38 weeks pregnant severe leg pain
Leg cramps during pregnancy | Pregnancy Birth and Baby
Leg cramps during pregnancy | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
Key facts
- Up to 3 in 10 people who are pregnant get leg cramps.
- Cramps are most common in your calf muscles.
- Cramps commonly happen at night in late pregnancy.
- To prevent leg cramps, try stretching your leg muscles before you go to bed and drink plenty of water.
- To ease a cramp, pull your toes up towards your ankle, rub the muscle, walk around or apply a heat pack.
What are leg cramps?
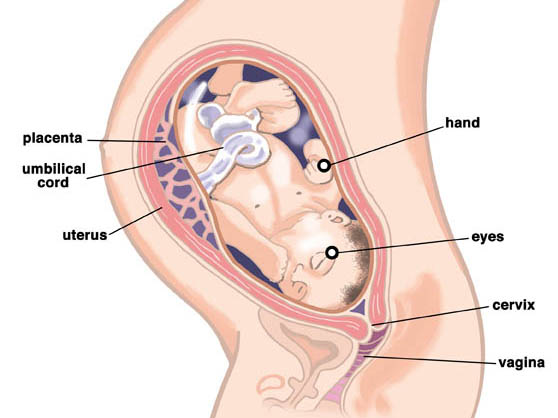
Leg cramps (pains) affect up to 3 in 10 people who are pregnant. They usually occur in your calf muscles, but can also occur in your thighs or feet. A cramp is a sign that your muscles are contracting very tightly when they shouldn’t be. This happens when acid builds up in your muscles.
Cramps usually happen at night. They are more common in your second and third trimesters.
Leg cramps are not the same as pelvic cramps.
What causes leg cramps during pregnancy?
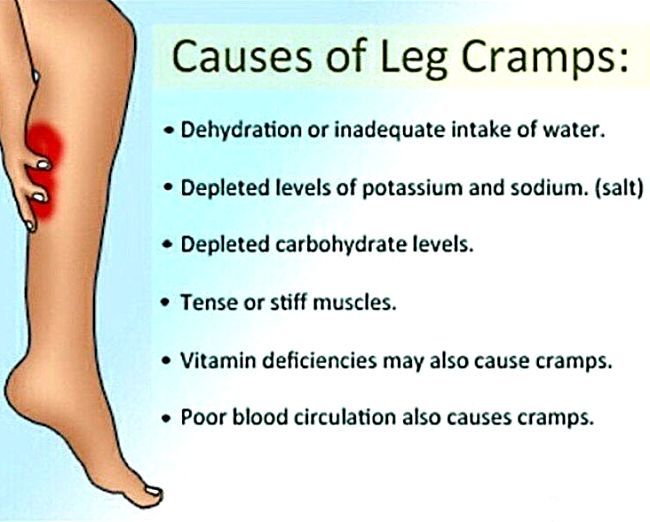
There are many reasons suggested for cramps while you’re pregnant, such as changes to your metabolism, having a vitamin deficiency, being too active or not being active enough. However, nobody really knows why they occur in pregnancy.
How can I get rid of cramps?
To ease a leg cramp, you can try:
- stretching the muscle by pulling your toes hard up towards the front of your ankle
- rubbing the muscle firmly
- walking around
- a heat pack
If you have a partner, you could ask them to help.
If your muscles are still sore after the cramp has gone, you can take paracetamol for pain relief.
How can I prevent leg cramps?
Things you can try that might help prevent cramps include:
- stretching your calf muscles before you go to bed
- drinking plenty of water
- having a warm bath before you go to bed
- eating a balanced diet
- avoiding stretching your leg while pointing your toes
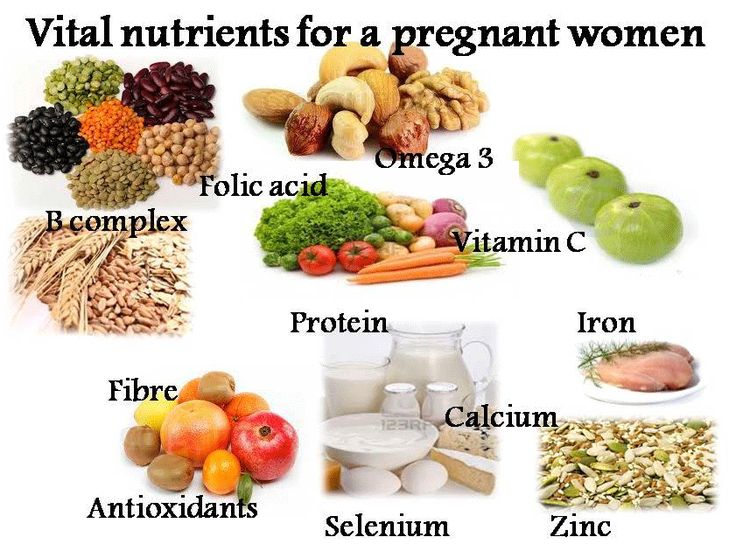
Magnesium, calcium, vitamin B and vitamin C have been suggested as a treatment for cramps. It’s not clear whether any of these supplements work, but people often try magnesium and calcium. If you’re interested in trying supplements, talk to your doctor or midwife about whether they might be suitable for you.
When should I talk to my doctor or midwife about cramps?
If leg cramps are bothering you, talk to your doctor or midwife.
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Therapeutic Guidelines (Muscle cramps, including leg cramps in pregnant women), NSW Government (Having a baby), Queensland Health (6 weird things that may happen to your body during pregnancy), King Edward Memorial Hospital (Minor Symptoms or Disorders in Pregnancy King Edward Memorial Hospital Clinical Guidelines: Obstetrics & Midwifery), Queensland Health (VTE in pregnancy (a blood clot in the vein)), NPS (Magnesium, a treatment for leg cramps?), Royal Women’s Hospital (Common concerns in early pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Common discomforts during pregnancy
- Swelling during pregnancy
- Varicose veins
Need more information?
Pregnancy at week 28
You are now in the third trimester and you'll probably be feeling many of the common discomforts of pregnancy, like a sore back, swelling, heartburn or cramps.
Read more on Pregnancy, Birth & Baby website
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
Pregnancy health problems & complications | Raising Children Network
Many pregnancy health problems are mild, but always call your doctor if you’re worried about symptoms. A healthy lifestyle can help you avoid health problems.
A healthy lifestyle can help you avoid health problems.
Read more on raisingchildren.net.au website
Pregnancy - signs and symptoms - Better Health Channel
All women experience pregnancy differently, and you will experience different symptoms at different stages of your pregnancy.
Read more on Better Health Channel website
Sleep during pregnancy
Sleep can become a problem when you're pregnant. Here are some tips to help you get as much sleep as possible so you’re ready for your baby's arrival.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 33
Your baby's brain and nervous system are now fully developed, and the baby is continuing to gain weight. You'll probably also be feeling sore and tired.
You'll probably also be feeling sore and tired.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 25
As you are approaching the end of the second trimester, you might be starting to feel a bit uncomfortable as your baby continues to grow.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 26
Your baby is starting to put on fat and muscle and as your baby grows, your centre of gravity will shift, so you might find that you are starting to walk differently and maybe even a little clumsy.
Read more on Pregnancy, Birth & Baby website
Pregnancy and your mental health - Better Health Channel
Finding out you are pregnant can be a very exciting time. But it can also make you feel uncomfortable, unwell, worried and make you wonder how you are going to cope. And it doesn’t stop when the baby arrives. Some mums find it easy to adjust to life with a new baby. But others don’t!
But it can also make you feel uncomfortable, unwell, worried and make you wonder how you are going to cope. And it doesn’t stop when the baby arrives. Some mums find it easy to adjust to life with a new baby. But others don’t!
Read more on Better Health Channel website
Sclerotherapy - MyDr.com.au
Sclerotherapy is a treatment that involves the injection of a chemical solution into blood vessels, usually spider veins or superficial (surface) varicose veins on the legs.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pregnant With Danger | PSNet
The Case
A 35-year-old woman, 38 weeks pregnant, presented to the emergency department (ED) in the middle of the night complaining of left leg pain. She also had some mild lower back pain, but no other symptoms. Hospital policy stated that all patients greater than 20 weeks’ gestation should go directly to labor and delivery unless their problem was clearly unrelated to the pregnancy. At ED triage, the pain was deemed to be non-obstetrical in nature, and so she was evaluated in the ED rather than being sent to labor and delivery.
At ED triage, the pain was deemed to be non-obstetrical in nature, and so she was evaluated in the ED rather than being sent to labor and delivery.
Physical examination revealed her left leg was slightly cooler than the right leg but was otherwise unremarkable. A Doppler venous ultrasound revealed no evidence of deep venous thrombosis, but there appeared to be decreased blood flow to the leg in the left-lying position with normal blood flow in other positions. After many hours of evaluation and observation in the ED, the pain was diagnosed as musculoskeletal. To facilitate evaluation by her obstetrician, she was transferred briefly to labor and delivery. Fetal monitoring was normal and the patient was discharged home.
The following morning, the patient’s husband found her dead at home. An emergency cesarean section was performed in the ED, but both the mother and the infant expired. Autopsy revealed a ruptured aortic dissection.
This case illustrates the frequent challenges that practitioners and institutions face in caring for pregnant women, who often present to EDs with complaints that may or may not be obstetrical in nature. Optimal evaluation of a pregnant woman with a non-obstetrical complaint requires an understanding of the physiology of pregnancy and possible pregnancy-related conditions. Just as essential, though, are a structured, systematic approach to caring for these patients, and open, clear lines of communication between obstetrical and emergency physicians.
Optimal evaluation of a pregnant woman with a non-obstetrical complaint requires an understanding of the physiology of pregnancy and possible pregnancy-related conditions. Just as essential, though, are a structured, systematic approach to caring for these patients, and open, clear lines of communication between obstetrical and emergency physicians.
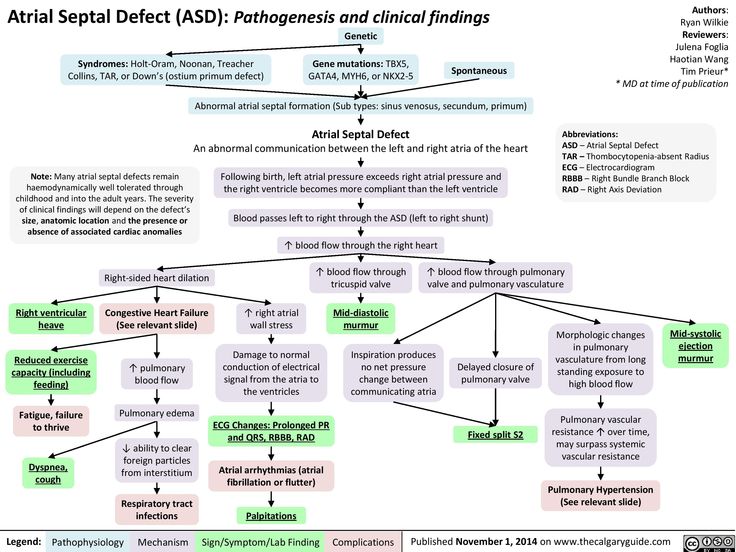
Although aortic dissection is an uncommon disorder in a woman of childbearing age, it is a potentially lethal condition and so it should be kept in mind in patients with compatible presentations. In this case, the diagnostic challenges were made even greater by a relatively unusual presentation, even for a disease that often presents with non-specific symptoms and signs. Aortic dissection is thought to result from a tear in the intima of the aorta often associated with degeneration of the media from age or other predisposing conditions. Young women who do develop aortic dissection generally have a risk factor for the disease, such as Marfan’s syndrome, Ehlers-Danlos syndrome, hypertension, or bicuspid aortic valve. Pregnancy has been considered by many to be a risk factor, and some have estimated up to half of all dissections in women younger than 40 occur during pregnancy, typically in the third trimester.(1) A recent review suggests that pregnancy’s role as a risk factor may be overstated.(2,3)
Pregnancy has been considered by many to be a risk factor, and some have estimated up to half of all dissections in women younger than 40 occur during pregnancy, typically in the third trimester.(1) A recent review suggests that pregnancy’s role as a risk factor may be overstated.(2,3)
The clinical presentation of aortic dissection varies and depends on the location and acuity of the dissection. Of more than 1,000 patients with aortic dissection included in a large registry, 76% of patients had chest pain as a presenting symptom, 55% had back pain, and 18% had migrating pain.(4) The mediastinum was widened on chest radiograph in 60%.(4) The pain is often described as ripping or tearing in nature. Ten percent of patients present with isolated leg ischemia as the initial symptom of an aortic dissection.(5) The location of the pain may help determine the location of the dissection (e.g., anterior chest pain is associated with dissection of the ascending aorta, neck and jaw pain with the aortic arch, pain in the interscapular area with the descending thoracic aorta, and pain in the lumbar area or abdomen with involvement below the diaphragm).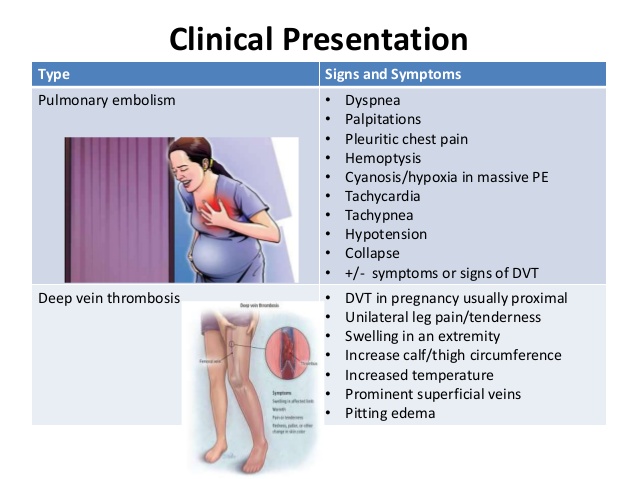 When the integrity of one of the branches of the aorta is compromised, ischemic manifestations usually follow.(1) Dissection into the iliac or femoral artery probably caused this patient’s leg pain.
When the integrity of one of the branches of the aorta is compromised, ischemic manifestations usually follow.(1) Dissection into the iliac or femoral artery probably caused this patient’s leg pain.
Little published data describe the clinical presentation of aortic dissection in pregnancy. The presentation of aortic dissection with initial symptoms of chest or back pain is similar between genders, though some suggest that dissection in women may be less likely to present with abrupt onset of pain.(6) Pregnancy-related dissection was rare in a group of more than 300 women with aortic dissection.(2) Degeneration of the collagen and elastin in the aortic media is considered a predisposing factor for dissection. This, together with increased wall stress from hypertension or valvular abnormalities (bicuspid aortic valve), is presumed to lead to intimal tear and dissection. Hypertension has been associated with 25% to 50% of cases of aortic dissection in pregnant women. The proximal aorta is the most common site of pregnancy-associated aortic dissection, with an intimal tear originating within 2 cm of the aortic valve in 75% of cases. (7) The aortic tear commonly occurs during the third trimester or during the first stage of labor.(8) It should be noted, though, that maternal and fetal mortality from aortic dissections in pregnancy have decreased substantially in the past two decades.(1)
(7) The aortic tear commonly occurs during the third trimester or during the first stage of labor.(8) It should be noted, though, that maternal and fetal mortality from aortic dissections in pregnancy have decreased substantially in the past two decades.(1)
Given its rarity and this atypical presentation, it is not entirely surprising that the diagnosis of dissection was missed in this patient. Nevertheless, some problems occurred in the triage and early management of this patient, and they help shine some light on more general safety issues regarding caring for pregnant patients with both obstetrical and non-obstetrical medical conditions. Five general principles should be addressed when developing a systematic approach to triage, evaluation, and management of urgent conditions that occur during pregnancy.
- Presenting Complaint Pregnant women can present with a myriad of complaints, making appropriate triage challenging. Complaints that clearly are obstetrical (e.g., episodic lower abdominal pain consistent with uterine contractions) should be triaged directly to the labor and delivery unit.
 However, presenting complaints that are non-obstetrical in nature or not clearly obstetrically related (e.g., chest pain, acute shortness of breath, leg pain) should be triaged depending upon the individual institution’s resources, consultant availability, and access to diagnostic testing. For example, a pregnant patient with acute chest pain or sudden shortness of breath may be more appropriately evaluated in the ED where there is often better access to diagnostic imaging than in labor and delivery. In contrast, pregnant patients in the second or third trimester with pregnancy-related complaints would be better served with an evaluation in labor and delivery. In either situation, clear communication between the emergency physician and obstetrician is important. Some examples of presenting complaints in pregnant women are included in Table 1 and may help guide an institution in developing a triage policy.
However, presenting complaints that are non-obstetrical in nature or not clearly obstetrically related (e.g., chest pain, acute shortness of breath, leg pain) should be triaged depending upon the individual institution’s resources, consultant availability, and access to diagnostic testing. For example, a pregnant patient with acute chest pain or sudden shortness of breath may be more appropriately evaluated in the ED where there is often better access to diagnostic imaging than in labor and delivery. In contrast, pregnant patients in the second or third trimester with pregnancy-related complaints would be better served with an evaluation in labor and delivery. In either situation, clear communication between the emergency physician and obstetrician is important. Some examples of presenting complaints in pregnant women are included in Table 1 and may help guide an institution in developing a triage policy. - Availability of Consultant/Clinical Expertise For obstetrically related issues, the availability of consultants and clinical expertise typically resides within labor and delivery.
 However, in other circumstances, such as presentation with leg pain, the expertise of the emergency physician and the rapid availability of consultants may make the ED a more appropriate setting for evaluation. Depending upon the health system’s structure, these resources may be equally available in the labor and delivery setting. Local administrators and clinical leaders should carefully evaluate their own consultant availability to determine how best to develop the system for triage depending upon availability of consultant and clinical expertise.
However, in other circumstances, such as presentation with leg pain, the expertise of the emergency physician and the rapid availability of consultants may make the ED a more appropriate setting for evaluation. Depending upon the health system’s structure, these resources may be equally available in the labor and delivery setting. Local administrators and clinical leaders should carefully evaluate their own consultant availability to determine how best to develop the system for triage depending upon availability of consultant and clinical expertise. - Timeliness of Testing Access to advanced imaging and testing should also help guide the development of institutional policies. In many settings, diagnostic testing such as computed tomography (CT) scanning or ultrasound is most expeditiously performed through the ED, whereas in others, an inpatient unit such as labor and delivery may be most effective. Exposure to radiation has always been a special concern during pregnancy. Fetal exposure is generally not a concern until 5 Rads (5000 mRad) of exposure has occurred.
 A CT scan of the abdomen typically results in 150-200 mRad fetal exposure, whereas a CT of the abdomen and pelvis delivers approximately 2000 mRad to the fetus.(9) In other words, concern about fetal radiation should not stand in the way of appropriate diagnostic evaluation.
A CT scan of the abdomen typically results in 150-200 mRad fetal exposure, whereas a CT of the abdomen and pelvis delivers approximately 2000 mRad to the fetus.(9) In other words, concern about fetal radiation should not stand in the way of appropriate diagnostic evaluation. - Need for Fetal Evaluation Most pregnant women with urgent or emergent complaints, unless clearly of no threat to the fetus, will undergo formal fetal monitoring. In most circumstances, fetal evaluation is done most expeditiously and thoroughly in a labor and delivery setting. However, maternal circumstances sometimes require prolonged stay in an ED (e.g., evaluation of multiple system trauma). In those circumstances, depending upon the viability of the fetus and the capabilities of the individual health system, arrangements for fetal evaluation should be made in the ED. Policies should be developed to assure the availability of appropriate clinical skills and equipment for continuous fetal monitoring in the ED when needed.
 Every ED should have the capacity to assess fetal heart rate, at a minimum by handheld Doppler. In an ED where a pregnant woman may require a prolonged stay, a protocol to provide fetal monitoring with appropriately trained personnel interpreting the monitor tracings should be developed. This can be accomplished by having a fetal monitor and labor and delivery nurse come to the ED, or, as in our institution, fetal monitoring initiated in the ED with remote interpretation of the monitor in labor and delivery.
Every ED should have the capacity to assess fetal heart rate, at a minimum by handheld Doppler. In an ED where a pregnant woman may require a prolonged stay, a protocol to provide fetal monitoring with appropriately trained personnel interpreting the monitor tracings should be developed. This can be accomplished by having a fetal monitor and labor and delivery nurse come to the ED, or, as in our institution, fetal monitoring initiated in the ED with remote interpretation of the monitor in labor and delivery. - Gestational Age at Presentation Some diagnoses are limited to certain timeframes in pregnancy and must be considered in the initial evaluation. For example, ectopic pregnancies most commonly occur between 5 and 10 weeks’ gestational age. However, they may occur as late as 14 to 15 weeks in interstitial (cornual) pregnancy. Women who present at or near the point of fetal viability (approximately 23 to 24 weeks) require special consideration, because they could require immediate fetal evaluation and potential delivery.
 Building a policy for triage and transfer between the ED and labor and delivery requires consideration of gestational age. For example, if a pregnant woman at 22 weeks’ gestational age presents to the ED with vaginal bleeding and has stable vital signs, she would be transferred to labor and delivery (see Table 2, scenario III). Nursing-to-nursing communication should take place at the time of transfer to assure transmission of information (presenting complaint, vital signs, etc.).
Building a policy for triage and transfer between the ED and labor and delivery requires consideration of gestational age. For example, if a pregnant woman at 22 weeks’ gestational age presents to the ED with vaginal bleeding and has stable vital signs, she would be transferred to labor and delivery (see Table 2, scenario III). Nursing-to-nursing communication should take place at the time of transfer to assure transmission of information (presenting complaint, vital signs, etc.).
The University of Michigan (a tertiary referral center) has developed a triage protocol for obstetrical patients presenting to the ED (Table 2). In the present case, the patient would fall into Category V (medical complaint not related to pregnancy, greater than 20 weeks' gestation) and would be evaluated in the ED. Careful attention to the differential diagnosis, appropriate consultation and the judicious use of diagnostic testing (e.g., CT scan) might have detected the aortic dissection before the discharge and subsequent tragic outcome. When resources and consultants are available, this system works well, but it would not work as well for a hospital without available obstetrical consultants. Nevertheless, even in such hospitals, it can be used as a general guide in developing institutional policies.
When resources and consultants are available, this system works well, but it would not work as well for a hospital without available obstetrical consultants. Nevertheless, even in such hospitals, it can be used as a general guide in developing institutional policies.
The mother and fetus in this case suffered a tragic outcome at a hospital that appeared to lack a structured protocol for triaging obstetric patients. It is unclear whether the outcome would have been different elsewhere. This case highlights the need to create clear guidelines for urgent management of pregnant patients and to maintain clear lines of communication between providers.
Take-Home Points
- Aortic dissection is a rare complication of pregnancy but carries substantial risk of morbidity and mortality.
- Institutions should establish structured protocols for the triage of obstetrical patients presenting with emergency complaints.
- In developing protocols, hospitals must consider many factors, including the nature of the complaints, consultant and testing availability, the need for fetal monitoring, and the fetal age.
Mark D. Pearlman, MD Professor and Vice Chair, Department of Obstetrics and Gynecology Professor of Surgery University of Michigan Medical Center
Jeffrey S. Desmond, MD Clinical Assistant Professor and Service Chief Department of Emergency Medicine University of Michigan Medical Center
References
1. Lewis S, Ryder I, Lovell AT. Peripartum presentation of an acute aortic dissection. Br J Anaesth. 2005;94:496-499. [ go to PubMed ]
2. Nienaber CA, Fattori R, Mehta RH, et al. Gender-related differences in acute aortic dissection. Circulation. 2004;109:3014-3021. [ go to PubMed ]
3. Oskoui R, Lindsay J Jr. Aortic dissection in women go to PubMed ]
4. Januzzi JL, Marayati F, Mehta RH, et al. Comparison of aortic dissection in patients with and without Marfan's syndrome (results from the International Registry of Aortic Dissection). Am J Cardiol. 2004;94:400-402. [ go to PubMed ]
5. Pacifico L, Spodick D. ILEAD--ischemia of the lower extremities due to aortic dissection: the isolated presentation. Clin Cardiol. 1999;22:353-356. [ go to PubMed ]
Clin Cardiol. 1999;22:353-356. [ go to PubMed ]
6. Konishi Y, Tatsuta N, Kumada K, et al. Dissecting aneurysm during pregnancy and the puerperium. Jpn Circ J. 1980;44:726-33. [ go to PubMed ]
7. Immer FF, Bansi AG, Immer-Bansi AS, et al. Aortic dissection in pregnancy: analysis of risk factors and outcome. Ann Thorac Surg. 2003;76:309-314. [ go to PubMed ]
8. Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest. 2002;122:311-328. [ go to PubMed ]
9. Goodsitt MM, Christodoulou EG. Diagnostic imaging during pregnancy: risks to the fetus. In: Pearlman MD, Tintinalli JE, Dyne PL, eds. Obstetric and Gynecologic Emergencies: Diagnosis and Management. New York, NY: McGraw-Hill; 2004:535-548.
Tables
Table 1. Case Examples
These cases are included to test how an institution’s ED triage policy would handle a variety of different types of patient presentations. One way to use these cases would be for both ED and OB service chiefs to review them, determine how they would handle the triage of these patients, and be certain that the expectations and outcomes of the triage are similar.
|
Table 2. Triage Guidelines for Obstetrical Patients Presenting to the Emergency Department (Adapted from University of Michigan Hospitals and Health Centers Emergency Department Guidelines)
All patients who present to emergency department triage will have a triage assessment completed and documented prior to labor and delivery (L&D) transfer
| Pregnant Patient with | Flow of Responsibility of Care |
|---|---|
| I.
| Evaluate in ED with immediate OB consult
|
| II. Emergent obstetrics problem
| Evaluated in ED with immediate OB consult
|
| III.
| Triage directly to birth center, unless stabilization required in ED
|
| IV. Medical complaint not related to pregnancy: | Evaluate in ED
|
| V. Medical complaint not related to pregnancy: >20 weeks’ gestation | If cardiac or respiratory: evaluate in ED
If not cardiac or respiratory: may be seen in ED
|
| VI. | Evaluate in ED with gynecology consult
|
| VII. Possible or active chickenpox Note: Apply surgical mask to patient upon arrival to ED | L&D services REQUIRED (If imminent delivery, follow II above)
L&D services NOT required—evaluated in ED
|
| VIII. Patient | Evaluate in birth center triage |
| IX. Patient >6 weeks postpartum | Evaluate in ED
|
This project was funded under contract number 75Q80119C00004 from the Agency for Healthcare Research and Quality (AHRQ), U. S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
38 weeks of pregnancy ► Your pregnancy, week by week
Here is the 38th week of pregnancy, which means that the baby is 38 weeks old, and perhaps he has already been born 🙂 In this case, we can only congratulate you and wish him health and many interesting events in life!
And if you are still waiting for his appearance... The child now weighs about 3 kg with a height of 49 cm. And his weight will increase until delivery. The uterus, in which he now lives, has risen 16-18 cm above the navel, but by now the tummy has already managed to drop a little. Your weight gain is from 10 to 14 kg, and if you want him to quickly return to your usual indicators after childbirth, try to eat often and in small portions. Of course, only the right products should be on the menu. Well, if now you give preference to cereals cooked in water, boiled meat and vegetables, give up sweets and pickles (if you haven’t done this before). nine0003
Your weight gain is from 10 to 14 kg, and if you want him to quickly return to your usual indicators after childbirth, try to eat often and in small portions. Of course, only the right products should be on the menu. Well, if now you give preference to cereals cooked in water, boiled meat and vegetables, give up sweets and pickles (if you haven’t done this before). nine0003
Despite the fact that the placenta continues to provide the child with everything necessary, its main functions begin to fade, and it itself “gets old”. Everything that the baby now receives from the mother is aimed at its growth. Therefore, it is extremely important for you to provide your body with the necessary components that are contained in the Pregna-5 complex.
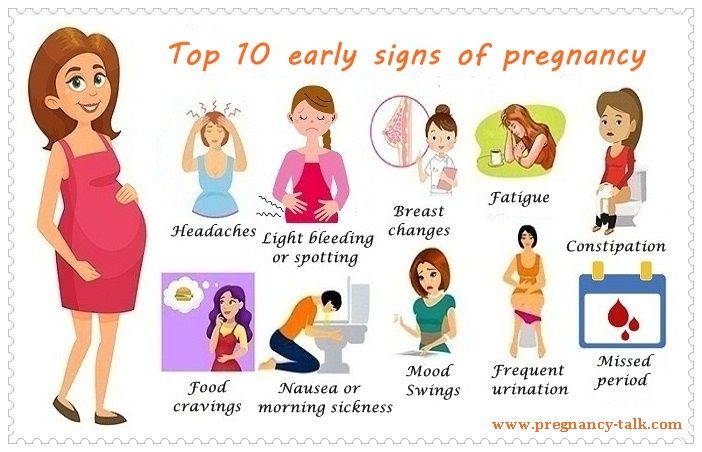
At the 38th week of pregnancy, the cervix becomes shorter, it opens up so that the baby can come out. In the meantime, it puts a lot of pressure on the bladder, forcing you to run to the restroom every now and then. To all other sensations, which either became easier or worsened throughout the pregnancy, at this stage, pain in the sacrum may be added. If, along with these sensations, your stomach began to sip, this indicates the imminent onset of childbirth. nine0003
If, along with these sensations, your stomach began to sip, this indicates the imminent onset of childbirth. nine0003
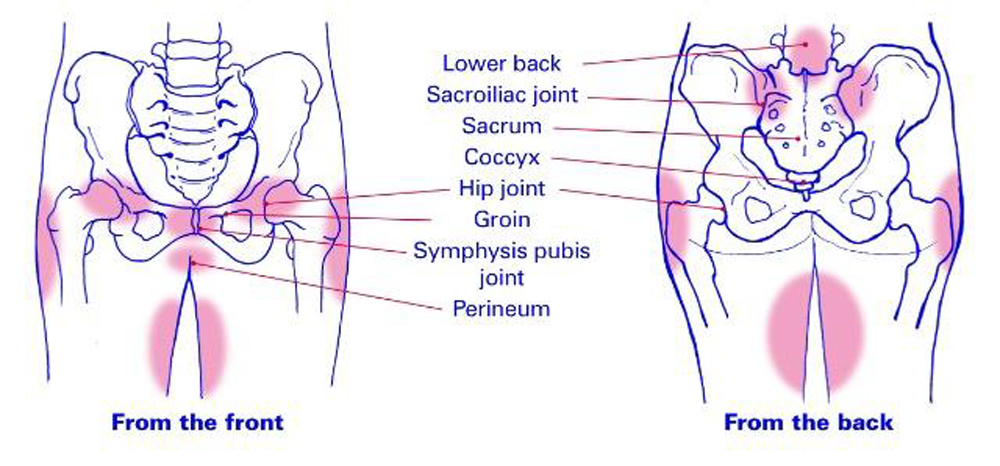
At 38 weeks of pregnancy, the pelvic bones continue to move apart, the joints become more mobile, and the cartilage and ligaments become softer. The baby's head is now pressing on the nerve endings, so you can feel sharp pains in the legs and perineum.
Training contractions become more active, and in order not to confuse them with real ones, remember: during real contractions, their frequency and strength increase. In addition, water leaves with them, and a mucous plug comes out a few days before or on the day of birth. Pay attention to the discharge: if you notice an admixture of blood, call the doctor. Remember also that your task is to ensure the purity of the birth canal so that the baby does not catch an infection during the birth! nine0003
The 38th week of pregnancy is a time when the legs and arms can swell, especially after a long stay in one position. By this point, stretch marks may have appeared, but if you take care of your skin with special products, there is a chance that it will recover faster and stretch marks will be less noticeable.
By this point, stretch marks may have appeared, but if you take care of your skin with special products, there is a chance that it will recover faster and stretch marks will be less noticeable.
The breast has become larger, its sensitivity has increased, veins appear on it. Colostrum can be intensively secreted. However, if it is not present, this is not a cause for concern - it does not and will not affect your ability to feed your baby. nine0003
A bit about close relationships with her husband, which many expectant mothers avoid for some reason. If you have a desire and the doctor does not forbid, you can spend time together. Moreover, sexual relations at the 38th week of pregnancy are useful for the expectant mother if both she and the partner do not have health problems.
38th week of pregnancy: information about the baby
Perhaps in the next few days he will make his first cry 🙂 By the way, some babies do not cry, but make a strange and not quite loud sound. In such cases, doctors slap them on the bottom to make the silent ones scream. nine0003
In such cases, doctors slap them on the bottom to make the silent ones scream. nine0003
And after birth, he will receive the first grades in his life: they are given by neonatologists on the Apgar scale after a thorough examination of the baby. Those who received 7-10 points can be considered excellent students!
Your child now has rather hard cartilages of the nose and ears, fingerprints and the skin pattern on the heels has become clearer. The child perfectly mastered the sucking and grasping reflex, and his muscles got stronger! The skin smoothed out, became rosy. He is a very cute fluff! nine0003
The baby can open his eyes, he has grown hairs, but their color may change after birth. Many children are born blonde, and over the years they begin to darken. The child's nails have grown and he can even scratch them. Don't be surprised if you find a few scratches during your first meeting!
At 38 weeks pregnant, he may move less. In general, at 9 months, the baby is not as mobile as before, since he literally has nowhere to turn around. He loves to touch everything that is around him, and sometimes playfully beats his mother with his legs. nine0003
He loves to touch everything that is around him, and sometimes playfully beats his mother with his legs. nine0003
Count your baby's movements: they should normally be at least 10 in 12 hours. He listens to you, rejoices when you talk to him, responds to strokes and attention in his own way. His mood depends on yours, remember this when you indulge in melancholy.
Most likely it has already taken its place “at the exit”, and the relaxin produced by the mother’s body makes the pelvic ring softer and prepares you for childbirth.
Key Recommendations
If you started nesting last week, the process can continue now. If putting things in order brings you pleasure - why not? nine0003
Going through and sorting things out, you can see if you forgot to prepare anything for the arrival of the baby. By the way, now, before the birth of a child, you can record a video message, which in the future will be reviewed with him! Can you imagine the range of feelings that will be in years to come?
Think through all the possible scenarios, if you have frightening questions, give yourself answers to them. For example, many women are worried about what will happen if childbirth begins when there is no husband or relatives nearby, or even right on the street. If you play all possible scenarios, it becomes much easier! nine0003
For example, many women are worried about what will happen if childbirth begins when there is no husband or relatives nearby, or even right on the street. If you play all possible scenarios, it becomes much easier! nine0003
Spend time doing something that brings you pleasure! Talk to your child : although he does not understand words, he can distinguish intonation perfectly. He is also worried, so support him, do not make him worry and nervous.
At the 38th week of pregnancy, the doctor will look at the height of the uterine fundus, the size and position of the baby, listen to his heartbeat, and send you for a general urine test. Additional tests may be ordered if necessary.
Pregnancy is coming to an end, and you and your partner are waiting for a lot of new experiences. Do not forget that in addition to being a mother, you have to be a wife and girlfriend for your man. Children very subtly feel when “something is wrong” in the family, this affects their sense of self and success. nine0003
nine0003
Spend time with your husband without a child every day, communicate with him. Mom should be “enough” for everyone. But you will definitely succeed! :)
harbingers of childbirth in multiparous and primiparas, what happens, fetal movement, baby's weight, ultrasound
What happens to the baby at this time?
Now the child's weight is 3000-3200 g. Sometimes a mother can feel in the abdomen not only the fetus moving, but also rhythmic tremors - this is the child hiccups, swallowing amniotic fluid. It is believed that hiccups are a kind of training before the start of spontaneous breathing. By this time, the baby has already taken its final position in the uterine cavity - head down, towards the exit from the uterus. The obstetrician determines the presentation of the fetus by probing the abdomen of the expectant mother. But sometimes doctors detect breech presentation, in this case, an examination is performed, ultrasound is performed and the tactics of childbirth are determined. nine0003
nine0003
Index
Norm
Weight gain of the mother
From 8.6 (with initial excess weight) to 14.5 kg (with initial weight deficit), average gain 10-12 kg
Fundal height03
35-38 cm
Fetal weight
3000-3200 g
Fetal height
48-52 cm
Important!
During the 38th week of pregnancy, the body of the expectant mother is actively preparing for the upcoming birth. It is important to know in advance, read the necessary information about this process (if you have not already done so) in order to clarify how to behave with the onset of contractions. nine0003
The first harbingers of childbirth appear in multiparous and primiparas. These are body changes, certain processes that set up the body and reproductive system for the birth of a child. The signs differ slightly depending on whether the mother is expecting her first baby or if this is her second and subsequent pregnancies.
Many mothers are afraid to miss or not recognize these important "calls". Don't worry about that - we've put together a handy labor checklist to help you figure out when it's time to go to the hospital. nine0003
Don't worry about that - we've put together a handy labor checklist to help you figure out when it's time to go to the hospital. nine0003
During this period, drops of a yellowish-whitish liquid - colostrum - can periodically be released from the nipples of the breast. So the mammary glands prepare for childbirth and subsequent feeding of the baby. In order not to stain the linen, you can use special absorbent pads for the chest. They are sold in pharmacies and children's stores, they are a small circle of absorbent materials that is inserted into a bra. If colostrum is absent, this is not a sign of pathology. In some women, the work of the mammary glands starts only after the birth of the crumbs. nine0003
Harbingers of childbirth in women expecting their first child
One of the first signs that labor is coming is easier breathing due to the fact that the stomach has drooped. This feeling is not always so vivid that the pregnant woman herself notices it, sometimes others focus on it. Although the child is also actively moving, the mother's shortness of breath decreases, breathing becomes easier, heartburn and mild nausea after eating less often occur or completely disappear. But due to the fact that the fetal head sank lower into the small pelvis, the uterus is increasingly in good shape, urination becomes more frequent due to pressure on the bladder. nine0003
Although the child is also actively moving, the mother's shortness of breath decreases, breathing becomes easier, heartburn and mild nausea after eating less often occur or completely disappear. But due to the fact that the fetal head sank lower into the small pelvis, the uterus is increasingly in good shape, urination becomes more frequent due to pressure on the bladder. nine0003
Sometimes the mother-to-be suddenly notices that the child is not moving much, his movements are not so sharp and active, he seems to calm down. This is a completely natural process, since every day there is less and less space inside the uterine cavity, the walls of its temporary “house” put more and more pressure on the arms and legs, tightly cover, and the amniotic fluid becomes a little less.
If the baby began to move less, he is also preparing for childbirth, gaining strength, but if for 10-12 hours you have not felt a single push or movement, it is better to consult a doctor. He will check if everything is fine with the baby. nine0003
nine0003
Important!
If the mother feels the fetal movements are excessive, a doctor's consultation is necessary. This is necessary to make sure that the crumbs do not have oxygen starvation, and the volume of amniotic fluid is normal.
If in earlier periods fetal movements were felt as various movements, pushes, kicks and even somersaults, then by this time more and more often it is pandiculation or slight movements. There is already little space for the baby, sometimes his movements are very noticeable - the woman notes that she is pulling her stomach in the area where the activity of the fetus is felt. nine0003
Preparing the body for childbirth
The 38th week of pregnancy is a period of active restructuring of the body. Under the influence of hormones, the body prepares for hard work: there is pain in the lower back, pulling the lower abdomen, there is an ache in the area of the pubic joint (the place where the pelvic bones are closed). The lower abdomen hurts due to the descent of the fetal head and its tight fit to the pelvic bones, the occurrence of more and more frequent training uterine contractions and the gradual loosening of the ligaments. Sometimes there is a feeling that the stomach is turning to stone - this is the tone of the uterus, muscle training for subsequent contractions. If these contractions are irregular, occur occasionally, they are not intense, you just need to lie on your side, rest, and they pass. If the same time passes between contractions, they become more and more sensitive, the interval is reduced - this is the beginning of labor, it's time to go to the maternity hospital. nine0003
Sometimes there is a feeling that the stomach is turning to stone - this is the tone of the uterus, muscle training for subsequent contractions. If these contractions are irregular, occur occasionally, they are not intense, you just need to lie on your side, rest, and they pass. If the same time passes between contractions, they become more and more sensitive, the interval is reduced - this is the beginning of labor, it's time to go to the maternity hospital. nine0003
There is one easy way to tell if contractions are false or true. You just need to count the number of contractions and the interval between them. Use a stopwatch on your smartphone, noting how long the contraction of the uterus lasts and how long the period of relaxation, rest, will then be. If the contractions of the uterus gradually increase, intensify, and the time intervals between them gradually decrease, this is a sign of the onset of labor. Then it was time to go to the maternity hospital. nine0003
Mucous discharge from the genital tract may occur during the 38th week. By the nature of the discharge, they look like lumps of dense transparent or whitish mucus with streaks of blood without any smell. This is the discharge of the mucous plug, which closed the cervix and prevented the penetration of pathogenic bacteria to the fetal membranes. The cervix gradually softens, opens slightly and the mucus gradually leaves.
By the nature of the discharge, they look like lumps of dense transparent or whitish mucus with streaks of blood without any smell. This is the discharge of the mucous plug, which closed the cervix and prevented the penetration of pathogenic bacteria to the fetal membranes. The cervix gradually softens, opens slightly and the mucus gradually leaves.
Good to know
In nulliparous women, the harbingers of imminent labor may appear approximately one to two weeks before the onset of labor. It's about 38 or 39th weeks of pregnancy.
In some cases, the mother-to-be may have loose stools at 38 weeks of gestation, although no changes in the woman's diet have occurred. This is an acceptable bowel reaction to changing hormone levels and preparing the body for childbirth. The intestines are gradually cleared of the contents. However, not always different sensations and changes in the work of digestion are explained precisely by prenatal changes. Diarrhea at this gestational age may also be the result of dietary errors, food poisoning, or other influences. nine0003
nine0003
A particularly alarming situation is when nausea and even vomiting occur against the background of diarrhea. In this case, you should immediately consult a doctor.
Harbingers of childbirth when expecting a second and subsequent children
If this is not the first pregnancy and childbirth for a woman, and the family is expecting a second, third baby, then the birth may come a little earlier. The body already knows what will happen and it takes less time for the preparatory phase. Thus, the appearance of the crumbs into the world can be expected in the period from the beginning of the 38th week of pregnancy. The processes themselves, which are associated with the preparation for childbirth, may not be so pronounced, sometimes they are absent or appear just a couple of days before the baby is born. nine0003
So, with repeated pregnancy, there may not be a pronounced and significant lowering of the abdomen. Often, the baby is initially located lower than during the first pregnancy, or the cervix relaxes just before the onset of childbirth. Then the woman feels that it has become easier to breathe, the pressure on the bladder has increased.
Then the woman feels that it has become easier to breathe, the pressure on the bladder has increased.
Important!
It is worth emphasizing that in multiparous mothers, the harbingers of childbirth may be completely absent. The birth process can begin suddenly, and the contractions will be stronger, the duration of labor will be shorter. Therefore, by the time of 38 weeks, you need to collect everything you need to go to the maternity hospital, all the necessary things and documents should be in an accessible place. nine0003
Childbirth is unique, it takes place differently in women, and even in the same woman childbirth is different. If this is the third birth or the fourth, often the precursors can be barely perceptible or completely absent. And the birth act itself proceeds quite quickly and sometimes even a little earlier than the date of birth, which is determined by the doctor. But, as for the second birth, this fact is not a strict pattern, childbirth is possible almost the same day with a pre-calculated date.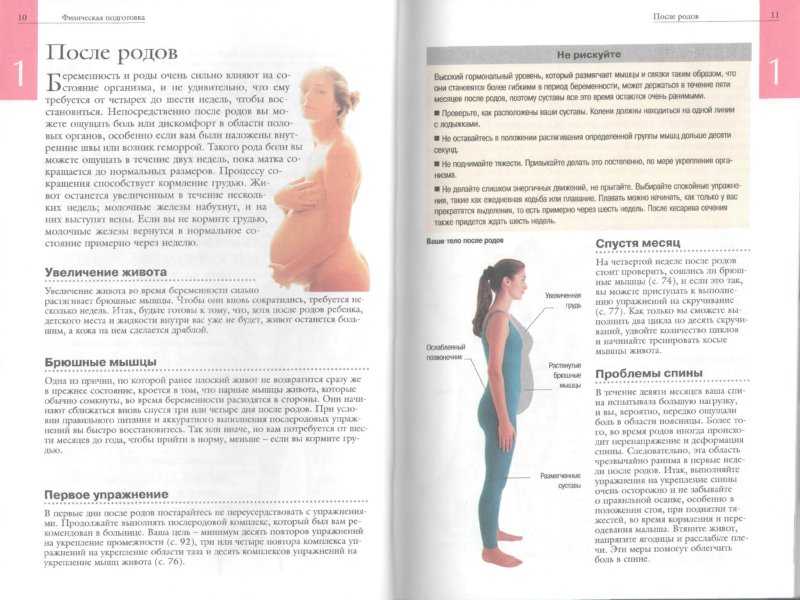
In any case, by the 38th week of pregnancy, it is necessary to collect everything necessary for a trip to the maternity hospital and immediately seek medical help at the first contractions. nine0003
Is it worth it to speed up labor at this time?
Many women experience fatigue towards the end of their pregnancy and want to have a baby as soon as possible. Therefore, they ask one question - how to speed up the onset of childbirth, is it possible to stimulate this process in order to meet the baby faster and return home, accept congratulations and raise the baby. But you don't need to think about inducing labor before the full term of 40 weeks. Although by the 38th week the baby is already full-term, he is still gaining weight, continues to develop, and nature knows better when he needs to be born. nine0003
- 1. Normal pregnancy (clinical guidelines) // Obstetrics and Gynecology: News. Opinions. Learning. 2020. No. 4 (30).
- 2. Burkitova A.M., Prokhorova V.

 Trauma
Trauma Pregnancy-related chief complaint: ≥13 weeks’ gestation
Pregnancy-related chief complaint: ≥13 weeks’ gestation Bleeding/cramping, hyperemesis gravidarum:
Bleeding/cramping, hyperemesis gravidarum: