional that you don’t have any other causes of burning pain and sore nipples.
- Avoid potential triggers: cigarette smoke and smoking, nicotine, caffeine, or any medications that promote vasoconstriction e.g. some decongestants10 and avoid stress where possible.
- Keep active with aerobic exercise.
Raynaud’s phenomenon
Raynaud’s is a disorder of the tiny blood vessels of the extremities which reduces blood flow. Cold temperatures or strong emotions cause the blood vessels in the extremities to go into spasms, which may cause pain, numbness, throbbing and tingling. Some women who have Raynaud’s in the fingers and toes may find they get Raynaud’s of the nipple when they breastfeed. This might be because breastfeeding affords lots of opportunities for nipples to get cold e.g. just before and after latching. Painful breastfeeding can also be stressful. Raynaud’s is often misdiagnosed as thrush or a poor latch .11
This might be because breastfeeding affords lots of opportunities for nipples to get cold e.g. just before and after latching. Painful breastfeeding can also be stressful. Raynaud’s is often misdiagnosed as thrush or a poor latch .11
Diagnosis of Raynaud’s
Raynaud’s symptoms affecting the nipple may be difficult to distinguish from nipple vasospasm caused by a poor latch:
- Symptoms can be triggered by cold and may still occur in spite of a good latch.
- Colour changes of the nipples e.g. from white to blue to red/purple may be seen with lighter skin tones.
- Raynaud’s may be linked with a history of migraines or a history of poor circulation 12.
- May be associated with previous breast surgery and nipple damage1314
Treatments for nipple vasospasm
In addition to using the above ideas to avoid getting vasospasm symptoms, there are a number of treatment options for nipple vasospasm that still persists after a poor latch has been corrected and other infections ruled out. Treatments options are discussed in the following patient information handout from the Goldfarb Breastfeeding Clinic and include pain relief, dietary supplements (calcium, magnesium and vitamin B6), omega fatty acids and prescription medication:
Excerpt from
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
- The use of Advil™ or Motrin™ (ibuprofen) and/or Tylenol™ (acetaminophen) may be very useful to treat the pain of nipple vasospasm. These medications are safe during breastfeeding.
- Your health professional may suggest high doses of calcium and magnesium, and vitamin B6.
Please consult your health professionals for doses specific to your case.
- Omega fatty acids may also help. Evening primrose oil (up to 12 capsules a day) and fish oil capsules are rich sources of omega fatty acids.
- Nifedipine (Adalat™) […] normally used for high blood pressure, can also be used for nipple vasospasm, and is safe for breastfeeding mothers and infants.
Nifedipine
Refer to the full Goldfarb article online for precautions regarding nifedipine and share this with your health care professional. The Breastfeeding Network discusses doses and side effects of nifedipine in their fact sheet Raynaud’s Phenomenon in Breastfeeding Mothers and for more places to find information about the safety of nifedipine online see Medications and Breastfeeding. Always discuss medications or medicinal doses of supplements with your health care provider.
Treatment tips from Dr Jack Newman
Jack Newman, a Canadian paediatrician and breastfeeding expert, has a protocol for treating vasospasm; see Vasospasm on his website. In addition to a discussion of certain vitamin and mineral supplements (also referred to in the patient handout quoted above), Dr Newman advocates:
In addition to a discussion of certain vitamin and mineral supplements (also referred to in the patient handout quoted above), Dr Newman advocates:
- All Purpose Nipple Ointment (APNO), a topical cream with antibacterial, antifungal and anti-inflammatory ingredients to help with soreness.
- Massaging olive oil into the nipples as an alternative to APNO.
- Pectoral muscle massage see Mammary Constriction Syndrome.
Complementary medicine
Scleroderma and Raynaud’s UK (SRUD) discuss natural and over the counter complementary medicine for scleroderma and Raynaud’s in Natural Therapies. They discuss how vitamin C, vitamin E, gamolenic acid (GLA), ginkgo bilboa and ginger may help symptoms in the general population but note this article is not specific to breastfeeding mothers. For the latest recommendations on the compatibility of individual supplements with breastfeeding check online at e-Lactancia or LactMed. Always discuss taking therapeutic doses of supplements with your qualified health professional to make sure they are compatible with your medical history and existing medication.
Always discuss taking therapeutic doses of supplements with your qualified health professional to make sure they are compatible with your medical history and existing medication.
The Breastfeeding Network fact sheet for Raynaud’s adds that it may be helpful to include ginger in the mother’s diet e.g. drink ginger tea, or even add a spoonful of ground ginger to bath water.
Summary
Nipple vasospasm is a narrowing of blood vessels in the nipple. It can be triggered by a baby breastfeeding in a shallow latch and can cause burning, stabbing or itching pain in the nipples after a breastfeed. Nipple vasospasm can also be associated with Raynaud’s phenomenon and can also cause Mammary Constriction Syndrome or deep breast pain. Treatment involves improving a baby’s latch and positioning at the breast, and avoiding the triggers of nipple vasospasm. Some medications and natural remedies may help symptoms.
Footnotes & References
-
Thomas.
 The problem with yeast. Too much diagnosis. Too little data. Adapted from Dr Jen’s Guide to Breastfeeding p98. 2012 [accessed 21 October 2022]
The problem with yeast. Too much diagnosis. Too little data. Adapted from Dr Jen’s Guide to Breastfeeding p98. 2012 [accessed 21 October 2022] -
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
-
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
-
Douglas. Re-thinking lactation-related nipple pain and damage. Women’s Health Volume 18: 1–29 2022
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Hills. Raynaud’s of the Nipple: Help for Pregnant & Breastfeeding Moms. Raynauds.org [accessed 20 October 2022]
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Newman. Vasospasm.
 2019
2019 -
Raynaud’s Information. Summerwarmth.co.nz [accessed 20 October 2022]
-
Raynaud’s Syndrome, Breastfeeding Network, 2019
-
Anderson et al, Raynaud’s Phenomenon of the Nipple: A Treatable Cause of Painful Breastfeeding, Pediatrics, 2004
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Anderson et al, Raynaud’s Phenomenon of the Nipple: A Treatable Cause of Painful Breastfeeding, Pediatrics, 2004
-
Hills. Raynaud’s of the Nipple: Help for Pregnant & Breastfeeding Moms. Raynauds.org [accessed 20 October 2022]
Breastfeeding | Tervisliku toitumise informatsioon
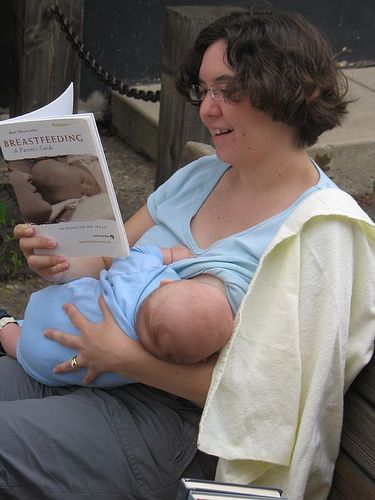
According to the Nordic Nutrition Guidelines based on research and advice from the WHO, only breast milk is the optimal nutrition for the first six months of a child's life.
A healthy child does not need any other fluids or supplements.
An exception is vitamin D, which pediatricians recommend giving as a fat-soluble supplement from the second week of life for the first two years at 10 micrograms (5 drops, or 500 IU) per day to ensure better skeletal development during a period of rapid growth. If a breastfeeding mother is a vegan or vegetarian, she should ensure that her baby is getting enough vitamin B12 to avoid deficiency.
From the second half of the year, continuing breastfeeding, you should gradually begin to give solid food even if the child grows well and on milk alone. A gradual transition to family food should begin at the end of the first year of life. A one-year-old child should receive half of the energy from breast milk, half from spoon-feeding, mainly vegetables and fruits, cereals and meat. You can continue breastfeeding as long as it is comfortable for both mother and baby.
Nature is an amazing creator of food for a baby.

The mother's breast produces just the right product for a rapidly growing and developing baby. Breastfeeding soothes the baby, promotes the development of his oral cavity and the formation of bite. Breast milk is always at the right temperature, always clean and cheap. Feeding does not require any aids, you can feed your baby almost anywhere. All components of breast milk are easily absorbed and accepted by the baby and support its overall development. Breast milk is rich in nutrients and bioactive compounds such as vitamins, minerals, fatty acids, and immune factors that have been shown to be beneficial to human health. Breast milk differs during one feed, during the day, in summer and winter, and constantly changes with the age of the child.
There is strong evidence that breastfeeding protects against overweight and many infections (ear, respiratory and digestive tract infections) in infancy and early childhood. Breast milk contains many protective factors that are thought to have an immunological effect for several years after breastfeeding has ended.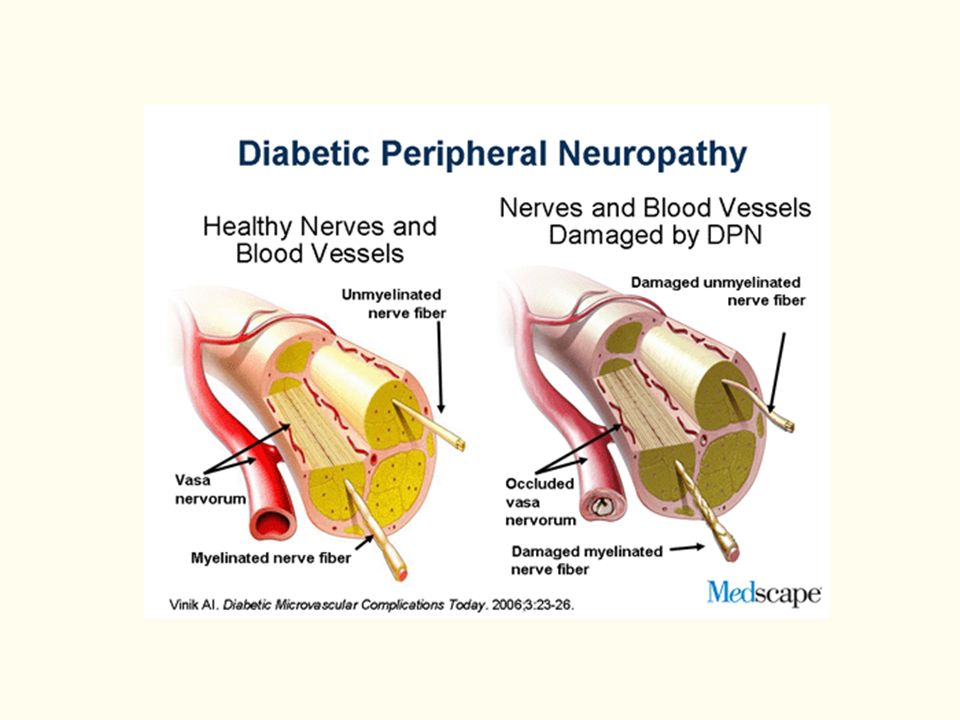 Breastfeeding is likely to have a positive effect on a child's IQ and cognitive development, and this effect is related to the duration of breastfeeding. It is also considered likely that breastfeeding has a protective role against celiac disease if, even when the child receives breast milk, small amounts of gluten-containing foods are given to him. Comparing breastfed versus non-breastfed infants suggests a protective effect of breastmilk against type 1 and type 2 diabetes. There are indications that breastfeeding may reduce the risk of overweight and cardiovascular disease in adulthood.
Breastfeeding is likely to have a positive effect on a child's IQ and cognitive development, and this effect is related to the duration of breastfeeding. It is also considered likely that breastfeeding has a protective role against celiac disease if, even when the child receives breast milk, small amounts of gluten-containing foods are given to him. Comparing breastfed versus non-breastfed infants suggests a protective effect of breastmilk against type 1 and type 2 diabetes. There are indications that breastfeeding may reduce the risk of overweight and cardiovascular disease in adulthood.
Since breastfeeding is part of the normal postnatal process, it is also ideal for women. Feeding promotes faster uterine contraction and postpartum recovery.
When normal nutrition is continued, body weight decreases faster after pregnancy, since the body of a woman additionally spends more than 500 kcal on the production of breast milk. Certain foods (nuts, halva), as a rule, do not lead to an increase in the amount of breast milk, but only contribute to weight gain.
The amount of breast milk does not depend on the amount of food consumed by the mother. It depends on the frequency of breast emptying, the duration of feeding and the effectiveness of the sucking technique of the child. Pregnant women should not be without food for more than 12 hours. Otherwise, ketone bodies are formed in the blood, which are dangerous for the fetal brain. The situation can threaten the life of the fetus if the mother has not eaten for more than 20 hours.
Breastfeeding is an energy intensive process and many breastfeeding mothers are encouraged to increase their energy intake. However, in the case of a positive energy balance and low physical activity, there is a risk of overweight during the feeding period. To avoid postpartum weight gain, it is recommended to increase physical activity rather than decrease it during the feeding period. Nursing mothers have a lower risk of developing breast and uterine cancer at a young age, and the risk of osteoporosis later in life also decreases. During the feeding period, it is recommended to consume amounts of liquid proportional to the amount of milk produced. The amount of 750 ml of breast milk during the first six months increases the need for fluid in a nursing mother by about 600-700 ml per day.
During the feeding period, it is recommended to consume amounts of liquid proportional to the amount of milk produced. The amount of 750 ml of breast milk during the first six months increases the need for fluid in a nursing mother by about 600-700 ml per day.
Feeding creates a particularly close relationship with the baby, nighttime feedings are more comfortable, and studies show that breastfeeding mothers are less likely to experience postpartum depression.
98% of women can breastfeed, however, according to Estonian statistics, only 40% of our children receive breast milk at the age of 6 months. Many common myths about breast milk and breastfeeding can also prevent successful feeding.
Golden rules for feeding:
- The whole body is turned towards the mother, the mother supports the child behind the back (not behind the head!), pressing his stomach tightly to her own, maintaining closeness.
- Before taking the breast, the baby's nose is at the nipple.

- The child's jaw and nose are pressed against the chest, the lower lip is turned down, the cheeks are puffed out.
- Sucking alternates with swallowing.
- If the mother is sitting while breastfeeding, the baby should be on a cushion so that the mother can sit as freely and relaxed as possible, with a straight back, leaning on something, neck and shoulders relaxed.
- The child asks for breasts at least eight times a day and calms down after feeding.
- Every day the child urinates profusely and in the first month of life begins to poop at least once a day.
- Monthly weight gain of the child is at least 500-600 grams, the child grows in length, and every month his head circumference increases.
Sometimes breastfeeding may be contraindicated for health reasons of the mother or child. Then, during the first year of life, the child should be given milk mixtures and make sure that they are prepared in strict accordance with the instructions on the package.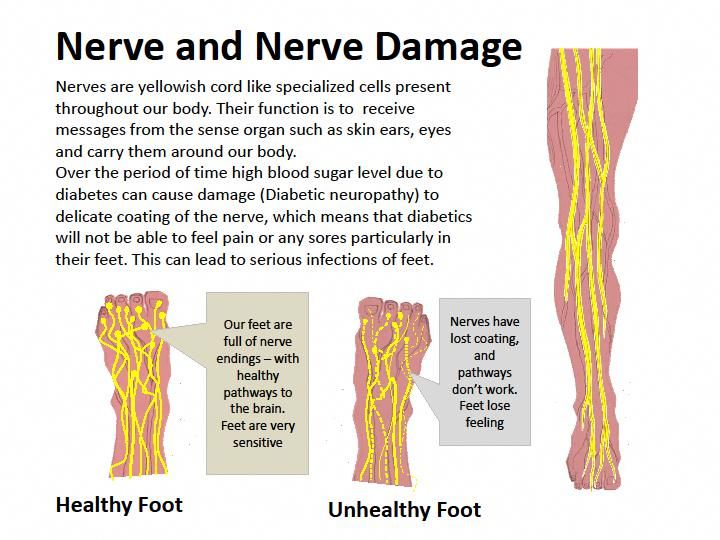 It is impossible to give cow's milk to a baby in the first year of life.
It is impossible to give cow's milk to a baby in the first year of life.
Do not breastfeed if:
- Baby has a rare metabolic disorder - galactosemia,
- The mother has a dangerous infectious disease: HIV, AIDS or acute incurable tuberculosis,
- The mother must take medicines that pass into milk - for example , anti-cancer, lithium, ergotamine, methotrexate, tranquilizers or sleeping pills,
- Mother is addicted to drugs.
Feeding may be difficult if:
- Women has a rare lack of glandular tissue or damage to the nerves of the nipple due to trauma or surgery that change the taste of breast milk, can reduce the amount and cause anxiety in the baby,
- The baby has health problems (cleft lip or palate, Down's syndrome, serious heart disease),
- The child has a very severe allergy.
In case of problems, contact your midwife or family doctor. In maternity hospitals, you can get help with consultations on feeding, you can also consult by phone.
Ida-Tallinn Central Hospital Breastfeeding Advice Center open on weekdays from 10:00 to 14:00, telephone 6207453 or 53041783
Tel.0082 – 666 5829
Articles
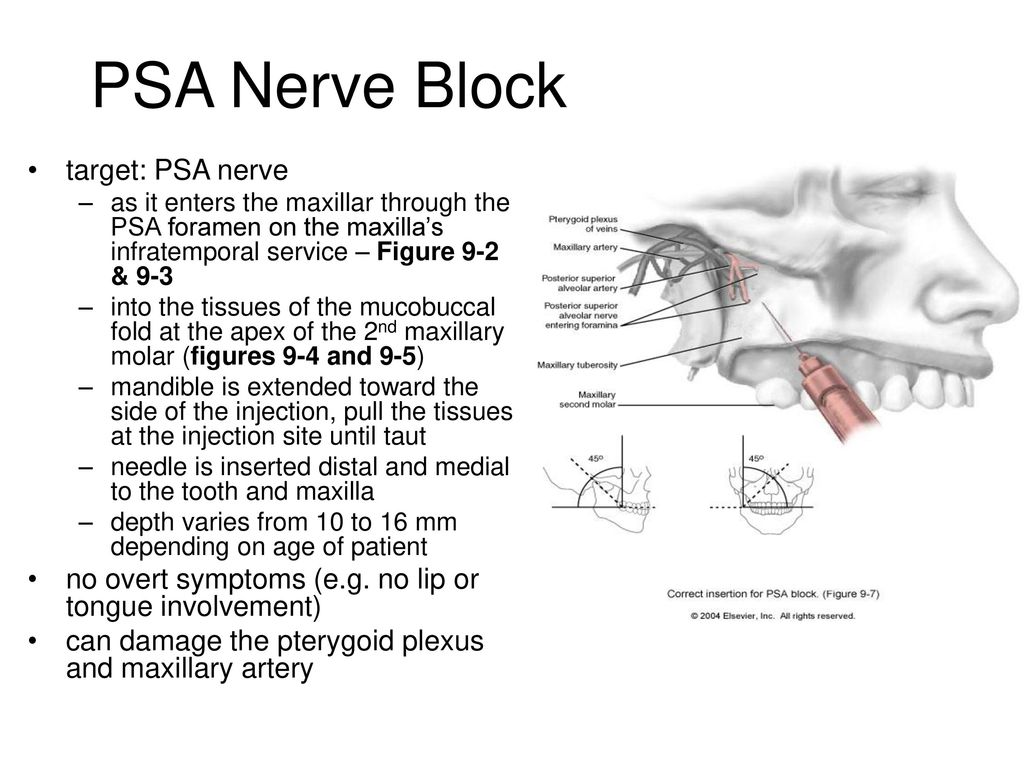
08/31/2020 Dental treatment with anesthesia while breastfeeding
Dental problems can occur at any age. Everyone is familiar with unbearable toothache, which does not allow a normal life. Attempts to remove it give only temporary relief, but a dentist can really help.
About whether teeth are treated during breastfeeding, how to do it so as not to harm the baby, and will be discussed in our article. From it you will learn the causes of dental diseases, is it possible to visit the dentist during breastfeeding, and most importantly, is it possible to continue feeding breastfeeding while visiting the dentist.
Causes of dental diseases
Tooth enamel is one of the strongest materials in the human body, but under the influence of various factors, even it begins to break down. The main cause of dental disease is the vital activity of bacteria, which cause caries. They absorb carbohydrates, releasing lactic acid, which destroys teeth. A “hole” in a tooth is formed when a lot of bacteria processes the food that has got there in a small space of the tooth, thereby releasing a large amount of acid.
The main cause of dental disease is the vital activity of bacteria, which cause caries. They absorb carbohydrates, releasing lactic acid, which destroys teeth. A “hole” in a tooth is formed when a lot of bacteria processes the food that has got there in a small space of the tooth, thereby releasing a large amount of acid.
This is not the only cause of dental disease. The causes are divided into congenital and acquired. In the first case, we are talking about teeth that have not yet grown. If the child's mother suffered a serious illness during pregnancy, received insufficient nutrition, then the child's teeth will be weak and prone to disease. This category also includes heredity.
In the second case, we are talking about factors affecting dental health, such as:
- absorption of excessive amounts of fluorine;
- mechanical damage;
- insufficient oral care;
- taking medication;
- lack of calcium or vitamin D.

Is it possible to visit the dentist during breastfeeding?
Often women face dental problems even during pregnancy, this is due to the fact that all valuable trace elements are spent on the formation and development of the fetus, and calcium deficiency begins in the mother's body. Lactation continues to aggravate the situation, but the woman is afraid to go to the dentist, so as not to harm the child. Actually teeth can not only be treated, but also necessary! There are several reasons for this.
Constant pain affects the psycho-emotional state of a person. The mother becomes nervous and irritable, which can directly affect the amount of milk, up to its complete disappearance.
Can breastfeeding continue during treatment?
Again, the answer is yes! Every mother worries that medicines will enter the child's body with milk, but modern anesthesia has no contraindications to breastfeeding.
The main thing is to warn the attending physician about your situation, and he will select the right drug.
How to prepare for treatment?
The main problem that arises before going to the dentist is fear. The best preparation is to find a good doctor that the woman can trust. For treatment, a positive attitude is needed, since increased emotional irritability can affect the effect of anesthesia.
Be sure to feed your baby before going to the doctor, since the first milk after treatment should be expressed.
If serious treatment is planned, it is necessary to consult with the doctor who sees you. He may advise you to stop breastfeeding, but do not stop it without the advice of a doctor.
If you have to stop breastfeeding, do not use a pacifier, the baby may get used to not breastfeeding. Also, to maintain lactation, milk must be expressed.
Basic principles
The main principle that guides the attending physician is to determine the optimal interval between feeding and excretion of the anesthetic from the mother's body.
The half-life of a modern anesthetic is at least 20 minutes. After two hours, the concentration of the drug in the body is no more than 1-2%, the risk of exposure to the child is minimized.
It happens that a tooth needs not only to be treated, but removed. In the presence of inflammatory diseases such as tonsillitis, stomatitis, oral candidiasis, gingivitis, colds, flu - tooth extraction is contraindicated!
Before removal, the following procedures must be carried out:
- the doctor takes an anamnesis;
- takes an x-ray;
- reveals contraindications;
- is collecting samples.
After the removal, the doctor will tell you how long not to feed the baby. The hole will hurt on the first day, you can take painkillers, but only after a doctor's recommendation. If the removal is accompanied by a purulent process, the doctor will prescribe antibiotics, The doctor will decide whether breastfeeding can be continued or should be interrupted .
If treatment with pain medications is safe, whitening is not such a harmless method. Whitening is more of a cosmetic than a medical procedure, but many mothers are wondering if it is safe to carry out during lactation. The procedure is harmful not so much because of the preparations used for whitening, but because the teeth are already weakened during this period.
After whitening, it takes time to restore the enamel, and since during breastfeeding, calcium is not supplied to the mother's body in sufficient quantities, the process may be delayed. Whitening during this period can damage your teeth and lead to cavities.
Effect of X-ray on lactation
If the doctor ordered an X-ray, then you should not be afraid:
- during the procedure, only the jaw and a little face are irradiated;
- protective elements are put on the chest that do not let rays through;
- the radiation dose is too low to affect the body in general and the quality of milk in particular.

Komarovsky's opinion
The well-known pediatrician Evgeny Olegovich also touched upon the topic of dental treatment during pregnancy and lactation. He is sure that if the mother took an insufficient amount of preparations containing calcium, then the problem with the teeth during lactation will be aggravated.
Dental treatment is necessary, especially if a woman is in severe pain, it promotes the production of adrenaline, which can adversely affect the fetus and milk supply. Komarovsky also draws attention to the need to report his condition to the attending physician.
Prevention
Any disease is easier to prevent than to treat later, this is especially true for nursing mothers, who are prohibited from a number of drugs. Measures to prevent dental diseases:
- oral hygiene is a guarantee of health;
- see your dentist regularly, pregnant and lactating women need more frequent check-ups, as their body is weakened and prone to disease;
- Use floss and mouthwash after every meal;
- choose pastes with fluorine;
- drink vitamin complexes containing calcium and vitamin D, but strictly on the advice of a doctor;
- eat foods containing calcium and vitamin D;
- change your toothbrush at least once a month;
These are basic tips and tricks for preventing oral disease.
Summarizing, we can say that teeth need to be treated, even if you are a nursing mother, especially if you experience unbearable pain. If the tooth still does not hurt, you should not bring caries to the destruction of the deep tissues of the tooth, especially since modern anesthetics are low-toxic, quickly excreted from the body and do not affect milk.
The main thing is to coordinate all actions with the doctor, be sure to inform the dentist that you are breastfeeding and tune in for treatment. Stress harms the mother and is bad for milk, and can also reduce the effectiveness of painkillers. Prevention is the best cure for disease!
Is it possible to treat and remove teeth with anesthesia during breastfeeding, do X-rays: rules for nursing mothers
During pregnancy, as well as after childbirth and during breastfeeding, almost every woman is faced with the choice of whether to treat her teeth or not. The growing fetus takes calcium from the mother's body, the condition of her teeth deteriorates significantly, therefore, with HB, the appearance of carious inclusions, flux, the development of serious oral diseases and loss of teeth are possible.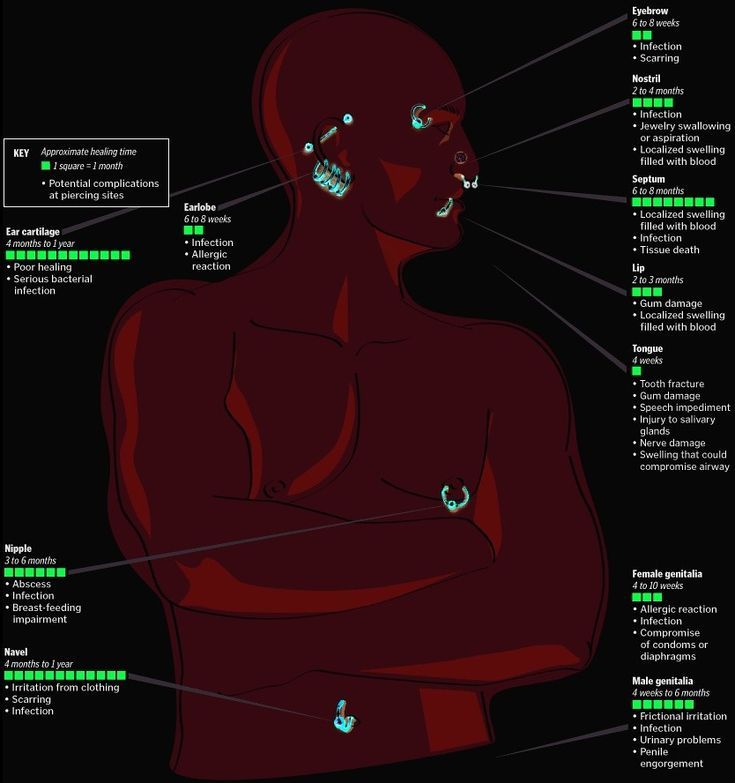 You can’t let everything take its course and be afraid of visiting the dentist, otherwise it will be extremely difficult to restore a beautiful smile in the future.
You can’t let everything take its course and be afraid of visiting the dentist, otherwise it will be extremely difficult to restore a beautiful smile in the future.
Dental treatment during lactation
Lactation is not a contraindication for dental treatment. Without treating the caries that has appeared or ignoring the pain, you can start irreversible processes in the oral cavity. Dental treatment during breastfeeding involves some prohibitions (taking antibiotics, implantation), but most often it is absolutely harmless. Otherwise, there is a risk of early loss of teeth and the appearance of severe inflammatory processes, as a result of which lactation will have to be stopped urgently.
Having taken care of the oral cavity during pregnancy and getting rid of caries and other problems, you can forget about it during lactation. The well-known doctor Komarovsky recommends that you definitely undergo treatment in the second trimester.
What can and can't be done with HB?
Tooth x-ray
Tooth x-ray is not contraindicated for nursing mothers.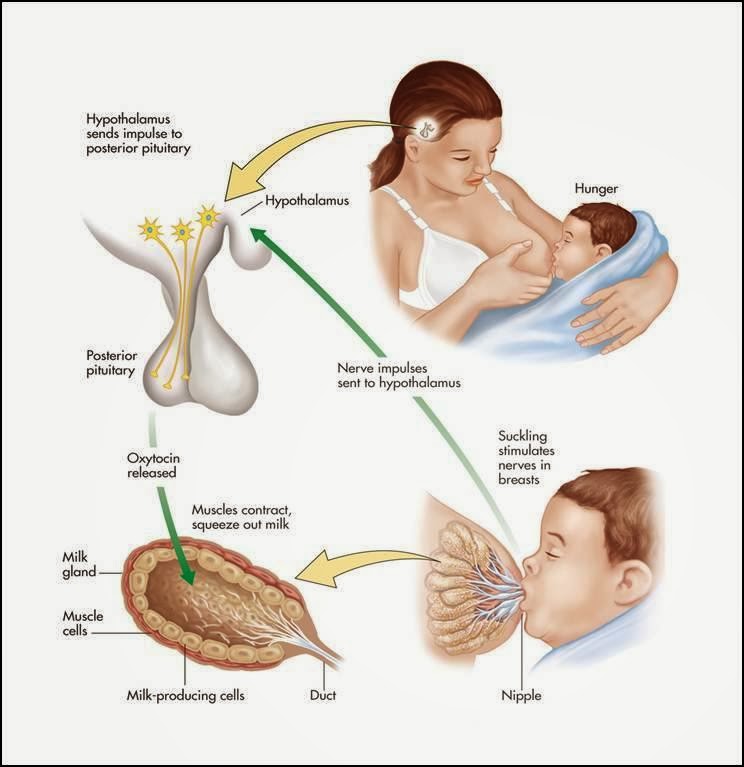 Doctors use a special protective apron that will save the baby from harmful compounds entering the body through milk. After the procedure is completed, it is necessary to express all the milk and pour it out, and at the next flush, you can already feed the baby. Do not worry if the amount of milk has decreased slightly after the x-ray. This is normal, so after a while lactation will be restored.
Doctors use a special protective apron that will save the baby from harmful compounds entering the body through milk. After the procedure is completed, it is necessary to express all the milk and pour it out, and at the next flush, you can already feed the baby. Do not worry if the amount of milk has decreased slightly after the x-ray. This is normal, so after a while lactation will be restored.
Treatment of caries or pulpitis
Treatment of caries, and even more so pulpitis, during breastfeeding is a necessary measure. Mechanical impact on the teeth of a nursing mother is not recommended only in one case: if she is in an unstable mental state caused by severe overwork.
- To eliminate pain, it is not forbidden to use anesthesia (Lidocaine, Ultracaine). It is worth remembering that modern drugs not only have a short half-life, but also do not affect the child in any way, since they enter the milk in small quantities.
- If further treatment requires antibiotics, consult your doctor.
 Antibacterial drugs can affect the health of the baby, so it is likely that breastfeeding will have to be stopped.
Antibacterial drugs can affect the health of the baby, so it is likely that breastfeeding will have to be stopped.
Wisdom tooth extraction
During breastfeeding, extraction of teeth, including wisdom teeth, is allowed. As a rule, with such a dental intervention, the same type of anesthesia is used as with filling. Modern drugs relieve the patient of pain and allow you to pull out a tooth without discomfort.
Another question if there is a need for antibiotics. The doctor must choose the appropriate treatment and prescribe drugs that are safe for her and the baby. The main thing is to warn the dentist about breastfeeding in advance.
Enamel whitening
Nursing mother should not endure toothache and caries. However, it is completely different when it comes to such a cosmetic procedure as whitening. It is not recommended to do it during lactation, since the recovery period after enamel whitening is much longer than in non-nursing women.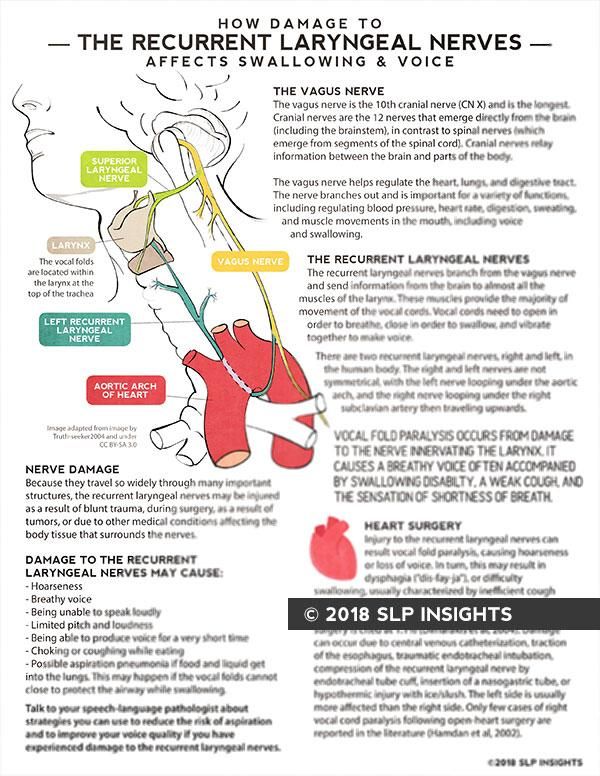 There is a risk of complications and the appearance of caries on bleached teeth due to insufficient amount of calcium absorbed by the mother's body.
There is a risk of complications and the appearance of caries on bleached teeth due to insufficient amount of calcium absorbed by the mother's body.
Whitening with special equipment can be replaced with toothpastes and professional gels intended for this purpose. Chewing gum is not prohibited. A more serious intervention can harm tooth enamel, so you should forget about a Hollywood smile for a while.
Types of anesthesia and contraindications
Anesthesia during the treatment and extraction of teeth is performed using topical preparations. Most often, dentists use Lidocaine. It is harmless to breastfeeding women and babies (with the exception of allergic reactions) because:
- Rare side effects;
- acts locally and for a short time;
- does not affect the functioning of internal organs;
- passes into milk in small quantities;
- has a short half-life.
The use of anesthesia during breastfeeding is possible at any stage. It will not harm the baby, if you remember a few things:
It will not harm the baby, if you remember a few things:
- to treat teeth after the 1st trimester of pregnancy;
- warn the doctor in advance about breastfeeding;
- do not use local anesthesia containing adrenaline;
- feed the child well before visiting the doctor;
- Express and discard the milk produced after the application of anesthesia (the drug is excreted from the body in about 5-6 hours).
Alternative
There are no alternatives to dental intervention in the presence of caries, pulpitis and other diseases of the oral cavity, since these problems can only be eliminated with the participation of a professional doctor.
Dental problems after childbirth
It should be noted that it is during the postpartum period that many women begin to notice that the condition of their teeth has worsened. There is such a common expression "teeth flew", which describes how rapidly dental problems arise in young mothers. And this is along with the fact that severe hair loss also begins, sometimes skin problems.
And this is along with the fact that severe hair loss also begins, sometimes skin problems.
Dental problems after childbirth are common
Indeed, such unpleasant changes are not uncommon. During lactation, the female body is significantly depleted - the reserves of calcium, various vitamins and minerals go first to bear the child, and then to feed him. Therefore, dental pathologies arise - caries, gum disease.
Usually the problem is already noticeable during pregnancy. But for some irrational reasons, future mothers are in no hurry to treat their teeth, postponing this moment for later. Meanwhile, if you do not treat the same gingivitis of pregnant women, a serious inflammation of the gums, the risk of premature birth increases significantly. Therefore, it is possible to treat teeth and gums during pregnancy, the most favorable period is the second trimester.
Hypertrophied form of gingivitis captures all gums
It is noted that untreated teeth during pregnancy, predisposition to dental problems, gum bleeding - all this becomes an imminent threat of urgent treatment approximately in the middle of lactation. And in order not to bring the matter to the extraction of teeth, the formation of large carious cavities, you need to go to the doctor, not being afraid of either the treatment itself or anesthesia.
And in order not to bring the matter to the extraction of teeth, the formation of large carious cavities, you need to go to the doctor, not being afraid of either the treatment itself or anesthesia.
When anesthesia is possible while breastfeeding
The first point that cannot be ignored is the refusal of anesthesia. Very often, patients ask for pain medication as soon as they sit in the dental chair. The doctor has not even touched the tooth yet, and the patient is already scared, and he wants to prevent pain with an anesthetic. And yet it is reasonable in such a situation, regardless of the condition (this is true for pregnant women, and for lactating women, and for women outside these special provisions), to give the doctor the opportunity to begin treatment without anesthesia. Sometimes, and quite often, there is simply no need for it. Either there is no pain at all, or it is tolerable, or the treatment process takes several minutes. In a word, you can suffer a little without resorting to anesthesia, which, one way or another, is stressful for any organism.