Multiple gestation meaning
Multiple Pregnancy | ACOG
-
A pregnancy with more than one fetus is called a multiple pregnancy.
-
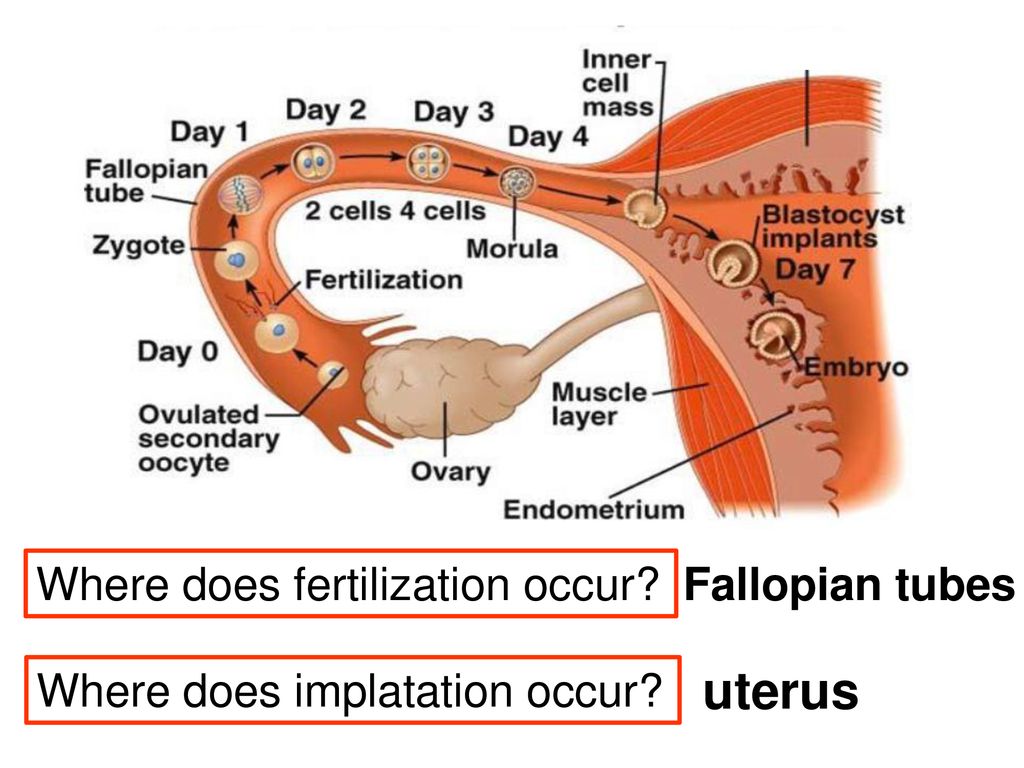
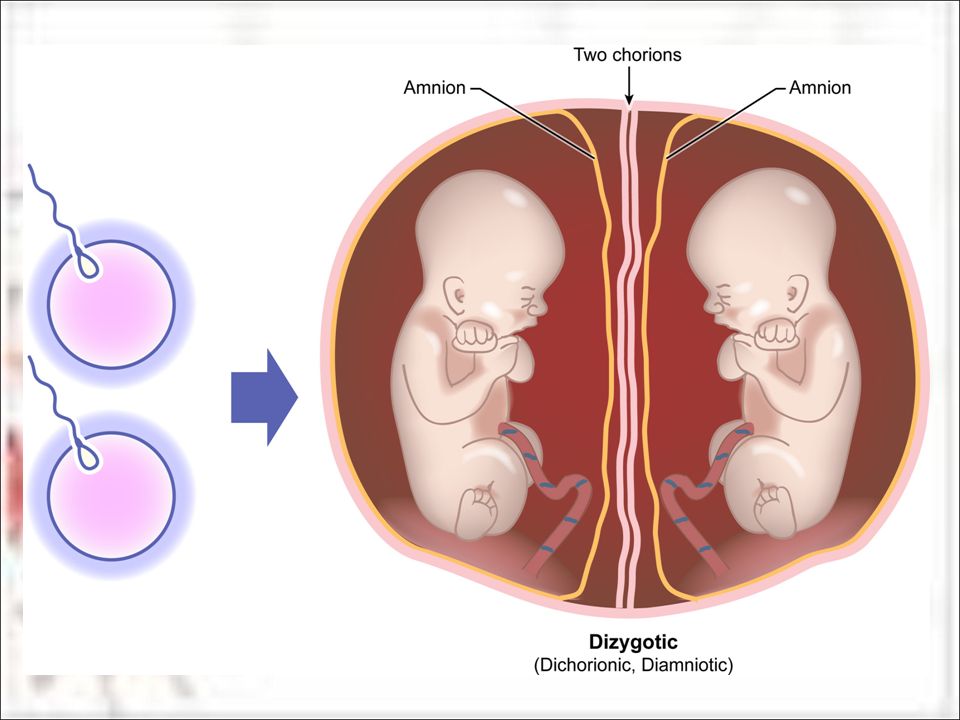
If more than one egg is released during the menstrual cycle and each egg is fertilized by a sperm, more than one embryo may implant and grow in the uterus. This type of pregnancy results in fraternal twins (or more). When a single fertilized egg splits, it results in multiple identical embryos. This type of pregnancy results in identical twins (or more). Fraternal twins are more common than identical twins.
-
The use of fertility drugs to induce ovulation often causes more than one egg to be released from the ovaries and can result in twins, triplets, or more.
In vitro fertilization (IVF) can lead to a multiple pregnancy if more than one embryo is transferred to the uterus.
Identical multiples also may result if the fertilized egg splits after transfer.
Women older than age 35 are more likely to release two or more eggs during a single menstrual cycle than younger women. So older women are more likely than younger women to become pregnant with multiples.
-
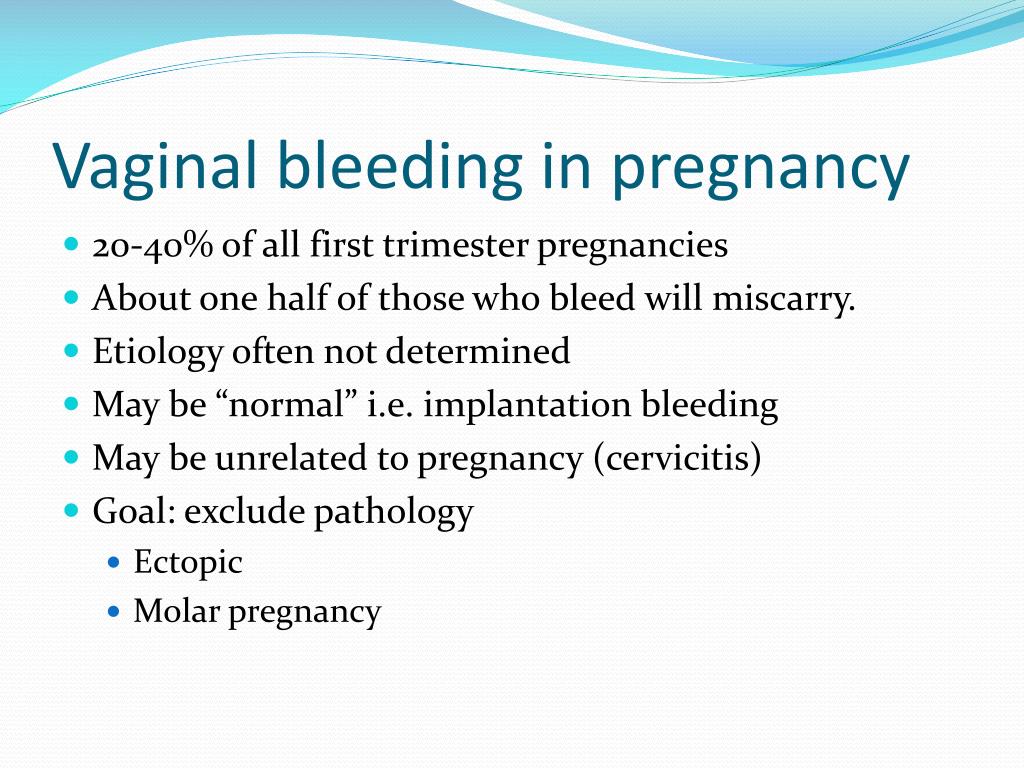
Women who are pregnant with multiples may have more severe morning sickness or breast tenderness than women who are pregnant with a single fetus. They also may gain weight more quickly. Most multiple pregnancies are discovered during an ultrasound exam.
-
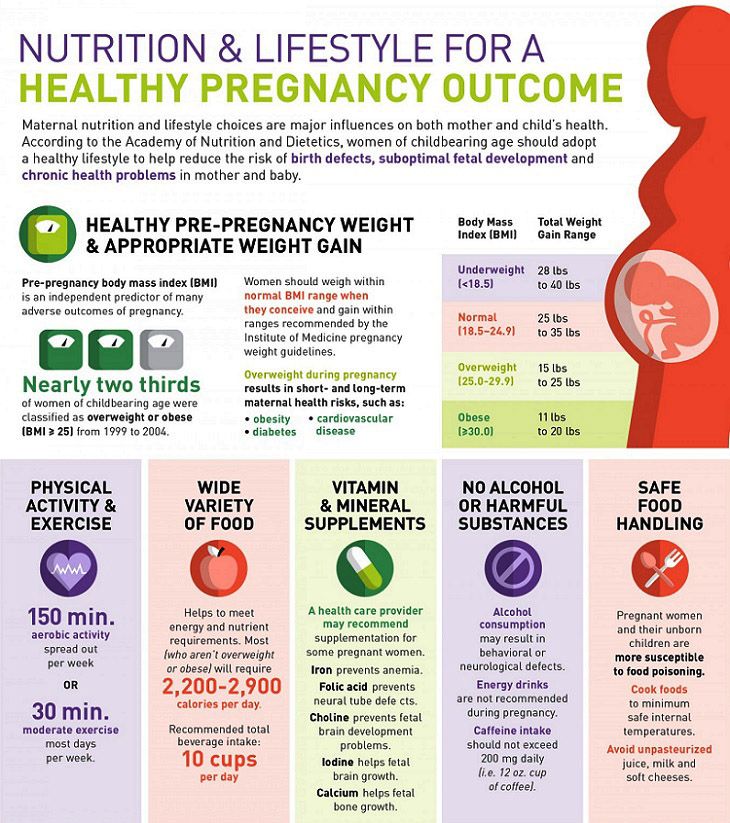
Most women who are pregnant with multiples need to gain more weight than women who are pregnant with one fetus. An extra 300 calories a day is needed for each fetus. For example, if you are pregnant with twins, you need an extra 600 calories a day.
 For triplets and more, talk with your obstetrician–gynecologist (ob-gyn) about the right amount of weight gain for your pregnancy.
For triplets and more, talk with your obstetrician–gynecologist (ob-gyn) about the right amount of weight gain for your pregnancy. -
Staying active during multiple pregnancy is important for your health, but you may need to avoid strenuous exercise. Try low-impact exercise, such as swimming, prenatal yoga, and walking. You should aim for 30 minutes of exercise a day. If problems arise during your pregnancy, your ob-gyn may recommend that you avoid exercise.
-
You likely will have more frequent prenatal care visits with your ob-gyn. Starting in your second trimester, you may have ultrasound exams every 4 to 6 weeks. If a problem is suspected, you may have special tests or more frequent ultrasound exams.
-
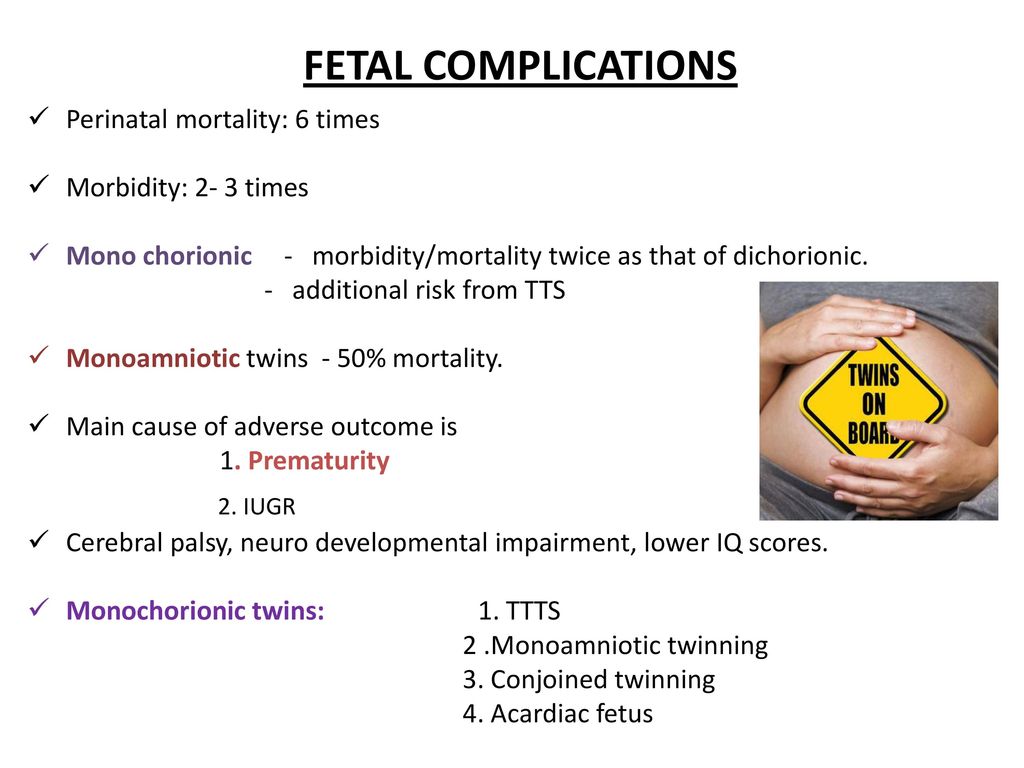
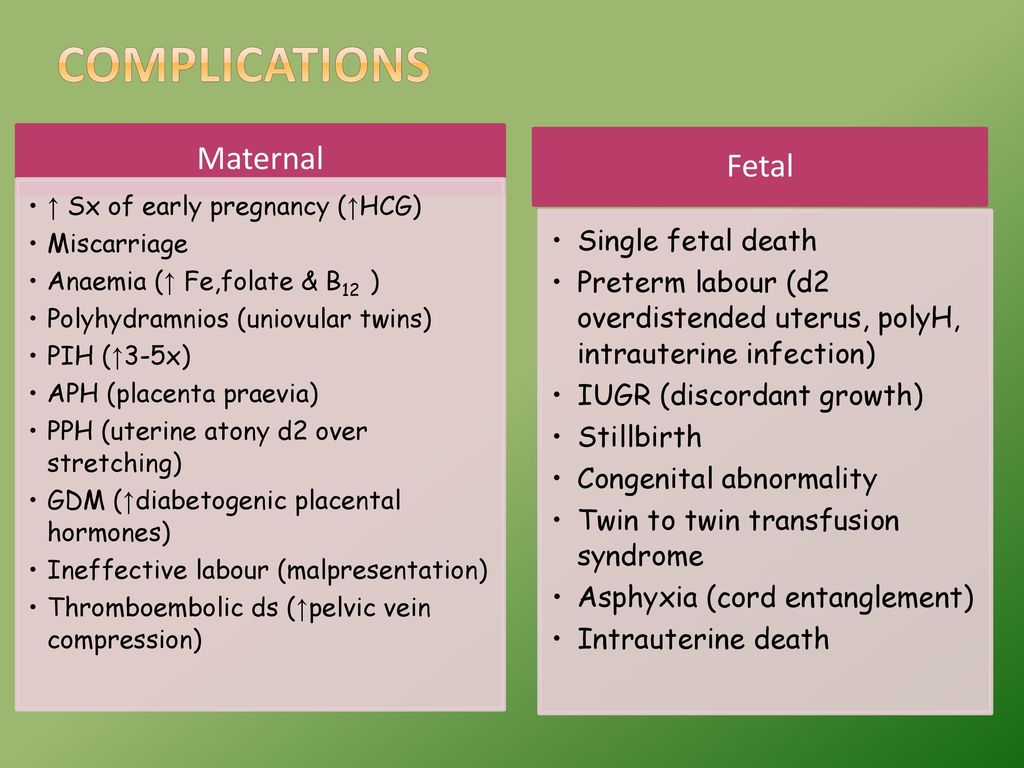
The most common complication of multiple pregnancy is preterm birth.
 More than one half of all twins are born preterm. Triplets and more are almost always born preterm.
More than one half of all twins are born preterm. Triplets and more are almost always born preterm. -
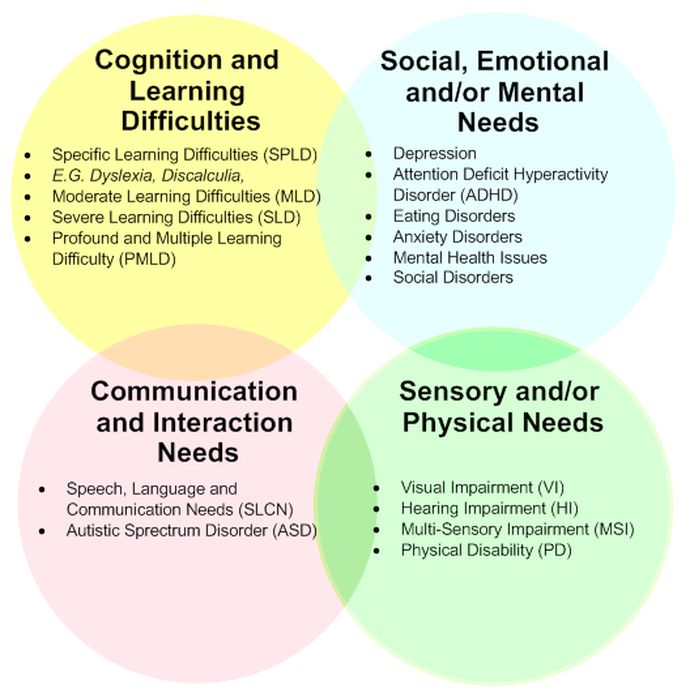
Babies born before 37 weeks of pregnancy may have an increased risk of short-term and long-term health problems, including problems with breathing, eating, and staying warm. Other problems, such as learning and behavioral disabilities, may appear later in childhood or even in adulthood. Very preterm babies (those who are born before 32 weeks of pregnancy) can die or have severe health problems, even with the best of care.
Preterm multiples also have a greater risk of serious complications that can lead to cerebral palsy. Children born with problems related to being preterm may need lifelong medical care.
-
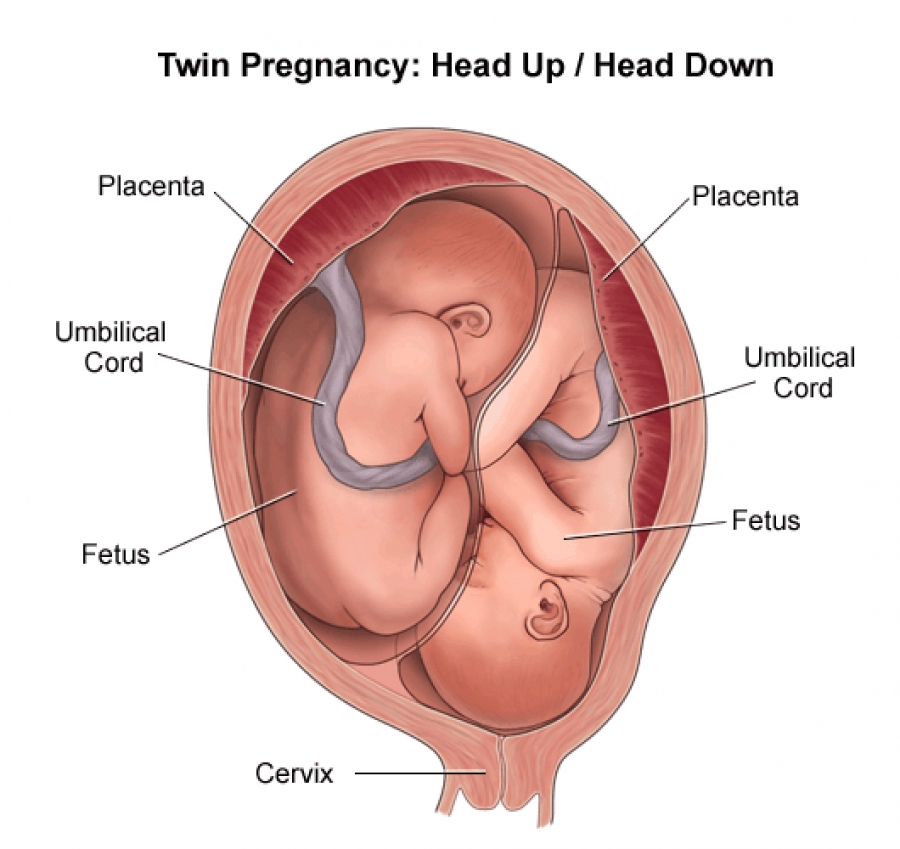
Early in a multiple pregnancy, an ultrasound exam is done to find out whether each fetus has its own chorion (chorionicity) and amniotic sac (amnionicity).
 There are three types of twins:
There are three types of twins:-
Dichorionic–diamniotic—Twins who have their own chorions and amniotic sacs. They typically do not share a placenta and can be fraternal or identical.
-
Monochorionic–diamniotic—Twins who share a chorion but have separate amniotic sacs. They share a placenta and are identical.
-
Monochorionic–monoamniotic—Twins who share one chorion and one amniotic sac. They share a placenta and are identical.
-
-
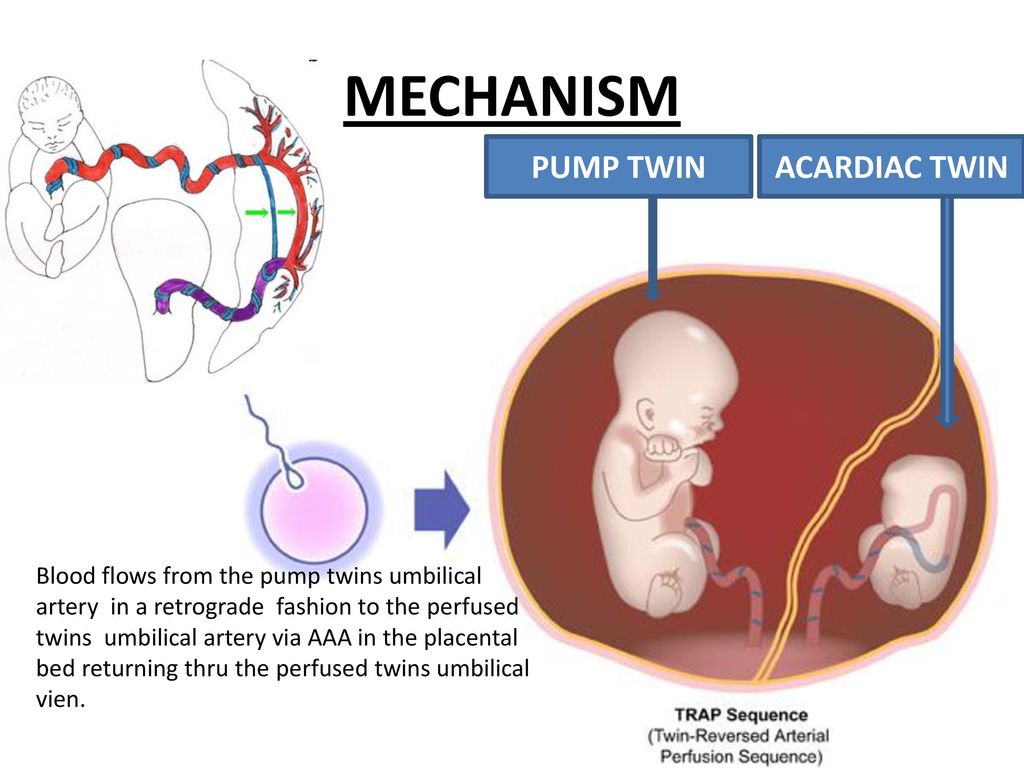
Monochorionic twins have a higher risk of complications than those with separate placentas. One problem that can occur in monochorionic–diamniotic babies is twin–twin transfusion syndrome (TTTS). In TTTS, the blood flow between the twins becomes unbalanced. One twin donates blood to the other twin. The donor twin has too little blood, and the recipient twin has too much blood.
 The earlier TTTS occurs in the pregnancy, the more serious the outcomes for one or both babies.
The earlier TTTS occurs in the pregnancy, the more serious the outcomes for one or both babies.Although monochorionic–monoamniotic babies are rare, this type of pregnancy is very risky. The most common problem is an umbilical cord complication. Women with this type of pregnancy are monitored more frequently and are likely to have a cesarean birth.
-
Preeclampsia is a blood pressure disorder that usually starts after 20 weeks of pregnancy or after childbirth. It occurs more often in multiple pregnancies than in singleton pregnancies. It also tends to occur earlier and is more severe in multiple pregnancies.
Preeclampsia can damage many organs in your body, most commonly your kidneys, liver, brain, and eyes. Preeclampsia that worsens and causes seizures is called eclampsia. When preeclampsia occurs during pregnancy, the babies may need to be delivered right away, even if they are not fully grown.
-
Women carrying multiples have a high risk of gestational diabetes. This condition can increase the risk of preeclampsia and of developing diabetes mellitus later in life. Newborns may have breathing problems or low blood sugar levels. Diet, exercise, and sometimes medication can reduce the risk of these complications.
-
Multiples are more likely to have growth problems than single babies. Multiples are called discordant if one fetus is much smaller than the others.
Discordant growth is common with multiples. It does not always signal a problem. Sometimes, though, a fetus’s restricted growth may be caused by an infection, TTTS, or a problem with the placenta or umbilical cord. If growth restriction is suspected in one or both fetuses, frequent ultrasound exams may be done to track how the fetuses are growing.
-
Screening tests for genetic disorders that use a sample of a woman's blood are not as sensitive in multiple pregnancy. It is possible to have a positive screening test result when no problem is present in either fetus.
-
Diagnostic tests for birth defects include chorionic villus sampling (CVS) and amniocentesis. These tests are harder to perform in multiples because each fetus must be tested. There also is a small risk of loss of one or all of the fetuses. Results of these tests may show that one fetus has a disorder, while the others do not.
-
The chance of cesarean birth is higher with multiples. In some cases, twins can be delivered by vaginal birth. How your babies are born depends on
-
the number of babies and the position, weight, and health of each baby
-
your health and how your labor is going
-
the experience of your ob-gyn
-
-
Having multiples might increase your risk of postpartum depression.
 If you have intense feelings of sadness, anxiety, or despair that keep you from being able to do your daily tasks, talk with your ob-gyn or other member of your health care team.
If you have intense feelings of sadness, anxiety, or despair that keep you from being able to do your daily tasks, talk with your ob-gyn or other member of your health care team. -
Yes, but it may take some practice. Your milk supply will increase to the right amount. You will need to eat healthy foods and drink plenty of liquids. Lactation specialists are available at many hospitals and in your community to help you work out any problems you may have.
[See How to Prepare for Breastfeeding in the Month Before Birth]
-
Amniocentesis: A procedure in which amniotic fluid and cells are taken from the uterus for testing. The procedure uses a needle to withdraw fluid and cells from the sac that holds the fetus.
Amnionicity: The number of amniotic (inner) membranes that surround fetuses in a multiple pregnancy.
 When multiple fetuses have only one amnion, they share an amniotic sac.
When multiple fetuses have only one amnion, they share an amniotic sac.Amniotic Sac: Fluid-filled sac in a woman’s uterus. The fetus develops in this sac.
Birth Defects: Physical problems that are present at birth.
Cerebral Palsy: A disorder of the nervous system that affects movement, posture, and coordination. This disorder is present at birth.
Cesarean Birth: Birth of a fetus from the uterus through an incision made in the woman’s abdomen.
Chorion: The outer membrane that surrounds the fetus.
Chorionic Villus Sampling (CVS): A procedure in which a small sample of cells is taken from the placenta and tested.
Chorionicity: The number of chorionic (outer) membranes that surround the fetuses in a multiple pregnancy.
Complication: A disease or condition that happens as a result of another disease or condition.
 An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Diagnostic Tests: Tests that look for a disease or cause of a disease.
Discordant: A large difference in the size of fetuses in a multiple pregnancy.
Eclampsia: Seizures occurring in pregnancy or after pregnancy that are linked to high blood pressure.
Egg: The female reproductive cell made in and released from the ovaries. Also called the ovum.
Embryo: The stage of development that starts at fertilization (joining of an egg and sperm) and lasts up to 8 weeks.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Fraternal Twins: Twins that have developed from two different fertilized eggs.
Genetic Disorders: Disorders caused by a change in genes or chromosomes.
Gestational Diabetes: Diabetes that starts during pregnancy.
Identical Twins: Twins that have developed from a single fertilized egg that are usually genetically identical.
In Vitro Fertilization (IVF): A procedure in which an egg is removed from a woman’s ovary, fertilized in a laboratory with the man’s sperm, and then transferred to the woman’s uterus to achieve a pregnancy.
Menstrual Cycle: The monthly process of changes that occur to prepare a woman’s body for possible pregnancy. A menstrual cycle is defined as the first day of menstrual bleeding of one cycle to the first day of menstrual bleeding of the next cycle.
Multiple Pregnancy: A pregnancy where there are two or more fetuses.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.

Ovaries: Organs in women that contain the eggs necessary to get pregnant and make important hormones, such as estrogen, progesterone, and testosterone.
Ovulation: The time when an ovary releases an egg.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Postpartum Depression: A type of depressive mood disorder that develops in the first year after the birth of a child. This type of depression can affect a woman’s ability to take care of her child.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain over the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Prenatal Care: A program of care for a pregnant woman before the birth of her baby.

Preterm: Less than 37 weeks of pregnancy.
Screening Tests: Tests that look for possible signs of disease in people who do not have signs or symptoms.
Sperm: A cell made in the male testicles that can fertilize a female egg.
Twin–Twin Transfusion Syndrome (TTTS): A condition of identical twins in which one twin gets more blood than the other during pregnancy.
Ultrasound Exam: A test in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Umbilical Cord: A cord-like structure containing blood vessels. It connects the fetus to the placenta.
Uterus: A muscular organ in the female pelvis. During pregnancy, this organ holds and nourishes the fetus. Also called the womb.
Don't have an ob-gyn? Search for doctors near you.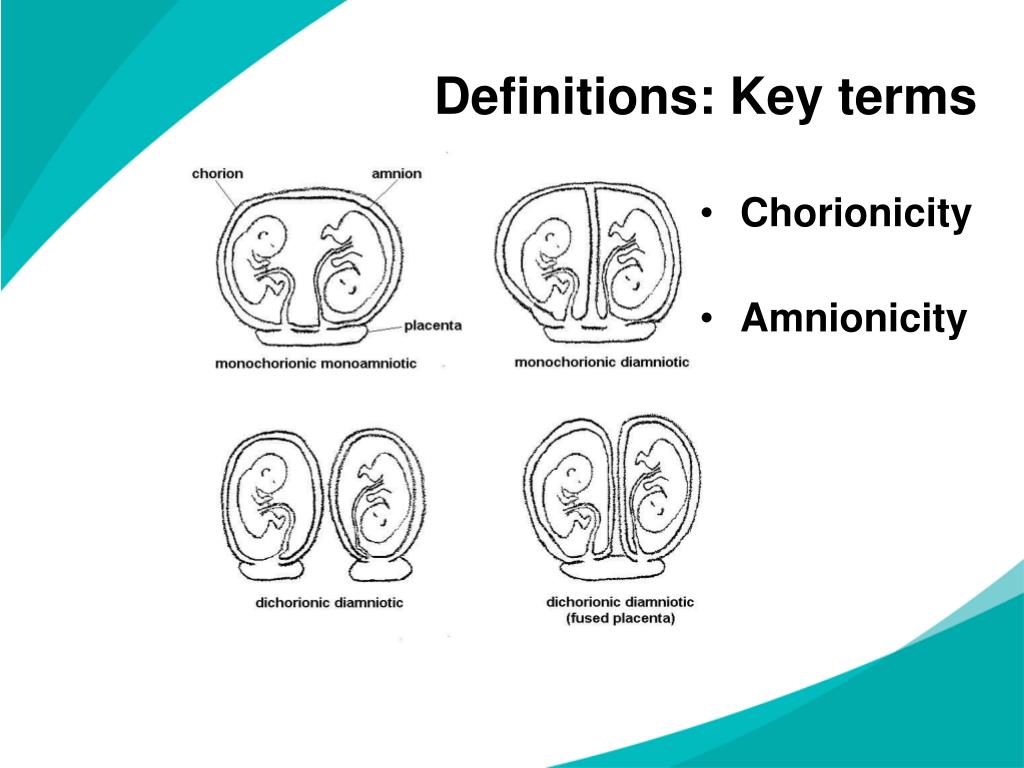
FAQ188
Last updated: February 2021
Last reviewed: June 2020
Copyright 2023 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information.
This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer.
Types of multiple pregnancy | Pregnancy Birth and Baby
Types of multiple pregnancy | Pregnancy Birth and Baby beginning of content5-minute read
Listen
A multiple pregnancy is when you are pregnant with more than one baby. You might be expecting twins, triplets or more!
You might be expecting twins, triplets or more!
In Australia, about 3 in 100 births are multiple babies. And most of these are twins.
How do multiple pregnancies occur?
Multiple pregnancies occur when more than one embryo implants in your uterus (womb). This can happen:
- if you release more than one egg during your menstrual cycle and each egg is fertilised by a sperm
- your fertilised egg splits into 2, resulting in 2 identical embryos
Multiple pregnancies are more common than they used to be. This is mainly because of the increasing use of in vitro fertilisation (IVF). The fertility medicines used in IVF often cause more than one egg to be released from the ovaries.
Sometimes with IVF, more than one fertilised embryo is transferred to the uterus. This can result in a multiple pregnancy.
Another way a multiple pregnancy can occur is if one of the transferred eggs splits in two. This results in twins.
Women aged 35 years and older are more likely to release more than one egg when they ovulate.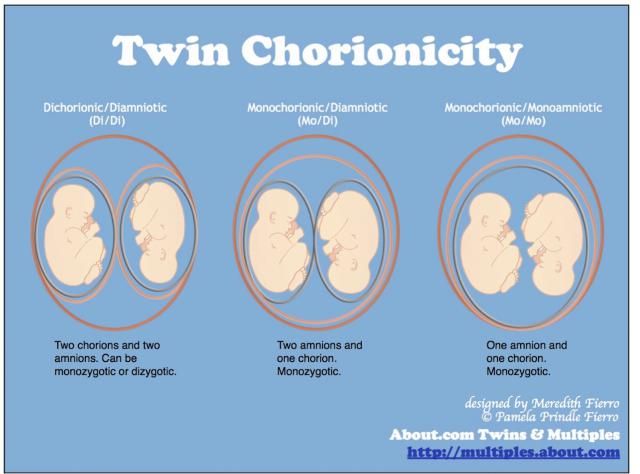 This means that you are more likely to have non-identical twins as you get older.
This means that you are more likely to have non-identical twins as you get older.
You are also more likely to have a multiple pregnancy if there is a history of non-identical twins on your mother’s side of the family. Identical twins do not run in families.
Diagnosis of multiple pregnancy
Signs that you might be expecting multiple babies include:
- you seem bigger than you should be for your dates
- twins run in your family
- you have had fertility treatment
A multiple pregnancy is confirmed by an ultrasound scan. This is usually in the first trimester (the first 12 weeks of pregnancy).
The ultrasound will confirm the type of multiple pregnancy. This includes:
- the number of placentas
- the number of amniotic sacs
These are all important factors for later in the pregnancy. It's important to identify these factors as early as possible.
If you are carrying multiple babies, you will have to see your doctor or midwife more often than someone who is expecting one baby.
Most multiple pregnancies progress smoothly. However, there's a higher chance of your babies:
- being born prematurely
- having a low birth weight
You may also have complications with your pregnancy, such as:
- gestational diabetes
- pre-eclampsia
- premature labour
- bleeding
Types of multiple pregnancy
The most common type of multiples include the following.
Fraternal twins
Two separate eggs are fertilised and implant in the uterus.
Your babies are:
- siblings
- share the same uterus
- may look similar or different
- may be the same gender (2 girls or 2 boys) or different genders (a boy and a girl)
A pregnancy with fraternal twins has the lowest risk of all multiple pregnancies. This is because each baby has its own placenta and amniotic sac.
You will sometimes hear fraternal twins referred to as 'dizygotic' twins.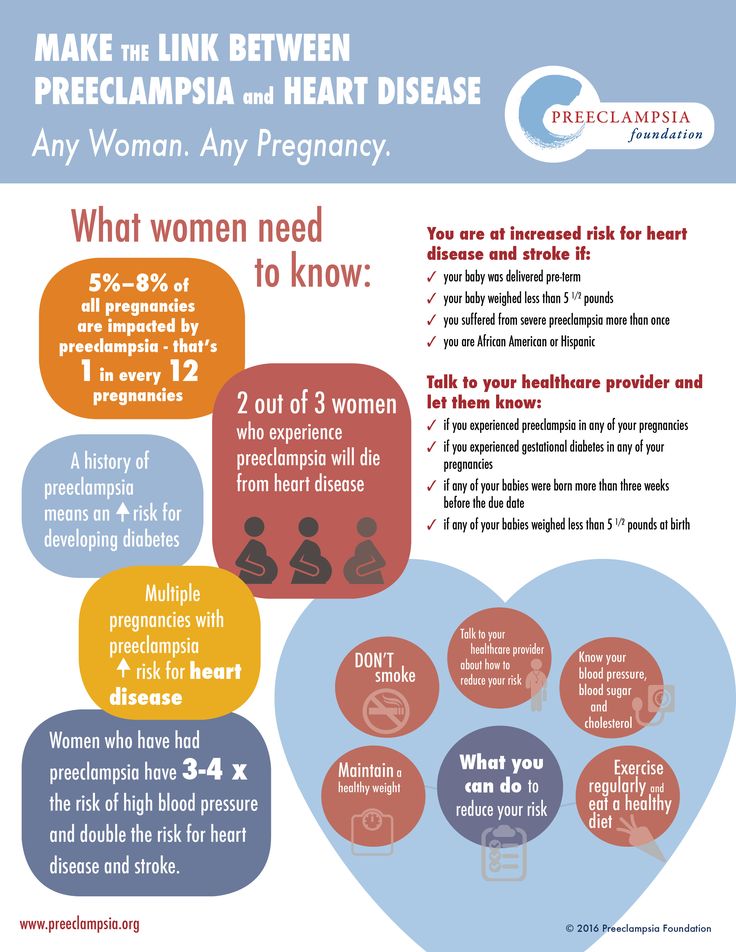 This refers to 2 zygotes (fertilised eggs).
This refers to 2 zygotes (fertilised eggs).
Identical twins
Identical twins are formed when a single fertilised egg splits in 2.
Each embryo is genetically identical, so the babies share the same DNA. That means that your babies will share many characteristics. But sometimes identical twins can look quite different. This is because their appearance is also influenced by the environment.
Identical twins may:
- share the same placenta and amniotic sac
- share a placenta but have their own amniotic sac
- have their own placenta and amniotic sac
You will sometimes hear identical twins referred to as 'monozygotic'. This refers to one zygote (fertilised egg).
Triplets and 'higher order multiples' (HOMs)
Triplets, quadruplets, quintuplets, sextuplets or more can be a combination both of identical and fraternal multiples.
For example, triplets can be:
- fraternal (trizygotic), forming from 3 individual eggs that are fertilised and implant in your uterus
- identical, when one egg divides into 3 embryos
- a combination of both fraternal and identical babies
Getting support
If you are having multiple babies, you will need a lot of support throughout your pregnancy and after the babies are born.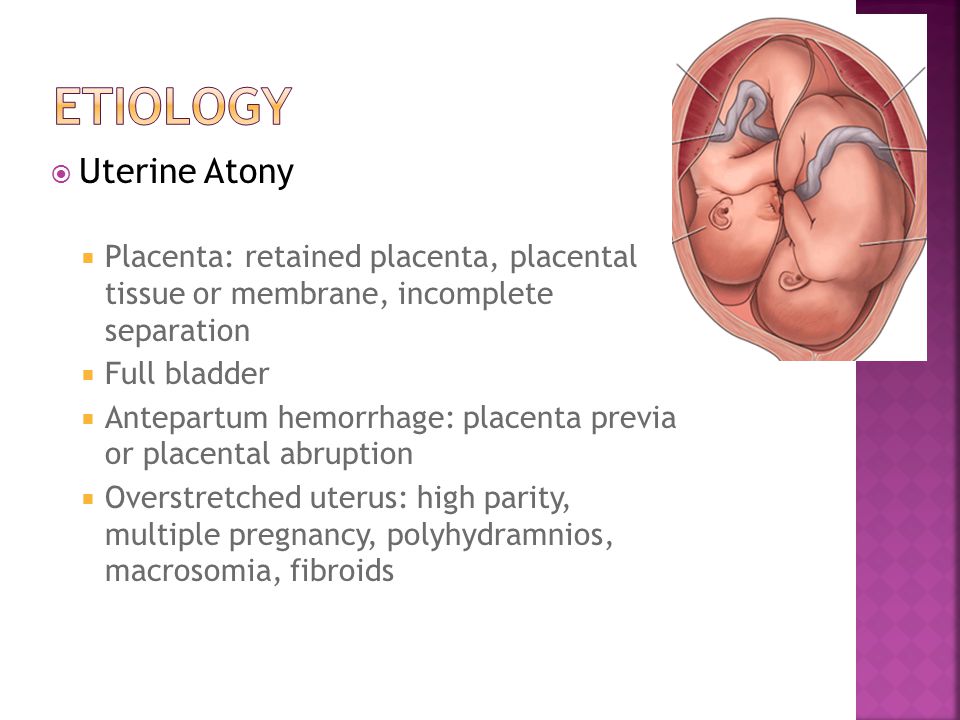
For support and resources, you can contact the Australian Multiple Birth Association. You can also call Pregnancy, Birth and Baby on 1800 882 436 for advice or support.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
AIHW (Mothers who have multiple births and their babies), NHS (Pregnant with twins), Royal College of Obstetricians and Gynaecologists (Multiple pregnancy: having more than one baby)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Twins, triplets and multiples
Need more information?
The psychology of raising twins and multiples
Helping twins to understand the psychology of their relationship means going right back to conception.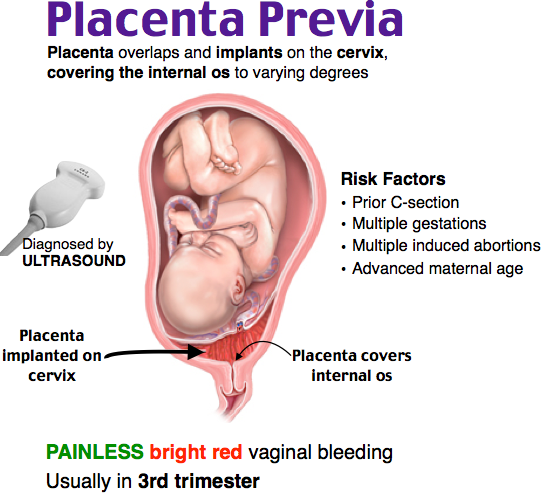 They've had to share space right from the time of conception, and that really sets the stage for sharing space right throughout life.
They've had to share space right from the time of conception, and that really sets the stage for sharing space right throughout life.
Read more on Twins Research Australia website
Fraternal twins & identical twins | Raising Children Network
Whether you’re having fraternal twins or identical twins, it’s good to find out during pregnancy. Get the facts you need about different types of twins.
Read more on raisingchildren.net.au website
Twins, triplets and multiples
If you are having twins, triplets or more, find out everything you need to know about your pregnancy, the birth, feeding and raising your babies.
Read more on Pregnancy, Birth & Baby website
Twins and multiple births - Better Health Channel
Multiple births are more common than they used to be, due to the increased use of assisted reproductive techniques, in particular the use of fertility drugs.
Read more on Better Health Channel website
Multiple birth - triplets or more
If you are pregnant with triplets or more, the birth will need careful planning. The main risk is that your babies will be born prematurely. Find out more here.
Read more on Pregnancy, Birth & Baby website
Multiple pregnancy (triplets or more)
Learning you're pregnant with triplets or more can be a shock, but overall, most parents find having multiple babies to be a positive experience.
Read more on Pregnancy, Birth & Baby website
What are the current multiple pregnancy and birth trends?
There has been an overall increasing trend in multiple births in the last two decades in Australia.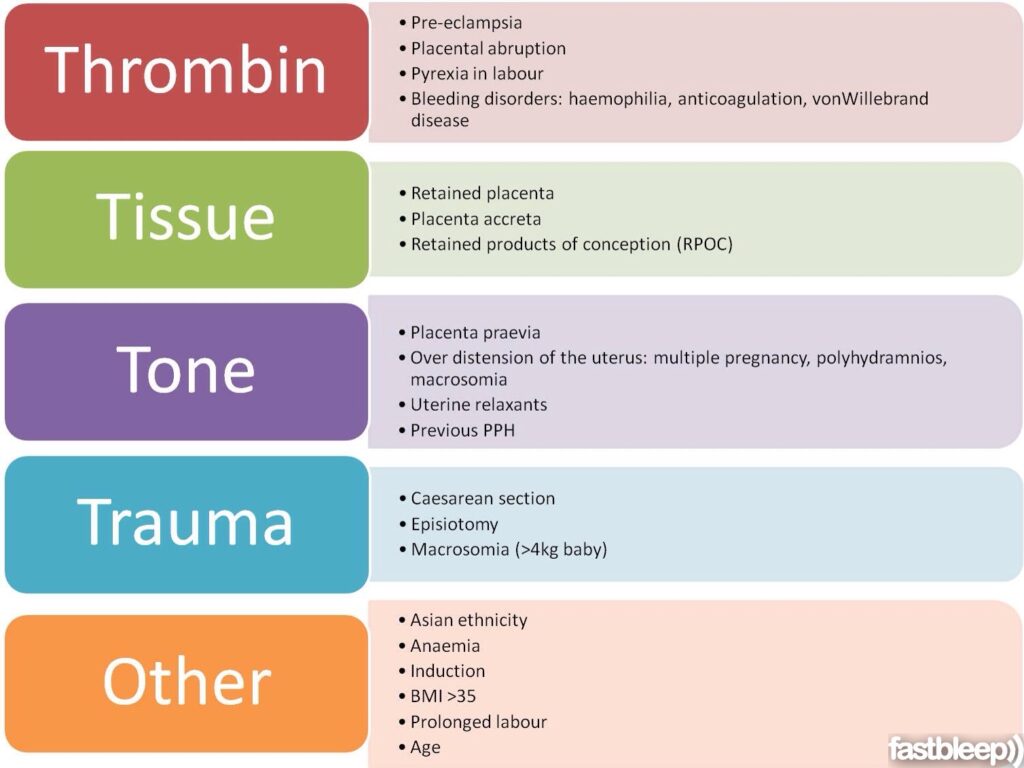 Attributed largely to the increased use of fertility drugs and assisted reproduction technology and the growing number of older mothers.
Attributed largely to the increased use of fertility drugs and assisted reproduction technology and the growing number of older mothers.
Read more on Twins Research Australia website
Expecting twins?
Congratulations from Twins Research Australia on your happy news. No doubt you are keen to find out as much as possible about twin pregnancy and the early days of parenting.
Read more on Twins Research Australia website
Pregnant with twins? About twin pregnancy | Raising Children Network
Pregnant with twins? Twin pregnancy can have more complications, so you’ll need more check-ups. Here’s what to expect in your pregnancy and antenatal care.
Read more on raisingchildren.net.au website
Pregnant with twins
If you're pregnant with twins, a healthy lifestyle and diet will help you manage your pregnancy and give your babies the best start in life.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.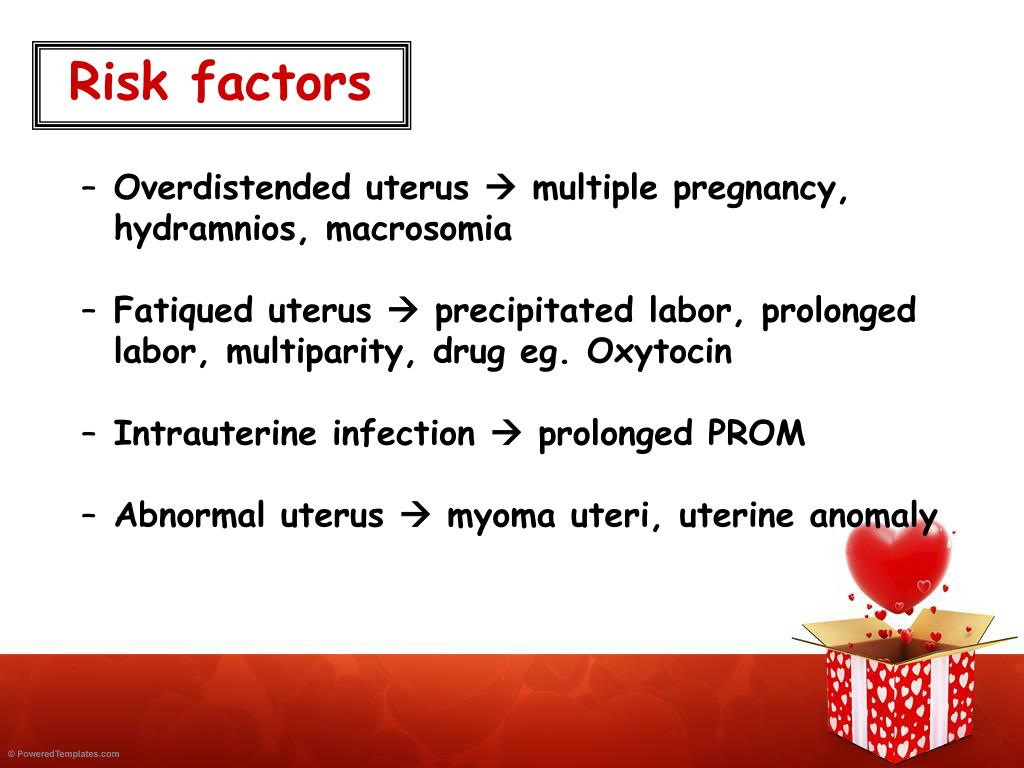
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Multiple pregnancy: a modern view on the problem of managing pregnancy and childbirth (literature review) | Tsivtsivadze E.B., Novikova S.V.
The problem of the appearance of twins has been worrying the minds since the existence of mankind, has ethnic, cultural, social and economic implications. Traditions associated with the birth of twins have appeared in all ages.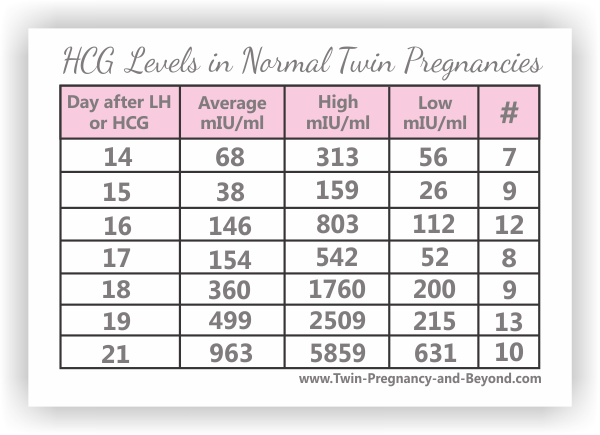 Hippocrates believed that twins were the result of the division of the seed into two parts, Democritus considered twins as the result of an excess of the seed, Aristotle explained the appearance of twins by the splitting of one germ into two. But even so far there is no unambiguous hypothesis explaining the formation of monozygotic twins. nine0003
Hippocrates believed that twins were the result of the division of the seed into two parts, Democritus considered twins as the result of an excess of the seed, Aristotle explained the appearance of twins by the splitting of one germ into two. But even so far there is no unambiguous hypothesis explaining the formation of monozygotic twins. nine0003
The relevance of the problem of multiple pregnancy lies in a significant number of complications during pregnancy and childbirth, an increase in the proportion of cesarean section, postpartum complications, an increased level of antenatal losses at various gestational periods, and a high incidence of neurological disorders in surviving children [44].
Multiple pregnancies occur in 1.5–2.5% of cases, more often in families where the mother or father, or both spouses, were born as a result of a multiple pregnancy [1]. In this case, the genotype of the mother plays the most significant role. It is impossible not to recall the well-known formula, according to which multiple pregnancies occur with a frequency of geometric progression, which is formed when the number is raised to the power of 80: one twin occurs in 80 births, triplets - in 80 births in a square (6400), quadruple - in 80 births in a cube ( 512,000), five - for 80 births in the fourth degree (40 960,000).
The interest in multiple pregnancies that has existed since ancient times has increased in the last 15–20 years due to the avalanche-like increase in multiple pregnancies associated with the introduction of assisted reproductive technologies.
Patients with multiple pregnancies remain at a high risk of perinatal complications. Even with the modern development of medicine, perinatal mortality during twin pregnancy is 5 times higher than in singleton pregnancy, intrauterine fetal death is 4 times higher, neonatal - 6 times, perinatal - 10 times. The frequency of cerebral palsy in children from twins is 3-7 times higher, with triplets - 10 times. The level of ante- and intranatal complications on the part of the mother is 2-10 times higher than that in patients with singleton pregnancies [7, 14, 17, 19, 35, 40, 60].
Perinatal morbidity and mortality in twins depend on chorionicity. According to Sebire studies, the perinatal mortality rate, mainly due to severe prematurity at birth, is higher in monochorionic twins than in dichorionic twins (5 and 2%, respectively).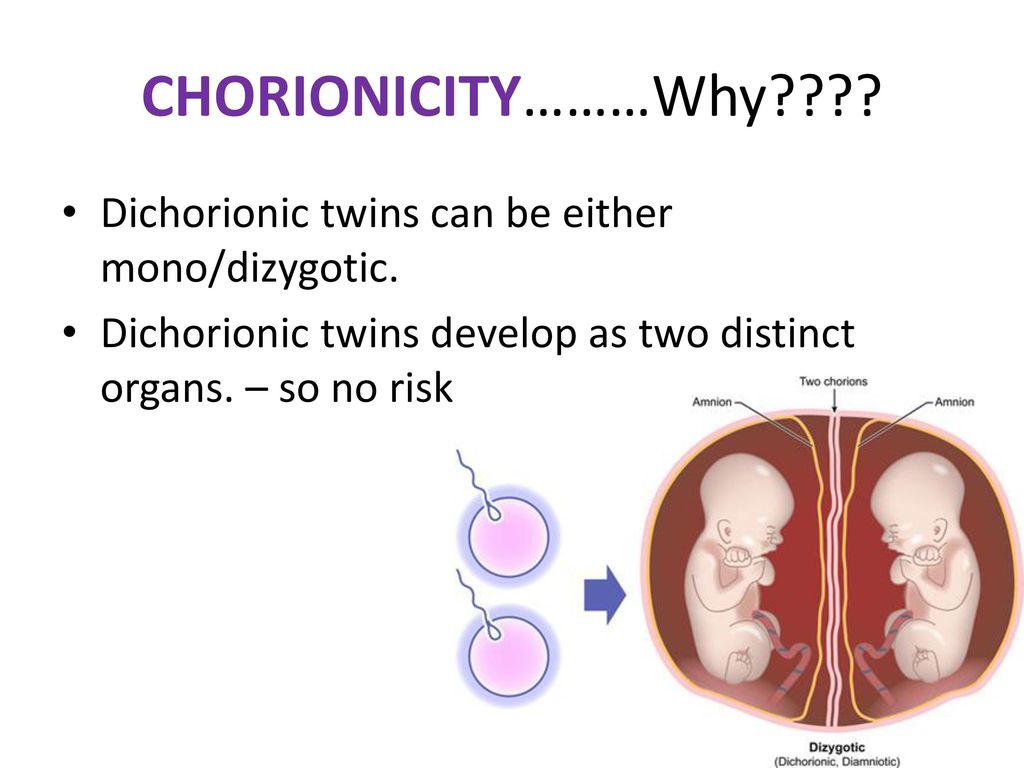 The frequency of preterm birth up to 32 weeks. in monochorionic pregnancy is 10% compared to 5% in dichorionic twins. The frequency of spontaneous abortion in the period from the 11th to the 24th week. with dichorionic twins it is 2%, with monochorionic twins it is about 10% [1, 33, 50, 64, 65]. nine0003
The frequency of preterm birth up to 32 weeks. in monochorionic pregnancy is 10% compared to 5% in dichorionic twins. The frequency of spontaneous abortion in the period from the 11th to the 24th week. with dichorionic twins it is 2%, with monochorionic twins it is about 10% [1, 33, 50, 64, 65]. nine0003
Interesting data were obtained by a group of authors who studied sex-associated differences in perinatal complications in 16,045 pregnant women with twins. Women with female twins have been found to have an increased risk of preeclampsia, but after birth, these twins had lower rates of neonatal and infant mortality, as well as a lower risk of respiratory disease than male twins [66].
Determination of zygosity before delivery is possible only when examining DNA in fetuses obtained as a result of amniocentesis, chorionic biopsy or cordocentesis. However, on the basis of zygosity, one cannot judge the type of placentation. Monozygotic twins can be either monochorionic or bichorionic [56].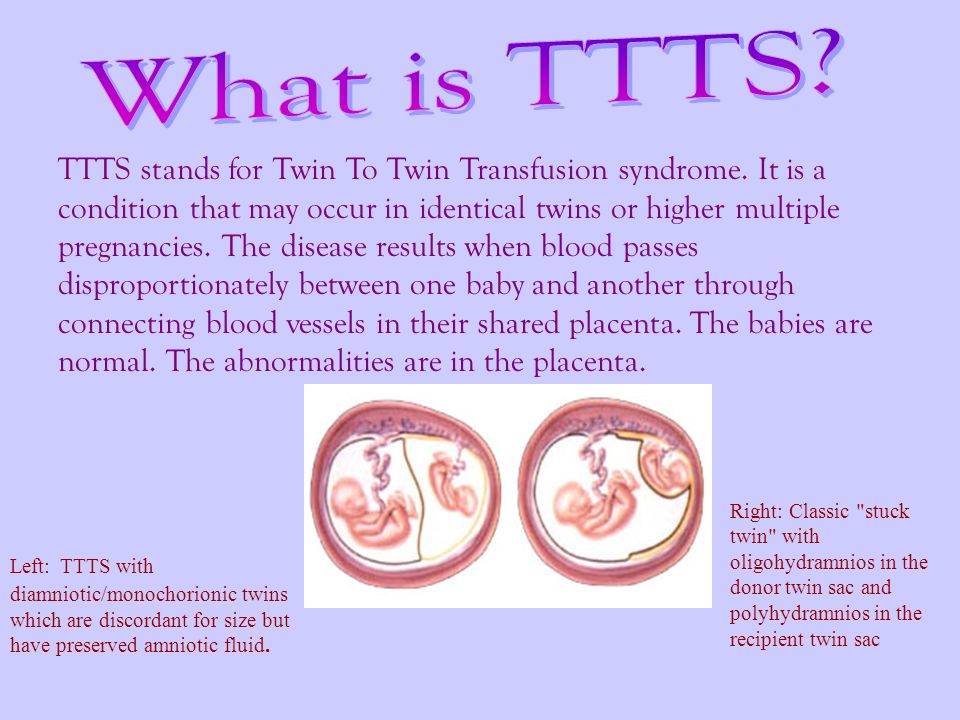 nine0003
nine0003
Determination of the chorionicity of the fetuses is possible during an ultrasound scan, during which the number of placentas, the sex of the fetuses, and the presence of an amniotic septum are determined. The optimal time for the diagnosis of chorionicity is 6–9 weeks. pregnancy. In the presence of dichorionic twins, two fetal eggs are determined, separated by a thickened septum of 2 mm or more. The use of this criterion makes it possible to diagnose mono- and bichorionic twins with an accuracy of up to 85% and 92.3%, respectively [71]. nine0003
Multiple pregnancy may be complicated by growth retardation of one or both fetuses, feto-fetal transfusion syndrome (FFTS), intrauterine death of one or both fetuses.
FFTS, first described by Schatz in 1982, occurs in 1 out of 5 monochorionic twins [47, 48]. Its morphological substrate is the anastomosing vessels between the two fetal circulatory systems [28]. This is a specific complication for monozygotic twins with a monochorionic type of placentation.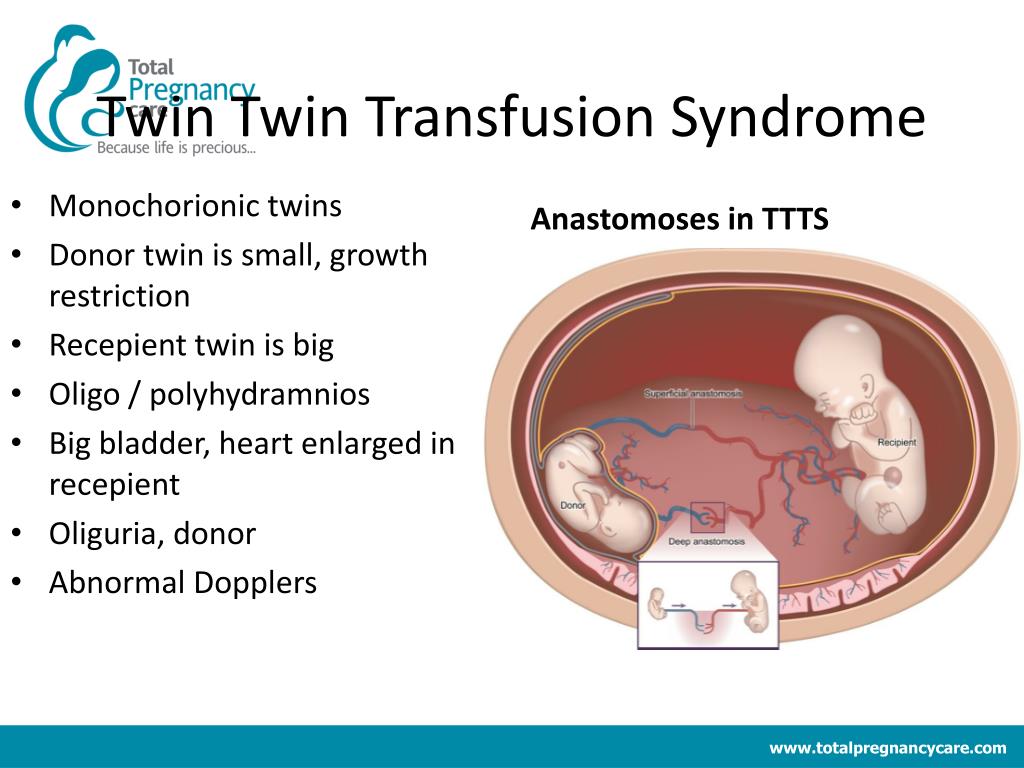 Of particular difficulty are monochorionic monoamniotic twins, when pregnancy is complicated not only by FTTS, but also by problems with the umbilical cords of the fetuses (Fig. 1). nine0003
Of particular difficulty are monochorionic monoamniotic twins, when pregnancy is complicated not only by FTTS, but also by problems with the umbilical cords of the fetuses (Fig. 1). nine0003
The criteria for FFTS are an intra-pair difference in weight of more than 20% and different concentrations of hemoglobin in fetuses [23]. For many years, the diagnosis of TTTS was established retrospectively in the neonatal period. Based on the data of ultrasound diagnostics, FFTS criteria were developed, which are used in practice to determine the management of pregnancy [63].
The most common factor associated with ante- and neonatal mortality and morbidity in twin pregnancies is low birth weight. In the vast majority of cases, low body weight of children is due to preterm birth. Various hypotheses of threatened miscarriage in multiple pregnancies are discussed in the literature. According to one of them (premature birth is a natural consequence of twin pregnancy), the main cause of premature development of labor is the overstretching of the muscle fibers of the uterus, the release of prostaglandins and reduced uteroplacental blood flow.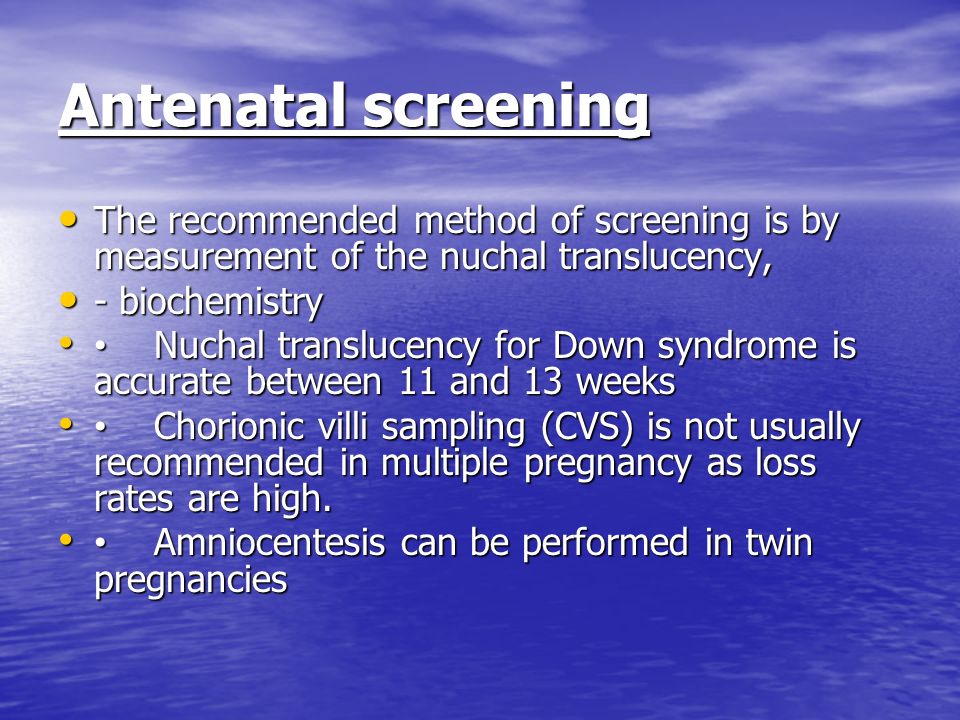 Another hypothesis is based on the data of the Joint Perinatology Project [4], indicating that infection of the amniotic membranes contributes to their premature rupture, which most often leads to preterm birth. nine0003
Another hypothesis is based on the data of the Joint Perinatology Project [4], indicating that infection of the amniotic membranes contributes to their premature rupture, which most often leads to preterm birth. nine0003
A systematic review of randomized controlled trials evaluating the efficacy of antenatal screening for lower genital tract infections and their treatment in reducing preterm birth and associated morbidity demonstrated the high efficacy of such screening programs. Thus, in the intervention group (2058 women) screening and treatment of bacterial vaginosis, trichomoniasis and candidiasis were performed, in the control group (2097 women) were not screened, they were examined only in the presence of complaints or clinical manifestations. Preterm birth before 37 weeks. were observed significantly less frequently in the intervention group (3% vs. 5% in the control group) with a relative risk (BP) of 0.55 (95% CI 0.41 to 0.75). The frequency of birth of children with low body weight (weighing 2500 g or less) was 52% lower in the intervention group (BP 0. 48, 95% CI 0.34 to 0.66), and very low birth weight children (weighing 1500 g or less) - 6% lower in the intervention group than in the control group (BP 0.34, 95% CI 0.15 to 0.75) [53].
48, 95% CI 0.34 to 0.66), and very low birth weight children (weighing 1500 g or less) - 6% lower in the intervention group than in the control group (BP 0.34, 95% CI 0.15 to 0.75) [53].
Thus, there is high-certainty evidence that screening and treatment programs for vaginal infections in pregnant women reduce preterm and low birth weight preterm births.
The high-risk group for complications during pregnancy and perinatal outcomes should include women with congenital anomalies in the development of the uterus. The results of numerous studies have shown that the outcome of pregnancy is largely due to the nature and severity of the malformation of the uterus. Relatively favorable outcomes were observed with a saddle uterus, unfavorable - with a bicornuate uterus and intrauterine septum [2, 9, 11, 38]. So, in the literature available to us, only 7 cases of multiple pregnancy in a bicornuate uterus were found. A. Bongain et al. (1994) suggest that the possibility of fertilization of two eggs in a pregnant woman with a congenital anomaly of the uterus (bicornuate, complete doubling) is 1:1,000,000.
Based on the foregoing, our clinical case of multiple pregnancy with complete duplication of the uterus is of scientific and practical interest.
Pregnant S., 1988 years of age, was observed under the conditions of MONIIAG in 2010 due to the presence of an anomaly in the development of the genitourinary system - complete doubling of the uterus and pregnancy with twins. The pregnancy proceeded with the phenomena of the threat of termination, for which inpatient treatment was repeatedly carried out. On December 28, 2010, emergency delivery was performed at a gestational age of 35 weeks. due to premature rupture of amniotic fluid. A Pfannenstiel transection was performed, caesarean sections were performed in the lower uterine segments of both uterus with Derfler incisions (Fig. 2). The children were born weighing 2320 and 2000, are currently healthy. nine0003
Neurological complications are a significant problem in multiple pregnancies [6, 44]. The greatest number of neurological complications is observed in premature babies and in children with malnutrition, as well as in the presence of FTTS.
Stillbirth and neonatal mortality in multiple pregnancies are recorded 3 times more often than in singleton pregnancies, and are respectively 14.9 and 19.8 per 1000 live births. The financial costs of providing medical care to each child from twins with multiple pregnancies during the first 5 years of life are 2 times higher than those for children born with a single pregnancy. nine0003
Prematurity is considered as the main cause of neonatal mortality in multiple pregnancies. Preterm birth is the leading cause of neonatal death, as well as early and delayed disability. The rate of preterm birth varies from 6% to 12% in developed countries, and this figure is usually higher in developing countries. About 40% of all preterm births occur before 34 weeks. and 20% - up to 32 weeks. The contribution of these preterm births to the total perinatal morbidity and mortality is more than 50% [38, 46]. nine0003
Despite a significant arsenal of tocolytic agents, the frequency of preterm births in the world is not decreasing, and the decrease in perinatal mortality is mainly due to the success of neonatologists in nursing premature babies.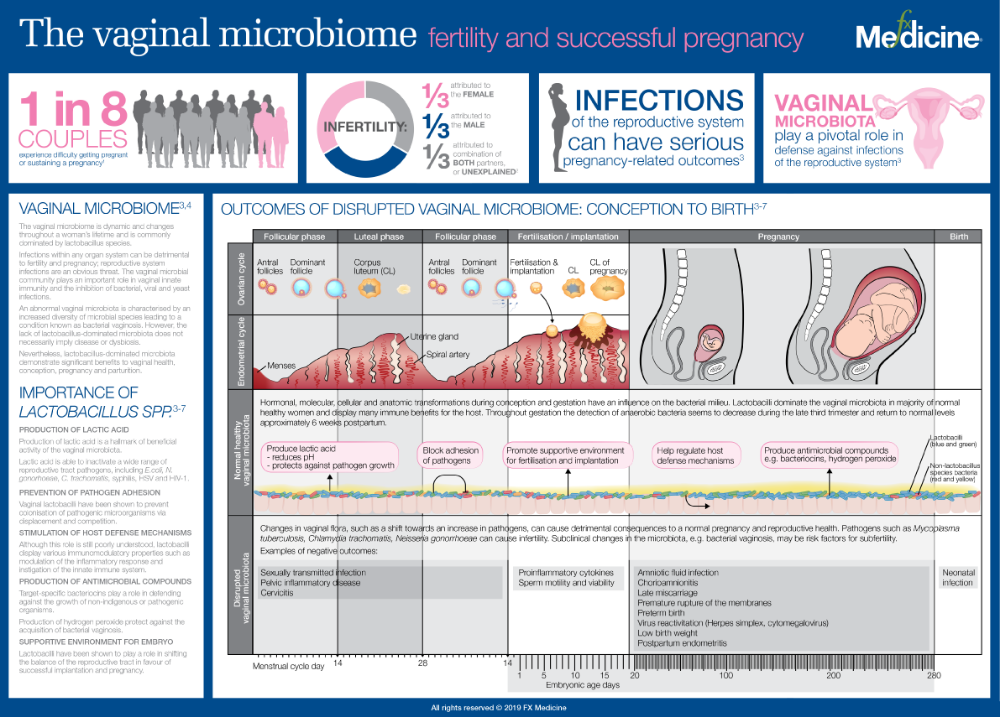 In connection with the foregoing, the tactics of managing and treating the threat of preterm labor should take into account the possible causes of their development, and not consist only in the appointment of symptomatic agents aimed at reducing the contractile activity of the uterus. nine0003
In connection with the foregoing, the tactics of managing and treating the threat of preterm labor should take into account the possible causes of their development, and not consist only in the appointment of symptomatic agents aimed at reducing the contractile activity of the uterus. nine0003
At present, some progress has been made in the treatment of threatened preterm labor due to drugs that suppress the contractile activity of the uterus.
In practical obstetrics, magnesium sulfate is often used. The mechanism of action of Mg2+ ions on smooth muscles has not been finally established. An important aspect of the use of magnesium sulfate in obstetric practice is the presence of an anticonvulsant effect in the drug, which allows it to be used to treat preeclampsia and eclampsia. With the threat of preterm birth, the prophylactic use of magnesium sulfate as a monotherapy has a less pronounced effect. nine0003
There is evidence of a relationship between the use of magnesium sulfate in the prenatal period in preterm labor or preeclampsia and a subsequent decrease in the risk of developing cerebral palsy in premature newborns with low birth weight.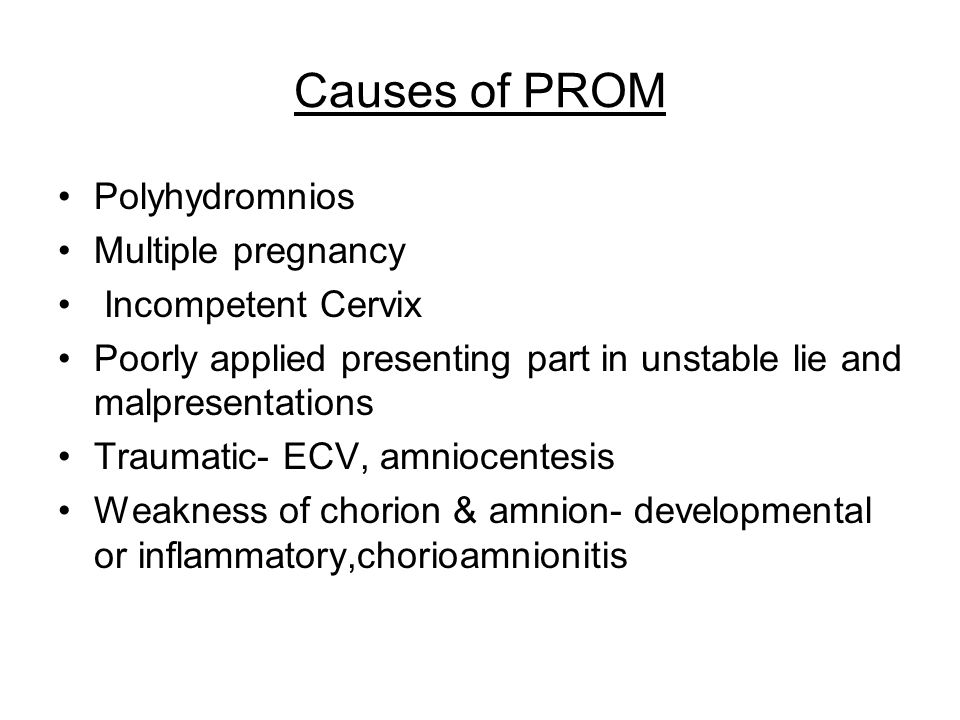 It should be emphasized that a neuroprotective effect was demonstrated for low total doses of magnesium sulfate (4 and 12 g), while for high total doses (>30 g) a toxic effect was demonstrated, which was accompanied by an increase in infant mortality. Incidence statistics were assessed using electronic databases and journal publications [25]. nine0003
It should be emphasized that a neuroprotective effect was demonstrated for low total doses of magnesium sulfate (4 and 12 g), while for high total doses (>30 g) a toxic effect was demonstrated, which was accompanied by an increase in infant mortality. Incidence statistics were assessed using electronic databases and journal publications [25]. nine0003
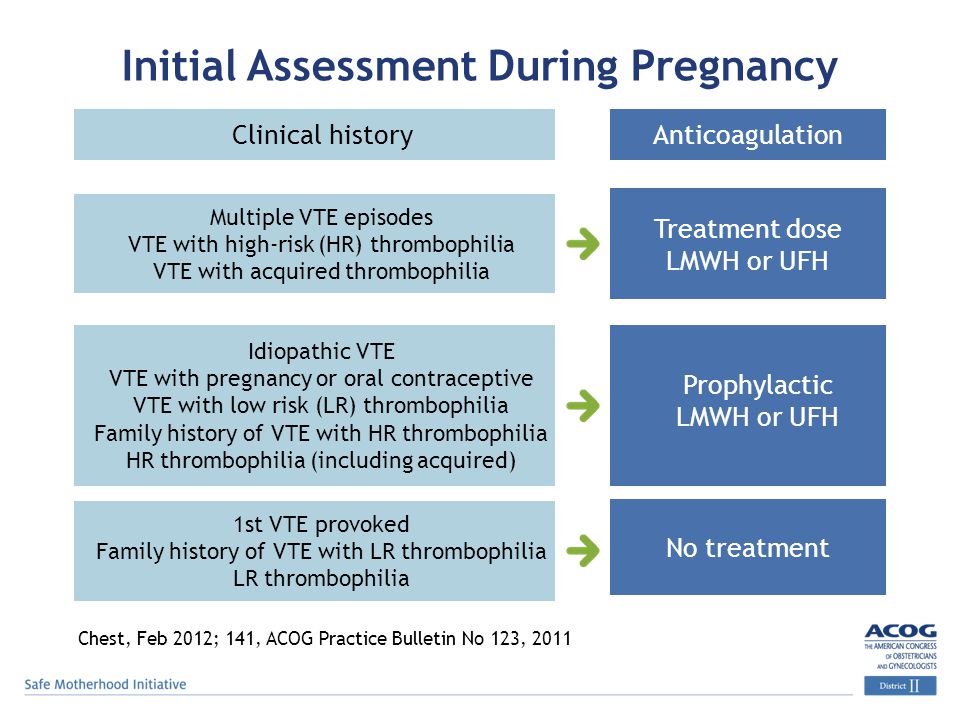
The Committee on Obstetrics of the American College of Obstetricians and Gynecologists (ACOG, March 2010), based on multicenter data on the neuroprotective effect of magnesium sulfate and the reduction in the incidence of cerebral palsy in preterm infants, recommends that the use of this drug be added to protocols for impending PR <30 weeks: bolus 4-6 g of magnesium sulfate, then infusion of 1-2 g/h for 12 hours [27, 32, 33].
In recent decades, both foreign and domestic researchers have accumulated considerable experience in the use of calcium channel blockers in obstetric practice, primarily in diseases accompanied by an increase in blood pressure. However, the use of calcium channel blockers as tocolytic agents in case of threatened miscarriage is often accompanied by undesirable effects. It should also be remembered that in Russia nifedipine is not registered as a tocolytic agent, therefore, before using it, it is necessary to obtain the written informed consent of the patient for its use [10, 22, 55]. nine0003
However, the use of calcium channel blockers as tocolytic agents in case of threatened miscarriage is often accompanied by undesirable effects. It should also be remembered that in Russia nifedipine is not registered as a tocolytic agent, therefore, before using it, it is necessary to obtain the written informed consent of the patient for its use [10, 22, 55]. nine0003
As you know, the decisive role in the regulation of the contractile function of the uterus during childbirth is assigned to biologically active substances of a lipid nature - prostaglandins (especially PGF2a). The tocolytic effect of prostaglandin synthesis inhibitors has been proven experimentally and as a result of clinical observations. However, without selective properties, prostaglandin synthesis inhibitors cause undesirable effects on the fetus and newborn. The most severe complications are manifested in premature closure of the arterial duct and a pronounced increase in pulmonary arterial pressure [59, 71].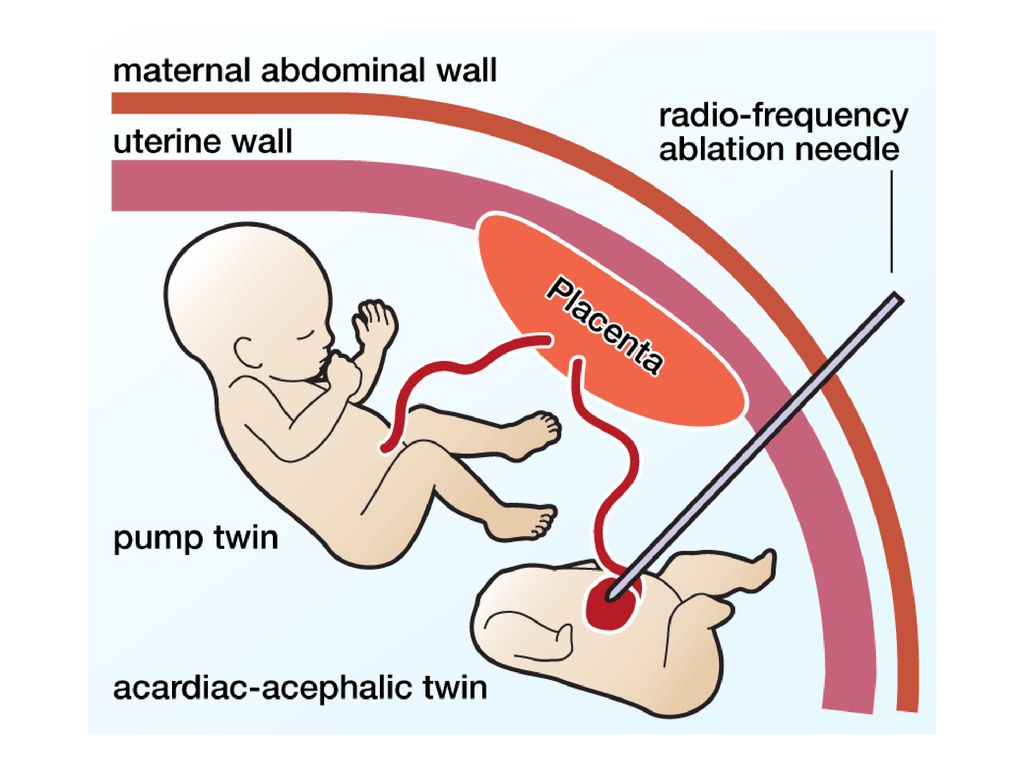
Progesterone, although not a tocolytic in the true sense of the word, is increasingly being used in the protocols of tocolytic therapy for preterm birth. There is no effective way to prevent preterm birth during twin pregnancy. At the same time, three large randomized trials have demonstrated that progesterone is effective in preventing preterm birth in high-risk singleton pregnancies. In recent years, the main (primarily immune) mechanisms for the implementation by gestagens of their protective function in relation to the fetus have been revealed [19, 35, 40, 74].
In patients belonging to the high-risk group (history of preterm birth or shortening of the cervix), the use of progesterone in the prenatal period led to a decrease in the frequency of early termination of pregnancy by 35% [28, 30, 52, 53, 63, 68].
It is noteworthy that the reduction in the incidence of preterm birth with the use of progesterone is not accompanied by a significant improvement in neonatal outcomes and a decrease in perinatal mortality. However, antenatal use of progesterone in singleton pregnancies has been found to be associated with a reduced risk of neonatal sepsis. nine0003
However, antenatal use of progesterone in singleton pregnancies has been found to be associated with a reduced risk of neonatal sepsis. nine0003
British experts conducted a study to evaluate the value of progesterone in the prevention of preterm birth in twins (STOPPIT - STudy Of Progesterone for the Prevention of Preterm Birth In Twins). It was concluded that the use of progesterone in twins does not reduce the incidence of preterm birth or intrauterine fetal death up to 34 weeks. pregnancy [21]. Perhaps this is due to the insufficient dosage of progesterone preparations [3].
Differences in the biological effectiveness of progesterone in multiple and singleton pregnancies should be the subject of further research. According to the authors, such differences are associated with the predominance in the pathogenesis of preterm labor with twin overstretching of muscle fibers, while in singleton pregnancy, infectious and inflammatory processes play the main role [58]. nine0003
When prescribing progesterone preparations, the informed consent of the woman is required, since the manufacturing companies, when registering these medicines in the Russian Federation, in the indications for the use of progesterone do not indicate threatening preterm labor and the possibility of using the drugs in the second and third trimesters of pregnancy.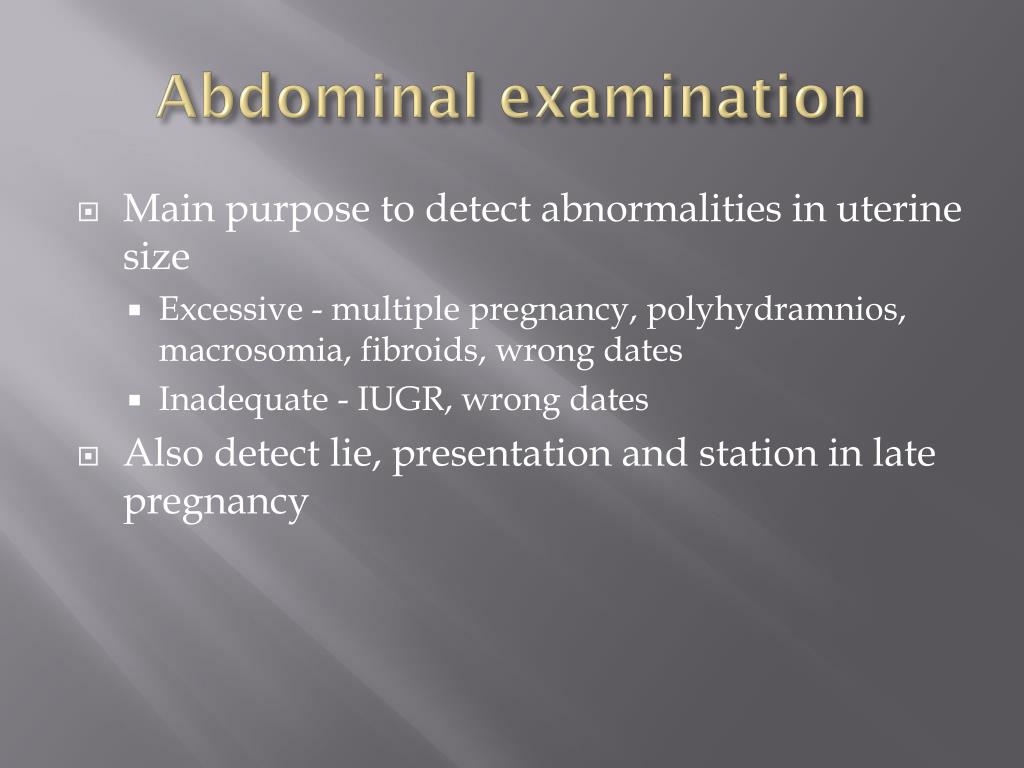
In recent years, in Russia, the most common and frequently used drug from the group of β-mimetic agents is hexoprenaline, a selective β2-sympathomimetic that relaxes the muscles of the uterus. However, according to the results of systematic reviews of randomized controlled trials, the effect of tocolytics alone on reducing the incidence of preterm birth has not been proven. The main goal of prescribing tocolysis is to delay delivery by 48 hours in order to transport the pregnant woman to the perinatal center and conduct a full course of antenatal steroids [31, 43, 56, 73]. nine0003
Risk of preterm birth: diagnostic criteria
Diagnosis of preterm labor is associated with certain difficulties, since there are no specific symptoms. The diagnosis of the onset of preterm labor can be clarified using transvaginal ultrasound with the measurement of the length of the cervix or the determination of fetal fibronectin in the cervico-vaginal secret [1, 70].
In 2010, Conde-Agudelo et al. summarized the available data on the accuracy of predicting spontaneous preterm birth in twins by measuring the length of the cervix. They conducted a systematic review and meta-analysis of 21 non-randomized studies (16 studies of pregnant women with clinical signs of possible preterm birth and 5 studies of pregnant women without symptoms of threatened miscarriage, a total of 3523 women). It was concluded that vaginal echocervicometry is a good diagnostic criterion for spontaneous preterm birth in the absence of clinical symptoms in pregnant women with twins at 20–24 weeks of gestation. [26]. nine0003
summarized the available data on the accuracy of predicting spontaneous preterm birth in twins by measuring the length of the cervix. They conducted a systematic review and meta-analysis of 21 non-randomized studies (16 studies of pregnant women with clinical signs of possible preterm birth and 5 studies of pregnant women without symptoms of threatened miscarriage, a total of 3523 women). It was concluded that vaginal echocervicometry is a good diagnostic criterion for spontaneous preterm birth in the absence of clinical symptoms in pregnant women with twins at 20–24 weeks of gestation. [26]. nine0003
In twin pregnancy, suturing the shortened cervix increases the risk of preterm birth [17].
At the same time, a number of authors describe the positive experience of applying U-shaped and circular sutures, which contribute to the prolongation of pregnancy until the birth of viable children with twins, triplets and even quadruplets [42].
In order to determine the risk of preterm birth, available express test systems are used to determine phosphorylated protein-1 that binds insulin-like growth factor (PSIFR-1) in cervical secretion [12]. These methods increase diagnostic accuracy and reduce the risk of iatrogenic complications, as they prevent overdiagnosis of preterm labor. nine0003
These methods increase diagnostic accuracy and reduce the risk of iatrogenic complications, as they prevent overdiagnosis of preterm labor. nine0003
Two indicators are important for the diagnosis of active preterm labor: regular contractions and dynamic changes in the cervix. The degree of cervical dilation is an indicator of the prognosis of the effectiveness of tocolysis. If the opening of the pharynx is more than 3 cm, tocolysis is likely to be ineffective. Changes in the cervix are a more objective indicator than the assessment of labor activity. With a cervical length of more than 3 cm, the probability of labor onset within the next week is about 1%, which does not require hospitalization of the patient [48]. nine0003
The algorithm of actions of a doctor in case of a threat of preterm birth depends on the clinical picture, gestational age, integrity of the membranes and consists of the following main areas: risk assessment of preterm birth, prevention of RDS of the newborn, prolongation of pregnancy to transfer the mother to the perinatal center, prevention and treatment of infectious complications, in including with premature rupture of the membranes.
At present, the most accurate marker of preterm labor should be considered the detection of fibronectin in the cervico-vaginal secretion at gestational age up to 35 weeks, which indicates an increased risk of preterm labor, especially within 2 weeks. since the test. It is very important for clinical practice that this test has a high predictive value of a negative result - in the absence of fibronectin in the vaginal secretion, the probability that a woman will give birth within 1 week is about 1% [37]. nine0003
Prescription of antenatal steroids significantly reduces morbidity and mortality in children from RDS, IVH, NEC, and patent ductus arteriosus.
Roberts et al. in a recent meta-analysis of 21 randomized trials, a single antenatal course of steroids (24 mg betamethasone or 24 mg dexamethasone over 48 hours) significantly reduced neonatal mortality by 31%, RDS by 34%, and early sepsis within the first 48 hours life - by 44% and the need for artificial lung ventilation - by 20%. A repeated antenatal course of corticosteroids may be useful in the case when more than 7 days have passed from the previous course and symptoms of threatened preterm labor continue or reappear. nine0003
A repeated antenatal course of corticosteroids may be useful in the case when more than 7 days have passed from the previous course and symptoms of threatened preterm labor continue or reappear. nine0003
Laswell et al. in 2010, conducted a meta-analysis of 41 publications that examined neonatal mortality among infants weighing <1500 g or <32 weeks gestation in perinatal centers compared with infants born in lower-level medical facilities. The results of the meta-analysis showed that timely transportation of a pregnant woman with a high risk of preterm birth to a perinatal center is an event that significantly increases the chances of survival of a premature baby. nine0003
Antibiotic therapy for premature rupture of membranes
The effect of prescribing antibiotics in reducing the incidence of chorioamnionitis and neonatal morbidity in cases of premature rupture of membranes has been confirmed in qualitative studies.
A systematic review of 22 randomized controlled trials showed that the use of antibiotics for preterm rupture of membranes and preterm pregnancy significantly reduces the incidence of chorioamnionitis and the number of children born within 48 hours after rupture of the membranes. In addition, the use of antibiotics in this clinical situation can reduce the incidence of neonatal infection, the need for surfactants, the use of oxygen therapy in the newborn, and the incidence of pathological symptoms in neurosonography. nine0003
In addition, the use of antibiotics in this clinical situation can reduce the incidence of neonatal infection, the need for surfactants, the use of oxygen therapy in the newborn, and the incidence of pathological symptoms in neurosonography. nine0003
All of the above suggests that those carrying multiple pregnancies are a special contingent that needs careful monitoring at all stages of pregnancy.
It is necessary to say a few words about childbirth. Undoubtedly, this group of pregnant women represents women whose caesarean section rate is much higher than in the population [13].
According to MONIIAG, in spontaneous multiple pregnancies, the percentage of spontaneous births and caesarean sections is 46.4 and 44.9, respectively.%. Delivery operations used at the birth of the second fetus account for 8.7%. Nevertheless, we do not deny the possibility of conducting childbirth through the natural birth canal. It should be noted that the course of the second stage of labor with twins is often unpredictable and uncontrollable, and much is determined by the skill of the obstetrician-gynecologist.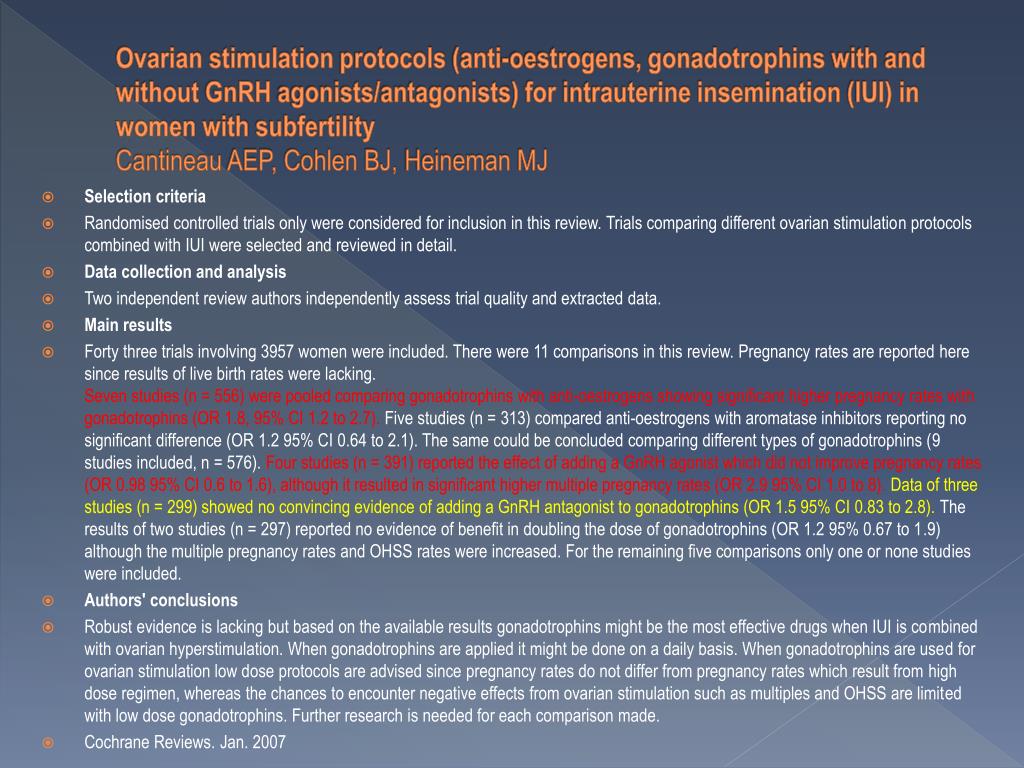 If the doctor has the necessary skill, then both the application of a vacuum extractor to the head of the second fetus and the extraction of the second fetus by the pelvic end will be common obstetric operations that do not affect the child's condition at birth and during the period of neonatal adaptation. nine0003
If the doctor has the necessary skill, then both the application of a vacuum extractor to the head of the second fetus and the extraction of the second fetus by the pelvic end will be common obstetric operations that do not affect the child's condition at birth and during the period of neonatal adaptation. nine0003
As for multiple pregnancies that occurred as a result of IVF, in many obstetric institutions, planned abdominal delivery is carried out. Under the conditions of MORIAG, 30% of pregnant women with multiple pregnancies resulting from IVF were delivered through the natural birth canal.
It should be emphasized that in general there can be no standards in obstetrics, and clinical success is possible only with an individual, balanced and thoughtful medical approach. nine0003
Thus, patients with multiple pregnancies constitute a high-risk group for the development of maternal and perinatal complications. This is directly related to the fact that, evolutionarily, the body of a pregnant woman is adapted for bearing one fetus.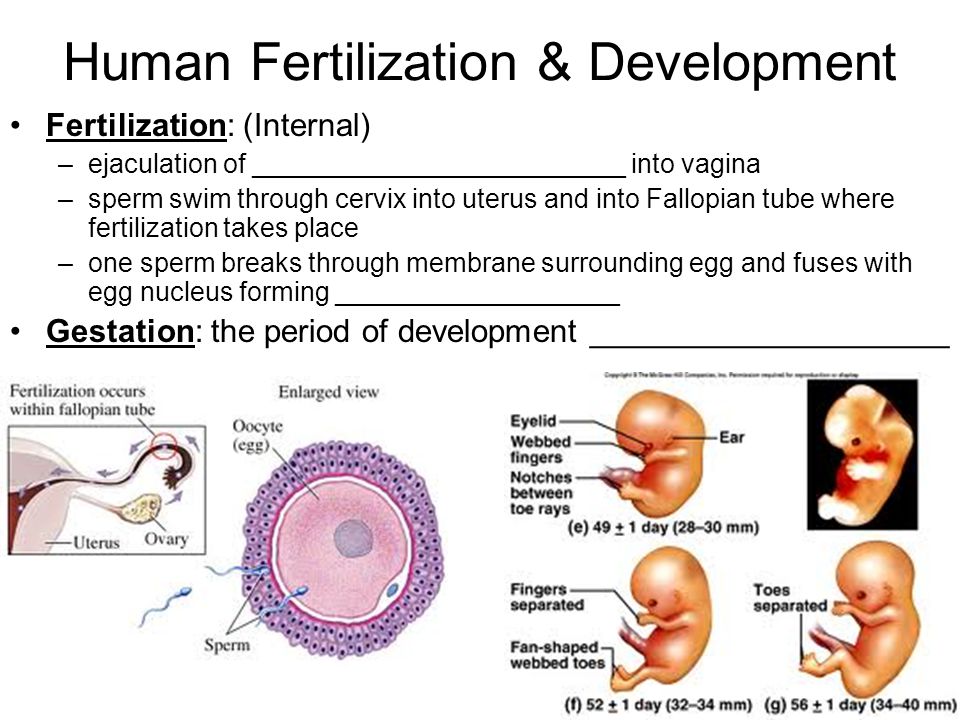
The key to the success of carrying multiple pregnancies and nursing newborns should be continuity in the activities of all obstetric and gynecological departments and departments of newborns. And, of course, further in-depth study of this problem should be aimed at reducing perinatal losses and maintaining the reproductive health of women. nine0003
Literature
Multiple pregnancy: modern aspects - Extempore
In recent years, the frequency of multiple pregnancies has increased, which is associated with the use of assisted reproductive technologies, and this entails the occurrence of many complications both on the part of the mother and newborns, requiring careful monitoring, timely treatment and delivery. One of the main tasks of the Perinatal Center is to provide assistance in case of premature birth, which often occurs in multiple pregnancies. nine0126
The birth of twins is a miracle! From the point of view of emotions, this is, of course, understandable: a double joy - it is unusual to become parents of two absolutely identical babies at once. But no matter how cute children look, walking in a double, triple stroller in the same overalls and similar to each other like two drops of water, from the point of view of a specialist, multiple pregnancy is a high risk factor for the occurrence of perinatal and maternal pathology. This is due, first of all, to a large number of complications, features of the development of the fetus, increased requirements for the mother's body. That is why, despite many years of studying this issue, it still remains relevant not only in the medical, but also in the socio-economic aspect. And the lack of clearly formulated recommendations, protocols and orders approved by the Ministry of Health, regulating the tactics of managing women with multiple pregnancies, prompts us to highlight the main points of multiple pregnancy from conception to birth. nine0003
But no matter how cute children look, walking in a double, triple stroller in the same overalls and similar to each other like two drops of water, from the point of view of a specialist, multiple pregnancy is a high risk factor for the occurrence of perinatal and maternal pathology. This is due, first of all, to a large number of complications, features of the development of the fetus, increased requirements for the mother's body. That is why, despite many years of studying this issue, it still remains relevant not only in the medical, but also in the socio-economic aspect. And the lack of clearly formulated recommendations, protocols and orders approved by the Ministry of Health, regulating the tactics of managing women with multiple pregnancies, prompts us to highlight the main points of multiple pregnancy from conception to birth. nine0003
Only in the last few years the frequency of multiple pregnancies has increased significantly, and in most European countries it ranges from 0. 7 to 1.5%. Over the past year, 144 cases of such births have been registered in the Kyiv Perinatal Center, of which 139 (96.5%) are twins and 5 (3.5%) are triplets.
7 to 1.5%. Over the past year, 144 cases of such births have been registered in the Kyiv Perinatal Center, of which 139 (96.5%) are twins and 5 (3.5%) are triplets.
The frequency of multiple pregnancy can be determined (according to Heilin) as follows: twins occur once in 80 births, triplets - once in 80 2 , and in 80 3 - one quarter, etc.
The widespread introduction of assisted reproductive technologies has led to a change in the ratio of spontaneous and induced multiple pregnancy: 70% and 30% in the 80s versus 50% and 50% in the late 90s, respectively.
Historical aspects
Since ancient times, the birth of twins has been the subject of myths and legends. The twins were credited with supernatural abilities, they were considered either the culprits of misfortune, or the harbingers of future events. People have always been struck by the resemblance of twins. In cases where their external features were opposite, it was believed that one of them personifies good, and the other - evil.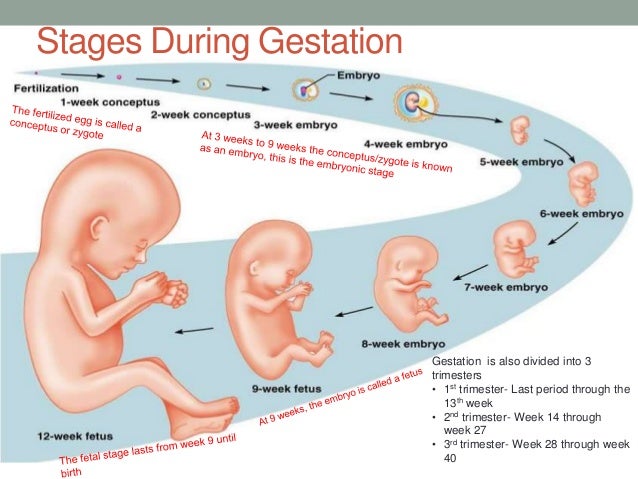 nine0003
nine0003
Twins are known from Greek mythology: Apollo (god of art) and Artemis (goddess of hunting), the twins of Diocura are patrons of seafarers. The twins Romulus and Remus are immortalized in the city coat of arms of Rome.
Since ancient times, twins were treated differently: for example, the Peruvians, the inhabitants of the Congo and the natives of North America - with demonic fear. Among the ancient Hindus, Assyrians, Babylonians and Egyptians, the birth of twins was considered as a consequence of adultery, and in Europe until the Middle Ages, mothers of twins were accused of cohabitation with the devil and burned at the stake with their children (W. Friedrich, 1985).
For many centuries, scientists around the world have tried to understand and study the processes that cause the appearance of twins. Back in the 5th century BC. e. the famous philosophers Empedocles and Democritus, and later Hippocrates, explained the birth of two or more children at once by “an excess of semen” - a substance from which, according to their ideas, an embryo is formed. The ideas of Aristotle looked more scientific, who noted the connection between multiple pregnancy in chickens and various anomalies and said that there is an analogy between the occurrence of congenital deformities and the birth of twins. nine0003
The ideas of Aristotle looked more scientific, who noted the connection between multiple pregnancy in chickens and various anomalies and said that there is an analogy between the occurrence of congenital deformities and the birth of twins. nine0003
In the 18th century, interest in various anomalies and deformities increased significantly. The Russian embryologist K.M. Baer believed that the appearance of conjoined twins was the result of the splitting of one embryo. Other scientists believed that in such cases two embryos merge with identical parts: a head with a head, a spine with a spine, etc. This made it possible to express the idea of the existence of not one, but two types of twins. nine0003
Origin of twins
Multiple pregnancy in humans can be represented as two biological phenomena - monozygotic (identical, homologous, identical) and dizygotic twins (fraternal, heterologous).
Dizygotic twins are more common (66–75% of all twins). The birth rate varies from 4 to 50 per 1000 births. Dizygotic twins occur when two separate eggs are fertilized. The maturation of two or more eggs can occur both in one ovary and in two. These twins can be either of the same or opposite sex, and are in the same genetic relationship as siblings. nine0003
The birth rate varies from 4 to 50 per 1000 births. Dizygotic twins occur when two separate eggs are fertilized. The maturation of two or more eggs can occur both in one ovary and in two. These twins can be either of the same or opposite sex, and are in the same genetic relationship as siblings. nine0003
They are always characterized by a dichorionic, diamniotic type of placentation. In this case, there will always be two autonomous placentas that can touch, forming, as it were, one placenta, but they can be separated. The two fetuses are separated by two chorionic and two amniotic membranes. One of the main reasons for the formation of dizygotic twins is a powerful hormonal stimulation of the ovaries. A high level of FSH can cause multiple follicles in one or both ovaries to mature and ovulate at the same time, or the formation of two eggs in one follicle. Most often, two eggs come from one follicle. nine0003
It is also possible that activation of hypothalamic releasing factors leads to stimulation of the pituitary gland and further poliovulation. It is possible that as a result of different sensitivity of the receptors of the anterior pituitary gland, the level of FSH can vary widely, sometimes leading to poliovulation. A similar pattern of poliovulation against the background of an elevated level of FSH can also develop during stimulation (hyperstimulation), ovulation with clomiphene citrate, clostilbegit, chorionic gonadotropin. nine0003
It is possible that as a result of different sensitivity of the receptors of the anterior pituitary gland, the level of FSH can vary widely, sometimes leading to poliovulation. A similar pattern of poliovulation against the background of an elevated level of FSH can also develop during stimulation (hyperstimulation), ovulation with clomiphene citrate, clostilbegit, chorionic gonadotropin. nine0003
A certain relationship was noted between a number of factors and the incidence of dizygotic twins. Thus, among women with multiple pregnancies, patients aged 35 to 40 years are more common. Among these women predominate re-pregnant, with a relatively large body weight and height. Those women who have already had dizygotic twins are more likely to have it again. Most likely, the predisposition to the development of dizygotic twins can be inherited through the maternal line in a recessive manner. If there is a history of monozygotic twins, the chance of its recurrence in the same woman is no greater than in the general population. nine0003
nine0003
There is a higher frequency of twins with anomalies in the development of the uterus (bicornuate uterus, septum in the uterus). With a bifurcation of the uterus, more often than with its normal structure, two or more eggs mature simultaneously, which can be fertilized.
Assisted reproductive technologies have had a direct impact on the increase in the frequency of dizygotic twins, which is a consequence of the stimulation of FSH and LH used, which in turn leads to multiple ovulation. It is assumed that almost all induced pregnancies are multizygous. This is due to the fact that as a result of stimulation, ovulation of several follicles occurs immediately. With the simultaneous fertilization of several eggs, some of them can split, and this forms a "mixture" of dizygotic and monozygotic twins. nine0003
Theoretically, there is a possibility of fertilization of two eggs of different ovulation periods, with the onset of a new pregnancy in the presence of an earlier one, since another ovulation may occur in this case.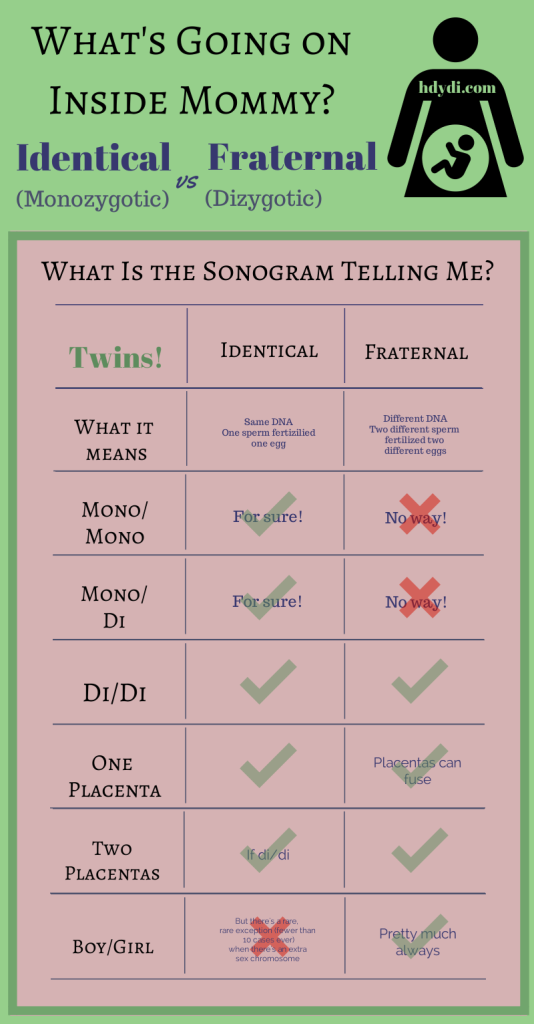
Monozygotic twins are formed as a result of the separation of one fetal egg at various stages of its development and make up 1/3 of all twins. Unlike dizygotic twins, their prevalence rate is constant and is 3-5 per 1000 births. In contrast to the dizygotic variant, the prevalence of monozygotic twins does not depend on ethnicity, maternal age, parity of pregnancy and childbirth. nine0003
It is believed that division of a fertilized egg may occur as a result of implantation delay and oxygen deficiency. This theory also makes it possible to explain the higher frequency of developmental anomalies among monozygotic twins compared to dizygotic twins. The implantation delay process has also been confirmed in animal experiments.
It is possible that the cause of polyembryony may be mechanical separation of blastomeres (in the early stages of crushing), resulting from cooling, violation of the acidity and ionic composition of the medium, exposure to toxic and other factors. nine0003
nine0003
The occurrence of monozygotic twins is also associated with the fertilization of an egg that had two or more nuclei. Each nucleus connects with the nuclear substance of the sperm, resulting in the formation of germinal rudiments. Oocytes with three nuclei have also been described. In the process of development of the fetal egg, the chorion is first laid, then the amnion and, in fact, the embryo. Therefore, the nature of placentation in the formation of monozygotic twins depends on the stage of development of the fetal egg, at which its division occurred. nine0003
If the separation of the fetal egg occurs during the first 3 days after fertilization, that is, before the formation of the inner layer of cells - the embryoblast (at the blastocyst stage) and the transformation of the outer layer of blastocyst cells into a trophoblast, then monozygotic twins have two chorions and two amnions. In this case, monozygotic twins will be diamniotic and dichorionic. This variant occurs in 20-30% of all monozygotic twins. If the division of the fetal egg occurs between 4–8 days after fertilization at the blastocyst stage, when the formation of the embryoblast is completed and the chorion is laid from the outer layer, but before the laying of the amniotic cells, then two embryos will form, each in a separate amniotic sac. The two amniotic sacs will be surrounded by a common chorionic membrane. Such monozygotic twins will be diamniotic and monochorionic. Most monozygotic twins (70-80%) are represented by this type. If division occurs by 9-10th day after fertilization, by the time the amnion formation is completed, two embryos with a common amniotic sac are formed. Such monozygotic twins will be monoamniotic and monochorionic. Among monozygotic twins, this is the rarest type, occurring in approximately 1% of all monozygotic twins and representing the highest risk in terms of pregnancy. If the egg is separated at a later date on the 13-15th day after conception (after the formation of the embryonic disk), the separation will be incomplete, which will lead to incomplete splitting (fusion) of the twins.
If the division of the fetal egg occurs between 4–8 days after fertilization at the blastocyst stage, when the formation of the embryoblast is completed and the chorion is laid from the outer layer, but before the laying of the amniotic cells, then two embryos will form, each in a separate amniotic sac. The two amniotic sacs will be surrounded by a common chorionic membrane. Such monozygotic twins will be diamniotic and monochorionic. Most monozygotic twins (70-80%) are represented by this type. If division occurs by 9-10th day after fertilization, by the time the amnion formation is completed, two embryos with a common amniotic sac are formed. Such monozygotic twins will be monoamniotic and monochorionic. Among monozygotic twins, this is the rarest type, occurring in approximately 1% of all monozygotic twins and representing the highest risk in terms of pregnancy. If the egg is separated at a later date on the 13-15th day after conception (after the formation of the embryonic disk), the separation will be incomplete, which will lead to incomplete splitting (fusion) of the twins. This type is quite rare. nine0003
This type is quite rare. nine0003
The origin of triplets, quadruplets and more twins varies. So, triplets can be formed from three separate eggs, from two or one egg. They can be monozygotic and heterozygous. Quadruples can also be monozygotic and fraternal (the most common are double twins and triplets with one single fetus).
All this dictates the need for early diagnosis, detection of multiple pregnancy in women, an adequate assessment of the development of the fetus and the condition of the mother, as well as preventive measures aimed at preventing the adverse outcome of multiple pregnancy. nine0003
Diagnosis of multiple pregnancy
The issue of multiple pregnancy diagnosis is extremely relevant and requires detailed study. Early and full-fledged diagnosis of multiple pregnancies, careful monitoring of the antenatal clinic doctor in the future determine the adequate tactics of pregnancy and childbirth.
As for the frequency of visits to pregnant women's clinics, it is regulated by the current order of the Ministry of Health of Ukraine dated July 15, 2011 No.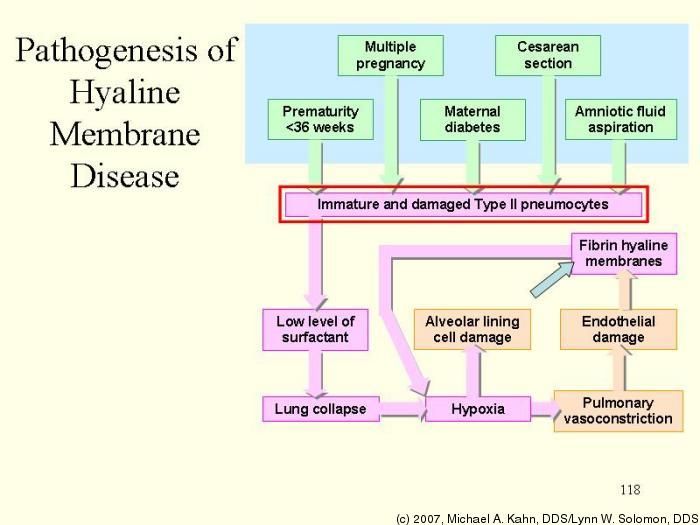 417 and averages 8–9once. However, it should be noted that the frequency of visits in case of detection of twins, especially in women with extragenital or obstetric pathology, can be extended to 11–12 visits. If there are any deviations from the normal course of pregnancy, the schedule for visiting the LCD is determined strictly individually, depending on the situation. Unfortunately, today the number of visits to the LCD by women with multiple pregnancies is much less than indicated in these recommendations, and therefore the number of complications increases. The reason for the low attendance of HCs is to a large extent related to the lack of sufficient information support for women who are ready to become mothers, especially in the case of multiple pregnancies. nine0003
417 and averages 8–9once. However, it should be noted that the frequency of visits in case of detection of twins, especially in women with extragenital or obstetric pathology, can be extended to 11–12 visits. If there are any deviations from the normal course of pregnancy, the schedule for visiting the LCD is determined strictly individually, depending on the situation. Unfortunately, today the number of visits to the LCD by women with multiple pregnancies is much less than indicated in these recommendations, and therefore the number of complications increases. The reason for the low attendance of HCs is to a large extent related to the lack of sufficient information support for women who are ready to become mothers, especially in the case of multiple pregnancies. nine0003
The first acquaintance of a woman with a doctor begins with the clarification of complaints and a thorough history taking. First of all, you should find out from the pregnant woman if she or her close relatives on the side of her father and mother have indications of multiple pregnancies, if there are such prerequisites, then the possibility of developing a multiple pregnancy should be borne in mind. You should also find out if ovulation stimulation was performed the day before, or if assisted reproductive technologies were used.
You should also find out if ovulation stimulation was performed the day before, or if assisted reproductive technologies were used.
With regard to clinical studies, one of the early objective signs of multiple pregnancy is an increase in the size of the uterus and its mismatch with the gestational age. In the second trimester of pregnancy, a “jump” symptom occurs (especially a rapid increase in the uterus). The circumference of the abdomen also exceeds its dimensions characteristic of this period of pregnancy, and by the end of pregnancy it is more than 100 cm. Although this issue is quite controversial, in our practice there were cases when the circumference of the abdomen of a pregnant woman with multiple pregnancies did not exceed 94 see
Obstetric examination is characterized by the determination in the uterus of three or more large parts of the fetus (two heads and one pelvic end or two pelvic ends and one head). An important diagnostic sign in recognizing multiple pregnancies is the low location of the presenting part in relation to the entrance to the small pelvis. This sign is observed in 92.5% of women with multiple pregnancies. Another feature is listening to the fetal heartbeat at two different points with a "zone of silence" between them. nine0003
This sign is observed in 92.5% of women with multiple pregnancies. Another feature is listening to the fetal heartbeat at two different points with a "zone of silence" between them. nine0003
The most reliable method for diagnosing multiple pregnancy is an echographic examination, the accuracy of which is 99.3%. With the help of ultrasound, we not only carry out early diagnosis of multiple pregnancy, but also determine:
- Position and presentation of fetuses, the nature of their development.
- Location, structure and number of placentas.
- Number of amniotic cavities.
- The volume of amniotic fluid. nine0218
- Congenital malformations and antenatal fetal death.
- The state of the fetus from a functional point of view.
- Character of BMD and FPC by Doppler.
According to the latest Cochrane Library guidelines, ultrasound should be performed in all women in early pregnancy, optimally at 10-13 weeks of gestation, when vital signs, chorionicity, and neck wrinkle thickness can be determined.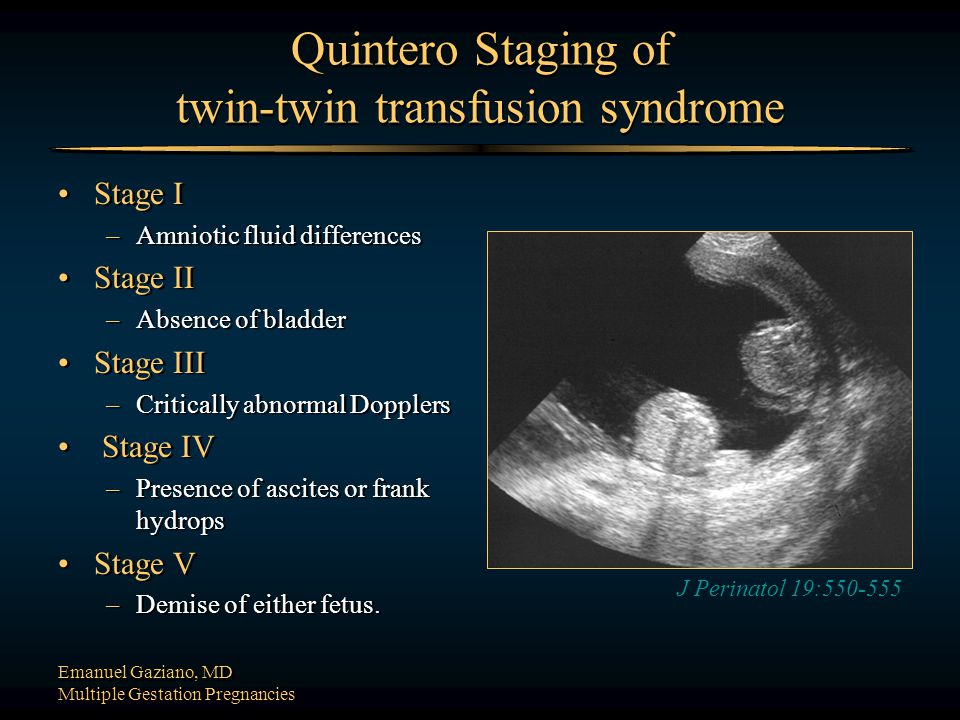 When diagnosing a multiple pregnancy, every effort must be made to determine the chorionicity. It is chorionality that determines the course of pregnancy, its outcome, perinatal morbidity and mortality. According to the latest world studies, monochorionic twins, compared with dichorionic twins, are accompanied by a significantly higher risk of perinatal mortality, intrauterine fetal death, discordant fetal development, and necrotizing enterocolitis in newborns. nine0003
When diagnosing a multiple pregnancy, every effort must be made to determine the chorionicity. It is chorionality that determines the course of pregnancy, its outcome, perinatal morbidity and mortality. According to the latest world studies, monochorionic twins, compared with dichorionic twins, are accompanied by a significantly higher risk of perinatal mortality, intrauterine fetal death, discordant fetal development, and necrotizing enterocolitis in newborns. nine0003
The presence of specific ultrasound criteria - T- or λ-signs, which are formed near the base of the interfetal septum, with a high degree of certainty, allows the diagnosis of mono- or dichorionic twins. The determination of the λ-sign on ultrasound at any stage of pregnancy indicates a dichorionic type of placentation, the T-sign indicates monochorionicity. In addition to specific ultrasound criteria, there are generally accepted criteria for differentiating monochorionic twins from dichorionic twins. Monochorionic twins are characterized by the presence of one placenta, both fetuses will be of the same sex, and the thickness of their interamniotic membrane is <2 mm (2 layers, both amniotic).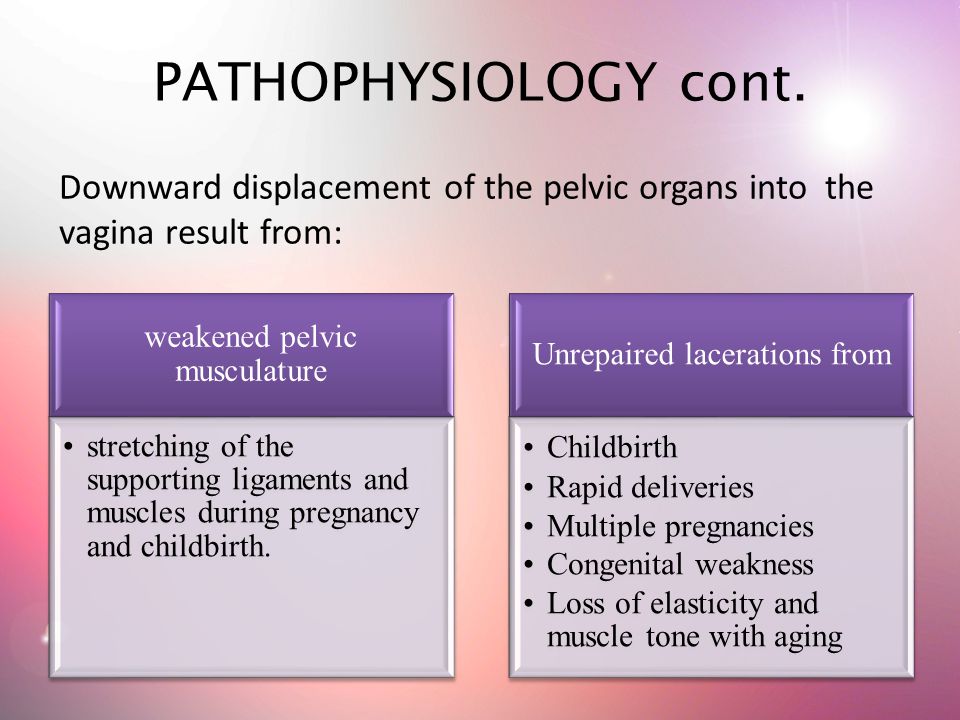 Dichorionic twins are characterized by two or one placenta, their fetuses can be same-sex or opposite-sex, and the thickness of the interamniotic membrane is > 2 mm (4 layers: 2 amniotic and 2 chorionic). A follow-up ultrasound is performed at 18–21 weeks of gestation to detect structural abnormalities in the fetus. nine0003
Dichorionic twins are characterized by two or one placenta, their fetuses can be same-sex or opposite-sex, and the thickness of the interamniotic membrane is > 2 mm (4 layers: 2 amniotic and 2 chorionic). A follow-up ultrasound is performed at 18–21 weeks of gestation to detect structural abnormalities in the fetus. nine0003
Given the high perinatal morbidity and mortality in multiple pregnancies, it is advisable to supplement the ultrasound examination with a functional ultrasound assessment of the twins, including the study of the respiratory movements of the fetuses, their motor activity and tone. Important is the Doppler assessment of BMD and FPC.
In multiple pregnancy, as a rule, lower values of peripheral vascular resistance indices in the uterine arteries are noted, which is probably an adaptive reaction of the pregnant woman's body. nine0003
Doppler examination of blood flow in the umbilical arteries confirms dissociated fetal development. In the presence of IGR of one of the fetuses, an increase in the values of peripheral vascular resistance indices in the arteries of its umbilical cord is detected. Doppler examination of FPC also makes it possible to clarify the diagnosis of transfusion syndrome.
Doppler examination of FPC also makes it possible to clarify the diagnosis of transfusion syndrome.
Early diagnosis of multiple pregnancies helps to optimize the management of pregnancy and childbirth, has an impact on the incidence of perinatal morbidity and mortality of twins. nine0003
What should be avoided during multiple pregnancy?
Multiple pregnancy makes increased demands on a woman's body, forcing all organs and systems to function with great stress. In this regard, various complications are much more common. The most common complications at the Perinatal Center in Kyiv include the following:
- Preterm birth - 75 (52%).
- Threatened miscarriage - 136 (94.5%).
- Pre-eclampsia (mild - 56 (82.3%), moderate - 7 (10.3%) and severe - 5 (7.4%)). A total of 68 (47%).
- Premature rupture of membranes - 63 (43.7%).
- Anemia (mild - 74 (72.5%), moderate - 18 (12.5%) and severe - 10 (7%)).
 In total - 102 (70.8%).
In total - 102 (70.8%). - Birth defects - 5 (3.4%).
- Premature detachment of a normally located placenta - 3 (2%).
- Abnormal amount of amniotic fluid - 38 (26.4%). nine0218
- Postpartum haemorrhage - 3 (2.0%).
There are different opinions about the prevention of the above complications. According to the RCOG, preventive prevention of complications associated with multiple pregnancy is not carried out in most foreign countries. On the territory of our state, preventive measures are still recommended, although not significantly, but still reducing perinatal and maternal losses.
Often, for the prevention of varying degrees of anemia, pregnant women with multiple pregnancies after 12 weeks of gestation are prescribed preventive antianemic therapy, which includes not only iron preparations, but also folic acid for up to 3 months. The use of iron preparations in combination with folic acid significantly reduces the incidence of low hemoglobin levels, and also reduces the need for blood transfusions in the postpartum period.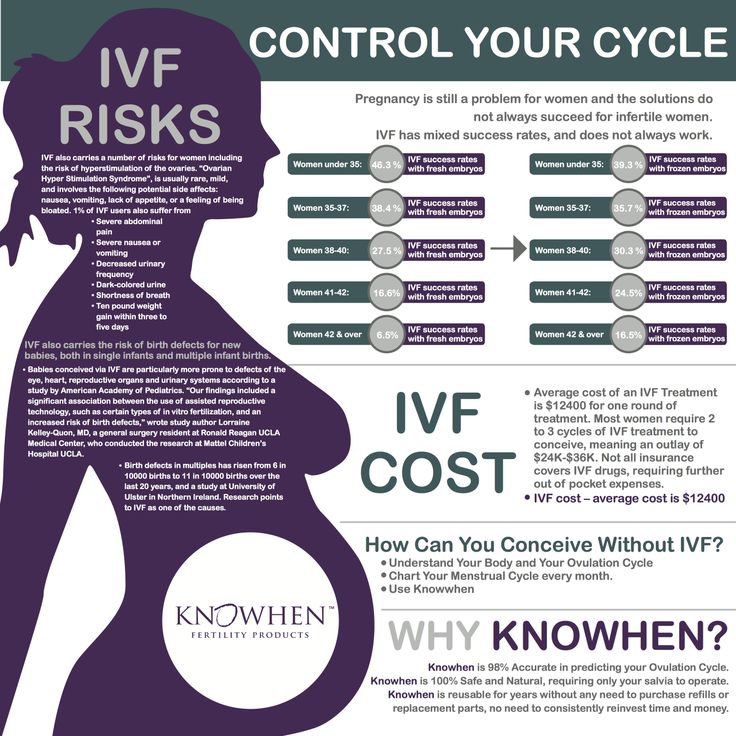 nine0003
nine0003
When preventive measures are taken to prevent preeclampsia, maternal morbidity and mortality are significantly reduced by 20%. For this, Ca preparations (1 g / day) are used starting from 16 weeks of pregnancy, aspirin (50–150 mg / day) after 20 weeks of pregnancy. Of particular importance is the use of aspirin in pregnant women with varicose veins of the lower extremities, heart defects, prosthetic heart valves, etc.
In order to prevent preterm birth in pregnant women with multiple pregnancies, many obstetrician-gynecologists recommend hospitalization, prophylactic administration of tocolytic drugs, a suture on the cervix, teaching pregnant women to monitor uterine contractions. However, most systematic reviews of randomized controlled trials have found that hospitalization of pregnant women with multiple pregnancies increases the likelihood of preterm birth compared to women who were not hospitalized; the use of a prophylactic suture on the cervix 2 times increases the risk of preterm birth; the routine use of tocolytics does not affect the rate of reduction in preterm birth. nine0003
nine0003
Thus, the issue of choosing preventive measures today is quite debatable, requiring detailed study.
What is the tactics of delivery of pregnant women with multiple pregnancies?
The tactics of conducting such childbirth is ambiguous and is determined purely individually. The choice of method of delivery involves an assessment of the possibility of safe vaginal delivery and indications for caesarean section. Before making this difficult choice, the obstetric situation should be assessed globally, taking into account the following factors: fetal position and presentation, estimated weight, chorionicity, fetal condition, maternal pelvic dimensions, maternal condition and obstetric history. nine0003
If the pregnancy is full-term and no abnormalities have been noted, then the course of labor will be determined by the presentation of the first fetus and its estimated weight. If both fetuses are in cephalic presentation, childbirth is carried out through the natural birth canal, and only in case of deviations from the normal course of labor, the management plan is revised in favor of caesarean section.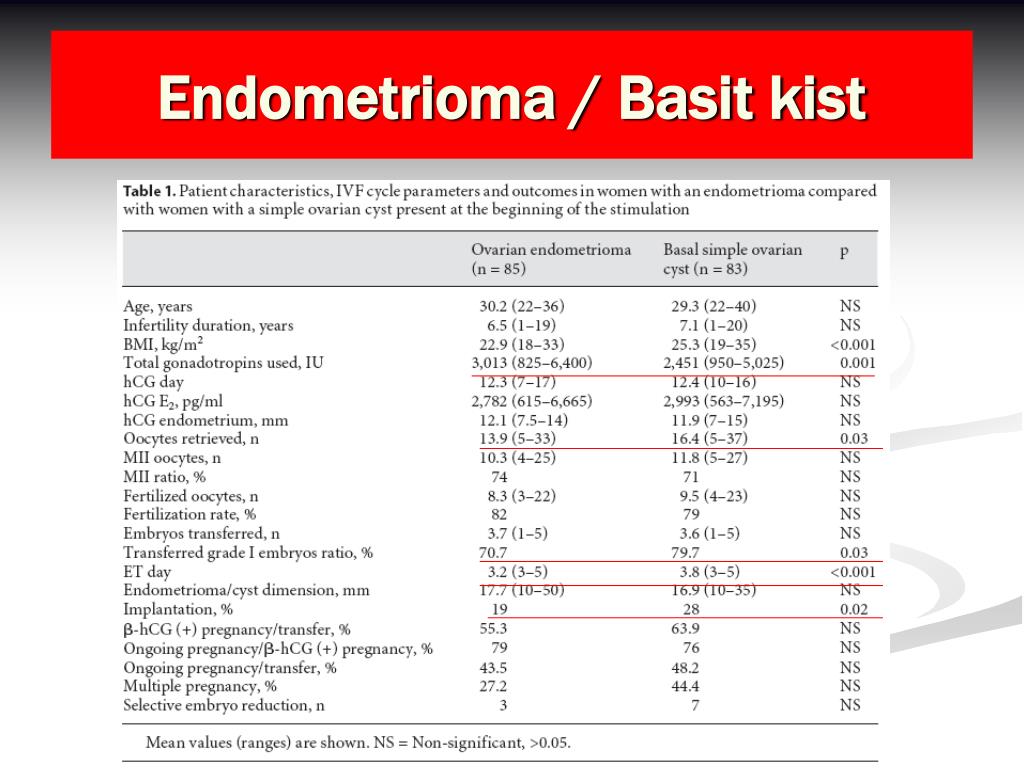
As much as many women would like a caesarean section, this operation has strict indications indicated in Protocol No. 977 dated 12/27/2011. These include:
- Breech presentation or malposition of the first fetus in a multiple pregnancy (D).
- Monoamniotic twins (D) (the best method of delivery is CS surgery at 32 weeks of gestation after RDS prophylaxis in level 3 hospitals).
- Syndrome of growth retardation of one of the fetuses in multiple pregnancy.
- Conjoined twins.
- Other obstetric and extragenital indications. nine0218
According to the statistics of our center, 84 women (58.3%) had a caesarean section for one reason or another, enshrined in existing protocols, and only 60 women (41.7%) had vaginal delivery. In the practice of the Perinatal Center, several births were noted through the natural birth canal in the breech presentation of both fetuses with a favorable outcome for both the mother and newborns.
Scheduled delivery: what is the optimal time? nine0126
According to global guidelines, the optimal gestational age for twins is 36-37 weeks gestation. To date, the recommended delivery time for monochorionic monoamniotic twins is 32 weeks of gestation after a course of corticosteroids, which is primarily due to a significant increase in perinatal losses after 32 weeks of gestation.
Summarizing all of the above, we can conclude that the management of multiple pregnancy requires the highest degree of professionalism and attention from a specialist. Each factor is important, everything must be taken into account - and only then, under the strict supervision of a doctor and with strict adherence to the recommendations, healthy babies are born safely - identical twins and fraternal twins. nine0003
Some of the recommendations for management of multiple pregnancies (according to RCOG, ACOG)
- All women with multiple pregnancies should be offered ultrasound at 10-13 weeks of gestation to assess viability, chorions, major congenital malformations, and nuchal space .

- Women with multiple pregnancies should be asked about the presence of nausea, epigastric pain, and other unusual symptoms of the third trimester, as they are at increased risk of developing HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets), and before symptoms of preeclampsia appeared. nine0218
- The high incidence of gestational diabetes and hypertension warrants screening and monitoring for these complications in multiple pregnancies.
- Women should be informed of the high risk of multiple pregnancies before starting assisted reproductive technology (ART).
- Delivery in multiple pregnancies should most often be scheduled between 36 and 37 weeks' gestation.
- It is reasonable to seek vaginal delivery unless specific clinical indications for caesarean section are identified, such as breech presentation of the 1st fetus or a previous caesarean section. nine0218
- After the death of one of the fetuses in a monochorionic pregnancy, surviving twins have a risk of neurological disorders of the order of 12%.