Miscarriage amniotic fluid
Miscarriage - what you might actually see and feel
Miscarriage - what you might actually see and feel | Pregnancy Birth and Baby beginning of content7-minute read
Listen
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
A miscarriage requires prompt medical care. If you think you are having a miscarriage, call your doctor or midwife for advice and support. Go to the Emergency Department if:
- you are bleeding very heavily (soaking more than 2 pads per hour or passing clots larger than golf balls)
- you have severe pain in your tummy or shoulder
- you have a fever (a temperature above 38 degrees C)
- you are dizzy, fainting or feel like fainting
- you notice fluid coming from your vagina that smells bad
- you have diarrhoea or pain when you have a bowel motion (do a poo)
Miscarriage is a very unfortunate and sad outcome of pregnancy that takes a significant emotional and physical toll on a woman. It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
Despite close to one in 5 pregnancies ending in miscarriage, what actually happens and what a woman needs to know and do when faced with a possible miscarriage are subjects that rarely get discussed.
This article aims to give you an idea of what happens and what a woman needs to know and do at different stages in her pregnancy.
Please call Pregnancy, Birth and Baby on 1800 882 436 if you have any concerns or wish to discuss the topic further.
What might I feel during a miscarriage?
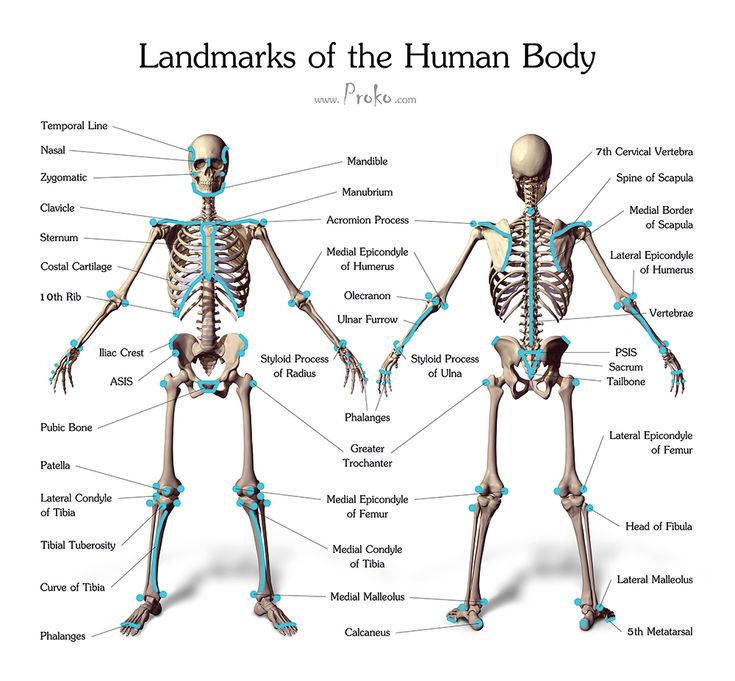
Many women have a miscarriage early in their pregnancy without even realising it. They may just think they are having a heavy period. If this happens to you, you might have cramping, heavier bleeding than normal, pain in the tummy, pelvis or back, and feel weak. If you have started spotting, remember that this is normal in many pregnancies — but talk to your doctor or midwife to be safe and for your own peace of mind.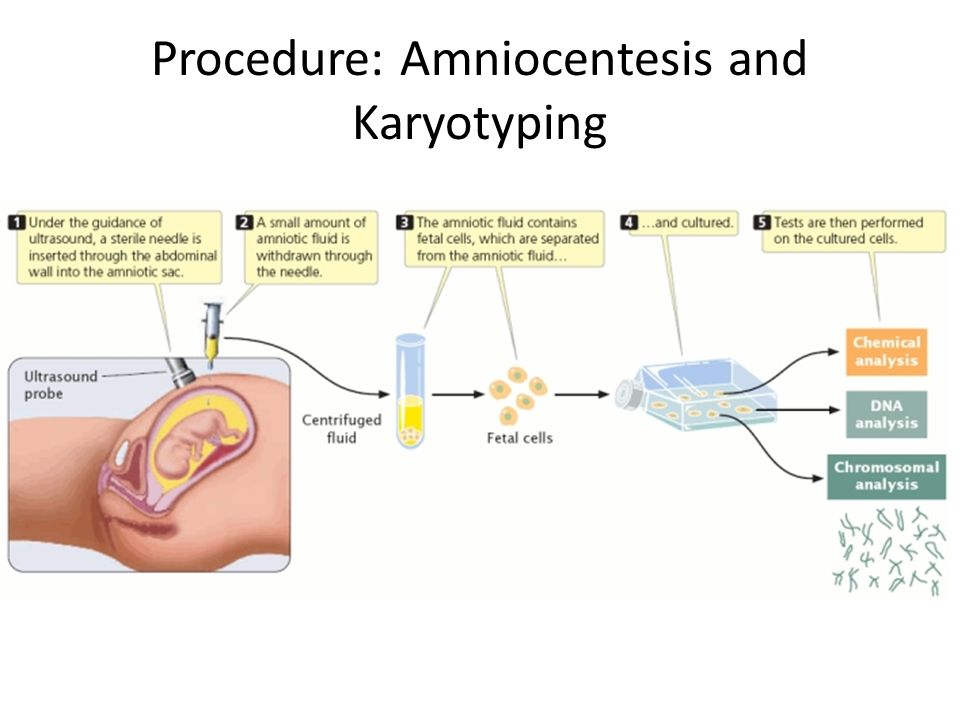
Later in your pregnancy, you might notice signs like cramping pain, bleeding or passing fluid and blood clots from your vagina. Depending on how many weeks pregnant you are, you may pass tissue that looks more like a fetus, or a fully-formed baby.
In some types of miscarriage, you might not have any symptoms at all — the miscarriage might not be discovered until your next ultrasound. Or you might just notice your morning sickness and breast tenderness have gone.
It is normal to feel very emotional and upset when you realise you’re having a miscarriage. It can take a while to process what is happening. Make sure you have someone with you, for support, and try to be kind to yourself.
What happens during a miscarriage?
Unfortunately, nothing can be done to stop a miscarriage once it has started. Any treatment is to prevent heavy bleeding or an infection.
Your doctor might advise you that no treatment is necessary. This is called 'expectant management', and you just wait to see what will happen.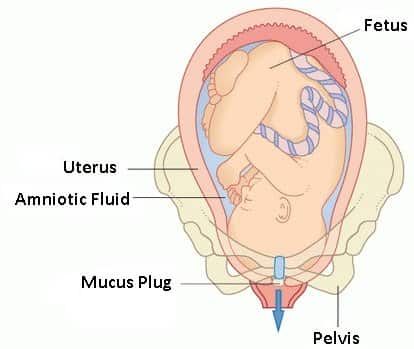 Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
It can be very hard emotionally to wait for the miscarriage because you don’t know when it will happen. When it starts, you will notice spotting and cramping and then, fairly quickly, you will start bleeding heavily. The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
Some women opt to have medicine to speed up the process. In this case, the pregnancy tissue is likely to pass within a few hours.
If not all the tissue passes naturally or you have signs of infection, you may need to have a small operation called a ‘dilatation and curettage’ (D&C). You may need to wait some time for your hospital appointment. The operation only takes 5 to 10 minutes under general anaesthetic, and you will be able to go home the same day.
While you are waiting for a miscarriage to finish, it’s best to rest at home — but you can go to work if you feel up to it.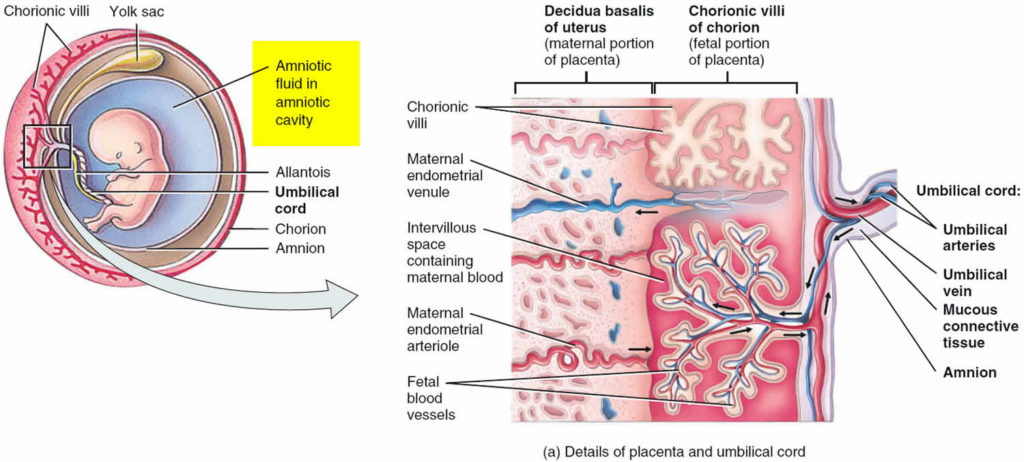 Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
What might I see during a miscarriage?
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very hard to see. You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
At 6 weeks
Most women can’t see anything recognisable when they have a miscarriage at this time. During the bleeding, you may see clots with a small sac filled with fluid. The embryo, which is about the size of the fingernail on your little finger, and a placenta might be seen inside the sac. You might also notice something that looks like an umbilical cord.
At 8 weeks
The tissue you pass may look dark red and shiny — some women describe it as looking like liver. You might find a sac with an embryo inside, about the size of a small bean.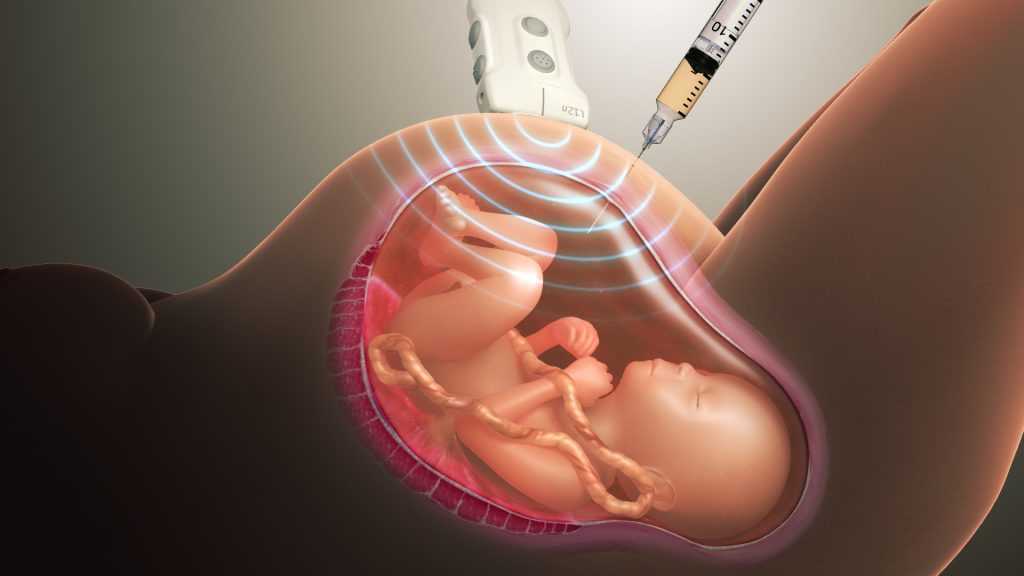 If you look closely, you might be able to see where the eyes, arms and legs were forming.
If you look closely, you might be able to see where the eyes, arms and legs were forming.
At 10 weeks
The clots that are passed are dark red and look like jelly. They might have what looks like a membrane inside, which is part of the placenta. The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
At 12 to 16 weeks
If you miscarry now, you might notice water coming out of your vagina first, followed by some bleeding and clots. The fetus will be tiny and fully formed. If you see the baby it might be outside the sac by now. It might also be attached to the umbilical cord and the placenta.
From 16 to 20 weeks
This is often called a 'late miscarriage'. You might pass large shiny red clots that look like liver as well as other pieces of tissue that look and feel like membrane. It might be painful and feel just like labour, and you might need pain relief in hospital. Your baby will be fully formed and can fit on the palm of your hand.
After the miscarriage
You will have some cramping pain and bleeding after the miscarriage, similar to a period. It will gradually get lighter and will usually stop within 2 weeks.
The signs of your pregnancy, such as nausea and tender breasts, will fade in the days after the miscarriage. If you had a late miscarriage, your breasts might produce some milk. You will probably have your next period in 4 to 6 weeks.
Remember, it’ll be normal to feel very emotional and upset at this time.
More information
Read more about miscarriage:
- What is a miscarriage?
- What happens after a miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.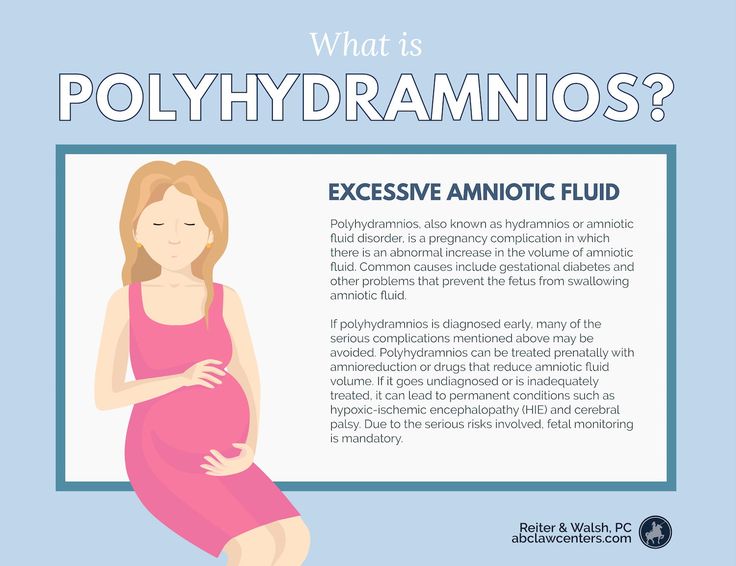
Sources:
KidsHealth (Understanding miscarriage), The Royal Women's Hospital (Treating miscarriage), Pink Elephants Support Network (Sorry for your loss), Women’s and Children’s Health Network (Miscarriage), Patient.com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- What happens after miscarriage
- Miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
What happens after miscarriage
There are a number of things you may need to consider after a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.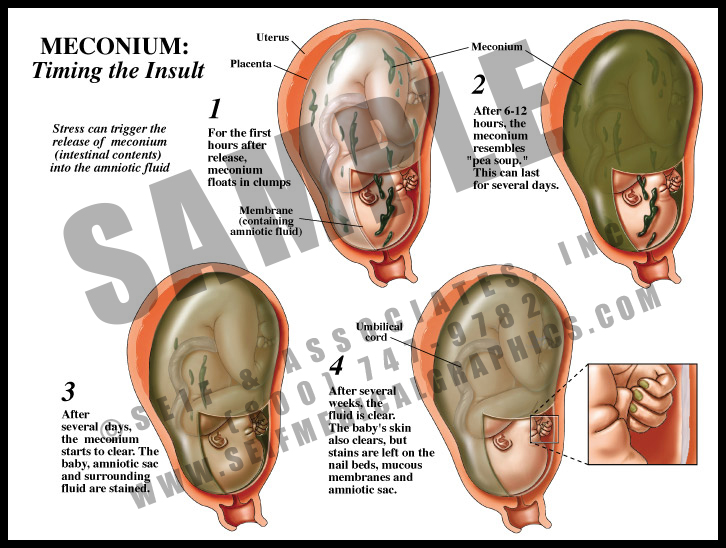
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.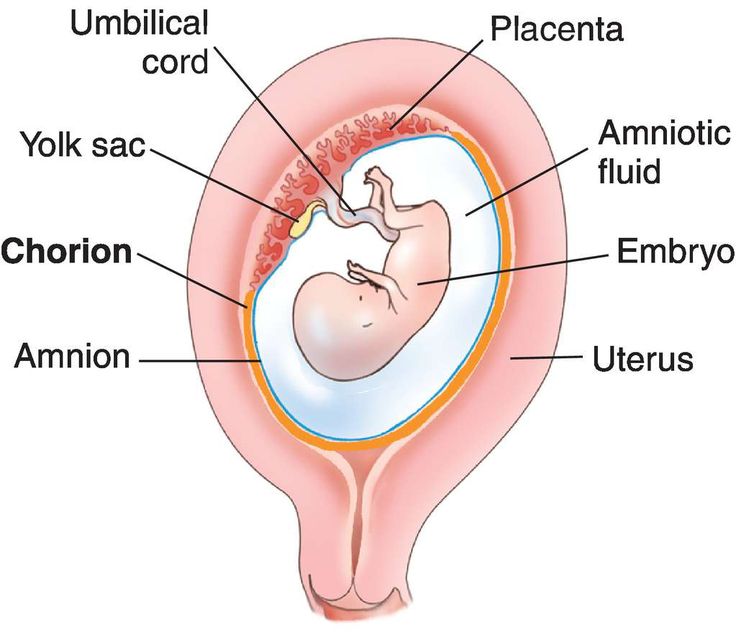
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.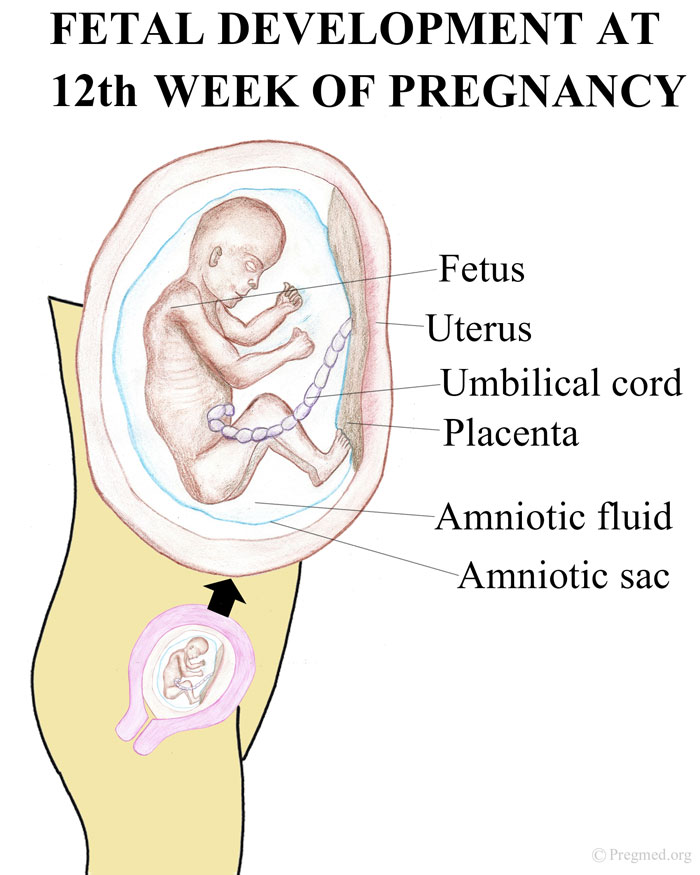
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Amniocentesis - Mayo Clinic
Overview
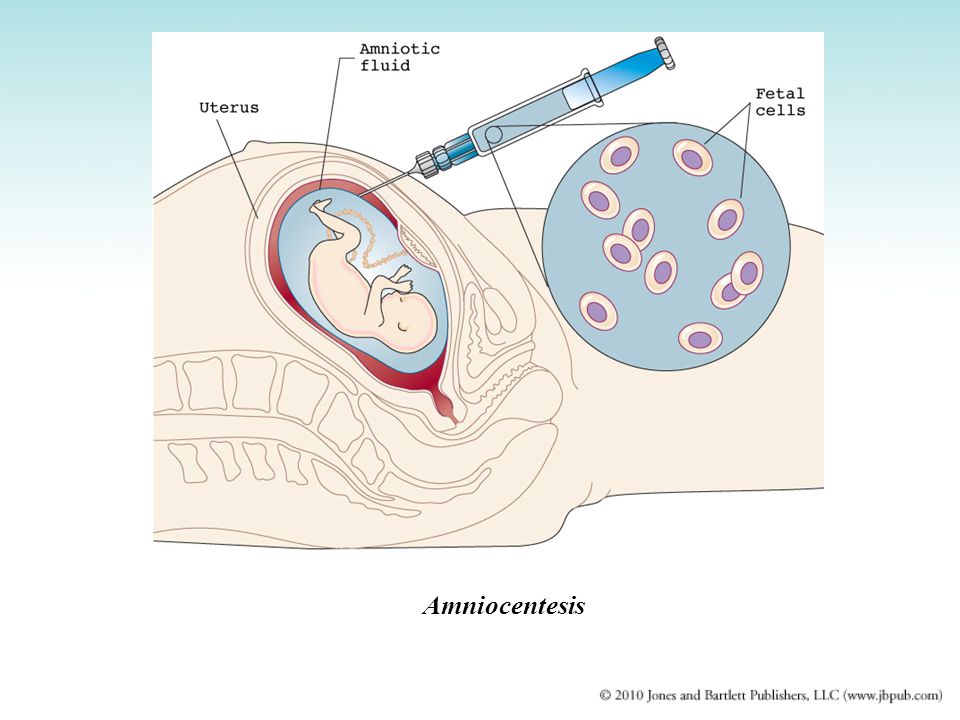
Amniocentesis
Amniocentesis
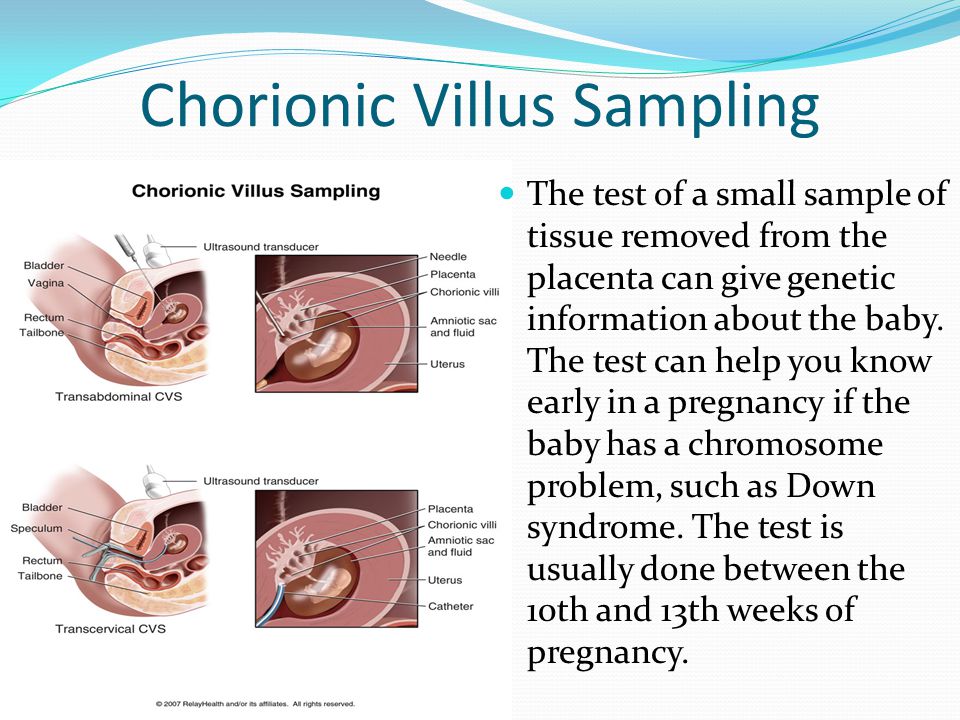
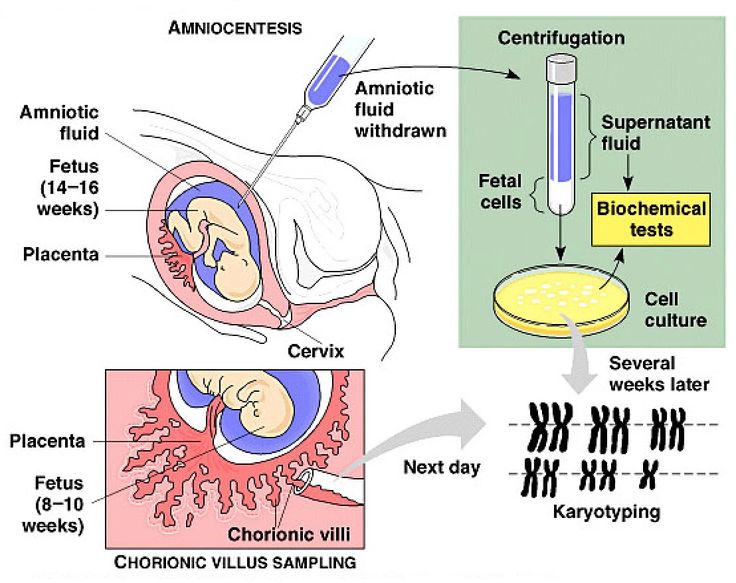
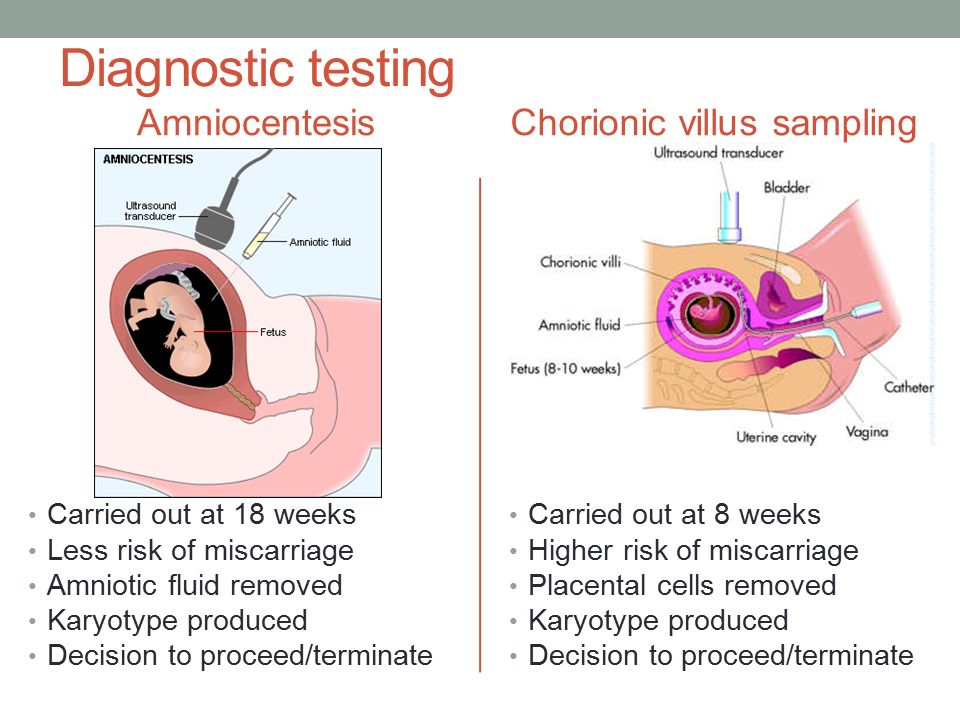
Amniocentesis is a test done during pregnancy. During amniocentesis, an ultrasound wand (transducer) is used to show a baby's position in the uterus on a monitor. A sample of amniotic fluid, which contains fetal cells and chemicals produced by the baby, is then taken for testing.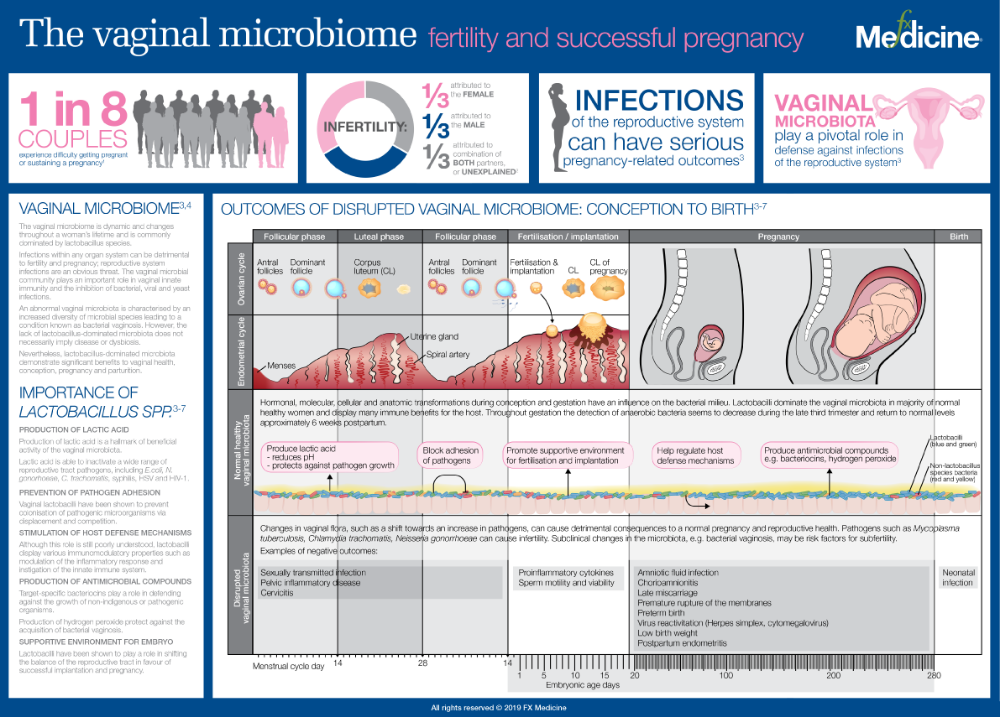
Amniocentesis is done to remove amniotic fluid and cells from the uterus for testing or treatment. Amniotic fluid surrounds and protects a baby during pregnancy.
Amniocentesis can provide useful information about a baby's health. But it's important to know the risks of amniocentesis — and be prepared for the results.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
Amniocentesis can be done for a number of reasons:
- Genetic testing. Genetic amniocentesis involves taking a sample of amniotic fluid and testing the DNA from the cells for diagnosis of certain conditions, such as Down syndrome. This might follow another screening test that showed a high risk of the condition.
- Diagnosis of fetal infection. Occasionally, amniocentesis is used to look for infection or other illness in the baby.
- Treatment. Amniocentesis might be done to drain amniotic fluid from the uterus if too much has built up — a condition called polyhydramnios.
- Fetal lung testing. If delivery is planned sooner than 39 weeks, amniotic fluid might be tested to help find out whether a baby's lungs are mature enough for birth. This is rarely done.
Genetic amniocentesis
Genetic amniocentesis can provide information about the baby's genes. Generally, genetic amniocentesis is offered when the test results might affect how to manage the pregnancy.
Genetic amniocentesis is usually done between weeks 14 and 20 of pregnancy. Amniocentesis done before week 14 of pregnancy might lead to more complications.
Reasons to consider genetic amniocentesis include:
- Having positive results from a prenatal screening test. If the results of a screening test — such as the first-trimester screen or prenatal cell-free DNA screening — show high risk or are worrisome, amniocentesis might confirm or rule out a diagnosis.
- Having an earlier pregnancy affected by a genetic condition.
 A health care provider might suggest amniocentesis to look for that condition.
A health care provider might suggest amniocentesis to look for that condition. - Being 35 or older. Babies born to people 35 and older have a higher risk of chromosomal conditions, such as Down syndrome. A health care provider might suggest amniocentesis to rule out these conditions if prenatal cell-free DNA screening is positive.
- Having a family history of a genetic condition, or if the parents are carriers of a genetic condition. Besides identifying Down syndrome, amniocentesis can be used to diagnose other genetic conditions, such as cystic fibrosis.
- Having unusual ultrasound findings. A health care provider might recommend amniocentesis to diagnose or rule out genetic conditions associated with unusual ultrasound findings.
More Information
- Cleft lip and cleft palate
- Congenital adrenal hyperplasia
- Cytomegalovirus (CMV) infection
- Down syndrome
- Hunter syndrome
- Incompetent cervix
- Spina bifida
- Thalassemia
- Toxoplasmosis
- Triple X syndrome
- Turner syndrome
Request an Appointment at Mayo Clinic
Risks
Amniocentesis carries risks, which occur in approximately 1 in 900 tests. They include:
They include:
- Leaking amniotic fluid. Rarely, amniotic fluid leaks through the vagina after amniocentesis. In most cases, the amount of fluid lost is small and stops within one week with no effect on the pregnancy.
- Miscarriage. Second-trimester amniocentesis carries a slight risk of miscarriage — about 0.1% to 0.3% when done by a skilled person using ultrasound. Research suggests that the risk of pregnancy loss is higher for amniocentesis done before 15 weeks of pregnancy.
- Needle injury. During amniocentesis, the baby might move an arm or leg into the path of the needle. Serious needle injuries are rare.
- Rh sensitization. Rarely, amniocentesis might cause the baby's blood cells to enter the pregnant person's bloodstream. Those with Rh negative blood who haven't developed antibodies to Rh positive blood are given an injection of a blood product, Rh immune globulin, after amniocentesis.
 This prevents the body from making Rh antibodies that can cross the placenta and damage the baby's red blood cells.
This prevents the body from making Rh antibodies that can cross the placenta and damage the baby's red blood cells. - Infection. Very rarely, amniocentesis might trigger a uterine infection.
- Infection transmission. Someone who has an infection — such as hepatitis C, toxoplasmosis or HIV/AIDS — might transfer it to the baby during amniocentesis.
Remember, genetic amniocentesis is usually offered to pregnant people for whom the test results might greatly affect how they manage the pregnancy. The decision to have genetic amniocentesis is yours. Your health care provider or genetic counselor can give you information to help you decide.
How you prepare
Your health care provider will explain the procedure and ask you to sign a consent form. Consider asking someone to accompany you to the appointment for emotional support or to drive you home afterward.
What you can expect
Amniocentesis is usually done in an outpatient obstetric center or a health care provider's office.
During the procedure
First, a health care provider will use ultrasound to pinpoint where the baby is in the uterus. You'll lie on your back on an exam table with your belly showing. Your health care provider will apply a gel to your belly and then use a small device known as an ultrasound transducer to show your baby's position on a monitor.
Next, your health care provider will clean your abdomen. A numbing medication generally isn't used. Most people report only mild soreness during the procedure.
Guided by ultrasound, your health care provider will insert a thin, hollow needle through your stomach wall and into the uterus. A small amount of amniotic fluid is drawn into a syringe. The needle is then removed.
You need to lie still while the needle is put in and the amniotic fluid is taken out. You might feel a sting when the needle enters your skin.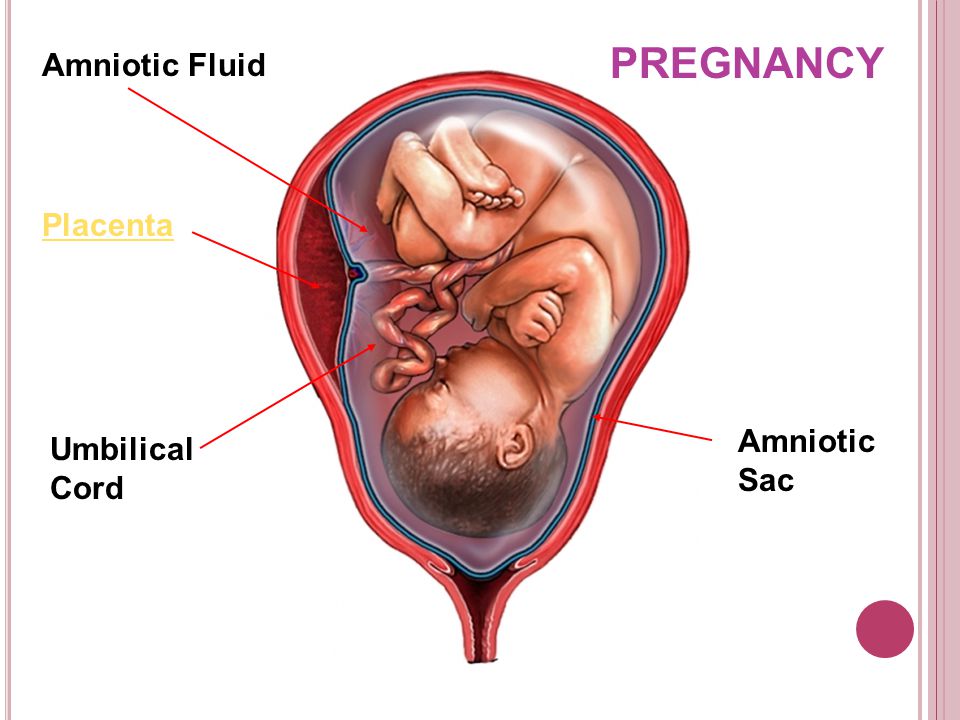 You might feel cramping when the needle enters your uterus.
You might feel cramping when the needle enters your uterus.
After the procedure
After amniocentesis, your health care provider will continue using the ultrasound to monitor your baby's heart rate. You might have cramping or mild pelvic pain after an amniocentesis.
You can return to your regular activities after the test.
The sample of amniotic fluid will be looked at in a lab. Some results might be available within a few days. Other results might take several weeks.
Contact your health care provider if you have:
- Bleeding or loss of amniotic fluid through the vagina
- Severe uterine cramping that lasts more than a few hours
- Fever
- Redness where the needle was inserted
- Fetal activity that is different than usual or no fetal movement
Results
Your health care provider or a genetic counselor will help you understand your amniocentesis results.
For genetic amniocentesis, test results can rule out or diagnose some genetic conditions, such as Down syndrome.![]() Amniocentesis can't identify all genetic conditions and birth defects.
Amniocentesis can't identify all genetic conditions and birth defects.
If amniocentesis suggests that your baby has a genetic or chromosomal condition that can't be treated, you might face hard decisions. Seek support from your health care team and your loved ones.
By Mayo Clinic Staff
Related
Products & Services
Bill for weeks or hours
28/02/2018 - 11:35
Specialists of the Chelyabinsk Regional Perinatal Center were the first in the region to learn how to prolong pregnancy for women whose amniotic fluid began to leak prematurely. A couple of years ago, such a pathology unequivocally ended in childbirth or a caesarean section within the next day. Now, under the supervision of doctors, the baby can be born on time, or he will be prepared for early birth with minimal complications. nine0004
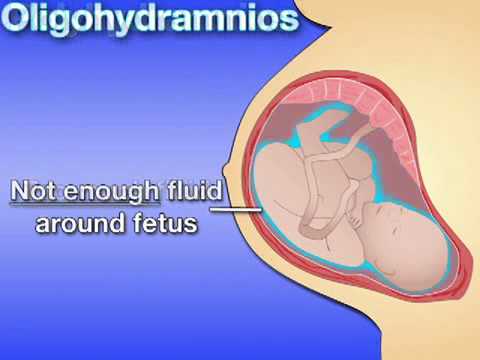
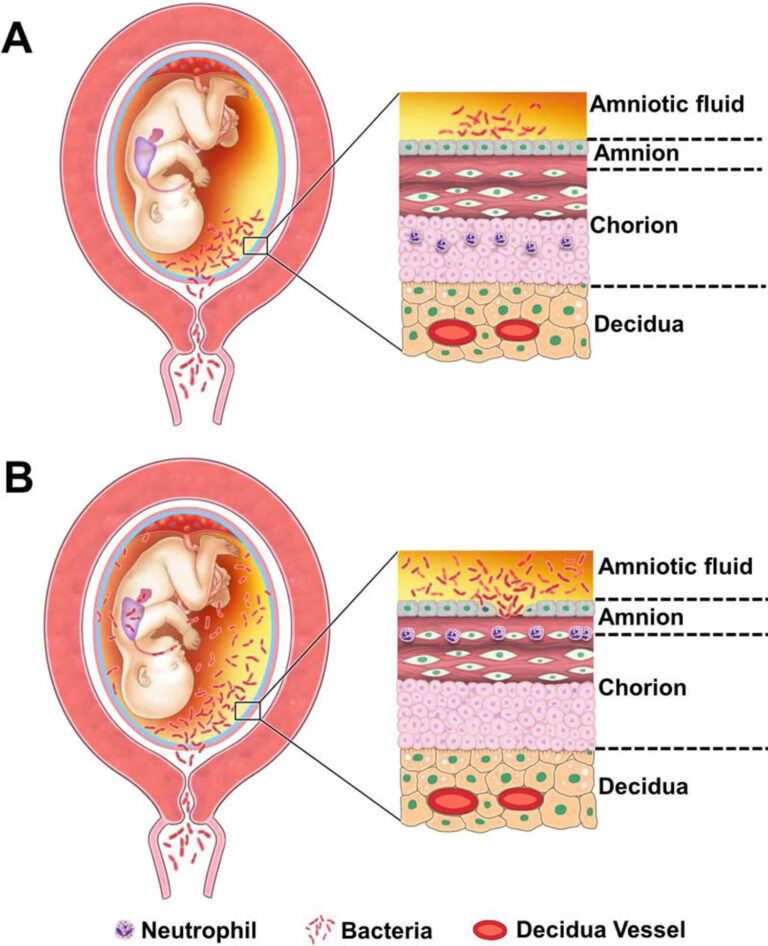
Amniotic fluid is the fluid that surrounds the fetus, protecting it and providing it with nutrients.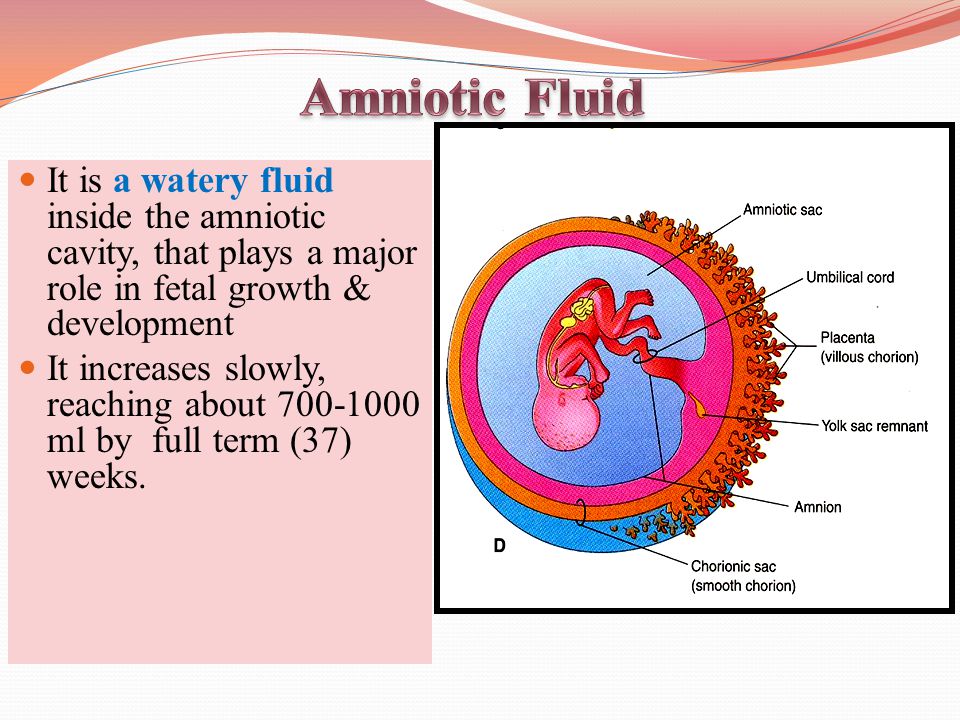 Normally, the water leaves (i.e., the fetal bladder opens) directly in childbirth or before the onset of labor at full term. If this happens ahead of schedule, then there is a serious threat to the life of the health of the mother and baby.
Normally, the water leaves (i.e., the fetal bladder opens) directly in childbirth or before the onset of labor at full term. If this happens ahead of schedule, then there is a serious threat to the life of the health of the mother and baby.
The head of the pregnancy pathology department of the OPC, an obstetrician-gynecologist of the highest qualification category 9 told the Ural-press-inform agency about how doctors help women with amniotic fluid rupture0016 Natalia Zhukova .
- Natalya Vladimirovna, how long can you prolong pregnancy after amniotic fluid discharge?
- Everything is individual. As much as possible last year, we were able to prolong the pregnancy by 86 days, this year - by 82 days so far. We have patients who are admitted with amniotic fluid leakage, we carry out the necessary treatment and let the woman go home. In due time, she safely comes to us to give birth.
- What is the treatment?
- The woman is in the hospital under the supervision of doctors, she is undergoing the necessary examinations. Antibacterial therapy is used to avoid infections, and tocolytics are administered to prevent preterm labor. Hormonal preparations are also used to accelerate the maturation of the baby's lungs, since most often such births are premature.
Antibacterial therapy is used to avoid infections, and tocolytics are administered to prevent preterm labor. Hormonal preparations are also used to accelerate the maturation of the baby's lungs, since most often such births are premature.
- How does a baby manage without amniotic fluid?
- The production of amniotic fluid continues throughout pregnancy, they are produced by the placenta and the kidneys of the child. If the patient has a tear of the fetal bladder, then this place “sticks” during treatment, and the water is restored in the required amount.
- Does this prolongation affect the health of babies?
- No. We aim to extend the pregnancy to at least 34 weeks. All over the world it is believed that from this period the child has every chance not only for life, but also for good health. Last year we prolonged pregnancy in 96 women. Most of them carried to term, and an absolutely healthy child was born. If the birth occurred prematurely, then we had time to prepare the baby, and he was born with minimal respiratory disorders.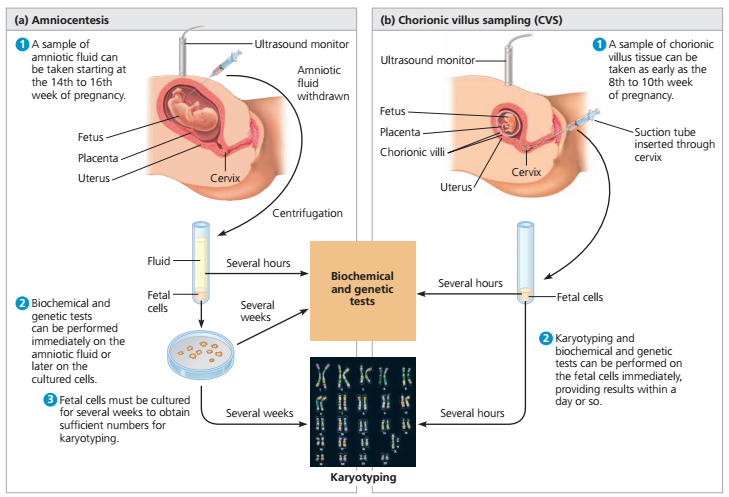 After all, this is the main problem in newborns at this time.
After all, this is the main problem in newborns at this time.
- Why does premature outflow of water occur and how can this be avoided?
- A common cause of premature rupture of water is infection. For example, if a woman suffers from chronic diseases of the pelvic organs, or during pregnancy she repeatedly suffered ARVI. This also happens when there are many abortions in the anamnesis. But sometimes it is difficult to name the exact reason. Therefore, the main advice to women: take care of yourself, take care of your women's health, avoid viral infections and contact with patients during pregnancy. nine0005
- How can a woman avoid contact with the sick, if before maternity leave she most often has to work, go shopping ...
- I agree, this is already a social problem. There are women who give birth for themselves and have to work hard. But in any case, a woman should love herself, try to relax more, treat herself during this period, like a crystal vase from the time of Louis IV. And her family should create such conditions. A husband should not transfer problems at work to the house, he may well go to the store himself, take his wife to the cinema for a good movie or give flowers. nine0005
And her family should create such conditions. A husband should not transfer problems at work to the house, he may well go to the store himself, take his wife to the cinema for a good movie or give flowers. nine0005
Of course, you shouldn't go to extremes and create a vacuum around yourself. Pregnancy is not a disease. But it is also not recommended to work until the very birth, and then come to the hospital while driving a car. For social reasons, most women today can experience the happiness of pregnancy only once or twice in their lives. Therefore, you need to make sure that these wonderful sensations are remembered for a lifetime: the first feeling of the birth of life inside oneself, the first movements of the baby, communication with the “tummy”. A woman should enjoy her pregnancy. To do this, she needs to come to this stage of life as healthy as possible. And it should also lead to a doctor who will notice any deviation in time and help prevent the consequences. And, of course, the family should give a woman only positive emotions during this period. nine0005
nine0005
Expectant mothers should remember that the suspicion of amniotic fluid leakage is not a reason for panic, but for an early visit to the gynecologist. Today, only specialists of the Regional Perinatal Center have such opportunities in the Chelyabinsk Region. Women from both the region and Chelyabinsk are admitted to the LCPC with this problem.
The original article is available at http://uralpress.ru/reviews/schet-na-nedeli-ili-chasy-chelyabinskie-vrachi-nauchilis-prodlevat-beremennost
Missed miscarriage. What is a Missed Miscarriage?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
A failed miscarriage is the intrauterine death of an embryo or fetus, which is accompanied by myometrial unreactivity and retention of the fetal egg in the uterine cavity.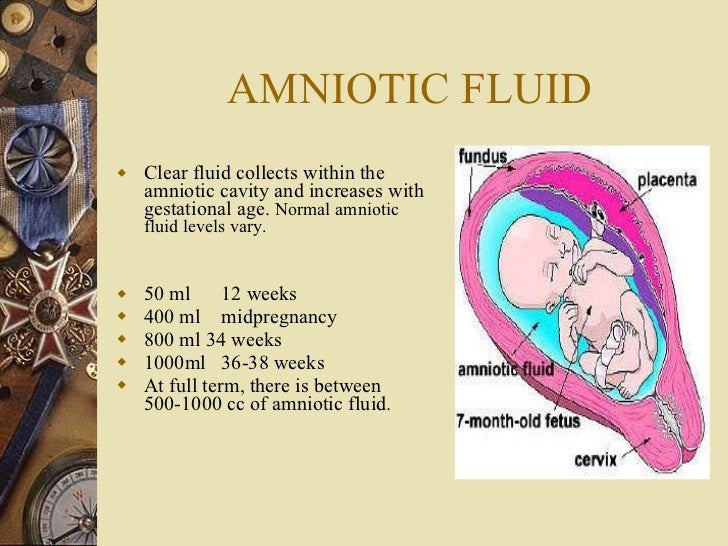 At first, there are no signs of a threat of spontaneous miscarriage, but later spotting appears, the size of the uterus lags behind the gestational age. For diagnosis, ultrasound is performed, a blood test for hCG. Treatment depends on the duration of pregnancy. Up to 14 weeks, it is possible to carry out vacuum aspiration, curettage of the uterine cavity. In the 2nd trimester, intravenous oxytocin or prostaglandins are administered into the amnion cavity. nine0005
At first, there are no signs of a threat of spontaneous miscarriage, but later spotting appears, the size of the uterus lags behind the gestational age. For diagnosis, ultrasound is performed, a blood test for hCG. Treatment depends on the duration of pregnancy. Up to 14 weeks, it is possible to carry out vacuum aspiration, curettage of the uterine cavity. In the 2nd trimester, intravenous oxytocin or prostaglandins are administered into the amnion cavity. nine0005
ICD-10
O02.1 Miscarriage
- Causes
- Pathogenesis
- Classification
- Symptoms of missed miscarriage
- Complications
- Diagnostics
- Treatment of miscarriage
- Prognosis and prevention
- Prices for treatment
General
Missed miscarriage, or non-developing pregnancy (from Latin missed abortion), is 45-90% of all cases of spontaneous interruptions of gestation.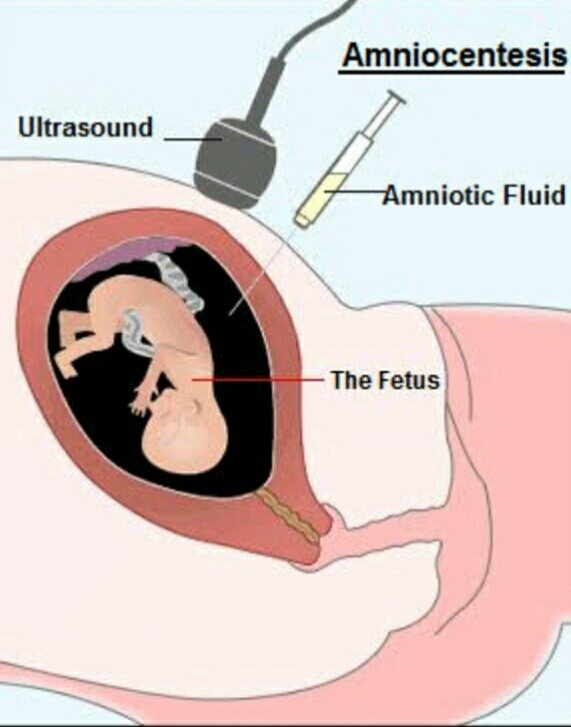 Pathology often occurs at the beginning of the gestation period, about 20% of cases are observed in the second trimester. The majority of patients are re-pregnant women, most of them did not plan to conceive. In half of the pregnant women, the emptying of the uterine cavity occurs spontaneously within 14 days, but in the third part, the remains of the embryo are delayed for a longer period, which is an indication for obstetric and gynecological care.
Pathology often occurs at the beginning of the gestation period, about 20% of cases are observed in the second trimester. The majority of patients are re-pregnant women, most of them did not plan to conceive. In half of the pregnant women, the emptying of the uterine cavity occurs spontaneously within 14 days, but in the third part, the remains of the embryo are delayed for a longer period, which is an indication for obstetric and gynecological care.
Missed miscarriage nine0005
Causes
A failed abortion is characterized by the fact that when the development of the embryo stops and its death does not occur, the expulsion of the fetal egg does not occur. This is possible in violation of the neurohumoral regulation of myometrial contractility. The development of pathology is influenced by several factors at the same time, the main reasons are:
- Chronic endometritis. It is diagnosed in most women with a failed miscarriage.
 Most often, microbial associations are determined from opportunistic microorganisms, the herpes virus, chlamydia, gonococci, Trichomonas, cytomegalovirus are detected. nine0080
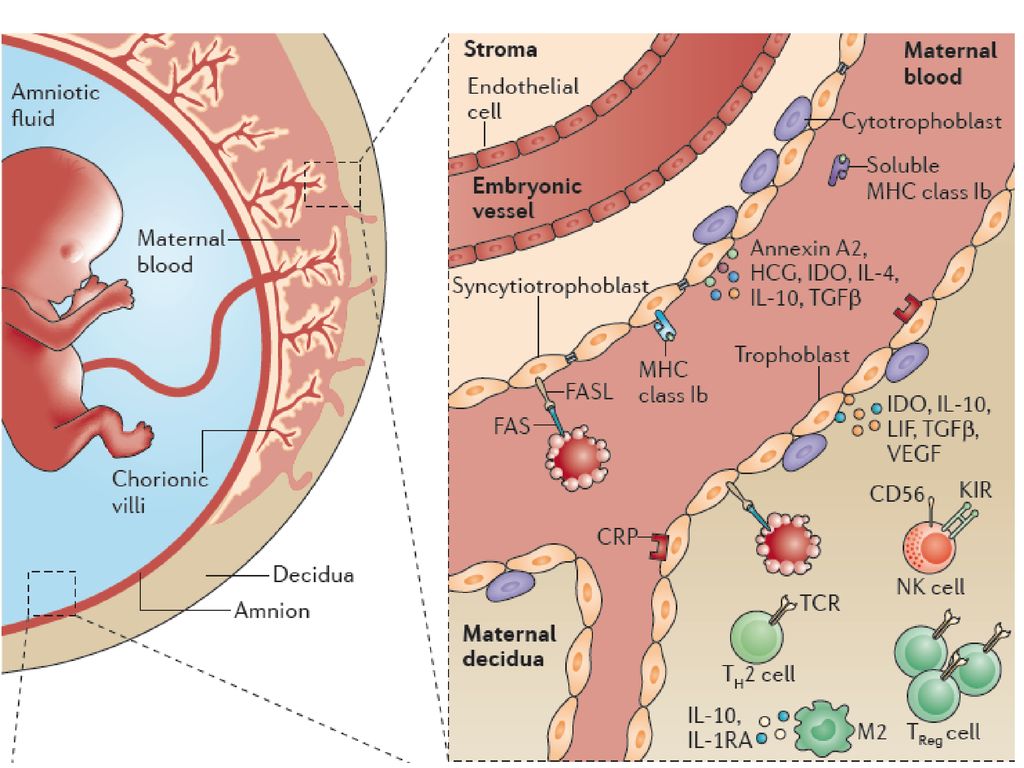
Most often, microbial associations are determined from opportunistic microorganisms, the herpes virus, chlamydia, gonococci, Trichomonas, cytomegalovirus are detected. nine0080 - Dense attachment of the chorion. With structural inferiority of the endometrium caused by endometritis, frequent abortions and high proliferative activity of trophoblast villi, the forming placenta grows deep into the wall of the uterus and delays the miscarriage.
- Immune factors. Rejection of the dead embryo does not occur with a high immunological compatibility of the mother and fetus. In some cases, there is a pronounced immunosuppression under the influence of progesterone-induced blocking protein - a specific protein of pregnant women. nine0080
- Contractile hypofunction of the myometrium. Chronic inflammation reduces the number of receptors for endogenous uterotonics. If the metabolism is disturbed, there is a deficiency of enzymes and hormonal factors involved in the expulsion of the fetus.
Pathogenesis
A failed miscarriage is more often associated with chronic endometritis, other factors act as additional ones. Viruses or bacteria that persist in the genitals can damage the cells of the fetus. Under the influence of infectious factors, the immune system is activated, the synthesis of inflammatory cytokines increases, the production of growth factors decreases, invasion is disturbed, and trophoblast cells are damaged. nine0005
With a failed abortion up to 5 weeks, the fetal egg is preserved and continues to develop, but anembryony is diagnosed due to autolysis of its contents. If infection occurred after the laying of internal organs, fetal death may occur at a later date, so a fetus is found that does not correspond to the day of gestation. Rejection does not occur due to a decrease in endometrial reactivity.
The dead embryo can linger inside the uterine cavity for 20 days or more.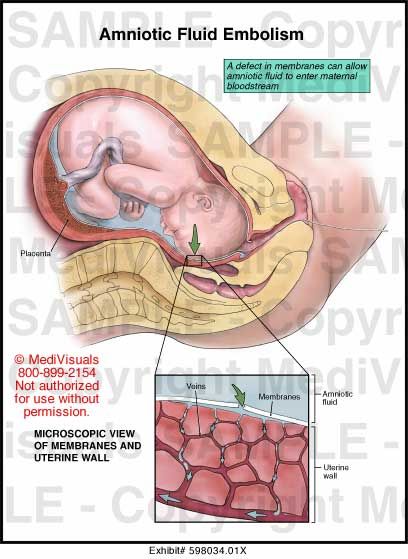 Its tissues undergo destruction and necrosis, and later they are able to mummify or petrify. When embryonic remains are preserved for more than a month, blood clotting factors are released, coagulopathy develops, which can turn into DIC. nine0005
Its tissues undergo destruction and necrosis, and later they are able to mummify or petrify. When embryonic remains are preserved for more than a month, blood clotting factors are released, coagulopathy develops, which can turn into DIC. nine0005
Classification
A failed miscarriage can develop in the 1st or 2nd trimester; this definition is not used for later terms. In the 3rd trimester, the condition is called antenatal death. In clinical gynecology, a classification is accepted depending on the gestational period in which the complication developed:
- Missed early miscarriage. Occurs before 12 weeks of gestation.
- Missed late miscarriage. The fetus dies between 12 weeks and 21 weeks of gestation. nine0080
Symptoms of missed miscarriage
With the death of the embryo, subjective sensations are absent for a long time. After 10-14 days, due to hormonal changes, non-specific signs of bearing a child decrease.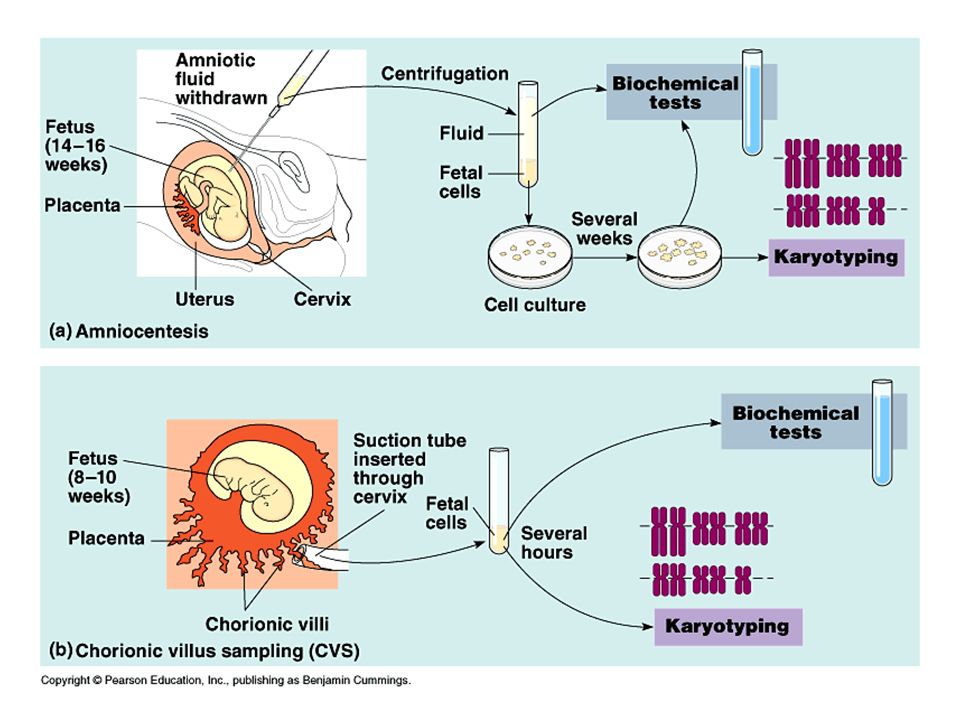 The patient feels the disappearance of morning sickness, soreness of the mammary glands, fatigue and drowsiness. Appetite, mood gradually return to normal, but amenorrhea persists.
The patient feels the disappearance of morning sickness, soreness of the mammary glands, fatigue and drowsiness. Appetite, mood gradually return to normal, but amenorrhea persists.
If the child dies at the end of the 2nd trimester, the pregnant woman stops feeling his movement, the size of the abdomen stops increasing, and body weight also does not grow. Pain over the bosom, which radiates to the sacrum, inguinal region or perineum, begins to disturb 14-30 days after a failed miscarriage. At the same time, spotting spotting from the genital tract may appear. nine0005
Sometimes the amniotic fluid is absorbed into the mother's bloodstream, the dead fetus is dehydrated and mummified. The deposition of calcium salts in the tissues of the child causes petrification. Such changes occur with prolonged retention of the fetus in the uterine cavity. A mummified and calcified fetus can be asymptomatic in the uterus for years.
Complications
With prolonged preservation of the remains of the embryo, concomitant colpitis, endometritis, an infected abortion occurs.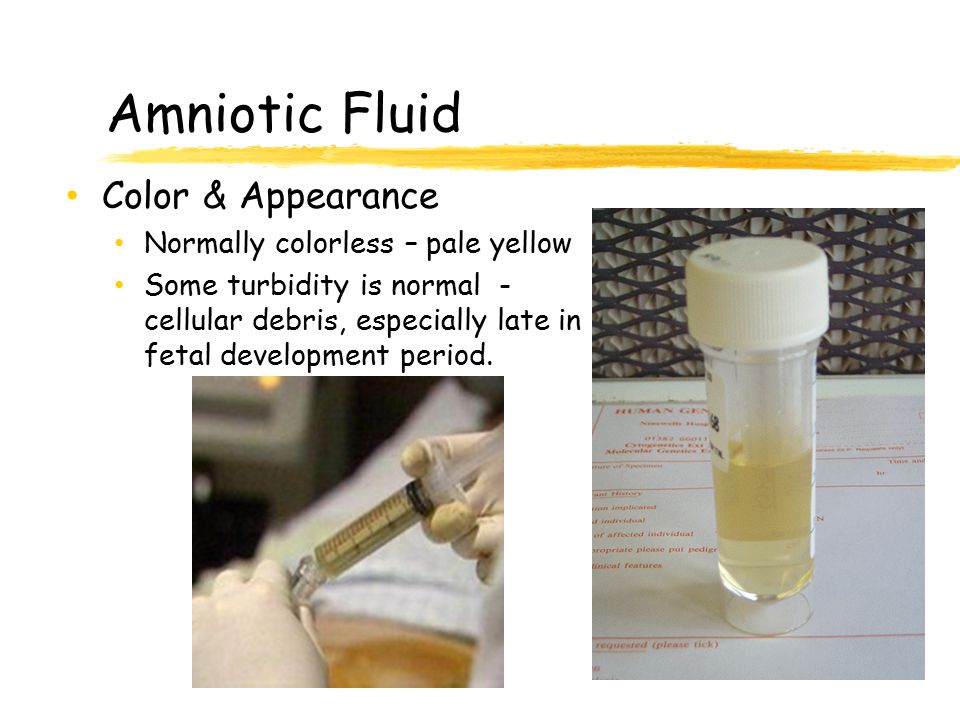 In a pregnant woman, signs of intoxication become pronounced, body temperature rises, fetid discharges appear from the genital tract. If treatment is not started, dissemination of pathogens to the pelvic cavity occurs, pelvioperitonitis, peritonitis and sepsis develop. nine0005
In a pregnant woman, signs of intoxication become pronounced, body temperature rises, fetid discharges appear from the genital tract. If treatment is not started, dissemination of pathogens to the pelvic cavity occurs, pelvioperitonitis, peritonitis and sepsis develop. nine0005
With prolonged preservation of the dead embryo, the blood coagulation system is activated. This causes coagulopathy, impaired hemostasis. Therefore, a pregnant woman with a missed miscarriage has a high risk of severe uterine bleeding and DIC.
Diagnosis
An obstetrician-gynecologist of the antenatal clinic conducts an examination of a woman with a suspicion of a failed abortion. In the early period, dynamic observation is necessary to confirm the diagnosis. Consultation with an anesthesiologist is carried out only in the appointment of surgical treatment or the risk of severe complications. The following methods are used for diagnosis: nine0005
- Gynecological examination.
 The height of the uterine fundus is less than the gestation period; during vaginal examination, the cervix is closed, and small bleeding may be observed.
The height of the uterine fundus is less than the gestation period; during vaginal examination, the cervix is closed, and small bleeding may be observed. - Ultrasound of the uterine cavity. The size of the uterus lags behind the gestation period by 2 weeks or more. In the 1st trimester, anembryony can be determined - an empty fetal egg. In other cases, there is no fetal heartbeat, and after 12 weeks there are no signs of movement.
- HCG assay. A failed interruption is accompanied by a discrepancy between the concentration of the hormone in the blood and the time of gestation. Upon re-examination, the level of hCG decreases rapidly, which confirms the death of the embryo. nine0080
- Coagulogram. A failed abortion is an indication for determining blood clotting time, aPTT, INR, prothrombin time and fibrinogen in order to anticipate hemostasis disorders and prevent them in time.
Treatment of miscarriage
After the death of the embryo, the preservation of pregnancy is impossible.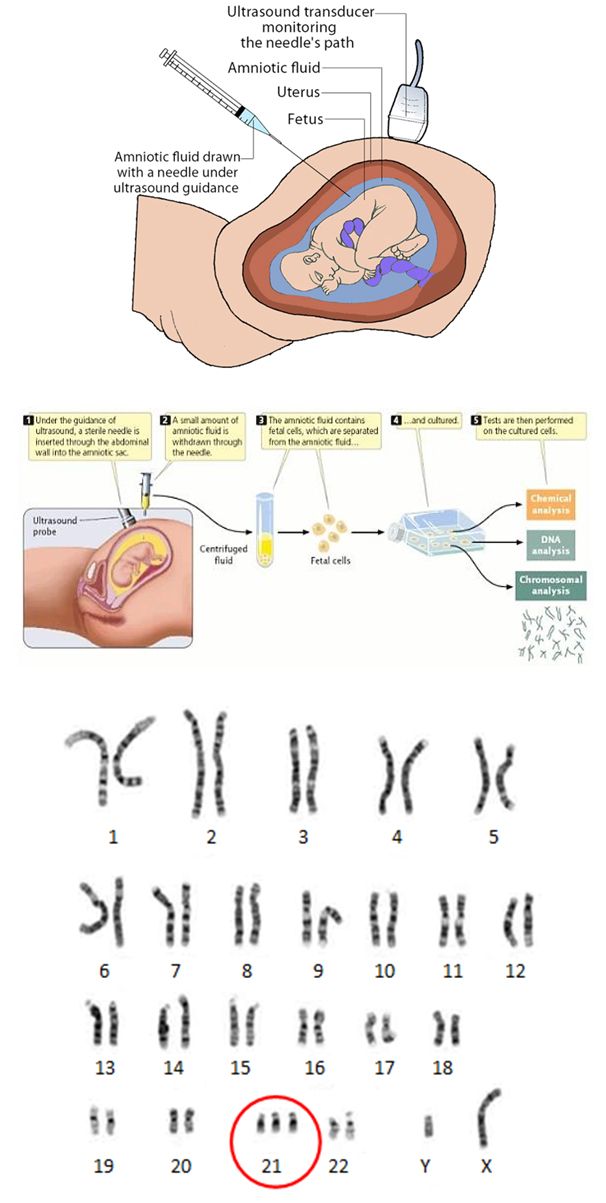 Mandatory hospitalization in the gynecological department to remove the remnants of the fetus and monitor the patient. Outpatient rehabilitation and treatment of concomitant chronic endometritis can be carried out. With a failed miscarriage, the following methods of therapy are used: nine0005
Mandatory hospitalization in the gynecological department to remove the remnants of the fetus and monitor the patient. Outpatient rehabilitation and treatment of concomitant chronic endometritis can be carried out. With a failed miscarriage, the following methods of therapy are used: nine0005
- Vacuum suction. Can be used in pregnant women up to 14 weeks. This is a gentle treatment method that does not damage the uterine walls. The procedure is performed under general anesthesia.
- Curettage of the uterine cavity. Manipulation is carried out up to 12-14 weeks under anesthesia. Curettage requires dilation of the cervical canal. Special tools remove the mucous membrane, the remnants of the fetal egg.
- Administration of prostaglandins. After 14 weeks drugs are injected into the amniotic cavity in the form of a solution or into the vagina in the form of suppositories. The drug causes the opening of the cervical canal, contraction of the myometrium and rejection of the remnants of the fetal egg.
 nine0080
nine0080 - Use of misoprostol. The drug is effective up to 24 weeks. The dosage is selected individually, in the first trimester it is 2 times more than in the second. A miscarriage occurs after 2-5 days.
- Oxytocin injections. The hormone causes uterine contractions, but sensitivity to it appears only from the 20th week of gestation. To cause a miscarriage, the drug is administered in a large dose intravenously.
Prognosis and prevention
For a woman diagnosed with miscarriage, the prognosis depends on the time of the visit to the doctor and the cause of the disease. In chronic endometritis, there is a possibility of recurrence of this condition, so testing for sexually transmitted infections and their treatment is necessary. After the addition of uterine bleeding, DIC, the risk of severe consequences or death increases. nine0005
To prevent pregnancy complications, it is necessary to plan conception, treat sexual infections and somatic pathologies.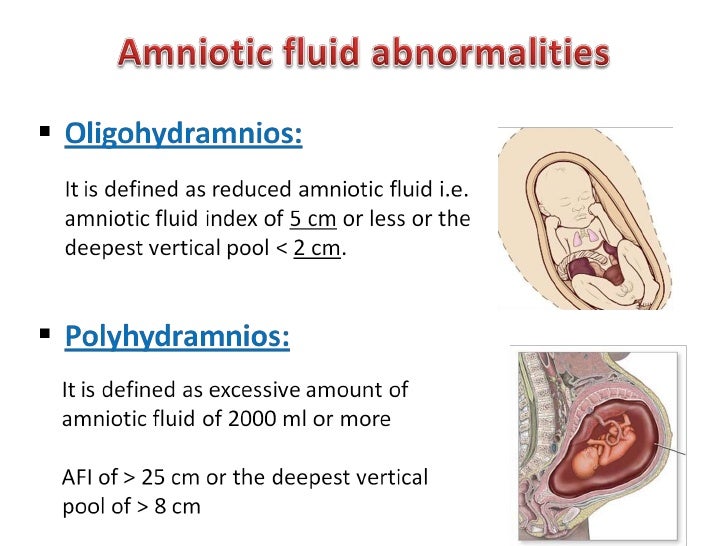 To protect against infection, casual sex should be avoided and a condom should be used. If a frozen pregnancy is repeated two or more times, an in-depth examination is required.
To protect against infection, casual sex should be avoided and a condom should be used. If a frozen pregnancy is repeated two or more times, an in-depth examination is required.
You can share your medical history, what helped you in the treatment of a missed miscarriage.
Sources
- Miscarriage. Causes and possibilities of rehabilitation / Yu.E. Dobrokhotova, Zh.A. Mandrykina, M.R. Narimanov // Russian Bulletin of an obstetrician-gynecologist. - № 4 - 2016.
- Spontaneous miscarriage. clinical protocol. Approved September 19, 2013.
- Obstetrics / ed. Savelieva G.M. - 2000
- Non-developing pregnancy. Guidelines for MARS (Interdisciplinary Association of Reproductive Medicine Specialists) / V.E. Radzinsky et al. - 2015.
- This article was prepared based on the site: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment.