Missed miscarriage after heartbeat
Missed miscarriage: how to tell if you’re having one
What is a missed miscarriage?
A missed (or silent) miscarriage happens when the embryo stops developing and instead of being expelled from the body remains in the uterus.
There are often no typical miscarriage signs associated with a missed miscarriage and as a result they regularly go unnoticed. Missed miscarriage is usually discovered during the first routine scan in early pregnancy.
How likely is a missed miscarriage?
On average miscarriage occurs in 12 – 24% of clinically confirmed pregnancies. Missed miscarriage contributes to over 50% of miscarriages.
How do you know if you have a missed miscarriage?
What are the symptoms of a missed miscarriage?
There are often very few obvious signs of a missed miscarriage. Although the embryo has stopped growing your placenta may still be producing hormones that cause early pregnancy symptoms which can mask the pregnancy loss.
Some women may notice mild cramping or light bleeding observed as a brownish discharge. Others may notice a loss or lessening of pregnancy symptoms such as nausea, breast tenderness and fatigue.
It is important to remember however that pregnancy symptoms may come and go as part of a normal pregnancy, and a lessening of symptoms is not necessarily any cause for concern.
What are the first signs of a missed miscarriage?
Missed miscarriage often goes unnoticed because of a lack of symptoms—this type of miscarriage doesn’t usually look like anything in terms of symptoms or bleeding that you could observe. This means that the first signs of a missed miscarriage are usually discovered during the first pregnancy scan.
How is a missed miscarriage diagnosed?
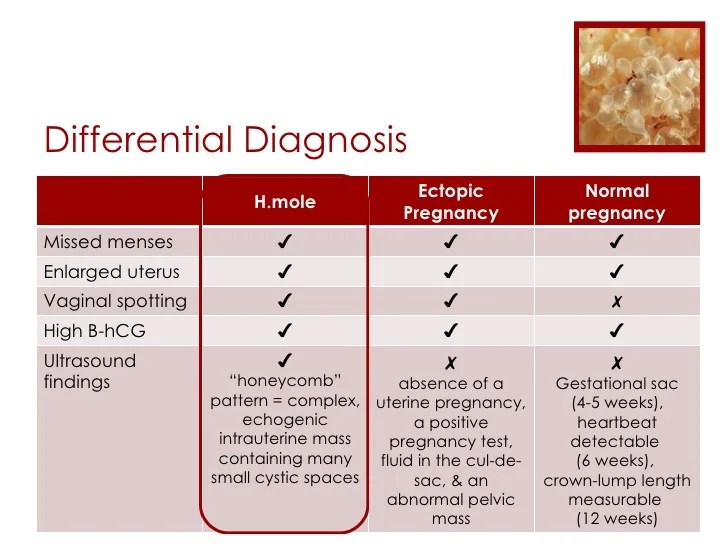
Missed miscarriage is usually diagnosed by ultrasound. Your doctor will not be able to detect a heartbeat, or the embryo will appear too small for the date of the pregnancy. It is common for the diagnosis to be confirmed by a repeat scan at a later date, usually seven to 14 days later.
Hormone measurements do not tend to be used to diagnose missed miscarriage.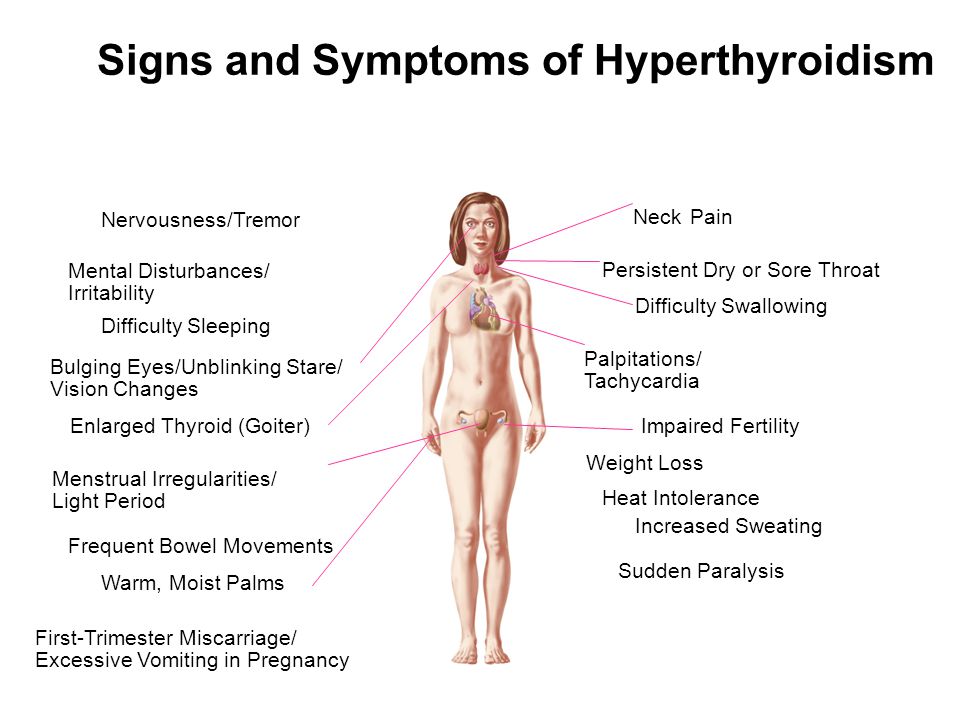 The pregnancy hormone hCG normally doubles every 24 – 48 hours during the first 8 weeks of pregnancy, peaking at 10 weeks. Slower doubling times of hCG in the first trimester can be associated with an increased risk of miscarriage.
The pregnancy hormone hCG normally doubles every 24 – 48 hours during the first 8 weeks of pregnancy, peaking at 10 weeks. Slower doubling times of hCG in the first trimester can be associated with an increased risk of miscarriage.
Studies have found that the doubling time of hCG can vary widely between women which means hCG measurements alone are not reliable enough to diagnose miscarriage.
If you are less than 10 weeks pregnant however your doctor may monitor the level of hCG in your blood for a few days and use this information in combination with your ultrasound scan to confirm your diagnosis.
Missed miscarriage after heartbeat
Although it is possible, the risk of any type of miscarriage after the detection of a fetal heartbeat is very rare. Following a healthy scan at eight weeks the chance is less than 2%. The risk of miscarriage continues to decrease as pregnancy continues, falling to less than 1% at 10 weeks.
How long can missed miscarriage go undetected?
Because the symptoms tend to be very mild, a missed miscarriage can go undetected for several weeks.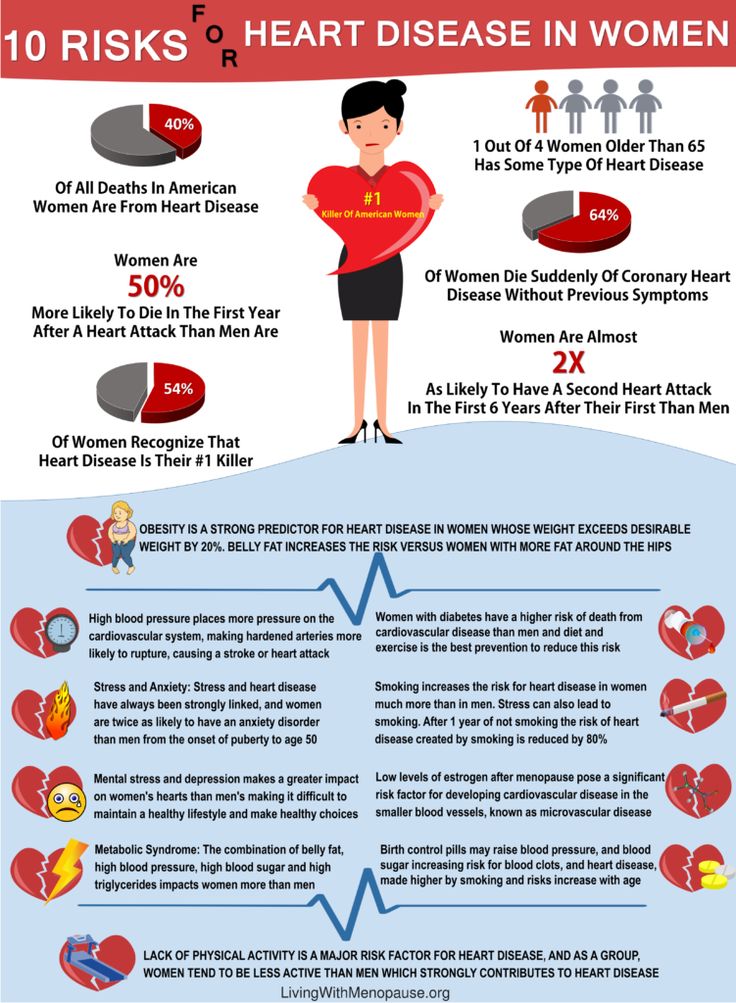 Missed miscarriage is usually discovered at the first trimester scan between 11 and 14 weeks.
Missed miscarriage is usually discovered at the first trimester scan between 11 and 14 weeks.
How does a missed miscarriage happen?
What happens when you have a missed miscarriage?
Missed miscarriage may occur because of a condition known as a blighted ovum. A blighted ovum is a fertilized egg which implants into the uterus forming a gestational sac but fails to develop. On ultrasound it is detected as an empty gestational sac.
Sometimes the implanted embryo will begin to form but then development stops. In these cases, a fetal pole or fetus can be observed in the gestational sac but will no fetal heartbeat will be detected.
What are the reasons for a missed miscarriage?
Like other types of miscarriage chromosomal abnormalities are the most common cause and contribute to over 50% of miscarriages.
In a viable pregnancy each parent contributes one set of chromosomes which contains the genetic material. Abnormalities occur if the sperm or egg that have fused to form the embryo do not have the correct amount of genetic material.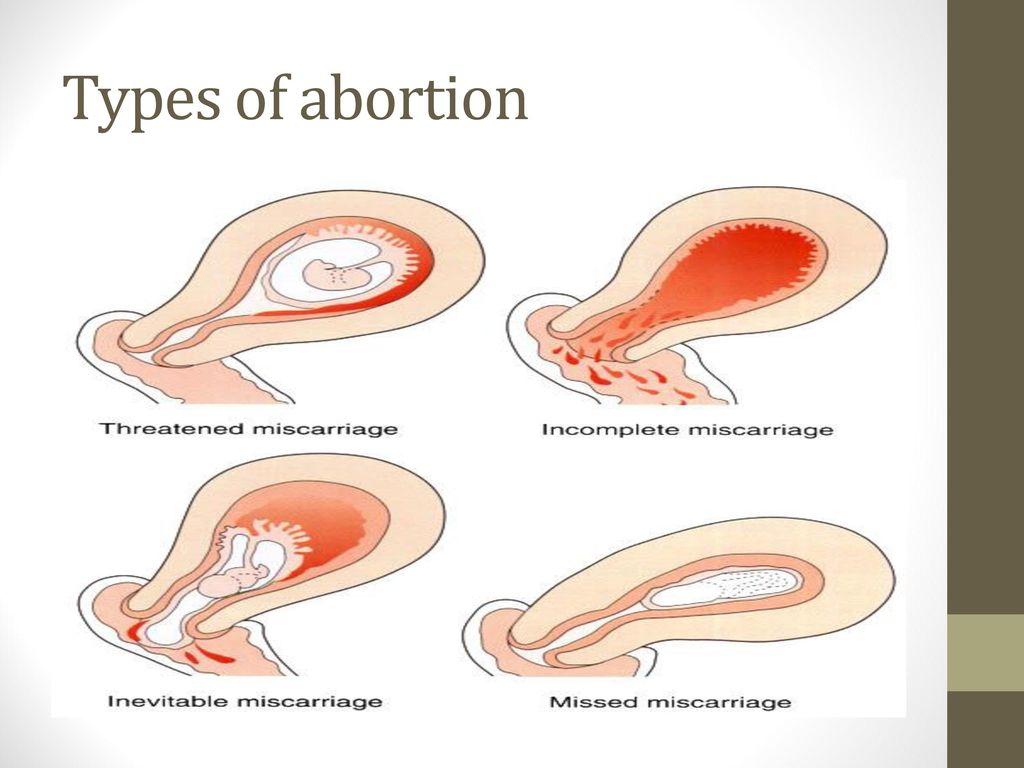 These abnormalities can either be genetically inherited or occur spontaneously.
These abnormalities can either be genetically inherited or occur spontaneously.
The risk of spontaneous chromosomal abnormalities increases with maternal age. A number of studies now suggest that paternal age may play a small part too but this has only recently become a focus of research.
Other less common risk factors for miscarriage include:
- Lifestyle choices, including smoking and excessive alcohol and caffeine intake
- Structural abnormalities of the uterus
- Poor eating habits (malnutrition, obesity or being underweight)
- Poorly managed endocrine disorders such as polycystic ovary syndrome, thyroid disease, and type I diabetes
Can I prevent missed miscarriage?
It is important to remember that miscarriage caused by chromosomal abnormalities accounts for the highest number of pregnancy losses and this cannot be prevented.
You can however increase your chances of a healthy pregnancy. Before conceiving again focus should be on ensuring good general health and well-being and making sensible lifestyle choices.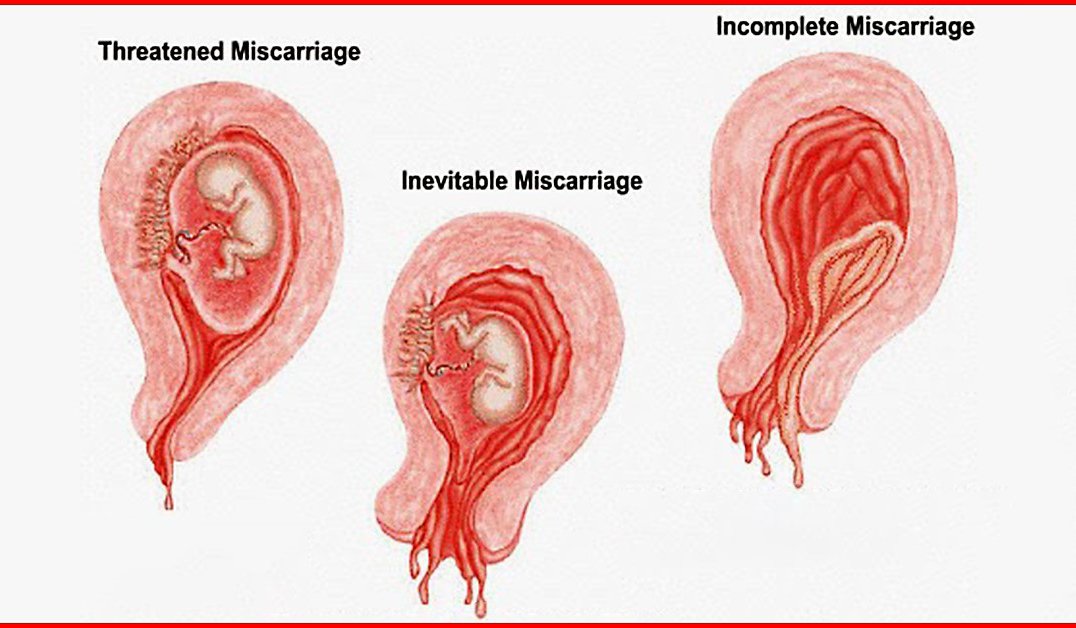 This means eating well, taking regular exercise, managing stress, and maintaining a healthy weight.
This means eating well, taking regular exercise, managing stress, and maintaining a healthy weight.
Sometimes couples experience recurrent miscarriage (three or more consecutive pregnancy losses). If you have experienced this your doctor will usually carry out further investigations.
This may involve examining the structure of your uterus, looking at blood hormone levels, as well as genetic tests of both you and your partner. There is also recent research to suggest that sperm quality could be linked to recurrent miscarriage.
If you have experienced multiple previous pregnancy losses and have become pregnant again you may be offered an earlier ultrasound scan at seven or eight weeks gestation to reassure you that the pregnancy is progressing normally.
Can stress cause missed miscarriage?
There is limited evidence to suggest stress is linked to missed miscarriage. When looking to conceive again focus should be on maintaining good physiological and mental well-being.
What are the treatment options for a missed miscarriage?
Unfortunately, once a miscarriage has started there is nothing that can be done by you or your doctor.
Following diagnosis, the next steps will be focussed on ensuring the embryo is passed or removed from the body, as well as ensuring the miscarriage does not lead to further complications such as uterine infection.
Your doctor will outline several possible treatment options for you:
Expectant Management
Expectant management involves waiting for the tissue to pass naturally out of your body. You will experience symptoms similar to a heavy period. Once started, the bleeding usually slows down within a week although spotting may continue for another week or so.
Studies have shown that expectant management is not always successful and can have a higher rate of complications compared to other treatments. Women can also find the uncertainty of not knowing when the bleeding will start difficult to manage.
Medical Miscarriage
You may also choose to take a medication—either orally or vaginally—called misoprostol. Misoprostol triggers the body to expel the tissue by causing the cervix to open and the uterus to contract. The process will usually start within hours of taking the pill.
Misoprostol does not work for all women and sometimes a second dose is required. Some studies have also shown that combining misoprostol with a drug called mifepristone can be more effective.
D&C
If the tissue does not pass naturally or with medication a small surgical procedure called dilatation and curettage (D&C) can be performed. After dilating your cervix, your doctor will use a spoon-shaped object called a curette to remove tissue from the inner lining of your uterus.
Surgery can be more effective than expectant management and misoprostol if you are further along in your pregnancy.
Trying again after a missed miscarriage: how long to wait?
If you have suffered a miscarriage it is natural to feel apprehensive about trying to conceive again.
Having one miscarriage however does not affect your chances of getting pregnant again or your risk of miscarriage.
There is no medical reason to delay trying again after a missed miscarriage. Assuming you feel emotionally ready it is perfectly safe have sex again once the miscarriage bleeding has stopped.
One study has even shown that trying to conceive within three months may increase your chances of having a full-term pregnancy. Another study suggests that women who conceive within six months are less likely to have miscarriage than those who wait longer.
By Elizabeth Oliver, PhD |
Tags: miscarriage, pregnancy
View sources
Jurkovic D, Overton C, Bender-Atik R, Diagnosis and management of first trimester miscarriage, The BMJ, 2013
Linnakaari R, Helle N et al, Trends in the incidence, rate and treatment of miscarriage-nationwide register-study in Finland, 1998-2016, Human reproduction, 2019
Lower AM, Yovich JL, The value of serum levels of oestradiol, progesterone and beta-human chorionic gonadotrophin in the prediction of early pregnancy loss, Human reproduction, 1992
Tong S, Kaur A et al, Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit, Obstetrics and gynecology, 2008
Sartorelli EM, Mazzucatto LF, de Pina-Neto JM, Effect of paternal age on human sperm chromosomes, Fertility and sterility, 2001
Andersen AM, Andersen PK et al, Moderate alcohol intake during pregnancy and risk of fetal death, International journal of epidemiology, 2012
Bech BH, Nohr EA et al, Coffee and fetal death: a cohort study with prospective data, American journal of epidemiology, 2005
Boots C, Stephenson MD, Does obesity increase the risk of miscarriage in spontaneous conception: a systematic review, Seminars in reproductive medicine, 2011
Jayasena CN, Radia UK et al, Reduced testicular steroidogenesis and increased semen oxidative stress in male partners as novel markers of recurrent miscarriage, Clinical chemistry, 2019
Schreiber CA, Creinin MD et al, Mifepristone pretreatment for the medical management of early pregnancy loss, The New England journal of medicine, 2018
Schliep KC, Mitchell EM et al, Trying to conceive after an early pregnancy loss: an assessment on how long couples should wait, Obstetrics and gynecology, 2016
Love ER, Bhattacharya S et al, Effect of interpregnancy interval on outcomes of pregnancy after miscarriage: retrospective analysis of hospital episode statistics in Scotland, The BMJ, 2010
▷ Missed miscarriage - Everything you need to know
The shock of a missed miscarriage can be very difficult to deal with – as is any baby loss. Understanding the facts of exactly what a missed miscarriage is and how it will affect your body will help you cope with this difficult time.
Understanding the facts of exactly what a missed miscarriage is and how it will affect your body will help you cope with this difficult time.
A missed miscarriage, sometimes called delayed miscarriage, is when your baby has died in the womb but you haven’t passed the pregnancy tissue yet. This might mean you haven’t bled or experienced any pain usually associated with losing your baby, or you may have experienced only very mild symptoms. It can also be called a silent miscarriage (usually when there have been no symptoms at all).
As in these circumstances, women do not experience the classic miscarriage signs, it can go unnoticed. This means that missed miscarriages are often discovered during routine antenatal scans, such as your 11-14 week dating scan.
Your doctor or sonographer may see there is no heartbeat or that your baby is too small for the date of your pregnancy. Sometimes they will need to confirm the diagnosis by bringing you back for a further scan a week later.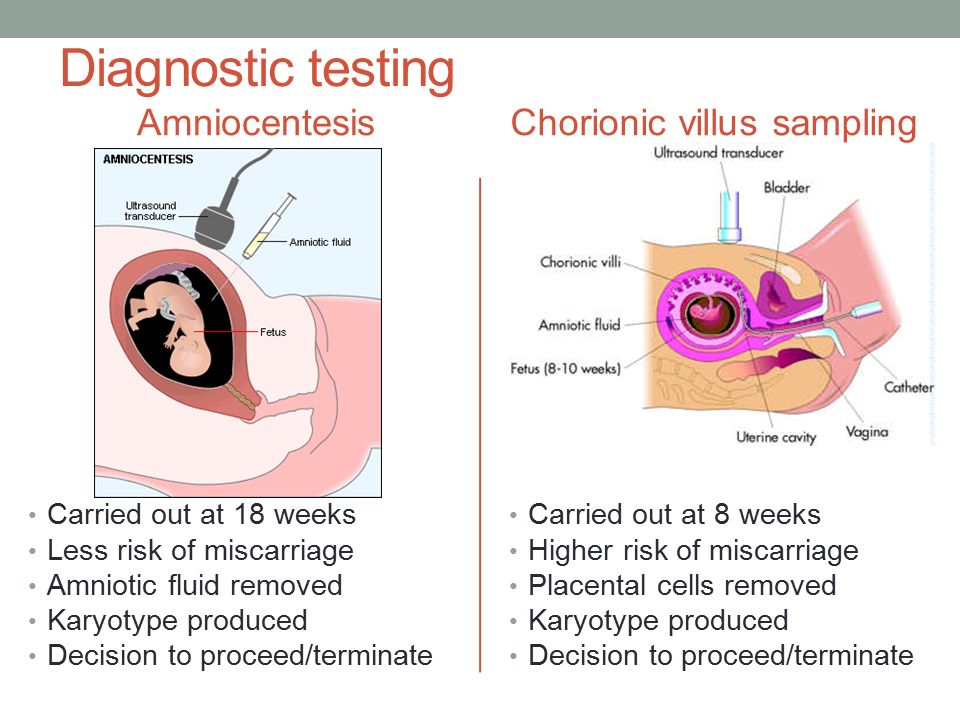
Are there any symptoms of a missed miscarriage?
Often women do not experience any symptoms at all – or may experience some mild bleeding or cramping. Some women experience a sudden loss of pregnancy symptoms – such as morning sickness and breast tenderness. But this doesn’t always happen.
Even if you have had a silent miscarriage, your body still thinks you’re pregnant. Whilst the baby may have died, your placenta may still be producing hormones that cause pregnancy symptoms.
However, it’s important to remember that a loss of pregnancy symptoms can also happen during a healthy pregnancy. After the first trimester, symptoms like sickness and fatigue tend to resolve, so a loss of these symptoms is usually no cause for concern.
So, can you have a miscarriage and not bleed?
You can be diagnosed with a miscarriage without having had any bleeding. However, for the pregnancy tissue to pass, and the lining of the womb to shed, you will need to have some bleeding at some point (or a surgical procedure to remove the pregnancy tissue).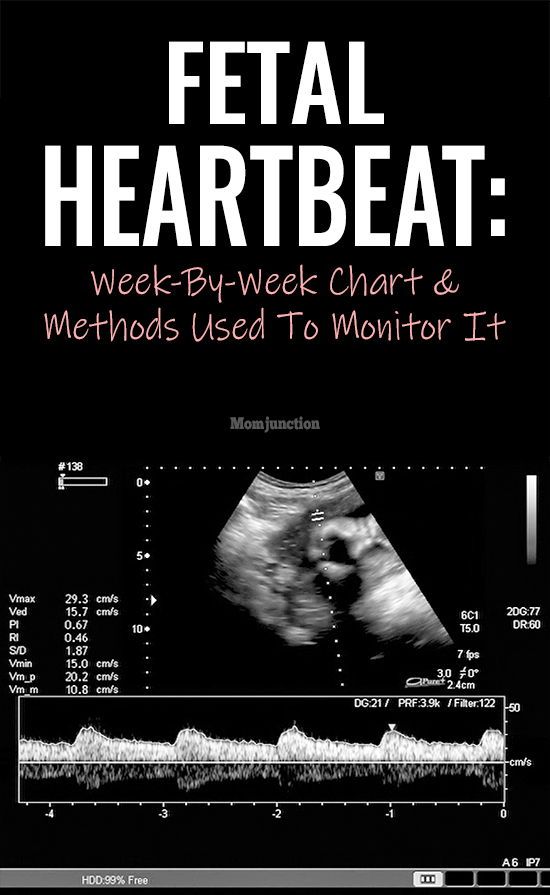
It’s also important to understand that many pregnant women will experience light spotting at some point during their pregnancy. This is quite common and usually will not affect the health of your growing baby. However, if you are experiencing spotting you should always check in with your GP.
When can a missed miscarriage occur?
A missed miscarriage can occur at any point during your pregnancy. However, it is much more likely to happen in the first few weeks of being pregnant. Many silent miscarriages are discovered at the first-trimester scan, between 11 and 14 weeks.
When is the highest risk for silent miscarriage?
As with any miscarriage, the risk is always higher in the first trimester. Miscarriages can occur later in the pregnancy but that is far less common.
How common are missed miscarriages after seeing a heartbeat?
After a scan at 8 weeks showing a healthy foetal heartbeat, your chances of miscarriage, silent or otherwise, drops to 2%. However, most people don’t have a scan until the standard NHS time of 11-14 weeks. The risk of miscarriage continues to reduce as your pregnancy goes on.
However, most people don’t have a scan until the standard NHS time of 11-14 weeks. The risk of miscarriage continues to reduce as your pregnancy goes on.
Can you have a miscarriage without a positive pregnancy test?
For some women, who have a very early miscarriage, they may assume that the bleeding and cramps are just a normal period. In these cases, they may not have done a pregnancy test at all, or the pregnancy may have been so early that a test hadn’t picked it up. However, most modern tests are able to pick up very low levels of HCG, so people are finding out they are pregnant earlier than before.
How long can a missed miscarriage last?
Sometimes, it can take some time to make a diagnosis. Early pregnancy units will always err on the side of caution. If at a scan, your pregnancy looks smaller or much less advanced than would be expected by the timing of your last period, or the time at which your pregnancy test was first positive, it will raise a concern about the possibility of a miscarriage.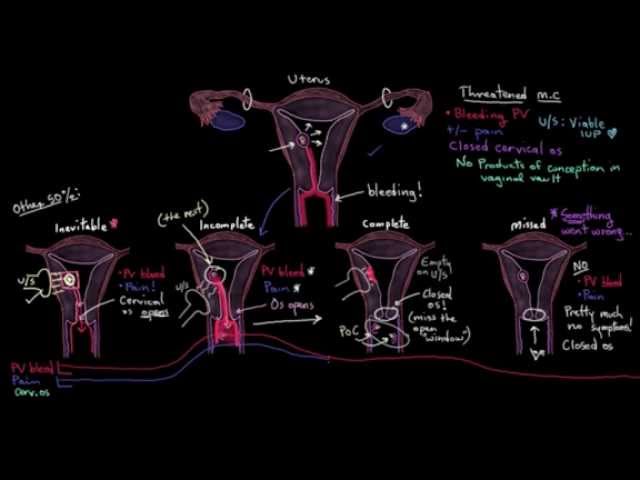
However – it is obviously extremely important not to get this diagnosis wrong, and diagnose a miscarriage incorrectly – so in many cases, when things are not absolutely certain, they will ask you to come back for another scan in one or two weeks (depending on what they saw). They will call this a pregnancy of uncertain viability. At this point, you may have miscarried naturally. If not, the doctor will confirm the missed miscarriage and offer you support and advice on next steps.
If you have a missed miscarriage diagnosed, and choose expectant management – where you wait for the pregnancy tissue to pass – then a miscarriage can take many weeks to start. Usually, the worst part of a miscarriage is over in a day or two, once it starts – but bleeding can continue for two weeks (or longer if some tissue is left behind).
What will happen if I have had a silent miscarriage?
If you have a silent miscarriage confirmed, your doctor will offer you a few different options.
One option is to wait for this miscarriage to happen naturally (often called expectant or conservative management). However, some women find it difficult not knowing when the bleeding will start.
Another option may be to take tablets to start the process of a miscarriage (usually misoprostol, which are given as small tablets which can be placed inside the vagina). This is called medical management.
A final option is to have surgical management of miscarriage. Historically this has been called an ERPC (Evacuation of Retained Products of conception), or your parents generation may call it a ‘D&C’ (dilatation and curettage – but note, we don’t use curettage these days). For this, the neck of the womb (cervix) is gently opened, and a small suction tubing placed inside the womb to remove the tissue. It is a very quick procedure and is usually done while you are asleep (under general anaesthetic).
Some hospitals are able to offer this with you awake – in which case it is usually referred to as an MVA (or Manual Vacuum Aspiration).
The choice of management is very personal – and you should discuss the pros and cons of each with your doctor. None of the choices has been shown to have any differences in terms of your future ability to have children. Expectant and Medical management is less ‘predictable’ – so you are more likely to need to be admitted to hospital with heavy bleeding, for example.
It’s for this reason that many people choose surgical management. Your doctor may also guide you towards surgical management if you are further along in the pregnancy (more than 10 weeks), or at risk of heavy bleeding from medical or expectant management.
Can I get pregnant again after a missed miscarriage?
Yes. Whilst emotionally, this will obviously be an incredibly trying time, remain positive – you should be able to get pregnant again. If you have miscarried naturally, with medication or surgery you will be able to try again after your first cycle, if of course, you feel emotionally and physically ready to do so. There is no increased risk of miscarriage from starting trying quickly.
There is no increased risk of miscarriage from starting trying quickly.
How can I avoid miscarriage?
Miscarriage is, unfortunately, almost impossible to predict or avoid.
The vast majority of miscarriages are down to genetic problems. This means that the complex chemical reactions that occur during conception are not quite as they should be. Sadly miscarriages happen because the body knows that the baby would not be able to develop healthily and survive to the end of the pregnancy. This is why the majority of miscarriages aren’t preventable.
In a few cases, there may be some physical issues that could put you at risk of recurrent miscarriage. These will usually be identified as recurring miscarriage (3 or more miscarriages). There is also recent research to indicate that sperm health could be linked to recurrent miscarriage. All too often, the focus is on a woman’s body, but both partners should be tested if miscarriage is happening each time you fall pregnant.
The most important thing to remember is that miscarriage is not your fault. It is usually completely random and you should be able to have a healthy pregnancy after a miscarriage.
What should I eat to avoid miscarriage?
Your diet will not help you prevent a miscarriage, and there is no magical food that will help you avoid it. However, a healthy, balanced diet will increase your chances of a healthy pregnancy. Your baby needs nutrients to grow and develop, and it gets all its sustenance from your diet. If you are trying to get pregnant, having a fertility diet plan can be useful for keeping you on track.
Whilst there’s no food that will directly prevent miscarriage, there are unhealthy habits you should avoid to reduce your risk. Smoking, drinking alcohol and taking drugs whilst pregnant can make miscarriage more likely.
Can folic acid prevent miscarriage?
Whilst taking folic acid will not directly prevent miscarriage, it will help you have a healthy pregnancy.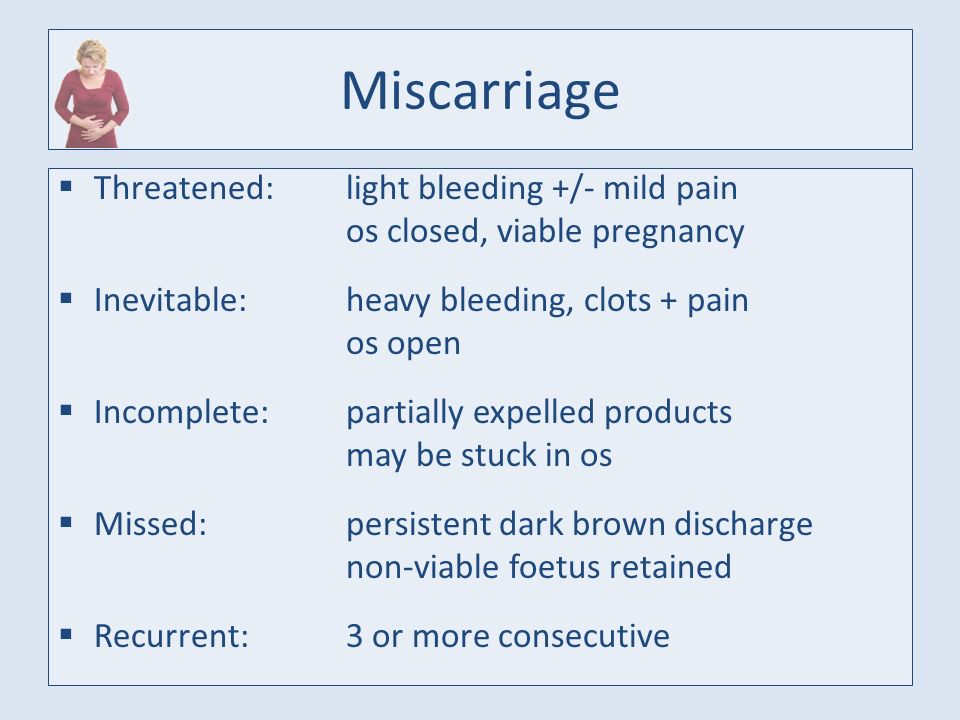 Taking folic acid will help prevent certain defects that can occur in the very early stages of pregnancy. Specifically, folic acid has been linked to reducing cases of Neural Tube Defects. These occur in the first few weeks of pregnancy and include spina bifida and anencephaly.
Taking folic acid will help prevent certain defects that can occur in the very early stages of pregnancy. Specifically, folic acid has been linked to reducing cases of Neural Tube Defects. These occur in the first few weeks of pregnancy and include spina bifida and anencephaly.
You can read more about the impact of folic acid and how you can incorporate it into your preconception care in our folic acid blog.
There is also evidence to support that Vitamin D deficiency could be linked to miscarriage amongst women with previous pregnancy loss. Whilst you can help increase your vitamin D levels by getting lots of natural sunlight and eating a vitamin D rich diet, it may also be advisable to take a vitamin D supplement as part of your preconception care plan. You can read more about the benefits of Vitamin D in our Vitamins for Fertility blog post.
Can stress cause a missed miscarriage?
There is no proven link between miscarriage and stress. This is a fertility myth that unfortunately many women believe – putting unnecessary blame on themselves at what is already a difficult time.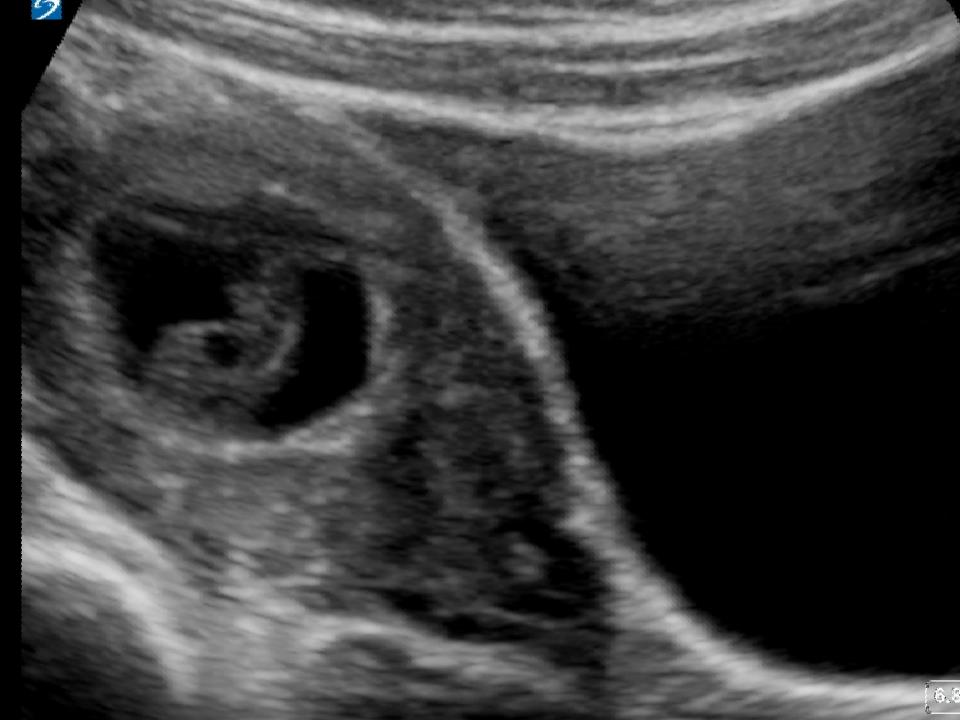 Fertility struggles of any kind are understandably going to cause stress. For your own sake, learning how to manage your emotions healthily will help you have resilience on your fertility journey.
Fertility struggles of any kind are understandably going to cause stress. For your own sake, learning how to manage your emotions healthily will help you have resilience on your fertility journey.
Common symptoms of stress include lack of sleep, unhealthy habits, and bad diet. Whilst these symptoms won’t directly cause miscarriage or fertility struggles, a healthy lifestyle will improve your chances of a healthy pregnancy.
How can I cope with a miscarriage?
Experiencing a miscarriage at any point in your pregnancy can be understandably devastating and impact your mental health. Even if you were in the early stages, it’s likely you will have been planning for the future and already very much in love with your baby. You have every right to deal with your grief in any way you like, and you should surround yourself with people who are understanding and supportive of you.
Whilst it can be tempting to retreat into yourself during this tough time, talking to other people will help. Whilst there is no proven link between fertility and stress, looking after your mental wellbeing when you’re on a fertility journey and getting the support you need is important. Don’t be afraid to ask for help when you need it.
Whilst there is no proven link between fertility and stress, looking after your mental wellbeing when you’re on a fertility journey and getting the support you need is important. Don’t be afraid to ask for help when you need it.
Remember, miscarriage is more common than we think, so you may have friends or family members who have experienced the same thing. There are many charities out there that can offer support to couples and families going through a miscarriage. Tommy’s is a great source of guidance and support and we also love the incredible work Saying Goodbye does.
There are also lots of books that deal with coping with infertility and loss, we’ve recommended some of our favourite fertility books here. It’s important to remember that this is not your fault and you are not alone.
This article was reviewed and approved by experts on Parla.
Join Parla for free today to access more educational content like this, hormone tests and free quizzes, and our community of fertility health experts
Non-developing pregnancy - Official website of the FGBUZ KB No.
 85 FMBA of Russia
85 FMBA of Russia General brief information
Non-developing or missed pregnancy is a cessation of fetal development due to its death, in which there are no signs of miscarriage. Most often, this pathology occurs in the early stages - in the 1st trimester. Another variety of it is a non-developing pregnancy of the type of anembryony. This is a situation in which fertilization has occurred and the fetal membranes have begun to form, but there is no embryo in the fetal egg. nine0005
Symptoms
Unfortunately, in most cases, a woman does not know that her child has already died, since an early pregnancy that does not develop does not have the bright symptoms that are characteristic of a miscarriage. With this pathology, the placenta does not stop producing hormones, which is why the woman continues to feel pregnant. However, in some cases, a woman may notice that her symptoms such as breast tenderness, nausea, and fatigue have disappeared. At later stages, the fading of pregnancy is characterized by the absence of fetal movements in the uterus. nine0005
Causes
Unfortunately, it is not always possible to determine why a woman has an undeveloped pregnancy. If embryonic death occurs during the 1st trimester, it is usually caused by problems in the unborn child. Approximately 3/4 of miscarriages occur during this period. If the fetus dies during the 2nd or 3rd trimester, this may be due to the presence of diseases in the mother.
Diagnosis
The diagnosis of non-progressing pregnancy is most often established after an ultrasound examination, which detects the absence of a heartbeat in the fetus. Ultrasound is performed through the anterior abdominal wall or transvaginally. The latter technique is more accurate, but its implementation is accompanied by some discomfort. To exclude errors with a diagnosis, at least two examination procedures are performed. The doctor can detect the absence of a heartbeat in the fetus later in pregnancy with the help of auscultation with an obstetric stethoscope.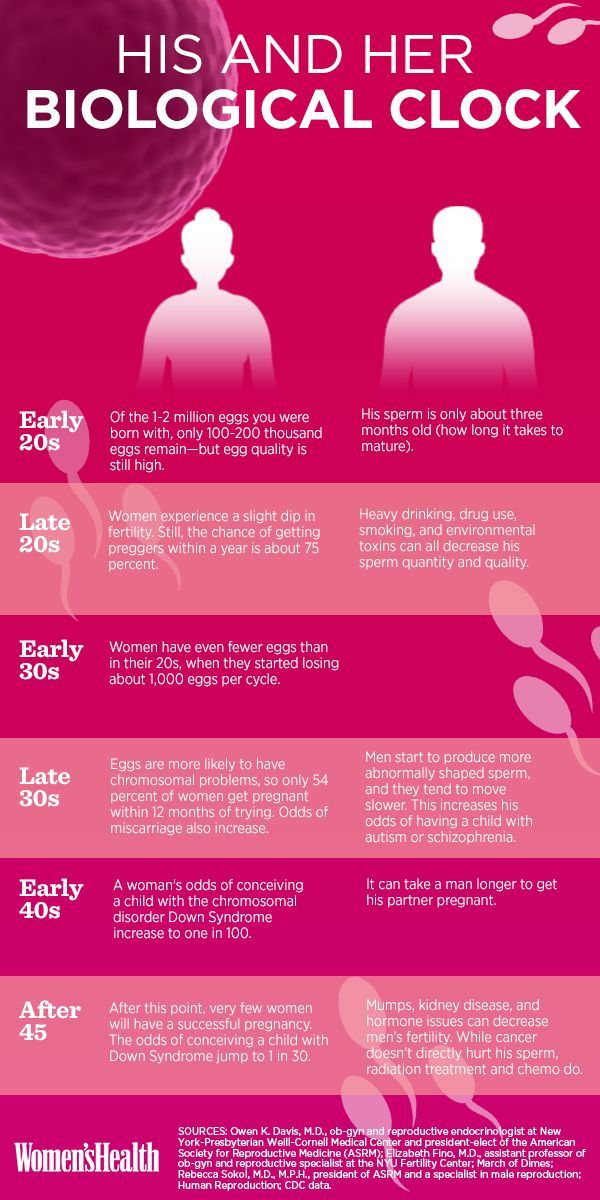 Cardiotocography, a technique for recording the fetal heartbeat and uterine tone, will help confirm the fears. Also, the level of human chorionic gonadotropin and progesterone, hormones associated with pregnancy, can be determined. In some cases, the diagnosis is not immediately possible. For example, a non-developing pregnancy before a gestational age of 6-7 weeks is difficult to confirm, since only at this time does the fetus develop a heartbeat. In this case, doctors usually recommend a re-examination in 1-2 weeks. Sometimes fetal death is discovered by chance during a screening ultrasound examination. After a case of pregnancy fading, a man and a woman need to undergo a complete examination, with the help of which specialists will try to identify possible causes of fetal death. Unfortunately, in half of the cases, the etiology of a non-developing pregnancy cannot be detected. nine0005
Cardiotocography, a technique for recording the fetal heartbeat and uterine tone, will help confirm the fears. Also, the level of human chorionic gonadotropin and progesterone, hormones associated with pregnancy, can be determined. In some cases, the diagnosis is not immediately possible. For example, a non-developing pregnancy before a gestational age of 6-7 weeks is difficult to confirm, since only at this time does the fetus develop a heartbeat. In this case, doctors usually recommend a re-examination in 1-2 weeks. Sometimes fetal death is discovered by chance during a screening ultrasound examination. After a case of pregnancy fading, a man and a woman need to undergo a complete examination, with the help of which specialists will try to identify possible causes of fetal death. Unfortunately, in half of the cases, the etiology of a non-developing pregnancy cannot be detected. nine0005
Methods of treatment
As a rule, a woman is offered one of the following options: Expectant management. In the early stages of pregnancy, with intrauterine death of the embryo, it is possible to expect a natural rejection of its tissues by the woman's body. At this time, careful monitoring and observation is carried out. However, you can't wait too long - it's dangerous. As a rule, active treatment can be delayed only up to 2 weeks from the diagnosis. Doctors are not too fond of expectant management during a missed pregnancy. Surgical tactics. After establishing and clarifying the diagnosis, a small obstetric operation is performed - dilation of the cervix and curettage (curettage of the uterine cavity). During this surgical intervention, the tissues of the fetus, its membranes and the placenta are removed from the uterine cavity. The operation is usually performed under general anesthesia. medical tactics. Termination of an undeveloped pregnancy in the early stages (up to 8 weeks of gestation) can also be carried out by a conservative method. For this purpose, drugs are used that cause the uterus to contract and push the fetal tissues and placenta out of its cavity.
In the early stages of pregnancy, with intrauterine death of the embryo, it is possible to expect a natural rejection of its tissues by the woman's body. At this time, careful monitoring and observation is carried out. However, you can't wait too long - it's dangerous. As a rule, active treatment can be delayed only up to 2 weeks from the diagnosis. Doctors are not too fond of expectant management during a missed pregnancy. Surgical tactics. After establishing and clarifying the diagnosis, a small obstetric operation is performed - dilation of the cervix and curettage (curettage of the uterine cavity). During this surgical intervention, the tissues of the fetus, its membranes and the placenta are removed from the uterine cavity. The operation is usually performed under general anesthesia. medical tactics. Termination of an undeveloped pregnancy in the early stages (up to 8 weeks of gestation) can also be carried out by a conservative method. For this purpose, drugs are used that cause the uterus to contract and push the fetal tissues and placenta out of its cavity. With intrauterine death of the fetus in the 3rd trimester, delivery is necessary. To this end, doctors either induce labor through the birth canal or perform a caesarean section. nine0005
With intrauterine death of the fetus in the 3rd trimester, delivery is necessary. To this end, doctors either induce labor through the birth canal or perform a caesarean section. nine0005
Illegal pregnancy: causes, diagnosis, termination
- Services
- In Vitro Fertilization (IVF) nine0038
- Pregnancy management and prenatal diagnosis
- Biopsy of the endometrium nine0038
- Prostate treatment
- Diabetes mellitus in pregnancy nine0038
- Endocrine (hormonal) infertility in women
- Oocyte donation nine0038
- IVF for polycystic ovaries
- Center for Complex Pathologies nine0038
- Biopsy of the cervix
- Treatment of cystitis in women and men nine0038
- PRP therapy for the uterus and ovaries
- Sperm donation nine0038
- Embryo cryopreservation
- Screening ultrasound in the first trimester nine0038
- Pediatric gynecology
- Treatment of urethritis nine0038
- Fertilization of eggs and cultivation of embryos
- Screening ultrasound in the second trimester nine0038
- cervical dysplasia
- Treatment of varicocele nine0038
- Videocolposcopy
- Pregnancy management programs nine0038
- IVF according to compulsory medical insurance for residents of the regions
- Expert ultrasound 3D/4D during pregnancy nine0038
- Non-invasive prenatal genetic test
- Preimplantation genetic testing nine0038
- IVF under CHI for residents of St.
 Petersburg
Petersburg - IVF according to compulsory medical insurance in the Leningrad region nine0038
- Infertility treatment
- ultrasonic cavitation nine0038
- Transfer of embryos into the uterus
- Screening ultrasound in the third trimester nine0038
- Erosion of the cervix (ectopia)
- Treatment of submucosal fibroids nine0038
- Implatest - Endometrial Receptivity Study
- Gynecologist-endocrinologist appointment nine0038
- Colposcopy
- Reception of a mammologist nine0038
- Endometrial polyp
- Laparoscopy of an ovarian cyst nine0038
- Fetal cardiotocography (fetal CTG)
- Hysteroscopy nine0038
- Office hysteroscopy
- Office diagnostic hysteroscopy nine0038
- Office hysteroscopy with endometrial biopsy
- Laboratory diagnostics nine0038
- Day hospital
- Follicle puncture nine0038
- Stimulation of superovulation
- Preeclampsia nine0038
- Ultrasound examination of folliculogenesis with biophysical profile of the uterus
- Hysteroresectoscopy nine0038
- Hysterosalpingography
- Fallopian tube laparoscopy nine0038
- Laparoscopy in gynecology
- Laser vaporization of the cervix nine0038
- Treatment of endometriosis
- Treatment of an ovarian cyst nine0038
- Laparoscopy of uterine fibroids
- Non-developing pregnancy nine0038
- Pathology of the endometrium
- Pathology of the cervix nine0038
- Treatment of the endometrial polyp
- Polyp of the cervix nine0038
- Preventive examination by a gynecologist
- radio wave surgery nine0038
- polycystic ovary syndrome
- Ultrasound hysterosalpinography (USGSG) nine0038
- human papillomavirus
- Vulvovaginal candidiasis nine0038
- Frozen pregnancy
nine0035 Specialists - Cost of services
- Reviews nine0038
- Stock
Sign up
8 812 565-18-40
An expert approach to happiness!
Our branches
Auxiliary
reproductive technology Obstetrics
and gynecology Fetal Medicine Center
Urology
and andrology
Assisted Reproductive Technologies obstetrics and gynecology Center for Fetal Medicine Urology and Andrology nine0005
St. Petersburg, Torez avenue, 72
Petersburg, Torez avenue, 72
Center for Reproduction and Family Planning Medica in St. PetersburgServicesMiscarriage
Frozen pregnancy, non-developing pregnancy or miscarriage. All these terms mean one thing - the embryo (fetus) stops in development. In this case, there was no miscarriage and the embryo remained in the uterine cavity. nine0005
Enroll
Most often this happens in the early stages. And then women who have been diagnosed with this pregnancy can continue to bear and give birth to healthy children. But if this situation is repeated two or more times in a row, then we can talk about habitual miscarriage or habitual miscarriage. This is a serious diagnosis, it requires additional examination, observation and treatment.
How a missed pregnancy is diagnosed
The diagnosis of a non-developing pregnancy is made by an obstetrician-gynecologist together with an ultrasound doctor, taking into account the following signs:
- no growth of the gestational sac within 1-2 weeks;
- the absence of an embryo with the size of the fetal egg at least 25 mm;
- Absence of the heartbeat of the embryo with a coccyx-parietal size of more than 7 mm.

Read more
nine0225 About directionAt the Center for Reproduction and Family Planning "MEDICA" future parents: Independently (if desired) choose an obstetrician-gynecologist who will conduct the pregnancy; Together with the doctor, they choose the optimal pregnancy management program; They receive the most attentive, caring attitude and are always surrounded by warmth and care; Do not stand in queues, but get an appointment with specialists at the appointed time; They are constantly in contact with their obstetrician-gynecologist, they can always contact him personally and ask any questions; Together with an obstetrician-gynecologist, they decide where to give birth and what tactics of childbirth to choose. nine0005
Cost of services
Full price list for referral servicesObstetrician-gynecologist, primary appointment
2 350 ₽ nine0005
Enroll
Obstetrician-gynecologist, repeated appointment
2 100 ₽
Enroll
Obstetrician-gynecologist (highest category / candidate of medical sciences / doctor of medical sciences), initial appointment
2 900 ₽
Enroll
Obstetrician-gynecologist (highest category / candidate of medical sciences / doctor of medical sciences), repeated appointment
2 500 ₽ nine0005
Enroll
show moreVideo
Embryo biopsy
Oocyte vitrification and delayed motherhood program - childbirth (,) cannot be (,) delayed 18+
nine0002 Reproductologist Elena Tanchuk about indications for ART (assisted reproductive technologies) Human papillomavirus (HPV) and cervical cancer - diagnosis, treatment, prevention. Samoilova Svetlana Gennadievna
Samoilova Svetlana Gennadievna
Treatment of infertility in different age periods. Yusupova Oksana Nikolaevna CPS Medica 18+
Hormonal contraceptives COCs - truth and myths. Kovaleva Natalia Sergeevna CPS Medica 18+
Hysterosalpingography (HSG) at the Center for Reproduction and Family Planning Medica
The female factor in infertility. Tanchuk Elena Valerievna. Reproduction Center Medica 18+
Frozen pregnancies - why pregnancy does not develop. Bokach Olga Mikhailovna
Sexually transmitted infections (STIs) - types, transmission, diagnosis. Sheikhov Magomedsadiq 18+
How to plan a healthy pregnancy. Yusupova Oksana Nikolaevna
Yusupova Oksana Nikolaevna
Cryopreservation of germ cells and embryos. Kozhevnikov Igor Valerievich
Treatment of infertility in different age periods. Yusupova Oksana Nikolaevna CPS Medica 18+
The menstrual cycle - the norm and pathology. Danielyan Roza Martunovna. CPS Medica. 18+
Male fertility - when should a man start to worry and anti-age therapy CPS Medica 18+
Reproduction doctor's appointment - we plan pregnancy correctly. Pisaroglo Maria Ivanovna. CPS Medica
Psychosomatics of infertility - all diseases are caused by nerves. Konon Ksenia Mikhailovna. CPS Medica 18+
Reproductologist Elena Tanchuk about indications for assisted reproductive technologies (ART)
PCOS (polycystic ovary syndrome). Danielyan Roza Martunovna. Reproduction Center Medica 18+
Danielyan Roza Martunovna. Reproduction Center Medica 18+
Testosterone and its effect on the human body. Kudryavtsev Artemy Alexandrovich. CPS Medica 18+
Ultrasound screening of pregnant women - why and how often. Ten Natalya Alekseevna. CPS Medica
Successful embryo implantation during natural pregnancy and after IVF. Konon Xenia Mikhailovna.18+
Endometriosis. Zakharova Oksana Vadimovna Center for Reproduction and Family Planning Medica 18+
The episode of the broadcast of the hysteroscopy operation in the 'Center for Reproduction and Family Planning 'Medica'
Erectile dysfunction - diagnosis, treatment, prevention. Sheikhov Magomedsadyk Gasanovich. 18+
Sheikhov Magomedsadyk Gasanovich. 18+
03/27/2021
The lifestyle of the father and his age affect the health of the child
Age, addiction to alcohol and other bad habits of the father can cause birth defects in the unborn child.
Read more
03/20/2021
Expertise on contraception
In developed countries, about 40% of adolescents aged 15-19years have sexual experience.
Read more
02/15/2021
10 questions about IVF
In a couple of years, the world's first "test-tube baby" - Lisa Brown - will be 40 years old.
Read more
01/14/2021
Together against cancer nine0005
February 4th is World Cancer Day.
Read more
All articles
Address
Family Planning Center "MEDICA"
Address:
Torez Ave., 72 (hospital of the Russian Academy of Sciences, 2nd floor)
nine0366 Specific
lakes
nine0366 Pl.