Iron levels during pregnancy
Low iron in pregnancy: Spot the symptoms of anemia
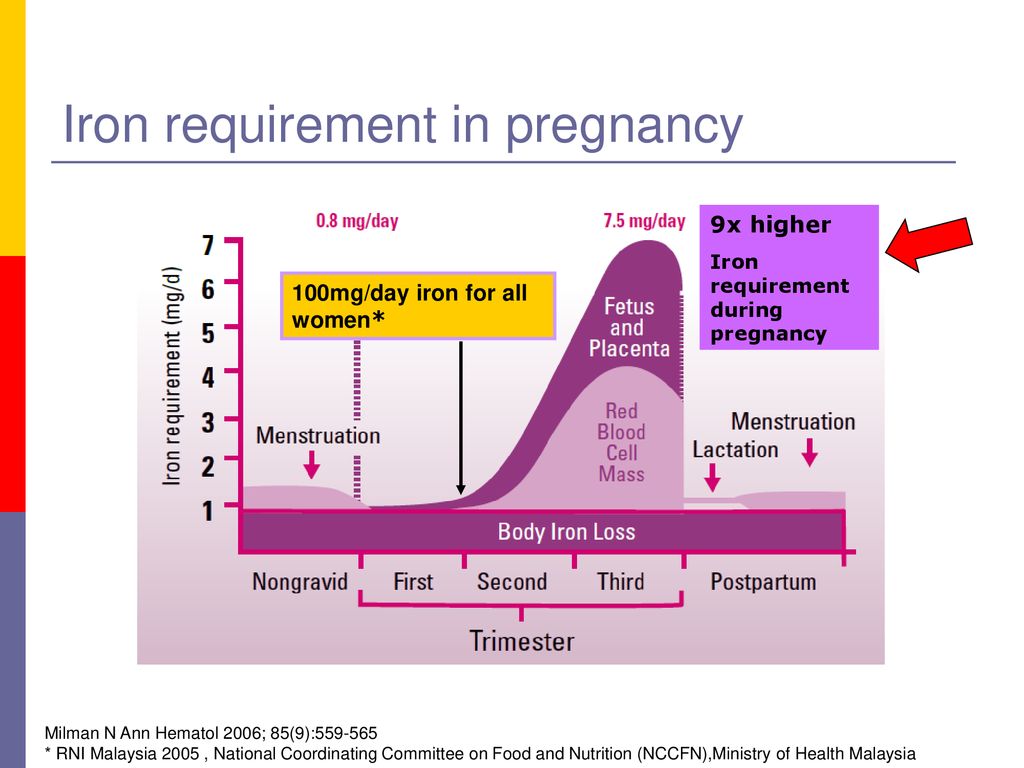
During pregnancy, a woman needs twice the amount of iron that a nonpregnant woman needs.
You need iron to keep yourself healthy and to also support your developing baby. Iron helps your red blood cells deliver oxygen to the baby and to your tissues. Without high iron stores or consuming enough iron during pregnancy, you could develop iron deficiency anemia.
Risks associated with anemia during pregnancy include:
- Premature birth
- Low birth weight baby
- Infection
- Poor healing
- Prenatal and postpartum depression
Maternal anemia can also place the mother at an increased risk of death during and after childbirth. Severe anemia can lead to circulatory decompensation, increased cardiac output, an increased risk of hemorrhage and decreased ability to tolerate blood loss, leading to circulatory shock and death. Infants born of iron-deficient mothers are at high risk for having iron deficiency at birth.
Getting enough iron is important for both you and your baby.
Anemia symptoms in women
Symptoms of anemia include:
- Feeling lightheaded or dizzy
- Feeling weak or tired
- Trouble concentrating
- Constant feeling of being cold
- Shortness of breath
- Rapid heartbeat
- Trouble sleeping
- Headaches
If you experience any of these symptoms, call your doctor right away.
Who is considered anemic?
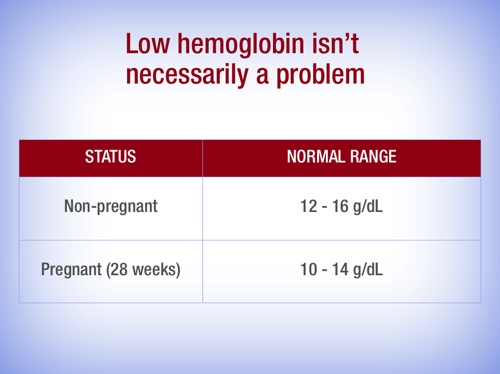
The World Health Organization (WHO) defines anemia in pregnant women as:
- First trimester: hemoglobin less than 11.0 g/dL
- Second trimester: hemoglobin less than 10.5 g/dL
- Third trimester: hemoglobin less than 11.0 g/dL
Pregnant women are routinely screened for anemia at their first prenatal visit and again between 24 and 28 weeks.
For nonpregnant women, hemoglobin lower than 12.0 g/dL is considered anemic according to the WHO.
Iron supplements during pregnancy
Without iron supplementation, iron deficiency anemia occurs in many pregnant women.
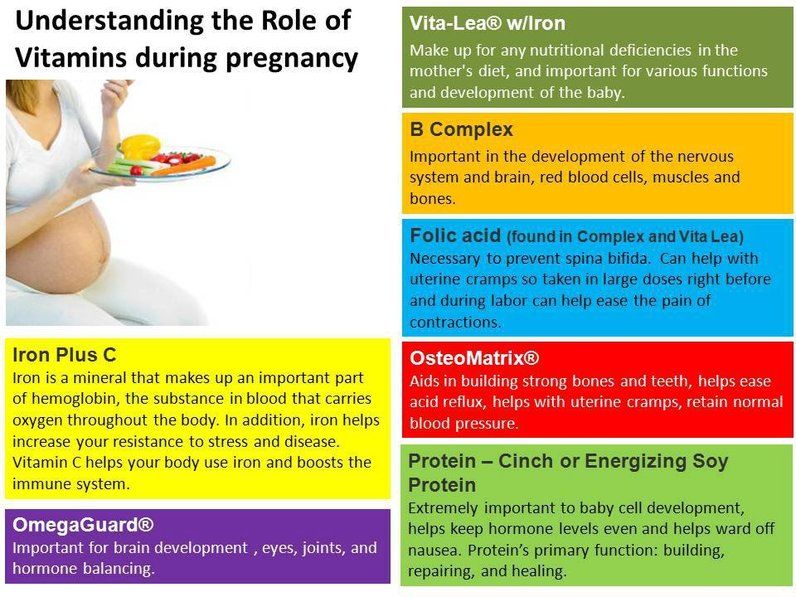
While nonpregnant women only need 18 mg of iron per day, pregnant women require 27 mg of iron daily. This amount is found in most prenatal vitamins. Please keep in mind that most gummy vitamins do not contain iron (as a safety precaution). If taking a gummy prenatal, you will also need an iron supplement. Placing your prenatal vitamin in a designated place such as near your toothbrush or setting an alarm on your phone may help to remind you to take this important vitamin every day.
If anemia is diagnosed, your doctor or midwife will prescribe extra iron for you to take daily. In severe cases, iron can be given intravenously. It takes several weeks, sometimes months to increase iron stores in your body so taking iron routinely as prescribed is important. Continue taking your prenatal vitamin and/or supplemental iron for six to eight weeks after delivery, to increase iron stores due to blood loss after delivery.
Iron-rich foods to eat during pregnancy
In addition to taking a prenatal vitamin with iron, eat a balanced diet that includes iron-rich foods. There are two types of iron in foods: heme and nonheme. Meat, poultry and fish contain heme iron, which is much more easily absorbed by the body than nonheme or plant-based iron.
There are two types of iron in foods: heme and nonheme. Meat, poultry and fish contain heme iron, which is much more easily absorbed by the body than nonheme or plant-based iron.
Sources of meat-based (heme) iron:
- Beef
- Chicken
- Turkey
- Organ meats
- Oysters, clams and mussels
Sources of plant-based (nonheme) iron:
- Beans
- Spinach and other leafy greens
- Potato with skin
- Nuts and seeds
- Dried fruit
- Enriched breads and cereals
Vitamin C can help your body absorb iron. When eating plant (nonheme) sources of iron, include a good source of vitamin C, like fruit or fruit juice. When drinking juice, limit to one 8 ounce glass per day due to the high sugar content.
Sources of vitamin C:
- Oranges
- Grapefruit
- Kiwi
- Broccoli
- Peppers
- Strawberries
- Watermelon
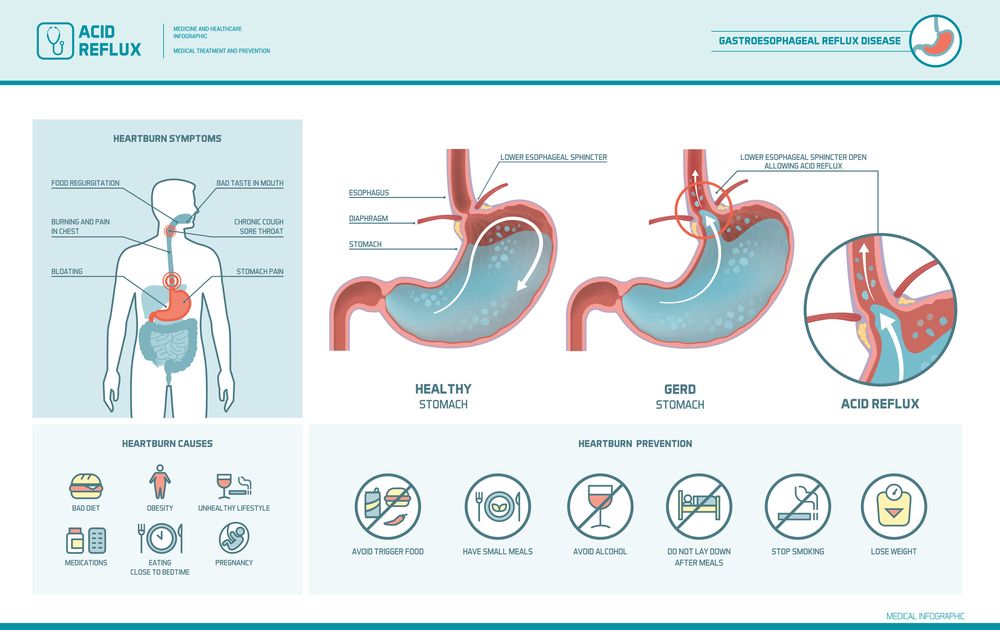
Some foods decrease the body's absorption of iron. Avoid eating high-calcium foods at the same time as iron-rich foods. Calcium is an important nutrient during pregnancy, but calcium and iron compete in the body for absorption. For best results, space your high calcium foods from your high iron foods and prenatal vitamin. Some medications such as antacids and drinking excessive coffee or tea can also reduce the absorption of iron.
Avoid eating high-calcium foods at the same time as iron-rich foods. Calcium is an important nutrient during pregnancy, but calcium and iron compete in the body for absorption. For best results, space your high calcium foods from your high iron foods and prenatal vitamin. Some medications such as antacids and drinking excessive coffee or tea can also reduce the absorption of iron.
Get your pregnancy questions answered
Call 800.922.0000 to schedule an appointment at the Olson Center for Women's Health.
Related stories:
You asked, we answered: What causes premature labor and how can you prevent it?
Preterm birth is currently defined as deliveries between 20 and 37 weeks of gestation. There are two main categories.
Read More
You asked, we answered: Is rib pain during pregnancy normal?
I'm pregnant for the first time and I have pain in the upper left side by my ribs – is this normal?
Read More
Anemia in Pregnancy: Causes, Symptoms, and Treatment
Written by Jen Uscher
In this Article
- Types of Anemia During Pregnancy
- Risk Factors for Anemia in Pregnancy
- Symptoms of Anemia During Pregnancy
- Risks of Anemia in Pregnancy
- Tests for Anemia
- Treatment for Anemia
- Preventing Anemia
When you're pregnant, you may develop anemia. When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
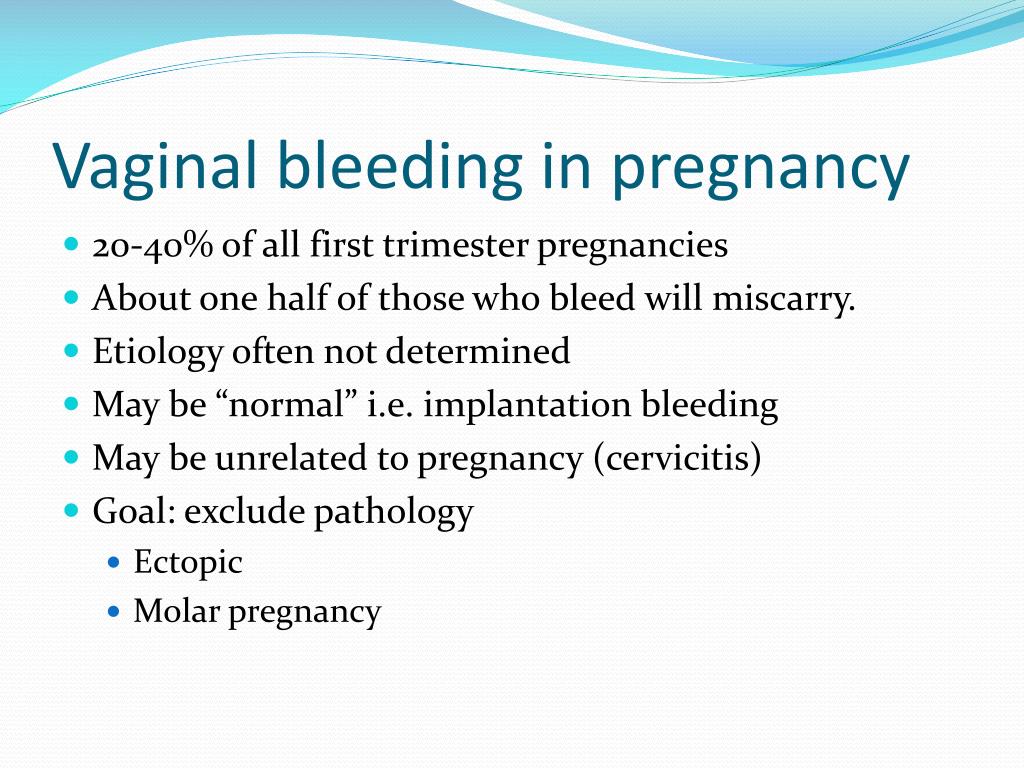
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons.
Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
Types of Anemia During Pregnancy
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia. This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate is the vitamin found naturally in certain foods like green leafy vegetables A type of B vitamin, the body needs folate to produce new cells, including healthy red blood cells.
During pregnancy, women need extra folate. But sometimes they don't get enough from their diet. When that happens, the body can't make enough normal red blood cells to transport oxygen to tissues throughout the body. Man made supplements of folate are called folic acid.
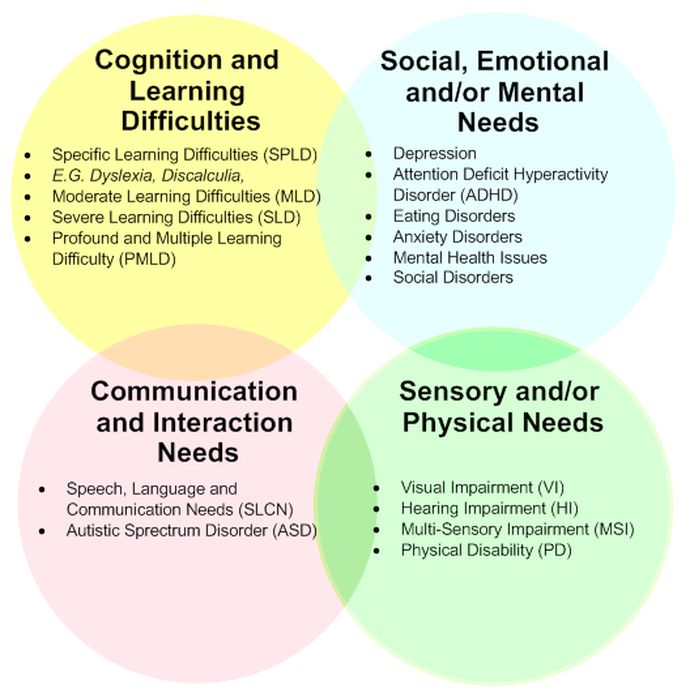
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.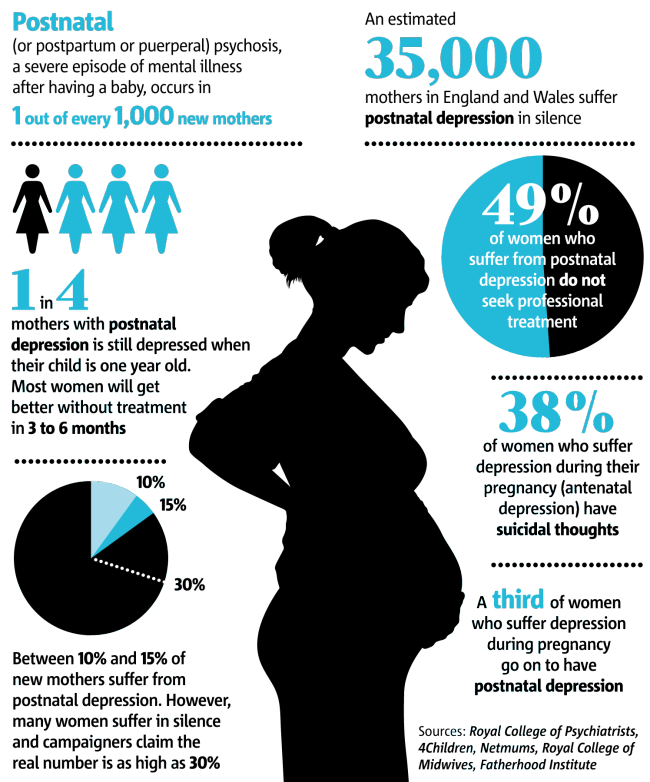
Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red blood cells. When a pregnant woman doesn't get enough vitamin B12 from their diet, their body can't produce enough healthy red blood cells. Women who don't eat meat, poultry, dairy products, and eggs have a greater risk of developing vitamin B12 deficiency, which may contribute to birth defects, such as neural tube abnormalities, and could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk for becoming anemic. That's because they need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have obvious symptoms. And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.
Tests for Anemia
During your first prenatal appointment, you'll get a blood test so your doctor can check whether you have anemia. Blood tests typically include:
Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If you have lower than normal levels of hemoglobin or hematocrit, you may have iron-deficiency anemia. Your doctor may check other blood tests to determine if you have iron deficiency or another cause for your anemia.
Even if you don't have anemia at the beginning of your pregnancy, your doctor will most likely recommend that you get another blood test to check for anemia in your second or third trimester.
Treatment for Anemia
If you are anemic during your pregnancy, you may need to start taking an iron supplement and/or folic acid supplement in addition to your prenatal vitamins. Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.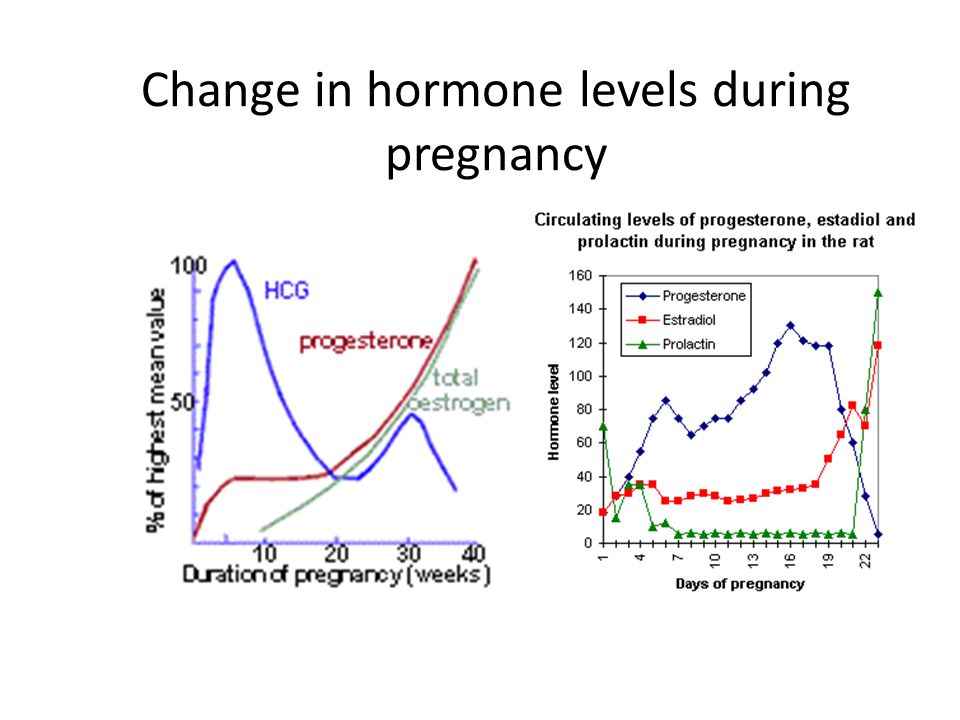
In addition, you'll be asked to return for another blood test after a specific period of time so your doctor can check that your hemoglobin and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in anemia/ blood issues. The specialist may see you throughout the pregnancy and help your OB manage the anemia.
Preventing Anemia
To prevent anemia during pregnancy, make sure you get enough iron. Eat well-balanced meals and add more foods that are high in iron to your diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron. These include:
These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try eating those foods at the same time that you eat iron-rich foods. For example, you could drink a glass of orange juice and eat an iron-fortified cereal for breakfast.
Also, choose foods that are high in folate to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- dried beans
- breads and cereals fortified with folic acid
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians and vegans should talk with their doctor about whether they should take a vitamin B12 supplement when they're pregnant and breastfeeding.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
ANEMIA AND PREGNANCY, OUTPATIENT PRACTICE
Anemia of pregnancy is a series of anemic conditions that occur during pregnancy, complicate its course and usually disappear soon after childbirth or after its termination. Since the prevalence of anemia in pregnant women is much higher than in non-pregnant women, it is logical to assume that most of these anemias are related to the pregnancy itself. Isolation in the ICD-10 anemia of pregnant women (this code is O 99.0) in a separate heading emphasizes the peculiarity of this group of anemia, which consists in the existence of physiological and pathophysiological changes characteristic of pregnancy that contribute to the development of anemia. nine0003
Since the prevalence of anemia in pregnant women is much higher than in non-pregnant women, it is logical to assume that most of these anemias are related to the pregnancy itself. Isolation in the ICD-10 anemia of pregnant women (this code is O 99.0) in a separate heading emphasizes the peculiarity of this group of anemia, which consists in the existence of physiological and pathophysiological changes characteristic of pregnancy that contribute to the development of anemia. nine0003
The most common consequences of anemia in pregnancy are miscarriage, premature birth, intrauterine growth retardation and an increased risk of low birth weight babies. The development of anemia in the 1st and 2nd trimesters of pregnancy is associated with a two-fold increase in the risk of preterm birth.
Most researchers believe that iron stores in the fetus do not depend on the iron content in the mother's body. The transfer of iron from the mother through the placenta is regulated by the needs of the fetus, even against the concentration gradient, and mainly occurs in the 3rd trimester of pregnancy. That is why the development of iron deficiency is possible only in premature babies. nine0003
That is why the development of iron deficiency is possible only in premature babies. nine0003
These adverse effects of anemia in pregnancy are generally associated with hemoglobin levels < 90 g/l. With a hemoglobin level of 90-110 g / l in the second half of pregnancy, the prognosis for a woman and a child is favorable. At the same time, an increase in the concentration of Hb above 120 g / l in this period of gestation is fraught with a high risk of complications (in particular, preeclampsia).
Any pregnancy results in an increase in plasma volume, which averages 1250 ml. This is approximately 1.5 times the plasma volume in non-pregnant women. This condition is one of the main reasons for the relative decrease in Hb levels in pregnant women. nine0003
Today, the lower limit of the normal concentration of Hb in pregnant women is 110 g / l, Hb from 90 to 110 g / l is anemia of 1 degree, from 70 to 90 g / l - anemia of 2 degrees, < 70 g / l - anemia 3 tbsp.
According to WHO, 35-75% of pregnant women in the world are anaemic every year. In domestic obstetric practice, the prevalence of iron deficiency in pregnant women is considered to be high.
In domestic obstetric practice, the prevalence of iron deficiency in pregnant women is considered to be high.
Pregnancy anemia is multifactorial, and iron deficiency is an important, but by no means the only, cause of anemia during pregnancy. nine0003
FORMS OF ANEMIA.
| Acquired | Hereditary |
| 1. iron deficiency 2. Post -hemorrhagic 3. Folic -deficiency 4. INEMISIA ormias5. Hemolytic | 1. Thalassemias 2. Sickle cell diseases 3. Anemias in other hemoglobinopathies 4. Hemolytic anemias outside of hemoglobinopathies |
The most common types of anemia in pregnancy include iron deficiency anemia (IDA) and folic deficiency anemia, and less frequent are aplastic, megaloblastic, hemolytic anemias.
Factors that predispose to the development of IDA in pregnant women include frequent bleeding with placenta previa; anemia that existed in the patient's mother during pregnancy and prematurity of the patient, as well as seasonality and related changes in the composition of food (vitamin deficiency in the winter-spring period).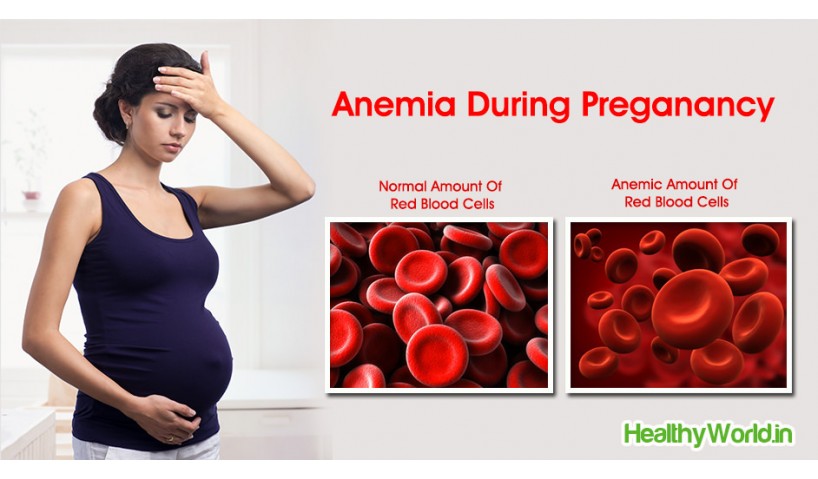 nine0003
nine0003
Anemia of inflammation - in recent years, there has been an increase in the number of women with urogenital infections (colpitis, cervicitis, bacterial vaginosis, pyelonephritis, etc.), which often occur latently. At the same time, about 30% of pregnant women with urogenital infections approach childbirth in a state of anemia, despite the repeated correction with iron preparations. This anemia is defined as "hypochromic anemia without iron deficiency" with normal or elevated iron stores in the body.
Complaints with anemia during pregnancy are usually rare, usually in the presence of concomitant pathology. The most characteristic are complaints of weakness, dizziness, fatigue, in more severe cases, shortness of breath, anxiety and impaired consciousness.
Examination and treatment at the outpatient stage of patients with anemia in pregnancy is carried out in accordance with the Order of the Ministry of Health of the Russian Federation dated 01.11.2012. No. 572n.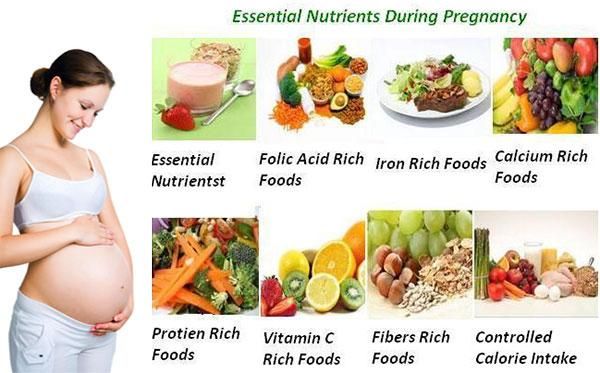
Examination at the outpatient stage:
1) Completed general clinical blood test once a month with leukocyte count, count of reticulocytes and platelets. nine0003
2) ECG in each trimester.
3) Biochemical blood test (total protein, serum iron, ferritin, transferrin, total and direct bilirubin).
4) Consultation with a general practitioner (hematologist) and further follow-up (1-2 times a month).
5) Clarification of the diagnosis and resolution of the issue of the possibility of continuing the pregnancy up to 10 weeks.
6) Bone marrow puncture (as prescribed by a hematologist).
7) CTG and dopplerometry in dynamics. nine0003
Outpatient treatment:
1) Diet rich in proteins, iron, vitamins and folates.
2) Preparations containing iron (in accordance with the Decree of the Government of the Russian Federation of December 26, 2015 N 2724-r, which contains a list of vital and essential drugs for medical use for 2016) - these are oral preparations of 3-valent iron - iron 3 hydroxide polymaltose (maltofer, fenyuls, ferrum lek).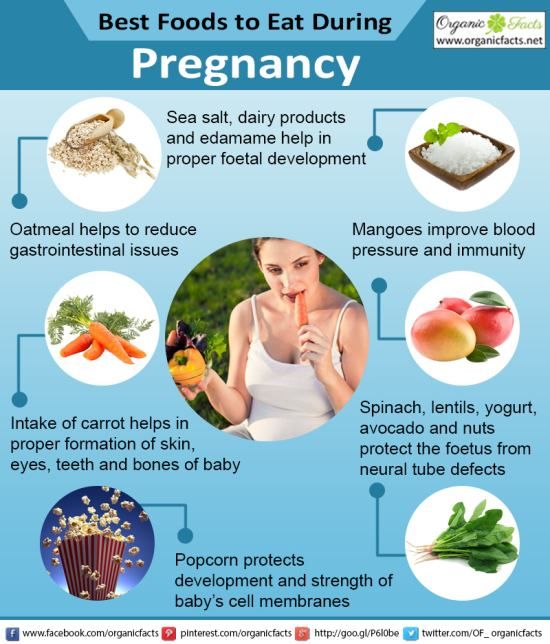 It is not recommended to stop taking iron supplements after normalization of hemoglobin levels. nine0091
It is not recommended to stop taking iron supplements after normalization of hemoglobin levels. nine0091
3) Treatment of underlying and concomitant diseases.
Indications for hospitalization:
1) Deterioration of the pregnant woman's condition, lack of effect from outpatient treatment of pregnancy complications.
2) Planned hospitalization for delivery at 38-39 weeks.
Prevention of anemia in pregnancy.
To maintain a normal iron balance during pregnancy, it is necessary that:
1. iron stores in the woman's body by the beginning of pregnancy are adequate; nine0003
2. The pregnant woman's diet contained sufficient bioavailable iron to ensure high levels of intestinal absorption in the 2nd half of pregnancy.
The daily iron requirement of a pregnant woman is estimated at 27 mg. Lower intake in women with inadequate iron stores may lead to anemia. Iron absorption is greatly increased in the presence of ascorbic acid. Therefore, it is most beneficial to consume foods containing iron in combination with foods fortified with vitamin C.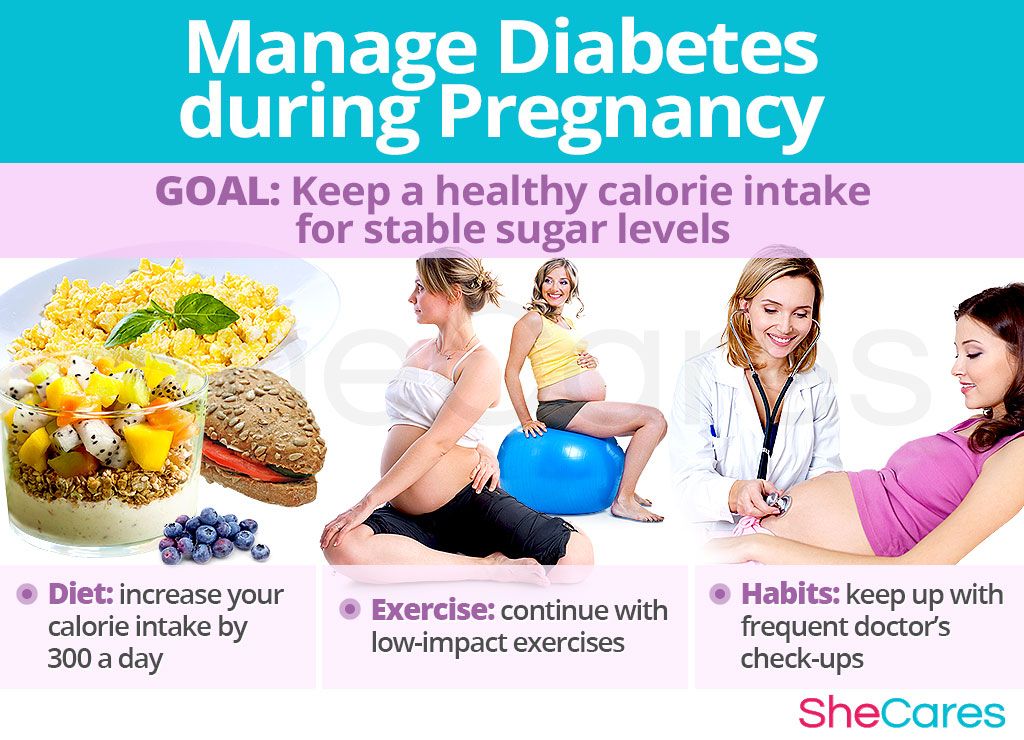
WHO recommends 60 mg iron per day for all pregnant women in areas where the prevalence of IDA is less than 20% and 120 mg where it is above this value.
Prevention of iron deficiency during pregnancy planning is an ideal form of prevention of IDA in pregnant women.
Primary prevention of IDA in pregnant women aims to reduce the prevalence of iron deficiency during pregnancy and prevent the adverse effects it can cause on the woman and fetus. nine0031
2014
1803
382
21,2
2015
1782
462
26
Statistical data on the incidence of anemia for 6 months. 2015 and 6 months 2016
| Finished pregnancy | Anemia in pregnancy | % | |
| 2015 | 845 | 155 | 18% |
6 mon.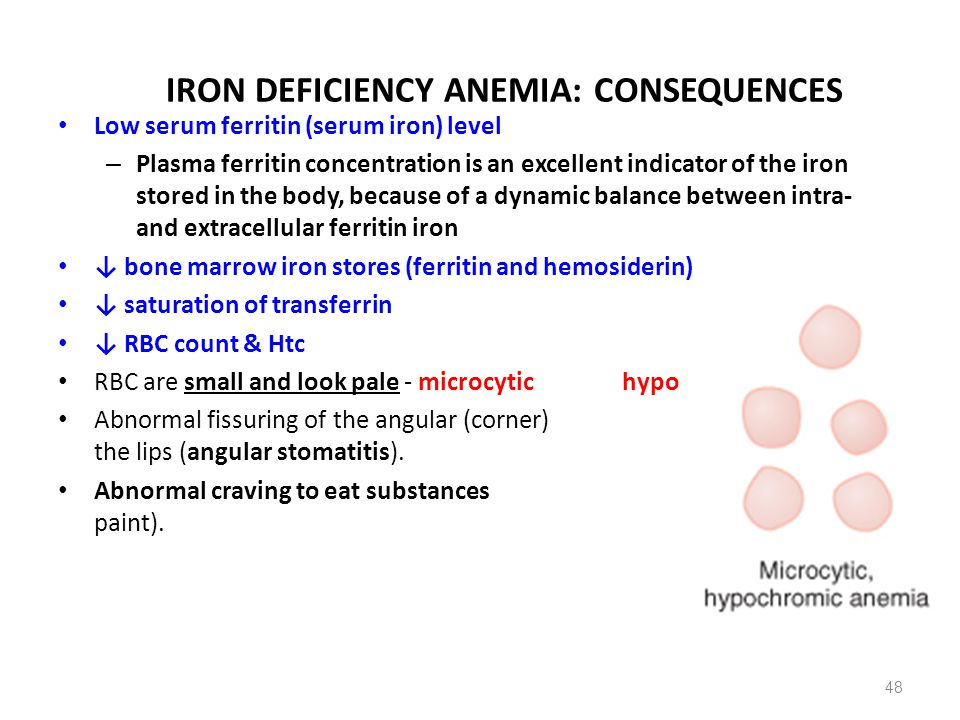 2016 2016 | 1118 | 250 | 22.3% |
If the above incidence of anemia in pregnant women over the past 3 years, then we can say the following in 2013. and in 2015 % of this pathology among pregnant women remained approximately at the same level, in 2014 there was a slight decrease in this indicator to 21.2%. nine0003
Management of patients with anemia of pregnancy in the w/c No. 2.
No. 572n.
2. When the diagnosis of anemia of pregnancy is established, the patient is referred for a consultation with a general practitioner f/c.
3. With anemia 2-3 tbsp. and not amenable to correction of anemia 1 tbsp. the woman is sent for a consultation with a hematologist.
4. Within the framework of the Birth certificate program, we prescribe free oral iron preparations to patients with anemia of pregnancy. nine0003
5. In accordance with the order of the Ministry of Health of the Republic of Kazakhstan of 21. 01. No. 54 “On providing adequate nutrition for pregnant women, nursing mothers, as well as children under the age of 3 years in the Ryazan region”, we issue certificates for receiving monthly monetary compensation before childbirth to pregnant women diagnosed with anemia of 2-3 tbsp.
01. No. 54 “On providing adequate nutrition for pregnant women, nursing mothers, as well as children under the age of 3 years in the Ryazan region”, we issue certificates for receiving monthly monetary compensation before childbirth to pregnant women diagnosed with anemia of 2-3 tbsp.
In order to prevent anemia in pregnant women during preconception preparation, taking into account the level of initial hemoglobin, patients are prescribed iron preparations.
As part of the classes at the "School of Pregnant Women", women from early pregnancy are told about the need for a full-fledged, rational nutrition during pregnancy in order to prevent anemia. nine0003
Anemia during pregnancy
220045, Minsk, st. Semashko, 10
This email address is being protected from spambots. You must have JavaScript enabled to view.
Version of the site for the visually visible
Healthcare Institution
Minsk Clinical Consultative Diagnostic Center
Call-Center (Registration)
| +375 17 311 10 19 (10 lines) | ||
| +375 17 355 94 50 (7 lines) | ||
| +375 29 238 00 90 (mobile MTS 4 lines) | ||
| +375 44 550 00 90 (mobile A1 4 lines) |
Apply online
Minsk Clinical Consultative and Diagnostic Center Book online Anemia refers to a decrease in the level of hemoglobin in the blood. During pregnancy, the amount of fluid in a woman's body increases, and hence the volume of circulating blood. Due to this, the blood "thinns" and the proportion of hemoglobin in its total volume falls. This is considered normal, and therefore the lower limit of the amount of hemoglobin during pregnancy is set at 110 g / l (at a rate of 120-140 g / l for a non-pregnant woman). But a further drop in hemoglobin levels is dangerous for the health and even the life of the expectant mother. nine0003 Depending on the values of this indicator, anemia during pregnancy can be: The most common complications of anemia during pregnancy are: So anemia during pregnancy is by no means a harmless condition. It has serious consequences for both mother and fetus. During pregnancy, iron is consumed not only for the mother's hematopoiesis, but also for the needs of the fetus. This consumption increases especially actively at the 16–20th week, when the process of hematopoiesis in the fetus starts. By the end of pregnancy, iron stores are depleted in any woman and it takes 2-3 years to fully restore them. nine0003 Other causes of anemia during pregnancy are: If we talk about risk groups for developing anemia during pregnancy, then they can include women: with multiple pregnancies and multiple births; who had menstruation for more than 5 days before pregnancy; who had symptoms of anemia during a previous pregnancy; with gestosis; with chronic diseases of the gastrointestinal tract, liver, chronic infections; vegetarians. Considering that during pregnancy the need of a woman's body for a microelement increases by 15–33%, symptoms indicating hypoxia usually come to the fore: weakness, fatigue; sleep disturbance: during the day - drowsiness, at night - insomnia; headaches; dizziness, tinnitus; dyspnea; heartbeat; fainting. The tolerance of anemia symptoms is individual: someone faints at relatively high hemoglobin values, someone refuses hospitalization with hemoglobin at a level of about 70 g / l, sincerely not understanding the severity of anemia and its danger during pregnancy. That is why a clinical blood test during pregnancy is mandatory and several times. The drop in the values of iron in the blood serum and serum ferritin is also important. A decrease in the amount of the latter to 12 μg / l indicates an iron deficiency, even if hemoglobin is still normal. Treatment of anemia while expecting a baby will include diet therapy. One of the foundations of both the prevention and treatment of anemia during pregnancy is proper nutrition. Nutrition for the prevention of anemia during pregnancy should contain a sufficient amount of the substances necessary for normal hematopoiesis - this is meat, fish. In these products, iron is initially divalent, so it is easily absorbed. But diet alone may not be enough even for prevention. Iron supplements are prescribed to treat anemia. Usually limited to means for oral administration (i.e., inside) - iron preparations in injections are recommended only in severe cases and only in a hospital setting. nine0003 Both Russian and foreign experts note that the prevention of anemia in pregnant women is more effective than its treatment, and the higher the hemoglobin level, the easier it is to bring it back to normal. However, common sense says the same. Therefore, when planning a pregnancy, and even more so already expecting a child, it is better to prevent anemia without waiting until iron deficiency becomes noticeable. +375 17 355 94 50 (Horizontal) +375 29 238 00 90 (mobile MTS) +375 44 550 00 90 (mobile A1) You are here:

Everyone at risk should especially carefully monitor their condition and, if possible, take care of the prevention of anemia during pregnancy. nine0003
 nine0003
nine0003