Natural birth with placenta previa
Placenta Previa: Can I Still Have a Natural Birth?
It’s disappointing to find out you have placenta previa. What does this mean for you and baby? What does it mean for your natural birth plan? Find out here.
You go to your 20-week anatomy scan and find out that your placenta is low lying or covering the cervix, known as placenta previa.
Or perhaps you skipped the 20-week scan and instead found out about your previa because of third trimester bleeding.
Either way, you’re disappointed and possibly scared.
What does this mean for you and your baby? And what does it mean for your natural birth plan?
We’ll answer those questions and more in this post.
What Is Placenta Previa?
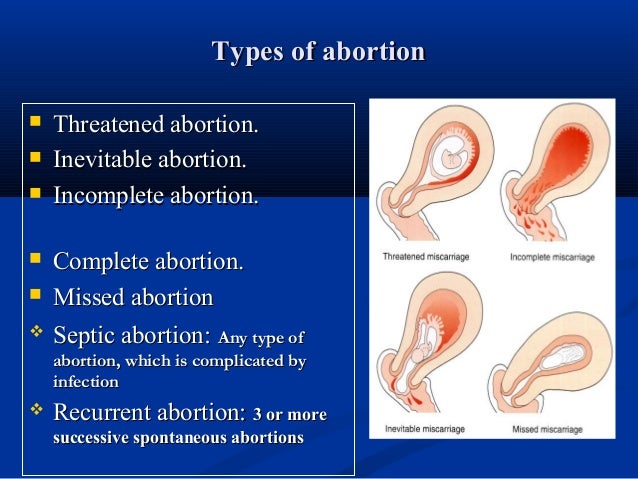
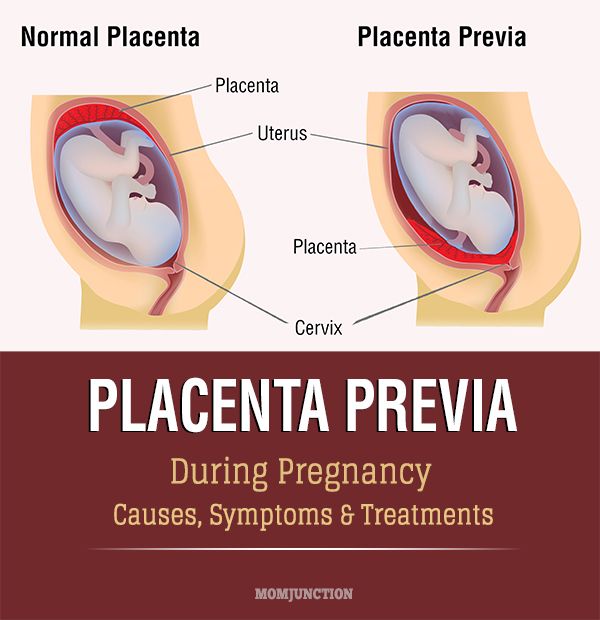
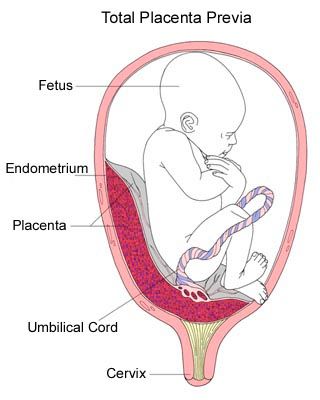
Typically the placenta (the organ that nourishes your baby during gestation) attaches to the upper part of the uterus. Placenta previa is a condition where the placenta is very low lying and/or covering all or part of the cervix. It affects 1 in 200 pregnancies by the third trimester. There are a few different kinds of previa:
- Total or complete previa – The placenta is covering the entire cervix.
- Marginal previa – The placenta is on the border of the cervix.
- Low-lying placenta – The placenta is within 2cm of the cervix but not bordering it.
What’s the big deal?
If you have placenta previa and the placenta is blocking your cervix, there’s no way for the baby to get out. Even if it’s only partly blocking or low lying, dilation may cause profuse bleeding which could cause death or require a blood transfusion. Additionally, placenta previa may cause:
- Slow fetal growth due to insufficient blood supply
- Fetal anemia
- Fetal distress due to low oxygen supply
- Infection and formation of blood clots
Pregnant? Get my FREE week-by-week updates! – Week by Week Promo [In-article]
Track your baby’s growth, find safe and natural remedies, and have fun along the way!
Get Pregnancy Updates!
Can I Prevent Placenta Previa?
There’s not much you can do to prevent placenta previa, though there are risk factors that you may or may not have any control over.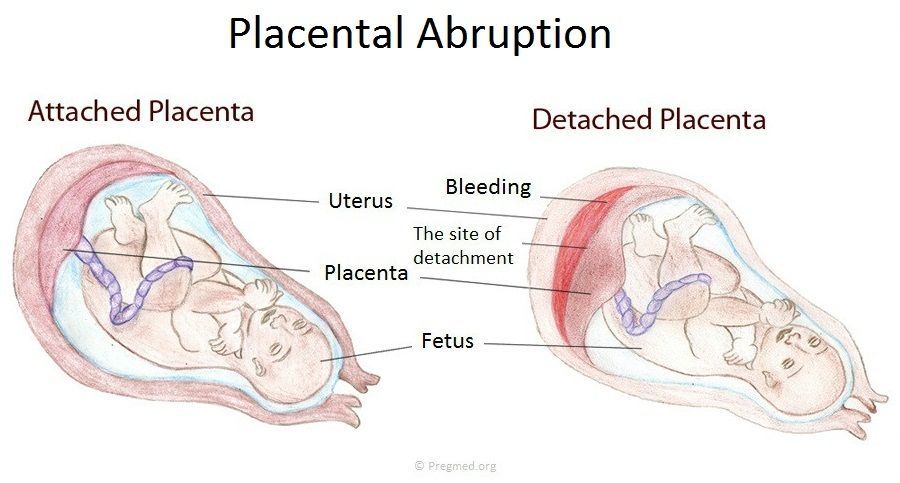 These include:
These include:
- Carrying multiples
- Having previously had a c-section
- Having had surgery on the uterus (fibroid removal, dilation and curettage (D&C), abortion, etc.)
- Having a short interpregnancy interval (the time between one pregnancy and the next)
- Being older than 35
- A previous condition of placenta previa
Diagnosis of Placenta Previa
Like placenta accreta, placenta previa doesn’t have many signs or symptoms. One most common sign is painless bleeding in the third trimester.
Other signs include:
- Pre-term contractions
- A transverse or breech baby
- Fundal measurements larger than expected
Diagnosis is often made from an ultrasound ordered after third trimester bleeding, or during the 20-week anatomy scan. However, as much as 90% of placentas seen as low-lying in the 20-week scan are no longer an issue in the third trimester. Because diagnosing a previa at that time is inaccurate at best, some mamas prefer to wait until closer to the third trimester for an ultrasound if they’re at all concerned about previa.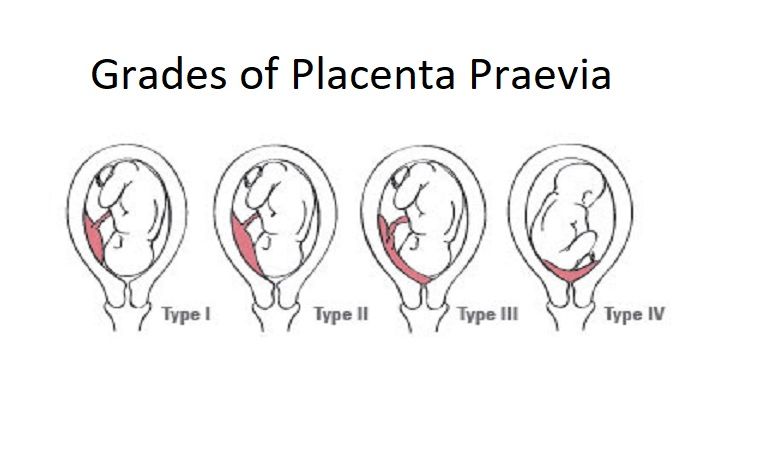
Treatment for Placenta Previa
When the placenta is low lying, like with a previa, there is increased risk of bleeding. This happens because the placenta is attached near or on the cervix which, when it dilates, can cause separation of the placenta from the uterus.
Treatment is bedrest and pelvic rest to reduce the risk of placental separation until as close to the due date as is safe. (Here’s our super accurate due-date calculator.) For many experiencing placenta previa, an early c-section may be necessary to avoid going into labor on your own.
What are my Birth Options with Placenta Previa?
With a marginal previa, where the placenta is near but not covering the cervix, you may be able to have a vaginal delivery. Many doctors will feel most comfortable if the placenta is 2cm away from the cervix, but talk with your doctor since each case is different. One study found that at least 60% of low-lying placenta cases ended with successful vaginal delivery. Your doctor will take into account whether there is also a placenta accreta present, which would likely mean a c-section is the safest route.
Your doctor will take into account whether there is also a placenta accreta present, which would likely mean a c-section is the safest route.
What’s a Natural Mama to Do?
If you have gotten a placenta previa diagnosis at your 20-week ultrasound, you will likely have nothing to worry about by delivery. Most placentas “move” higher in the uterus as the uterus grows so aren’t a problem by delivery.
If you are in your third trimester and your practitioner is still concerned about the placement of your placenta, you still have some options. As mentioned earlier, if your placenta is far enough away from the cervix, many doctors will be comfortable with a vaginal delivery (though they may ask you to labor in an operating room as a precaution). Ask for a second opinion if your doctor’s approach isn’t feeling right to you.
If you have a complete placenta previa, especially if an accreta is present, you likely need a c-section. This can be very disappointing for a natural mama.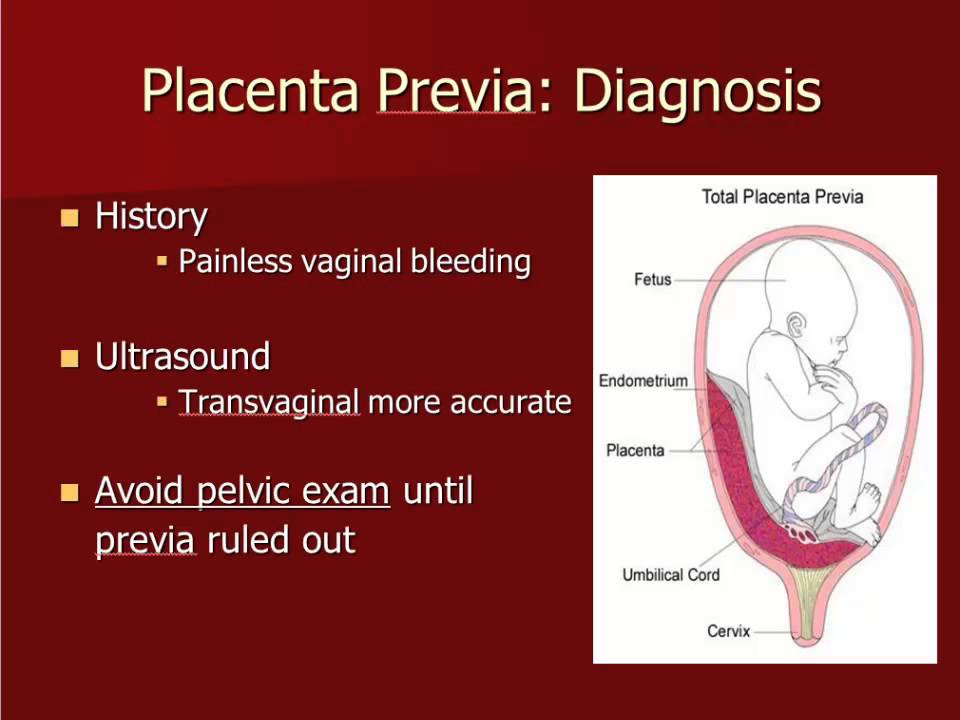 Just remember that your desire for a natural birth was so that you and your baby would have the safest birth experience. If a cesarean birth is medically needed to reach that goal, you are still a rockstar natural mama! Prepare for a gentle cesarean so that you and baby will have many of the health benefits of natural birth.
Just remember that your desire for a natural birth was so that you and your baby would have the safest birth experience. If a cesarean birth is medically needed to reach that goal, you are still a rockstar natural mama! Prepare for a gentle cesarean so that you and baby will have many of the health benefits of natural birth.
How About You?
What was your experience like with placenta previa? How did it affect your birth outcome?
Placenta Previa | March of Dimes
Placenta previa happens when the placenta lies low in the uterus and covers all or part of the opening to the vagina.
If you develop the condition early in your pregnancy, it usually isn’t a problem since the placenta grows upward with the uterus during pregnancy.
If you develop the condition later in pregnancy and the birth canal is blocked it can cause serious bleeding and may prevent vaginal delivery.
Talk with your providers about ways to deal with placenta previa, which could include having a planned c-section (caesarean birth).
The placenta attaches to the wall of the womb (uterus) and supplies the baby with food and oxygen through the umbilical cord.
Placenta previa is a condition in which the placenta lies very low in the uterus and covers all or part of the opening to the cervical opening that sits at the top of the vagina.
Placenta previa happens in about 1 in 200 pregnancies. If you have placenta previa early in pregnancy, it usually isn’t a problem because it may resolve as the pregnancy grows. However, if it persists it can cause serious bleeding and other complications later in pregnancy.
Normally, the placenta grows into the upper part of the uterus wall, away from the cervix. It stays there until your baby is born. During the last stage of labor, after the baby is born the placenta separates from the wall, and your contractions help push it into the birth canal (vagina). This is also called the afterbirth.
During labor, your baby passes through the cervix into the birth canal.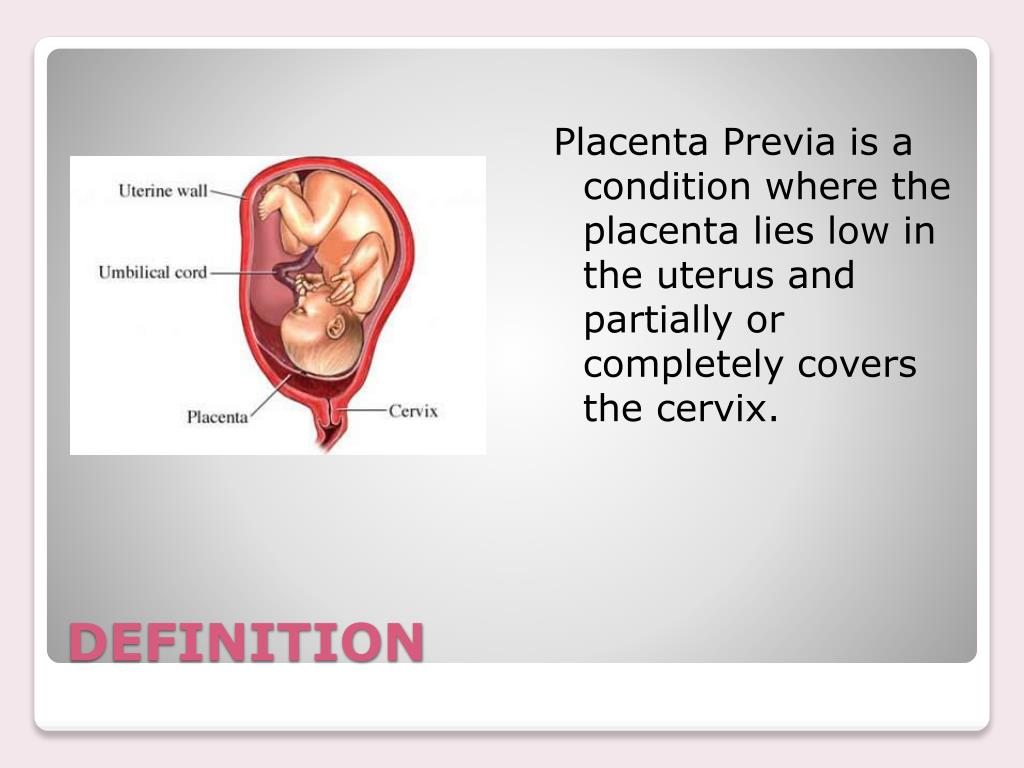 If you have placenta previa, when the cervix begins to thin out (efface) and open up (dilate), blood vessels connecting the placenta to the uterus may tear. This can cause severe bleeding during labor and birth, putting you and your baby in danger.
If you have placenta previa, when the cervix begins to thin out (efface) and open up (dilate), blood vessels connecting the placenta to the uterus may tear. This can cause severe bleeding during labor and birth, putting you and your baby in danger.
If a placenta previa is identified by ultrasound and appears to block the cervix, no vaginal exams are performed and an elective c-section is planned.
What causes placenta previa?
No one knows what causes placenta previa. However, you may be at higher risk for placenta previa if you:
- Have had a c-section in the past.
- Have had in vitro fertilization for infertility.
- Smoke cigarettes.
- Use cocaine.
- Are 35 or older.
- Have been pregnant before.
- Are pregnant with twins, triplets or more.
- Have had placenta previa in an earlier pregnancy.
- Have had surgery on your internal reproductive organs, such as myomectomy or tissue removal from the lining of your uterus (this is also called dilation and curettage or D&C).
 Some people have a D&C after miscarriage.
Some people have a D&C after miscarriage.
If you’ve had placenta previa before, what are your chances of having it again?
If you’ve had placenta previa in a past pregnancy, you have a 2 to 3 in 100 (2 to 3 percent) chance of having it again.
What are the symptoms of placenta previa?
Most of the time, placenta previa has no symptoms; it is often found during a routine ultrasound test.
For those who do have symptoms, the most common is painless bleeding from the vagina during the second half of pregnancy. You also may have contractions. Call your health care provider right away if you have vaginal bleeding anytime during your pregnancy. If the bleeding is severe, go to the hospital.
Not everyone who has placenta previa has vaginal bleeding. In fact, about one-third of people with placenta previa don’t have this symptom.
How is placenta previa diagnosed?
A prenatal test that uses sound waves to show a picture of your baby in the womb (ultrasound) usually can find placenta previa and determine the placenta’s location. In some cases, your provider may do an ultrasound through the birth canal (transvaginal ultrasound) or a translabial ultrasound instead. In places where it’s available, three-dimensional ultrasound may be used.
In some cases, your provider may do an ultrasound through the birth canal (transvaginal ultrasound) or a translabial ultrasound instead. In places where it’s available, three-dimensional ultrasound may be used.
Even if you don’t have vaginal bleeding, a routine, second trimester ultrasound may show that you have placenta previa. Don’t be too worried if this happens. Placenta previa found in the second trimester requires repeat follow-up ultrasounds to assure that the cervix is no longer blocked. If the placenta is no longer covering the cervical opening, you can usually have a vaginal delivery.
How is placenta previa treated?
Treatment depends on how far along you are in your pregnancy, the seriousness of your bleeding and the health of you and your baby. The goal is to keep you pregnant as long as possible. Your provider may recommend no vaginal exams or sex to prevent damage to the placenta and bleeding. Providers recommend c-section for nearly everyone with placenta previa to prevent severe bleeding.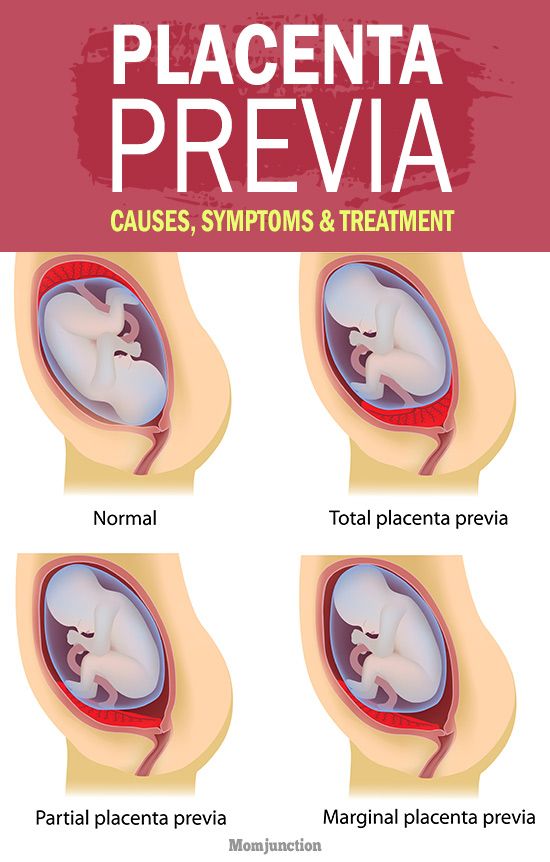
If you are early in your pregnancy and have no symptoms, your provider will probably recommend no treatment, but will schedule follow-up ultrasounds to make sure everything is normal.
If you are bleeding as a result of placenta previa, you need to be closely monitored in the hospital. If tests show that you and your baby are doing well, your provider may give you treatment to try to keep you pregnant for as long as possible.
If you have a lot of bleeding, you may be treated by having new blood put into your body (blood transfusions). Your provider also may give you medicines called corticosteroids to help speed up development of your baby’s lungs and other organs in case a preterm delivery is needed.
Your provider may want you to stay in the hospital until you give birth. If the bleeding stops, you may be able to go home. If you have severe bleeding due to placenta previa at about 34 to 36 weeks of pregnancy, your provider may recommend an immediate c-section.
At 36 to 37 weeks, your provider may suggest an amniocentesis to test the amniotic fluid around your baby to see if the lungs are fully developed. If they are, your provider may recommend an immediate c-section to avoid risks of future bleeding. Nowadays, providers may use corticosteroids to help the baby lung development while you are pregnant and to help avoid an immediate c-section.
If they are, your provider may recommend an immediate c-section to avoid risks of future bleeding. Nowadays, providers may use corticosteroids to help the baby lung development while you are pregnant and to help avoid an immediate c-section.
At any stage of pregnancy, an emergency c-section may be necessary if you have dangerously heavy bleeding or if you and your baby are having problems.
Is there anything you should avoid if you have placenta previa?
If you have placenta previa that doesn’t require immediate treatment right away, your provider may recommend that you avoid doing the following:
- Having sex that leads to orgasm
- Vaginal penetration or vaginal examinations
- Moderate and strenuous exercise
- Lifting more than 20 pounds
- Standing for more than four hours
All of these activities could lead to contractions that could lead to bleeding.
How can you reduce your risk for complications if you have placenta previa?
Have an ultrasound in the second trimester to identify location of the placenta.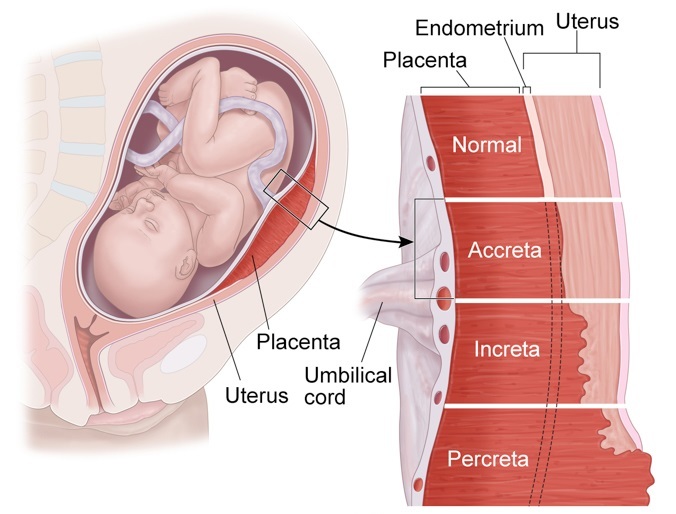 You may need follow up ultrasounds to help plan for a safe birth and delivery.
You may need follow up ultrasounds to help plan for a safe birth and delivery.
Follow your providers precaution instructions to prevent bleeding or complications. Contact your provider and go to the hospital if you have bleeding at any time during your pregnancy.
We don’t know how to prevent placenta previa, but you may be able to reduce your risk by not smoking and not using cocaine.
You also may be able to lower your chances of having placenta previa in future pregnancies by having a c-section only if it’s medically necessary. If your pregnancy is healthy and there are no medical reasons for you to have a c-section, it’s best to let labor begin on its own.
Last reviewed: January, 2022
Save the future - articles from the specialists of the clinic "Mother and Child"
SAVE THE FUTURE
PREGNANCY COMPLICATIONS ARE NOT SO RARE. IF A WOMAN DOES NOT UNDERSTAND WHAT IS HAPPENING TO HER, THEN STARTS TO PANIC AND THEREFORE ONLY aggravates the SERIOUS SITUATION.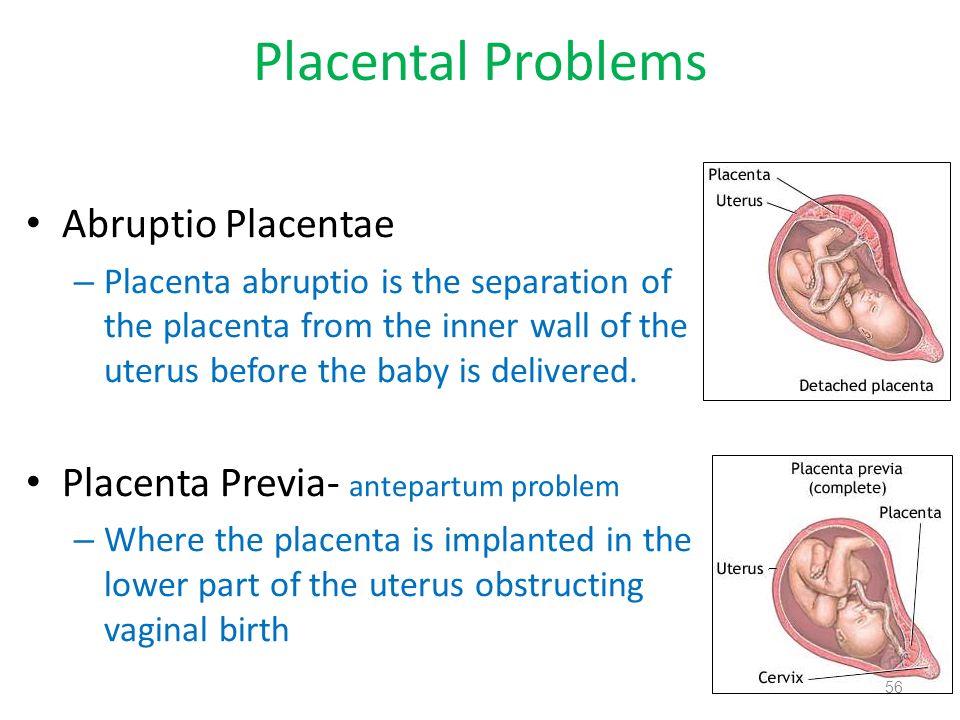 WHEN THE FUTURE MOTHER HAS A CLEAR VIEW OF THE CURRENT SITUATION, AND SHE REALIZES WHAT AND WHY DOCTORS DO, AND STRICTLY FOLLOWS THEIR RECOMMENDATIONS, IT IS EASIER FOR DOCTORS TO ACHIEVE SUCCESS AND SAVE THE PREGNANCY. nine0005
WHEN THE FUTURE MOTHER HAS A CLEAR VIEW OF THE CURRENT SITUATION, AND SHE REALIZES WHAT AND WHY DOCTORS DO, AND STRICTLY FOLLOWS THEIR RECOMMENDATIONS, IT IS EASIER FOR DOCTORS TO ACHIEVE SUCCESS AND SAVE THE PREGNANCY. nine0005
Pregnancy is a significant and very important period in the life of every woman. It can be divided into three trimesters, in each of which an “abnormal” situation may arise, that is, a complication of pregnancy. In such circumstances, the main thing is not to panic, but to immediately seek medical help. In order not to miss the moment and notice the first signs of trouble in time, the expectant mother should know what complications can occur in each of the trimesters and their symptoms. nine0006
I TRIMESTR
ERROR IS OUT
For the first time, a woman is suspected of being pregnant when her period is delayed. To make sure that this is really the case, a blood test for human chorionic gonadotropin, a hormone whose level rises sharply during pregnancy, helps.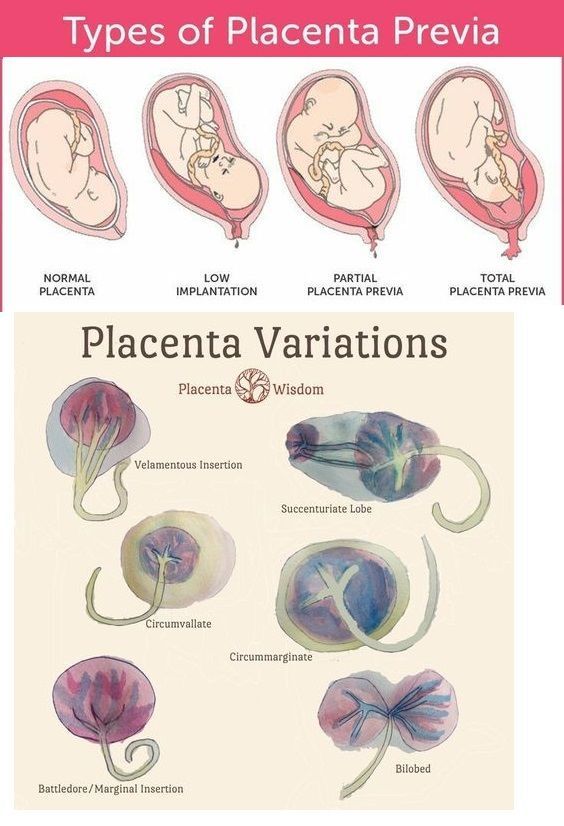 And here it is necessary, without delay, to visit an obstetrician-gynecologist and do an ultrasound. It should confirm that the fetal egg is in the uterine cavity. Sometimes (recently, according to the literature, the percentage is growing), a fetal egg can also attach outside the uterine cavity. nine0006
And here it is necessary, without delay, to visit an obstetrician-gynecologist and do an ultrasound. It should confirm that the fetal egg is in the uterine cavity. Sometimes (recently, according to the literature, the percentage is growing), a fetal egg can also attach outside the uterine cavity. nine0006
In this case, one speaks of an ectopic pregnancy. Its most common form is tubal, when the fetal egg begins to develop in the fallopian tube. It happens that it is attached in the ovary, abdominal cavity or in the cervix. This condition is life-threatening and requires urgent surgical intervention. The risk is that no organ other than the uterus itself is fit for carrying a baby. A pipe, for example, has a very small volume and, under the “onslaught” of a growing embryo, it will burst sooner or later. The resulting bleeding poses a serious threat to a woman's life. nine0006
Against the background of a delay in menstruation, paroxysmal pains, often accompanied by weakness, dizziness, nausea, and bloody discharge from the genital tract, should cause anxiety.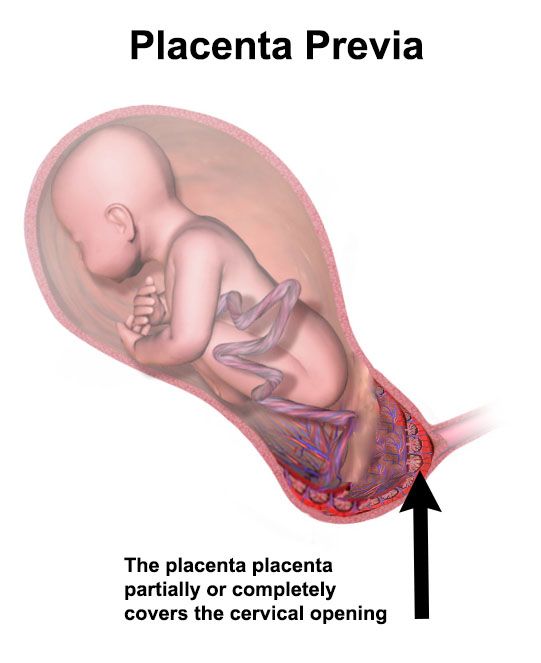 It is urgent to go to the doctor, since it is possible to accurately determine an ectopic pregnancy only with the help of ultrasound. When an ectopic pregnancy is detected, laparoscopic surgery is most often performed. After restorative treatment, a normal pregnancy often occurs.
It is urgent to go to the doctor, since it is possible to accurately determine an ectopic pregnancy only with the help of ultrasound. When an ectopic pregnancy is detected, laparoscopic surgery is most often performed. After restorative treatment, a normal pregnancy often occurs.
EXPECTED COMPLICATION - TOXICOSIS
Everyone has heard about it, everyone is waiting with horror when it comes. What is it? That's right - toxicosis. The most anticipated and most common complication of early pregnancy. Mild nausea, intolerance to certain odors, sometimes dizziness - these are the symptoms of early toxicosis, which, not without reason, are also considered indirect signs of pregnancy.
If vomiting is repeated no more than 3-5 times a day and the expectant mother generally feels fine, there is no need to change her usual lifestyle. But when nausea and vomiting occur 10 or even 20 times a day and any food and even a sip of water do not go for the future, a woman needs hospitalization.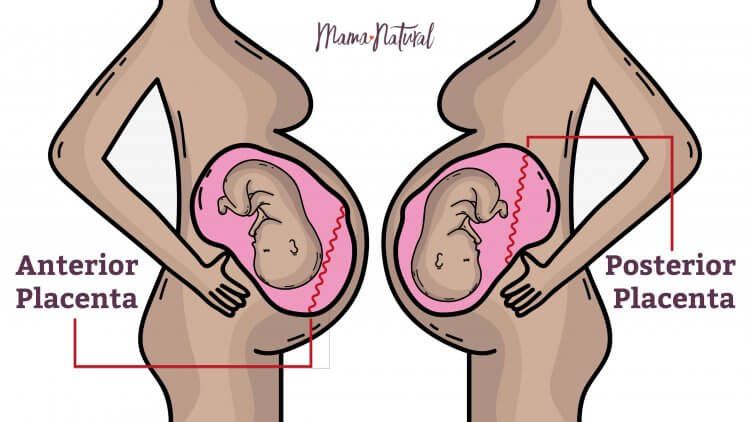 Lack of food and dehydration - that's what will worry doctors the most. After all, the expectant mother is losing weight, heart palpitations begin, blood pressure drops, but she needs strength to carry the baby. In the hospital, the fluid deficiency will be replenished with the help of droppers, vomiting will be eliminated with the help of special medications approved for pregnant women, and a full examination of the expectant mother will be carried out. Thanks to this, the unborn child and his expectant mother will feel much better and return to their normal lifestyle again. nine0006
Lack of food and dehydration - that's what will worry doctors the most. After all, the expectant mother is losing weight, heart palpitations begin, blood pressure drops, but she needs strength to carry the baby. In the hospital, the fluid deficiency will be replenished with the help of droppers, vomiting will be eliminated with the help of special medications approved for pregnant women, and a full examination of the expectant mother will be carried out. Thanks to this, the unborn child and his expectant mother will feel much better and return to their normal lifestyle again. nine0006
I-II TRIMESTER
THREAT OF TERMINATION OF PREGNANCY
At the beginning of pregnancy, this condition is associated with a hormonal imbalance. For some reason, the hormones that support pregnancy begin to be produced in smaller quantities. Genetic malformations of the embryo can also provoke such a complication. This will seem strange to many, but in Western Europe, doctors do not seek to keep the pregnancy at any cost in the early stages.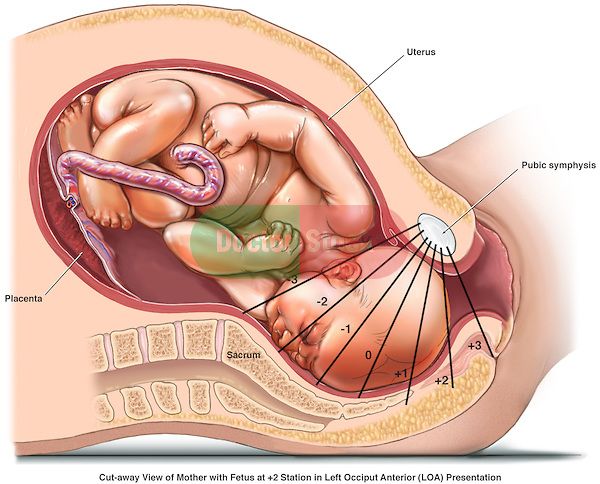 It is believed that in this way nature conducts natural selection. nine0006
It is believed that in this way nature conducts natural selection. nine0006
No matter how you feel about this problem and whatever the causes of the complication, the expectant mother should be alerted by pulling pains in the lower abdomen and lower back, bloody discharge from the genital tract. Any of these symptoms may indicate a threatened miscarriage. Moreover, if there is a discharge, the doctors diagnose "a miscarriage that has begun", but this does not mean that the situation cannot be reversed and the situation normalized. So, when you see such a record in medical documents, do not be alarmed. Doctors will make every effort to still save the pregnancy. nine0006
And in order for the efforts of doctors to be successful, you should visit a doctor as soon as possible and have an ultrasound scan done. With it, you can find out how the pregnancy develops, but if a woman is concerned about the discharge, then find out their cause: for example, malformations of the uterus or too low location of the placenta, as well as premature opening of the cervix caused by its shortening (isthmic-cervical insufficiency - ICI ).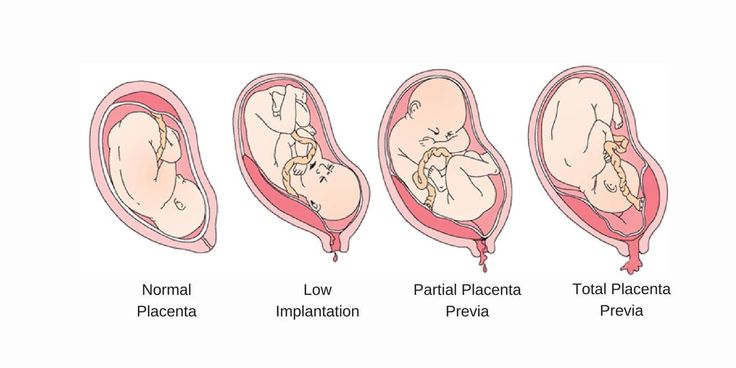 Another mandatory study is the level of hormones in the urine and blood.
Another mandatory study is the level of hormones in the urine and blood.
In any case, bleeding, too much pain in the lower abdomen, increased uterine tension are a good reason for hospitalization. If hormonal deficiency is detected, hormonal therapy is prescribed to maintain the pregnancy. With a low location of the placenta, a woman will be advised to lead a calm lifestyle and take drugs that relieve tension in the uterus.
When signs of CCI are detected, the cervix is sutured. All these measures help to prolong the pregnancy to full term - 37 weeks. If the baby is still born earlier, modern equipment and advances in medicine make it possible to nurse babies even with low body weight (from 500 g). nine0006
III TRIMESTER
PLACENTA PRESENTATION
The placenta is formed during pregnancy and is excreted from the body after childbirth. Normally, it should be located in the upper and middle third of the uterus so that the child can be safely born at the time appointed by nature. If the placenta occupies a place near the exit from the uterus, is attached at least partially to the cervix, they speak of placenta previa. The reasons for this situation may be malformations of the internal genital organs, chronic inflammation of the uterus and others. nine0006
If the placenta occupies a place near the exit from the uterus, is attached at least partially to the cervix, they speak of placenta previa. The reasons for this situation may be malformations of the internal genital organs, chronic inflammation of the uterus and others. nine0006
A characteristic symptom is bloody discharge from the genital tract, most often after 7 months of pregnancy. To determine this complication, it is enough to do an ultrasound. The woman is recommended hospitalization and bed rest, as well as drug therapy. If placenta previa persists at the time of delivery, the baby can only be born by caesarean section. The expectant mother is hospitalized at the 37-38th week of pregnancy (at this time the pregnancy is considered full-term) in order to prepare for the operation. But if a woman has heavy bleeding, a caesarean section will have to be done on an emergency basis. nine0006
PLACENTAL DETECTION
This complication occurs when the placenta separates from the uterine wall before the baby is born.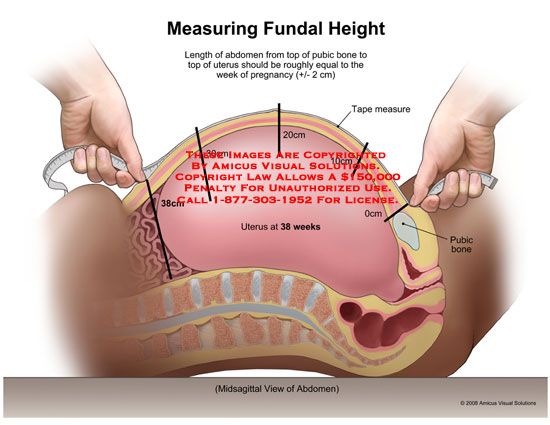 Most often this occurs at the end of the third trimester or during childbirth. Women with high blood pressure are most at risk, which is why doctors strongly recommend expectant mothers to carefully monitor their blood pressure levels and strictly follow the doctor's recommendations when it rises.
Most often this occurs at the end of the third trimester or during childbirth. Women with high blood pressure are most at risk, which is why doctors strongly recommend expectant mothers to carefully monitor their blood pressure levels and strictly follow the doctor's recommendations when it rises.
An expectant mother should be alerted by prolonged abdominal pain, increased activity of the uterus, bleeding from the genital tract. This situation is risky both for the woman herself and for her unborn child. The woman is threatened with blood loss, and the baby is in danger of hypoxia: extensive placental abruption in the truest sense of the word cuts off oxygen to him. The actions of doctors depend on how strong the labor activity is and how great the woman's blood loss is. If the bleeding is weak, the contractions continue, the baby's heartbeat is normal, the baby feels good, the doctors allow the birth to go naturally, but closely monitor the well-being of the mother and baby. With heavy bleeding and the appearance of signs of hypoxia in crumbs, an emergency caesarean section is performed.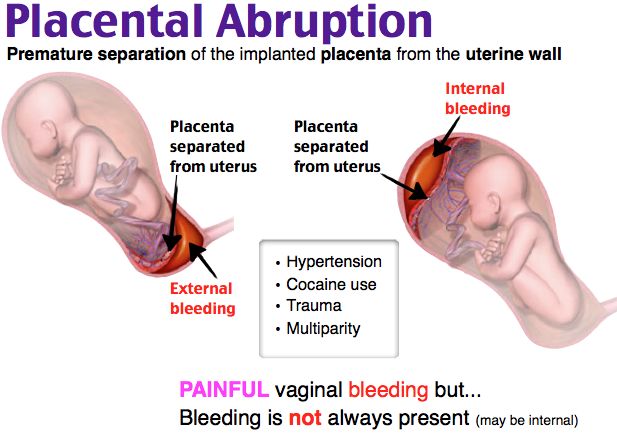 nine0006
nine0006
PREMATURE ROUTING OF WATER
This complication is said to occur when the amniotic fluid breaks before contractions begin. There can be many reasons for this development of events, but the main one is infection. That is why doctors carefully monitor expectant mothers and during pregnancy several times do bacteriological culture of flora from the cervical canal. According to modern international recommendations, it is also desirable to take a smear for group B streptococci before childbirth at about 36-37 weeks. If an infection is detected during childbirth, a woman is given antibiotic therapy. nine0006
If the amniotic fluid is shed, regardless of the gestational age, call an ambulance or go to the maternity hospital. Making sure that this is really amniotic fluid is quite simple. If the flow of urine can be stopped by tensing the muscles, then the amniotic fluid will continue to flow even if the muscles are tensed. In addition, you can use the amniotest (test for amniotic fluid). If amniotic fluid is expelled, the test strip will change color. There are also special pads that are much easier to use. The principle of their action is the same: if amniotic fluid gets on them, the pads change color. nine0006
If amniotic fluid is expelled, the test strip will change color. There are also special pads that are much easier to use. The principle of their action is the same: if amniotic fluid gets on them, the pads change color. nine0006
You should also see a doctor if the amniotic fluid starts to leak a little. Only a doctor can clarify the situation. Don't refuse hospitalization. If the leakage intensifies, medical attention is indispensable. In most cases, after the outflow of amniotic fluid, a woman and her unborn child begin to prepare for childbirth. If this happened before the 34th week of pregnancy, the baby is given medication to help his lungs open up. But when the waters have not completely poured out, it is possible to prolong the pregnancy. And the efforts of doctors will be directed precisely at this. nine0006
PRE-ECLAMPSIA
Another insidious complication in late pregnancy is preeclampsia, or, as it used to be called, preeclampsia. Another name for this complication is late toxicosis of pregnant women. Its main symptom is the presence of protein in the urine. It is for this reason that during pregnancy it is necessary to take this analysis so often. In addition, preeclampsia is manifested by an increase in blood pressure up to 130/90 mm Hg. and above, internal and external edema, due to which the expectant mother gains excess weight. DO NOT refuse hospitalization: adverse symptoms may increase, due to which the well-being of the unborn baby may deteriorate sharply. Complex therapy prescribed by the attending physician, as a rule, leads to a positive result. If the symptoms increase, you have to resort to emergency delivery - depending on the situation, induce labor or do a caesarean section. nine0006
Its main symptom is the presence of protein in the urine. It is for this reason that during pregnancy it is necessary to take this analysis so often. In addition, preeclampsia is manifested by an increase in blood pressure up to 130/90 mm Hg. and above, internal and external edema, due to which the expectant mother gains excess weight. DO NOT refuse hospitalization: adverse symptoms may increase, due to which the well-being of the unborn baby may deteriorate sharply. Complex therapy prescribed by the attending physician, as a rule, leads to a positive result. If the symptoms increase, you have to resort to emergency delivery - depending on the situation, induce labor or do a caesarean section. nine0006
To avoid trouble, doctors advise expectant mothers not to abuse salt, but rather to stop consuming it, lead a healthy lifestyle, drink 2 liters of fluid a day and observe a sleep and rest regimen.
A.V.A.T.A.R. - Marginal placenta previa
Marginal placenta previa is a pathological attachment of an embryonic organ that provides a connection between the mother and the fetus, in which there is a partial overlap of the internal os of the uterus (no more than a third of it).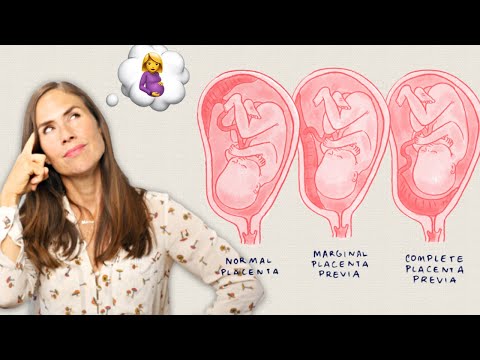 Clinically, the disease is manifested by bleeding of varying intensity, not accompanied by discomfort. It is possible to identify marginal placenta previa with the help of a planned ultrasound in the second trimester or when pathological signs occur. Treatment involves hospitalization, bed rest, symptomatic therapy. Expectant management is indicated before the term of the expected birth, subject to the normal condition of the woman and the fetus. nine0006
Clinically, the disease is manifested by bleeding of varying intensity, not accompanied by discomfort. It is possible to identify marginal placenta previa with the help of a planned ultrasound in the second trimester or when pathological signs occur. Treatment involves hospitalization, bed rest, symptomatic therapy. Expectant management is indicated before the term of the expected birth, subject to the normal condition of the woman and the fetus. nine0006
Marginal placenta previa is a pathology of pregnancy, accompanied by abnormal attachment of the placenta and partial overlap of the internal os of the uterus. This condition is dangerous for both the woman herself and the fetus. Marginal placenta previa in the early stages is associated with less risk, since with the subsequent growth of the baby and stretching of the myometrium, it can shift and acquire the correct location. Otherwise, there is a possibility of squeezing the supply vessels, partially blocking the access of oxygen and nutrients to the fetus, which can cause its hypoxia and even antenatal death. nine0006
nine0006
Marginal placenta previa can lead to placental abruption. This is due to the fact that the lower segment of the uterus has less ability to stretch. Also, marginal placenta previa often provokes massive bleeding during childbirth. Such an outcome is possible during natural childbirth, if there was a sharp separation of the membranes as a result of the passage of the fetus through the birth canal. In obstetrics, placenta previa occurs predominantly in repeated pregnancies. Pathology requires careful monitoring, since in about 25% of cases it is accompanied by stillbirth. nine0006
Marginal placenta previa may be due to abnormal attachment of the trophoblast during implantation or anatomical features of the myometrium. In the latter case, a violation of the structure of muscle fibers in the wall of the uterus occurs against the background of inflammatory changes, the consequences of genital infections. Marginal placenta previa is more often diagnosed with thinning of the myometrium, provoked by frequent curettage and abortion.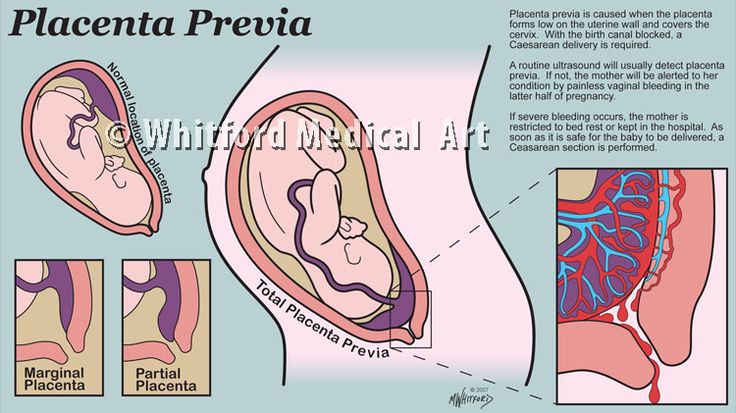 Also, the cause of abnormal attachment of the trophoblast can be uterine deformities caused by benign tumors or resulting from congenital pathologies. nine0006
Also, the cause of abnormal attachment of the trophoblast can be uterine deformities caused by benign tumors or resulting from congenital pathologies. nine0006
Marginal placenta previa often develops in women with concomitant diseases of the internal organs, in particular, with the pathology of the cardiovascular system. Due to insufficient blood circulation and congestion in the pelvis, the placenta cannot fully attach. In addition, marginal placenta previa is possible against the background of abnormal development of the embryo immediately after fertilization. A similar outcome is observed with a belated appearance of the enzymatic functions of the trophoblast. As a result, it attaches to the myometrium later than it normally does, staying in the lower part of the uterus. nine0006
Marginal placenta previa can be of two types depending on the place of its attachment:
- Localization along the anterior wall is the most dangerous variant of the pathology. With marginal placenta previa of this type, there is a high risk of mechanical damage to it, followed by detachment due to the physical activity of the woman, the movements of the baby, against the background of a strong stretching of the uterus in the third trimester of pregnancy.
 Despite this, when placing the embryonic organ on the anterior wall of the uterus, there is a possibility of its movement upwards. nine0122
Despite this, when placing the embryonic organ on the anterior wall of the uterus, there is a possibility of its movement upwards. nine0122 - Posterior attachment is a more favorable variant of marginal placenta previa. It is accompanied by a lower risk of complications in the process of gestation and childbirth for the mother and baby.
Both types of anomalies are pathologies of pregnancy and require obligatory observation by an obstetrician-gynecologist.
Marginal placenta previa has a characteristic symptomatology - the appearance of bloody discharge without deterioration in general well-being. Often this pathological symptom occurs at rest or at night. As for the timing of embryogenesis, the marginal placenta previa manifests itself mainly at 28-32 weeks. It is during this period that the uterus is characterized by increased activity due to the preparation of the myometrium for the upcoming birth. Somewhat less often, abnormal discharge is observed already at the beginning of the second trimester.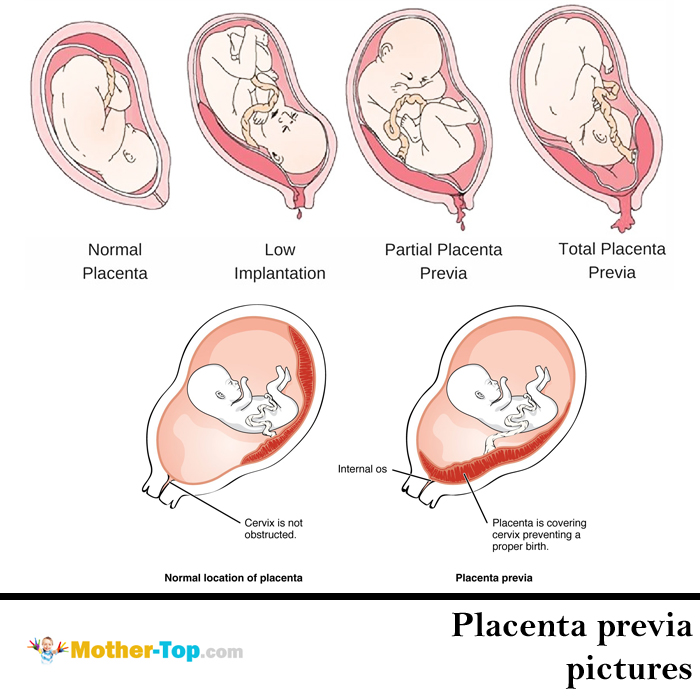 The volume of bleeding can be different and depends on the degree of damage to the vessels. nine0006
The volume of bleeding can be different and depends on the degree of damage to the vessels. nine0006
With marginal placenta previa in the third trimester of pregnancy, bleeding can be triggered by physical activity, sexual intercourse, fetal movement and other factors that provoke rupture of nutrient vessels. The appearance of this symptom is possible even during a gynecological examination. Sometimes marginal placenta previa is combined with the threat of miscarriage. With this combination, there is discomfort in the lower abdomen, hypertonicity of the uterus. With systematic bleeding in pregnant women with such a diagnosis, iron deficiency anemia develops. In such cases, there is increased fatigue, weakness. On the part of the fetus, growth and development may be slowed down, hypoxia due to insufficient intake of nutrients. Marginal placenta previa is often combined with an abnormal position of the fetus, which can be oblique or transverse. nine0006
A provisional diagnosis is established on the basis of the patient's complaints of spotting in the absence of pain.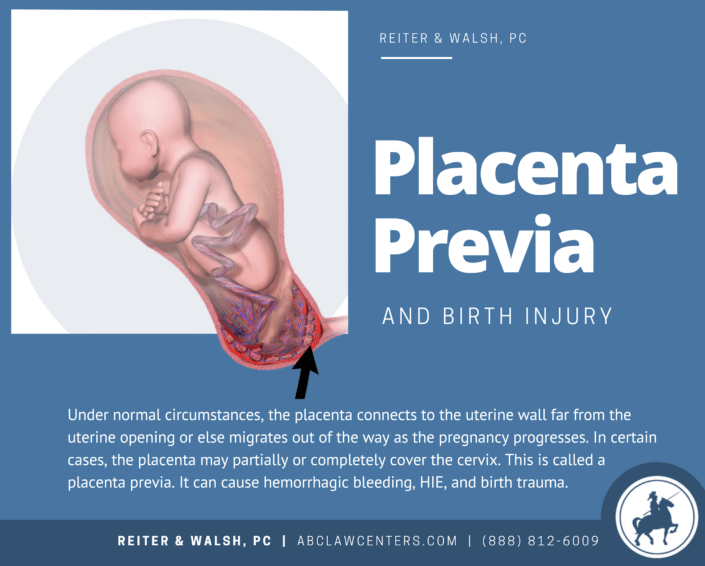 Another characteristic sign of the abnormal location of the embryonic organ is the high standing of the uterine fundus, which does not correspond to the period of embryogenesis. It is possible to confirm the marginal presentation of the placenta with the help of ultrasound. During the scanning process, a specialist can accurately visualize the location of the placenta and the degree of overlap of the uterine os, determine the condition of the child and assess the possible risks to the woman and the fetus. nine0006
Another characteristic sign of the abnormal location of the embryonic organ is the high standing of the uterine fundus, which does not correspond to the period of embryogenesis. It is possible to confirm the marginal presentation of the placenta with the help of ultrasound. During the scanning process, a specialist can accurately visualize the location of the placenta and the degree of overlap of the uterine os, determine the condition of the child and assess the possible risks to the woman and the fetus. nine0006
Treatment of placenta previa depends on the identified symptoms, the period of embryogenesis, as well as the condition of the expectant mother and fetus. If the diagnosis is established only on the basis of ultrasound scanning and bleeding is not observed, it is possible to control the patient's condition on an outpatient basis. Hospitalization is indicated if marginal placenta previa is accompanied by secretions of any volume of blood. In this case, careful monitoring in the hospital is required. Women with such a diagnosis are assigned complete rest, it is recommended to exclude sexual intercourse and stress. You must wear a bandage. In the second trimester, a special exercise therapy for pregnant women sometimes helps to correct the location of the placenta. nine0006
Women with such a diagnosis are assigned complete rest, it is recommended to exclude sexual intercourse and stress. You must wear a bandage. In the second trimester, a special exercise therapy for pregnant women sometimes helps to correct the location of the placenta. nine0006
Marginal placenta previa often develops anemia due to systematic blood loss. Therefore, pregnant women are shown a diet enriched with foods high in iron. The diet should contain red fish, offal, buckwheat, beef, apples. Pregnancy management with marginal placenta previa involves a protective regime in order to achieve the expected date of birth and the birth of a full-term baby. Also, patients with a similar diagnosis are prescribed medications, taking into account the general condition and comorbidities. nine0006
In case of marginal placenta previa, symptomatic drug therapy is carried out. With uterine hypertonicity, tocolytics and antispasmodics are used, and preparations containing iron are prescribed to eliminate anemia. To maintain the general condition of the patient and the fetus, vitamin complexes can be used. Sometimes, with marginal placenta previa, it is advisable to use sedatives. According to indications, antiplatelet agents are introduced, the doctor calculates the dosage of drugs in order to avoid a negative impact on the baby. nine0006
To maintain the general condition of the patient and the fetus, vitamin complexes can be used. Sometimes, with marginal placenta previa, it is advisable to use sedatives. According to indications, antiplatelet agents are introduced, the doctor calculates the dosage of drugs in order to avoid a negative impact on the baby. nine0006
If placenta previa is accompanied by massive bleeding, delivery is carried out regardless of the time of embryogenesis by emergency caesarean section. In the case of a full-term pregnancy, vaginal delivery is acceptable provided that the cervix is ripe, active labor activity, and the patient and fetus are in good condition. When opening the cervix by 3 cm, an amniotomy is performed. Oxytocin is administered to prevent bleeding. If, with marginal presentation, the placenta significantly overlaps the uterine os or childbirth through the natural canal is impossible, a caesarean section is indicated. nine0006
The prognosis for marginal placenta previa is favorable.