Milk allergy in newborns symptoms
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP or health visitor to discuss your concerns.
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
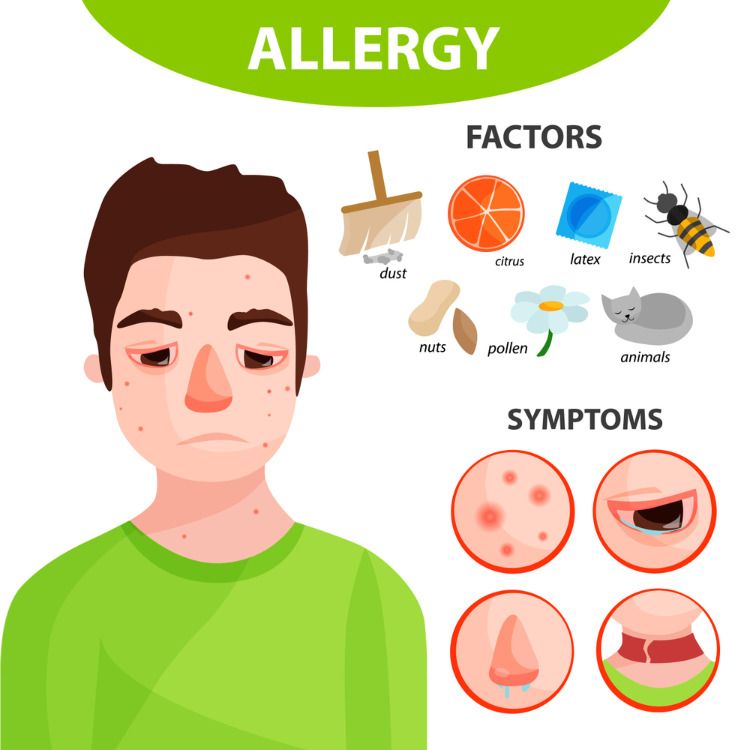
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as an itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction (anaphylaxis) is a medical emergency. Call 999 for an ambulance immediately if you think your child has anaphylaxis (even if they start to feel better).
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed around every 6 to 18 months to see if they have grown out of their allergy.
Read more about cows' milk allergy in children on National Institute for Health and Care Excellence (NICE).
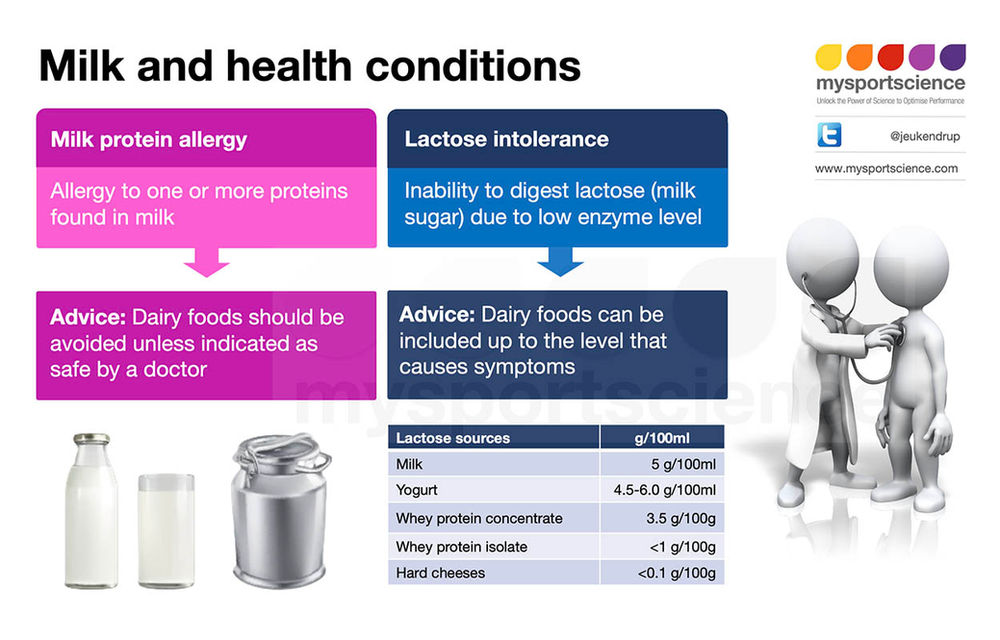
Could it be lactose intolerance?
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.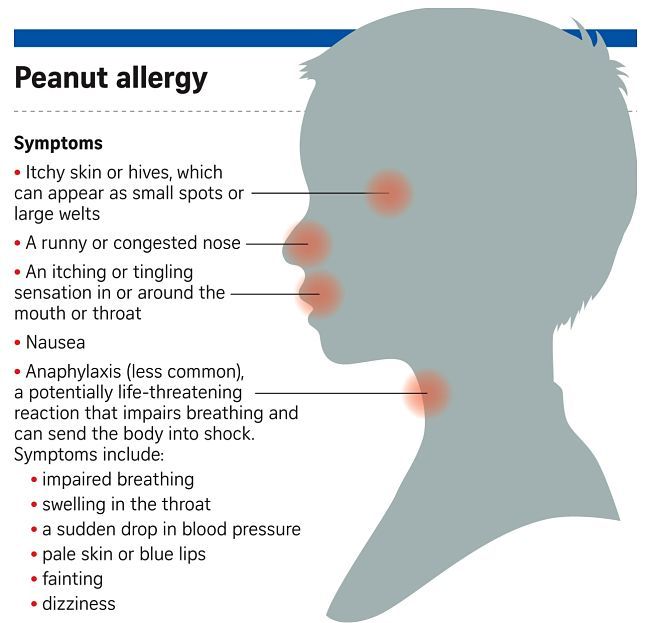
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- Your baby's first solid foods
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 28 November 2022
Next review due: 28 November 2025
Milk Allergy in Infants (for Parents)
What Is a Milk Allergy?
When a baby is allergic to milk, it means that their immune system, which normally fights infections, overreacts to proteins in cow's milk. Every time the baby has milk, the body thinks these proteins are harmful invaders and works hard to fight them.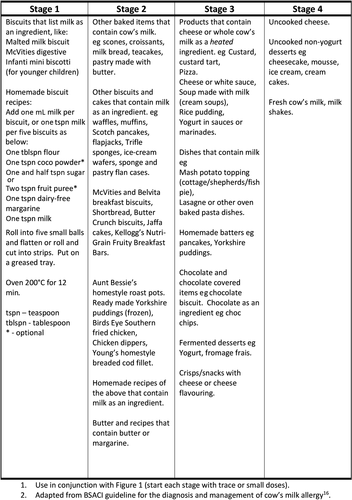 This causes an allergic reaction in which the body releases chemicals like
This causes an allergic reaction in which the body releases chemicals like
histamine.
Cow's milk is in most baby formulas. Babies with a milk allergy often show their first symptoms days to weeks after they first get cow milk-based formula. Breastfed infants can show symptoms when their mother has had milk products.
People of any age can have a milk allergy, but it's more common in young children. Many kids outgrow it, but some don't.
What Are the Signs & Symptoms of a Milk Allergy?
In children who show symptoms shortly after they have milk, an allergic reaction can cause:
- wheezing
- trouble breathing
- coughing
- hoarseness
- throat tightness
- stomach upset
- vomiting
- diarrhea
- itchy, watery, or swollen eyes
- hives
- swelling
- a drop in blood pressure causing lightheadedness or loss of consciousness
The severity of allergic reactions to milk can vary. The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
Children also can have:
- an intolerance to milk in which symptoms — such as loose stools, blood in the stool, refusal to eat, or irritability or colic — appear hours to days later
- lactose intolerance, which is when the body has trouble digesting milk
If you're not sure if your child has an intolerance versus an allergy, talk to your doctor.
How Is a Milk Allergy Diagnosed?
If you think your infant is allergic to milk, call your baby's doctor. The doctor will examine your baby, and might order some stool tests and blood tests. The doctor may refer you to an allergist, who might do skin testing. In skin testing, the doctor or nurse will place a tiny bit of milk protein on the skin, then make a small scratch on the skin. If your child reacts to the allergen, the skin will swell a little in that area like an insect bite.
If the allergist finds that your baby is at risk for a serious allergic reaction, they'll prescribe epinephrine auto-injectors.
How Is an Allergic Reaction Treated?
If your baby has a milk allergy (or any kind of serious food allergy), always have two epinephrine auto-injectors available in case of a severe reaction.
An epinephrine auto-injector is a prescription medicine that comes in a small, easy-to-carry container. It's easy to use. Your doctor will show you how. Kids who are old enough can be taught how to give themselves the injection. If they carry the epinephrine, it should be nearby, not left in a locker or in the nurse's office.
The doctor can also give you an allergy action plan, which helps you prepare for, recognize, and treat an allergic reaction. Share it with anyone who takes care of your child, including relatives, daycare providers, and babysitters.
Every second counts in an allergic reaction. If your child starts having serious allergic symptoms, like trouble breathing, give the epinephrine auto-injector right away. Also give it right away if the symptoms involve two different parts of the body, like hives with vomiting. Then call 911 and take your child to the emergency room. Your child needs to be under medical supervision because even if the worst seems to have passed, a second wave of serious symptoms can happen.
Also give it right away if the symptoms involve two different parts of the body, like hives with vomiting. Then call 911 and take your child to the emergency room. Your child needs to be under medical supervision because even if the worst seems to have passed, a second wave of serious symptoms can happen.
Sometimes allergists recommend also carrying over-the-counter (OTC)
antihistamines, as these can help treat mild allergy symptoms. Use an antihistamine after — not as a replacement for — the epinephrine shot during a life-threatening reaction.
What Can I Do if My Baby Has a Milk Allergy?
If You Breastfeed
If your breastfed infant has a milk allergy, talk to the allergist to see what changes you should make to your diet.
If You Formula Feed
If you're formula feeding, your doctor may advise you to switch to an extensively hydrolyzed formula or an amino acid-based formula in which the proteins are broken down into particles so that the formula is less likely to trigger an allergic reaction.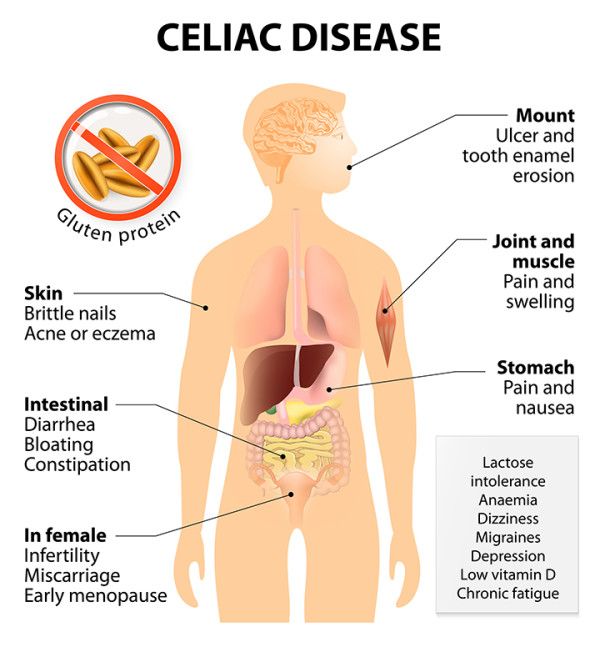
You also might see "partially hydrolyzed" formulas, but these aren't truly hypoallergenic and can lead to a significant allergic reaction.
If you're concerned about a milk allergy, it's always best to talk with your child's doctor and work together to choose a formula that's safe for your baby.
Do not try to make your own formula. Commercial formulas are approved by the U.S. Food and Drug Administration (FDA) and created through a very specialized process that cannot be duplicated at home. Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
When your child is ready for solids foods, the best way to be sure a food is milk-free is to read the food label. Manufacturers of foods sold in the United States must state on their labels whether the foods contain milk. Check the ingredients list first.
Some foods look OK from the ingredient list, but while being made they can have contact with milk. This is called cross-contamination. Look for advisory statements such as "May contain milk," "Processed in a facility that also processes milk," or "Manufactured on equipment also used for milk." Not all companies label for cross-contamination, so if in doubt, call or email the company to be sure.
This is called cross-contamination. Look for advisory statements such as "May contain milk," "Processed in a facility that also processes milk," or "Manufactured on equipment also used for milk." Not all companies label for cross-contamination, so if in doubt, call or email the company to be sure.
If you have any questions or concerns, talk with your child's doctor.
For more about managing food allergies, visit:
- Food Allergy Research and Education Network (FARE).
Reviewed by: Larissa Hirsch, MD
Date reviewed: January 2023
Cow's milk protein allergy in children (CMP)
Cow's milk protein allergy (common abbreviation - CMP) ranks first among all allergies in children of the first year of life.
The article was written by the leading allergist-immunologist, Euromed Kids pediatrician Artem Andreevich Batin
011 cow's milk.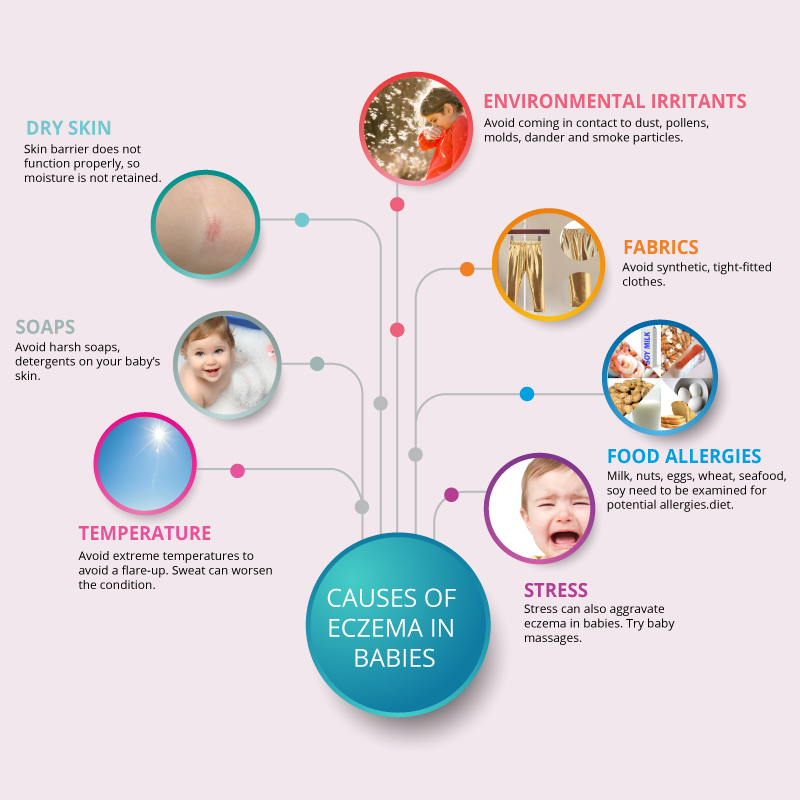
Allergy to milk protein is due to the fact that the child's immune system perceives this protein as foreign and activates the body's defense reactions.
Milk intolerance is the result of insufficient work or an insufficient amount of enzymes necessary for its digestion. This condition is called lactase deficiency , and it is quite successfully corrected by the additional intake of enzymes.
Important: even if the baby is exclusively breastfed, allergies can occur if milk is present in the mother's diet.
One of the most common manifestations of cow's milk protein allergy is atopic dermatitis .
Favorite localizations - face, especially cheeks, elbows, popliteal fossae, but often elements appear on the body. At first, the skin becomes dry, and with an increase in symptoms, cracks, weeping, and crusts appear.
More about atopic dermatitis…
In addition to the so-called “skin symptoms”, there are other manifestations associated with the digestive system:
- regurgitation;
- vomiting;
- intestinal colic;
- flatulence, diarrhoea;
- the child worries, cries, does not sleep well.
IMPORTANT! Information from the article cannot be used for self-diagnosis and self-treatment! Only a doctor can prescribe the necessary examinations, establish a diagnosis and draw up a treatment plan for a consultation!
If you notice even some of these symptoms, bring them to the attention of a pediatrician who constantly monitors your child. You will also need to consult a pediatric allergist-immunologist to clarify the diagnosis.
At the appointment, the doctor will conduct a thorough survey of the parents to clarify all the characteristics of the child, assess the symptoms of the disease, and, if necessary, recommend an allergological examination to confirm the diagnosis.
The treatment of allergy to cow's milk protein consists in following a special diet , which completely excludes the allergen (protein) from entering the child's body.
To restore and care for the skin, the doctor will definitely recommend various products and emollients that will restore the integrity of the skin and sufficiently moisturize it.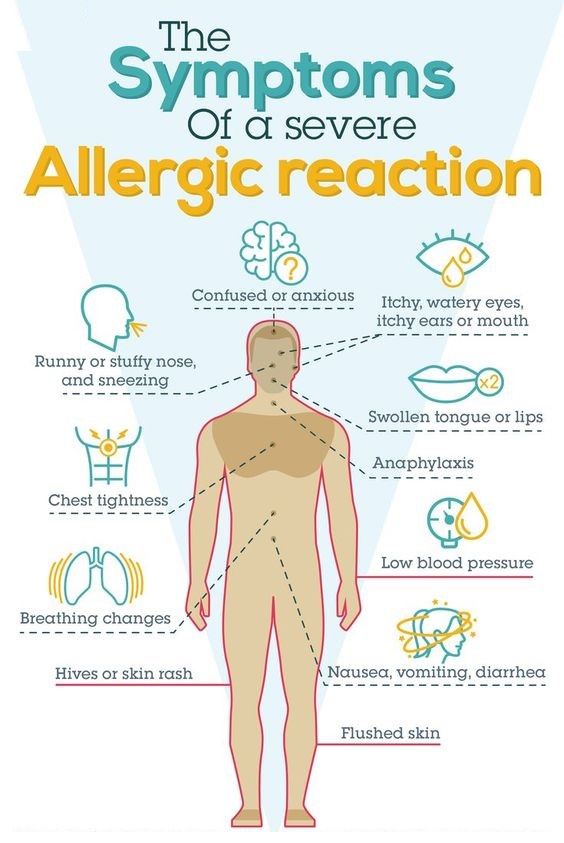
If the child is breastfed , then a diet that completely excludes milk and products containing milk is intended for the mother. Especially carefully you need to monitor the content of milk in various semi-finished products, cookies, etc.
If the baby is formula-fed , the attending physician will certainly recommend several special therapeutic mixtures.
What makes these formulas different from regular formulas is that they allow your baby to get all the nutrients they need to grow and develop without encountering an allergen. The choice of mixture depends on various factors: the severity of the disease, the taste preferences of the child. For mild and moderate degrees, mixtures based on highly hydrolyzed proteins are recommended, for severe degrees, amino acid mixtures; but in each case, this issue is decided individually.
The prognosis for allergy to cow's milk protein is favorable: by the age of 5-6 years, in 90% of allergic children, this type of allergy disappears without a trace.
Therefore, if your baby has anxiety symptoms, do not postpone a visit to the doctor.
Allergy to cow's milk protein in children
Food allergy is a food-induced adverse (pathological) reaction based on immune mechanisms. In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
A distinction is made between cow's milk protein allergy and cow's milk protein intolerance. In the first case immune mechanisms are involved, in the second case - the baby simply does not have enough enzymes to digest cow's milk protein (for example, lactase deficiency).
There are only 36 cow's milk protein allergens, but 4 of them most often cause food allergies.
Casein is 80% BCM, it is heat stable (does not break down when boiled) and is not a species-specific protein. This means that if you are allergic to it, you may be allergic to the milk of other animal species.
This means that if you are allergic to it, you may be allergic to the milk of other animal species.
β - lactoglobulin has the highest allergenic activity, species-specific, does not break down when boiled. This protein is not found in human milk.
α - lactalbumin is destroyed by boiling, species-specific.
Bovine serum albumin is not destroyed by boiling If an allergy to this cow's milk protein is detected, the child may also react to beef and veal meat.
It should be noted that mainly children who are formula-fed formulas based on cow's milk protein suffer from allergy to cow's milk protein.
Also, this type of allergy can develop in children who are breastfed - if the diet of a nursing mother contains products containing cow's milk protein (milk, cheese, cottage cheese, sour cream, butter, fermented milk products), especially in large quantities.
Which symptoms suggest that the baby may be allergic to CMP:
- Skin manifestations (dry skin, dry numb rash, skin itching).
- Gastrointestinal manifestations (bloating, regurgitation, vomiting, loose stools, possibly stools with mucus and blood streaks).
- Respiratory manifestations (itchy eyes, cough, nasal congestion and even urticaria and Quincke's edema). These symptoms are rare in toddlers, but still possible.
Diagnosis
I must say that if the first manifestations of food allergy in a baby appeared after switching to artificial feeding with a “regular” adapted formula based on cow's milk, then this is a reason to suspect cow's milk proteins as an allergen.
Further correctness is important history taking : the doctor will definitely find out if anyone in your family suffers from allergic diseases (bronchial asthma, allergic rhinitis, atopic dermatitis, hay fever). If the family has these diseases, the risk of developing allergies in the baby increases.
At the doctor's discretion, it is possible to take blood from a child for the presence of immunoglobulin E (IgE) antibodies to cow's milk proteins, which were mentioned above.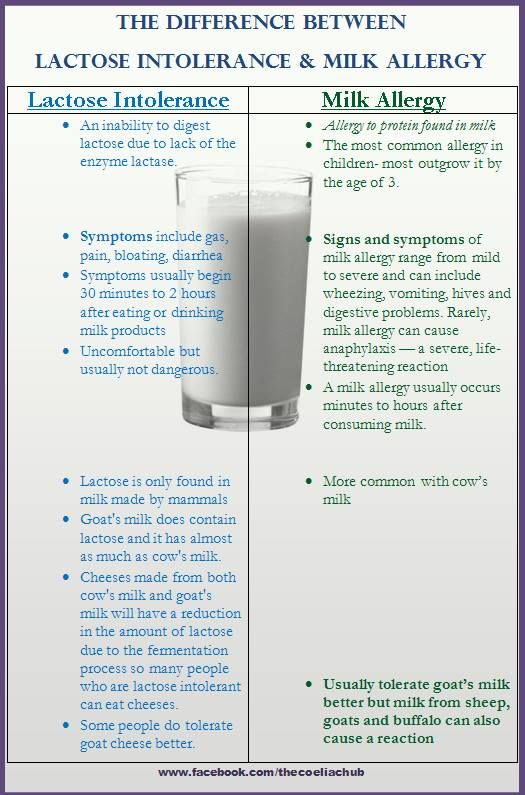 In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy. Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy. Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
And the simplest, most important and accessible method is the diagnostic diet with the exclusion of products from the child's diet (or from the mother's diet during breastfeeding) containing CMB. The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
If the child's condition improves, you may need challenge test . This means the introduction of dairy products into the child's diet again. And if the manifestations of allergies return, this will prove an allergy to BCM. This test is carried out under strict medical supervision.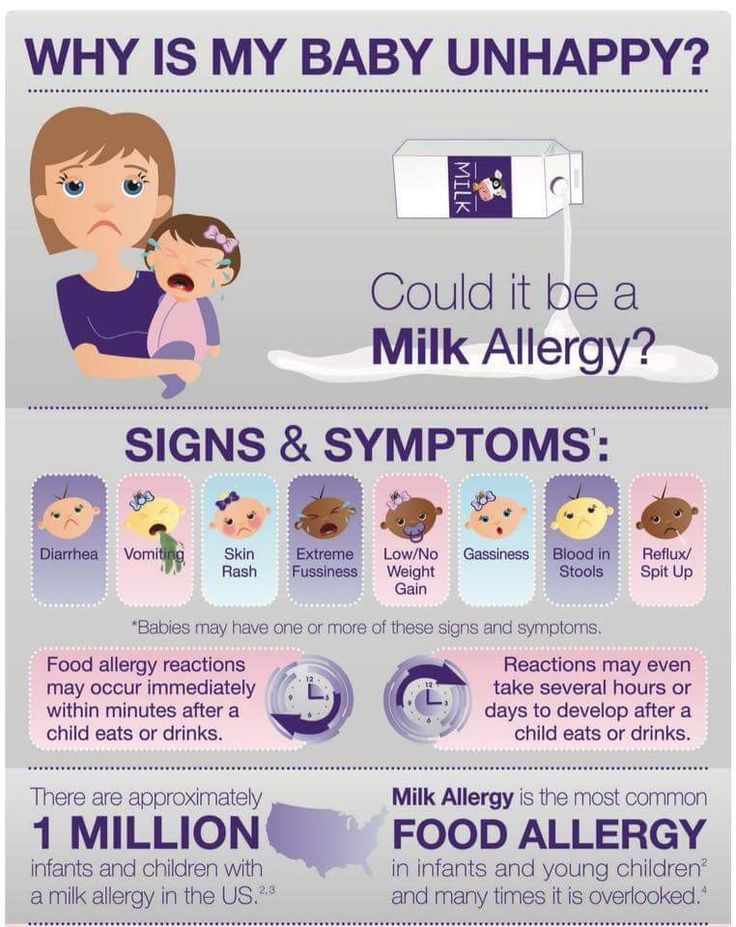
In children who are fed exclusively with breast milk, it is necessary to exclude products containing CMP from the diet of mothers .
There are 3 types of mixtures:
- based on the hydrolysis of whey proteins;
- based on the hydrolysis of the casein fraction;
- based on amino acids.
Allergy is possible for the first two options, the reaction is very unlikely for the third option.
If the baby is bottle-fed, then it must be transferred to amino acid blend or highly hydrolyzed blend. Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Usually, allergists first transfer children to mixtures based on complete hydrolysis of BCM or casein, if there is no proper effect within 2-3 weeks, it is recommended to transfer the baby to an amino acid mixture.
Perhaps, if the child has severe manifestations of food allergies, the doctor will advise you to immediately transfer the baby to an amino acid mixture. By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
Amino acid mixtures are more easily tolerated by children with various forms of food allergies, as they do not have the bitter taste characteristic of mixtures with a high degree of protein hydrolysis.
Amino acid mixtures can be used both for the short term diagnosis of CMP allergy and as a dietary base for long term use in children with food allergies.
Diet duration - at least 6 months . Then the issue of transferring the baby to a hypoallergenic mixture is decided. In case of recurrence of symptoms, the introduction of dairy products is postponed for another 6 months.
The prognosis for CMP allergy in infants and young children with the right tactics of managing patients is favorable.