Cracked and sore nipples breastfeeding
Breastfeeding with Sore Nipples - La Leche League International
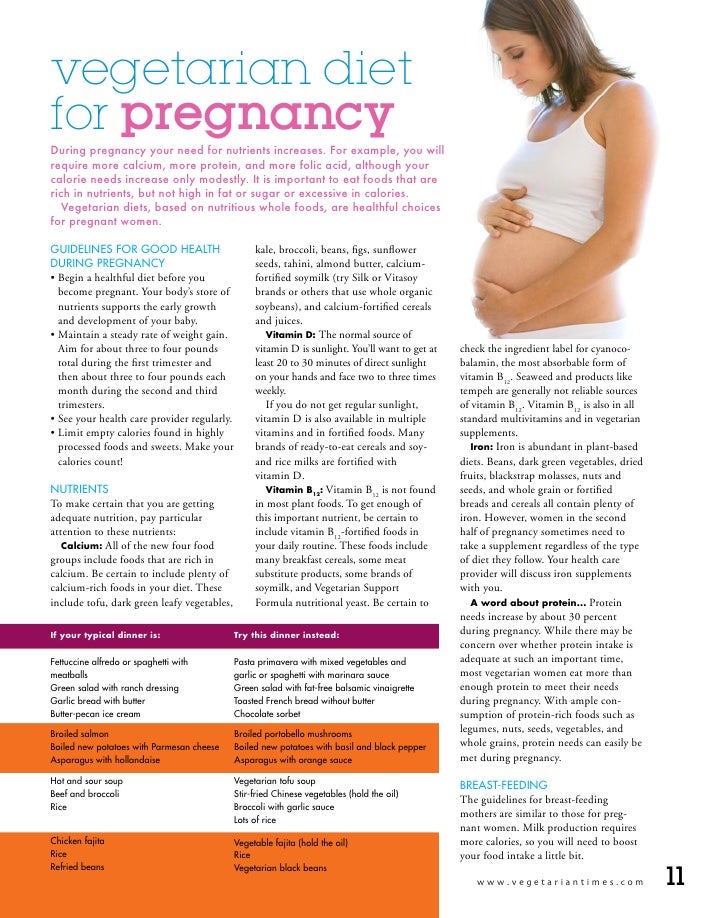
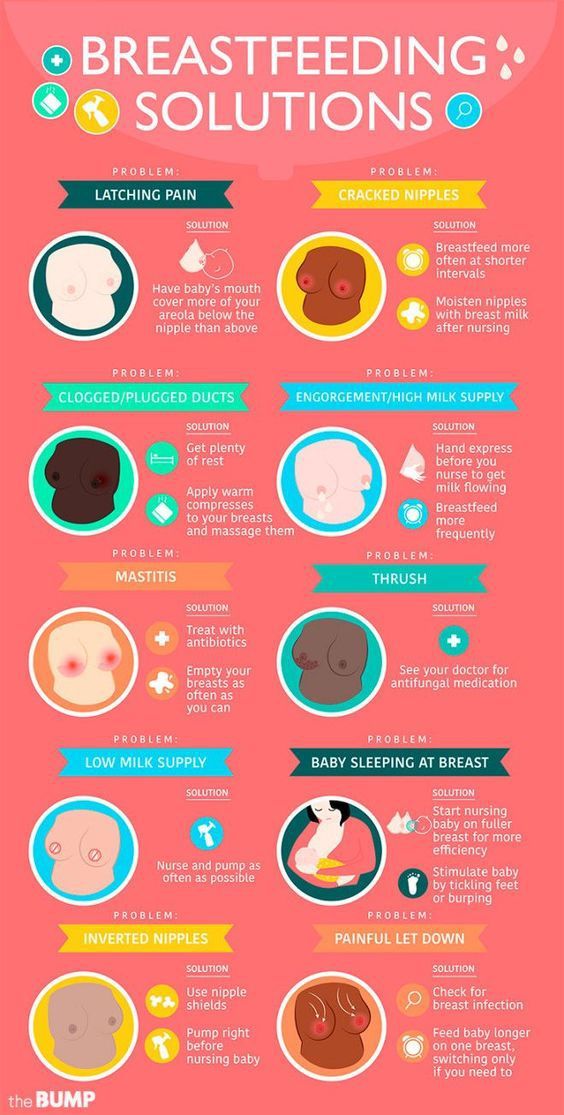
Breastfeeding is something only you can do for your baby. It should be a pleasant experience for both of you. A healthy, full-term baby is likely to know instinctively what to do at the breast. In the first three to five days after birth, if you experience nipple soreness beyond a slight tenderness when your baby latches on, it may be a sign that something isn’t right with the baby’s latch, position, or suck. An adjustment to the latch or positioning can help you and your baby to be more comfortable. With proper positioning and latch-on techniques, you can expect little or no nipple soreness. Correcting poor positioning or latch-on can often alleviate sore, cracked nipples and allow healing to begin.
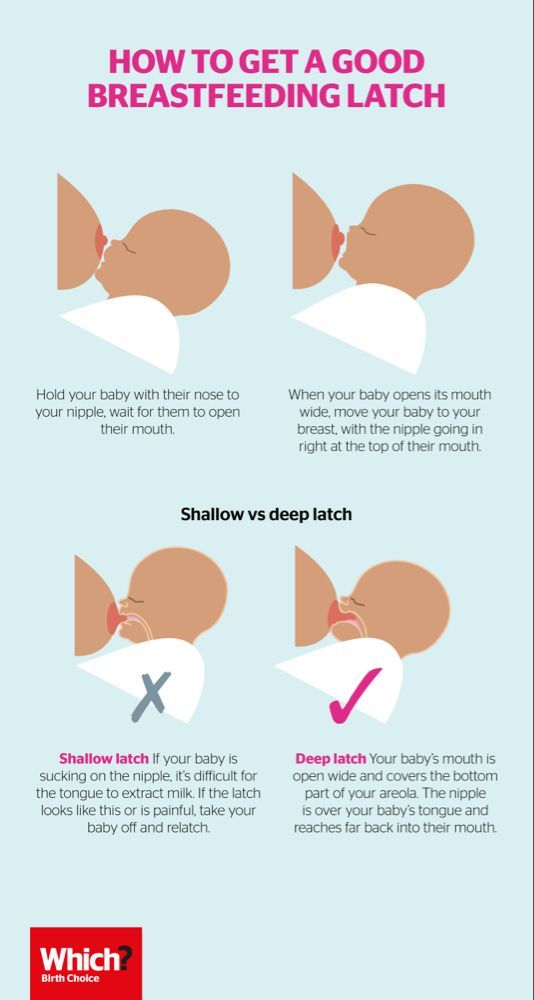
If nipple pain worsens after the early days of breastfeeding your nipple pain may be due to other causes like thrush, bacterial infection, or tongue-tie. Contact a La Leche League Leader for help if you need further assistance to improve your sore nipples.
Learn to recognize your baby’s early feeding cues so you have time to get in a good position and comfortable before he becomes desperately hungry. Early cues include opening his mouth and moving his head side-to-side—known as the rooting reflex—or sucking on hands or fingers. Don’t wait for baby to cry to let you know he is hungry. Crying is a very late hunger cue.
Adjusting the position can improve breastfeeding pain. If you have pain, try different positions such as laid-back, football or cradle position.
Laid-back position- Position yourself comfortably in bed, on the couch or in a recliner with back support, pillows to also support your head, shoulders, arms. Since you’re leaning back, your baby can rest on you in any position you like.
- If you are seated, support your feet with a footrest or a telephone book.
- Let your baby’s whole front touch your whole front.
 His mouth and nose should be facing your nipple. Let your baby’s cheek rest somewhere near your bare breast.
His mouth and nose should be facing your nipple. Let your baby’s cheek rest somewhere near your bare breast. - Rub your nipple on baby’s upper lip to encourage baby to open wide. Bring your baby close. Have his chin touch your breast first, and then his nose will touch your breast.
- Position baby close to you, with his hips flexed, so that he does not have to turn his head to reach your breast. Baby’s feet need to feel supported by your body so they don’t dangle in the air.
- Use one hand to support your breast, if needed, and the other to support baby’s thigh or bottom.
- If you are feeling pain, detach baby gently by using your finger to touch the corner of baby’s mouth and try again.
- This is a good position for a mother who has had a Cesarean birth, as it keeps the baby away from the incision.
- Baby’s is to your side on the same side you are breastfeeding and under your arm. Support your baby’s head in your hand and his back along your arm beside you.

- Support your breast with a “C” hold.
- Have baby facing the nipple, with his mouth at nipple height. Use pillows to bring the baby to the correct height.
- Your baby’s legs and feet are tucked under your arm with his hips flexed and his legs resting along side your back rest so the soles of his feet are pointed toward the ceiling. (This keeps him from being able to push against your chair.)
- Make sure you are relaxed and comfortable as your baby feeds. Lean back in your chair, supporting your back with a bed pillow turned vertically if needed. Don’t lean forward and hunch over your baby. Raise your feet off the floor, using an ottoman or even a phone book. Breathe deeply and be sure to relax and drop your shoulders.
- Position your baby on his side, with his whole body facing yours and angled so his chest is securely against your abdomen. Baby should not have to turn his head to nurse.
- Cradle baby in the arm on the same side as the breast he will be nursing from.
 If you’re breastfeeding on the right breast, baby’s head will rest on your right forearm near your elbow, his nose at the level of your nipple, and his head tilted slightly back. He is supported by your forearm with your hand holding his bottom or thigh.
If you’re breastfeeding on the right breast, baby’s head will rest on your right forearm near your elbow, his nose at the level of your nipple, and his head tilted slightly back. He is supported by your forearm with your hand holding his bottom or thigh. - Support your breast with your other hand well back from the nipple and baby’s mouth, keeping your fingers positioned either above or below or on either side of the breast.
- Bring your baby to the breast. Trigger his natural response to open his mouth wide by touching his lips lightly with your nipple. Light, repeated tapping or brushing triggers a wide-open mouth.
- As you bring baby to the breast with his head slightly tilted back, his chin will press into the breast first. More of your breast will be covered with his lower jaw.
- Aim your nipple toward the roof of baby’s mouth and gently bring him onto the breast as he latches on.
- When baby is latched well, his chin should be pressed into the breast, and his nose slightly away from it.
- If you leave the hand supporting the breast in place, be sure you do not press down with your thumb, which can pull your nipple to the front of baby’s mouth. If you remove the supporting hand from your breast, make sure baby has enough head control to keep him well latched. If your breasts are large, it can be helpful to put a small rolled-up towel beneath them for support.
- This position is a variation of the cradle position, called the cross-cradle position.
- For this position, your baby is supported on a pillow across your lap to help raise him to your nipple level.
- Pillows should also support both elbows so your arms don’t hold the weight of the baby; they will tire before the feeding is finished.
- If you are preparing to breastfeed on the left breast, your left hand supports that breast in a “U” hold.
- You support your baby with the fingers of your right hand. Do this by gently placing your hand behind your baby’s ears and neck with your thumb and index finger behind each ear.

- Your baby’s neck rests in the web between the thumb, index finger and palm of your hand, forming a “second neck” for baby. The palm of your hand is placed between his shoulder blades.
- As you prepare to latch on your baby, be sure his mouth is very close to your nipple from the start. When baby opens his mouth wide, you push with the palm of your hand from between the shoulder blades. His mouth will be covering at least a half-inch from the base of your nipple.
If baby is not latched on well or if it hurts, remove him from the breast by inserting your finger into the side of his mouth and try again.
Look at your nipple after breastfeeding, if it looks blanched or pinched, review the latch and positioning tips to see if you can find adjustments to make. The nipple should look the same way it did before breastfeeding, neither pinched nor blanched.
If nipple soreness persists, contact a La Leche League Leader for help. Mild soreness, if left untreated, can lead to more pain.
You may also find this post about Positioning useful.
Causes of Sore NipplesImproper latch-on occurs when baby does not grasp enough breast tissue or his tongue is positioned improperly. Baby must be able to compress your breast tissue with your nipple positioned deep in his mouth. First, check baby’s body position. Be sure that he opens his mouth very wide, like a yawn, before you offer your breast, checking to see that his tongue is cupped and forward in his mouth. His lower lip should not be tucked in—it should be fanned outward on the breast. If you gently pull down the corner of the baby’s mouth while he is nursing, you should see the underside of his tongue, which should extend over his lower gum line, cupping the breast
Sometimes babies latch deeply, but slide down the nipple during the feed—watch for more distance between his nose and your breast. If this happens, break the suction and re-latch your baby, being sure that he is well supported.
Tongue-tie can also cause sore nipples. When baby cries, can you see if his tongue is able to reach past his lower lip? If baby’s tongue appears heart-shaped, it could be a short or restricted frenulum (tongue-tie) that prevents a good latch-on. Contact a La Leche League Leader if your baby does not seem to be latching on well.
Flat or inverted nipples can make it difficult for baby to grasp your breast in his mouth and properly latch on. With proper latch-on, your baby’s sucking can effectively draw out flat or inverted nipples. Gentle pumping or special exercises are sometimes recommended to draw the nipple out. If you received IV fluids for several hours during the birth process, this can be a cause of edema (swelling) in the breast and nipple. Reverse Pressure Softening can help create a softer nipple/areola that baby can grasp. Reverse Pressure Softening involves using gentle finger pressure around the base of the nipple. This temporarily moves some of the swelling slightly backward and upward into the breast. This technique is also helpful in preventing sore nipples if your breasts become engorged (swollen and uncomfortable) when your milk supply comes in several days after birth, making it difficult for baby to latch on comfortably.
This technique is also helpful in preventing sore nipples if your breasts become engorged (swollen and uncomfortable) when your milk supply comes in several days after birth, making it difficult for baby to latch on comfortably.
Removing baby from the breast without breaking the suction first can be painful and cause damage to sensitive breast tissue. If baby is latched on and sucking well, he will end the feeding himself by letting go of the breast or releasing the nipple as he falls asleep. Allowing baby to determine the end of the feeding will ensure that he is getting the right balance of foremilk at the beginning of the feed, which is more watery and quenches baby’s thirst, and hindmilk at the end of the feed, which is creamy milk that is higher in calories and satisfies baby’s hunger. If you decide to take baby off the breast before he is finished, you can break the suction by pressing down on your breast near baby’s mouth, pulling down on baby’s chin, or inserting your finger into the corner of baby’s mouth.
Personal care practices may lead to nipple soreness. Avoid bras that are too tight and put pressure on your nipples. Be vigilant about thorough rinsing of nursing bras to be sure any laundry detergent residue is removed. Soap, shampoo, body wash, and alcohol can dry your nipples. Take care when applying cologne, deodorant, hair spray, or powder near your nipples. When bathing, rinsing breasts with clear water is all that is needed to keep your breasts and nipples clean.
When your nipples are sore you can gently apply your own milk or an emollient that is safe for the baby to ingest, such as HPA® Lanolin. Either of these can be very soothing. Contact a La Leche League Leader for suggestions.
Be aware that more than one cause can be contributing to nipple soreness at the same time. Avoid limiting the length of nursing sessions, a practice that is mistakenly thought of as a way to avoid sore nipples. Instead, aim to coordinate optimal positioning with careful personal care practices, and contact a La Leche League Leader for helpful tips.
While the cause of sore nipples is being determined and corrected, continued breastfeeding is important. When baby is latched on well with your nipple deep in his mouth, the nipple is protected from further damage. You may want to try one or more of these comfort measures while the cause of your sore nipples are being corrected.
Vary nursing positions—cradle hold, cross cradle hold, football (clutch) hold, and lying down—in order to vary the position of baby’s mouth on your breast. (For information on various nursing positions, contact an LLL Leader for assistance.)
Begin to nurse on the least sore side until the letdown occurs, then gently switch baby to the other breast, paying careful attention to good positioning and latch-on. Some mothers use relaxation breathing until their milk lets down.
Express a little milk or colostrum onto your nipples after nursing. In many cultures, human milk’s antibacterial properties are used to treat skin irritations. However, this is not recommended when soreness is due to thrush, which is a yeast infection of the nipples.
However, this is not recommended when soreness is due to thrush, which is a yeast infection of the nipples.
When your nipples are sore, apply some of your own milk on your nipples. Your milk has healing properties to relieve soreness. Also, a small pea-sized portion of ultrapure modified lanolin, such as HPA® Lanolin, between clean fingertips and apply to the nipple and areola. Gently pat it on: do not rub it in. It does not need to be removed before feedings. This provides a moisture barrier that will slow down the loss of internal moisture, which is vital to healthy, supple skin, eases discomfort, and promotes healing without scab formation. This process is known as “moist wound healing.” Gel pads may provide relief from soreness and promote healing.
Lanolin or gel pads are not recommended if you have a yeast infection.
If the pressure of your clothing or your bra causes further discomfort for your nipples, apply ultrapure lanolin after feedings to help soothe, protect, and heal nipples, then use breast shells with large openings.
In most cases, sore or cracked nipples are no longer painful once good positioning and latch on are achieved. It is rarely necessary to discontinue breastfeeding. The many benefits to both baby and mother make continuing to breastfeed worthwhile.
It is not typically recommended any more that mothers dry sore nipples with a hair dryer or use a sun lamp. These practices have been shown to dehydrate skin further and cause additional damage to tender nipple tissue.
Sore or cracked nipples when breastfeeding
If you get sore nipples when breastfeeding, it's usually because your baby is not positioned and attached properly at the breast.
It's important not to stop breastfeeding. With help, feeding should quickly become more comfortable again.
Get help early for sore nipples
If you find 1 or both nipples hurt at every feed, or your nipples start to crack or bleed, it's important to get help from your midwife, health visitor or breastfeeding supporter as soon as you can.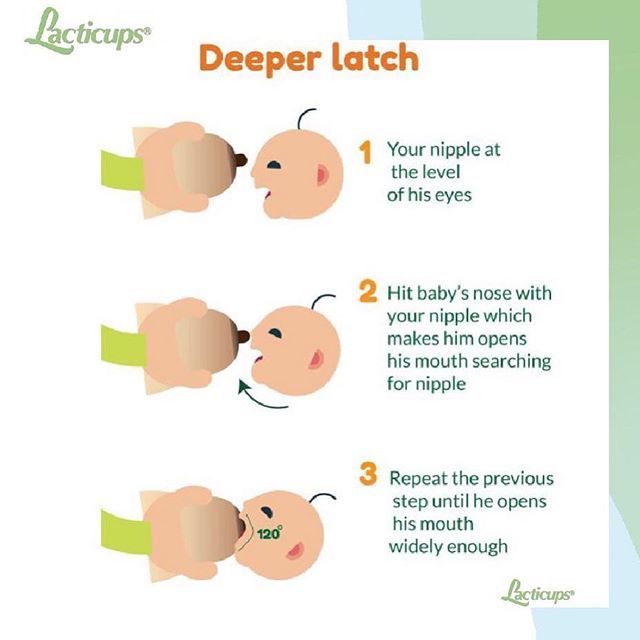
They can watch as you feed your baby and help you get them correctly positioned and attached to the breast.
When your baby is effectively attached, your nipple rests comfortably against the soft palate at the back of their mouth.
If your baby is poorly attached to the breast, the nipple is nearer the front of their mouth and can be pinched against the hard palate, causing pain.
Flattened, wedged or white nipples at the end of a feed are a sign your baby may not be properly attached. Your baby may also seem unsettled after feeds.
Having sore nipples when you're trying to breastfeed a new baby can be stressful and upsetting.
Try to carry on breastfeeding or express milk by hand if you can, and ask for help early.
Learn more about expressing milk by hand
Self-help tips for sore nipples
Bear in mind that self-help tips will not be effective if your baby is poorly attached during breastfeeds.
But you may find it helps to:
- change breast pads at each feed (if you're using them) – if possible, use pads without a plastic backing
- wear a cotton bra so air can circulate
- keep feeding your baby for as long as they want – keeping breastfeeds short to "rest" your nipples will not ease nipple pain and could affect your milk supply
- avoid using nipple shields (a thin, protective cover worn over your nipple as you breastfeed) or breast shells (a hard, protective cover worn inside your bra) – these will not improve your baby's attachment to the breast
If your nipples start to crack, try dabbing a little expressed breast milk onto them after feeds.
Important
Get help early if your nipples are cracked or bleeding, as this increases your risk of getting an infection in your nipple.
If nipple pain does not improve
If your baby is properly positioned and attached at the breast during feeds and your nipples are still sore, ask your midwife, health visitor or breastfeeding supporter for help.
There may be an underlying problem, such as an infection like thrush.
Find out more about breastfeeding and thrush
Video: How do I know if my baby is properly latched?
In this video, a midwife talks about how to check if your baby is latched on properly when breast feeding.
Media last reviewed: 4 October 2022
Media review due: 4 October 2025
Page last reviewed: 8 November 2022
Next review due: 8 November 2025
Cracked nipples | Medela
Amir, L.H. ABM Clinical Protocol #4: Mastitis, Revised March 2014. Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Jacobs, A. et al. S3-Guidelines for the Treatment of Inflammatory Breast Disease during the Lactation Period: AWMF Guidelines, Registry No. 015/071 (short version) AWMF Leitlinien-Register Nr. 015/071 (Kurzfassung). Geburtshilfe Frauenheilkd . 73, 1202–1208 (2013). - Jacobs A. et al., "Recommendations S -3 for the management of inflammatory breast disease during breastfeeding: guidelines AWMF , registration number 015/071 (abbreviated version)" Leitlinjen- Registration number 015/071 (Kurzfassung). Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding handbook for physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
- American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
Lawrence , R . A . & nine0004 Lawrence , R . M . Breastfeeding : a guide for the medical profession ( Elsevier Mosby , Maryland Heights , MO , 2011). - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
McClellan, H.L. et al. Infants of mothers with persistent nipple pain exert strong sucking vacuums. Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." nine0004 Pediatrics 97, 1205–1209 (2008).
Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." nine0004 Pediatrics 97, 1205–1209 (2008).
McClellan, H.L. et al. Breastfeeding frequency, milk volume, and duration in mother-infant dyads with persistent nipple pain. Breastfeed Med 7, 275–281 (2012). — McClellan H.L. et al., "Breastfeeding frequency, milk quantity and duration of feedings in case of persistent sore nipples in the mother", Brestfeed Med (Breastfeeding Medicine) 7, 275–281 (2012). nine0004
McClellan, H.L. et al. Nipple pain during breastfeeding with or without visible trauma. J Hum Lact 28, 511–521 (2012). — McClellan H.L. et al., "Nipple pain during breastfeeding with or without visible lesions." J Hum Lakt (Journal of the International Association of Lactation Consultants" 28, 511–521 (2012).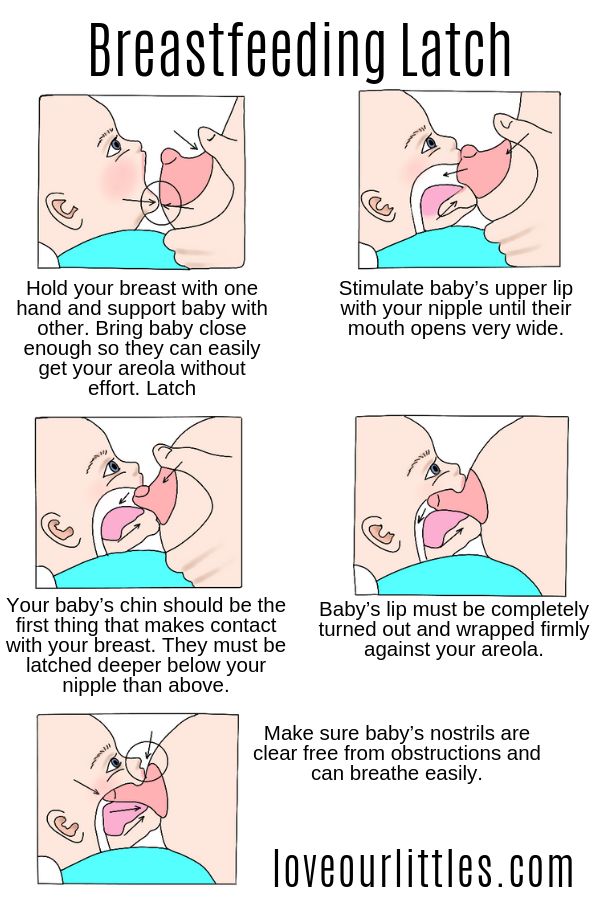
Hale, T.W., & Rowe H.E., Medications and mothers' Milk 2014 (Hale Publishing, Plano, 2014). - Hale T . and Row X . and ., " medicinal Preparations in Maternal milk ". Publishing Hale
Nursing nipple care | Breast Care
Breastfeeding is good for you and your baby, but it can be a real challenge for the nipples. Check out our tips and tricks to help reduce the pain.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
A mother of three, Sioned Hilton has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians. nine0011
In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians. nine0011
New mothers often hear: "Breastfeeding doesn't have to be painful." However, in the early days, many are faced with the opposite.
During pregnancy, most women's nipples enlarge and become more sensitive. When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
Feedings can be prolonged for a long time, sometimes up to an hour, and the child may ask to be breastfed up to 13 times a day. nine0248 1 This sucking, pressure and saliva of the baby can cause sore nipples.
Remember how your lips crack in the wind and sun. The more often you lick them, the more they will dry and become inflamed. Therefore, lips require good hydration to soften, protect and speed up the healing of cracks. The same thing happens with nipples.
However, sore nipples usually don't last more than a couple of weeks and go away as your baby and your breasts get used to breastfeeding. It is important to start nipple care as early as possible to prevent the situation from worsening. Therefore, if your nipples become very inflamed, crack or bleed, contact your doctor as soon as possible. nine0248 2
Prevention is better than cure, so check out our tips.
Check your baby's latch on
Correct latch is the key to pain-free breastfeeding. When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
For the first few days, see a lactation consultant or specialist to check for proper latch. He will be able to give you advice on how to solve problems and recommend other feeding positions that will make it less painful for you to feed your baby. nine0011
nine0011
Check tongue frenulum
Tongue frenulum (ankyloglossia) occurs in 4-11% of
newborns. 4 At the same time, the strip of skin with which the tongue is attached at the bottom of the mouth - the so-called frenulum - is too short. A child with a shortened frenulum will not be able to open his mouth wide enough to latch onto the breast well, and his tongue will not cover the lower gum when sucking. As a result, the baby will be nervous, and your nipples may become inflamed.
The doctor or lactation consultant must examine the baby to make this diagnosis. The problem of a shortened bridle is solved by a simple undercutting procedure. It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. nine0248 5
Less common in children is a short frenulum of the upper lip. In this case, it is necessary to dissect the skin that connects the upper lip to the gum.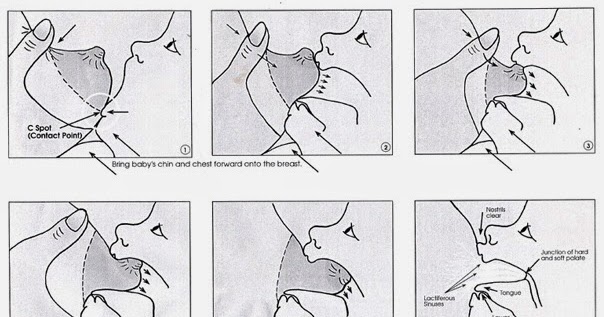 A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
Breastfeeding Nipple Tips
- Wash your breasts with water only when you shower or bathe. Small bumps on the areola (Montgomery's glands) secrete oil that moisturizes and protects your nipples. Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6
- Pat the nipples gently with a soft towel or let them air dry. In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past! nine0288
- Do not wash breasts or nipples before feeding. The bacteria found on the surface of the breast actually help the baby's intestinal microflora to develop. 7
- Fresh breast milk helps to heal cracked nipples, 8 so rub a few drops of milk into them before and after feeding.

- Change your bra pads often if they get wet. This will reduce the risk of bacterial and fungal infections, including thrush. nine0248 6
- It is not necessary to increase the intervals between feedings to give the nipples a "rest". For a baby to be healthy and grow well, it needs to be fed on demand. Remember, frequent feeding stimulates and maintains milk production, so keep feeding despite the pain. 9
Healthy teat care products
- Pure lanolin teat cleaner, a natural product derived from sheep's wool. It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding. nine0288
- Hydrogel Pads* can be applied to sore nipples to relieve pain while feeding and help promote healing. They can even be stored in the refrigerator to enhance the soothing cooling effect.
- Breast pads* fit inside a bra. They help prevent nipple irritation from clothing and have air holes to help nipples heal.

- Nursing Bras** are made from breathable material such as cotton or a special fabric that dries quickly and wicks moisture away from sore nipples. nine0288
- Nursing pads* are special silicone pads that fit over the nipples. They have small holes through which milk flows when you are breastfeeding. The pads help to protect the skin underneath and help the baby to better latch on to the nipple by making the nipple stiffer. Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant. nine0288
When to Seek Medical Care
The soreness should go away as your nipples and baby get used to breastfeeding. It is worth repeating that the main cause of sore nipples is improper grip. If your lactation consultant has not been able to resolve your pain while feeding, see another specialist and a third if necessary.
If nipple pain persists or if you notice unusual symptoms, talk to your doctor. The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. nine0248 2
The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. nine0248 2
Literature
1 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol#26: Persistent pain with breastfeeding. Breastfeeding Medicine. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.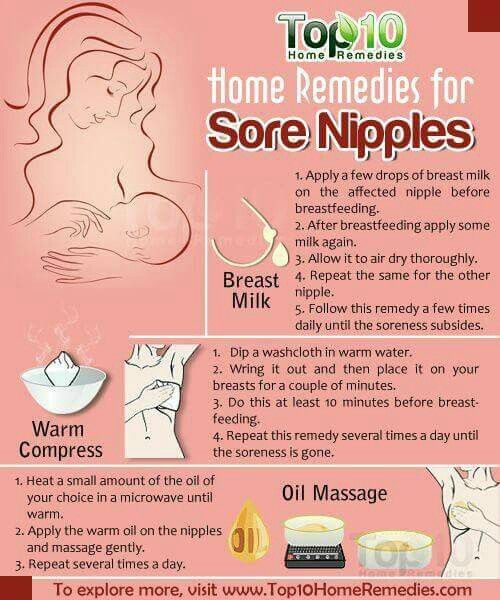
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. nine0004 2007;52(6):638-42. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Segal LM et al. Prevalence, diagnosis, and treatment of ankyloglossia: methodological review. Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033. nine0004
5 O'Shea JE et al. Frenotomy for tongue - tie in newborn infants. The Cochrane Library. 2017. - O'Shea J.I. et al., "Dissection of the frenulum in the newborn", The Cochrane Labrery (Cochrane Library), 2017.
6 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P. S. Pannaraj et al., "Bacterial communities in breast milk and their association with the occurrence and development of the neonatal gut microbiome." JAMA pediatric. 2017;171(7):647-654.
S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P. S. Pannaraj et al., "Bacterial communities in breast milk and their association with the occurrence and development of the neonatal gut microbiome." JAMA pediatric. 2017;171(7):647-654.
8 Mohammadzadeh A et al. The effect of breast milk and lanolin on sore nipples. Saudi medical journal. 2005;26(8):1231-1234. — Mohammedzade A. et al., "Effects of breast milk and lanolin on sore nipples." Saudi Medical Journal. 2005;26(8):1231-1234.