Malposition of the uterus
Retroversion of the uterus Information | Mount Sinai
Uterus retroversion; Malposition of the uterus; Tipped uterus; Tilted uterus
Retroversion of the uterus occurs when a woman's uterus (womb) tilts backward rather than forward. It is commonly called a "tipped uterus."
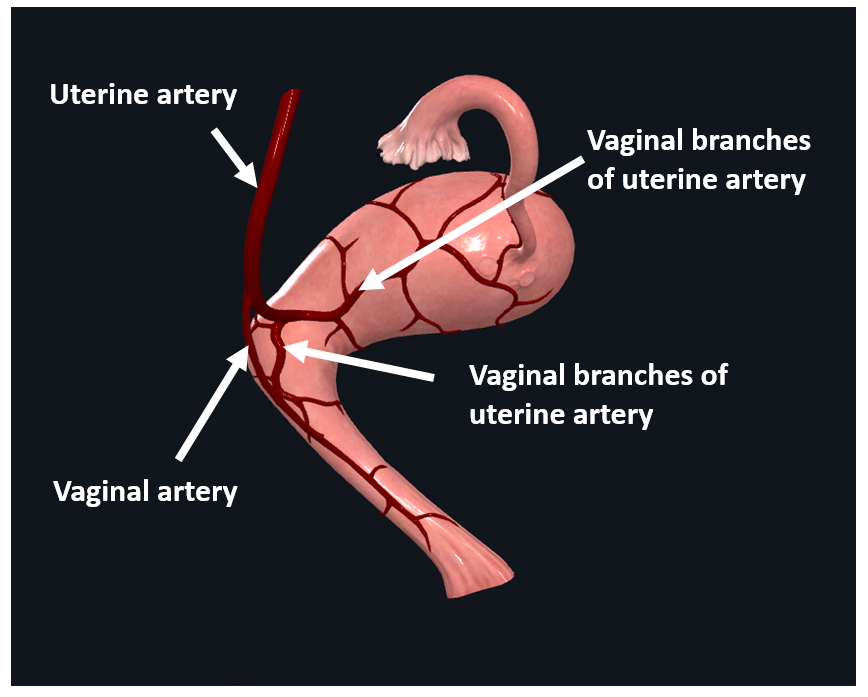
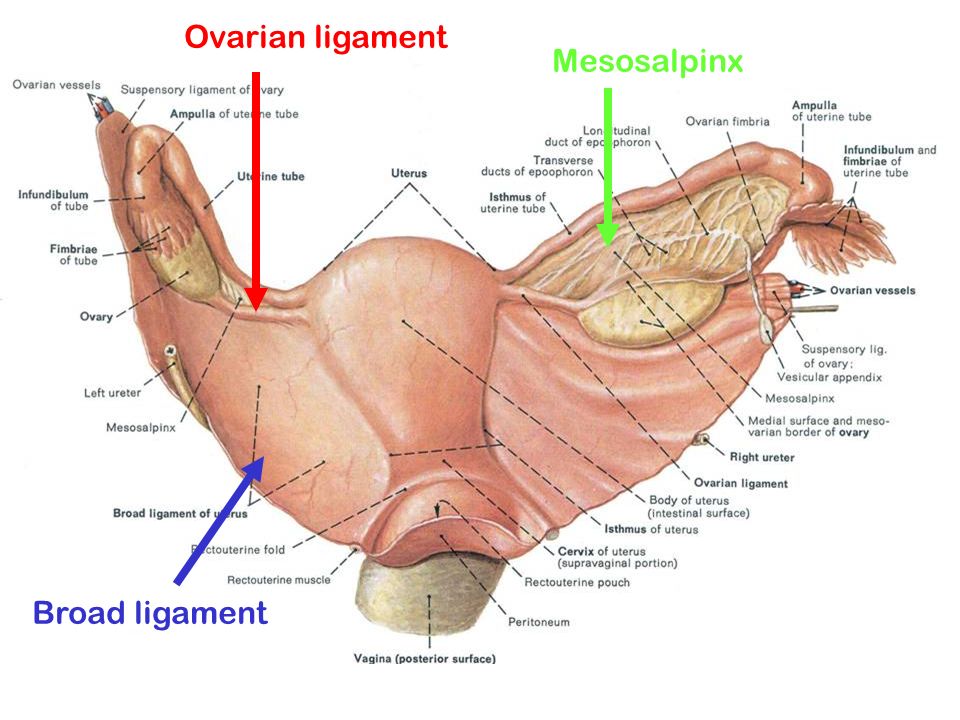
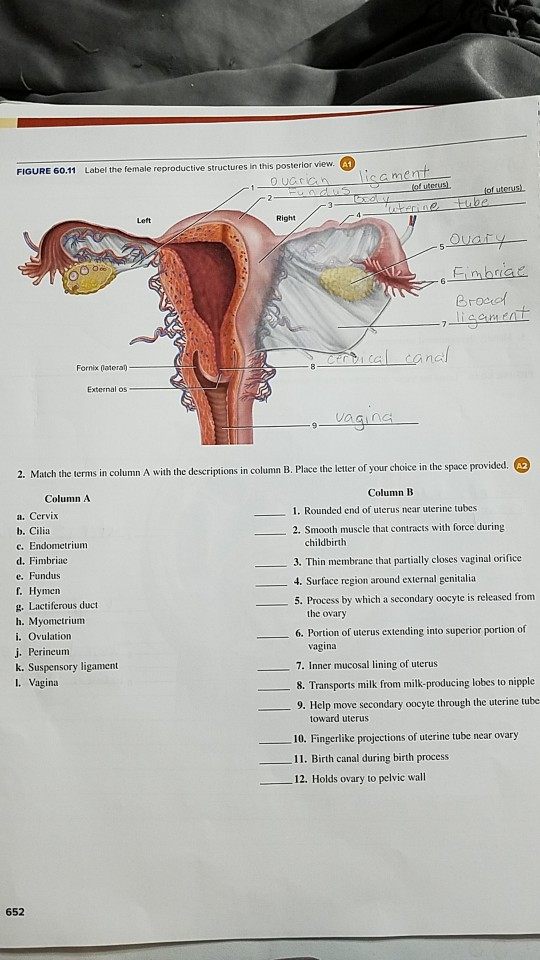
External structures of the female reproductive anatomy include the labium minora and majora, the vagina and the clitoris. Internal structures include the uterus, ovaries, and cervix.
The uterus is a hollow muscular organ located in the female pelvis between the bladder and rectum. The ovaries produce the eggs that travel through the fallopian tubes. Once the egg has left the ovary it can be fertilized and implant itself in the lining of the uterus. The main function of the uterus is to nourish the developing fetus prior to birth.
Causes
Retroversion of the uterus is common. Approximately 1 in 5 women has this condition. The problem may also occur due to weakening of the pelvic ligaments at the time of menopause.
Scar tissue or adhesions in the pelvis can also hold the uterus in a retroverted position. Scarring may come from:
- Endometriosis
- Infection in uterus or tubes
- Pelvic surgery
Symptoms
Retroversion of the uterus almost never causes any symptoms.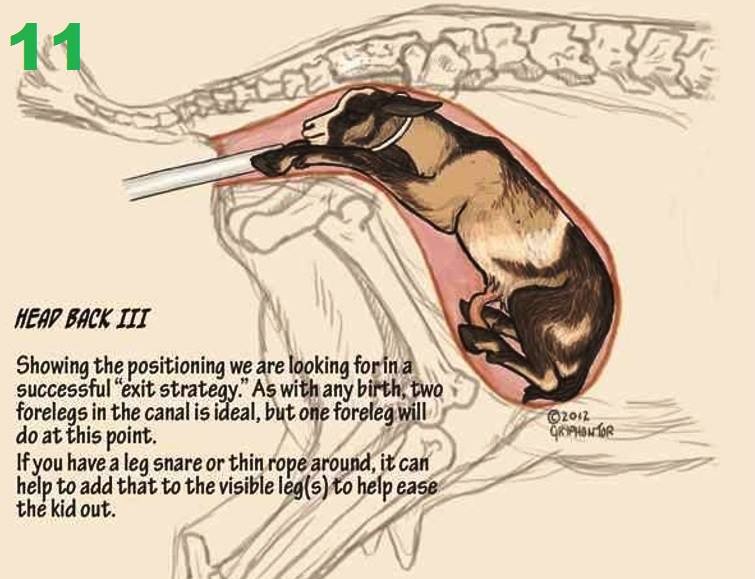
Rarely, it may cause pain or discomfort.
Exams and Tests
A pelvic exam will show the position of the uterus. However, a tipped uterus can sometimes be mistaken for a pelvic mass or a growing fibroid. A rectovaginal exam may be used to distinguish between a mass and a retroverted uterus.
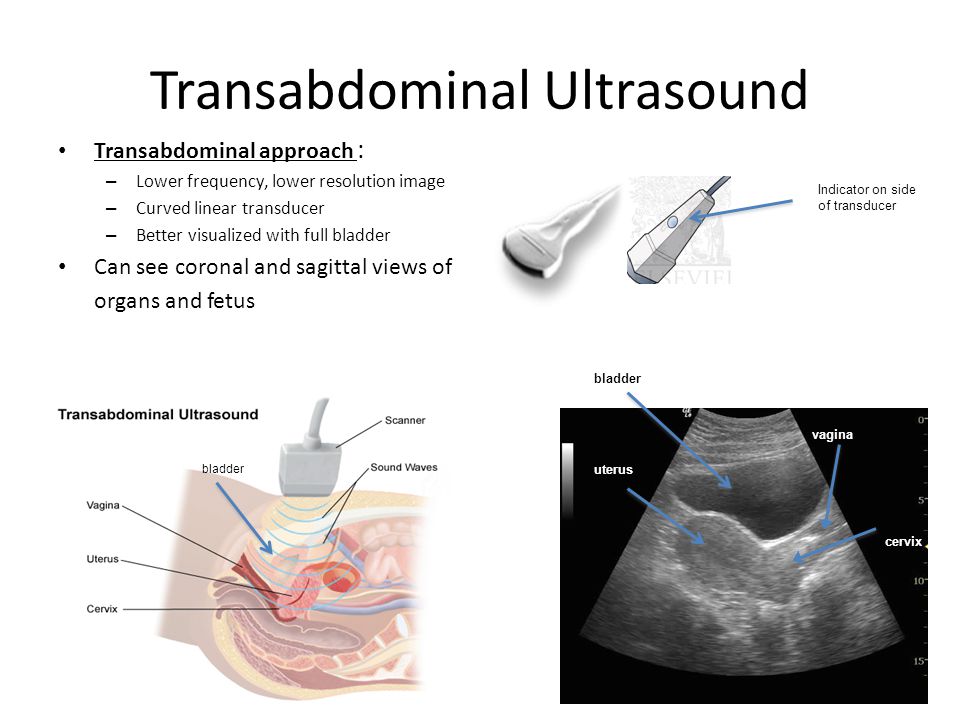
An ultrasound exam can accurately determine the exact position of the uterus.
Treatment
Treatment is not needed most of the time.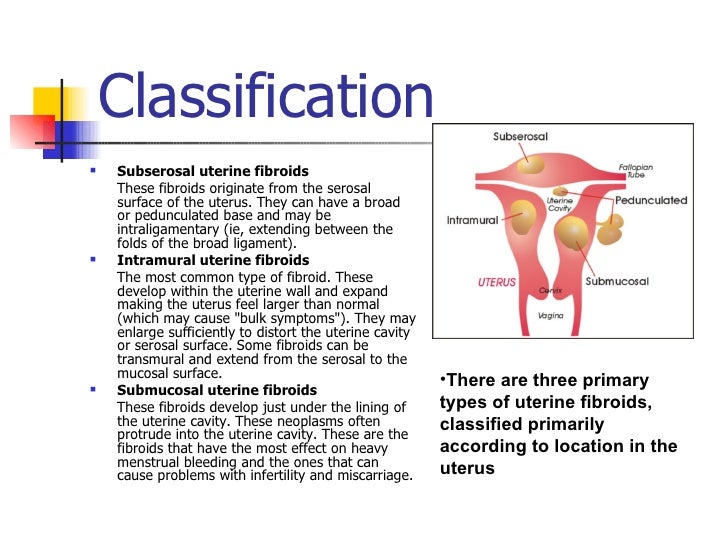 Underlying disorders, such as endometriosis or adhesions, should be treated as needed.
Underlying disorders, such as endometriosis or adhesions, should be treated as needed.
Outlook (Prognosis)
In most cases, the condition does not cause problems.
Possible Complications
In most cases, a retroverted uterus is a normal finding. However, in some cases it may be caused by endometriosis, salpingitis, or pressure from a growing tumor.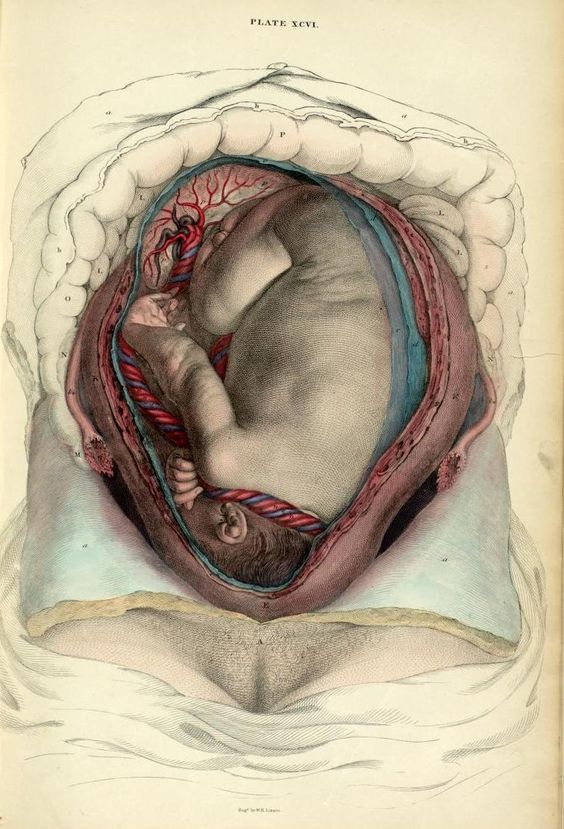
When to Contact a Medical Professional
Call your health care provider if you have ongoing pelvic pain or discomfort.
Prevention
There is no way to prevent the problem. Early treatment of uterine infections or endometriosis may reduce the chances of a change in the position of the uterus.
Advincula A, Truong M, Lobo RA.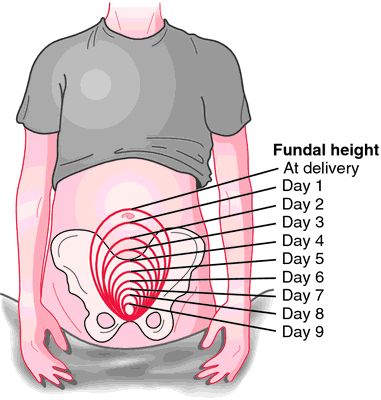 Endometriosis: etiology, pathology, diagnosis, management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 19.
Endometriosis: etiology, pathology, diagnosis, management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 19.
Ball JW, Dains JE, Flynn JA, Solomon BS, Stewart RW. Female genitalia. In: Ball JW, Dains JE, Flynn JA, Solomon BS, Stewart RW, eds. Seidel's Guide to Physical Examination. 10th ed. St Louis, MO: Elsevier; 2023:chap 19.
Hertzberg BS, Middleton WD. Pelvis and uterus. In: Hertzberg BS, Middleton WD, eds. Ultrasound: The Requisites. 3rd ed. Philadelphia, PA: Elsevier; 2016:chap 23.
Last reviewed on: 4/19/2022
Reviewed by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Laparoscopy Hospital - Frequently asked questions about Malposition of Uterus
Frequently asked questions about Malposition of Uterus
Mal-position of the Uterus
Intermittent myometrial contractions and changes in uterine position are normal during pregnancy.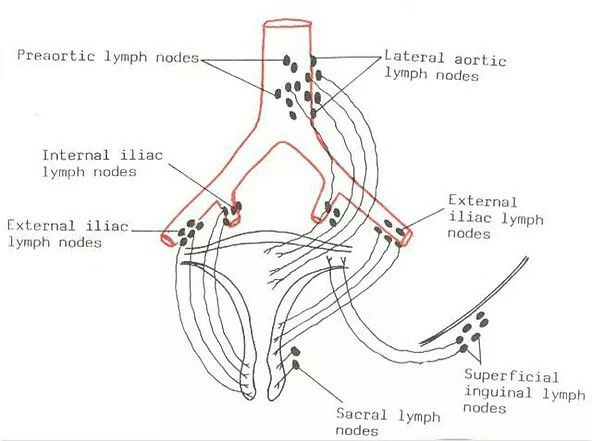 Infrequently, various obstetric complications result from uterine malpositioning (retroversion or incarceration), inversion, and, in rare cases, prolapse, torsion, or herniation. Special devices and many surgical techniques were developed to either reposition the uterus or to hold it in its presumed correct location. These operations and manipulations were believed to be necessary for the maintenance or restoration of normal functioning.
Infrequently, various obstetric complications result from uterine malpositioning (retroversion or incarceration), inversion, and, in rare cases, prolapse, torsion, or herniation. Special devices and many surgical techniques were developed to either reposition the uterus or to hold it in its presumed correct location. These operations and manipulations were believed to be necessary for the maintenance or restoration of normal functioning.
In modern time, surgery for the correction of uterine retroversion in the absence of evidence of endometriosis or other specific pathologic conditions has fallen into disrepute.
Retroversion from any cause becomes an issue of clinical importance if it progresses to uterine incarceration once a pregnancy is established. Fixation of the uterus by adhesions is also a risk factor for the rare complication of uterine torsion.
Uterine Retroversion or Incarceration
Frequency
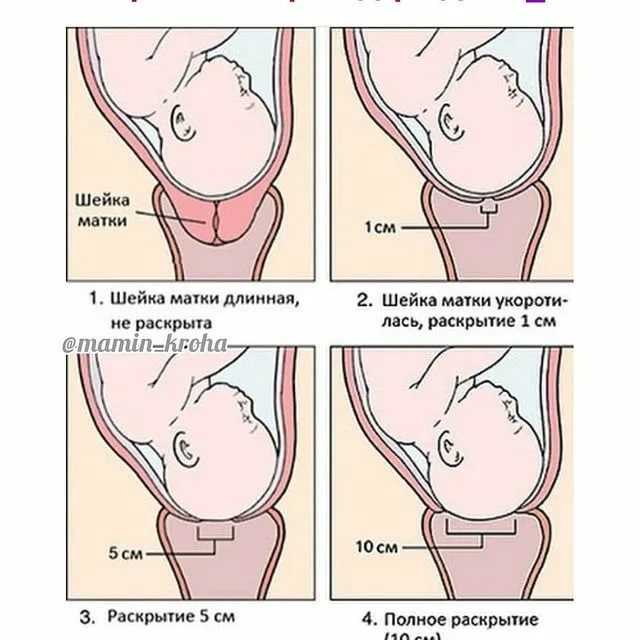
During early pregnancy, uterine retroversion is a normal positional variant.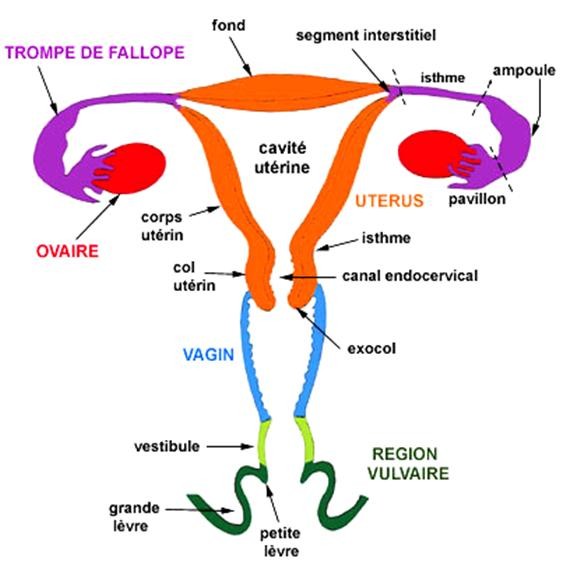 Typically, first-trimester retroversion is intermittently present 10-20% of the time. If retroversion persists into the mid trimester, uterine incarceration is possible, but the likelihood of this complication is low.
Typically, first-trimester retroversion is intermittently present 10-20% of the time. If retroversion persists into the mid trimester, uterine incarceration is possible, but the likelihood of this complication is low.
Pathophysiology
Normal pelvic anatomy permits the fundus of the uterus to move relatively freely in the sagittal, vertical, oblique, and anteroposterior planes. In retroversion, the uterus is tipped posteriorly and may be fixed in this position by the presence of adhesions. Cases of marked retroversion with the uterine fundus positioned below the sacral promontory in the hollow of the pelvis lead to incarceration as the uterus enlarges during pregnancy. As the uterus becomes bigger, the fundus progressively moves posteriorly as it cannot escape from the cul de sac. As this occurs, the cervix is driven underneath and then behind the pubic symphysis. At some critical juncture of uterine size, tissue laxity, and other unknown factors, the uterus becomes entrapped.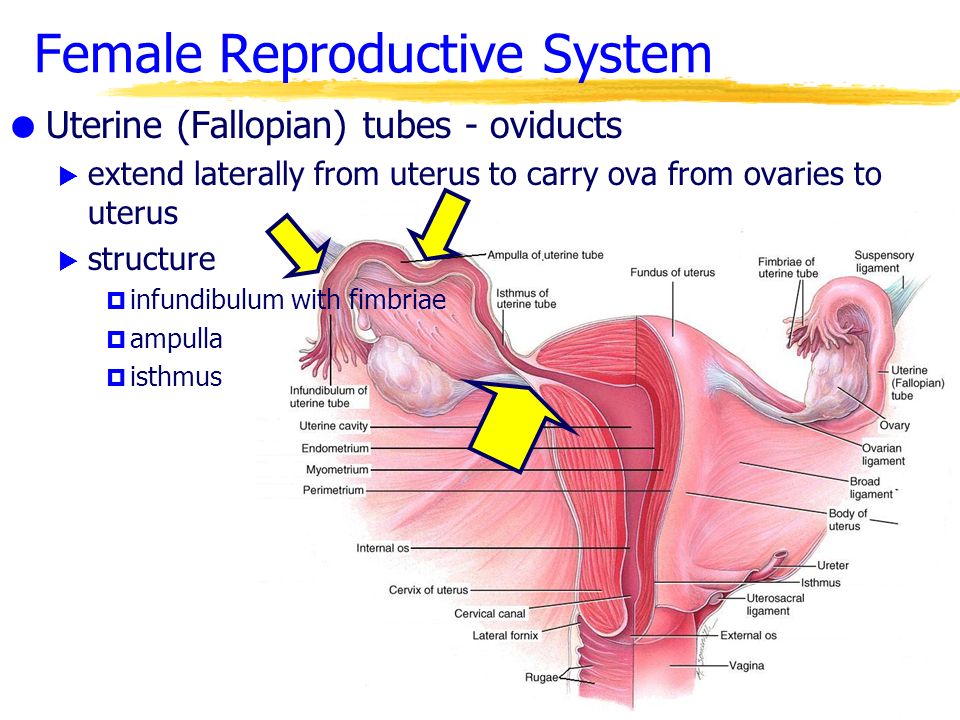 At this point, the fundus cannot easily exit the hollow of the sacrum or it is incapable of spontaneously rotating anteriorly past the sacral promontory.
At this point, the fundus cannot easily exit the hollow of the sacrum or it is incapable of spontaneously rotating anteriorly past the sacral promontory.
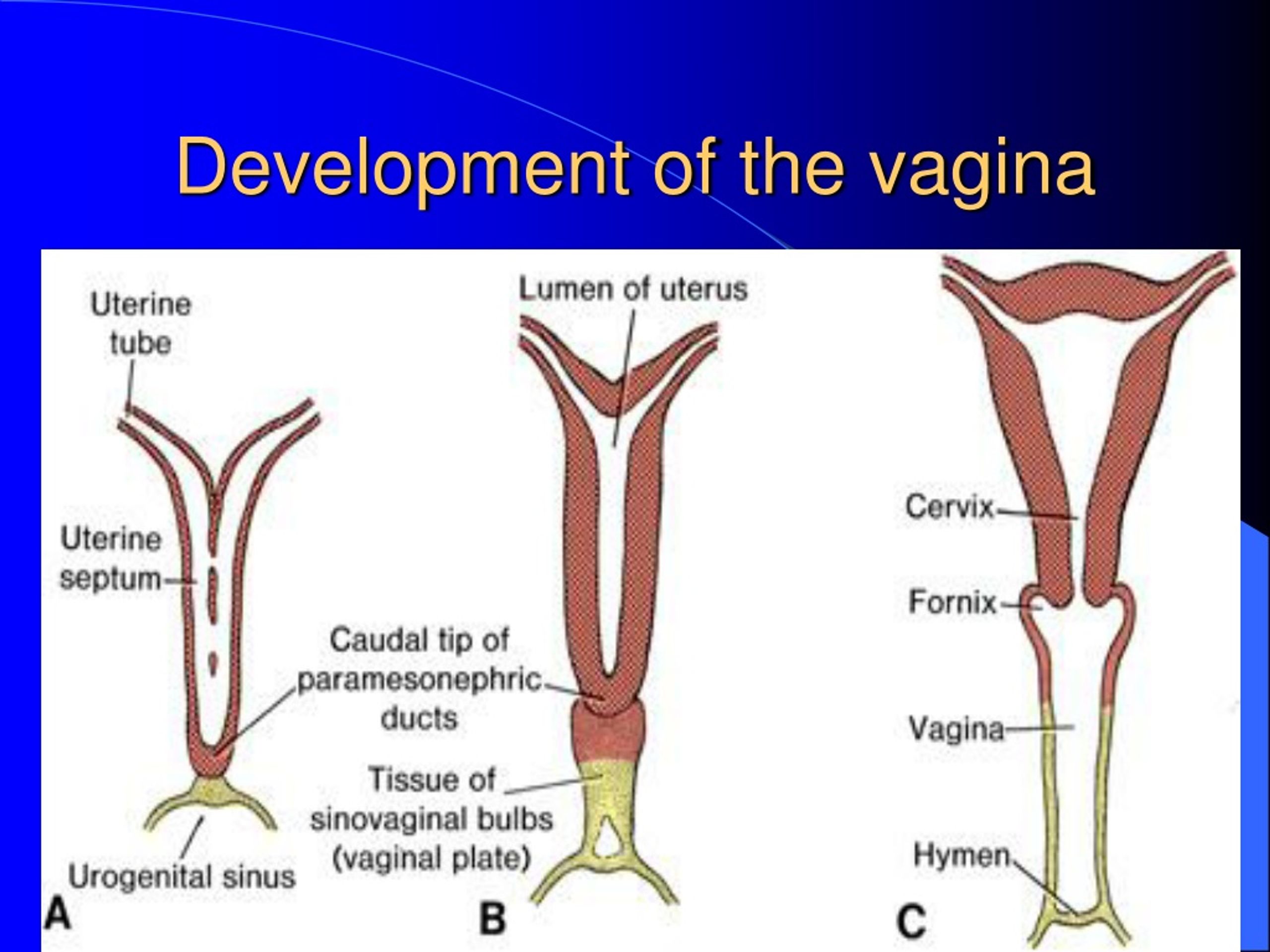
Entrapment usually occurs after the 12th week of gestation. However, it may occur earlier if special conditions such as a multiple gestation or a müllerian anomaly exist, or if a strategically located leiomyoma or adnexal tumor is present.
In cases, a variety of conditions are possible:
- Adhesions due to previous surgery
- Adhesions due to endometriosis
- Adhesions due to previous pelvic inflammatory disease
- Müllerian abnormalities with a posterior uterine horn or a rudimentary horn
- Adnexal tumor or a fundal or posterior leiomyoma
As gestation advances, the incarceration worsens. Because the enlarging uterus cannot rotate anteriorly, it is wedged progressively firmly into the hollow of sacrum while the cervix exerts increasing pressure toward the urethra and/or bladder. Normal voiding eventually becomes difficult or impossible as progressive upward cervical pressure restricts normal funneling of the bladder outlet and obliterates the posterior uterovesical angle.
Clinical Presentation
Recurrence is possible. Thus, women with a history of symptomatic incarceration should be evaluated frequently in the late first trimester and early second trimester to ensure that the uterus does not become fully incarcerated if it remains retroverted.
When incarceration occurs, the acute symptoms mimic those of more common obstetric conditions. Yet, in most instances, the correct diagnosis is readily established by reviewing the clinical history and performing a pelvic examination. Conducting a real-time ultrasonic examination is confirmatory.
Uterine repositioning is usually easy and successful if the diagnosis is made early.
Common clinical symptoms include the following:
- Vaginal bleeding (threatened spontaneous abortion)
- Pain
- Uterine contractions or cramping
- Paradoxical urinary symptoms (e.g., incontinence, frequency, and, eventually, retention)
- Bowel dysfunction (e.g., tenesmus, rectal pressure, constipation)
Diagnosis
The diagnosis of incarceration is established by performing a pelvic examination and pelvic sonography and by considering these data in combination with the characteristic clinical history.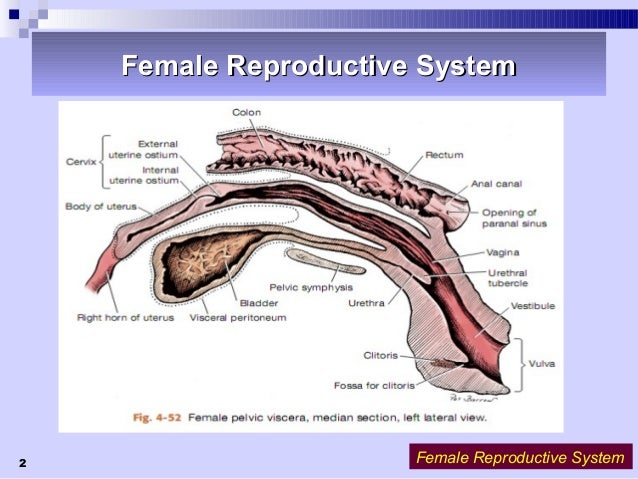
In cases of retroversion with incarceration, clinical examination usually yields the following striking findings:
- A soft, smooth, non tender mass filling the cul-de-sac
- Acute anterior angulation of the vagina
- A cervix abutting firmly against or positioned well behind the pubic symphysis
- An inability to palpate the uterus during abdominal examination or a uterine fundus too small for the known gestational age
Treatment
Possible therapies for retroversion with incarceration include the following:
- Manual uterine replacement: manipulation of the uterus into its usual anatomic position, with or without tocolysis and/or anesthesia
- Bladder decompression by means of intermittent or indwelling catheter drainage
- Colonoscopic manipulation of the uterine fundus with the patient under anesthesia
- Patient positioning (e.g., intermittent knee-chest or all-fours positioning, sleeping prone)
- Application of specialized and rarely attempted techniques of replacement (e.
 g., use of a mercury-filled Voorhees bag in the vagina, amniocentesis with manipulations or surgical exploration and replacement)
g., use of a mercury-filled Voorhees bag in the vagina, amniocentesis with manipulations or surgical exploration and replacement)
Bladder decompression and patient positioning
The best initial treatment for symptomatic mid trimester incarceration of a normal uterus is a trial of bladder decompression combined with a program of patient positioning. Such management relieves most cases.
Manipulation of the uterus
Before the procedure begins, the woman is instructed to void, or, if a Foley catheter was placed, it is fully drained. An attendant is present to support and encourage the patient and to help prevent a fall. In the replacement procedure, a speculum is passed and the anterior lip of the cervix is grasped by using a long Allis clamp or another atraumatic clamp.
The patient is then placed in the knee-chest or all-fours position. The surgeon inserts a finger into the vagina or rectum and applies pressure to the incarcerated fundus while simultaneously applying gentle but constant traction to the cervix.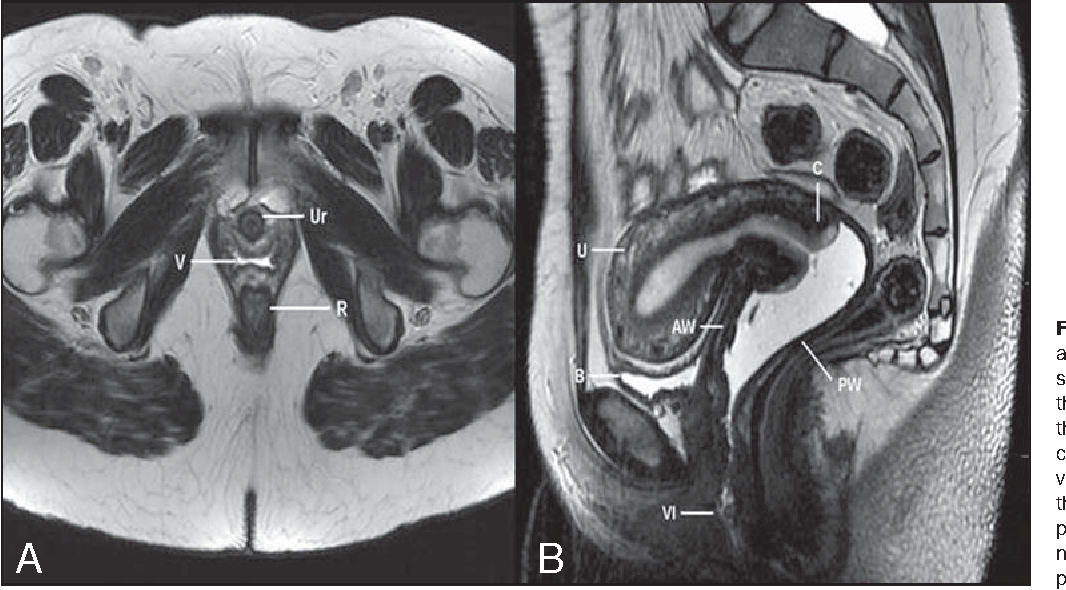 With this combined technique, the uterus should slowly rotate into its normal position. In theory, passing the fundus to either side of the sacral promontory, where more room is available, is probably best. Use of real-time sonographic guidance during manipulation procedures is prudent. Successful replacement is verified by means of palpation and real-time ultrasonography.
With this combined technique, the uterus should slowly rotate into its normal position. In theory, passing the fundus to either side of the sacral promontory, where more room is available, is probably best. Use of real-time sonographic guidance during manipulation procedures is prudent. Successful replacement is verified by means of palpation and real-time ultrasonography.
Postprocedural care
After any procedures to attempt uterine replacement, administration of Rh immunoglobulin is indicated in Rh-negative patients who are not isoimmunized.
In rare cases of chronic uterine retroversion, ballooning out of the uterine wall (sacculation) may permit the uterus to expand abdominally. If this occurs, the pregnancy may progress even into the third trimester. In such instances, the correct diagnosis is established only when dystocia in labor ensues or when abdominal and/or pelvic examination reveals markedly unusual findings that lead to an MRI study. In the rare case that reaches the third trimester, the uterine malpositioning is fixed and cesarean delivery is required. In the mid trimester, spontaneous abortion may occur because of incarceration alone, or it may follow manual uterine replacement. The risk of such loss is believed to be low.
In the mid trimester, spontaneous abortion may occur because of incarceration alone, or it may follow manual uterine replacement. The risk of such loss is believed to be low.
Etiology of retroversion
In non pregnant women, if retroversion alone is the cause of symptoms, these are usually minimal. Pelvic pain and similar symptoms are principally due to coincidental pathology. Evidence to show that isolated retroversion is responsible for abortion or infertility is lacking. When these conditions are encountered, another etiology must be sought.
Multiple gestations
Multiple gestations, which now often occur in association with assisted reproductive technologies, are special cases. In this setting, the uterus can become incarcerated earlier in gestation than when only a single fetus is present. This change is presumably due simply to the increased size of the uterus. Therefore, if characteristic symptoms occur in women with known multiple gestations—even when the pregnancy has not reached 12 weeks of gestation—retroversion or incarceration should remain in the differential diagnosis.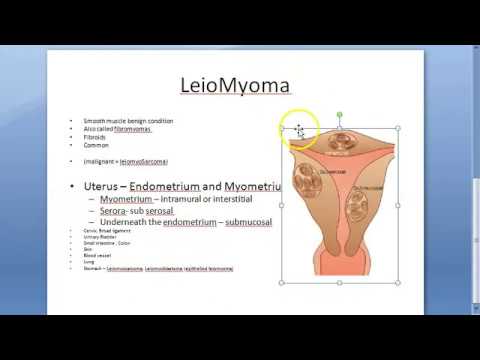
Persistent retroversion
In a few cases, the uterus remains retroverted and cannot be repositioned despite the administration of tocolysis and the use of regional anesthesia. The best management strategy in this setting is moot.
Counseling
Patients should be informed that both symptomatic incarceration and efforts for its relief carry some risk of pregnancy loss.
Ultrasonography
Because of the general uncertainties, a real-time sonographic examination should precede any intervention. This imaging study is done to reassure both the patient and practitioner, to verify the original diagnosis, to confirm that an anatomically normal and living fetus is present, and to verify that a mass or tumor is not the cause of the incarceration. The study is repeated after repositioning to confirm success of the procedure to verify the presence of an active fetus and normal amniotic fluid.
Other Syndromes of Pelvic Pain/Retroversion
Allen-Masters syndrome: The pelvic congestion syndrome
In non pregnant patients, the evaluation of chronic pelvic pain that accompanies uterine retroversion includes a consideration of 2 indistinct and somewhat suspect syndrome complexes: pelvic congestion syndrome (PCS) and Allen-Masters syndrome (AMS).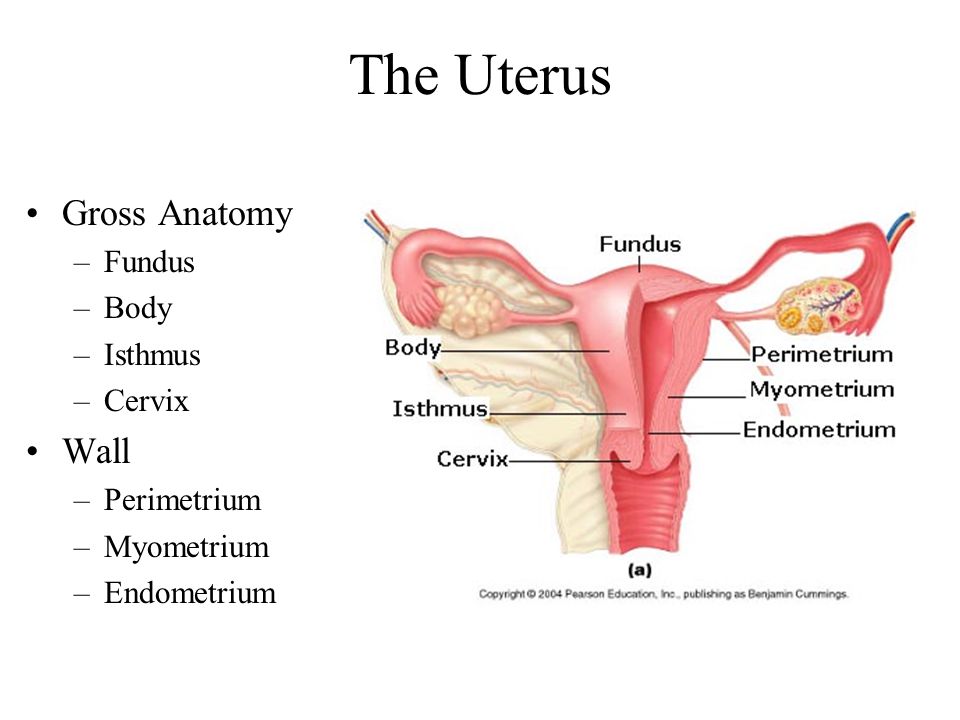
Pelvic congestion (Taylor) syndrome
Another possible diagnosis is PCS, or Taylor syndrome. This condition is characterized by menometrorrhagia and symptoms of continuous pelvic pain. On examination, the uterus is variably enlarged and soft, and some degree of tenderness is present. Uterine retroversion is again a common but not invariable finding. The cervix may be patulous or cyanotic. Among other treatment possibilities, both hysterectomy and vascular embolization have been used to manage PCS. The symptoms of this condition are nonspecific and poorly defined. Both this and the AMS are suspect diagnostic entities. In unusual or difficult cases, MRI can safely complement ultrasonography to help establish the correct diagnosis.
Uterine Torsion
Frequency
Uterine torsion is a rare condition in humans, and the existing papers are restricted to scattered case reports. Most cases of torsion are reported in the veterinary literature.
Pathophysiology
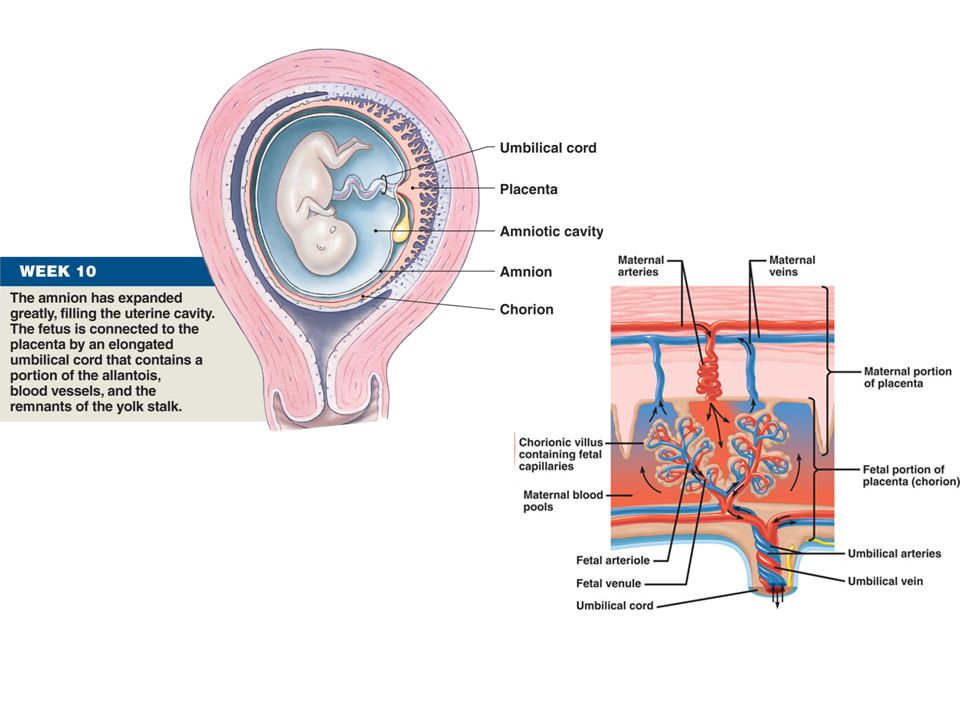
Dextrorotation is the most common finding. This is the normal orientation of the myometrial fibers. In rare situations, the torsion is of a sufficient degree to interfere with uterine circulation. This results in acute maternal symptoms or threatens fetal survival by directly restricting blood flow or by inducing abruption placentae.
This is the normal orientation of the myometrial fibers. In rare situations, the torsion is of a sufficient degree to interfere with uterine circulation. This results in acute maternal symptoms or threatens fetal survival by directly restricting blood flow or by inducing abruption placentae.
Entities reportedly associated with torsion include the following:
- External cephalic version procedures
- Interstitial pregnancy
- Abnormal fetal presentation (e.g., a transverse lie)
- Pelvic adhesions
- Distortion in uterine shape due to uterine leiomyomas
- Müllerian anomalies
- Large ovarian neoplasms that distort the shape or position of the uterus
- Congenital weakness at the junction of the cervix and uterine corpus
- Sudden maternal movements, as may occur during automobile accidents or, most rarely, during normal activity
- Long or rigid cervix or structural weakness at the junction of the cervix and the uterine corpus (possibly after a prior cesarean delivery)
- Abnormal pelvic architecture
- Hydramnios
- Multiple gestation
- Hyperactive fetus
- Unknown and/or idiopathic factors
Clinical Presentation
If the torsion occurs at term, obstructed labor is possible, or an acutely abnormal electronic fetal monitoring tracing may develop.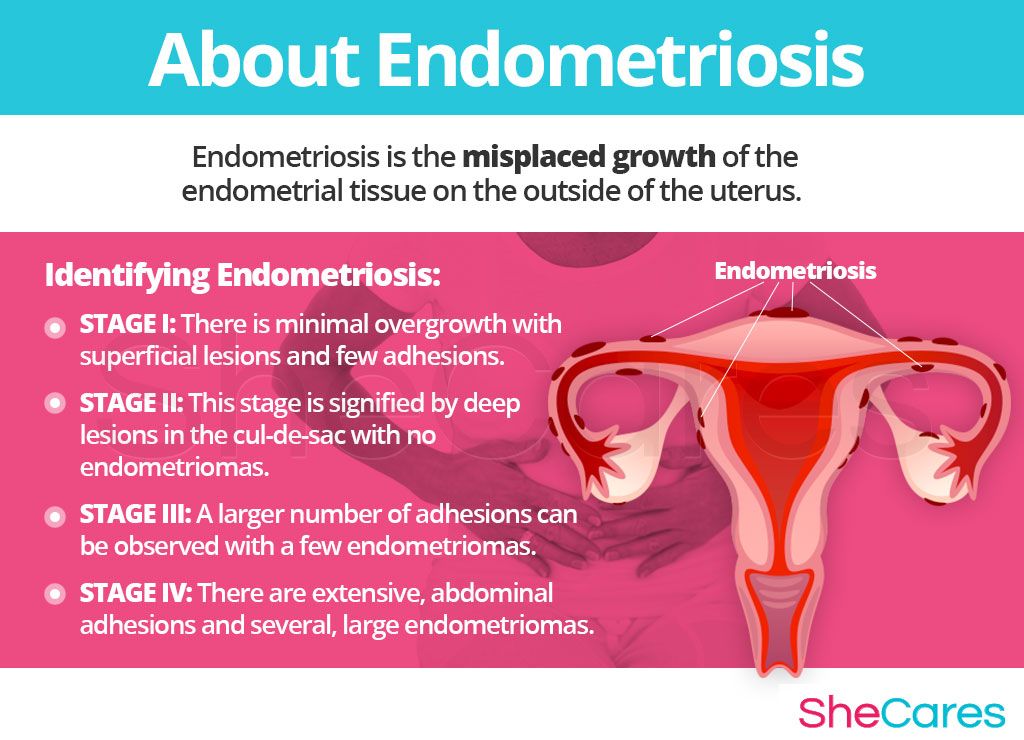
Diagnosis
The clinical challenge of uterine torsion lies in its elusive diagnosis. However, MRI has recently been used to make the diagnosis prior to exploratory surgery.
Uterine torsion is a rare obstetric complication. Nonetheless, because of its associated risks, torsion should be included in the differential diagnosis when severe but nonspecific abdominal pain occurs during pregnancy.
Treatment
In general, treatment of torsion depends on the gestational age. When torsion is discovered during exploratory surgery before the period of presumed fetal survival (i.e., before 23-24 wk), promptly returning the uterus to the normal position is the principal therapy.
When the fetus is beyond the 34th week at the time of diagnosis, the best approach is cesarean delivery at the time of the original laparotomy procedure.
Timing of diagnosis and maternal/fetal risk
Because potentially serious sequelae are possible, establishing the correct diagnosis of uterine torsion early, before complications ensue, is the challenge for clinicians.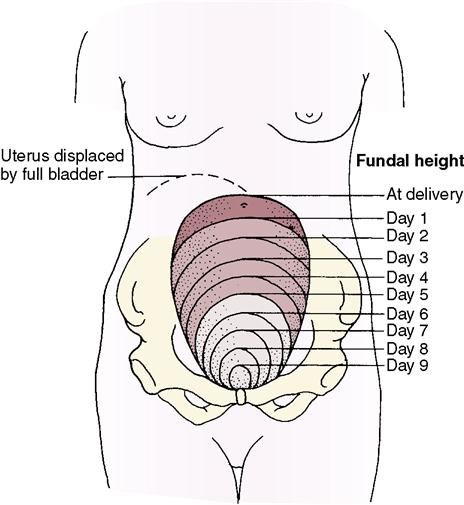
Uterine Herniation
Frequency
Herniation of the uterus through an abdominal wall defect (also known as incisional hernia or umbilical hernia of pregnancy) is, at best, an uncommon condition.
Presentation
The clinical presentation is striking. Usually during the mid-trimester, the uterus prolapses into the hernia sac via anterior anteflexion. The protrusion of the abdomen is remarkable. Necrosis or ulceration of overlying skin is also possible.
Pathophysiology
A number of potentially serious complications including spontaneous abortion, strangulation/incarceration, abruptio placentae, uterine rupture, and intrauterine death have been associated with these hernias. The constant pressure of the uterus against the hernia sac may also result in ulceration of the overlying skin.
Diagnosis
The diagnosis is confirmed by a combination of simple palpation and real time ultrasound scanning.
Treatment
Both incarceration and serious complications are possible with this disorder.
Herniorrhaphy has been performed during pregnancy but definitive repair of the abdominal wall defect is normally conducted only following delivery. The abdominal wall is often so attenuated that extensive repair with a permanent mesh is required.
Uterine Inversion
Frequency
Postpartum partial or complete uterine inversion is an uncommon but potentially life-threatening obstetric complication.
Pathophysiology
Terminology for the severity of an inversion is based on 2 clinical features: (1) the extent of prolapse in relation to the cervix and (2) how far down the birth canal the resultant mass extends.
Associations with uterine inversion include the following:
- Idiopathic factors
- Precipitate labor
- Fetal macrosomia
- Excessive cord traction or a short umbilical cord
- Intrapartum fundal pressure (Credé maneuver)
- Myometrial weakness or uterine sacculation
- Trials of vaginal birth after cesarean delivery (VBAC)
- Placenta accreta, increta, or percreta
- Fundal implantation of the placenta
- Chronic endometritis
- Acute tocolysis with nitroglycerin or other potent tocolytic drugs
- Cesarean delivery
Clinical Presentation
Early-onset postpartum hemorrhage and the sudden appearance of a vaginal mass followed by various degrees of maternal cardiovascular collapse are the classical symptoms.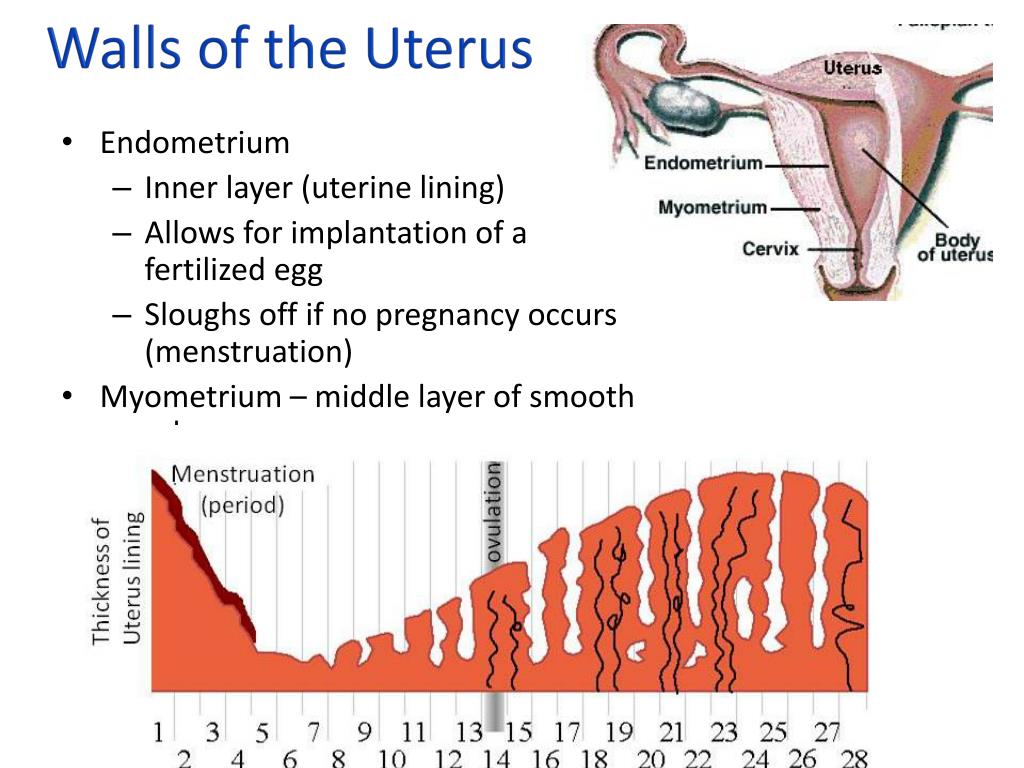 Postpartum hemorrhage is usually the most striking symptom and initially commands the clinician's attention.
Postpartum hemorrhage is usually the most striking symptom and initially commands the clinician's attention.
Due to the potential complexities of presentation, prompt ultrasonographic scanning is the most helpful technique in uncertain cases. If accompanying hemorrhage or shock is sufficiently alarming to prompt immediate surgical exploration, the correct diagnosis may be established only at laparotomy.
Chronic uterine inversion:
This diagnosis is difficult to establish on clinical grounds alone. Here again, real-time ultrasonography is especially helpful. Most of these late cases will require surgical procedures for replacement.
Diagnosis
The following entities are included in the differential diagnosis of uterine inversion:
- Occult laceration of the genital tract
- Prolapse of a uterine tumor or a large cervical polyp
- Uterine rupture
- Foreign body in the vagina
- Passage of previously unsuspected secundines or a succenturiate lobe
- Gestational trophoblastic disease
- Severe uterine atony
- Unanticipated delivery of a second twin
Treatment
Rapid diagnosis and aggressive management of uterine inversion minimizes the principal risks of acute inversion, which are hemorrhage, and cardiovascular collapse or shock. Proper treatment tests the ability of the institution to mount a prompt team-based response to this normally unanticipated, but potentially serious, obstetric complication. After uterine inversion occurs, prompt treatment of hemorrhage and shock is vital in limiting maternal morbidity and the risk of mortality.
Proper treatment tests the ability of the institution to mount a prompt team-based response to this normally unanticipated, but potentially serious, obstetric complication. After uterine inversion occurs, prompt treatment of hemorrhage and shock is vital in limiting maternal morbidity and the risk of mortality.
Manage shock
Summon nursing assistance and another surgeon.
Begin fluid resuscitation with 2 large-bore intravenous lines. Promptly administer 1 L or more of an isotonic salt solution (Ringer's lactate).
Submit specimens to the laboratory to prepare for possible transfusion of blood or blood products. Also send samples to determine baseline values of the following:
- Hematocrit
- Hemoglobin concentration
- Coagulation factors (e.g., prothrombin time, activated partial thromboplastin and time, level of fibrinogen)
Insert a Foley catheter.
Immediately summon an anesthesiologist.
Treat aggressively
Administer oxygen.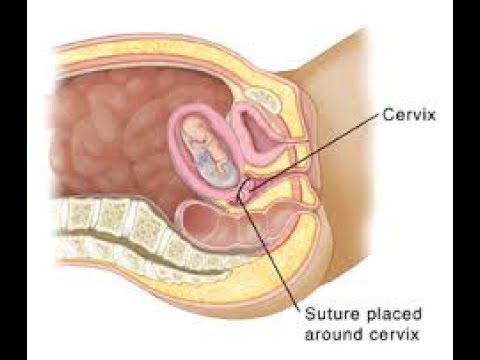
Order the appropriate surgical equipment, and instruct assistants to prepare the operating room for possible laparotomy.
Once in the operating room, administer tocolytics to promote uterine relaxation. These drugs may include one of following:
- Terbutaline 0.100-0.250 mg given slowly intravenously
- Nitroglycerin 0.250-0.500 mg given intravenously over 1-2 minutes (preferred)
- Magnesium sulfate 4-6 g administered intravenously over 20 minutes (less effective and not recommended as initial treatment)
Attempt prompt replacement of the uterus:
- Begin with a trial of manual replacement per vagina. Conducted with adequate uterine relaxation, this maneuver is highly likely to be successful.
- If manual replacement fails, promptly perform laparotomy to achieve surgical replacement unless the clinician is trained in one of the vaginal surgical approaches. During laparotomy, general anesthesia with a uterine-relaxing agent is best, especially if a parenteral tocolytic was not previously given or if it appears to have failed.
Repair
Manually replace uterus.
Suture lacerations of the birth canal and any surgical incisions in the cervix or vagina,
Perform uterine massage after replacement of the uterus.
Administer uterotonics.
Closely monitor the patient for several hours after the uterus is replaced to detect spontaneous reinversion.
Surgical techniques
If 2 or more attempts at manual replacement are unsuccessful despite adequate tocolysis and analgesia, a surgical procedure is indicated. An abdominal approach for uterine replacement is favored.
Inversion in non pregnant women
Inversion is rarely observed in non pregnant women. The characteristic finding in these most unusual patients is a pedunculated subserosal leiomyoma or other neoplasm at or adjacent to the uterine fundus. The usual culprits are endometrial polyps and pedunculated leiomyomata.
Consultations
In the rare case when pregnancy-related inversion is long standing or when manual replacement is unsuccessful and surgical replacement is required, consultation with an experienced clinician is advised.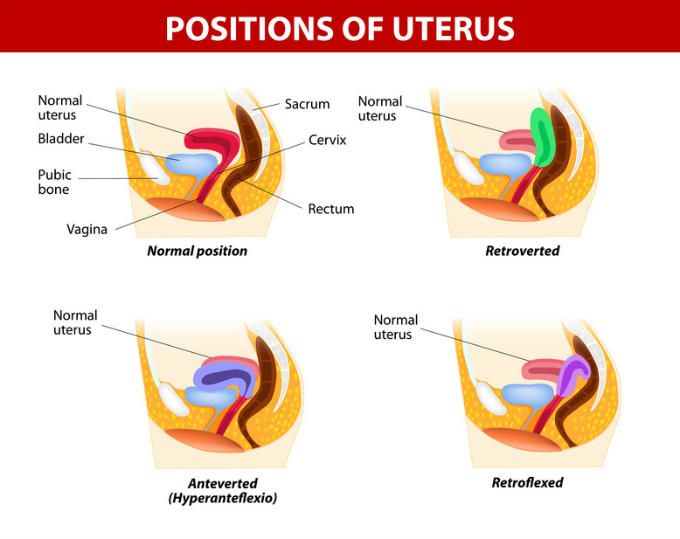 During surgery, the presence of 2 operators speeds above-and-below procedures and reduces the risk of iatrogenic injury to the uterus or adjacent structures
During surgery, the presence of 2 operators speeds above-and-below procedures and reduces the risk of iatrogenic injury to the uterus or adjacent structures
Uterine Prolapse
Frequency
Uterine prolapse during gestation is an infrequent clinical problem, though moderate degrees of descensus are common before pregnancy, especially in multiparas. If not severe, pregnancy-associated prolapse often partially or completely resolves in the mid trimester as the fundus grows and the uterus becomes an abdominal organ, drawing the cervix upward. In such cases, symptomatic prolapse usually recurs in the third trimester, or, on occasion, it is first observed at this time.
Pathophysiology
The female pelvic viscera are best considered to be suspended from above and supported from below. To maintain the pelvic organs in their proper position, their suspensory and support structures must remain intact and interact. This joint function depends on the integrity of the muscular, fascial, and neurologic components of these various tissues.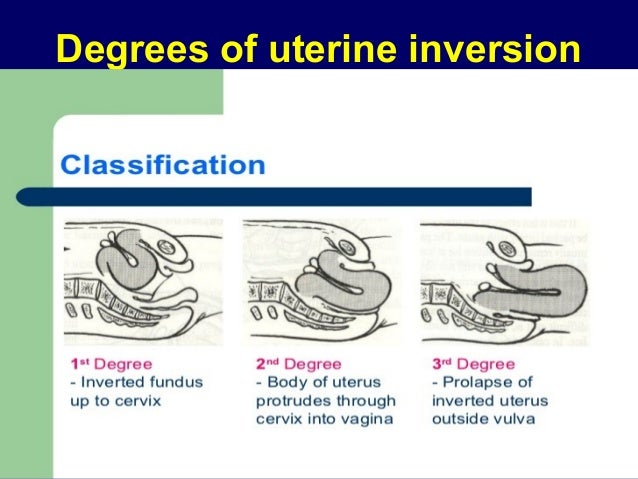 Substantial injury to one or more of these systems can result in a loss of support and result in a degree of prolapse that may prove permanent.
Substantial injury to one or more of these systems can result in a loss of support and result in a degree of prolapse that may prove permanent.
Clinical Presentation
Signs and symptoms associated with uterine prolapse may include the following:
- Preterm labor
- Pelvic pressure or discomfort
- Preterm membrane rupture
- Lower back pain
- Cervicitis, vaginitis, vaginal discharge
- Urinary tract infection
- Vaginal or perineal mass
- Paradoxical urinary tract symptoms (e.g., acute retention, incontinence)
- Bleeding due to mucosal ulcerations or cervicitis
- Constipation
Diagnosis
Establishing the diagnosis is not a challenge. On examination, the clinician observes unusual cervical descent, accompanied by variable protrusion of the anterior and posterior vaginal walls.
Uterine distortion due to tumors such as large leiomyomas or other masses, prolapse of a cervical or endocervical tumor, or a müllerian anomaly must be considered in the differential diagnosis.
Results from physical examination and ultrasonographic study should promptly establish the correct diagnosis.
Treatment
Aspects of treatment are as follows:
- Restrict activity.
- Aggressively treat cervicitis or soft tissue erosions of the birth canal.
- Conduct a trial of a pessary.
- Treat associated urinary tract infections.
- Determine the fetal fibronectin value.
- Administer corticosteroids to enhance fetal pulmonic maturity.
- Serially assess fetal growth, and sonographically verify normality of fetal anatomy.
- If appropriate, conduct ultrasound.
Serious complications
A number of serious complications are there in association with prolapse during pregnancy.
Among non pregnant women, hysterectomy with vault suspension is usually required to definitively repair advanced degrees of prolapse. The necessary procedure depends on the severity of the problem and on the individual's pelvic anatomy.
Treatment of abnormal position of the uterus in Moscow
Note: in a healthy, non-pregnant and non-nursing woman, the uterus is located in the middle of the small pelvis, its bottom is directed up and forward and does not protrude beyond the plane of the entrance to the small pelvis, and the vaginal part of the cervix is down and back, and it is located on ischium level. In this case, the axis of the uterus is tilted to the front, a natural bend is formed between the body and the neck, the angle of which is obtuse and open forward.
The position of the uterus changes with age. The norm is considered to be slightly higher than the uterus in girls and the omission and deviation of the organ back in older women.
Types of malposition of the uterus
The uterus can move vertically, in a horizontal plane or around the longitudinal axis.
To the displacement of the uterus "up and down" include:
- lift;
- omission;
- dropout;
- eversion.
Violation of the position of the uterus in the horizontal plane can also be of several types:
- displacement of the entire organ;
- wrong inclination;
- pathological bending of the body.
Around the longitudinal axis, the uterus can turn to the right or left along with the cervix (rotation of the uterus), or only the lower part of the body unfolds with a fixed cervix (torsion of the uterus).
Treatment of abnormal position of the uterus in the SMC "Best Clinic"
The incorrect position of the uterus, if it does not cause functional disorders and subjective complaints, does not require special treatment. Only in cases where pain, frequent and painful urination, urinary incontinence, menstrual irregularities, sexual and reproductive dysfunction are observed, conservative or surgical treatment is performed.
Conservative treatment consists of "manual" correction of the position of the uterus, followed by the installation of a pessary. Also, to strengthen the ligaments of the uterus, gynecological massage can be applied and physiotherapy exercises are prescribed. If an inflammatory or infectious cause of a change in the position of the uterus is identified, the underlying disease is treated.
Also, to strengthen the ligaments of the uterus, gynecological massage can be applied and physiotherapy exercises are prescribed. If an inflammatory or infectious cause of a change in the position of the uterus is identified, the underlying disease is treated.
Important! A properly selected and well-placed pessary effectively keeps the uterus in a normal position and does not cause any discomfort to the woman.
Surgical treatment is an operation to restore the normal position of the uterus by correcting its ligamentous apparatus and fixing the organ to the anterior abdominal wall. In SMC "Best Clinic" such operations are performed laparoscopically - the most sparing, reliable and safe method of treatment. After the operation, the use of a pessary is no longer required.
To make an appointment with the gynecologists of the Best Clinic SMC, call the numbers listed on our website or fill out a short appointment form. If it is not possible to arrive on time, please notify us in advance so that we can arrange another time for you.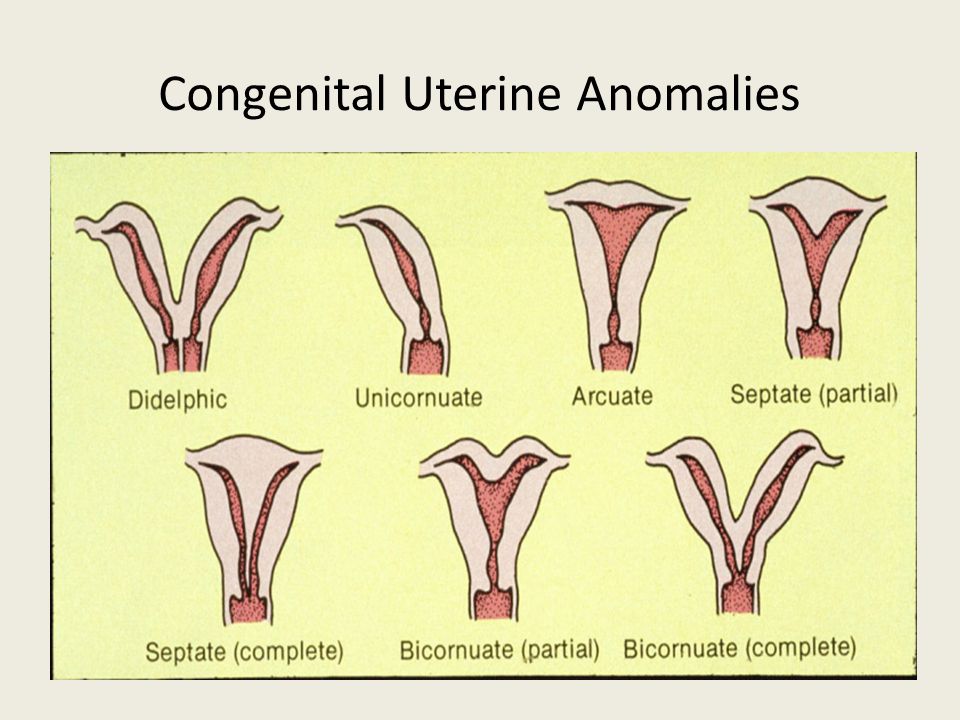
Retrodeviation of the uterus. What is Uterine Retrodeviation?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Retrodeviation of the uterus is a violation of the position in which the body of the organ posteriorly deviates, and the cervix anteriorly, with time an angle open back (retroflection) is formed. In most cases, the condition is asymptomatic, depending on the cause, pelvic pain, pathological leucorrhea, and dysmenorrhea may be disturbing. The diagnosis is established during a two-manual examination, ultrasound, MRI may be required for confirmation. Treatment is carried out in the presence of symptoms of the disease. Conservative methods, exercise therapy, a gynecological pessary are used.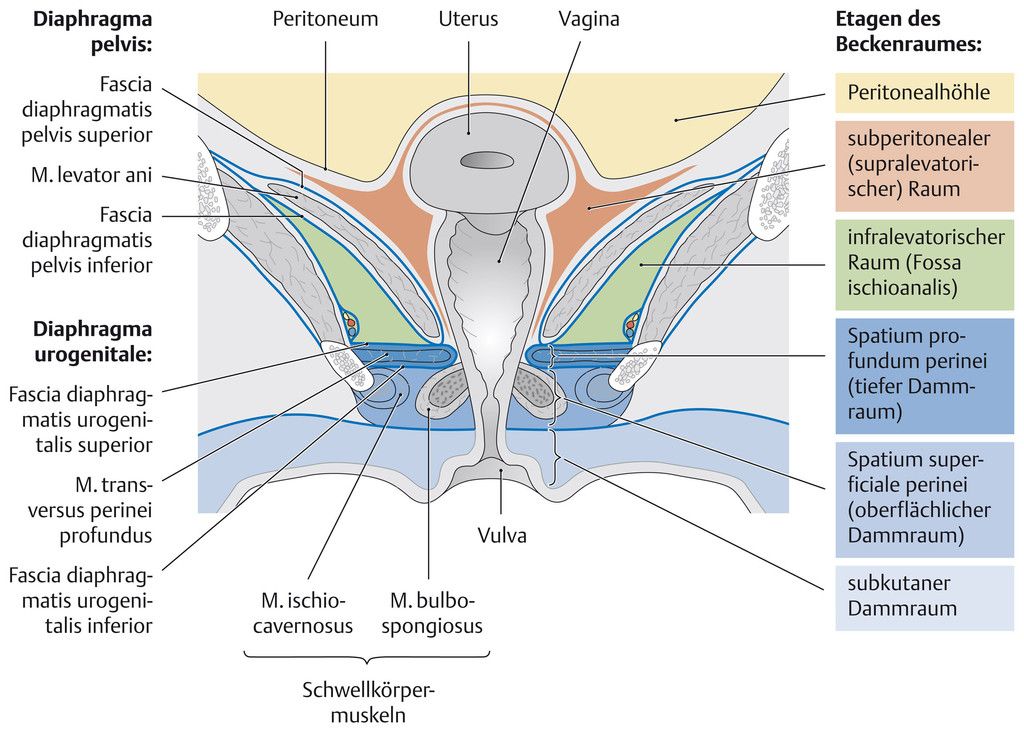 In case of inefficiency, surgical correction is resorted to.
In case of inefficiency, surgical correction is resorted to.
ICD-10
N85.4 Malposition of uterus
- Causes
- Pathogenesis
- Classification
- Symptoms of uterine retrodeviation
- Complications
- Diagnostics
- Treatment of uterine retrodeviation
- Prognosis and prevention
- Prices for treatment
General
Retrodeviation of the uterus (retroflection-retroversion) is a rare pathology found in adolescents and women of reproductive age. The exact prevalence is unknown, the incidence increases in groups of patients with asthenic physique, hyperplastic processes in the pelvic cavity, and traumatic childbirth. In girls with congenital disorders of connective tissue development, posterior deviation of the uterus is determined in 10% of cases. Pathology is often combined with hypoplasia, infantilism and other developmental anomalies.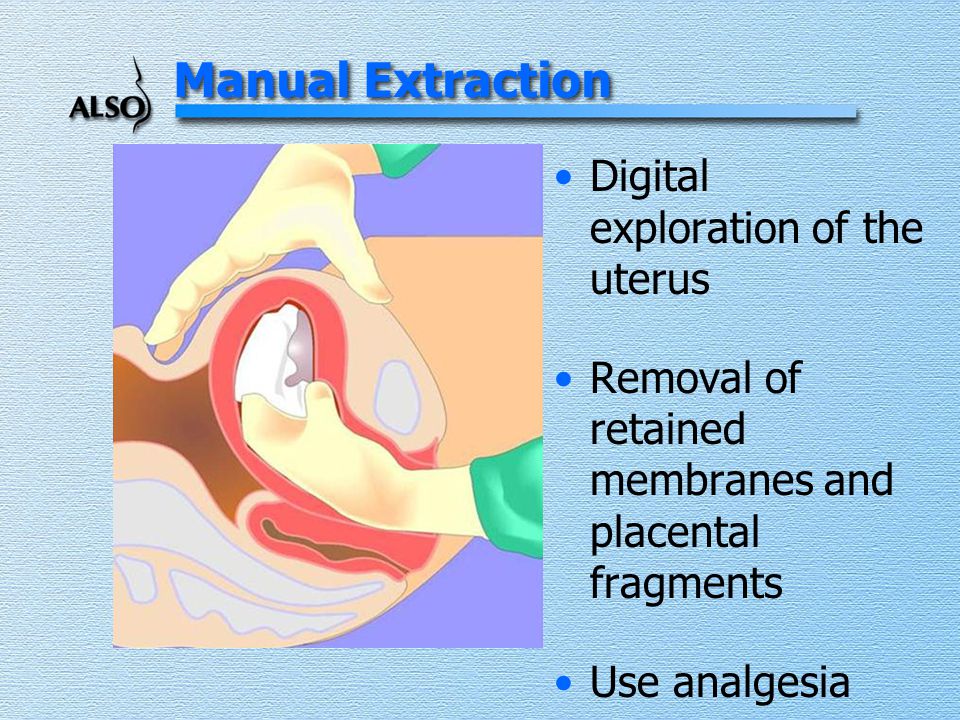
Retrodeviation of the uterus
Causes
For the development of retrodeviation of the uterus, it is necessary to weaken the ligamentous apparatus of the small pelvis and maintain the elasticity of its muscles. Sometimes the formation of pathology is influenced by increased intra-abdominal pressure. Pregnancy does not act as a provoking factor. The causes of the condition are congenital and acquired:
- Connective tissue dysplasia. In girls with a violation of the formation of the ligamentous apparatus, the genitals do not have normal fixation, therefore, as the uterus grows, it deviates backwards. At the same time, the pelvic muscles do not allow prolapse to develop. Retrodeviation of the uterus occurs in Shereshevsky-Turner syndrome, combined with other anomalies of the genital organs.
- Asthenic physique. Adipose tissue located in the cavity of the abdomen and small pelvis is involved in maintaining the position of the internal organs.
 With low weight, sudden weight loss, a state of exhaustion, an asthenic type of constitution, the uterus loses additional support and can change position. A set of body weight does not lead to correction of the position of the genital organs.
With low weight, sudden weight loss, a state of exhaustion, an asthenic type of constitution, the uterus loses additional support and can change position. A set of body weight does not lead to correction of the position of the genital organs. - Diseases of the reproductive organs. Retrodeviation is provoked by inflammatory processes in the small pelvis, which are accompanied by the formation of adhesions that fix the uterus in the wrong position. The cause can also be tumor processes of a benign and malignant nature. A temporary violation of the situation occurs with an ectopic pregnancy.
- Birth injuries. With rapid childbirth, a large fetus, high parity, there is a risk of overstretching of the ligamentous apparatus, its weakening. The chances of the formation of retrodeviation of the uterus increase with endometritis, parametritis in the postpartum period. Heavy physical labor, the constant carrying of a large child in her arms increase the likelihood of developing disorders of the position of the uterus.

Pathogenesis
For the formation of retrodeviation, it is necessary that the woman has a weakening of the ligaments while maintaining the tone of the uterus and the elasticity of the muscles of the pelvic floor. In girls, the formation of an anomaly in the position is possible only after the exit of the uterine body into a wide part of the pelvic cavity, when the size of the uterus begins to exceed the size of the cervix. This condition is observed at the age of at least 10 years.
Retrodeviation of the uterus is facilitated by other congenital anomalies. The short posterior wall of the vagina, the conical and long uterine neck, the insufficient angle of the small pelvis contribute to a change in the position of the organs. With an increase in intra-abdominal pressure, intestinal loops press on the uterus. If the uterus remains toned, but the ligaments are weakened, it deviates back. The factor contributing to the bend is the levator muscle, which pushes the uterine body backwards.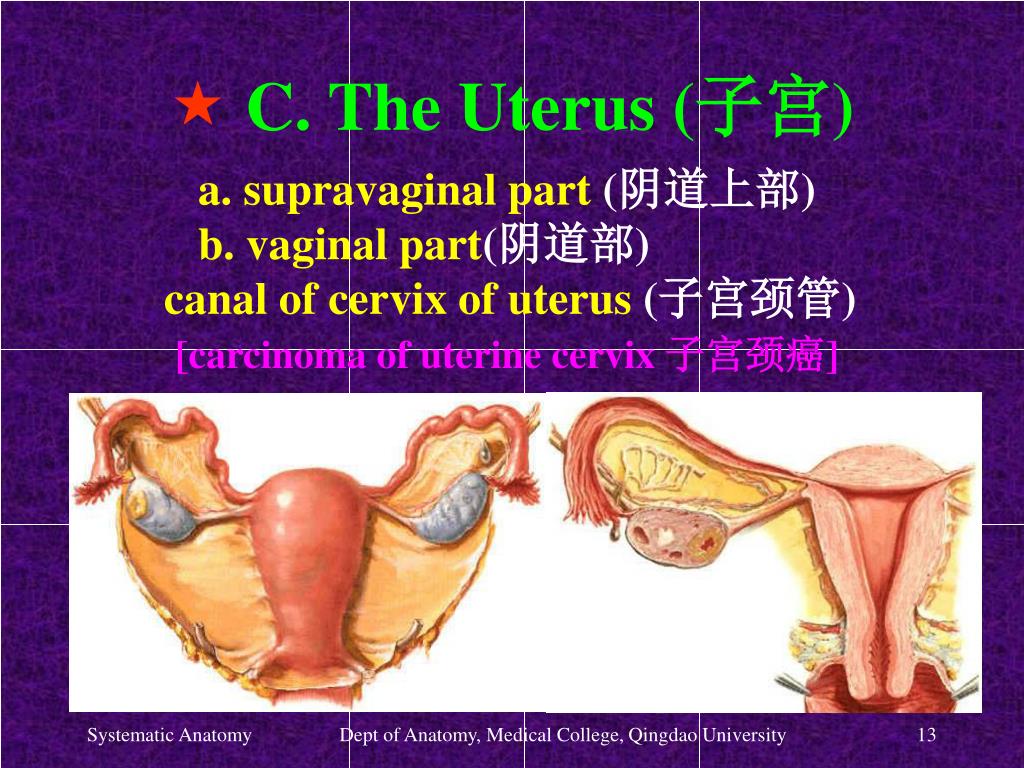
After starting the process of deviation, the intestinal loops get freer access to the small pelvis. The growth or maintenance of high intra-abdominal pressure completes the formation of the first degree of retrodeviation. If the provoking factor is not eliminated, the condition gradually progresses towards an increase in the angle of inclination.
Classification
Retrodeviation of the uterus is congenital and acquired. Separately, a fixed type of pathology is distinguished, in which the organ is tightly soldered to neighboring tissues. The stage classification reflects the position of the uterus relative to the cervix in the pelvis, but the severity of clinical symptoms does not have a direct relationship with the magnitude of the angle of inclination. There are the following degrees of condition:
- Retroclination (grade 1). The uterus is tilted back, anteflexia is preserved.
- Retroversion (grade 2). The uterus deviated backwards is revealed, a pronounced angle between the body and the neck is not formed.
- Retroflection (3rd degree). The body of the uterus is tilted back, and the cervix is forward, a pronounced angle is formed between them.
Symptoms of uterine retrodeviation
Pathology is not always accompanied by severe symptoms, sometimes it becomes an accidental finding during a gynecological examination. Some women complain of frequent pain in the pelvic area, radiating to the sacrum. Pain intensifies after a long vertical position of the body, motionless standing. Disturbed by painful menstruation. With a pronounced deviation of the uterus, the outflow of blood may be difficult, which is accompanied by the appearance of large clots during menstruation.
Preservation of the remnants of secretions in the uterine cavity leads to their disintegration, the appearance of an unpleasant odor. A secondary infection may join, acute endometritis occurs with a tendency to become chronic. This condition is characterized by symptoms of inflammation, increased pain in the abdomen, and the release of purulent leucorrhoea.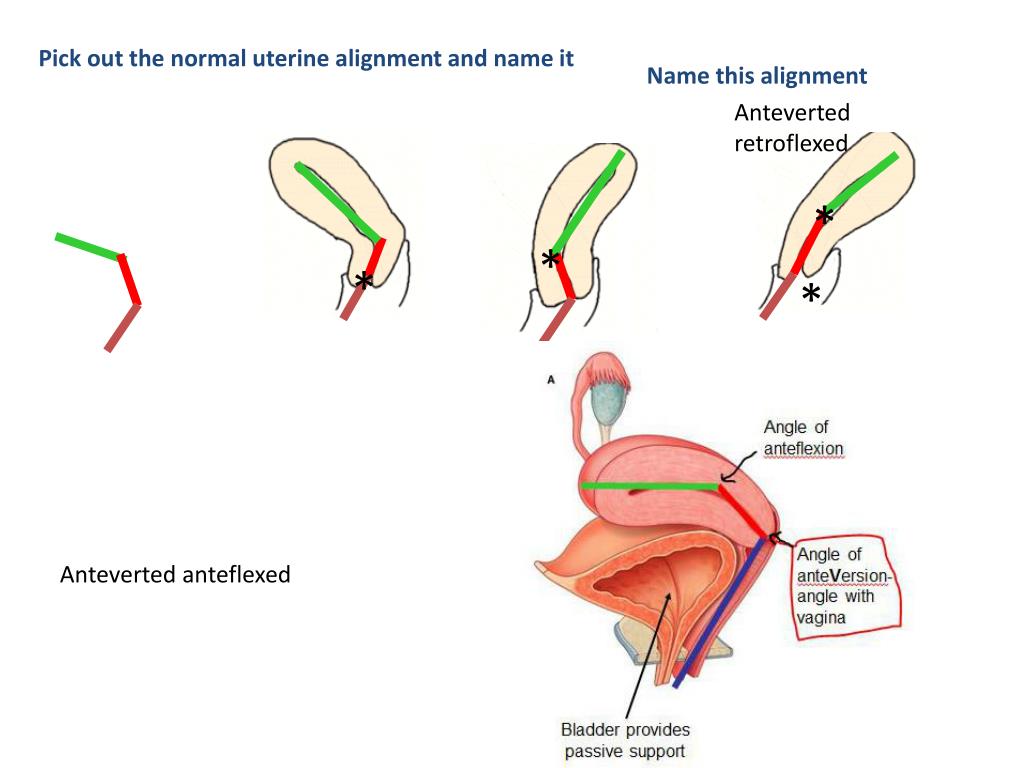 Sometimes metrorrhagia occurs.
Sometimes metrorrhagia occurs.
There are no difficulties with conception; with pronounced forms of retrodeviation of the uterus, miscarriages may develop in the early stages. More often they are associated with concomitant diseases, chronic inflammation. In other cases, the uterus gradually increases in size and after 16 weeks takes a normal position that does not affect the course of pregnancy and the process of childbirth.
Complications
Anomalies in the position of the genital organs rarely lead to complications. In violation of the formation of connective tissue retrodeviation of the uterus may be accompanied by prolapse of the genital organs. In this case, due to the displacement of the position of the bladder, urethra, dysuric disorders appear, urges become more frequent, incontinence worries. When squeezing the rectum, constipation may occur.
A pronounced deviation of the uterus back becomes the cause of its infringement, a critical violation of blood flow.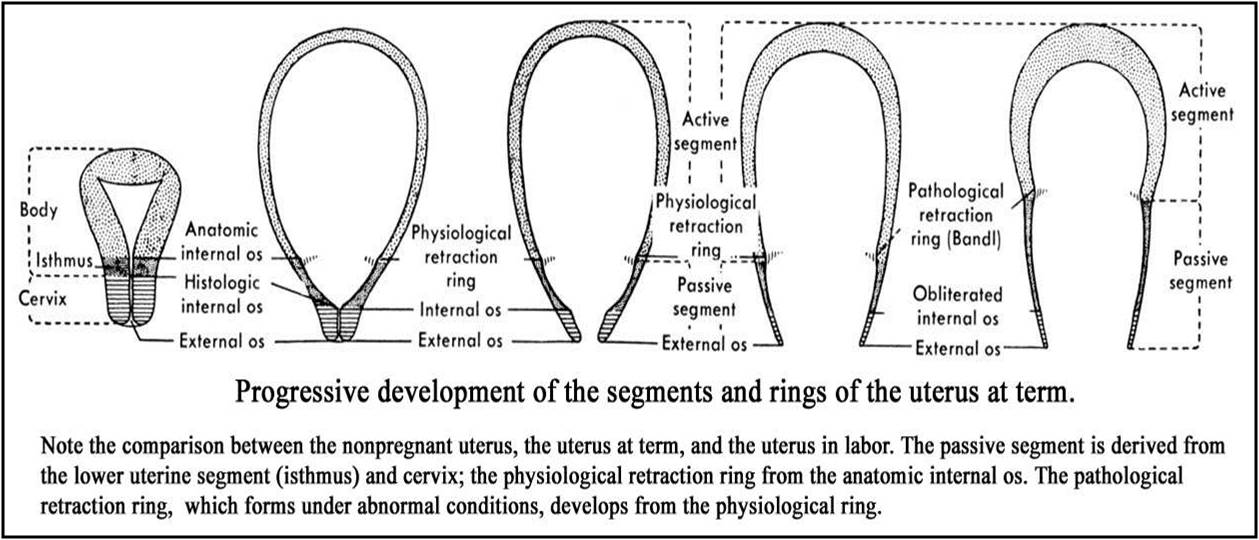 This is facilitated by the great depth of the Douglas space, narrow pelvis, and perimetric adhesions. Lack of blood flow, venous congestion lead to the development of edema, tissue hypoxia, and acute pain syndrome. In a neglected case, necrosis is possible with untimely access to a doctor.
This is facilitated by the great depth of the Douglas space, narrow pelvis, and perimetric adhesions. Lack of blood flow, venous congestion lead to the development of edema, tissue hypoxia, and acute pain syndrome. In a neglected case, necrosis is possible with untimely access to a doctor.
Diagnostics
To examine and search for the causes of retrodeviation of the uterus, a woman should contact an obstetrician-gynecologist. If you suspect a malignant tumor, you may need to consult an oncologist. Diagnosis is usually non-invasive, with severe pathology resorting to invasive examination methods. The following methods are used:
- Gynecological examination. During a bimanual examination, the doctor can determine the deviation of the uterine body backwards, the abnormal location of the cervix. There is a dense consistency of the organ, its mobility or cohesion with the surrounding tissues, pain on palpation.
- Ultrasound of the genital organs.
 Ultrasound can be used to study the structure of tissues. Sometimes myomatous nodes, volumetric formations of presumably malignant origin, adhesions in the pelvic region, and inflammatory tissue changes are detected.
Ultrasound can be used to study the structure of tissues. Sometimes myomatous nodes, volumetric formations of presumably malignant origin, adhesions in the pelvic region, and inflammatory tissue changes are detected. - MRI of the pelvis. It is necessary with a pronounced degree or fixed retrodeviation of the uterus. Allows you to set the number and location of myomatous nodes, confirm the fixation of the uterine body due to a pronounced adhesive process, and detect other neoplasms.
- Diagnostic laparoscopy. For examination, hospitalization in the gynecology department is necessary. The method is used in severe cases to clarify the severity of the adhesive process, it can be used simultaneously for treatment and differential diagnosis with ectopic pregnancy.
Treatment of uterine retrodeviation
In the absence of symptoms, treatment is not indicated; in other cases, conservative therapy is performed. Symptomatic remedies are used, the causes that caused the position anomalies are eliminated. Hospitalization is not required for most patients, the course of therapy is controlled by the doctor of the antenatal clinic. The following approaches are applied:
Hospitalization is not required for most patients, the course of therapy is controlled by the doctor of the antenatal clinic. The following approaches are applied:
- exercise therapy. A consultation with a physiotherapy doctor is prescribed, which selects exercises aimed at strengthening the ligamentous apparatus and changing the position of the body of the uterus. In the advanced stage, exercise therapy is ineffective.
- Gynecological pessary. Silicone products are installed, which are selected individually, temporarily (during the period of wearing) change the position of the organ. They can contribute to an even greater weakening of the ligamentous apparatus, the addition of pelvic organ prolapse, the development of inflammation and bedsores.
- Anti-inflammatory therapy. It is recommended if retrodeviation is combined with endometritis. Broad-spectrum antibiotics, non-steroidal anti-inflammatory drugs, enzymes to dissolve adhesions are used. With a pronounced and chronic adhesive process, drug lysis does not bring the desired result.
- Physiotherapy. It can be used for a fixed form of retrodeviation of the uterus. Effective mud therapy, iontophoresis, diathermic treatment. After physiotherapy, gynecological massage can be performed.
- Uterine reposition. Rarely used due to low efficiency. Restoring the position does not eliminate the cause of the anomaly, so the uterus may soon return to its previous position. The procedure is performed with an empty bladder and rectum. The technique is used according to Schulze, Ott or using bullet forceps according to Kustner.
- Surgical treatment. It is necessary with a large number of adhesions, volumetric formations in the pelvic organs. Connective tissue bridges are dissected, neoplasms are removed. To fix the uterus and eliminate retrodeviation, the Pestalozzi or Kakushkin operation is performed.
Prognosis and prevention
With timely access to a gynecologist and compliance with the recommendations, the prognosis is favorable, retrodeviation of the uterus rarely causes pregnancy complications and does not impair reproductive function.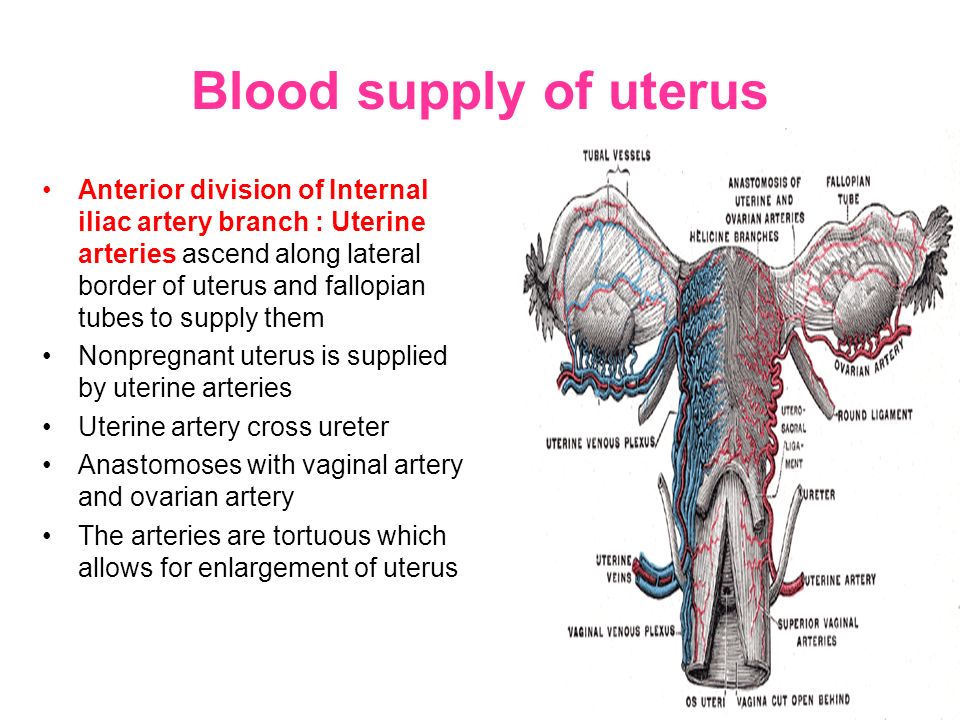 With severe degrees of deviation, full treatment is required. The anomaly may resolve on its own after pregnancy and successful uncomplicated delivery.
With severe degrees of deviation, full treatment is required. The anomaly may resolve on its own after pregnancy and successful uncomplicated delivery.
For prevention, it is necessary to have good nutrition in adolescence, the rejection of strict diets. To prevent inflammation in the uterus, you need to avoid casual sex, use barrier contraceptives. After operations on the organs of the abdomen or small pelvis, cesarean section, preventive anti-adhesion treatment is prescribed. Rational and careful management of childbirth is required.
You can share your medical history, what helped you in the treatment of retrodeviation of the uterus.
Sources
- Gynecology / Radzinsky V.E. – 2005.
- Reproductive health of adolescent girls with phenotypic manifestations of connective tissue dysplasia / Skosyreva G.A., Kim L.B., Peterson V.D., Gauser V.V., Ryabichenko T.I., Smirnova E. G. - 2005.
- Gynecology. Guidelines for doctors and students / Petchenko A.