Miscarriage rates first trimester
Miscarriage | March of Dimes
Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Some women have a miscarriage before they know they’re pregnant.
We don’t know all the causes of miscarriage, but problems with chromosomes in genes cause most.
It can take a few weeks to a month or more for your body to recover from a miscarriage. It may take longer to recover emotionally.
Talk to your health care provider about having medical tests before you try to get pregnant again.
Most women who miscarry go on to have a healthy pregnancy later.
What is miscarriage?
Miscarriage (also called early pregnancy loss) is when a baby dies in the womb (uterus) before 20 weeks of pregnancy. For women who know they’re pregnant, about 10 to 15 in 100 pregnancies (10 to 15 percent) end in miscarriage. Most miscarriages happen in the first trimester before the 12th week of pregnancy. Miscarriage in the second trimester (between 13 and 19 weeks) happens in 1 to 5 in 100 (1 to 5 percent) pregnancies.
As many as half of all pregnancies may end in miscarriage. We don’t know the exact number because a miscarriage may happen before a woman knows she’s pregnant. Most women who miscarry go on to have a healthy pregnancy later.
What are repeat miscarriages?
If you have repeat miscarriages (also called recurrent pregnancy loss), you have two or more miscarriages in a row. About 1 in 100 women (1 percent) have repeat miscarriages. Most women who have repeat miscarriages (50 to 75 in 100 or 75 percent) have an unknown cause. And most women with repeat miscarriages with an unknown cause (65 in 100 women or 65 percent) go on to have a successful pregnancy.
What causes miscarriage and repeat miscarriages?
We don’t know what causes every miscarriage. But some miscarriages and repeat miscarriages can be caused by:
Problems with chromosomes
About half of all miscarriages are caused when an embryo (fertilized egg) gets the wrong number of chromosomes.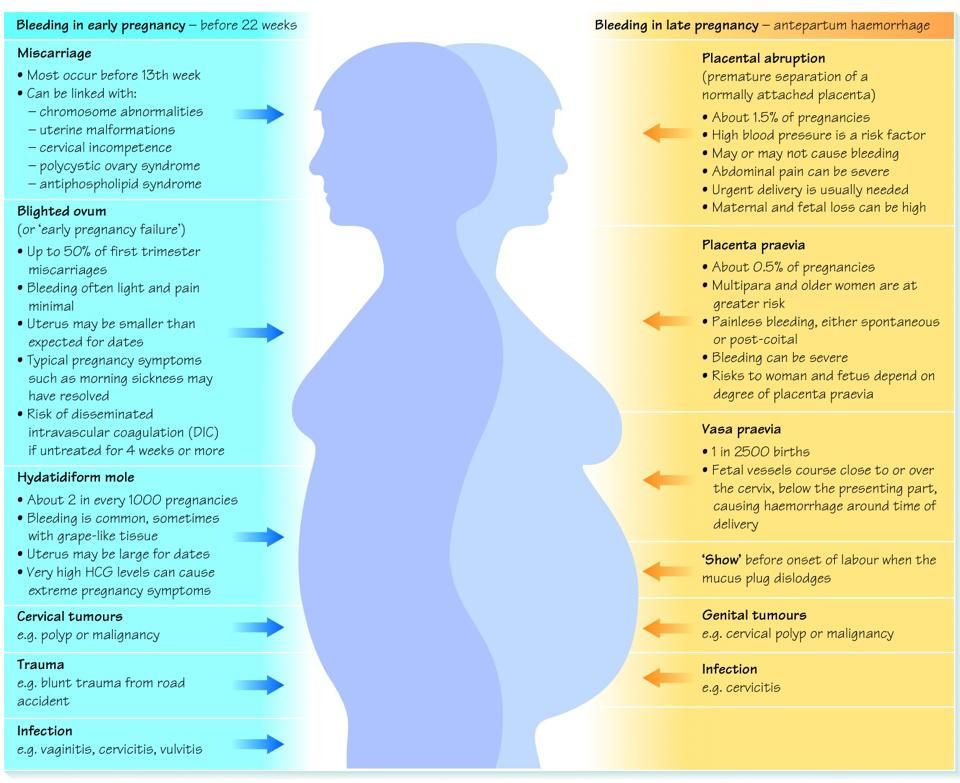 This usually happens by chance and not from a problem passed from parent to child through genes. Chromosomes are the structures in cells that holds genes. Each person has 23 pairs of chromosomes, or 46 in all. For each pair, you get one chromosome from your mother and one from your father. Examples of chromosome problems that can cause miscarriage include:
This usually happens by chance and not from a problem passed from parent to child through genes. Chromosomes are the structures in cells that holds genes. Each person has 23 pairs of chromosomes, or 46 in all. For each pair, you get one chromosome from your mother and one from your father. Examples of chromosome problems that can cause miscarriage include:
- Blighted ovum. This is when an embryo implants in the uterus but doesn’t develop into a baby. If you have a blighted ovum, you may have dark-brown bleeding from the vagina early in pregnancy. If you’ve had signs or symptoms of pregnancy, like sore breasts or nausea (feeling sick to your stomach), you may stop having them.
- Intrauterine fetal demise. This is when an embryo stops developing and dies.
- Molar pregnancy. This is when tissue in the uterus forms into a tumor at the beginning of pregnancy.
- Translocation. This is when part of a chromosome moves to another chromosome.
 Translocation causes a small number of repeat miscarriages.
Translocation causes a small number of repeat miscarriages.
Problems with the uterus or cervix.
The cervix is the opening to the uterus that sits at the top of the vagina. Problems with the uterus and cervix that can cause miscarriage include:
- Septate uterus. This is when a band of muscle or tissue (called a septum) divides the uterus in two sections. If you have a septate uterus, your provider may recommend surgery before you try to get pregnant to repair the uterus to help reduce your risk of miscarriage. Septate uterus is the most common kind of congenital uterine abnormality. This means it’s a condition that you’re born with that affects the size, shape or structure of the uterus. Septate uterus is a common cause of repeat miscarriages.
- Asherman syndrome. If you have this condition, you have scars or scar tissue in the uterus that can damage the endometrium (the lining of the uterus).
 Before you get pregnant, your provider may use a procedure called hysteroscopy to find and remove scar tissue. Asherman syndrome may often cause repeat miscarriages that happen before you know you’re pregnant.
Before you get pregnant, your provider may use a procedure called hysteroscopy to find and remove scar tissue. Asherman syndrome may often cause repeat miscarriages that happen before you know you’re pregnant. - Fibroids (growths) in the uterus or scars from surgery on the uterus. Fibroids and scars can limit space for your baby or interfere with your baby’s blood supply. Before you try to get pregnant, you may need a surgery called myomectomy to remove them.
- Cervical insufficiency (also called incompetent cervix). This is when your cervix opens (dilates) too early during pregnancy, usually without pain or contractions. Contractions are when the muscles of your uterus get tight and then relax to help push your baby out during labor and birth. Cervical insufficiency may lead to miscarriage, usually in the second trimester. To help prevent this, your provider may recommend cerclage. This is a stitch your provider puts in your cervix to help keep it closed.

Infections
Infections, like sexually transmitted infections (also called STIs) and listeriosis, can cause miscarriage. An STI, like genital herpes and syphilis, is an infection you can get from having sex with someone who is infected. If you think you may have an STI, tell your health care provider right away. Early testing and treatment can help protect you and your baby. Listeriosis is a kind of food poisoning. If you think you have listeriosis, call your provider right away. Your provider may treat you with antibiotics to help keep you and your baby safe. Having certain infections may cause miscarriage, but they’re not likely to cause repeat miscarriages.
Are you at risk for a miscarriage?
Some things may make you more likely than other woman to have a miscarriage. These are called risk factors. Risk factors for miscarriage include:
- Having two or more previous miscarriages
- Being 35 or older.
 As you get older, your risk of having a miscarriage increases.
As you get older, your risk of having a miscarriage increases. - Smoking, drinking alcohol or using harmful drugs. If you’re pregnant or thinking about getting pregnant and need help to quit, tell your provider.
- Being exposed to harmful chemicals. You or your partner having contact with harmful chemicals, like solvents, may increase your risk of miscarriage. A solvent is a chemical that dissolves other substances, like paint thinner. Talk to your provider about what you can do to protect yourself and your baby.
Some health conditions may increase your risk for miscarriage. Treatment of these conditions before and during pregnancy can sometimes help prevent miscarriage and repeat miscarriages. If you have any of these health conditions, tell your health care provider before you get pregnant or as soon as you know you’re pregnant:
- Autoimmune disorders.
 These are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake. Autoimmune disorders that may increase your risk of miscarriage include antiphospholipid syndrome (also called APS) and lupus (also called systemic lupus erythematosus or SLE). If you have APS, your body makes antibodies that attack certain fats that line the blood vessels; this can sometimes cause blood clots. If you have APS and have had repeat miscarriages, your provider may give you low-dose aspirin and a medicine called heparin during pregnancy and for a few weeks after you give birth to help prevent another miscarriage. Lupus can cause swelling, pain and sometimes organ damage. It can affect your joints, skin, kidneys, lungs and blood vessels. If you have lupus, your provider may treat you with low-dose aspirin and heparin during pregnancy.
These are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake. Autoimmune disorders that may increase your risk of miscarriage include antiphospholipid syndrome (also called APS) and lupus (also called systemic lupus erythematosus or SLE). If you have APS, your body makes antibodies that attack certain fats that line the blood vessels; this can sometimes cause blood clots. If you have APS and have had repeat miscarriages, your provider may give you low-dose aspirin and a medicine called heparin during pregnancy and for a few weeks after you give birth to help prevent another miscarriage. Lupus can cause swelling, pain and sometimes organ damage. It can affect your joints, skin, kidneys, lungs and blood vessels. If you have lupus, your provider may treat you with low-dose aspirin and heparin during pregnancy. - Obesity. This means you have too much body fat and your body mass index (also called BMI) is 30 or higher.
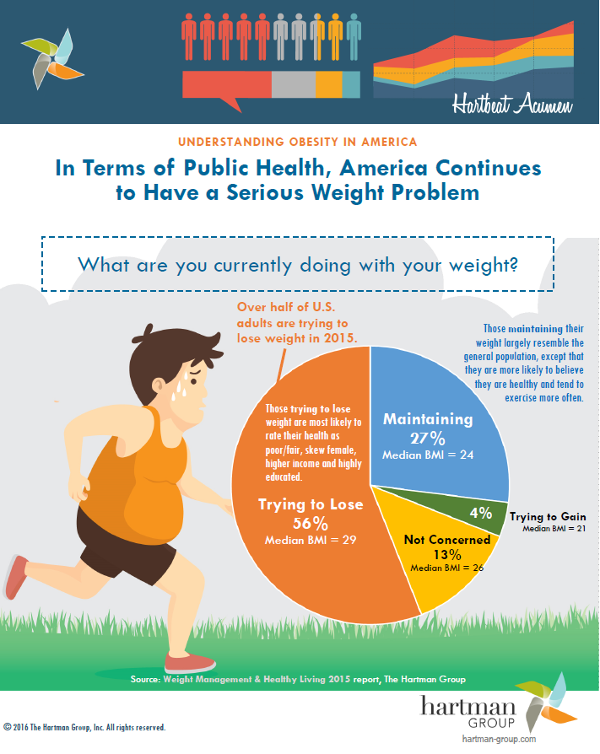
 BMI is a measure of body fat based on your height and weight. If you’re obese, your chances of having a miscarriage may increase. To find out your BMI, go to cdc.gov/bmi.
BMI is a measure of body fat based on your height and weight. If you’re obese, your chances of having a miscarriage may increase. To find out your BMI, go to cdc.gov/bmi. - Hormone problems, like polycystic ovary syndrome (also called PCOS) and luteal phase defect. Hormones are chemicals made by the body. PCOS happens when you have hormone problems and cysts on the ovaries. A cyst is a closed pocket of that contains air, fluid or semi-solid substances. If you’re trying to get pregnant, your provider may give you medicine to help you ovulate (release an egg from your ovary into the fallopian tubes). Luteal phase defect can cause repeat miscarriages. It’s when you have low levels of progesterone over several menstrual cycles. Progesterone is a hormone that helps regulate your periods and gets your body ready for pregnancy. If you have luteal phase defect, your provider may recommend treatment with progesterone before and during pregnancy to help prevent repeat miscarriages.

- Preexisting diabetes (also called type 1 or type 2 diabetes). Diabetes is when you have too much sugar (also called glucose) in your blood. Preexisting diabetes means you have diabetes before you get pregnant.
- Thyroid problems, including hypothyroidism and hyperthyroidism. The thyroid is a butterfly-shaped gland in your neck. Hypothyroidism is when the thyroid gland doesn’t make enough thyroid hormones. Hyperthyroidism is when the thyroid gland makes too many thyroid hormones.
Having certain prenatal tests, like amniocentesis and chorionic villus sampling. These tests have a slight risk of miscarriage. Your provider may recommend them if your baby is at risk for certain genetic conditions, like Down syndrome.
Having an injury to your belly, like from falling down or getting hit, isn’t a high risk for miscarriage. Your body does a good job of protecting your baby in the early weeks of pregnancy.
Your body does a good job of protecting your baby in the early weeks of pregnancy.
You may have heard that getting too much caffeine during pregnancy can increase your risk for miscarriage. Caffeine is a drug found in foods, drinks, chocolate and some medicine. It’s a stimulant, which means it can help keep you awake. Some studies say caffeine may cause miscarriage, and some say it doesn’t. Until we know more about how caffeine can affect pregnancy, it’s best to limit the amount you get to 200 milligrams each day. This is what’s in about one 12-ounce cup of coffee.
What are the signs and symptoms of miscarriage?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
Signs and symptoms of miscarriage include:
- Bleeding from the vagina or spotting
- Cramps like you feel with your period
- Severe belly pain
If you have any of these signs or symptoms, call your provider. Your provider may want to do some tests to make sure everything’s OK. These tests can include blood tests, a pelvic exam and an ultrasound. An ultrasound is a test that uses sound waves and a computer screen to show a picture of your baby inside the womb.
Your provider may want to do some tests to make sure everything’s OK. These tests can include blood tests, a pelvic exam and an ultrasound. An ultrasound is a test that uses sound waves and a computer screen to show a picture of your baby inside the womb.
Many women have these signs and symptoms in early pregnancy and don’t miscarry.
What treatment do you get after a miscarriage or repeat miscarriages?
If you’ve had a miscarriage, your provider may recommend:
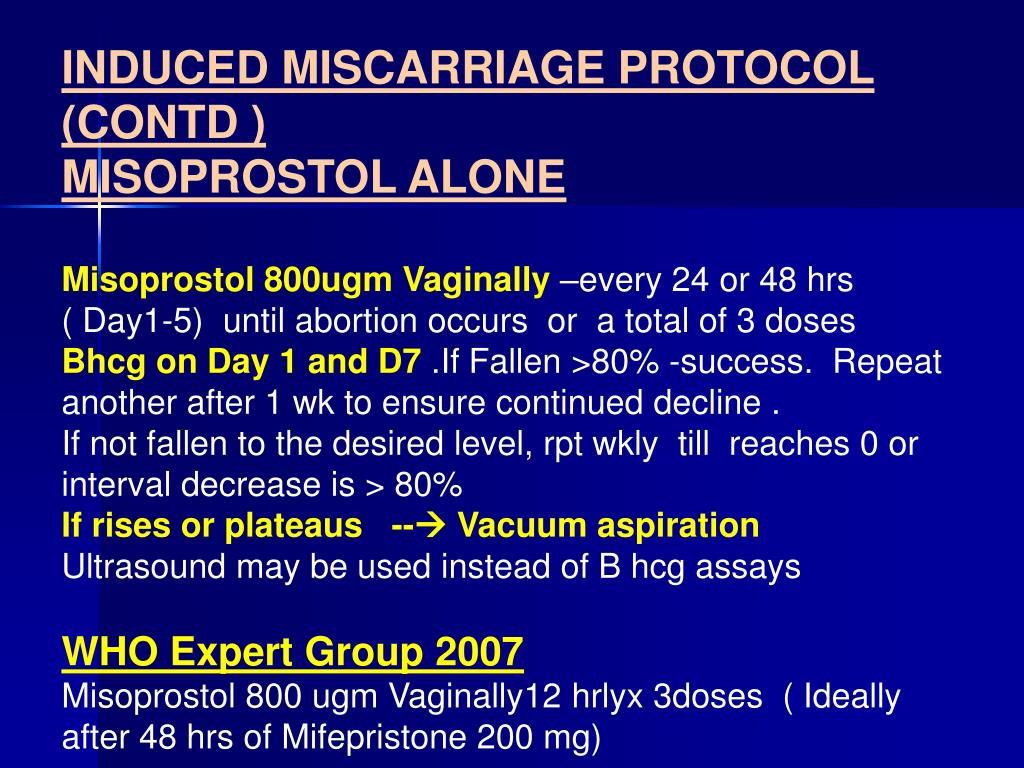
- Dilation and curettage (also called D&C). This is a procedure to remove any remaining tissue from the uterus. Your provider dilates (widens) your cervix and removes the tissue with suction or with an instrument called a curette.
- Medicine. Your provider may recommend medicine that can help your body pass tissue that’s still in the uterus.
Do you need any medical tests after a miscarriage or repeat miscarriages?
If you miscarry in your first trimester, you probably don’t need any medical tests.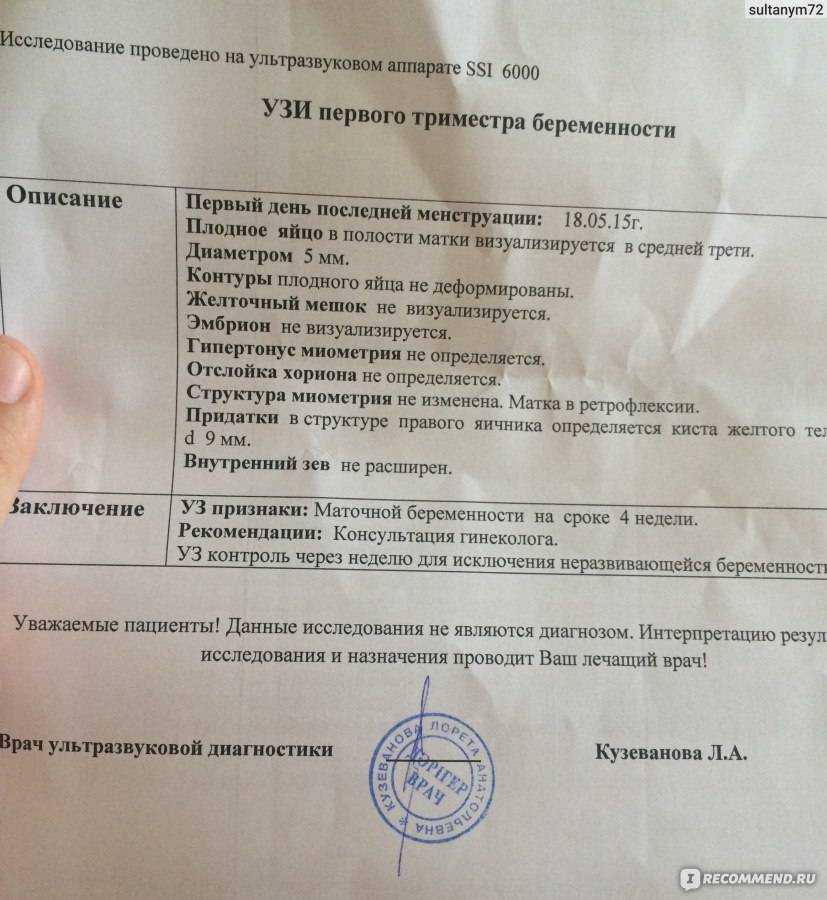 Because we don’t often know what causes a miscarriage in the first trimester, tests may not be helpful in trying to find out a cause.
Because we don’t often know what causes a miscarriage in the first trimester, tests may not be helpful in trying to find out a cause.
If you have repeat miscarriages in the first trimester, or if you have a miscarriage in the second trimester, your provider usually recommends tests to help find out the cause. Tests can include:
- Chromosome tests. You and your partner can have blood tests, like karyotyping, to check for chromosome problems. Karyotyping can count how many chromosomes there are and check to see if any chromosomes have changed. If tissue from the miscarriage is available, your provider can test it for chromosomal conditions.
- Hormone tests. You may have your blood tested to check for problems with hormones. Or you may have a procedure called endometrial biopsy that removes a small piece of the lining of the uterus to check for hormones.
- Blood tests to check your immune system. Your provider may test you for autoimmune disorders like, APS and lupus.

- Looking at the uterus. You may have an ultrasound, a hysteroscopy (when your provider inserts a special scope through the cervix to see your uterus) or a hysterosalpingography (an X-ray of the uterus).
How long does it take to recover from a miscarriage?
It can take a few weeks to a month or more for your body to recover from a miscarriage. Depending on how long you were pregnant, you may have pregnancy hormones in your blood for 1 to 2 months after you miscarry. Most women get their period again 4 to 6 weeks after a miscarriage.
It may take longer to recover emotionally from a miscarriage. You may have strong feelings of grief about the death of your baby. Grief is all the feelings you have when someone close to you dies. Grief can make you feel sad, angry, confused or alone. It’s OK to take time to grieve after a miscarriage. Ask your friends and family for support, and find special ways to remember your baby. For example, if you already have baby things, like clothes and blankets, you may want to keep them in a special place. Or you may have religious or cultural traditions that you’d like to do for your baby. Do what’s right for you.
Or you may have religious or cultural traditions that you’d like to do for your baby. Do what’s right for you.
Certain things, like hearing names you were thinking of for your baby or seeing other babies, can be painful reminders of your loss. You may need help learning how to deal with these situations and the feelings they create. Tell your provider if you need help to deal with your grief. And visit Share Your Story, the March of Dimes online community where you can talk with other parents who have had a miscarriage. We also offer the free booklet From hurt to healing that has information and resources for grieving parents.
If you miscarry, when can you try to get pregnant again?
This is a decision for you to make with your partner and your provider. It’s probably OK to get pregnant again after you’ve had at least one normal period. If you’re having medical tests to try to find out more about why you miscarried, you may need to wait until after you’ve had these tests to try to get pregnant again.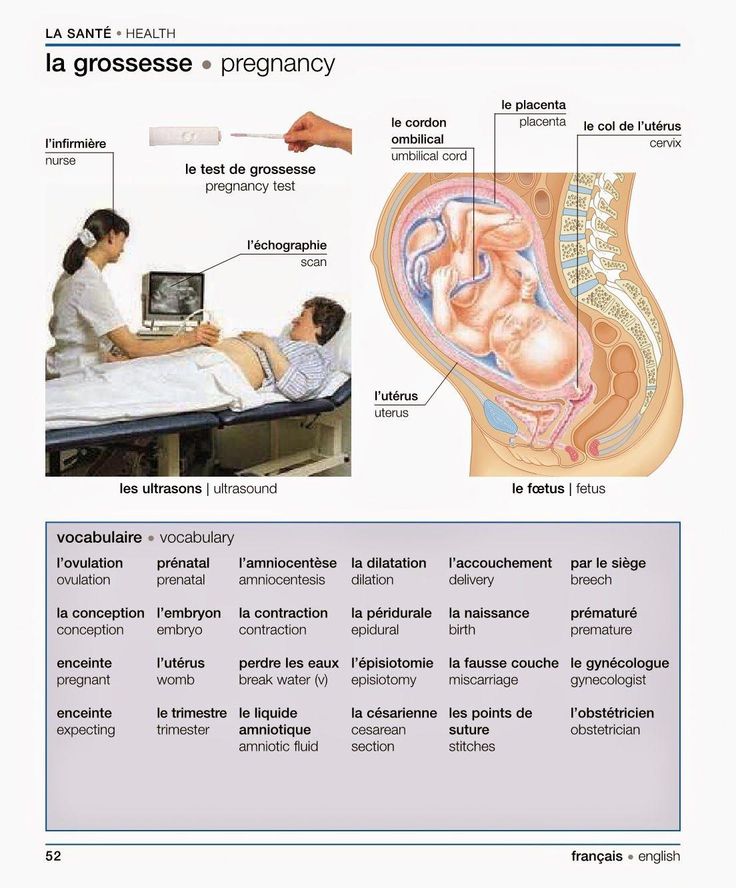
You may not be emotionally ready to try again so soon. Miscarriage can be hard to handle, and you may need time to grieve. It’s OK if you want to wait a while before trying to get pregnant again.
More information
From hurt to healing (free booklet from the March of Dimes for grieving parents)
Share Your Story (March of Dimes online community for families to share experiences with prematurity, birth defects or loss)
Centering Corporation (grief information and resources)
Compassionate Friends (resources for families after the death of a child)
Journey Program of Seattle Children’s Hospital (resources for families after the death of a child)
Lupus Research Alliance: Pregnancy and family planning
Share Pregnancy & Infant Loss Support (resources for families with pregnancy or infant loss)
Last reviewed: November, 2017
Miscarriage Rates by Week: Causes and Risks
Miscarriage Rates by Week: Causes and RisksMedically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
Overview
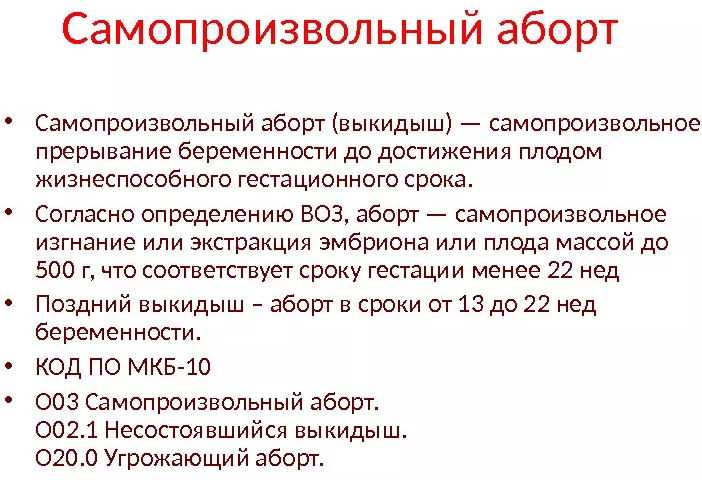
Miscarriage is a word used to describe the early loss of a pregnancy before 20 weeks of pregnancy. It usually happens in the first trimester.
It usually happens in the first trimester.
Unfortunately, between 10 and 15 percent of known pregnancies end in miscarriage.
You may have heard of couples waiting to announce a pregnancy until the risk of having a miscarriage is lower. The further you are into the pregnancy, the less likely you are to miscarry.
Read on to learn about what causes miscarriages and the risk for miscarriage during pregnancy.
Causes
Dr. Kaylen Silverberg, a Texas-based fertility specialist, says miscarriages are very common.
“Women think that when they have one miscarriage, they are doomed to miscarry again,” he says. However, the likelihood of having recurrent miscarriages (at least 2 or 3) is low, only occurring in about 1 percent of women.
Studies have shown an increased risk for miscarriage in women who have had recurrent miscarriages in the past. Conversely, some studies indicate that having a successful pregnancy before a current pregnancy may decrease the risk for miscarriage in the current pregnancy.
Several factors have to be accounted for in these cases, however. This includes maternal age and other medical conditions present. Most doctors will begin to investigate for a cause after you have had two to three losses. This will include reviewing your medical history in detail and performing certain tests.
Here are the five most common miscarriage causes.
Genetics
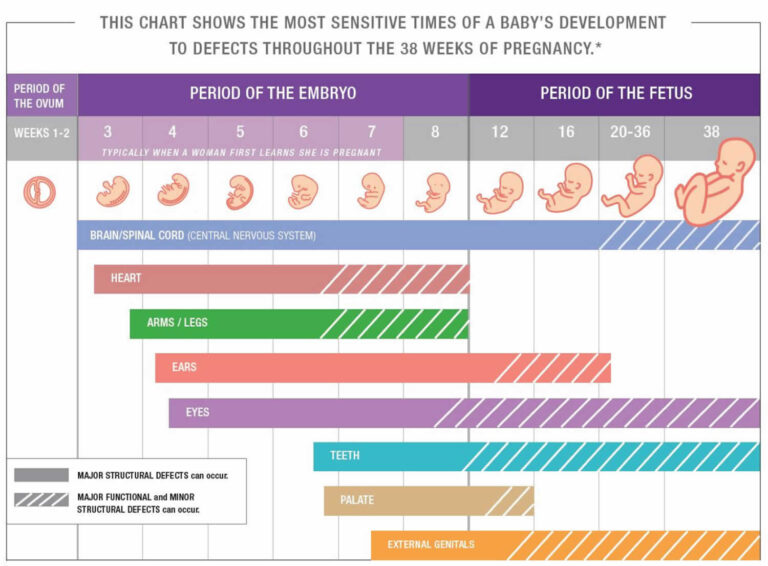
When the sperm and egg meet, the cells come together. They then begin to divide to start forming the genetic material that makes up a person.
Each of us is supposed to have 46 total chromosomes. That’s 23 from one parent and 23 from the other. If something goes wrong when the cells are dividing, a chromosome may be missing or repeated.
About 50 percent of all first trimester miscarriages are because of chromosomal abnormalities. This can occur more frequently in women who are considered advanced maternal age, or greater than 35 years old at pregnancy term.
Infections
Uterus or cervix infections can be dangerous to a developing baby and lead to miscarriage.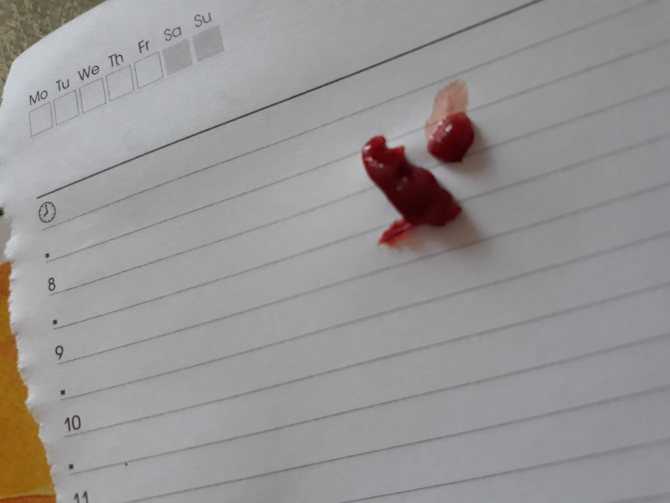 Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Some of these infections include:
- listeria
- parvovirus B19
- toxoplasma gondii
- rubella
- herpes simplex
- cytomegalovirus
Anatomic problems
This refers to defects of the uterus cavity. If a woman’s uterus didn’t form correctly when she was developing, it may be unable to support a healthy pregnancy.
Clotting disorders
Clotting disorders are conditions that cause your body to form more blood clots than normal. Examples include lupus anticoagulant and antiphospholipid syndrome.
In the case of pregnancy, blood clots can form in the placenta. This prevents nutrition and oxygen from getting to the baby-to-be, and prevents waste from being carried away.
Risk rates
The first trimester of pregnancy is considered weeks 0 to 13. About 80 percent of miscarriages happen in the first trimester. Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Weeks 0 to 6
These early weeks mark the highest risk of miscarriage. A woman can have a miscarriage in the first week or two without realizing she’s pregnant. It may even seem like a late period.
Age plays a role in a woman’s risk factor. One study indicated that compared to women younger than 35:
- Women ages 35 to 39 have a 75 percent increase in risk
- Women ages 40 and older are at 5 times the risk
Weeks 6 to 12
Once a pregnancy makes it to 6 weeks and has confirmed viability with a heartbeat, the risk of having a miscarriage drops to 10 percent. According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
Weeks 13 to 20
By week 12, the risk may fall to 5 percent.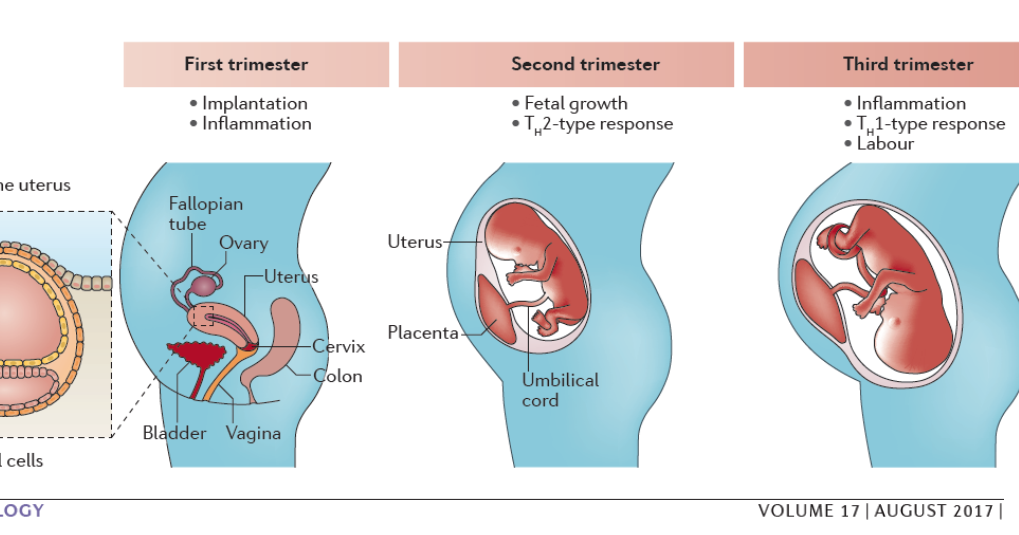 But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
Signs and symptoms
The most common signs of a miscarriage are bleeding and cramping that are felt in the abdomen, pelvis, or lower back.
Some women have spotting (light bleeding) during pregnancy. A few drops or light flow of brown or dark red doesn’t necessarily mean trouble. But call your doctor right away if you see bright red blood, particularly in large amounts.
Cramping can also happen in normal pregnancies. But if it’s severe or occurring more on one side of the pelvis, you should call your doctor.
Prevention
The majority of miscarriages are the result of genetic abnormalities or other health factors that are beyond our control. For that reason, there isn’t a whole lot you can do for prevention.
The best thing you can do is to keep yourself as healthy as possible before trying to conceive and throughout your pregnancy. Here are some tips to staying healthy during pregnancy:
Here are some tips to staying healthy during pregnancy:
- Eat a well-balanced diet.
- Exercise regularly.
- Avoid alcohol, recreational drugs, and cigarette smoking.
- Reduce caffeine to 200 mg or less per day.
- Get regular prenatal visits.
If you’re worried about your risk of having a pregnancy affected by chromosomal issues, you can speak to your doctor about genetic testing before trying to conceive. A blood sample will be taken from one or both partners, and then sent to a laboratory to be evaluated for major genetic disorders. This testing and other evaluation are generally done after someone has recurrent losses.
The takeaway
The experience of a miscarriage can be physically and emotionally painful. But it’s important to remember that it’s not your fault. Talk to trusted friends and family, and ask for help when you need it.
Your doctor may be able to recommend a support group or therapist in your area. There are also many online organizations and support groups like March of Dimes that offer a safe place to share your story and grieve with others.
Share on Pinterest
Rena Goldman is a journalist and editor who lives in Los Angeles. She writes about health, wellness, interior design, small business, and the grassroots movement for campaign finance reform. When she’s not glued to a computer screen, Rena likes to explore new hiking spots in Southern California. She also enjoys walking in her neighborhood with her dachshund, Charlie, and admiring the landscaping and architecture of LA homes she can’t afford. Follow her on Twitter: @ReeRee_writes
Last medically reviewed on October 3, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chromosomal conditions. (2018).
marchofdimes.org/baby/chromosomal-conditions.aspx - Early pregnancy loss: FAQs. (2015).
acog.org/Patients/FAQs/Early-Pregnancy-Loss - Early pregnancy loss: Practice bulletin. (2015).
acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Early-Pregnancy-Loss - Ford HB, et al. (2009). Recurrent pregnancy loss: Etiology, diagnosis, and therapy.
ncbi.nlm.nih.gov/pmc/articles/PMC2709325/ - Maconochie N, et al. (2007). Risk factors for first-trimester miscarriage—results from a UK-population-based case-control study.
obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.2006.01193.x - Miscarriage. (2017).
marchofdimes.org/complications/miscarriage.aspx - Regan L, et al. (1989). Influence of past reproductive performance on risk of spontaneous abortion.
uptodate. com/contents/definition-and-etiology-of-recurrent-pregnancy-loss/abstract/19
com/contents/definition-and-etiology-of-recurrent-pregnancy-loss/abstract/19 - Repeated miscarriages. (2016).
acog.org/Patients/FAQs/Repeated-Miscarriages - Tong S, et al. (2008). Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit.
ncbi.nlm.nih.gov/pubmed/18310375 - Tulandi T. (2018). Patient information: Miscarriage (beyond the basics).
uptodate.com/contents/miscarriage-beyond-the-basics
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Rena Goldman
Medically Reviewed By
Holly Ernst, PA-C
Share this article
Medically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
related stories
How to Tell if You’re Having a Miscarriage Without Bleeding
When Is the Best Time to Announce Your Pregnancy?
What’s a Chemical Pregnancy?
How Long Does a Miscarriage Last?
Late Miscarriage: Symptoms and Finding Support
Read this next
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
When Is the Best Time to Announce Your Pregnancy?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
If you’re expecting, you might be wondering when it’ll be safe to tell family and friends. Here’s how to decide when to share the news of your…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
A chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
Late Miscarriage: Symptoms and Finding Support
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
It can be devastating to experience a miscarriage in your second trimester. Find support and information here.
READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
Threatened Abortion (Threatened Miscarriage)
Threatened abortion refers to vaginal bleeding during the first 20 weeks of pregnancy. Learn about its symptoms, risk factors, and diagnosis.

READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
ᐈ Threatened miscarriage - Reproductive medicine, gynecology, pregnancy monitoring, urology
Laser treatment and vaginal rejuvenation
Read more
Once again about hormones or the list of must-haves for the week
Read more
A visit to the urologist. For or Against?
For or Against?
Read more
Preservation of reproductive health
Read more
Pregnancy with uterine fibroids
Read more
Practical skills in examining infertile couples
Read more
Pregnancy with endometriosis: Modern view
Read more
Breast cancer
Read more
varicocele and violation of spermatogenesis
Read more
Secretary and obstructive infertility in men
Read more (KOS)
More
Miscarriage. What is the reason?
More
Hysteroscopy and its role in the treatment of infertility
Read more
Why you can’t get pregnant
Read more
How to calculate the gender of the child before conception
Read more
The obstruction of the uterine pipes
Read ovary hypermostimulation syndrome: modern views on the problem
Read more
Pregnancy with endometriosis - a modern view
Read more
Immunological infertility and the role of antisperm antibodies in it
More
What is cervical pathology?
Read more
Natural cycle IVF: pros and cons
Read more
Practical skills in the examination of infertile couples
Read more
Artificial insemination
Skin whitening and laser removal Read more
Read more
Unable to get pregnant.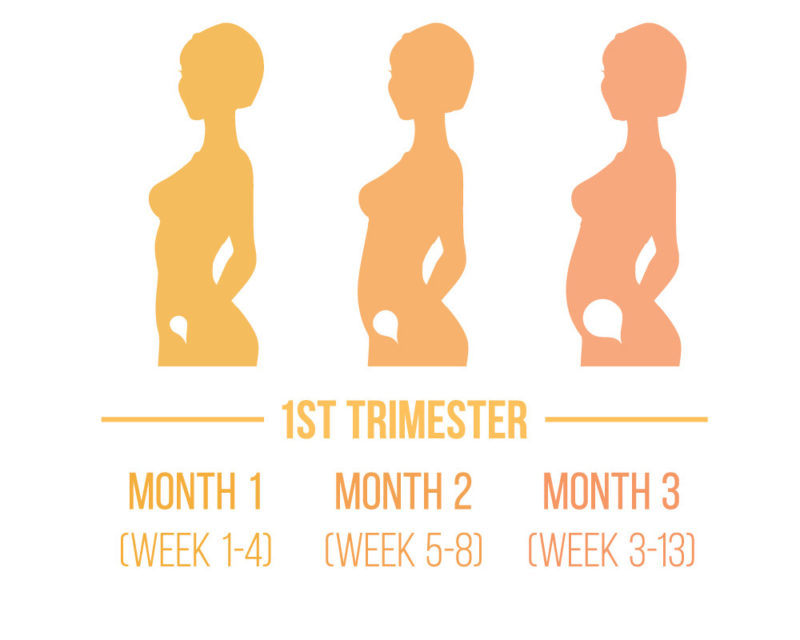 Where to run? Where to begin?
Where to run? Where to begin?
More
What prospective parents need to know (most popular questions)
More
Endometriosis. Some important questions
Read more
Prolactin increase. Should I be afraid?
Read more
Obstruction of the fallopian tubes, what to do next?
More
Human papillomavirus. Basic information
Read more
KAMALIYA: “I consider Vladimir Kotlik the godfather of my children”
Read more
Infertility and cancer: why men should definitely visit a reproductive specialist
Read more
Sex, children, rock and roll: reproductive specialists on what can increase the chances of IVF
Read more
Portrait of a female doctor: 5 signs of good gynecologist
Read more
Is sex during IVF a good idea?
Read more
Never say never.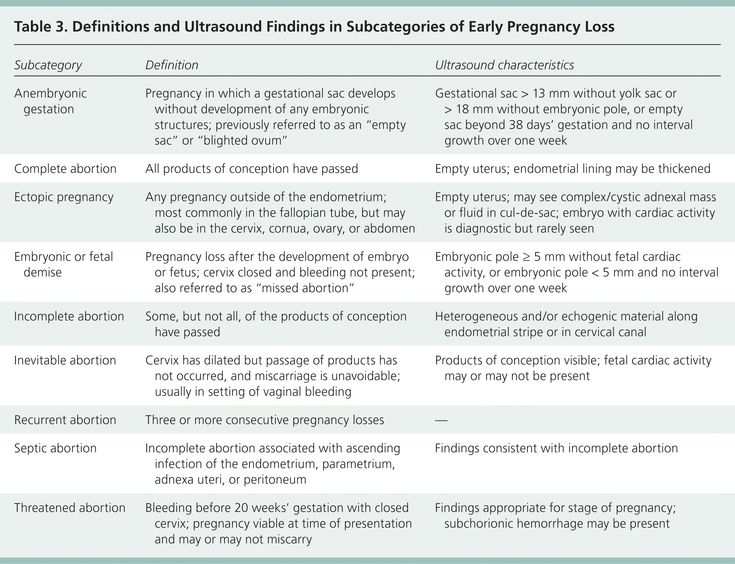 Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
More details
How to plan health, longevity and parenthood: practical advice from doctors for 2020
More details
From virus to cancer: hidden threats to women's health
More details
Threatened abortion
Reproductive health of teenage girls: what children and their parents need to knowRead more
Life is like magic: how to believe in a miracle if you are a pragmatist - a doctor's story
Read more
Beautiful skin in youth is the key to happy motherhood
Read more
Charged for success. What determines the effectiveness of ART
More
Why do not all eggs become embryos?
More details
Maxim Gapchuk in "Mother and child" ambitious future
More details
Unsuccessful IVF, how to survive? Expert advice
Read more
What should an Rh-negative woman know? nine0003
Read more
9 tips for future parents
Read more
Eco: Modern methods and approaches in the treatment of female infertility
Read more
icSI: Men's infertility - NOT a sentence
Read more
Laparoscopy: Advantages over traditional surgery
Read more
Uterine examination: what you need to know about hysteroscopy
Read more
Artificial intrauterine insemination: the essence of the method, stages and results
Read more
Infertility Diagnostics in men
Read more
10 reasons to contact a man to andrologist
more — what kind of technology is this
More
Premature menopause in men: how to recognize and what is dangerous
More
Why visit a gynecologist for preventive examinations
More details
Laser therapy in gynecology: without anesthesia and pain
More details
Outpatient gynecology - timely seeking qualified help
More details
examinationMore details
Causes and prevention of female infertility
More details
One-day surgery: a modern approach to treatment
3
More details
Pregnancy management: to keep the baby healthy and mother's well-being
More details
Pregnancy after IVF: what future parents need to remember
More details
Anomalies of the uterus and their impact on the onset and carrying of pregnancy.
Read more
Scar on the uterus after caesarean section
Read more
The most common mistakes during pregnancy
Read more
Varicose veins and hemorrhoids during pregnancy
More details
Pregnancy planning (lifestyle)
More details
First aid kit for pregnant women during the war
More details
Periods disappeared during the war. What to do?
More details
Freezing of husband's sperm before the war
More details
A visit to a reproductive specialist during the war
More details
I learned that I was pregnant before the war. What to do? nine0003
Read more
What does vaginal discharge mean
Read more
Why can't I get pregnant?
Read more
How to get pregnant if you don't ovulate?
Read more
Diagnosis of male infertility
Read more
When to see a gynecologist
Read more
Infertility treatment program guide
Read more
What you need to know0003
Read more
You are given a chance.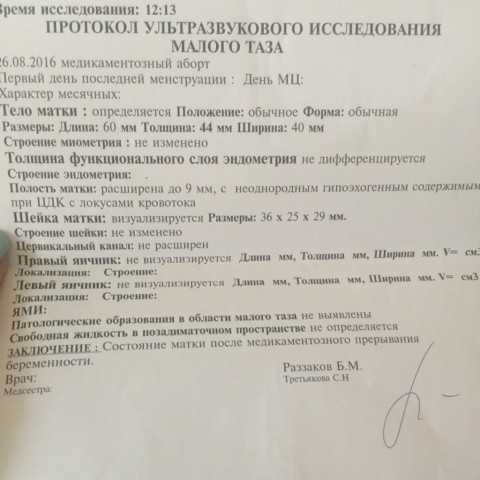 What you need to know about artificial insemination
What you need to know about artificial insemination
More
What causes thrush and why it comes back
More
Threatened miscarriage
will answer frequently asked questions on this topic.
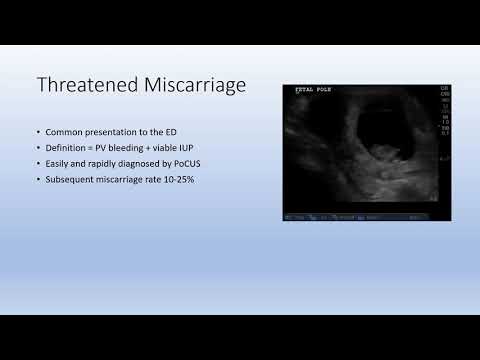
- Inna Igorevna, what is the threat of miscarriage?
Termination of pregnancy from conception to 22 weeks is called spontaneous abortion (miscarriage), and in terms of 28-37 weeks of pregnancy - premature birth. Its interruption in terms from 22 to 28 weeks is referred to as very early preterm birth. The threat of abortion is one of the main problems of obstetrics. According to world statistics, spontaneous miscarriages occur in 15-20% of cases of desired pregnancies. The highest frequency, up to 80%, of threatened miscarriage occurs in the first trimester of pregnancy (from the moment of conception to 14 weeks of pregnancy). nine0003
— What are the reasons? Why might this happen?
The reasons that can lead to a threatened miscarriage are very diverse, but there are cases when it is not possible to establish the true nature of the occurrence of this pathology.
For example, at the earliest stages, the causes of spontaneous abortion are most often malformations of the embryo, chromosomal abnormalities.
At any stage of pregnancy, the threat of miscarriage may be caused by somatic pathology of the expectant mother: thyroid disease, diabetes mellitus and other endocrinopathies; hypertension, kidney disease, the presence of foci of chronic infection, etc. We always focus a woman's attention on the fact that you need to take care of your health even before planning a pregnancy. After all, the presence of gynecological pathology - a violation of the menstrual cycle, an anomaly of development or uterine fibroids, endometriosis, chronic urogenital infection, as well as many other problems of the female genital area can also provoke a threat of termination of pregnancy. nine0003
Many other, both medical and social factors can lead to the threat of abortion:
- use of drugs without taking into account the presence and duration of pregnancy
- acute viral infection,
- stress, bad habits (smoking, alcohol, drugs).
— What symptoms accompany a threatened miscarriage? What are the first signs?
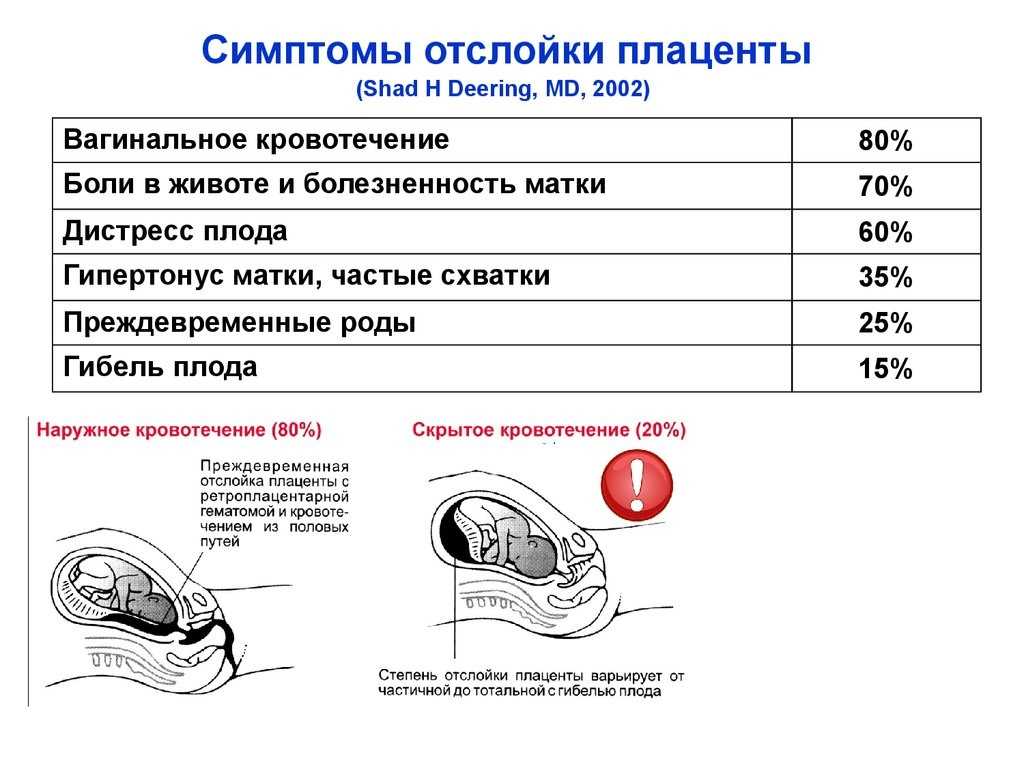
Spontaneous termination of pregnancy is characterized by the appearance of uterine contractions, leading to detachment of the fetal egg and its expulsion from the uterine cavity. nine0003
Most often, the first manifestation of a threatened miscarriage is the appearance of a feeling of heaviness in the lower abdomen, aching pains with a tendency to increase and sometimes have a cramping character.
The next important symptom is the appearance of bloody discharge from the genital tract. They can be combined with a pain syndrome, but they can also appear against the background of "complete well-being", in the absence of pain. Bloody discharge can be scanty, spotting, brownish (clotted blood), moderate to profuse, bright. nine0003
— What should a woman do if she has the above symptoms?
If these clinical symptoms appear, regardless of their severity, you should immediately consult a doctor.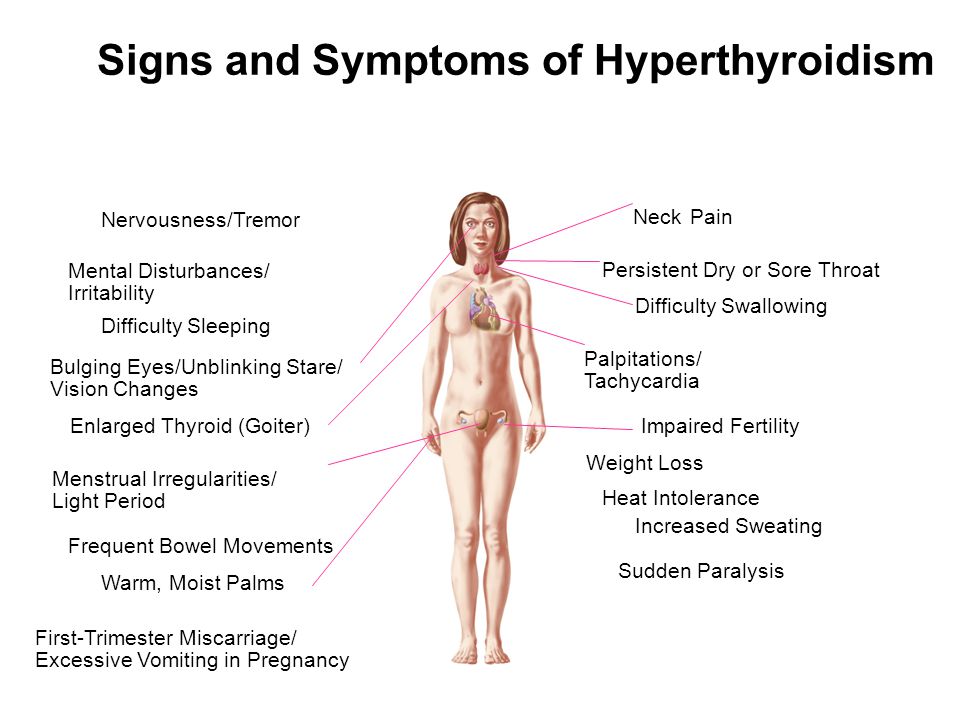
If possible, it is better to call an ambulance.
In a specialized hospital, clinical and laboratory examinations and an examination will be carried out, which will allow a correct assessment of the severity of the threat. After that, a course of adequate therapy will be prescribed: antibacterial (if necessary), hormonal, hemostatic, magnesian or some other. nine0003
After stopping the signs of a threat and confirming the data on the full progression of pregnancy, further observation and supportive therapy, if necessary, is carried out already on an outpatient basis.
The solution to the issue of physical activity, visiting the pool, long trips, sexual life in each case is decided strictly individually. It depends on the reasons that led to the threat of miscarriage. If this is placenta previa or isthmic-cervical insufficiency, or such a threat that requires not only long-term conservative, but also surgical treatment, then the restrictive regimen can be extended up to 37 weeks of pregnancy. nine0003
nine0003
— How do you solve this problem in your maternity hospital? Is there a specialized hospital?
Our obstetrician-gynecologists always try to keep the pregnancy, especially if this pregnancy is desired and planned. Therefore, it is necessary to identify the symptoms of a violation of the course of pregnancy in time and begin treatment.
The Maternity Hospital on Furshtatskaya has developed a number of programs aimed at maintaining pregnancy, starting from the earliest possible dates.
Our Pregnancy Pathology Correction Center (professional name - Department of Pregnancy Pathology) has the latest diagnostic equipment and highly qualified experienced staff, as well as all the necessary facilities that allow you to bear and give birth to a healthy baby. nine0003
- How to get to your hospital?
The Pregnancy Pathology Correction Center will accept you to keep your pregnancy under several conditions, which are best checked with your doctor. Preference for admission is given to those women who conduct their pregnancy at the Center for Gynecology and Obstetrics or have a contract for childbirth.
Our Center for Gynecology and Obstetrics has pregnancy management programs for different periods. Patients always have the opportunity to contact their doctor and discuss all issues related to their beautiful position. nine0003
The doctor told at what age they will give birth in 10 years
The desire to fulfill the dream of motherhood will be as long as the world exists. A woman of the 21st century stands on the same level as a man in achieving career growth. It is only after reaching full perfection in the business sphere that most couples think about having a baby. This, of course, is not the only reason for postponing the birth of children until a later time, but the trend towards an increase in the age of women who decide to become mothers is worldwide. nine0003
Pregnancy and childbirth after 35
The desire to fulfill the dream of motherhood will be as long as the world exists. A woman of the 21st century stands on the same level as a man in achieving career growth.