Low risk nipt
Non-invasive prenatal testing (NIPT) | Pregnancy Birth and Baby
Non-invasive prenatal testing (NIPT) | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Key facts
- The non-invasive prenatal test (NIPT) screens your baby for genetic health conditions.
- You may want to consider genetic counselling before having an NIPT to help you make an informed decision.
- If your NIPT result shows that your baby is likely to have a chromosomal difference, a diagnostic test such as chorionic villus sampling or amniocentesis can confirm your result.
What is the non-invasive prenatal test (NIPT)?
The non-invasive prenatal test (NIPT) is a very accurate screening test. Screening tests are used to see if your baby has a high chance of a genetic health condition. These conditions include Down syndrome and other chromosomal differences. The NIPT involves a simple blood test that is done in your first trimester of pregnancy.
There are different kinds of prenatal testing available to check the health of your baby. It’s your choice if you would like to have these tests. Talk about your options with your doctor or genetic counsellor and give yourself some time to make your decision.
Screening tests are different to diagnostic tests. Diagnostic tests are often more invasive. However they confirm for certain if the result is positive.
During pregnancy, some of the baby’s DNA passes into your bloodstream. The non-invasive prenatal test analyses the genetic information contained in this DNA. It’s used to screen for a number of genetic conditions. The test is particularly sensitive to Down syndrome. It was first offered in Australia in 2012.
In Australia, NIPTs are offered in private centres and involve an out-of-pocket cost. They are sometimes referred to by different names, depending on the company that makes them.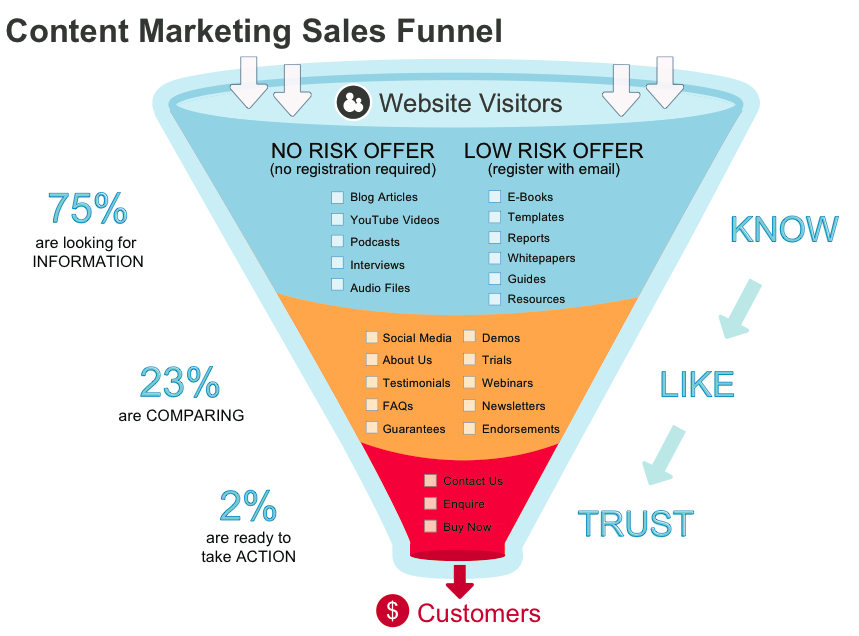 They might be called: Harmony, Generation or Percept.
They might be called: Harmony, Generation or Percept.
An NIPT is done from 10 weeks into the pregnancy. Before the test you will be asked to give consent.
What does it test for?
The NIPT is a safe and very effective way of screening for certain conditions. These include:
- Down syndrome (also called trisomy 21)
- Edwards syndrome (trisomy 18)
- Patau syndrome (trisomy 13)
- Turner syndrome
Some laboratories also test the sex of your baby and look for differences with the sex chromosomes.
The test identifies many chromosomal anomalies. It doesn’t screen for genetic disorders such as:
- cystic fibrosis
- thalassaemia
- sickle cell anaemia
Screening will tell you how likely it is that your baby has a chromosomal difference. The only way of knowing for sure is to have a diagnostic test such as:
- chorionic villus sampling (CVS)
- amniocentesis
Should I have an NIPT?
The NIPT is very sensitive.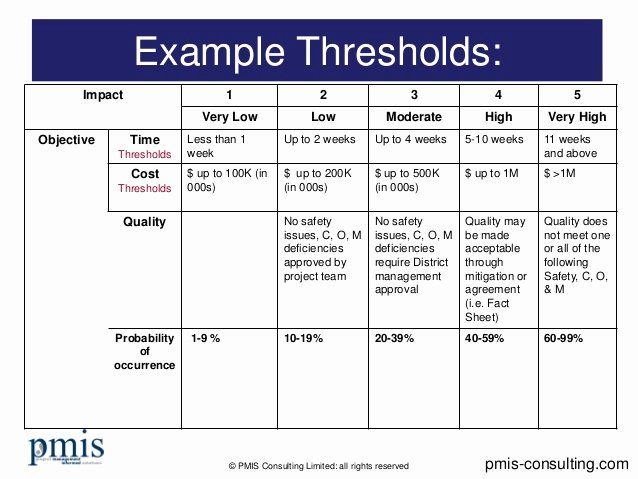 It picks up more than 99% of cases of Down syndrome. But it is a screening test rather than a diagnostic test.
It picks up more than 99% of cases of Down syndrome. But it is a screening test rather than a diagnostic test.
It can tell you whether there is an increased chance of having a baby with a genetic condition. It doesn’t give you a definitive answer. For some parents, information from screening tests can help them decide about whether to have diagnostic testing.
You might choose to have an NIPT test if:
- Your first trimester combined screening test shows you have an increased chance of having a baby with Down syndrome (this test combines results from a blood test at 10 to 12 weeks and an ultrasound at 11 to 13 weeks).
- You did not have the first trimester combined screening test because it was too late or the test wasn't available in your area.
- You want to understand your chance of having a baby with Down syndrome before considering diagnostic tests such as amniocentesis or CVS.
- You have an increased chance of having a baby with Down syndrome because you are older or you or your partner already have a baby with Down syndrome or another genetic condition.
It’s a good idea to consider genetic counselling before you have an NIPT to help you make an informed decision. It’s important to understand the risks and benefits of having the test.
Genetic counsellors can:
- review your family and medical history
- give you information about genetic tests
- help you learn about how the condition is inherited
- offer advice on support services
If your pregnancy is affected by a genetic condition, your genetic counsellor can:
- help support you
- help you understand what the results mean for you and your family
What can I expect from my NIPT results?
It can take up to 2 weeks to get the result of your NIPT.
If your NIPT result shows that your baby is likely to have a chromosomal difference, a diagnostic test such as: CVS or amniocentesis can confirm the result.
You should discuss your options with your doctor, midwife or genetic counsellor.
How much does the NIPT cost?
The NIPT is not covered by Medicare or private health insurance in Australia. You can expect to pay about $400 to $500 for an NIPT.
You may also need to pay for: an appointment with your doctor to get a referral, as well as an ultrasound.
You should speak with your doctor or a genetic counsellor before getting an NIPT. You can find genetic counselling services near you using the healthdirect Service Finder here.
You can read more about genetic counselling here.
If you have any questions about the NIPT, you can call the Pregnancy Birth and Baby helpline.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
The Royal Women's Hospital Victoria (Genetic testing in pregnancy), NSW Health (Genetic and genomic testing for intellectual disability and childhood syndromes), O&G Magazine (Developments in non-invasive prenatal testing: is bigger better?), Allied Health Professions Australia (Genetic Counselling)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Questions to ask your doctor about tests and scans
- Antenatal care during your pregnancy
- Your first antenatal visit
- Blood tests during pregnancy
- Prenatal screening and testing
Need more information?
NIPT - non-invasive prenatal testing - Pathology Tests Explained
Learn about why, when and how NIPT testing is done
Read more on Pathology Tests Explained website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
What is prenatal screening?
Prenatal screening won't tell you if your baby has a health condition, but it can assess your risk. Learn more here about deciding whether to have a prenatal screening test.
Learn more here about deciding whether to have a prenatal screening test.
Read more on Pregnancy, Birth & Baby website
A guide to blood tests in pregnancy | Know Pathology Know Healthcare
The following guide outlines the different pathology tests available throughout each trimester, and the purpose of your prenatal blood tests.
Read more on Know Pathology Know Healthcare website
Screening for carrier status
Screening for carrier status assesses whether you and your partner carry genes that could mean your baby is born with a health condition. Find out more here about whether the test might be right for you.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 10
Think about the prenatal screening tests you might have, and whether you want a dating scan to confirm your due date.
Read more on Pregnancy, Birth & Baby website
Prenatal Screening for Chromosomal and Genetic Conditions
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Nuchal translucency scan
A nuchal translucency scan is an ultrasound scan that helps in estimating your risk of having a baby with chromosomal abnormality.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 12
By week 12, your baby is the size of a plum but fully formed, with their organs, muscles, limbs and bones in place.
Read more on Pregnancy, Birth & Baby website
Screening for Down syndrome
Down syndrome is a chromosomal disorder that affects 1 in 1,00 babies. Find out about the screening and diagnostic tests that can detect the condition.
Find out about the screening and diagnostic tests that can detect the condition.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Increased nuchal translucency after low-risk noninvasive prenatal testing: What should we tell prospective parents?
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Wiley
Full text links
Review
. 2021 Sep;41(10):1305-1315.
2021 Sep;41(10):1305-1315.
doi: 10.1002/pd.6024. Epub 2021 Aug 6.
Joanne Kelley 1 , George McGillivray 1 2 , Simon Meagher 1 3 4 , Lisa Hui 1 4
Affiliations
Affiliations
- 1 Department of Perinatal Medicine, Mercy Hospital for Women, Heidelberg, Victoria, Australia.
- 2 Victorian Clinical Genetics Services, Murdoch Children's Research Institute, Royal Children's Hospital, Parkville, Victoria, Australia.
- 3 Monash Ultrasound for Women, Monash IVF Group, Melbourne, Victoria, Australia.
- 4 Department of Obstetrics and Gynaecology, University of Melbourne, Parkville, Victoria, Australia.
- PMID: 34297420
- DOI: 10.1002/pd.6024
Review
Joanne Kelley et al. Prenat Diagn. 2021 Sep.
. 2021 Sep;41(10):1305-1315.
doi: 10.1002/pd.6024. Epub 2021 Aug 6.
Authors
Joanne Kelley 1 , George McGillivray 1 2 , Simon Meagher 1 3 4 , Lisa Hui 1 4
Affiliations
- 1 Department of Perinatal Medicine, Mercy Hospital for Women, Heidelberg, Victoria, Australia.

- 2 Victorian Clinical Genetics Services, Murdoch Children's Research Institute, Royal Children's Hospital, Parkville, Victoria, Australia.
- 3 Monash Ultrasound for Women, Monash IVF Group, Melbourne, Victoria, Australia.
- 4 Department of Obstetrics and Gynaecology, University of Melbourne, Parkville, Victoria, Australia.
- PMID: 34297420
- DOI: 10.1002/pd.6024
Abstract
Three decades ago, the observation that first trimester fetuses with excess fluid accumulation at the back of the neck were more likely to be aneuploid, gave rise to a new era of prenatal screening. The nuchal translucency (NT) measurement in combination with serum biomarkers and maternal age, resulted in the first trimester combined screening (FTCS) program. The introduction of noninvasive prenatal testing (NIPT) over the past decade has introduced the option for parents to receive highly sensitive and specific screening information for common trisomy from as early as 10 weeks gestation, altering the traditional pathway FTCS pathway. The retention of the 11-13-week NT ultrasound remains important in the detection of structural anomalies; however, the optimal management of pregnancies with a low-risk NIPT result and an isolated increased NT measurement in an era of advanced genomic testing options is a new dilemma for clinicians. For parents, the prolonged period between the initial diagnosis in first trimester, and prognostic information at each successive stage of investigations up to 22-24 weeks, can be emotionally challenging. This article addresses the common questions from parents and clinicians as they navigate the uncertainty of having a fetus diagnosed with an increased NT after a low-risk NIPT result and presents suggested approaches to management.
The nuchal translucency (NT) measurement in combination with serum biomarkers and maternal age, resulted in the first trimester combined screening (FTCS) program. The introduction of noninvasive prenatal testing (NIPT) over the past decade has introduced the option for parents to receive highly sensitive and specific screening information for common trisomy from as early as 10 weeks gestation, altering the traditional pathway FTCS pathway. The retention of the 11-13-week NT ultrasound remains important in the detection of structural anomalies; however, the optimal management of pregnancies with a low-risk NIPT result and an isolated increased NT measurement in an era of advanced genomic testing options is a new dilemma for clinicians. For parents, the prolonged period between the initial diagnosis in first trimester, and prognostic information at each successive stage of investigations up to 22-24 weeks, can be emotionally challenging. This article addresses the common questions from parents and clinicians as they navigate the uncertainty of having a fetus diagnosed with an increased NT after a low-risk NIPT result and presents suggested approaches to management.
© 2021 John Wiley & Sons Ltd.
Similar articles
-
Reexamining the optimal nuchal translucency cutoff for diagnostic testing in the cell-free DNA and microarray era: results from the Victorian Perinatal Record Linkage study.
Hui L, Pynaker C, Bonacquisto L, Lindquist A, Poulton A, Kluckow E, Hutchinson B, Norris F, Pertile MD, Gugasyan L, Kulkarni A, Harraway J, Howden A, McCoy R, da Silva Costa F, Menezes M, Palma-Dias R, Nisbet D, Martin N, Bethune M, Poulakis Z, Halliday J. Hui L, et al. Am J Obstet Gynecol. 2021 Nov;225(5):527.e1-527.e12. doi: 10.1016/j.ajog.2021.03.050. Epub 2021 May 3. Am J Obstet Gynecol. 2021. PMID: 33957116
-
Prenatal screening for fetal aneuploidy in singleton pregnancies.
Chitayat D, Langlois S, Douglas Wilson R; SOGC GENETICS COMMITTEE; CCMG PRENATAL DIAGNOSIS COMMITTEE.
 Chitayat D, et al. J Obstet Gynaecol Can. 2011 Jul;33(7):736-750. doi: 10.1016/S1701-2163(16)34961-1. J Obstet Gynaecol Can. 2011. PMID: 21749752
Chitayat D, et al. J Obstet Gynaecol Can. 2011 Jul;33(7):736-750. doi: 10.1016/S1701-2163(16)34961-1. J Obstet Gynaecol Can. 2011. PMID: 21749752 -
Prenatal screening for and diagnosis of aneuploidy in twin pregnancies.
Audibert F, Gagnon A; Genetics Committee of the Society of Obstetricians and Gynaecologists of Canada; Prenatal Diagnosis Committee of the Canadian College of Medical Geneticists. Audibert F, et al. J Obstet Gynaecol Can. 2011 Jul;33(7):754-67. J Obstet Gynaecol Can. 2011. PMID: 21749753
-
Nuchal translucency of 3.0-3.4 mm an indication for NIPT or microarray? Cohort analysis and literature review.
Petersen OB, Smith E, Van Opstal D, Polak M, Knapen MFCM, Diderich KEM, Bilardo CM, Arends LR, Vogel I, Srebniak MI.
 Petersen OB, et al. Acta Obstet Gynecol Scand. 2020 Jun;99(6):765-774. doi: 10.1111/aogs.13877. Epub 2020 May 12. Acta Obstet Gynecol Scand. 2020. PMID: 32306377 Free PMC article. Review.
Petersen OB, et al. Acta Obstet Gynecol Scand. 2020 Jun;99(6):765-774. doi: 10.1111/aogs.13877. Epub 2020 May 12. Acta Obstet Gynecol Scand. 2020. PMID: 32306377 Free PMC article. Review. -
[Prospective cohort study of fetal nuchal translucency in first-trimester and pregnancy outcome].
Tang HR, Zhang Y, Ru T, Li J, Yang L, Xu Y, Duan HL, Wang Y, Wang Y, Hu YL, Zhang Y, Zheng MM. Tang HR, et al. Zhonghua Fu Chan Ke Za Zhi. 2020 Feb 25;55(2):94-99. doi: 10.3760/cma.j.issn.0529-567X.2020.02.007. Zhonghua Fu Chan Ke Za Zhi. 2020. PMID: 32146737 Chinese.
See all similar articles
Cited by
-
Implementation of Public Funded Genome Sequencing in Evaluation of Fetal Structural Anomalies.
So PL, Hui ASY, Ma TWL, Shu W, Hui APW, Kong CW, Lo TK, Kan ANC, Kan EYL, Chong SC, Chung BHY, Luk HM, Choy KW, Kan ASY, Leung WC. So PL, et al. Genes (Basel). 2022 Nov 10;13(11):2088. doi: 10.3390/genes13112088. Genes (Basel). 2022. PMID: 36360323 Free PMC article.
References
-
- Nicolaides KH, Azar G, Snijders RJ, Gosden CM. Fetal nuchal oedema: associated malformations and chromosomal defects. Fetal Diagn Ther. 1992;7:123-131.
-
- Snijders RJ, Noble P, Sebire N, Souka A, Nicolaides K. UK multicentre project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10-14 weeks of gestation. Fetal Medicine Foundation First Trimester Screening Group. Lancet. 1998;352:343-346.
-
- Hui L, Bianchi DW.
 Noninvasive prenatal testing for aneuploidy - the vanguard of genomic medicine. Annu Rev Med. 2017;68:459-472.
Noninvasive prenatal testing for aneuploidy - the vanguard of genomic medicine. Annu Rev Med. 2017;68:459-472.
- Hui L, Bianchi DW.
-
- Gadsbøll K, Petersen OB, Gatinois V, et al. The NIPT-map Study Group. Current use of noninvasive prenatal testing in Europe, Australia and the USA: a graphical presentation. Acta Obstet Gynecol Scand. 2020;99:722-730.
-
- Lindquist A, Hui L, Poulton A, et al. State-wide utilization and performance of traditional and cell-free DNA-based prenatal testing pathways: the Victorian Perinatal Record Linkage (PeRL) study. Ultrasound Obstet Gynecol. 2020;56(2):215-224.
Publication types
MeSH terms
Substances
Grant support
- Medical Research Future Fund emerging leader fellowship
Full text links
Wiley
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Non-invasive prenatal test Panorama | DNA test in Moscow and St.
 Petersburg
Petersburg Warning : mysql_fetch_array() expects parameter 1 to be resource, boolean given in /home/p570384/www/dnk-center.ru/nipt.php on line 5
Warning : mysql_fetch_array() expects parameter 1 to be resource, boolean given in /home/p570384/www/dnk-center.ru/nipt.php on line Non-invasive prenatal test Panorama | DNA test in Moscow and St. Petersburg - DNA center
Moscow
- Moscow
- St. Petersburg
st. 3 Tverskaya-Yamskaya 52
+7 (495) 777-96-32
- +7 (495) 777-96-32
- +7 (916) 097-84-88
Mon-Fri 8-18, Sat 10-16
At an early stage
From 9 weeks pregnant
Safe and convenient
Routine venous blood sampling nine0017
High accuracy
Accuracy 99.9%
Free consultation
Geneticist will answer questions
Non-invasive prenatal test - the most advanced genetic test in early pregnancy, which determines the risk of chromosomal abnormalities, such as Down syndrome, and the sex of the unborn child, by maternal blood, with an accuracy of 99. 9%.
9%.
| Members | Pregnant woman, term from 9weeks | |
| Price | 29900 RUR rub - basic test; 47900 rub - extended test | |
| Deadline | 12-15 working days | |
| Material | venous blood | |
| Documents | Contract, receipt | |
| Where to return | Moscow, st. 3rd Tverskaya-Yamskaya 52 St. Petersburg, st. Driving around 7 | Enroll |
| Rating | Your vote has been counted! 4.9 / 5.0 ( 12 votes) | |
Benefits of NIPT Panorama
- with 9weeks of pregnancy, due date 12-14 days
- the most complete test - Down's syndrome and 12 more chromosomal abnormalities, fetal sex
- 99.9% accuracy
- safe - only maternal venous blood needed
- free consultation by a laboratory geneticist, before or after the test
What can be determined using the Panorama NIPT test?
Panorama non-invasive test screens for common genetic conditions caused by extra or missing chromosomes in a baby's DNA:
Basic test
- Down syndrome (trisomy 21)
- Edwards syndrome (trisomy 18)
- Patau syndrome (trisomy 13)
- Triploid
- Sex chromosome anomalies:
Klinefelter syndrome (XXY), Jacob syndrome (XYY), Triple X Syndrome (XXX), Turner syndrome (monosomy X)Gender of child
Price: 29 900 rubles nine0017
Extended test
Basic test + Microdeletions
- 22q11.
 2 deletion syndrome (Di Giorgi)
2 deletion syndrome (Di Giorgi) - 1p36 deletion syndrome
- Angelman syndrome
- Prader-Willi Syndrome
- Cat cry syndrome
Child gender
Price: 47 900 rubles
Non-invasive DNA test result
Low risk
Your child is unlikely to have one of the conditions on the test panel.
High risk
Your child is at high risk for this condition.
Each result, except for the risks of chromosomal abnormalities, contains information about the gender of the unborn child: boy or girl
In a small percentage of cases, the test cannot extract enough information from your blood sample to determine an accurate result. If this occurs, a second blood sample may be requested, free of charge. nine0017
Risk of Down syndrome according to maternal age
Enter mother's age (from 20 to 49):
Risk:
Which laboratory performs the Panorama test?
Natera is the world leader in prenatal genetic testing. The company was founded in 2004 by a group of doctors, geneticists, bioinformatics and software developers. Natera has developed its own Panorama NIPT test algorithm, and from 2012 to date, more than 1,500,000 pregnant women worldwide have taken this test. Natera's certified laboratory is located in Silicon Valley, California, USA. nine0017
The company was founded in 2004 by a group of doctors, geneticists, bioinformatics and software developers. Natera has developed its own Panorama NIPT test algorithm, and from 2012 to date, more than 1,500,000 pregnant women worldwide have taken this test. Natera's certified laboratory is located in Silicon Valley, California, USA. nine0017
Nathera Laboratory Certificates
What is the guarantee that NIPT Panorama is performed in the Nathera Laboratory?
According to the results of the analysis, you can order a free genetic consultation . Geneticist from the laboratory of Nater (USA) will call your phone number and take 15 minutes to answer questions about the Panorama NIPT test. The consultation will take place with a translation service.
Why such a low price? We do not cooperate with doctors and do not pay them remuneration. In addition, we have direct contract with Nater's laboratory , so we can offer the lowest price.
Each patient can register on the laboratory website natera.com and track their results. This is not a mandatory procedure, you will receive the result by mail faster. To register, you need to enter your full name in English, number test tubes (Kit ID) - a barcode that is pasted on test tubes. The number of tubes can be obtained in 4-5 business days when the samples arrive and are processed in the laboratory. nine0017
NIPT limitations panorama
The NIPT test is intended for all pregnant women, regardless of age, except for women with the following types of pregnancy:
- Failed twins, with a known missing twin, embryonic reduction, i.e. a singleton pregnancy, which initially started as twins;
- higher order of multiple pregnancies, than twins - triplets, quadruplets;
- pregnancy with twins from a surrogate mother or from donor eggs (for pregnancy with an egg donor or surrogate motherhood, only singleton pregnancy is accepted)
For pregnancy with missing twin or twins using surrogacy or egg donation We recommend the NIPS test.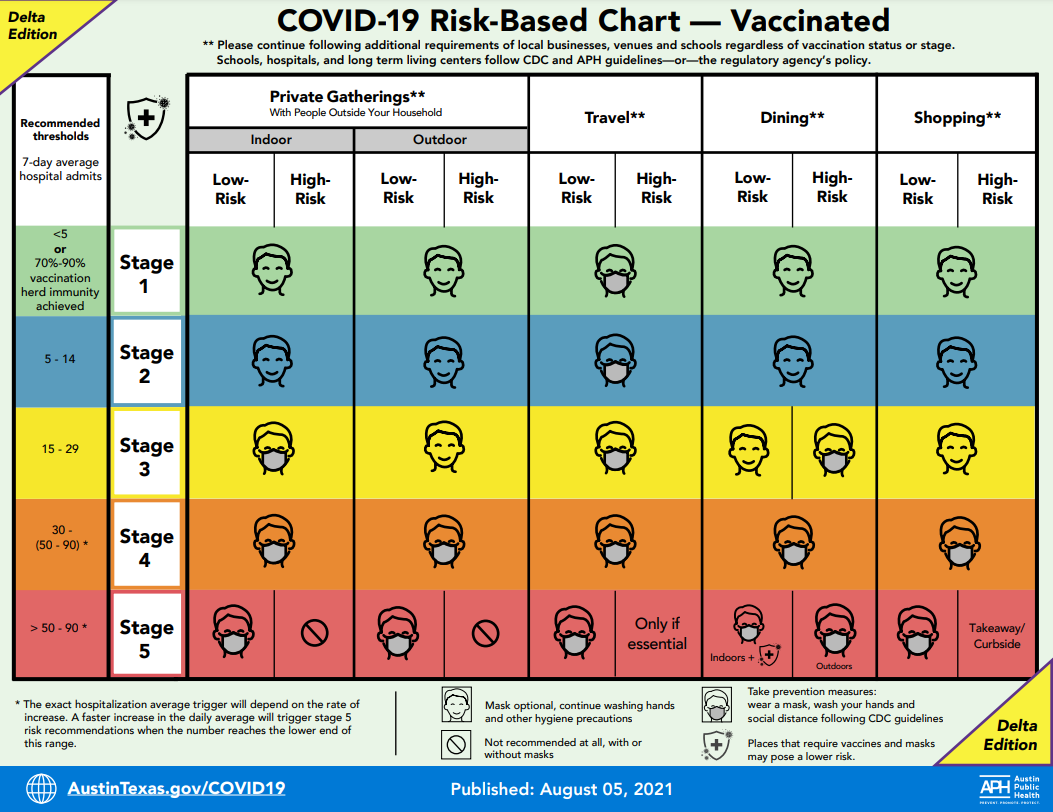
| Results for | Singleton pregnancy (including IVF) | Monozygotic twins | Dizygotic twins | Egg donor and surrogacy (singleton only) |
|---|---|---|---|---|
| Trisomy 21 | Yes | Yes | Yes | Yes |
| Trisomy 18 | Yes | Yes | Yes | Yes |
| Trisomy 13 | Yes | Yes | Yes | Yes |
| Monosomy X | Yes | Yes | No | No |
| Sex chromosome trisomy* | Yes | Yes | No | No |
| 22q11.2 deletion | Yes | Yes | No | No |
| Triploid | Yes | No | No | No |
| Microdeletions: Prader-Willi syndrome Angelman syndrome Cat's cry syndrome 1p36 deletion | Yes | No | No | No |
| Sex of fetus | Yes | Yes, separately for each fetus | Yes, separately for each fetus | Yes |
* - reported when detected
A feature of the Panorama test is that it determines the sex of the fetus separately for each child , and also determines the zygosity - monozygotic or dizygotic . This information is needed by an obstetrician-gynecologist for the correct management of pregnancy.
This information is needed by an obstetrician-gynecologist for the correct management of pregnancy.
Reviews of NIPT Panorama in Moscow and St. Petersburg
My choice - NIPT Panorama
After the second trimester screening, the doctors sent me for an amniocentesis - invasive procedure. Down's syndrome was suspected. Or, if financially feasible, do NIPT, which is safe and accurate. I chose NIPT Panorama, it showed low risk, and I didn't have to pierce my stomach.
Irina, Moscow
I have a healthy boy!
I am 38 years old and automatically fall into the risk group for Down syndrome. And although the screening was normal, the doctors didn't care recommended further testing. NIPT Panorama became my choice, the exact risk and gender of the child is determined by the mother's blood. NIPT showed me a low risk and the sex of the child is a boy! nine0017
Svetlana, Moscow
Excellent service
I received the Panorama NIPT test result, the result was understandable - a low risk of chromosomal aneuploidy and a female sex. But I wanted to know more about some indicators, so I booked a consultation with Nater's lab geneticist. The geneticist called me free of charge on the phone and explained everything.
But I wanted to know more about some indicators, so I booked a consultation with Nater's lab geneticist. The geneticist called me free of charge on the phone and explained everything.
Marina, St. Petersburg
NIPT Panorama the most accurate
I decided to check the health of the unborn child as early as possible, before the first trimester screening because I am over 35 years old. At 9 weeks I donated blood, it was completely painless. After 10 days, the result was ready, low risk and sex - a boy. I calmed down and no longer worried, until the birth.
Ani, Moscow
Questions about Panorama NIPT
Is Panorama NIPT right for me?
The NIPT test is a mandatory test for all pregnant women in the US and developed countries in Europe. It is recommended to absolutely every pregnant woman. Some women are more likely to have certain conditions, such as Down syndrome, in their baby, especially if they: nine0017
- pregnant woman over 35;
- in the family history there is a patient with genetic abnormalities;
- abnormal ultrasound findings;
- abnormal blood chemistry results.

How is the NIPT test performed?
The non-invasive prenatal Panorama test is performed on a sample of the mother's blood from a vein in her arm. During pregnancy, some DNA the baby passes into the mother's bloodstream. The Panorama test looks at these DNAs for signs of certain genetic conditions that can affect child's health. Already since 9weeks, the concentration of fetal DNA (fetal DNA) is sufficient for testing.
What other options are there for prenatal testing?
1. Conventional screening tests - Ultrasound and blood chemistry screening - not as accurate as the NIPT test, and screening for fewer conditions. If screening shows an abnormal result, NIPT is recommended.
2. Diagnostic invasive tests such as amniocentesis or chorionic villus sampling give a definitive diagnosis and are able to identify a greater number of conditions, but are associated with a 1-2% risk of pregnancy complications, including termination of pregnancy. If NIPT shows a low risk, these dangerous procedures should not be done. If NIPT shows high risk, it is recommended to confirm with invasive procedures.
If NIPT shows a low risk, these dangerous procedures should not be done. If NIPT shows high risk, it is recommended to confirm with invasive procedures.
| Test type | Test validity | Degree of risk |
|---|---|---|
| 1st trimester screening | Low (80 - 95%) | Safe. No risk to mother or baby |
| Invasive Prenatal Diagnostics | High (> 99%) | 1 in 200 risk of miscarriage |
| High (> 99%) | Safe. No risk to mother or baby |
What is the fetal fraction?
Fetal fraction - the proportion of fetal DNA in the mother's blood. If the proportion of DNA is less than 2%, the result will not be issued, and you will need to retake blood In 2 weeks. If the woman is not pregnant, the fetal fraction will be low and the test will not show a result. Sometimes a low fetal fraction can indicate fetal abnormalities.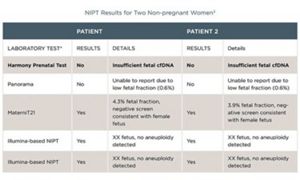
Why is testing for microdeletions recommended?
- Microdeletions are small missing portions of chromosomes.
- They are common and can be severe
- They often go undiagnosed
- Same risk for mothers of any age
- They respond to early childhood intervention
- The combined incidence of these five microdeletion syndromes at birth is approximately 1:1000
Other than low risk and high risk of Down syndrome, what other outcomes are there?
There is a high risk result of Turner syndrome in girls - monosomy X. nine0017
Boys are often at high risk for Klinefelter's syndrome.
Sign up for analysis "NIPT Panorama"
If there is no collection point in your city, you can order a set from us and send us samples.
What NIPT results might look like and what they mean
YOUR MAIN PREGNANCY TEST
Accurate and safe prenatal DNA test (NIPT)
Get tested today ,
get the result
Select date Order a test
The term of the study is from 2 to 7
calendar days from the date of receipt of
biomaterials in the laboratory in Moscow
- Test range
- About study
- Questions and answers
- Clinical Information
Traditional prenatal screening methods using serum proteins and ultrasound (combined screening) produce many false positives, so an additional invasive procedure (chorionic biopsy or amniocentesis) is often required to distinguish false positives from true ones. nine0017
nine0017
No less dangerous are false-negative results of combined screening, which do not reveal chromosomal pathology, which leads to the birth of a sick child.
NIPT results contain important information about the health of the unborn child, which in most cases is understandable and does not require additional comments.
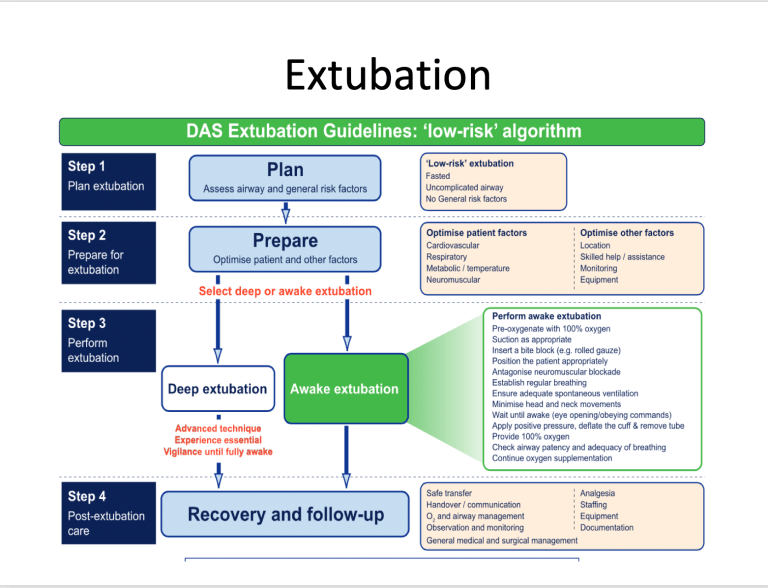
Consider the main options for conclusions based on the results of NIPT:
1. Low risk of fetal chromosome abnormality
This result means that the probability of encountering the studied chromosomal abnormalities is extremely low. It is necessary to continue observation by an obstetrician-gynecologist with the implementation of planned ultrasound examinations of the fetus.
Separate consideration should be given to low-risk NIPT results for ultrasound markers or fetal malformations.
Since there are many more possible causes of these abnormalities than NIPT can detect, we recommend that you discuss prenatal chromosome microarray testing with your geneticist and OB/GYN. nine0017
nine0017
We do not recommend NIPT if ultrasound markers or fetal malformations were identified prior to NIPT and there are no contraindications for chorion biopsy or amniocentesis.
2. High risk of a chromosomal abnormality in the fetus
If a high risk is identified, a geneticist should be consulted.
Available data suggest that out of 1000 patients at high risk of having a child with Down syndrome, this chromosomal abnormality is confirmed in 999 during invasive diagnostics. nine0017
Since NIPT is a screening test, confirmation of the result by prenatal chromosome microarray analysis is required when a high risk is detected, especially if it is a continuation of the pregnancy.
3. No result. Low fetal fraction
Thanks to the measurement of the level of the fetal fraction during all NIPT in the Genomed laboratory, false results are avoided.
However, in some cases, the amount of fetal DNA is not enough to conduct the study. nine0017
This may be due to various reasons, including those related to the weight of the pregnant woman and the characteristics of her placenta.