When should a baby turn in the womb
Breech pregnancy | Pregnancy Birth and Baby
Breech pregnancy | Pregnancy Birth and Baby beginning of content8-minute read
Listen
How will I know whether my baby is in the breech position or not?
Most babies settle into a head-down position, ready for birth, by about the last month of pregnancy. Health professionals call this a ‘vertex’ or ‘cephalic’ position.
When a baby is positioned bottom-down late in pregnancy, this is called the breech position.
It is fairly common for a baby to be in a breech position before 35 to 36 weeks gestation, but most gradually turn to the head-down position before the last month.
Your doctor or midwife will feel your abdomen when you have your pregnancy check-ups in second and third trimesters — this is called an 'abdominal palpation'. When they feel your abdomen at 35 to 36 weeks, they will assess whether the baby has settled into a head-down position in preparation for birth. If they suspect your baby might be in a breech position, they can confirm this with an ultrasound scan.
There are 3 main types of breech position. All of them involve the baby being in a bottom-down, head up, position. The variations of breech include:
- frank breech — the baby’s legs are straight up in front of its body in a V shape, so its feet are up near its face
- complete or flexed breech — the baby is in a sitting position with its legs crossed in front of its body and its feet near its bottom
- footling breech — one or both of the baby’s feet are hanging below its bottom, so the foot or feet are coming first
What does it mean for my baby?
While your baby is still in the womb, it is just as safe for them to be in a breech position as it is for them to be head-down. There are no long-term effects on children who were in a breech position during pregnancy. The birth process, however, is often more challenging when babies are still breech at the start of labour.
There are no long-term effects on children who were in a breech position during pregnancy. The birth process, however, is often more challenging when babies are still breech at the start of labour.
Why do some babies remain in a breech position?
Often it is unclear why a baby remains in a breech position. Some of the common reasons include:
- too much or too little amniotic fluid around the baby
- the length of the umbilical cord
- multiple pregnancy — for example, often one twin will be in a head-down position and the other in a breech position
- uterine fibroids
- an irregular size or shape of the mother’s uterus
Can my baby still turn after 36 weeks?
Some breech babies turn themselves naturally in the last month of pregnancy. If this is your first baby and they are breech at 36 weeks, the chance of the baby turning itself naturally before you go into labour is about 1 in 8. If you’ve already had a baby and this one is breech at 36 weeks, the chance of them turning naturally is about 1 in 3.
If your baby is in a breech position at 36 weeks, your doctor or midwife might suggest you think about an ECV, or external cephalic version, after 37 weeks. This will increase your chances of your baby turning to a head-down position. However, ECV is not suitable for everyone, so it’s important to discuss this option with your doctor or midwife.
Some people think that you might be able to encourage your baby to turn by holding yourself in certain positions, such as kneeling with your bottom in the air and your head and shoulders flat to the ground. Other options you might hear include acupuncture, a Chinese herb called moxibustion and chiropractic treatment. There is no good evidence that these work.
Talk to your doctor or midwife before trying any techniques to be sure they do not harm you or your baby.
What are my options if my baby is breech?
If you don’t have an ECV, or if you have it but it doesn’t work, then your options are to have an elective caesarean birth or to have a vaginal birth. Things may be different if you have had a caesarean section before — in this case, if you wish to explore the option of vaginal breech birth, you will need to discuss this with your obstetrician. You may be advised to have a caesarean section again.
Things may be different if you have had a caesarean section before — in this case, if you wish to explore the option of vaginal breech birth, you will need to discuss this with your obstetrician. You may be advised to have a caesarean section again.
Often, women are encouraged to have a caesarean birth if their baby is breech because it might be safer for the baby. But a vaginal birth is still an option in the right circumstances, such as:
- no other issues that would suggest a vaginal birth is unsafe, such as placenta praevia
- you are giving birth in facilities that can handle an emergency caesarean, if necessary
- you have an obstetrician or midwife who is skilled in vaginal breech births
What is involved in a vaginal breech birth?
When babies are in a cephalic (head-down position) ready for birth, the birth process is more straightforward because the crown of the baby’s head is born first. The head is the largest part of the baby’s body, so it makes way for the rest of the body to follow.
The birth process might be more challenging if your baby is breech. When a baby is born bottom first, the baby’s body is born before the largest part, its head. Often this doesn’t cause a problem. But there is a chance that the head, or the head and arms, may not follow easily, once the body is born. In this case, it is important that a midwife or obstetrician with skills and experience in breech births is present to assist your baby to be born.
Upright maternal positions, such as kneeling or a hands and knees position, are recommended when you give birth to a breech baby. The obstetrician or midwife will be standing by, observing closely, with a ‘hands off‘ approach, unless your baby's progress during the birthing process slows down. In such cases, there are a number of techniques that can be used to assist your breech baby to complete the birth vaginally, or it may be necessary to proceed to an emergency caesarean section.
The progress of your labour will be monitored closely. If there is any delay in the descent of your baby, a caesarean section might be recommended. This is because a delay in the baby’s descent inside may be an indication that the birth process could also be delayed, which is more risky for your baby.
If there is any delay in the descent of your baby, a caesarean section might be recommended. This is because a delay in the baby’s descent inside may be an indication that the birth process could also be delayed, which is more risky for your baby.
In many settings where vaginal breech births are offered, it is preferred that your baby is monitored continuously with a cardiotocograph (CTG). If available, you may prefer a cordless, waterproof CTG so you can remain upright and mobile, and so you can use the bath or shower for pain management during labour.
What should I ask my doctor or midwife?
It is worth discussing whether you might benefit from an ECV, because if this is successful, you can go on to try a vaginal birth.
You should also ask if:
- a vaginal birth is safe for the type of breech position your baby is in
- the health service you are planning to use can manage a breech vaginal birth
- your doctor or midwife has training and experience in managing a breech vaginal birth
Do all hospitals offer vaginal breech birth?
Not all hospitals have obstetricians and midwives on staff with the skills and experience in assisting women with a vaginal breech birth. If it is important to you, and your doctor or midwife can’t offer you a vaginal breech birth, you can ask to be referred to another health service.
If it is important to you, and your doctor or midwife can’t offer you a vaginal breech birth, you can ask to be referred to another health service.
What if I am planning a home birth and my baby is breech?
If you are planning a home birth, discuss options for your care with your midwife. The Australian College of Midwives and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists recommend that you should be referred to an obstetrician if your baby is breech at the start of labour. This usually means being transferred to give birth in a hospital. In most cases, your midwife will be able to continue supporting you during your birth in hospital and also continue postnatal care at home after your baby is born.
Sources:
The Society of Obstetricians and Gynaecologists Canada (Breech childbirth), BioMed Central (Does moxibustion work? An overview of systematic reviews (BMC Research Notes 20103:284)), Department of Health (Clinical practice guidelines: Pregnancy care), Cochrane Library (Planned caesarean section for term breech delivery), NSW Health (Breech baby at term), SA Department for Health and Ageing (Perinatal practice guideline: Breech presentation), Australian College of Midwives (Transfer from planned birth at home guidelines), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Breech Presentation at the End of your Pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2020
Back To Top
Related pages
- External cephalic version (ECV)
Need more information?
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website
Malpresentation
Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Read more on Pregnancy, Birth & Baby website
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
External cephalic version (ECV)
ECV is a procedure to try to move your baby if they are in a breech position to the head-down position.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 28
You are now in the third trimester and you'll probably be feeling many of the common discomforts of pregnancy, like a sore back, swelling, heartburn or cramps.
Read more on Pregnancy, Birth & Baby website
Glossary of pregnancy and labour
Glossary of common terms and abbreviations used in pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - pelvis
The pelvis helps carry your growing baby and is especially tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 32
Your baby doesn't have a lot of room, but they will still be moving. The extra weight might cause you some back and pelvic pain which can make it difficult for you to move around.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 39
Your baby's weight gain should slow down since they are now ready to be born. You might soon start to notice the early signs of labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
When Does A Baby Turn Its Head Down?
Home » Pregnancy Concerns » When will my baby turn head down?
As you progress through pregnancy the baby’s position becomes a more important consideration. At about 30 weeks about 25% of babies are not in a “cephalic” (head down) position. It is normal for the baby to turn head down even by about 34 weeks. So don’t worry!
It is normal for the baby to turn head down even by about 34 weeks. So don’t worry!
It is a concern if the baby is not head down at 36 weeks and beyond. This does not mean that spontaneous turning will not happen. Indeed occasionally a baby can turn even as late as the onset of labour.
Why are most babies head down?
A singleton baby’s position is related to the size of your baby and the size and shape of your uterus.
In early pregnancy, there is plenty of room for your baby in the uterus and so there is no reason why your baby should be head down. As the pregnancy becomes more advanced there is less room for your baby to move in your uterus and so your baby wants to adopt a more comfortable position. As the buttock area is greater, a more comfortable position is for the buttock area to be at the top (“fundus”) of the uterus and the head to be towards the pelvis.
If your uterus has been overstretched because of previous pregnancies, if you have excessive amniotic fluid (“liquor”) in your uterus or your baby is unusually small then your baby may be quite mobile in advanced pregnancy.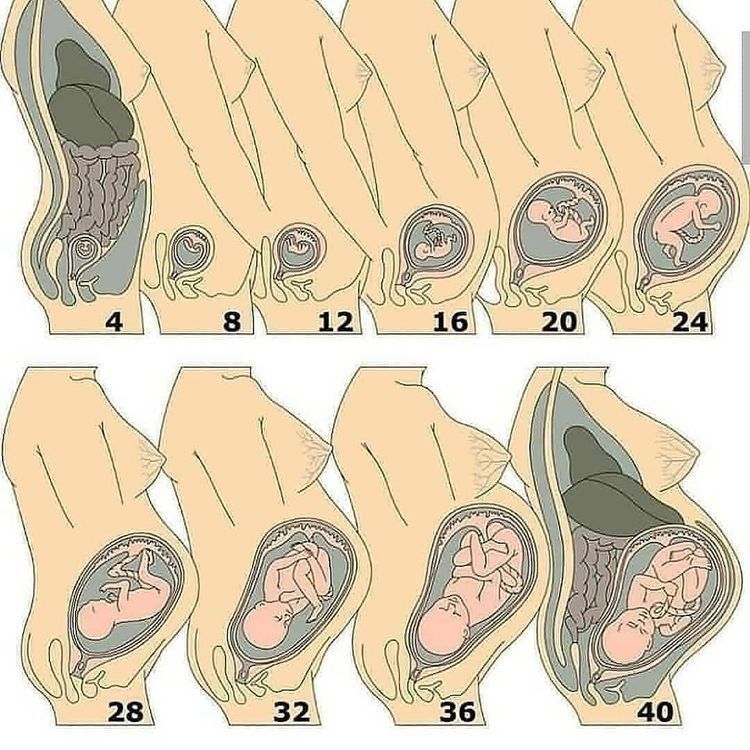 We refer to this an “unstable lie”.
We refer to this an “unstable lie”.
If you have an abnormality of the uterus such as a fibroid protruding into your uterine cavity or you have a uterine shape abnormality, or you have an unusual shape to your pelvis then your baby can be prevented for adopting a head down position. If you have twins often one is not head down and sometimes both.
What can be done about it?
There is no need for concern until more advanced pregnancy. The reasons need to be considered as to why your baby is not in a head down position. I will monitor you each visit with an ultrasound scan so we can monitor your baby’s position.
If your baby has been breech and turns to head down spontaneously, then this is a very encouraging sign. It usually then stays head down. If your baby remains breech toward the end of the pregnancy, then there is usually a good reason. A procedure (“external cephalic version“) to try to turn your baby around to head down can be done, but only after a careful ultrasound scan and giving you a medication to relax the uterus.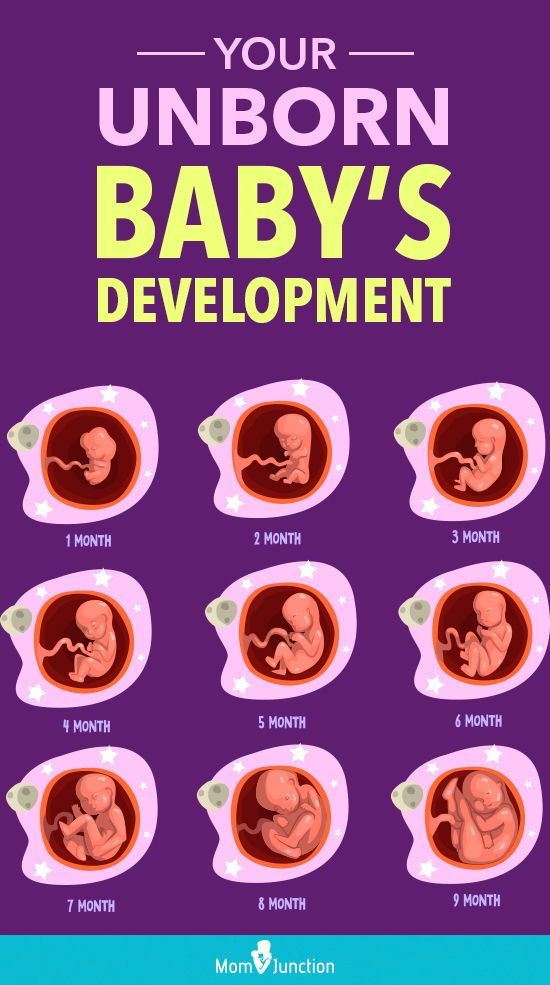 External cephalic version will be done very carefully and with close monitoring on the labour ward/birth unit of your baby and you with the procedure. This is because studies have shown the external cephalic version procedure has risk to your baby’s wellbeing because it can cause an umbilical cord accident, placental separation and preterm labour. Also, it is generally considered that the babies who turn easily with external cephalic version procedures would have turned anyway and the so the procedure was not necessary.
External cephalic version will be done very carefully and with close monitoring on the labour ward/birth unit of your baby and you with the procedure. This is because studies have shown the external cephalic version procedure has risk to your baby’s wellbeing because it can cause an umbilical cord accident, placental separation and preterm labour. Also, it is generally considered that the babies who turn easily with external cephalic version procedures would have turned anyway and the so the procedure was not necessary.
If the lie is unstable and you go into labour or your waters go then you must attend the labour ward/birth unit immediately so your baby’s position and presentation can be checked and umbilical cord presentation/prolapse can be excluded. Sometimes with an unstable lie, a careful stabilising induction is a safer option than waiting for spontaneous labour onset.
Also see my video titled ‘When will my baby turn head down?‘
- Monday all day 9.
 00am to 4.30pm
00am to 4.30pm - Tuesday all day 9.00am to 4.30pm
- Wednesday all day 9.00am to 4.30pm
- Thursday morning 9.00am to 12.30pm
- Thursday alternate afternoons 2.00pm to 4.30pm
- Friday alternate mornings 9.00am to 1.00pm
- Friday afternoon 2.00pm to 4.30pm
- Saturday mornings 9.30am to 12.00 midday*
*Saturday morning appointments are not available for initial antenatal visit.
At what week of pregnancy should the baby turn head down | Mamovediya
Expectant mothers are in constant contact with their tummy, listen to every movement. The slightest signals and movements are important: both in order to be calmer that the child is active in the stomach, and to find out if he has turned his head down.
But is there an easy way to tell if a baby's body is upside down and at what gestational age it should turn over?
In the vast majority of cases, in the last weeks of pregnancy, the fetus turns, and is in the most suitable position for vaginal delivery - cephalic presentation, i.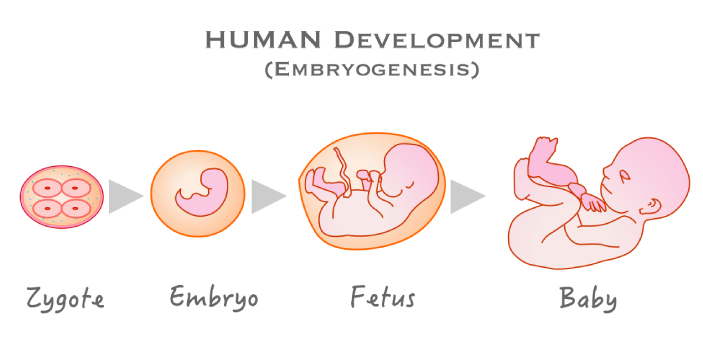 e. head down the pelvis, and buttocks and legs up. However, in 5-10% of cases, the opposite happens: the baby's head remains at the top, and the buttocks at the bottom of the mother's abdomen. In this case, we are talking about the pelvic (buttock) presentation of the fetus.
e. head down the pelvis, and buttocks and legs up. However, in 5-10% of cases, the opposite happens: the baby's head remains at the top, and the buttocks at the bottom of the mother's abdomen. In this case, we are talking about the pelvic (buttock) presentation of the fetus.
How to understand the position of the fetus?
- Finding the position of the fetus on ultrasound
The surest way to understand if the baby turned his head towards the mother's pelvis is, of course, ultrasound. It occurs during the third trimester, approximately between the 30th and 34th weeks of pregnancy, when the fetus assumes a position in which it will remain until delivery. But this is not always the case: sometimes it happens that the baby has a lot of room for movement in the woman's stomach, or the fetus itself is small and very active, and remains active until birth. This is what worries many mothers that the baby may not turn into the right position before birth. nine0003
nine0003
- Head position
In the absence of ultrasound, you can understand how the child is positioned by feeling his stomach. The baby's head is a rather hard rounded protrusion: by its location, you can understand what is happening in the stomach. If a woman feels pain, heartburn, excessive pressure on the diaphragm , then the child's head is at the top, and if pressure on the bladder , then the child is in head presentation. Very rarely, in the last weeks of pregnancy, the baby rolls over into a horizontal position, that is, when the head and pelvis are on the sides of the mother's abdomen, and if it happens, then this is usually the transitional position of the fetus! nine0003
- Understanding the position of the fetus from kicks
The child's legs are not small, especially if there is little time left before the birth. And he knows how to use them perfectly: any woman who has been pregnant remembers well the pain in her stomach from kicks! If you feel or see a small, raised bump in your upper abdomen, it's almost certainly a leg. If there are two, the chances increase. Of course, it is difficult to reliably understand whether the child has accepted the head presentation by the location of his legs, so we repeat once again that the only sure way is ultrasound. nine0003
If there are two, the chances increase. Of course, it is difficult to reliably understand whether the child has accepted the head presentation by the location of his legs, so we repeat once again that the only sure way is ultrasound. nine0003
Why doesn't the baby roll over?
From the thirtieth week of pregnancy, the period begins when the baby usually assumes the final position before delivery, and turns down, head towards the pelvis. His knees are bent, his arms and legs are crossed, and his chin rests on his chest.
In 10% of cases, the baby does not roll over and remains in the breech position until delivery. Why is this happening? Some categories of women are more prone to this condition: pregnancy with twins, mothers who have a narrow pelvis, women with placenta previa. nine0051 There are many reasons why a baby remains in a breech position at the time of delivery. The most famous of them:
- polyhydramnios - there is a high mobility of the child, because of which he does not take the right position on time;
- oligohydramnios - limited ability of a child to move, which prevents him from turning his head down;
- pregnancy with twins - in this case, the babies interfere with each other, it is very difficult for them to move due to lack of space; and in principle, in multiple pregnancies, "traditional" cephalic presentation is quite rare throughout pregnancy; nine0016
- umbilical cord entanglement - it happens that a very active baby, when turning over in the mother's womb, can wrap the umbilical cord around himself so much that it becomes completely impossible for him to take the correct position for childbirth;
- uterine pathology - if a woman suffers from certain diseases of the uterus (for example, fibroids), this can directly affect the position of the fetus.
In some cases, in the presence of the problems described above, the breech presentation of the fetus may threaten the following complications:
- premature birth;
- hypoxia - if the child in the breech presentation has clamped the umbilical cord;
- Difficult delivery, risk of injury to both mother and child.
Can a baby roll over at 38 weeks?
Until what week does the baby usually turn upside down? Theoretically, the baby can roll over at any time, in reality this happens before the 38th week. Variables on which this depends are the size of the fetus, the length of the umbilical cord, and, presumably, the amount of amniotic fluid. nine0003
It is estimated that babies in breech position between 33 and 36 weeks of pregnancy are only 9%: some remain in this position until delivery, although among full-term babies they are only 3%. It is now known that caesarean section is safer than vaginal breech delivery , so if your baby is still in this position at 37 weeks, your doctor may suggest operative delivery. But, first, it is recommended to try to turn the baby down with some external maneuvers, which succeed in 40% of cases in mothers with a first child and in 60% of cases in women who have already given birth. nine0003
But, first, it is recommended to try to turn the baby down with some external maneuvers, which succeed in 40% of cases in mothers with a first child and in 60% of cases in women who have already given birth. nine0003
What does the abdomen look like in breech presentation?
By what signs can a woman understand that the baby's head has not yet sunk into the pelvis and the fetus is still in breech presentation?
A gynecologist diagnoses a breech presentation of the fetus at the appointment. The baby's heartbeat is heard at or above the woman's navel. To confirm, the doctor may examine the abdomen with his hands. With a breech presentation, the gynecologist will feel the child's buttocks. If the baby rests on the pelvis with the legs, the doctor can feel the heels or fingers. nine0003
Also, an indirect sign of the breech presentation of the fetus at the end of pregnancy is the stomach, or rather, the fact that it has fallen or not. With a breech presentation, the abdomen practically does not change its position, and does not fall down, as happens with a head presentation. But, again, we insist that the exact position of the child can be found on ultrasound.
But, again, we insist that the exact position of the child can be found on ultrasound.
How can you tell if a baby has turned head down?
There are cases when women felt the so-called "tumbling", that is, a movement that allows the child to change position, moving from the gluteal position to the head (or vice versa). At the same time, the other women shrug their shoulders and say they didn't notice something was happening. nine0051 In addition to somersaults, to understand what position the baby is in, hiccups of the child will help us . Hiccups appear as a rhythmic movement that the woman feels in the upper abdomen, and in this particular case, it can be concluded that the child has taken a breech presentation. When the baby is in the head presentation, and his head is turned to the birth canal, hiccups are felt in the pelvic area, closer to the groin.
Another signal to understand what is going on is the thrusts: if they are directed to the stomach, this is a sign that the child has turned upside down, otherwise the pressure was felt closer to the bladder. nine0051 If the child is still not in a favorable position for birth, the doctor can perform "obstetric coup" , although the child often returns to the previous position after such manipulations.
nine0051 If the child is still not in a favorable position for birth, the doctor can perform "obstetric coup" , although the child often returns to the previous position after such manipulations.
There are also special exercises by which a woman can help the child turn his head towards the pelvis on his own. But keep in mind that such exercises should be performed under the supervision of a doctor , and in no case should you self-medicate, this can lead to premature birth or other tragic results. nine0003
Most importantly, stay calm. If the baby does not turn head down after 38 weeks, the doctor will suggest you have a caesarean section. Consult a doctor you trust, natural childbirth with a breech presentation is also possible if there is no entanglement of the umbilical cord, and the fetus itself is not very large.
At what week should the baby turn head down?
At what week should the baby turn head down?
Closer to the expected date of delivery, the baby turns his head towards the pelvis. This usually occurs towards the end of the third trimester of pregnancy and is called cephalic presentation. nine0003
This usually occurs towards the end of the third trimester of pregnancy and is called cephalic presentation. nine0003
This position is a sign that the baby is almost ready to be born.
When does the baby turn head down?
Between 27 and 40 weeks, the doctor performs an examination to determine the position of the fetus in the uterus. It is then that his previa will be revealed. From the presentation - that is, the position of the child depends on how the birth will proceed.
Much fewer surprises await a woman if the child occupies the classic position in the uterus - upside down. The head position of the fetus is the most favorable for childbirth, since in this case the risk of complications for the baby is minimal. However, do not be afraid if the position in the uterus of your baby is different: pelvic or transverse. Such a doctor's verdict is also not critical, it's just that your birth will be different.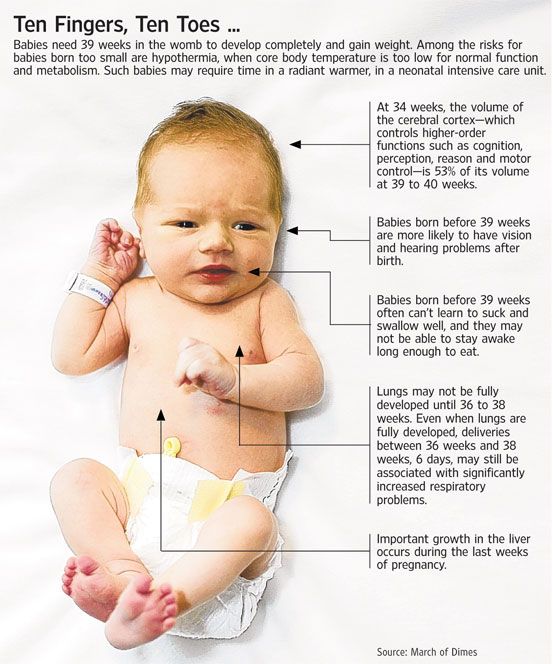 And they will pass under the close attention of doctors. nine0003
And they will pass under the close attention of doctors. nine0003
Fetal position
Head position of the fetus (fetus head down): detected at 7 months of pregnancy when the doctor palpates the abdomen of the future woman in labor. This will also be confirmed by the results of examination through the vagina and ultrasound.
Breech presentation of the fetus (the child either “sits” on the ass, raising the legs up, or “squats”, lowering them down, or pulls the legs under him) is recognized from the 32nd week of pregnancy: in the upper part of the uterus, the doctor gropes the firm head of the child, and at the bottom - the soft ass. nine0003
Transverse presentation of the fetus (the fetus lies across) is determined from the 20th week of pregnancy. Having probed the belly of the expectant mother, the doctor will “discover” the head and buttocks of the child on the sides.
There is no specific week or day in which women can expect their child to be in the required position. In some cases, the baby turns over already at the onset of labor or a few hours before the onset. For other women, this happens a few days or weeks before the onset of labor. nine0003
In some cases, the baby turns over already at the onset of labor or a few hours before the onset. For other women, this happens a few days or weeks before the onset of labor. nine0003
A cephalic reversal closer to the day of delivery usually occurs in women who already have children. This is because their body is already familiar with labor, so it may take less time for the pelvis to adjust to the process.
Women who are pregnant for the first time may find that the baby rolls over a few days or weeks before delivery. This may be because their pelvic muscles take longer to adjust for childbirth. nine0003
If a woman thinks her baby is upside down, she should talk to her doctor. The doctor can check the position of the baby, which will help him predict when labor will begin.
What does it look like?
Some women may feel the roll of the baby as a sudden, palpable movement. Others may not feel anything at all and miss this moment.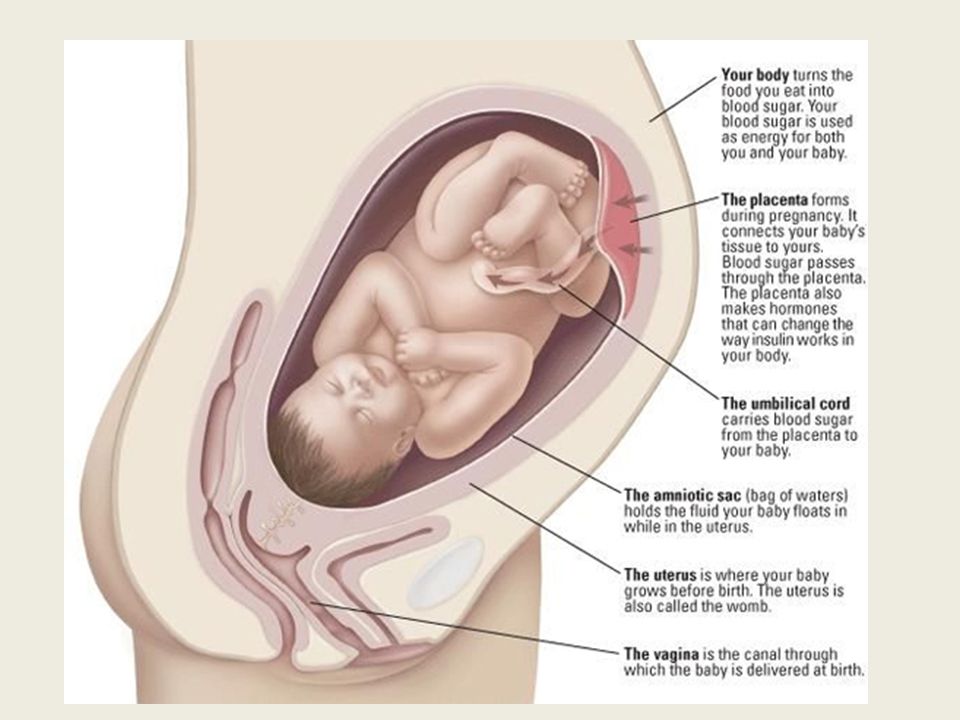
Some women may notice that their stomach seems to be lighter after the baby rolls over. Perhaps this is due to the fact that the child has moved into the pelvic area, leaving more free space in the abdomen. This feeling of free space in the stomach is the reason why turning over is also called relief. However, for some, this relief can be frightening. Sometimes, as the baby moves down, women feel like they have a bowling ball between their legs. Every woman has her own unique experience of turning a baby. nine0003
Nine signs that the baby is head down Pregnancy
When the baby rolls over, the belly may look like it has dropped a little.
Pressing pain in the pelvic region . As the baby moves into the pelvis, the pressure in that area may increase. This can cause a woman to feel like she is rocking from side to side while walking. nine0003
Pelvic pain outbreaks . When a baby rolls over, some women may experience flare-ups of pelvic pain. This may be due to the fact that the baby's head is pressed against the ligaments in the pelvis.
When a baby rolls over, some women may experience flare-ups of pelvic pain. This may be due to the fact that the baby's head is pressed against the ligaments in the pelvis.
Easier breathing. When the baby rolls over and lowers into the pelvis, there is less pressure on the diaphragm. This can make breathing easier.
Hemorrhoids. After the baby is in the prenatal position, the head may put pressure on the nerves in the pelvis and rectum. This pressure can cause hemorrhoids. nine0003
More allocations. Moving the baby towards the pelvis increases pressure on the cervix. This causes her to secrete mucus that sits at the top of her cervix for the rest of her pregnancy. This is to ensure that bacteria do not enter the uterus. After the baby rolls over, mucus may come out of the vagina as a jelly-like discharge.
Frequent need to urinate. As the baby moves down into the pelvis, the head may put pressure on the bladder. This can cause a woman to urinate frequently. nine0003
This can cause a woman to urinate frequently. nine0003
Back pain. The baby's cephalic presentation can put extra pressure on the muscles in the lower back. This can cause back pain.
Feeling of hunger. Proper prenatal positioning of the baby can relieve pressure on the stomach. It can relieve heartburn and increase hunger.
The role of intrauterine position in childbirth
If a woman thinks her baby has turned upside down, she should see a doctor. The doctor can determine what position the child is in using a special scale. Some doctors use a three-point scale, while others use a five-point scale. nine0003
The five-point scale is more traditional and more widely used. A 2015 scientific article describes it as a system that divides the pelvis above and below the ischial spines into five segments. The ischial spines are located on the pelvis. When the baby is ready to be born, his head is level with them.
When the baby is ready to be born, his head is level with them.
The five-point scale is measured from -5 to +5. Each step forward on the scale means the baby is one centimeter closer to birth. Before the baby rolls over, the woman can be at point -5. As the baby rolls over (and moves deeper into the pelvis), the woman may be at zero point. When the baby descends into the vagina, the woman may be at +5. nine0003
According to a 2014 study, 95 percent of women are at or below the zero point during full dilation. To assess what stage a woman is in, the doctor examines the woman's vagina and tries to feel for the baby's head.
How can I help my baby get into the correct position before birth?
If the due date is close and the baby has not yet rolled over, the woman can try certain actions to get the baby into position. These include:
- Hiking
- Childbirth ball seat
- Squats
- Pelvic tilt
These activities help to open the hips and stretch the pelvic muscles.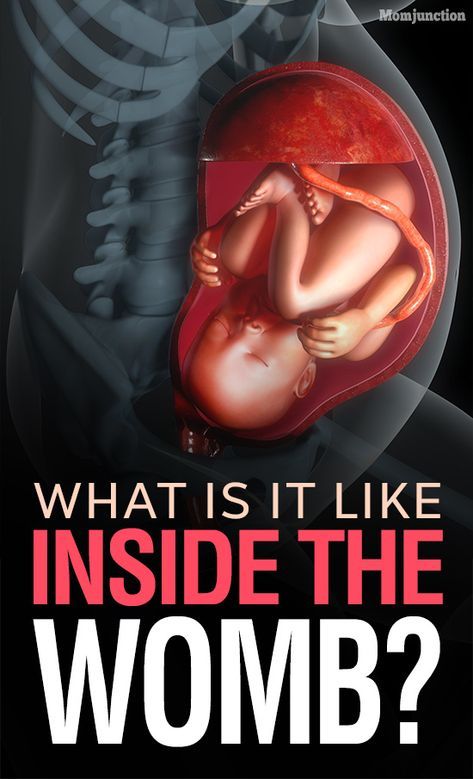 This may encourage the baby to move into the pelvis.
This may encourage the baby to move into the pelvis.
When should I see a doctor?
It is normal to feel pain in the pelvic area after the baby is in the prenatal position. However, some types of pelvic pain may need to be evaluated. Talk to your doctor if pelvic pain is constant or regular. Or if it's accompanied by:
- Bleeding
- Fluid Loss
- Fever
Turning the baby usually occurs towards the end of pregnancy. This can happen both immediately at the onset of labor, and a few hours, and sometimes weeks before that. In women who are pregnant with their first child, this process is likely to occur a few weeks before delivery.
This maneuver may feel like a sudden, jerky movement, however, some women do not even notice when it occurs. The head presentation of the baby can make breathing easier and increase appetite. This happens because there is space in the abdomen and pressure on the organs is reduced.