After labor pains
Warning signs of health problems after birth
Some discomforts after giving birth are normal. But new moms may be at risk of serious health conditions that need medical care.
Learning signs and symptoms of health complications may help save your life. Getting treatment quickly may help prevent certain life-threatening conditions.
Life-threatening conditions that can happen after giving birth include infections, blood clots, postpartum depression and postpartum hemorrhage.
Warning signs to watch out for include chest pain, trouble breathing, heavy bleeding, severe headache and extreme pain.
If you think your life is in danger, call emergency services (911) or go to a hospital emergency room.
When do you need medical care after giving birth?
Your body goes through lots of changes after giving birth, and it needs time to heal. It’s normal to feel some discomforts in the weeks after you give birth, like being sore and really tired. But some women have complications after having a baby that can cause serious, life-threatening health problems. If you’re worried about how you feel or you have pain or discomforts that don’t feel right, call your health care provider. If you think your life is in danger, call emergency services (911) or go to a hospital emergency room.
All women need postpartum care after giving birth. Postpartum care is medical care for women who just had a baby. Go to all of your postpartum checkups, even if you’re feeling fine. These are medical checkups you get to make sure you’re recovering well from labor and birth. They help your health care provider spot and treat health conditions you may have. Postpartum care is important because new moms are at risk of serious and sometimes, life-threatening health complications in the days and weeks after giving birth. Too many new moms die from problems that could have been prevented.
What are warning signs to look for after giving birth?
In general, warning signs of serious health conditions include chest pain, trouble breathing, heavy bleeding and extreme pain. If you have any of these signs or symptoms, call your provider right away. If you think your life is in danger, call emergency services (911) or go to the emergency room.
If you have any of these signs or symptoms, call your provider right away. If you think your life is in danger, call emergency services (911) or go to the emergency room.
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
Call your provider if you have any of these signs or symptoms:
Signs and symptoms of infection
- Fever higher than 100.4 F. You get a fever when your body is trying to kill the virus or bacteria that caused an infection.
- Discharge, pain or redness that doesn’t go away or gets worse around a c-section incision (cut), episiotomy or perineal tear. A c-section (also called cesarean birth) is a surgery in which your baby is born through a cut that your doctor makes in your belly and uterus (womb). An episiotomy is a cut made at the opening of the vagina to help let the baby out during birth.
 A perineal tear is a tear in the perineum, which is the area between the vagina and the rectum. Your perineum may tear naturally during vaginal birth.
A perineal tear is a tear in the perineum, which is the area between the vagina and the rectum. Your perineum may tear naturally during vaginal birth. - Pain or burning when you urinate (pee), pain in your lower back or side or needing to pee often. You may have a urinary tract infection (also called UTI), like a bladder infection called cystitis or a kidney infection called pyelonephritis.
- Red streaks on your breasts or lumps in your breast that are new and hurt. You may have a breast infection called mastitis. This can happen when you have a plugged duct, you miss or delay breastfeeding or your breasts become engorged (swollen and full of milk).
- Severe pain in your lower belly. You may have endometritis. This is inflammation (redness or swelling) in the lining of the uterus.
- Vaginal discharge that smells bad. You may have endometritis or an infection called bacterial vaginosis (also called BV).
 BV happens when there’s too much of a certain bacteria in the vagina.
BV happens when there’s too much of a certain bacteria in the vagina.
Sometimes the body has an extreme response to infection called sepsis. Sepsis can be life-threatening. Call 911 or go to the emergency room if you have any of these signs or symptoms of sepsis after giving birth:
- Chills or feeling very cold
- Clammy or sweaty skin
- Fast breathing
- Fast heart rate
- Feeling confused
- Fever
- Having extreme pain or discomfort
Signs and symptoms of other health conditions
- Bleeding that’s heavier than your normal period or bleeding that gets worse over time. You may have postpartum hemorrhage (also called PPH). PPH is when a woman has heavy bleeding after giving birth. It’s a serious, but rare condition that can happen up to 12 weeks after having a baby.
- Pain, swelling, redness, warmth or tenderness in your legs, especially in your calves. You may have deep vein thrombosis (also called DVT).
 This happens when a blood clot forms deep in the body, usually in the lower leg or thigh.
This happens when a blood clot forms deep in the body, usually in the lower leg or thigh. - Changes in vision, dizziness, severe headache, pain in the upper right belly or in the shoulder, trouble breathing, sudden weight gain or swelling in the legs, hands or face. You may have postpartum preeclampsia. This is a serious condition that happens when a woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working normally after giving birth.
- Chest pain, coughing or gasping for air. You may have a pulmonary embolism (also called PE). An embolism is a blood clot that moves from where it formed to another place in the body. When the clot moves to a lung, it’s PE. PE is an emergency.
- Feeling sad or hopeless for more than 10 days after giving birth. You may have postpartum depression (also called PPD), a kind of depression some women get after having a baby. PPD is strong feelings of sadness, anxiety (worry) and tiredness that last for a long time after giving birth.
 These feelings can make it hard for you to take care of yourself and your baby. PPD is a medical condition that needs treatment to get better.
These feelings can make it hard for you to take care of yourself and your baby. PPD is a medical condition that needs treatment to get better. - Feeling sick to your stomach or throwing up. You may have PPH or cardiovascular disease (also called heart disease). Heart disease includes conditions that affect the heart and blood vessels. They often affect the heart muscle or involve narrowed or blocked blood vessels that can lead to a heart attack or stroke.
Last reviewed: July, 2018
See also: Your body after baby: The first 6 weeks, Your postpartum checkups, Maternal death and pregnancy-related death
Your body after baby: The first 6 weeks
Your body changes a lot after you give birth. Some changes are physical and others are emotional.
Learn about common postpartum discomforts and what do to about them. If you’re worried about a discomfort, call your health care provider.
Talk to your provider before you take any medicine to treat a discomfort.
 If you’re breastfeeding, some medicines aren’t safe for your baby.
If you’re breastfeeding, some medicines aren’t safe for your baby.Go to all of your postpartum checkups, even if you’re feeling fine. Some health conditions after pregnancy need medical care.
How does your body change in the weeks after giving birth?
Many things are happening in your body right after you have a baby. During pregnancy, your body changed a lot. It worked hard to keep your baby safe and healthy. Now that your baby is here, your body is changing again. Some of these changes are physical, like your breasts getting full of milk. Others are emotional, like feeling extra stress.
Many discomforts and body changes after giving birth are normal. But sometimes they’re signs or symptoms of a health problem that needs treatment. Go to all of your postpartum checkups, even if you’re feeling fine. These are medical checkups you get after having a baby to make sure you’re recovering well from labor and birth. At your checkups, your health care provider can help spot and treat health conditions. Postpartum care is important because new moms are at risk of serious and sometimes life-threatening health complications in the days and weeks after giving birth.
Postpartum care is important because new moms are at risk of serious and sometimes life-threatening health complications in the days and weeks after giving birth.
PHYSICAL CHANGES
What is perineum soreness?
The perineum is the area between your vagina and rectum. It stretches and may tear during labor and vaginal birth. It’s often sore after giving birth, and it may be more sore if you have an episiotomy. This is a cut made at the opening of the vagina to help let your baby out.
What you can do:
- Do Kegel exercises. These exercises strengthen the muscles in the pelvic area. To do Kegel exercises, squeeze the muscles that you use to stop yourself from passing urine (peeing). Hold the muscles tight for 10 seconds and then release. Try to do this at least 10 times in a row, three times a day.
- Put a cold pack on your perineum. Use ice wrapped in a towel. Or you can buy cold packs that you freeze in your freezer.

- Sit on a pillow or a donut-shaped cushion.
- Soak in a warm bath.
- Wipe from front to back after going to the bathroom. This can help prevent infection as your episiotomy heals.
- Ask your provider about pain medicine.
What are afterbirth pains?
Afterbirth pains are belly cramps you feel as your uterus (womb) shrinks back to its regular size after pregnancy. The cramps should go away in a few days. Right after you give birth, your uterus is round and hard and weighs about 2½ pounds. By about 6 weeks after birth, it weighs only 2 ounces.
What you can do:
Ask your provider about over-the-counter medicine you can take for pain. Over-the-counter medicine is medicine you can buy without a prescription from your provider.
What body changes can happen after a c-section?
Cesarean birth (also called c-section) is surgery in which your baby is born through a cut that your provider makes in your belly and uterus. A c-section is major surgery, so it may take a while for you to recover. You may be really tired for the first few days or weeks after a c-section because you lost blood during the surgery. The incision (cut) on your belly may be sore.
A c-section is major surgery, so it may take a while for you to recover. You may be really tired for the first few days or weeks after a c-section because you lost blood during the surgery. The incision (cut) on your belly may be sore.
What you can do:
- Ask your provider for pain medicine. Check with him before you take any medicine for pain.
- Ask your partner, family and friends to help you with the baby and around the house.
- Get rest when you can. Sleep when your baby sleeps, even when he naps during the day.
- Don’t lift from a squatting position. Don’t lift anything heavier than your baby.
- Support your belly with pillows when you’re breastfeeding.
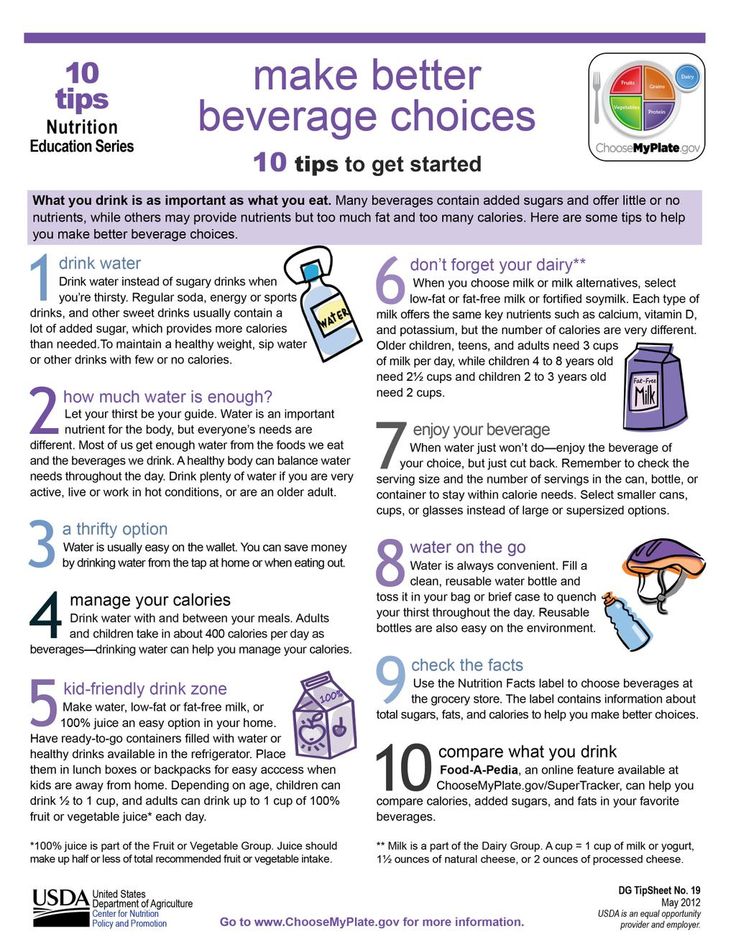
- Drink plenty of water to help replace fluids in your body.
What is vaginal discharge?
After your baby is born, your body gets rid of the blood and tissue that was inside your uterus. This is called vaginal discharge or lochia. For the first few days, it’s heavy, bright red and may contain blood clots. Over time, the flow gets less and lighter in color. You may have discharge for a few weeks or even for a month or more.
Over time, the flow gets less and lighter in color. You may have discharge for a few weeks or even for a month or more.
What you can do:
Use sanitary pads until the discharge stops.
What is breast engorgement?
This is when your breasts swell as they fill with milk. It usually happens a few days after giving birth. Your breasts may feel tender and sore. The discomfort usually goes away once you start breastfeeding regularly. If you’re not breastfeeding, it may last until your breasts stop making milk, usually within a few days.
What you can do:
- Breastfeed your baby. Try not to miss a feeding or go a long time between feedings. Don’t skip night feedings.
- Before you breastfeed your baby, express a small amount of milk from your breast with a breast pump or by hand.
- Take a warm shower or lay warm towels on your breasts to help your milk flow. If your engorgement is really painful, put cold packs on your breasts.

- If your breasts are leaking between feedings, wear nursing pads in your bra so your clothes don’t get wet.
- Tell your provider if your breasts stay swollen and are painful.
- If you’re not planning to breastfeed, wear a firm, supportive bra (like a sports bra).
What is nipple pain?
If you’re breastfeeding, you may have nipple plain during the first few days, especially if your nipples crack.
What you can do:
- Talk to your provider or a lactation consultant to be sure your baby is latching on to your breast the right way. A lactation consultant is a person trained to help women breastfeed, even women who have breastfeeding problems. Latching on is when your baby’s mouth is securely attached to (placed around) your nipple.
- Ask your provider about cream to put on your nipples.
- After breastfeeding, massage some breast milk onto your nipples. Let your breasts air dry.
What is swelling?
Lots of women have swelling in their hands, feet and face during pregnancy. It’s caused by extra fluids in your body. It may take time for the swelling to go away after you have your baby.
It’s caused by extra fluids in your body. It may take time for the swelling to go away after you have your baby.
What you can do:
- Lie on your left side when resting or sleeping.
- Put your feet up.
- Try to stay cool and wear loose clothes.
- Drink plenty of water.
What are hemorrhoids?
Hemorrhoids are painful, swollen veins in and around the anus that may hurt or bleed. Hemorrhoids are common during and after pregnancy.
What you can do:
- Soak in a warm bath.
- Ask your provider about using an over-the-counter spray or cream for pain.
- Eat foods that are high in fiber, such as fruits, vegetables and whole-grain breads and cereals.
- Drink lots of water.
- Try not to strain when you’re having a bowel movement (pooping).
What is constipation?
Constipation is when you don’t have bowel movements, you don’t have them often or your stools (poop) are hard to pass. You also may have painful gas. This may happen for a few days after you give birth.
You also may have painful gas. This may happen for a few days after you give birth.
What you can do:
- Eat foods that are high in fiber.
- Drink lots of water.
- Ask your provider about medicine to take.
What urinary problems can happen after giving birth?
In the first few days after giving birth, you may feel pain or burning when you urinate (pee). Or you may try to urinate but find that you can’t. Sometimes you may not be able to stop urinating. This is called incontinence. It usually goes away as your pelvic muscles become stronger again.
What you can do for pain, burning or if you have trouble urinating:
- Drink lots of water.
- Run water in the sink when you go to the bathroom.
- Soak in a warm bath.
- If the pain continues, tell your provider.
What you can do for incontinence: Do Kegel exercises to strengthen your pelvic muscles.
Why do you sweat a lot after giving birth?
This happens often to new moms, especially at night. It’s caused by all the changing hormones in your body after pregnancy.
What you can do:
- Sleep on a towel to help keep your sheets and pillow dry.
- Don’t use too many blankets or wear warm clothes to bed.
Why do you feel tired after giving birth?
You may have lost blood during labor and birth. This can make your body tired. And your baby probably doesn’t let you sleep all night!
What you can do:
- Sleep when your baby sleeps, even when he naps during the day.
- Eat healthy foods, like fruits, vegetables, whole-grain breads and pasta, and lean meat and chicken. Limit sweets and foods with a lot of fat.
- Ask your partner, family and friends to help with the baby and around the house.
- Limit visitors. You’ll have plenty of time for family and friends to meet your new baby when you’re feeling rested.
When can you start losing weight after giving birth?
You lose about 10 pounds right away after giving birth and a little more within the first week. This is a great time to get to a healthy weight, no matter how much you weighed before you got pregnant. Eating healthy and being active every day helps boost your energy level and can make you feel better. If you’re at a healthy weight, you’re less likely to have health conditions, like diabetes and high blood pressure, than if you’re over- or underweight. And just in case you get pregnant again, or if you’re planning to have another baby sometime in the future, it’s best to be at a healthy weight before your next pregnancy.
What you can do:
- Talk to your provider about your weight. If you were overweight before pregnancy, you may want to lose more weight than you gained during pregnancy.
- Eat healthy foods. Limit sweets and foods with a lot of fat.
- Drink lots of water.
- Ask your provider about being active, especially if you’ve had a c-section. Begin slowly and increase your activity over time. Walking and swimming are great activities for new moms. Do something active every day.
- Breastfeed your baby. Breastfeeding helps you burn calories. This can help you lose the weight you gained during pregnancy faster than if you weren’t breastfeeding.
- Don’t try to lose too much weight too fast. Your body needs nutrients from food to heal. If you’re breastfeeding, losing weight too fast can reduce your milk supply.
- Don’t feel badly if you don’t lose the weight as quickly as you’d like. It takes time for your body and your belly to get back in shape. Staying fit over time is more important than getting in shape right after giving birth.
What skin changes can happen after giving birth?
You may have stretch marks on your belly where your skin stretched during pregnancy. Some women also get them on their thighs, hips and bottom. They may not disappear after giving birth, but they do fade over time.
What you can do:
Use creams or lotions on your skin. They don’t make stretch marks go away, but they can help reduce itching that comes with stretch marks.
What hair changes can happen after giving birth?
Your hair may have seemed thicker and fuller during pregnancy. This is because high hormone levels in your body made you lose less hair during pregnancy. After your baby is born, your hair may thin out. You may even lose hair. Hair loss usually stops within 6 months after you give birth. Your hair should regain its normal fullness within a year.
What you can do:
- Eat lots of fruits and vegetables. The nutrients in fruits and veggies may help protect your hair and help it grow.
- Be gentle with your hair. Don’t wear tight ponytails, braids or rollers. These can pull and stress your hair.
- Use the cool setting on your hair dryer.

When do you get your period again after pregnancy?
If you’re not breastfeeding, your period may start again 6 to 8 weeks after giving birth. If you are breastfeeding, it may not start again for months. Some women don’t have a period again until they stop breastfeeding. When your period returns, it may not be the same as before you were pregnant. It may be shorter or longer than it was. Over time it often returns to the way it was before you got pregnant.
When can you get pregnant again?
Many health care providers recommend waiting 4 to 6 weeks after giving birth to give your body time to heal before you have sex. When you’re ready for sex, be careful – you can get pregnant even before your period starts. This is because you may ovulate (release an egg) before you get your period again.
What you can do:
Use birth control to help make sure you don’t get pregnant again until you’re ready. Birth control helps keep you from getting pregnant. Examples of birth control include intrauterine devices (also called IUDs), implants, the pill and condoms. Talk to your provider about which birth control to use, especially if you’re breastfeeding. Some types of birth control can reduce your milk supply. Breastfeeding is not birth control. It does not prevent pregnancy.
Birth control helps keep you from getting pregnant. Examples of birth control include intrauterine devices (also called IUDs), implants, the pill and condoms. Talk to your provider about which birth control to use, especially if you’re breastfeeding. Some types of birth control can reduce your milk supply. Breastfeeding is not birth control. It does not prevent pregnancy.
For most women, it’s best to wait at least 18 months (1½ years) between giving birth and getting pregnant again. Too little time between pregnancies increases your risk of premature birth (before 37 weeks of pregnancy). Premature babies are more likely to have health problems than babies born on time. Your body needs time to fully recover from your last pregnancy before it’s ready for your next pregnancy.
EMOTIONAL CHANGES
What can you do about feeling stressed and overwhelmed?
Your baby didn’t come with a set of instructions. You may feel overwhelmed trying to take care of her. Taking care of a baby is a lot to think about.
Taking care of a baby is a lot to think about.
What you can do:
- Tell your partner how you feel. Let your partner help take care of the baby.
- Ask your friends and family for help. Tell them exactly what they can do for you, like going grocery shopping or making meals.
- Find a support group of new moms. A support group is a group of people who have the same kinds of concerns. They meet together to try to help each other. Ask your provider to help you find a support group of new moms near where you live. Or look for a support group online.
- Eat healthy foods and do something active every day.
- Don’t smoke, drink alcohol or use harmful drugs. All of these things are bad for you and can make it hard for you to handle stress.
What are the baby blues and postpartum depression?
Baby blues (also called postpartum blues) are feelings of sadness a woman may have in the first few days after having a baby. Baby blues can happen 2 to 3 days after you have your baby and can last up to 2 weeks. They usually go away on their own, and you don’t need any treatment.
Baby blues can happen 2 to 3 days after you have your baby and can last up to 2 weeks. They usually go away on their own, and you don’t need any treatment.
Postpartum depression (also called PPD) is a kind of depression that some women get after having a baby. It's strong feelings of sadness, anxiety (worry) and tiredness that last for a long time after giving birth. These feelings can make it hard for you to take care of yourself and your baby. PPD is a medical condition that needs treatment to get better. It’s the most common complication for women who have just had a baby.
What you can do about the baby blues:
- Get as much sleep as you can.
- Don’t drink alcohol, use street drugs or use harmful drugs. All of these can affect your mood and make you feel worse. And they can make it hard for you to take care of your baby.
- Ask for help from your partner, family and friends. Tell them exactly what they can do for you.
- Take time for yourself.
 Ask someone you trust to watch your baby so you can get out of the house.
Ask someone you trust to watch your baby so you can get out of the house. - Connect with other new moms. Ask your provider to help you find a support group of new moms.
- If you have sad feelings that last longer than 2 weeks, tell your health care provider.
What you can do about postpartum depression:
- If you think you have PPD, tell your provider.
- Learn about risk factors for PPD and signs and symptoms of PPD.
- Ask your provider about treatment for PPD.
- If you’re worried about hurting yourself or your baby, call emergency services (911) right away.
How can you handle going back to work or school?
It may be hard for you to leave your baby with a caregiver all day, even if it’s a family member or a close friend. It also may be hard to find a caregiver you trust. You and your partner may disagree about what type of child care is best for your baby. You may be upset that you can’t stay home with your baby all the time.
What you can do:
- Talk to your partner about child care. Figure out how much you can spend and what kind of care you want. For example, you can have a caregiver come to your home to take care of your baby. Or you can take your baby to a child care center.
- Ask friends and family about child care they use. Maybe you can use the same person or service.
- If you’re using a child care center, ask for names and phone numbers of people who use the center. Call to ask how they feel about the center’s care.
- Ask your boss if you can ease back into work. Maybe you can work a few hours a day at first, or just a few days a week.
How can you and your partner get used to being new parents?
Both you and your partner are getting used to having a baby around. Your partner may be just as stressed and nervous about being a parent as you are. Rely on each other to figure things out.
What you can do:
- Learn about taking care of your baby together.
 Read baby-care books and go to baby-care classes.
Read baby-care books and go to baby-care classes. - Let your partner help with the baby. Don’t try to do everything yourself.
- Talk to each other. Talking about your feelings can help keep you from feeling hurt and frustrated.
- Make time for just the two of you. Go for a walk or out to dinner. Ask someone you trust to take care of the baby for an hour or two.
- Tell your partner what your provider says about how long to wait to have sex again. Ask your provider to talk to your partner, if you think that’s helpful.
Last reviewed: July, 2018
See also: Your postpartum checkups, Warning signs and symptoms of health problems after giving birth, Maternal death and pregnancy-related death, Postpartum depression, Baby blues after pregnancy, Keeping breast milk safe and healthy, Birth control, How long should you wait before getting pregnant again
Recovery after childbirth
In most cases, the recovery of normal health is not rapid. The first sensation of incredible relief has passed, and now you notice that the stomach is still large, and even a little sore. To take its former size, the uterus must still be contracted for a long time and diligently. Its weight decreases from 1 kg to 50 g within 6-8 weeks.
The first sensation of incredible relief has passed, and now you notice that the stomach is still large, and even a little sore. To take its former size, the uterus must still be contracted for a long time and diligently. Its weight decreases from 1 kg to 50 g within 6-8 weeks.
Since the contraction of the uterus occurs due to the work of the muscles, this is accompanied by pain sensations of varying intensity, reminiscent of light contractions. You may notice an increase in pain while breastfeeding your baby. The thing is that stimulation of the nipple causes an increase in the level of oxytocin in the blood, which contributes to uterine contractions. nine0003
For better uterine contraction, it is recommended to lie on your stomach after childbirth. If you feel good, try to move more and do gymnastics.
Another disturbing circumstance is pain in the perineum, which appears even if there were no tears and the doctor did not make an incision. This is due to the fact that the tissues have undergone a strong stretch during childbirth.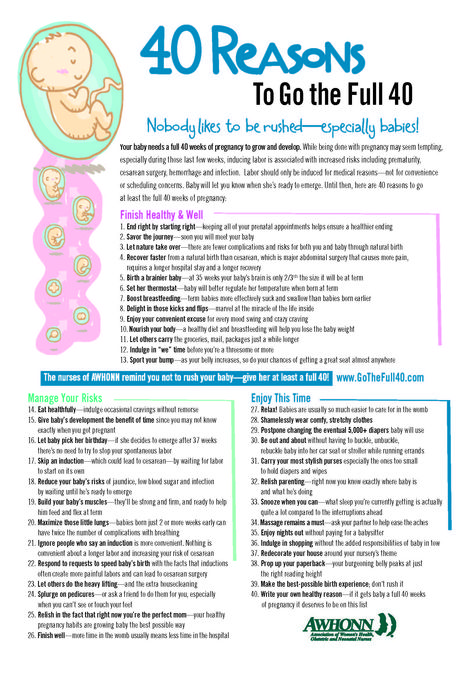 Usually the pain is not very intense and disappears in 2-3 days. But if there were tears or a perineal incision, then it can hurt longer - 7-10 days. You should carefully monitor the seams, carry out hygiene after each visit to the toilet. In addition, it is necessary to treat the sutures daily with antiseptic solutions, you can not sit for 2 weeks. nine0003
Usually the pain is not very intense and disappears in 2-3 days. But if there were tears or a perineal incision, then it can hurt longer - 7-10 days. You should carefully monitor the seams, carry out hygiene after each visit to the toilet. In addition, it is necessary to treat the sutures daily with antiseptic solutions, you can not sit for 2 weeks. nine0003
Haemorrhoids often appear after childbirth. Careful hygiene and daily evening showers help reduce pain. Do not forget about the diet, include in your diet foods rich in fiber and with a slight laxative effect: seaweed, beets, baked apples, cauliflower, germinated cereals. Medications are usually not used because the inflammation usually goes away with time. If everything does not go away by itself and the woman continues to suffer from hemorrhoids, you need to consult a doctor and apply the medicines prescribed by him or take a course of physiotherapy procedures. nine0003
Constipation that occurred during pregnancy may also remind of itself in the postpartum period. They are, in particular, caused by the fear of damaging the seams in the perineum. However, such fear is unfounded. In addition, during a bowel movement, you can hold the area where the stitches are applied with a napkin, which will reduce the stretching of the tissues, and the bowel movement will be less painful. The chair usually does not happen immediately after childbirth, but after 2-3 days. To prevent constipation, eat prunes and dried apricots, drink mineral water. And only if there was no bowel movement on the 3rd day, you can use a laxative candle. nine0003
They are, in particular, caused by the fear of damaging the seams in the perineum. However, such fear is unfounded. In addition, during a bowel movement, you can hold the area where the stitches are applied with a napkin, which will reduce the stretching of the tissues, and the bowel movement will be less painful. The chair usually does not happen immediately after childbirth, but after 2-3 days. To prevent constipation, eat prunes and dried apricots, drink mineral water. And only if there was no bowel movement on the 3rd day, you can use a laxative candle. nine0003
After childbirth, especially strong discharge from the uterus is observed on the first day, then it decreases. After 3 days, the discharge becomes muco-bloody. By the 5-6th week after birth, the discharge from the uterus stops altogether. During this period, hygiene must be carefully observed, because an infection that has entered the uterus can lead to endometritis (an inflammatory process of the uterine mucosa).
For 9 months, all the organs of the female body worked to ensure the child's proper development and good health.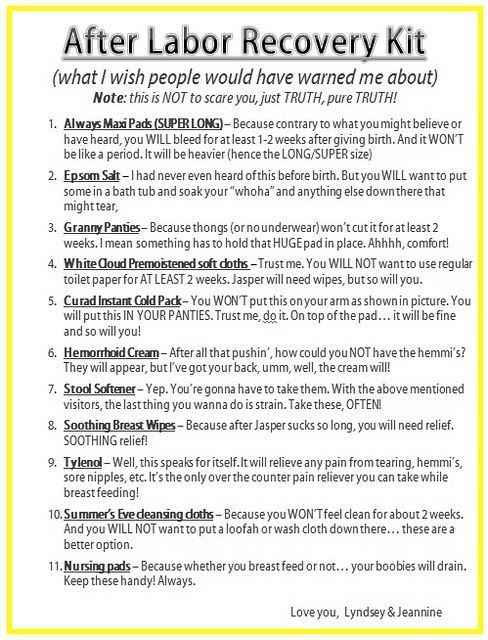 Now he was born and became quite "independent". However, the functions of a woman-mother did not end there. The main one - to provide the baby with food - is taken over by the mammary glands. In the body of a woman, hormonal changes continue, due to which significant changes occur in the mammary glands, and they begin to produce milk. In the first 2-3 days, colostrum is released, and already on the 3-4th day - transitional milk, which gradually turns into mature breast milk. Feeding your baby stimulates milk production. Therefore, in case of insufficient lactation, more frequent breastfeeding is recommended. nine0003
Now he was born and became quite "independent". However, the functions of a woman-mother did not end there. The main one - to provide the baby with food - is taken over by the mammary glands. In the body of a woman, hormonal changes continue, due to which significant changes occur in the mammary glands, and they begin to produce milk. In the first 2-3 days, colostrum is released, and already on the 3-4th day - transitional milk, which gradually turns into mature breast milk. Feeding your baby stimulates milk production. Therefore, in case of insufficient lactation, more frequent breastfeeding is recommended. nine0003
However, women often face the opposite problem - an excess amount of milk and difficulty in its outflow. This, in turn, leads to its stagnation and engorgement of the mammary glands - they harden, increase in volume, and painful sensations appear in the chest area. It may even increase body temperature. How to prevent such occurrences?
First of all, try to breastfeed your baby regularly, and in the first 3-4 days after birth, limit fluid intake to 800 ml per day. Then the mammary glands will gradually become soft again. In addition, it is important to know that in the first days after childbirth, the skin of the nipples is very delicate and may crack. This makes them vulnerable to infection, the entry of which into the cracks is fraught with the development of mastopathy. Therefore, you need to take good care of the nipples and wear a comfortable bra, which will help the proper development of lactation. nine0003
Then the mammary glands will gradually become soft again. In addition, it is important to know that in the first days after childbirth, the skin of the nipples is very delicate and may crack. This makes them vulnerable to infection, the entry of which into the cracks is fraught with the development of mastopathy. Therefore, you need to take good care of the nipples and wear a comfortable bra, which will help the proper development of lactation. nine0003
To prevent cracks in the nipples, it is necessary to apply the baby to each breast in turn in the first 2-3 days after childbirth. First, give the baby one for 5-7 minutes, then another for 5-7 minutes. To prevent cracks, there is a special cream that needs to be used between feedings, and before them, carefully wash off its remnants.
That's all the troubles that are easily forgotten and seem not so significant against the background of new worries. Now your attention will be constantly occupied by the baby. However, it is very important not to forget about yourself, maintain your health and restore your former beauty. Not everyone succeeds, which contributes to the development of postpartum depression. nine0003
Not everyone succeeds, which contributes to the development of postpartum depression. nine0003
Lochiometer
After childbirth, under the influence of cellular enzymes secreted by the granulation shaft, blood clots and fragments of the decidua remaining on the walls of the uterus are liquefied. In addition, leukocytes, erythrocytes, plasma and lymph penetrate into the uterine cavity through the wound surface. All these elements form lochia - a postpartum wound secret, which normally actively flows from the uterine cavity through the cervical canal into the vagina.
The first 2-3 days after birth, lochia have a bloody character, then, from the 4th-5th day, they acquire a dark red and brownish hue, and after a week they become yellowish-white due to the high content of leukocytes. From the 10th day, the discharge becomes light, watery, serous-mucous consistency. Gradually, the number of lochia decreases, and by the end of the 3rd week, the discharge practically stops and soon disappears completely. nine0003
nine0003
With a delay in the outflow of postpartum secretions, they speak of a lochiometer - stagnation of lochia in the uterine cavity. The danger of developing lochiometers lies in the high probability of infection of the contents of the uterus, since lymph, serum, blood, and tissue remnants serve as the best nutrient medium for the reproduction of microbial flora. Most often, against the background of lochiometers, endometritis develops.
Causes of the development of lochiometers
The development of lochiometers is due to mechanical obstacles to the outflow of secretions in the cervical canal or insufficient uterine contractility. nine0003
Mechanical obstruction may be due to kinking (hyperanteflexia) of the uterus or obstruction of the cervical canal by blood clots, remnants of the decidua, and flaking uterine tissue.
Insufficient contractile activity of the uterus in the postpartum period usually develops as a result of overstretching of the uterus (with a large fetus, polyhydramnios or multiple pregnancy), weak or discoordinated labor, spasm of the internal os, caesarean section. nine0003
nine0003
The development of lochiometers is facilitated by prolonged bed rest and low activity after childbirth.
Symptoms of lochiometer
Lochiometer develops 5-7 days after birth, characterized by a marked decrease or cessation of postpartum discharge from the uterus. At the same time, there is an increase in the size of the uterus compared to the norm for the current postpartum day, its soreness on palpation. The general health and objective condition of a woman with a lochiometer does not suffer, body temperature is normal, tachycardia is absent. nine0003
When delaying timely therapeutic tactics in relation to lochiometers, fever appears (body temperature 38-40 ° C), chills, cramping pains, turbid discharge with an unpleasant odor, tachycardia. After 1-2 days, the temperature drops critically with the simultaneous appearance of liquid purulent lochial discharge.
Diagnosis lochiometers
Lochiometers are diagnosed by characteristic clinical signs. With the help of a gynecological examination, an unevenly enlarged and painful uterus is determined, which has a densely elastic consistency, often - the closure of the internal pharynx, the bend of the uterus. nine0003
With the help of a gynecological examination, an unevenly enlarged and painful uterus is determined, which has a densely elastic consistency, often - the closure of the internal pharynx, the bend of the uterus. nine0003
Clarifying lochiometer diagnostics includes ultrasound. during which the expansion of the uterine cavity is revealed, the presence of hyperechoic blood clots and liquid blood in it.
Treatment of lochiometers
Treatment of lochiometers consists in ensuring the free outflow of lochia, taking into account the cause that caused this condition.
When lochiometers are detected, the gynecologist prescribes injections of antispasmodics (papaverine, no-shpy) to relieve spasm of the uterine os. In the treatment of lochiometers, uterotonic (contracting the uterus) agents are used - oxytocin, methylergometrine. For a free outflow of secretions, the puerperal is recommended to lie on her stomach 2-3 times a day for 1-2 hours. nine0003
In case of hyperanteflexion of the uterus, the bend is eliminated during the bimanual examination; exercise therapy is prescribed. In the case of a lochiometer due to blockage of the cervical canal by clots, when viewed on a chair, digital dilatation of the cervical canal and careful removal of clots are performed.
In the case of a lochiometer due to blockage of the cervical canal by clots, when viewed on a chair, digital dilatation of the cervical canal and careful removal of clots are performed.
Situations when the lochiometer is not allowed within 2-3 days are considered by clinical gynecology as an indication for instrumental removal of the contents of the uterus with a curette or vacuum apparatus under hysteroscopy control. For the prevention and treatment of postpartum infections against the background of lochiometers, antibiotics are prescribed, taking into account the results of a bacteriological smear. nine0003
Complications of lochiometers
If, after the elimination of lochiometers, uterine tenderness, its poor contraction, hyperthermia persist, one should think about the development of postpartum metroendometritis.
If the infection progresses, the condition of the puerperal may worsen due to the development of purulent-resorptive fever, manifested by intoxication, abdominal pain, purulent discharge with a putrid odor. Against this background, the transition of lochiometers to pyometra is noted.
Against this background, the transition of lochiometers to pyometra is noted.
Prevention and prognosis with lochiometer
To prevent the development of lochiometers, competent management of pregnancy and preparation of the woman for childbirth are required, as well as careful monitoring of the puerperal during the postpartum period: regular monitoring of uterine contractions (daily palpation determination of its sensitivity, consistency, fundus height), volume and nature of discharge .
In the postpartum period, a woman needs to monitor the timeliness of emptying the bladder and intestines, breastfeed the newborn on demand, perform postpartum exercises, and lie on her stomach. nine0003
After discharge from the maternity hospital, a young mother should also monitor her well-being and discharge from the genital tract. In the event of an increase in temperature, a delay in lochia, a change in their nature or smell, an immediate appeal to a gynecologist is necessary.
The prognosis for timely detection and elimination of lochiometers is favorable.
Observation in the postpartum period. Complications and diseases of the postpartum period
Postpartum period - the period of time during which the female body returns to normal after childbirth. It begins immediately after the birth of the child and ends after 6-8 weeks. Usually this period is normal, but sometimes there are complications that require medical attention.
1
Postpartum care
2
Postpartum care
3
Postpartum care
What changes occur in the postpartum period? nine0103
Immediately after giving birth, a woman's uterus begins to contract. The walls of the uterus are compacted, the vessels of the placental site (i.e., the place of attachment of the placenta) are compressed. In the future, the uterus continues to shrink and acquires its original size.
During the postpartum period, regeneration of the uterine mucosa occurs, accompanied by secretions (lochia). Depending on the period of the postpartum period, lochia has a different color and character - from bloody at the beginning to serous at the end. nine0003
The cervix is finally formed 2-3 weeks after birth.
The vagina shrinks and shortens within three weeks. The perineum is restored in 10-12 days.
Features of the lactation period
Due to changes in the level of hormones in the postpartum period, a woman develops lactation. As a rule, 3-4 days after birth, the mother has milk.
Women's breasts increase in volume, become hard and painful. Body temperature may rise. With proper observance of the feeding regimen, these unpleasant features gradually disappear. nine0003
In the first three days, colostrum is secreted from the mammary glands of a woman. Unlike milk, it contains a large amount of immunoglobulins and protein. There is not much colostrum, but it is 10 times more nutritious than milk, so even a small amount is enough to feed the baby. Then milk appears in the breast. But in order to always have enough of it, you need to follow a simple rule - regularly apply the baby to the breast and do not supplement the baby.
Then milk appears in the breast. But in order to always have enough of it, you need to follow a simple rule - regularly apply the baby to the breast and do not supplement the baby.
1
Gynecological consultation in MedicCity
2
Gynecological consultation in MediCity
3
Ultrasound in MedicCity
Postpartum care
After labor is completed, each woman's cervix, vagina and perineum are assessed. If breaks are found, they are immediately sewn up.
In the first few days, the mother is in the maternity hospital under medical supervision. This is extremely necessary, since the vast majority of postpartum complications, such as bleeding associated with poor uterine contractility, incomplete discharge of placental tissue, occur on the first day after childbirth. nine0003
At the maternity hospital, a doctor and a midwife take care of the mother and baby every day. They try to prevent the occurrence of purulent-inflammatory diseases in the newborn and the woman in labor.
They try to prevent the occurrence of purulent-inflammatory diseases in the newborn and the woman in labor.
The general well-being of the woman in labor, the condition of the uterus, external genital organs, mammary glands, as well as the nature of the discharge are necessarily evaluated. Body temperature is checked twice a day, blood pressure and pulse are measured daily.
In the case of a normal postpartum period, the newborn is vaccinated with BCG, and the mother and baby are discharged home for 3-4 days. Further observation is carried out by a gynecologist of the antenatal clinic. nine0003
Some mothers for some reason think that after the birth of a baby, only the baby needs regular medical care. But this is a misconception!
To avoid numerous health problems, mothers also need to see a gynecologist!
What problems can appear in the postpartum period?
Constipation and urinary retention
Problems with urination may occur in the first days after childbirth. This is especially true for childbirth that is long in time or carried out by caesarean section. In such cases, urine is released using a catheter. nine0003
This is especially true for childbirth that is long in time or carried out by caesarean section. In such cases, urine is released using a catheter. nine0003
With a tendency to constipation, exercise and simple morning exercises help to restore bowel function. In the absence of a chair within 4 days, you can use a laxative candle.
Quite often, after childbirth, a woman develops hemorrhoids, the treatment of which should be entrusted to a professional proctologist.
1
Proctologist's consultation
2
Proctologist's consultation
3
Proctologist's consultation
Vaginal discharge
The appearance of blood from the vagina in the first days after childbirth is a common phenomenon. In the first 2-3 days, the discharge is quite plentiful, then they become smaller and turn brown.
Cracked nipples
Cracked nipples are also quite common. To avoid cracks, try not to breastfeed your baby for more than 7 minutes in the first days. Before each application of the child to the breast and after feeding, wash the mammary glands with warm water and soap, dry them with a towel. Be sure to wash your hands before feeding. You can use a special cream for cracked nipples. nine0003
To avoid cracks, try not to breastfeed your baby for more than 7 minutes in the first days. Before each application of the child to the breast and after feeding, wash the mammary glands with warm water and soap, dry them with a towel. Be sure to wash your hands before feeding. You can use a special cream for cracked nipples. nine0003
Drawing pains in the lower abdomen
Contractions of the uterus are accompanied by pain sensations that are a bit like contractions. The pain may be exacerbated by breastfeeding. Performing postpartum exercises helps strengthen the muscles of the small pelvis and achieve faster rehabilitation.
Pain in the perineum occurs in women who have received tears in this area during childbirth. Healing occurs within 7-10 days. For severe pain, the doctor may prescribe pain medication to the patient. nine0003
The baby does not suck out all the milk
If the baby does not suck out all the milk, it is necessary to express the rest of the milk to avoid fluid retention in the breast. Thanks to this simple technique, you can increase lactation and prevent lactostasis.
Thanks to this simple technique, you can increase lactation and prevent lactostasis.
The postpartum period is characterized by exacerbation of chronic diseases, metabolic disorders, endocrinological problems, and the menstrual cycle may also change.
Postpartum conditions
Be sure to see your doctor if you have:
- painful lumps in the chest and high body temperature are symptoms of lactostasis or mastitis;
- pain at the site of the incision of the perineum and the appearance of discharge with an unpleasant odor are signs of infection or rupture of the sutures;
- severe (with scarlet clots) bleeding from the vagina is one of the symptoms of uterine bleeding;
- foul-smelling vaginal discharge, together with high fever and chills, may indicate an inflammatory process in the uterus; nine0196
- the appearance of hot, red, painful, swollen areas on the legs - symptoms of incipient thrombophlebitis.
1
Physician's consultation in MediCity
2
Phlebologist's consultation in MedicCity
3
A woman who has given birth may need the help of several doctors in addition to a gynecologist.