How to relieve pressure from breast milk
Causes and Tips for Relief
What is breast engorgement?
Breast engorgement is breast swelling that results in painful, tender breasts. It’s caused by an increase in blood flow and milk supply in your breasts, and it occurs in the first days after childbirth.
If you’ve decided not to breastfeed, you may still experience breast engorgement. It can happen in the first few days after delivery. Your body will make milk, but if you don’t express it or nurse, the milk production will eventually stop.
Breast engorgement is the result of increased blood flow in your breasts in the days after the delivery of a baby. The increased blood flow helps your breasts make ample milk, but it can also cause pain and discomfort.
Milk production may not occur until three to five days postpartum. Engorgement may occur for the first time in the first week or two after delivery. It can also reoccur at any point if you continue to breastfeed.
Not producing enough milk? Here are 5 tips to increase breast milk production.
Certain conditions or events may make you more likely to experience the swollen fullness that’s commonly associated with breast engorgement. These causes include:
- missing a feeding
- skipping a pumping session
- creating an overabundance of milk for the baby’s appetite
- supplementing with formula between nursing sessions, which may reduce nursing later
- weaning too quickly
- nursing a baby that’s ill
- difficulty with latching and sucking
- not expressing breast milk when it first comes in because you don’t plan to breastfeed
The symptoms of breast engorgement will be different for each person. However, breasts that are engorged may feel:
- hard or tight
- tender or warm to touch
- heavy or full
- lumpy
- swollen
The swelling may be contained to one breast, or it may occur in both. Swelling can also extend up the breast and into the nearby armpit.
The veins running under the breast’s skin may become more noticeable. This is a result of the increased blood flow, as well as the tightness of the skin over the veins.
This is a result of the increased blood flow, as well as the tightness of the skin over the veins.
Some with breast engorgement may experience a low-grade fever and fatigue in the first days of milk production. This is sometimes called a “milk fever.” You can continue to nurse if you have this fever.
However, it’s a good idea to alert your doctor to your increased temperature. That’s because some infections in the breast can cause fever, too, and these infections need to be treated before they become bigger issues.
Mastitis, for example, is an infection that causes inflammation of the breast tissue. It’s most commonly caused by milk trapped in the breast. Untreated mastitis can lead to complications such as a collection of pus in the clogged milk ducts.
Report your fever and any other symptoms you’ve recently experience to your doctor. They will want you to monitor for signs of an illness or infection so you can seek immediate treatment.
The treatments for breast engorgement will depend on whether you’re breastfeeding or not.
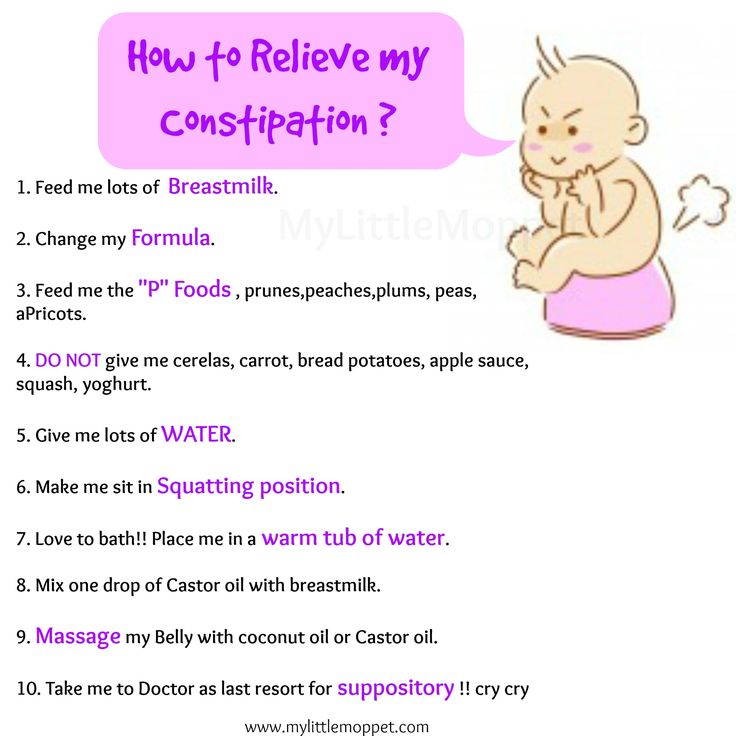
For those who are breastfeeding, treatments for breast engorgement include:
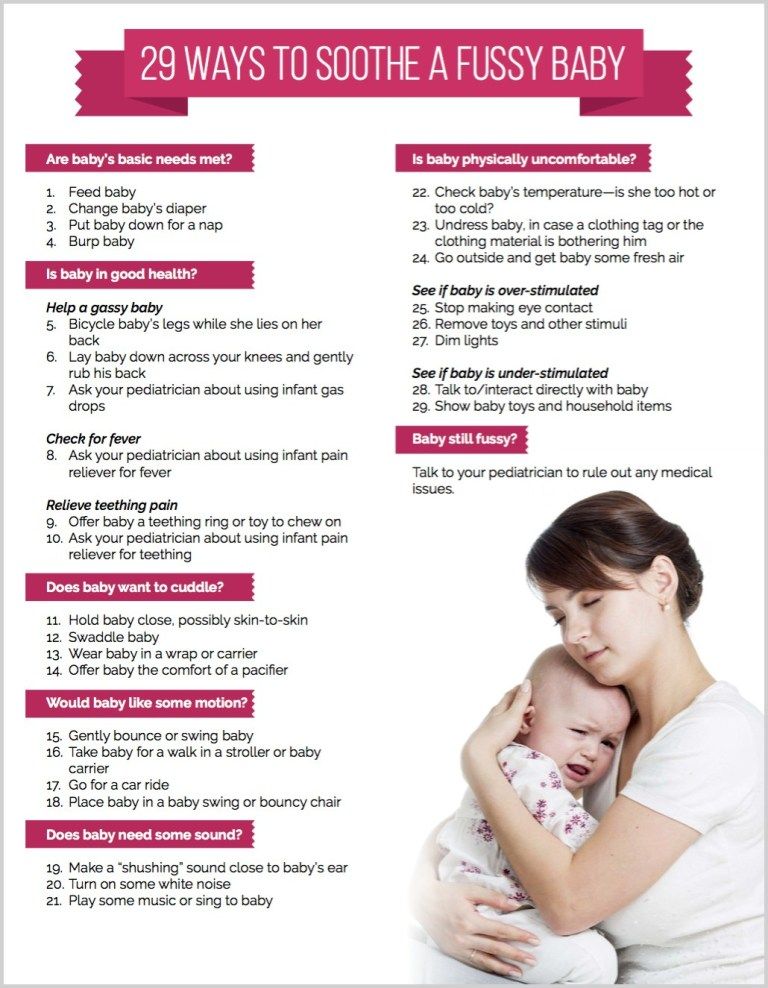
- using a warm compress, or taking a warm shower to encourage milk let down
- feeding more regularly, or at least every one to three hours
- nursing for as long as the baby is hungry
- massaging your breasts while nursing
- applying a cold compress or ice pack to relieve pain and swelling
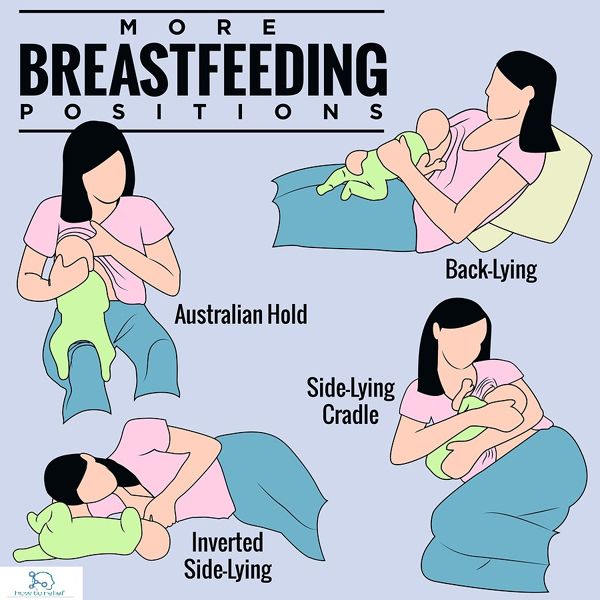
- alternating feeding positions to drain milk from all areas of the breast
- alternating breasts at feedings so your baby empties your supply
- hand expressing or using a pump when you can’t nurse
- taking doctor-approved pain medication
For those who don’t breastfeed, painful engorgement typically lasts about one day. After that period, your breasts may still feel full and heavy, but the discomfort and pain should subside. You can wait out this period, or you can use one of the following treatments:
- using a cold compress or ice packs to ease swelling and inflammation
- taking pain medication approved by your doctor
- wearing a supportive bra that prevents your breasts from moving significantly
You can’t prevent breast engorgement in the first days after giving birth. Until your body knows how to regulate your milk production, you may overproduce.
Until your body knows how to regulate your milk production, you may overproduce.
However, you can prevent later episodes of breast engorgement with these tips and techniques:
- Feed or pump regularly. Your body makes milk regularly, regardless of nursing schedule. Nurse your baby at least every one to three hours. Pump if your baby isn’t hungry or you’re away.
- Use ice packs to decrease supply. In addition to cooling and calming inflamed breast tissue, ice packs and cold compresses may help decrease milk supply. That’s because the cool packs turn off the “let down” signal in your breasts that tells your body to make more milk.
- Remove small amounts of breast milk. If you need to relieve the pressure, you can hand express some breast milk or pump a bit. Don’t pump or express too much, however. It could backfire on you, and your body may end up trying to produce more milk to make up for what you just removed.
- Wean slowly. If you’re too quick to stop nursing, your weaning plan may backfire. You could end up with too much milk. Slowly wean your child so your body can adjust to the decreased need.
If you don’t breastfeed, you can wait out breast milk production. In a matter of days, your body will understand it doesn’t need to produce milk and the supply will dry up. This will stop the engorgement.
Don’t be tempted to express or pump milk. You’ll signal to your body that it needs to produce milk, and you may prolong discomfort.
Breast engorgement is swelling and inflammation that occurs in your breasts because of increased blood flow and milk supply. In the days and weeks after giving birth, your body will begin to produce milk.
Until your body knows how much you need, it may produce too much. This can lead to breast engorgement. Symptoms include hard, tight breasts that are swollen and tender. Regular nursing or pumping can help prevent breast engorgement.
If you continue to experience the painful swelling of breast engorgement, reach out to a lactation consultant or a lactation support group at your local hospital. Both of these resources can help you with your questions and provide support.
Also, call your doctor if the engorgement doesn’t subside in three to four days or if you develop a fever. They’ll ask you to monitor for other signs that may indicate a more serious problem, such as a breast infection.
Engorged Breasts - avoiding and treating
You are here: Home / Breastfeeding information / Engorged Breasts – avoiding and treating
Engorged breasts are painful. They feel heavy, hard, warm and sensitive —as if they are ready to burst! As well as being painful, engorgement can lead to other breastfeeding problems if not treated. Being able to recognise engorgement will help you to treat it promptly, avoiding complications.
Most mothers experience some engorgement in the first weeks after birth. With changing hormone levels, your breasts swell and enlarge as milk production increases. It may seem as though they are filling up with milk, but engorgement is more than milk storage. Your body directs extra blood and fluids to your breasts to boost milk production. This causes congestion and swelling which will decrease as your body adjusts.
It may seem as though they are filling up with milk, but engorgement is more than milk storage. Your body directs extra blood and fluids to your breasts to boost milk production. This causes congestion and swelling which will decrease as your body adjusts.
Minimizing early engorgement
Treat engorgement to…
When to treat engorgement
After the first few weeks
Causes of engorgement
Treating engorgment
Be sure your baby is sucking effectively
Reverse pressure softening
Keep comfortable
Watch out for signs of mastitis
Minimizing early engorgement
New mothers vary in how engorged their breasts become in the weeks after birth; some experience little engorgement, others describe their breasts as feeling like watermelons!
Try these suggestions
- Breastfeed your baby frequently from birth: at least 8–12 times in 24 hours. Keeping your baby close makes it easier to nurse every hour or two.
- If your baby is sleepy, perhaps from a medicated birth, you may need to wake him and encourage him to nurse.

- Aim to be comfortable while breastfeeding, and learn how to get your baby latched on well.
- If your newborn is unable to breastfeed, hand express frequently until your milk ‘comes in’, then combine with using a hospital-grade electric breastpump to help establish your milk production and relieve engorgement. Your milk can be given to your baby until he is able to nurse.
Treat engorgement to…
Make breastfeeding easier
Even if you feel as though you have lots of milk, engorgement can make it harder for your baby to latch on to your breast and feed well. A poor latch-on can give you sore nipples. Your baby may also have trouble coping with the flow of milk from engorged breasts.
Protect milk production
When milk isn’t removed from your breasts, you will produce less milk. Treating engorgement gives your baby more milk now and helps protect milk production for when your baby is older.
Avoid blocked ducts or mastitis
Engorgement can result in blocked ducts leading to mastitis.
When to treat
Take action to relieve engorgement if your breasts feel firm, hard, shiny or lumpy. When milk is removed, blood circulation improves and swelling reduces. Use the suggestions below to reduce swelling and keep your milk flowing. Many mothers have a slight temperature when their breasts are engorged. Temperatures under 38.4ºC are not usually associated with infection. Keep your baby close and continue breastfeeding.
Engorgement after the first weeks
Treat as outlined below while working out the cause so you can prevent it happening again.
Common causes of engorgement are:
- A missed feed or expressing session.
This can easily happen during holidays and festivities or when visitors arrive. Encourage your baby to feed more often, or express more frequently if you’re apart from your baby. - Feeding a baby on a schedule
Recent research has revealed that mothers vary in how much milk their breasts can store without becoming uncomfortable. Mothers following routines often suffer from engorgement, mastitis and low milk production because their breasts are not drained often enough.
Mothers following routines often suffer from engorgement, mastitis and low milk production because their breasts are not drained often enough. - Expressing milk.
Some books advise expressing to keep milk production one step ahead of a baby’s needs. However, making more milk than your baby needs can increase your risk of engorgement and mastitis, especially if you go for several hours without feeding or expressing. - A baby who is unable or unwilling to nurse well for any reason
Expressing milk frequently until your baby can nurse well will help you maintain milk production and avoid blocked ducts or mastitis. - Weaning from the breast too quickly
If you experience engorgement during weaning, you may need to slow down the process. This will give your breasts time to adjust to the reduced demand for milk. If breastfeeding more often is not an option, try expressing just enough milk to relieve the fullness by hand or pump.
Treating engorgement
Reduce swelling and keep milk flowing:
- Aim to breastfeed every 1½ to 2 hours during the day, and at night every 2–3 hours from the start of one feed to the start of the next.
 Let your baby finish on the first breast before switching to the second
Let your baby finish on the first breast before switching to the second - Avoid using bottles or dummies. If a supplement is needed try using a spoon, flexible feeding cup or syringe.
- Between feeds, apply ice for 15–20 minutes at a time between feeds to reduce swelling. Use an ice pack, crushed ice in plastic bags or bags of frozen vegetables (that can be refrozen several times before being thrown away). Wrap them in a lightweight towel to protect your skin.
- Just before feeding, apply moist warmth to your breasts for up to two minutes to help milk flow. Try a warm wet towel, warm shower or immersing breasts in a bowl of warm water. Then, express to comfort if your baby isn’t ready to feed.
- Use gentle massage from the chest wall toward thenipple area in a circular motion.
Be sure your baby is sucking effectively:
Position your baby with his chest and tummy in full contact with your body. With his cheek in close contact with your breast, your baby can easily tip back his head to latch on. This way he’ll take a large mouthful of breast. Listen for swallowing as he feeds.
This way he’ll take a large mouthful of breast. Listen for swallowing as he feeds.
If your baby is finding it hard to latch on – when your baby bobs his head and licks the nipple, he naturally makes it easier to latch on.
For more information on getting your baby positioned and attached comfortably see here.
Reverse pressure softening
works by moving fluid away from the nipple area.
- Press all five fingertips of one hand around the base of the nipple. Apply gentle steady pressure for about a minute to leave a ring of small dimples on the areola.
- You can also press with the sides of fingers. Place your thumb on one side of the nipple and two fingers on the other side where your baby’s lips will be.
- If this isn’t enough, gently hand express a little milk before feeding to soften the areola. If you choose to use a breastpump, set it to minimum suction.
Keep comfortable:
- Ask your midwife or GP to recommend an over-the-counter, anti-inflammatory medication suitable for breastfeeding mothers to relieve pain and swelling.

- A well-fitting, supportive bra may help. Avoid bras (and underwires) that are tight or put pressure on specific areas of the breast.
- Cold, raw cabbage leaves worn inside a bra can be soothing. Change when they become wilted or after about 2 hours. Use only until swelling goes down as long-term use may reduce milk supply. Stop use if a skin rash or other signs of allergy appear.
Watch out for symptoms of mastitis:
- Inflamed, hot, red or darkened localised areas of your breast, depending on your skin tone. Changes in breast appearance may be harder to spot in darker skin. You may still have engorged breasts without a noticeable red or darkened area.
- Temperature over 38.4ºC or flu-like symptoms.
- Weaning can make a breast infection worse so continue to breastfeed frequently especially on the affected side and treat as for engorgement. Rest and drink fluids. If fever persists, continue breastfeeding and check with your GP as you may need antibiotics.
 More information on mastitis.
More information on mastitis.
Engorgement should improve within a day or two. If not, contact an LLL Leader for further suggestions. You may need to improve your baby’s breastfeeding technique or find ways to reduce your milk supply. These are not difficult problems to solve, especially if treated promptly.
Written by Karen Butler, Sue Upstone & mothers of La Leche League Great Britain
Further Reading
The Womanly Art of Breastfeeding. LLLI. London: Pinter & Martin, 2010.
Beginning Breastfeeding
Comfortable Breastfeeding
Dummies and Breastfeeding
Hand Expression of Breastmilk
Mastitis
My Baby Won’t Breastfeed
Nipple Pain – why and what to do
Positioning and Attachment
Sleepy Baby – why and what to do
This information is available to buy in printed format from our shop
Copyright LLLGB 2016
Filed Under: Breastfeeding information, Common Concerns Tagged With: blocked ducts, engorgement, express, expressing, lumps, mastitis, milk, newborn / beginning breastfeeding, red, reverse pressure softening, swollen
Termination of breastfeeding | Stopping breastfeeding
When is it time to stop breastfeeding and what is the best way to do it? Read our article for useful practical tips on weaning.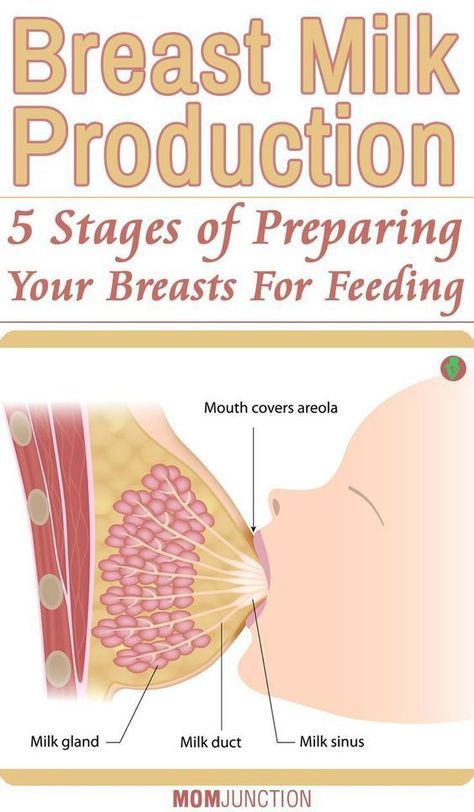
Share this information
How long should breastfeeding continue? Three months? Six? Year? Or maybe a few years?
The World Health Organization (WHO) and other authorities recommend that infants be exclusively breastfed for the first six months and then continue to be breastfed along with other foods (complementary foods) for at least two years. nine0011 1
The fact is that breast milk is not just food. It is a natural sedative if the child is anxious or tired. In addition, milk contains immune-boosting components, the amount of which increases dramatically when the baby gets sick. 2
According to anthropologists, the natural age of a person to stop breastfeeding is even more than two years. Given factors such as tooth development, body weight, comparison with other primates, and historical evidence, some scientists believe that breastfeeding may last up to two to four years. A number of researchers even believe that our ancestors breastfed children up to six or seven years of age. nine0011 3
nine0011 3
Today, more than 60% of mothers in developed countries start giving their babies formula or complementary foods before six months of age, 4 although WHO does not recommend this.
When is it time to stop breastfeeding?
Weaning means that you gradually stop breastfeeding your baby. Ideally, the first step in this process is the gradual introduction of complementary foods, starting at about six months of age. In this case, breastfeeding continues. The weaning process continues until the mother's milk has been completely replaced by other foods and drinks. nine0003
“After six months, the baby needs higher doses of certain nutrients, such as iron, zinc, vitamins B and D, that he cannot get from breast milk or from his own reserves,” says Sarah Beeson, health visitor from Great Britain.
“But solid food should at first only supplement the main diet with breast milk and gradually replace it. Mother's milk remains the main source of nutrition for the baby for many months to come. ” nine0003
” nine0003
On average, a seven-month-old baby gets 93% of its calories from breast milk. And even between the 11th and 16th months, milk provides him with about half of the daily calorie intake. 5
“Sometimes moms think that breastmilk isn't that important once a baby has started solid foods, but the truth is, no matter how many months old a baby is, there's nothing better than your milk,” continues Sarah.
In fact, the process of finishing breastfeeding can take as long as mother and baby want. “When to stop breastfeeding is up to you,” says Sarah. The only thing that matters is what you think is right for you and your child.” nine0003
How to wean
Whenever you decide to start weaning your baby, it's best to do it gradually. An abrupt cessation of breastfeeding can lead to lactostasis, blockage of the milk ducts and mastitis, and in a child such a sudden change can adversely affect the state of the digestive and immune systems. In addition, it will be difficult for both of you psychologically.
When should I stop breastfeeding?
Sometimes mothers mistakenly believe that it is time to stop breastfeeding, when in fact there is no reason to. If you're returning to work, breastfeeding can be a great way to stay close to your baby during this difficult time for both of you. You can express milk at work, and morning and evening feeding sessions will give you the opportunity to spend time alone with your baby. If you need to leave without your baby, you can also express milk and bring or send it home. nine0003
If you get sick, this is not always a reason to stop breastfeeding. Read our advice in the article on breastfeeding when sick and consult with your healthcare professional.
Weaning up to six months
If you cannot continue breastfeeding until six months and want to try weaning your baby, start by replacing one feeding a day with a bottle of formula.
“It's best to start with midday feedings. Babies are very alert and able to smell breast milk nearby, so ask your partner or relative to give your baby a bottle when you're in the other room,” Sarah advises. nine0003
nine0003
“Be hygienic when preparing meals. Be prepared for the fact that the baby will take fewer servings of expressed milk per day than if he was fed directly from the breast. Don't make him eat more milk than he wants."
You will probably feel that your breasts are fuller and more tender. This is due to the fact that your body is rebuilding to produce less milk. If this creates discomfort, try expressing some milk—just enough to relieve the discomfort without stimulating extra production. nine0003
When your body adjusts to the new volume - usually after a few days - replace with formula for one more meal a day. Continue this until you have changed all feedings and your baby is completely weaned.
“I had complications after my first birth, as a result I lost a lot of weight very quickly, and besides, I developed mastitis. Lactation was very weak, and at three months I was forced to stop breastfeeding,” recalls Jennifer, a mother of two from the UK, “I gradually replaced one feeding, so physically it was easy, but mentally it was hard for me.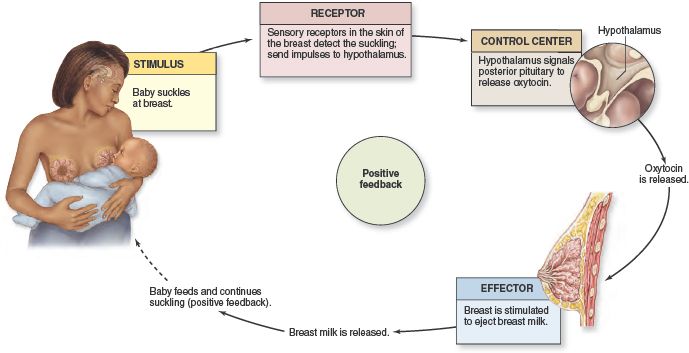 ” nine0003
” nine0003
If you want to maintain closeness with your baby and all the health benefits of breastfeeding, but still need to cut down on breastfeeding, try partial weaning, replacing only a few feeds a day with formula.
Weaning after six months
Once your baby starts eating solid foods (about six months old), you will notice that breastfeeding naturally occurs less and less. For a year, it can be reduced to just a couple of times a day, and feedings will be replaced by full meals and healthy snacks. nine0003
Anyway, if you intend to continue to reduce breastfeeding, do it gradually, replacing one feeding at a time. Use formula milk if your baby is under 12 months old. With cow's milk, you should wait at least up to a year.
“When I decided to wean my son, I breastfed him three times a day and gave him other foods three times plus light snacks. Gradually, I replaced all breastfeedings with formula. By 11 months, we only had one nighttime breastfeed left,” says Ruth, a UK mom.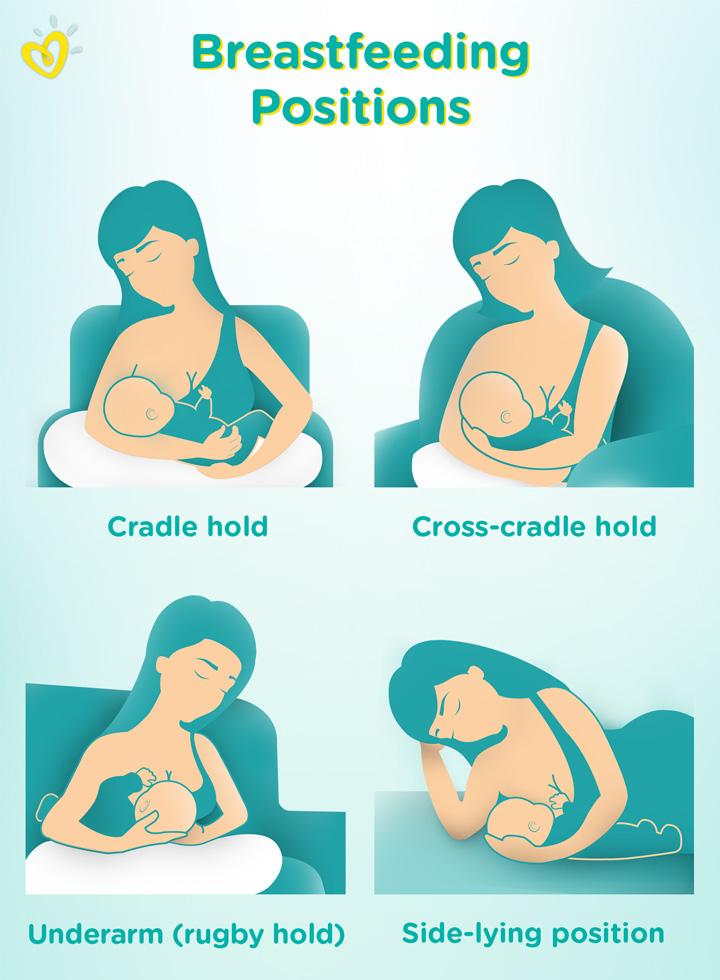 nine0003
nine0003
There are various ways to distract a child from changes in his diet. Some mothers suggest that instead of breastfeeding something to drink and eat together to maintain a sense of closeness. You can also change your daily routine, play your favorite game, or replace feeding with caresses - from you or from your partner. Some children take longer to get used to the new food, but in the end everything falls into place. If you are having difficulty weaning, ask your healthcare provider for advice. nine0003
Ending breastfeeding naturally
Ending breastfeeding can be guided by the baby's wishes. This is called baby-initiated weaning, or the natural termination of breastfeeding. Such a process is likely to be long and gradual. Month after month, feeding sessions will become shorter and less frequent, until one day the child completely loses interest in the breast.
“My daughter stopped breastfeeding on her own when she was four years old,” says Sarah, a mother from the UK.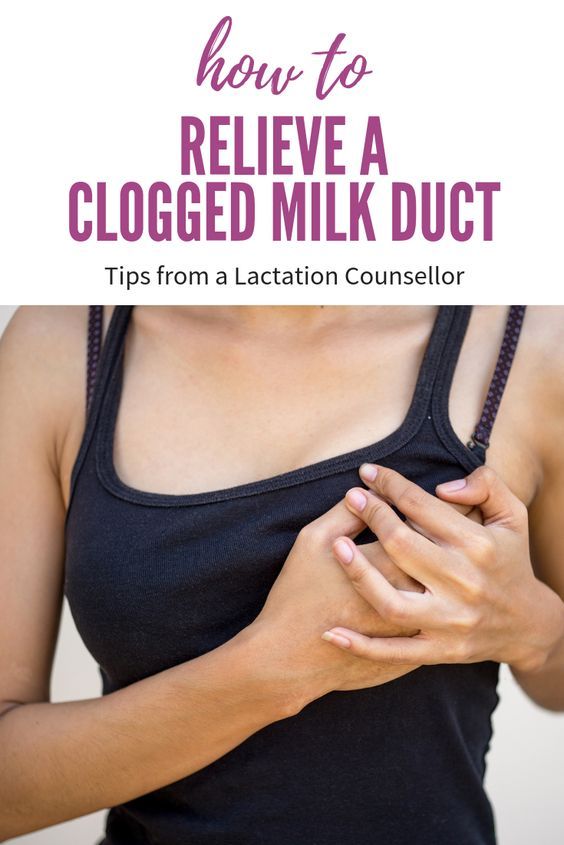 And once, when we were on vacation, she seemed to just forget about her breasts. Now, six months later, she sometimes still asks for breasts, but she already knows that there is no milk there. nine0003
And once, when we were on vacation, she seemed to just forget about her breasts. Now, six months later, she sometimes still asks for breasts, but she already knows that there is no milk there. nine0003
You will have a huge amount of time for the body to adapt, so there should be no discomfort or swelling of the breast. However, you may find it difficult emotionally, so spend more time petting and bonding with your baby.
“Child-initiated termination of breastfeeding was right for me because I never gave my son formula or a bottle. I didn’t want to abruptly stop feeding and refuse him,” recalls Kelly, a mother from the UK, “He himself lost interest in breasts at the age of two and a half years. For us, it was the best scenario, although emotionally it was not very easy for me.” nine0003
What if you need to stop breastfeeding quickly?
It is best not to stop breastfeeding abruptly, but sometimes it is necessary for medical reasons or because you cannot be near the baby.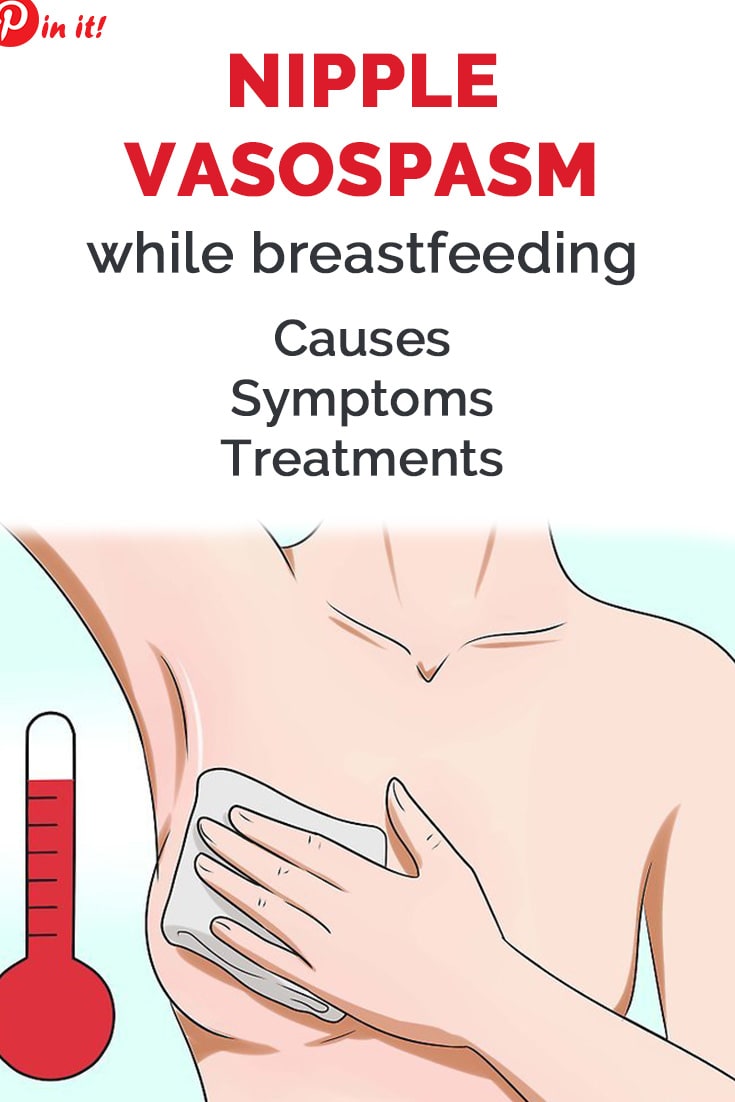
If you have been breastfeeding your baby up to this point, you will most likely have to express your milk to avoid breast swelling. Some mothers prefer to use a breast pump for this, others find it easier to express milk manually. You only need to pump a little, just to eliminate the discomfort, otherwise your body will take it as a signal to produce more milk. nine0003
At first, the breasts may swell and become tender, but this will pass. Breast milk contains a so-called feedback lactation inhibitor. When breastfeeding is stopped, this inhibitor tells your body to slow down milk production, but it can take days or even weeks for your breasts to rebuild.
Certain medications can relieve pain and should be discussed with your doctor. Always follow your pharmacist's instructions or directions, and consult your healthcare professional before taking any medication. nine0003
“I had to abruptly stop breastfeeding when my daughter was eight months old because she had to take strong painkillers,” says Peggy, a mother from Switzerland. “It was very difficult because the baby was constantly looking for a breast and crying. I held her tightly to me as I gave her a bottle. This calmed her, and after a month everything was all right.
“It was very difficult because the baby was constantly looking for a breast and crying. I held her tightly to me as I gave her a bottle. This calmed her, and after a month everything was all right.
Can I continue breastfeeding if I want to get pregnant again?
Breastfeeding is a natural contraceptive. However, this method is not the most reliable, especially after six months or if you are not exclusively breastfeeding. This means that you can get pregnant even while you are breastfeeding. nine0003
Pregnant and breastfeeding mothers sometimes receive conflicting advice about whether to stop breastfeeding. Consistent feeding of two children of different ages is of course possible, and with the advent of the second baby, your body will produce the kind of milk that both of them need.
It is not uncommon for an older child to refuse to breastfeed or skip feedings if the mother is pregnant. This may be due to changes in milk composition that occur during pregnancy. Milk can change the taste and become less sweet. nine0011 6 If your baby is under one year of age when he starts to stop breastfeeding, make sure he continues to gain weight.
Milk can change the taste and become less sweet. nine0011 6 If your baby is under one year of age when he starts to stop breastfeeding, make sure he continues to gain weight.
Talk to your doctor if you want to continue breastfeeding during pregnancy, but have had a preterm birth or miscarriage, or have any bleeding in the past.
If you need medical help to conceive, certain drugs and procedures may not be suitable while you are breastfeeding. Discuss all possible options before deciding to stop breastfeeding. nine0003
And finally...
Whenever you decide to end breastfeeding, and whatever method you choose to do so, be kind to yourself and your baby. This is a huge change for both of you physically, hormonally, and emotionally, so proceed thoughtfully and carefully.
“Although my body responded normally to stopping breastfeeding, it was psychologically difficult for me. The thing that united us for so long is over, - Jane, a mother of two children from the USA, shares her impressions, - I worked long hours, five days a week, and breastfeeding made me feel that I occupy a special place in the lives of children. But when it stopped, we soon found other ways to be together.” nine0003
But when it stopped, we soon found other ways to be together.” nine0003
Literature
1 World Health Organization. [Internet] Health Topics: Breastfeeding: 2018 [Accessed: 02/08/2018]. Available from : http://www.who.int/topics/breastfeeding/en - World Health Organization. "Health Issues: Breastfeeding" [Internet]. Geneva, Switzerland: WHO; 2018 [Visit 02/08/2018]. Article linked: http://www.who.int/topics/breastfeeding/e
2 Hassiotou et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
3 Dettwyler KA. When to wean: biological versus cultural perspectives. Clin Obstet Gynecol . 2004; 47(3)712-723. - Dettwiler KA, "Time to wean: weaning from a biological and cultural point of view". Klin Obstet Ginekol (Clinical obstetrics and gynecology). 2004; 47(3):712-723.
2004; 47(3)712-723. - Dettwiler KA, "Time to wean: weaning from a biological and cultural point of view". Klin Obstet Ginekol (Clinical obstetrics and gynecology). 2004; 47(3):712-723.
4 Victora CG Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. nine0131 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
5 Dewey KG et al. Breast milk volume and composition during late lactation (7-20 months). J Pediatr Gastroenterol Nutr . 1984;3(5):713-720. — Dewey C.G. et al., "Amount and composition of breast milk in late lactation (7-20 months)". nine0131 F Pediatrician Gastroenterol Nutr. 1984;3(5):713-720.
6 Prosser CG et al. Mammary gland function during gradual weaning and early gestation in women. Aust J Exp Biol Med 9021 9029 Sci. 1984;62( Pt 2):215-228. - Prosser S.G. et al., "Breast Function During Gradual Weaning and Early Gestation." Aust J Exp Biol Med Sai. nineteen84;62( Pt 2):215-228.
Mammary gland function during gradual weaning and early gestation in women. Aust J Exp Biol Med 9021 9029 Sci. 1984;62( Pt 2):215-228. - Prosser S.G. et al., "Breast Function During Gradual Weaning and Early Gestation." Aust J Exp Biol Med Sai. nineteen84;62( Pt 2):215-228.
Too much milk? Reduced lactation
Sometimes you may feel like you are producing too much milk, especially in the first weeks of breastfeeding. After reading our article, you will find out if you really have too much milk, and what can be done to reduce it.
Share this information
Breast milk is very healthy, so it's good to have a lot of it, right? However, this is not always the case. Babies can sometimes have a hard time coping with the rapid rush of milk that usually accompanies excess lactation.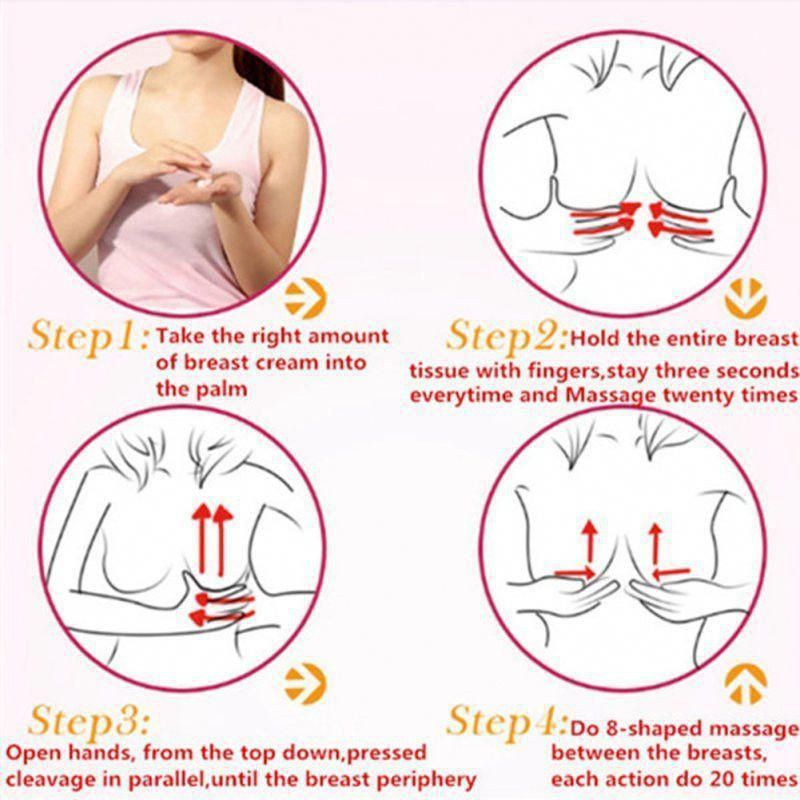 And mothers who have too much milk often experience discomfort due to the constant leakage of milk and often suffer from mastitis. nine0003
And mothers who have too much milk often experience discomfort due to the constant leakage of milk and often suffer from mastitis. nine0003
Fortunately, there are a number of ways to help in this situation. But before using them, answer two important questions:
Do I really have too much milk?
Some of the symptoms of over-lactation (listed below) may occur for very different reasons. You should not try to reduce the production of breast milk, if you are not sure that it is the overabundance of it that is the main problem. Otherwise, this can lead to the fact that your baby will produce less milk than your baby needs, especially in the critical first month when production is just being established. nine0003
Is being overweight a problem for me or my baby?
If you are sure that you have an excess of milk, but this does not cause problems for you and your baby, you do not need to do anything. In most cases, everything returns to normal within the first few months. As the baby grows, he will learn to better cope with the rapid flow of milk and will feed with pleasure.
As the baby grows, he will learn to better cope with the rapid flow of milk and will feed with pleasure.
Leakage is not always a sign of too much milk
During the first four to six weeks of your baby's birth, the level of prolactin, the hormone responsible for milk production, will rise each time the breast is emptied. In these first weeks, the breast learns to produce milk in the amount that the baby needs, depending on the time of day. Therefore, excessive leakage, rapid filling of the breast, and even splashing of milk during a rush are the norm. 1
At the same time, your baby is learning to suck and swallow milk, so you shouldn't be surprised if he suddenly coughs or chokes when he suckles. nine0003
After about four to six weeks, the spikes in prolactin levels will begin to fade and milk production will become more balanced, adjusting to your baby's needs on a supply and demand basis. 2 However, given the many hormonal changes that occur in the body of a young mother, such a restructuring may take some time. In some mothers, milk production is established quickly, in others a little longer.
In some mothers, milk production is established quickly, in others a little longer.
Behavior of the child, which may indicate an excess of milk
When overproduced, milk is usually released very quickly, especially during the first flush. As a result, the baby may cough or choke at the beginning of a feed, push back, or hold the breast loose in the mouth. The baby may pull away from the chest, frightened by a quick rush, and then cry because he hasn’t eaten. He can swallow milk in large volumes and with a lot of air, and after that he will spit up a lot. Try to be as careful as possible when you help him burp - sudden movements combined with a full tummy can cause the baby to vomit and scare him even more. nine0003
At the start of a feed, milk is relatively low in fat and consists mainly of lactose (sugar) and proteins. As the breast is fed and emptied, the fat content constantly increases. In the case of excess milk production, your baby may feel full before he completely empties his breast.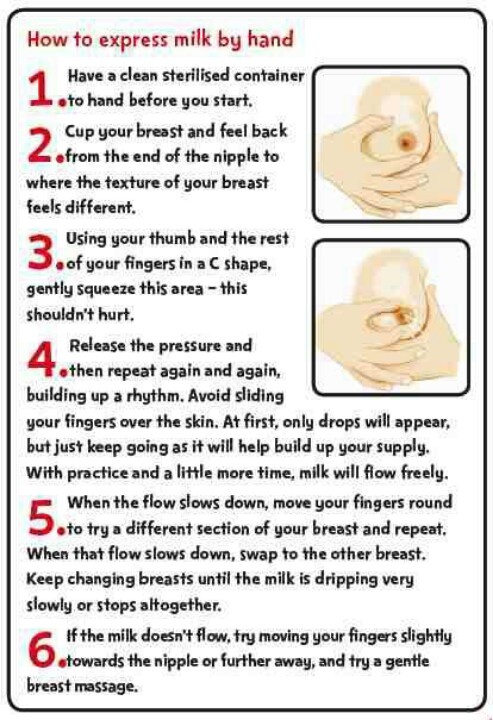 This means that he will get a lot of lactose-rich milk, but not enough fat-rich milk that comes towards the end of a feed. Excess lactose instead of a balanced diet can make digestion difficult and cause hard, frothy, and greenish stools. nine0003
This means that he will get a lot of lactose-rich milk, but not enough fat-rich milk that comes towards the end of a feed. Excess lactose instead of a balanced diet can make digestion difficult and cause hard, frothy, and greenish stools. nine0003
Oddly enough, in such a situation, the baby may constantly want to eat and behave restlessly between feedings. Despite the high calorie content, the low fat content of milk prevents it from being fully satiated. It is the fat contained in food that gives us a feeling of satiety. What happens if you eat a few dozen rice crackers or a slice of cheese with a cookie instead? You will fill up on cheese faster, as it is more saturated with fats.
However, all these symptoms can be caused by completely different problems, such as reflux, allergies, or even vice versa, insufficient milk production. An excess of breast milk can indeed cause these symptoms, but only if they are accompanied by excessive weight gain. Children usually dial around 900 g per month, but in the case of an excess of milk, they can gain much more, often almost twice as much. 1 If you feel like you have too much milk but your baby is gaining weight normally, talk to your lactation consultant or your doctor.
1 If you feel like you have too much milk but your baby is gaining weight normally, talk to your lactation consultant or your doctor.
Symptoms that may indicate an excess of milk in mothers
Mothers with an excess of breast milk often experience swelling and tightness in the breast, which constantly seems full. nine0011 3 As already noted, the leakage of breast milk in the first six weeks does not indicate its excess. However, if this continues at every feeding and after this period, it may be that the problem is in the overabundance.
A baby cannot always empty a full breast, so when there is an excess of breast milk, blockage of the milk ducts or periodic bouts of mastitis often occur. However, these problems can also be caused by other reasons.
How to reduce milk production
If you have found that you have too much breastmilk and this is causing you concern, here are a few simple things that can help. For some mothers, they are enough.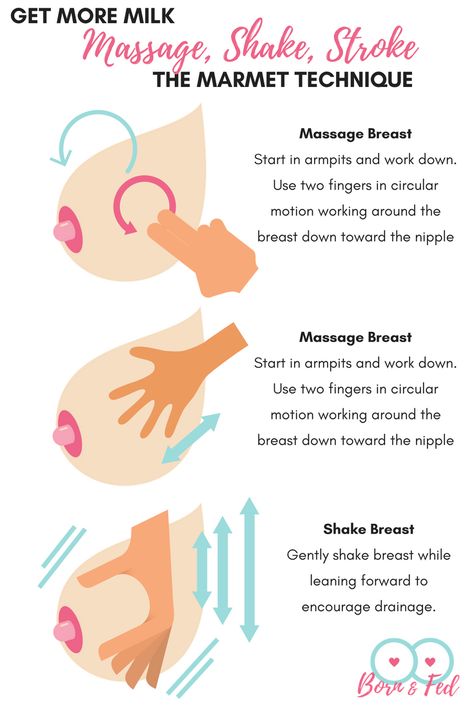
- Try to feed in a relaxed position. Reclining or lying down feeding will allow the baby to better control the process. In this position, the baby sets the rhythm of feeding himself and can always raise his head to take a break if the milk is released too quickly. Don't forget to put a towel over to soak up spilled milk. nine0324
- Release pressure. If full breasts make you uncomfortable, try expressing some milk by hand or with a breast pump, but try to express as little milk as possible. Every time you empty your breast, you send a signal to her to produce even more milk. Therefore, pumping provides short-term relief, but with prolonged use, it can only aggravate the situation. If you need to express and store milk to feed your baby when you are not around, it is best to address the excess production first. nine0324
- Try bra pads. If you have milk leaks, put special pads or pads in your bra to collect milk* to keep your underwear dry.
 If your milk leakage is moderate and already decreasing, or your breasts leak slightly during pregnancy, ultra-thin disposable pads will help you feel confident in any life situation.
If your milk leakage is moderate and already decreasing, or your breasts leak slightly during pregnancy, ultra-thin disposable pads will help you feel confident in any life situation. - Avoid teas and lactation supplements. nine0054 If you have been drinking teas, eating special biscuits, or taking supplements to improve breast milk production, this should be stopped now to resolve the problem.
Breast Watch to Reduce Milk Production
If all of the above fail, you can try a technique called breast watch to better control milk production. However, before trying this method, check with a lactation consultant or healthcare provider. nine0003
On breastfeeding, you feed your baby on demand, but only on one breast for four hours. The second breast during this time is strongly filled. Since breast milk contains what is known as a "feedback lactation inhibitor", due to overfullness, the body sends a signal to that breast to slow down milk production. This is a natural way to protect the breast from endless filling.
This is a natural way to protect the breast from endless filling.
This technique must be applied for 24 hours, changing breasts every four hours. If the milk does not become less, try increasing the duration of the "watch" to six hours. nine0003
Complete emptying and “breast duty” technique
If after another day there is still a lot of milk produced,
you can try another version of this technique, which is recommended in cases of extreme overabundance. It is called "complete emptying and duty of the breast." 3
In this method, both breasts must be completely emptied in the morning with an electric breast pump and breastfeeding should be started immediately. The flow of milk will be weaker and allow the baby to eat calmly. In addition, he will get more fat-rich milk, which comes at the end of feeding, which means he will feel more full. nine0003
After that, you can continue the "breast watch" for four hours, as described above. If that doesn't help, try increasing the interval to six, eight, or twelve hours the next day, depending on the extent of the problem.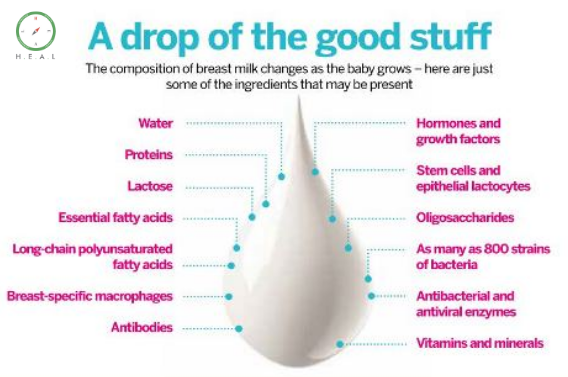 Before using this technique, be sure to consult with your doctor.
Before using this technique, be sure to consult with your doctor.
You may not need to completely empty your breasts after the first use of this technique, but some mothers have to do this once or twice. Improvement usually occurs within the first two days or a little later, but in no case should "breast watch" be used for more than five days. nine0003
Literature
1 Morbacher N. Breastfeeding answers made simple. Amarillo TX , USA : Hale 2010. - Morbacher N., "Simple answers to questions about breastfeeding." Amarillo, Texas, USA: Publishing Hale DB et al . Blood and milk prolactin and the rate of milk synthesis in women. Exp Physiol. 1996;81(6):1007-1020. - Cox D.B. et al., Effects of blood and milk prolactin on milk production in women. Exp Physiol. 1996;81(6):1007-1020.