Little red dots on baby belly
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Baby Rashes: Types, Symptoms & More
Baby’s have incredibly sensitive skin, which makes them more likely to develop rashes than adults and older kids. But with all the different types out there, it can be hard to identify what the baby rash is, what’s causing it and how to treat it. Plus, no parent wants to see their precious little one with a red or bumpy reaction on their soft skin. Many might wonder how rashes affect baby’s comfort level and whether they cause itchiness or pain. And how can parents tell if baby’s rash is a harmless diaper rash or something a little more serious?
And how can parents tell if baby’s rash is a harmless diaper rash or something a little more serious?
Because there are so many types of baby rashes, it’s important to be aware of the symptoms to look out for and know when to call the pediatrician. To help you better identify a baby rash on the body, we’ve put together a handy guide on all things rashes. Keep reading to learn more about the common types of baby rash, tell-tale signs and symptoms and the best remedies to treat them.
In this article:
Baby rash causes
baby acne or baby rash?
Baby heat rash
Meningitis rash
Strep rash
Chicken pox
Baby drool rash
Baby eczema rash
Hives
Baby allergy rash
Baby fungal rash
Cradle cap
When to be concerned about baby rashes
Baby Rash Causes
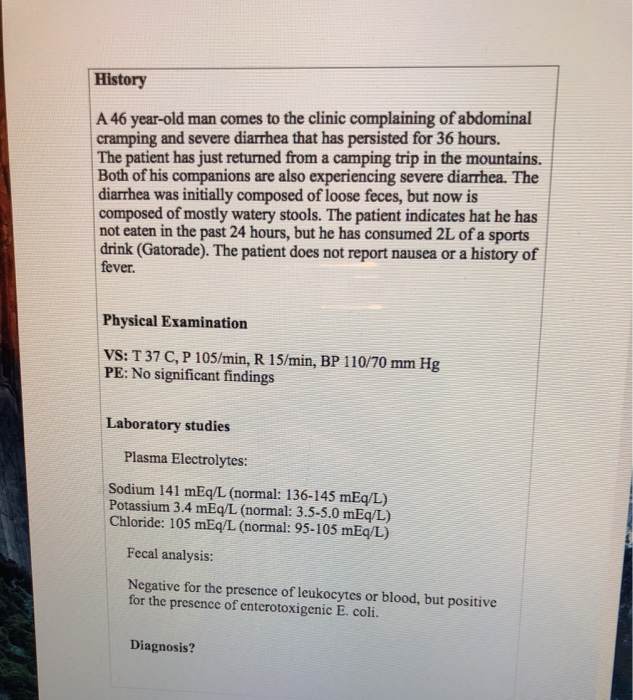
When it comes to baby rashes, there are many types and many culprits. Some common causes include:
-
Irritants. Common irritants that can bother baby’s sensitive skin are saliva and drool, poop, baby wipes, detergents, soaps, sunscreen and nickel.

-
Allergies. Allergic reactions can cause a baby rash to appear in a bunch of different forms. Rashes can be itchy, welt-like hives or dry, itchy patches. Eczema is the most common version of a baby rash caused by allergies.
-
Infections. Infections can lead to different types of baby rash, the most common of which are fungal rashes. Sometimes, however, a viral baby rash can develop. “These rashes occur when babies have specific viral illnesses and may be associated with fever or other symptoms,” says Anna Bender, MD, a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian. A viral baby rash can appear as small dots on the torso and sometimes arms and legs, and can last for several days to a week. It may spread for a few days and then begin to clear up.
“Baby’s skin barrier is especially fragile because it’s thinner, immature and the skin is still developing, so that makes it a lot more vulnerable to damage and dryness. It’s also more reactive, especially to things that could be irritants,” explains Lauren R. Crosby, MD, FAAP, a pediatrician at LaPeer Pediatrics in Beverly Hills, California. Baby’s skin is typically ultra-sensitive from birth until around age 2, although diaper rash can continue to rear its head past that age until kids are potty trained.
It’s also more reactive, especially to things that could be irritants,” explains Lauren R. Crosby, MD, FAAP, a pediatrician at LaPeer Pediatrics in Beverly Hills, California. Baby’s skin is typically ultra-sensitive from birth until around age 2, although diaper rash can continue to rear its head past that age until kids are potty trained.
In our guide below, we outline the different ways baby rashes look and behave. Keep reading for the most common types of baby rash to keep an eye out for, plus how to prevent and treat them. From heat rashes to chicken pox, we help make sense of any bumps or blotches you may find on baby.
Baby Acne or Baby Rash?
Breakouts aren’t just for teenagers—it’s actually totally normal for babies to get acne. “Also known as neonatal acne, it’s a common rash in babies during the first month of life,” Bender says. “It’s thought that maternal hormones—those that pass from mother to baby in utero—may cause baby acne to flare.”
But how can you tell if it’s baby acne or a baby rash? Baby acne typically looks like a bunch of small, red bumps, as opposed to the lacy red of a baby rash.
Image: iStock
Baby acne symptoms
- Pimples. Baby acne usually involves clusters of tiny red pimples and whiteheads.
- Irritated cheeks. Baby acne usually develops on the cheeks, but it can also appear on baby’s nose, forehead and sometimes behind the ears and on the scalp.
- Persistent symptoms. Baby acne can last up to three to four months.
Prevention and treatment
Usually, baby acne clears up on its own with gentle cleansing. Once in a while parents might need to see a dermatologist if it’s persisting beyond the normal three to four months, but that’s pretty rare.
Baby Heat Rash
Baby heat rash tends to happen when baby’s sweat glands become blocked and trap sweat under the skin, Crosby says. It’s usually seen in warm weather or when baby is overdressed. How do you know if the baby rash is caused by heat?
Image: Shutterstock
Heat rash symptoms
- Tiny red bumps.
 These typically appear on baby’s head, neck and shoulders, and sometimes on the chest.
These typically appear on baby’s head, neck and shoulders, and sometimes on the chest. - Itching. Sometimes heat rash can be itchy, so take note if baby is scratching at their irritated skin.
Prevention and treatment
To prevent baby heat rash, dress baby in lighter clothing to make sure they aren’t getting overheated or sweaty. In warm climates, it’s fine to let them sleep in just a onesie and diaper, and run a fan in the bedroom to keep the air cool and circulating. When baby heat rash does strike, “I recommend a daily bath with a non-fragrant sensitive skin cleanser to help clear out the sweat and keep the skin clear,” Crosby says. A baby rash from heat usually goes away on its own in three to four days, as long as baby isn’t overdressed and stays in a cool environment.
Baby Diaper Rash
It’s pretty self-explanatory where you can expect to see this baby rash. “Diaper rash can occur due to irritation from wet diapers and friction,” Bender says. Baby diaper rash is even more common in older babies who sleep through the night longer and may have wetter diapers in the morning.
Baby diaper rash is even more common in older babies who sleep through the night longer and may have wetter diapers in the morning.
Image: Shutterstock
Diaper rash symptoms
- Red patches. These typically appear on the rounded part of baby’s bottom.
- Puffy, warm skin. In some cases, baby’s skin may be slightly raised and feel warm to the touch.
Prevention and treatment
“Diaper rash can improve with frequent diaper changes and use of over-the-counter diaper paste containing zinc oxide, which helps in acting as a barrier to prevent friction and irritation in the diaper area,” Bender says. Ward off baby diaper rash by making sure the skin is completely dry before you put on a fresh diaper. In the past, baby powder was the go-to trick for absorbing moisture and protecting baby’s skin, but doctors no longer recommend using powder for diaper rash, since inhaled powder can irritate baby’s lungs.
Sometimes a rash on baby’s butt can actually be a yeast rash caused by fungus that lives on our skin.
Image: iStock
Yeast rash symptoms
- Pink patches. These patches usually appear in baby’s skin folds, accompanied by small pink dots or pustules around the edge.
Prevention and treatment
To treat a baby yeast rash, apply a topical, over-the-counter antifungal cream a few times a day. Prevent yeast rash by keeping baby clean and dry.
Meningitis Rash
Meningitis is when the lining around the brain and spinal cord (the meninges) is inflamed, and “is a serious infection because it can be present in the blood and brain and cause organ damage, permanent brain damage or death,” Bender says.
While the viral form of meningitis is serious, it’s almost never life-threatening, according to the Centers for Disease Control and Prevention (CDC). Bacterial meningitis, however, can be deadly and calls for immediate medical attention. There’s a vaccine for bacterial meningitis, but it typically isn’t given until later in childhood or before college. You can’t tell the difference between a baby rash caused by bacterial or viral meningitis, and in many cases a rash won’t appear at all.
There’s a vaccine for bacterial meningitis, but it typically isn’t given until later in childhood or before college. You can’t tell the difference between a baby rash caused by bacterial or viral meningitis, and in many cases a rash won’t appear at all.
Image: iStock
Meningitis symptoms
- High fever. Take baby’s temperature, since a high fever is a classic sign of meningitis.
- Lethargy. If baby is less active than usual, it could be another signal of meningitis.
- Vomiting. This symptom is more common in infants, along with a loss of appetite and irritability.
- Rashes. Meningitis rashes can vary in appearance, but the most common ones include pink or red dots all over, purple rashes that can look like tiny bruises or broken capillaries in the skin, and an itchy, red rash.
Prevention and treatment
Viral meningitis usually clears up on its own in seven to 10 days, but bacterial meningitis requires immediate medical attention so antibiotics can be given as soon as possible. Serious cases may call for hospitalization. If you think baby might have meningitis, call your doctor right away—they can determine if baby has the disease and the type of meningitis.
Serious cases may call for hospitalization. If you think baby might have meningitis, call your doctor right away—they can determine if baby has the disease and the type of meningitis.
Strep rash
A strep rash on baby is another type of viral baby rash. Your child is more prone to strep rash if other family members have been exposed to strep throat.
Image: iStock
Strep rash symptoms
- Bright red skin. Strep rash on baby can be bright red and beefy-looking with wet, oozing patches in neck folds, or as a bright red circle patch in the area around baby’s anus, Bender says.
- Blisters and scabbing. Spotting scabs and blisters on baby’s skin is another common sign of strep.
Prevention and treatment
Since strep can spread from person to person through close contact, keep baby away from infected people. Unlike your run-of-the-mill neck rash, which can be treated with over-the-counter antifungal creams, strep requires a visit to the doctor. Once the diagnosis of strep rash is confirmed—typically with a skin swab test—your pediatrician may prescribe an oral antibiotic as treatment.
Once the diagnosis of strep rash is confirmed—typically with a skin swab test—your pediatrician may prescribe an oral antibiotic as treatment.
Chicken Pox
Chicken pox appears as a baby rash on the body. Before the chicken pox—or varicella—vaccine became available in 1995, practically every child came down with chicken pox before age 9, according to the American Academy of Pediatrics (AAP). Nowadays, it’s pretty rare for babies to get chicken pox, thanks to the vaccine. It’s a super-contagious viral infection caused by the varicella zoster virus, so avoid contact with infected people to keep baby safe.
Image: Shutterstock
Chicken pox symptoms
- Red bumps and blisters. Chicken pox causes a blister-like baby rash on the skin, starting on the back, tummy or face and spreading all over baby’s body. The blisters are often in different stages of healing, so some may look like pink bumps, some look like scabbed bumps and others may look like blisters.

- Itchiness. Chicken pox rashes are renowned for their intense itchiness.
- Fever. A temperature of 101 to 102 degrees Fahrenheit is common with chicken pox.
Prevention and treatment
Doctors recommend daily baths and keeping baby’s nails short so they can’t scratch and dig into their skin, which could cause a secondary infection. Typically, the course of treatment for chicken pox is to wait it out—it can last five to seven days—but in severe cases (which aren’t common), an antiviral medication may be prescribed. To prevent chicken pox, the APP recommends that healthy babies get the first dose of the vaccine between 12 and 15 months old, followed by a second dose at age 4 to 6.
Baby Drool Rash
Noticing a baby rash on your little one’s face? When babies’ saliva glands turn on, usually around 3 or 4 months of age, they start to drool. A lot. “If you think about it, saliva is part of your digestive tract,” Crosby says. “It’s not just water, so it’s irritating.”
“It’s not just water, so it’s irritating.”
Image: Courtesy of Wissabo/Instagram
Baby drool rash symptoms
- A red, irritated baby rash on the face. Because the skin around baby’s mouth, chin and neck is constantly wet, these areas are especially prone to drool rash.
- Flaking skin. Baby rash from drool can also appear slightly flaky and dry-looking.
Prevention and treatment
One way to prevent and heal a baby rash caused by drool? Have a soft bib handy to keep the skin on baby’s face and chest dry. Apply a gentle over-the-counter ointment before and after meals as a barrier to prevent saliva from touching the skin, so baby’s drool rash can heal underneath it.
Baby Eczema Rash
Eczema, often-chronic red, dry patches of skin, is one of the most common skin disorders in babies—in fact, 60 percent of infants get eczema in the first year of life. “Sometimes babies scratch so much, it can lead to bleeding and can interfere with sleep,” Bender says. “Babies with eczema often scratch more in the evening when they’re put to bed or at night when they aren’t distracted by other activities.” Eczema can get infected if not treated, leading to scabbing and oozing skin spots.
“Babies with eczema often scratch more in the evening when they’re put to bed or at night when they aren’t distracted by other activities.” Eczema can get infected if not treated, leading to scabbing and oozing skin spots.
Image: iStock
Baby eczema symptoms
- Itchiness. The more severe baby’s eczema is, the more itchy the rash.
- Dry skin patches. This is a common sign of mild eczema.
- Pinker patches of dry, flaky skin. This signifies a moderate case of eczema.
- Red, flaky patches of skin. If baby’s skin is a darker red, it signifies severe eczema, which usually comes with worsened symptoms and intense itchiness across more of the body.
Prevention and treatment
Keeping baby’s skin well moisturized with a daily application of a thick cream can prevent the onset of eczema in infants who are at higher risk for the condition—aka those who have a strong family history of eczema or eczema-related diseases. A mild case of this baby rash can sometimes be treated with just moisturizer, while moderate eczema may need a cortisone cream or ointment to treat it. Severe eczema is treated with over-the-counter products.
A mild case of this baby rash can sometimes be treated with just moisturizer, while moderate eczema may need a cortisone cream or ointment to treat it. Severe eczema is treated with over-the-counter products.
“Hives can occur soon after baby eats something they’re allergic to or if baby is fighting a virus, in which case the hives may last for several days off and on,” Bender says. They can appear anywhere on the body, even if caused by food. If the baby rash is sparked by something your child touched, it usually appears on the part of baby’s body that came in contact with the allergen. If hives are accompanied by wheezing or if baby’s mouth or tongue starts to swell, see a doctor immediately.
Image: Shutterstock
Hive symptoms
- Pink, blotchy welts. These welts can come and go on baby’s skin.
- Itching. Hive welts are often very itchy.
Prevention and treatment
An oral antihistamine, such as Benadryl, can help treat hives. For a more natural remedy, try dabbing calamine lotion on the welts to soothe hives.
For a more natural remedy, try dabbing calamine lotion on the welts to soothe hives.
Baby Allergy Rash
As you expose baby to new products, foods and materials, there’s always a small chance they could be allergic to a certain ingredient or chemical. These rashes can be caused by food or medication that baby’s allergic to, or when baby’s skin comes into contact with an irritant, Crosby says.
So what does an allergy rash look like on a baby? A baby allergy rash can manifest in different ways, but the two most common signs are hives and eczema. As mentioned above, hives usually show up as pink blotchy welts, while eczema appears as red, dry, flaky patches. Both rashes are itchy.
Image: Shutterstock
Allergy symptoms
If you notice the following symptoms, take baby to the ER:
- Swelling of the lips or face. If baby’s lips or face become swollen, it’s a sign of a severe allergic reaction and should be treated by a doctor immediately.

- Wheezing. Any sign of difficulty breathing is a red flag.
Prevention and treatment
“Treatment depends on the age of the child and what is triggering it,” Crosby says. “You want to remove the allergen or trigger if you can, and use a topical or oral allergy medicine.” Sometimes a blood or skin test might be needed to figure out what baby is having an allergic reaction to, and then a baby rash treatment can be prescribed.
Baby Fungal Rash
A fungal baby rash is often caused by chronically wet or irritated skin. A yeast infection is the most common type of fungal rash. It can also appear in babies if another family member or family pet has ringworm.
Image: iStock
Fungal rash symptoms
- Pink, ring-like flaking patches of skin. These flaky patches can pop up anywhere on the skin, including the scalp and diaper area.
Prevention and treatment
“A fungal rash needs a special antifungal cream, or if it’s on the scalp and hair, it may need an oral antifungal medication,” Bender says. To prevent fungal baby rash, keep the skin clean and dry.
To prevent fungal baby rash, keep the skin clean and dry.
Cradle Cap
Essentially dandruff for babies, cradle cap is relatively common and typically caused by yeast. This type of baby rash usually shows up in the first month of life but can occur any time, Crosby says.
Image: iStock
Cradle cap symptoms
- Flaky skin. Rough, yellowish or pink crustry or oily scaly patches on the scalp are a classic sign of this type of baby rash.
- A slight oily scent. This results from the buildup of oil on baby’s scalp in moderate to severe cases.
Prevention and treatment
Most cases of cradle cap can be treated with regular shampooing and a soft scalp brush to loosen the flakes. If that doesn’t cut it, your pediatrician may recommend a medicated shampoo.
In general, the trick to preventing baby rash is keeping your child’s skin healthy. It’s best to keep baths to 10 minutes or less and use lukewarm water, since “during a bath, skin can really lose moisture, and babies are much more prone to getting dry skin,” Crosby says. Hydrating baby’s skin regularly is crucial. The best time to apply lotion? The first five minutes after a bath, to lock in moisture. “The skin is the largest organ in the body and it’s there to protect us from the elements and infections,” Crosby says. “The importance of really caring for it from infancy through adulthood can’t be stressed enough.”
Hydrating baby’s skin regularly is crucial. The best time to apply lotion? The first five minutes after a bath, to lock in moisture. “The skin is the largest organ in the body and it’s there to protect us from the elements and infections,” Crosby says. “The importance of really caring for it from infancy through adulthood can’t be stressed enough.”
Do baby’s lumps or bumps not line up with any of those listed in this guide? Baby can also develop a rash as a result of bug bites, sunburns, poison ivy and even dry skin. If you’re still not sure about baby’s rash, don’t hesitate to give your pediatrician a call or schedule an appointment.
When to Be Concerned About Baby Rashes
Now that you are familiar with some of the most common kinds of baby rashes, you’re probably wondering, “when should I be concerned about my baby’s rash?”
The truth is, many baby rashes are harmless, and some will come and go on their own without any medical treatment. The other good news is that there are vaccinations to prevent many serious rashes from developing in the first place.
With that said, there are some signs you should keep an eye out for when you notice a baby rash on the body. Some baby rashes can indicate a potentially grave condition, particularly if the rash is persistent or if baby is experiencing swelling or wheezing.
Contact a doctor if baby experiences any of the following:
- If there is pain at the site of the rash
- If baby runs a fever
- If the rash develops bruise-like lesions
- If the rash oozes, bleeds or blisters
- If the rash continues to spread across baby’s body
- If baby develops any cold symptoms (coughing, wheezing, etc.)
- If baby has swollen neck glands or swollen lips
- If the baby rash doesn’t go away after two days
It’s true babies tend to get rashes left and right, but that doesn’t mean you should shrug them off as nothing. Whenever you notice a baby rash on their face or body, keep a watchful eye on it and look out for other symptoms. When it comes to baby’s health, it’s always best to be precautious and proactive.
About the experts:
Anna Bender, MD, is a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian. She earned her medical degree from Columbia University College of Physicians and Surgeons in 2007. After completing her residency training in dermatology at New York Presbyterian Hospital - Weill Cornell Medical Center, Bender completed an additional year of specialized fellowship training in pediatric dermatology at the Johns Hopkins University School of Medicine.
Lauren R. Crosby, MD, FAAP, is a parenting expert and pediatrician at LaPeer Pediatrics in Beverly Hills, California. She earned her medical degree at UCLA School of Medicine and afterwards trained at Cedars-Sinai Medical Center, during which time she served as chief resident. She is a member and official spokesperson of the American Academy of Pediatrics.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Baby Skin Care 101
13 Diaper Rash Creams That Work Wonders
The Best Baby Eczema Creams, Shampoos and Washes
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the site
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child nine0034
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment nine0034
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
- nine0079
Parental leaflet on viral diseases
Parental leaflet.
Measles is a viral infection with a very high susceptibility. If a person has not had measles or has not been vaccinated against this infection, then after contact with the patient, infection occurs in almost 100% of cases. The measles virus is highly volatile. The virus can spread through ventilation pipes and elevator shafts - at the same time, children living on different floors of the house get sick. nine0003
The period from contact with a person with measles to the appearance of the first signs of the disease lasts from 7 to 14 days.
The disease begins with a severe headache, weakness, fever up to 40 degrees C. A little later, a runny nose, cough and almost complete lack of appetite join these symptoms.
Very characteristic of measles is the appearance of conjunctivitis - inflammation of the mucous membrane of the eyes, which is manifested by photophobia, lacrimation, sharp redness of the eyes, and subsequently - the appearance of purulent discharge. These symptoms last 2 to 4 days. nine0003
These symptoms last 2 to 4 days. nine0003
On the 4th day of illness, a rash appears , which looks like small red spots of various sizes (from 1 to 3 mm in diameter), with a tendency to merge. The rash occurs on the face and head (its appearance behind the ears is especially characteristic) and spreads throughout the body for 3-4 days. It is very characteristic of measles that the rash leaves behind pigmentation (dark spots that persist for several days), which disappears in the same sequence as the rash appears. nine0003
Measles can cause serious complications . These include inflammation of the lungs (pneumonia), inflammation of the middle ear (otitis media), and sometimes such a formidable complication as encephalitis (inflammation of the brain).
It must be remembered that after suffering from measles for a sufficiently long period of time (up to 2 months) there is a suppression of immunity, so the child can get sick with some cold or viral disease, so you need to protect him from excessive stress, if possible from contact with sick children. nine0003
nine0003
After measles, lifelong immunity develops. All those who have had measles become immune to this infection.
The only reliable protection against the disease is vaccination against measles, which is included in the National Immunization Schedule.
Reminder for parents.
Rubella is an airborne viral infection. As a rule, children who stay in a water room for a long time with a child who is a source of infection get sick. Rubella in its manifestations is very similar to measles, but it is much easier. nine0003
The period from contact to the appearance of the first signs of illness lasts from 14 to 21 days.
Rubella begins with an increase in the occipital lymph nodes and an increase in body temperature up to 38 degrees C. A runny nose, and sometimes a cough, joins a little later. A rash appears 2 to 3 days after the onset of the disease. Rubella is characterized by a pink, punctate rash that begins with a rash on the face and spreads throughout the body. Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days. nine0003
Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days. nine0003
The treatment of rubella is to relieve the main symptoms - the fight against fever, if any, the treatment of the common cold, expectorants.
Complications from rubella are rare.
After rubella, immunity also develops, re-infection is extremely rare, but can occur.
It is therefore very important to get the rubella vaccine, which, like the measles vaccine, is included in the National Immunization Schedule. nine0096
Note for parents.
Mumps (mumps) is a childhood viral infection characterized by acute inflammation in the salivary glands.
Infection occurs by airborne droplets. Susceptibility to this disease is about 50-60% (that is, 50-60% of those who were in contact and who were not ill and not vaccinated get sick).
It can take 11 to 23 days from contact with a sick mumps to the onset of illness. nine0003
Mumps begins with an increase in body temperature up to 39 degrees C and severe pain in or under the ear, aggravated by swallowing or chewing. At the same time, salivation increases. Swelling quickly grows in the area of the upper part of the neck and cheeks, touching this place causes severe pain in the child. Unpleasant symptoms disappear within three to four days: body temperature decreases, swelling decreases, pain disappears.
However, quite often mumps ends inflammation in glandular organs such as pancreas (pancreatitis), gonads. Past pancreatitis in some cases leads to diabetes mellitus . Inflammation of the gonads (testicles) is more common in boys. This significantly complicates the course of the disease, and in some cases may result in infertility. In especially severe cases, mumps can be complicated by viral meningitis (inflammation of the meninges), which is severe. nine0003
nine0003
After a disease, a strong immunity is formed, but complications can lead to disability.
The only reliable protection against the disease is vaccination against mumps, which is included in the National Immunization Schedule.
Reminder for parents.
Varicella (chickenpox) is a common childhood infection. Mostly young children or preschoolers are ill. Susceptibility to the causative agent of chickenpox (the virus that causes chickenpox refers to herpes viruses) is also quite high. About 80% of contact persons who have not been ill before develop chickenpox. nine0003
14 to 21 days pass from the moment of contact with a patient with chickenpox until the first signs of the disease appear.
The disease begins with a rash. Usually it is one or two reddish spots, similar to a mosquito bite. These elements of the rash can be located on any part of the body, but most often they first appear on the stomach or face. Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear.
Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear. This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears. nine0003
This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears. nine0003
Treatment of chickenpox is to reduce itching, intoxication and prevent bacterial complications. The elements of the rash must be lubricated with antiseptic solutions (as a rule, this is an aqueous solution of brilliant green or manganese). Treatment with coloring antiseptics prevents bacterial infection of rashes, allows you to track the dynamics of the appearance of rashes. It is necessary to monitor the hygiene of the mouth and nose, eyes - you can rinse your mouth with a solution of calendula, the mucous membranes of the nose and mouth also need to be treated with antiseptic solutions. nine0003
Complications of chickenpox include myocarditis - inflammation of the heart muscle, meningitis and meningoencephalitis (inflammation of the meninges, brain matter), inflammation of the kidneys (nephritis). Fortunately, these complications are quite rare. After chicken pox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
After chicken pox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
Reminder for parents.
Scarlet fever is the only childhood infection caused not by viruses but by bacteria (group A streptococcus). This is an acute disease transmitted by airborne droplets. Infection through household items (toys, dishes) is also possible. Children of early and preschool age are ill. The most dangerous in terms of infection are patients in the first two to three days of the disease. nine0003
Scarlet fever begins very acutely with fever up to 39 degrees C, vomiting, headache. The most characteristic symptom of scarlet fever is tonsillitis in which the mucous membrane of the throat has a bright red color, swelling is pronounced. The patient notes a sharp pain when swallowing. There may be a whitish coating on the tongue and tonsils. The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
By the end of the first beginning of the second day of illness, 9 appears0095 the second characteristic symptom of scarlet fever is a rash. It appears immediately on several parts of the body, most densely located in the folds (elbow, inguinal). Its distinguishing feature is that the bright red punctate scarlatinal rash is located on a red background, which gives the impression of a general confluent redness. When pressed against the skin, a white line remains . The rash may be spread over the entire body, but there is always a clean (white) area of skin between the upper lip and nose, and also the chin. Itching is much less pronounced than with chicken pox. nine0003 Rash lasts up to 2 to 5 days. The manifestations of sore throat persist a little longer (up to 7-9 days). Scarlet fever is usually treated with antibiotics because the causative agent of scarlet fever is a microbe that can be eliminated with antibiotics and strict adherence to bed rest . Almost exclusively children suffer from scarlet fever because with age a person acquires resistance to streptococci. Those who have been ill also acquire strong immunity. Memo for parents. Whooping cough is an acute infectious disease characterized by a long course. The hallmark of the disease is a spasmodic cough. The mechanism of transmission of infection is airborne. 3 to 15 days pass from the moment of contact with a person with whooping cough until the first signs of the disease appear. Whooping cough feature is a gradual increase in cough within 2 to 3 weeks after its onset. Typical signs of whooping cough: Whooping cough is often complicated by bronchitis, otitis media, pneumonia, rectal prolapse, umbilical and inguinal hernias. After having had whooping cough for a long time (several months), coughing fits may return, especially if the child catches a cold or during physical exertion. nine0003 The only reliable prevention against pertussis is vaccination with DTP, a vaccine included in the National Immunization Schedule. Parents' fears about the harmful effects of the vaccine are unfounded. The quality of the DTP vaccine is not inferior in its properties to vaccines produced in other countries. Memo for parents. Acute intestinal infections is a large group of diseases that occur with more or less similar symptoms, but can be caused by a huge number of pathogens: bacteria, viruses, protozoa. nine0003 In summer, the number of intestinal infections in children inevitably increases. Firstly, , in summer a large amount of raw vegetables, fruits and berries are consumed, on the unwashed surface of which a huge number of microbes, including potentially dangerous ones, live. Secondly, , children spend a lot of time outdoors in summer, and not always even their parents remember that eating with clean hands is a mandatory rule . The third reason : in the summer, getting into foodstuffs (dairy products, meat, fish, broths), some pathogens multiply at a tremendous speed and quickly reach the amount that successfully breaks through the protective barriers of the gastrointestinal tract. From the moment the pathogen enters the gastrointestinal tract to the onset of the disease, it can take from several hours to 7 days. The disease begins with fever, malaise, weakness, lethargy. Appetite is sharply reduced, nausea, vomiting quickly joins. Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.
Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.  A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.
A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.

 There are several reasons for this.
There are several reasons for this.  The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. nine0095 Self-treatment not allowed
The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. nine0095 Self-treatment not allowed
Prevention of intestinal infections requires strict adherence to general hygiene measures in the home, when preparing food and while eating.
In the summer, all foodstuffs should be protected from flies. Ready food should be stored in the refrigerator: at a low temperature, even if microbes get into the food, they will not be able to multiply. The disease can also be caused by illegibility when buying products that are eaten without heat treatment - from the hands, outside the markets, where they do not pass sanitary control. When swimming in open water, in no case should water be swallowed. If you eat on the beach, wipe your hands with at least special wet wipes. nine0003
nine0003
And remember that parental example is the best way to teach a child.
Parent Guide .
Tuberculosis is a chronic infectious disease caused by mycobacterium human tuberculosis, affecting mostly the respiratory organs, as well as all organs and systems of the body.
The source of infection for is people with tuberculosis. The most common is the air way of infection. Transmission factors are nasopharyngeal mucus, sputum and dust containing bacteria. nine0003
Reproduction of tuberculosis bacteria in the child's body leads to significant functional disorders with symptoms of intoxication: irritability appears or, conversely, lethargy, fatigue, headache, sweating. With a long course of the disease, the child loses weight, the skin becomes pale, and there is a tendency to inflammatory diseases. For children, a reaction from the lymph nodes is typical: they increase in size, become dense.