Blood tests in 8th month of pregnancy
Tests You Might Receive in 3rd Trimester of Pregnancy
Written by WebMD Editorial Contributors
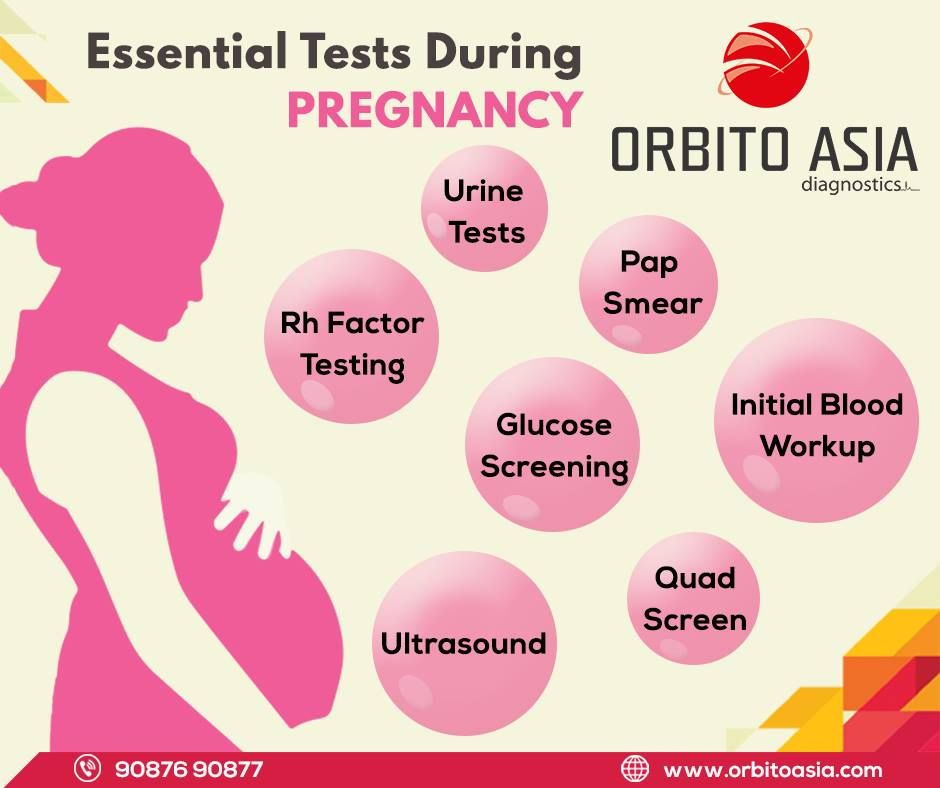
These tests are common in the third trimester of pregnancy:
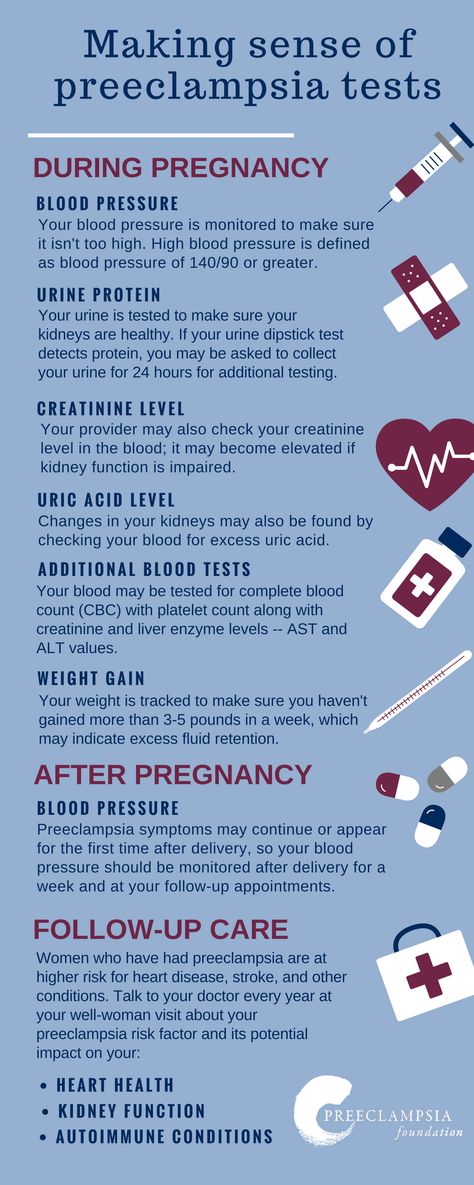
Blood and urine tests: Your doctor will continue to check your urine for protein and sugar and any signs of infection, keeping a close eye for signs of preeclampsia, a complication that is most common in the last weeks of pregnancy. You may have blood tests again for anemia.
Other measurements: Weight, blood pressure, and fundal height measurements also continue. Your baby's heartbeats are loud and clear!
Pelvic exams: In the last few weeks of pregnancy, your doctor will start doing pelvic exams again. This is to see if the cervix has started the ripening process for birth. Ripening is the softening, thinning, and opening (dilating) of the cervix.
These changes can happen slowly or quickly during the weeks, days, or hours before birth. So it's not uncommon to dilate a few centimeters a few weeks before your due date and then to stop dilating. This process is somewhat unpredictable.
Group B streptococcus screening: Vaginal and rectal swabs are taken at 35 to 37 weeks of pregnancy to detect group B strep bacteria. Although group B strep can be present in up to 30% of all healthy women, it's the leading cause of life-threatening infections in newborns and can also cause intellectual disability, impaired vision, and hearing loss. Women who test positive are treated with antibiotics during delivery to protect the baby from contracting the infection at birth. As an alternative, your physician or midwife may choose not to test for strep but to treat you in labor if certain risk factors develop.
Electronic fetal heart monitoring: Electronic fetal heart monitoring is done during pregnancy, labor, and delivery to monitor the heart rate of the fetus. The fetal heart rate can indicate whether the fetus is doing well or is in trouble and can be done any time after 20 weeks.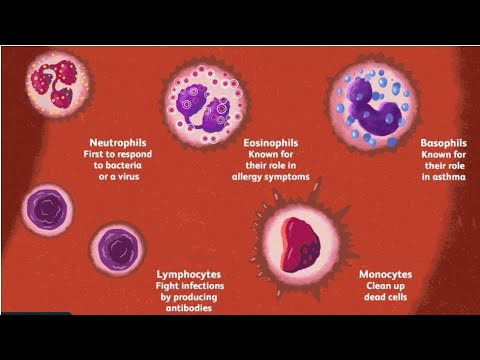
Nonstress test: Done weekly in many high-risk pregnancies, such as in cases where a women is carrying more than one fetus, or has diabetes or high blood pressure, this test involves using a fetal monitor strapped across the mother's abdomen to measure the baby's heart rate as it moves. It's also used for monitoring overdue babies.
Contraction stress test: Also done in high-risk pregnancies, a fetal monitor measures the baby's heart rate in response to contractions stimulated either by oxytocin (Pitocin) or nipple stimulation. Doctors use the measurements to predict how well the baby will cope with the stress of labor.
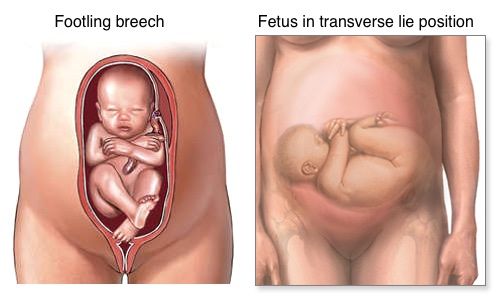
Ultrasound: Most pregnant women have just one or perhaps two ultrasounds. If you're having twins, you'll have this test more often, perhaps right up until birth, to check the position and growth of your babies. When needed, doctors can combine non-stress tests with ultrasound. This allows your doctor to check the babies' breathing motions, body movements, and muscle tone as well as the amount of amniotic fluid.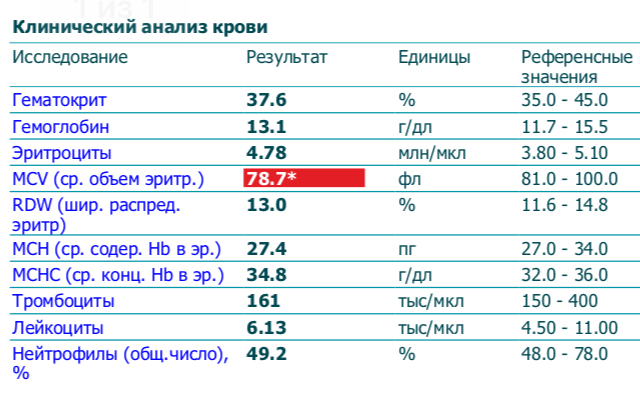
Biophysical profile: Can be done with just an ultrasound or with a combination of a nonstress test and an ultrasound.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Prenatal Tests: Third Trimester (for Parents)
Reviewed by: Thinh Phu Nguyen, MD
Fetal Medicine at Nemours Children's Health
en español Exámenes prenatales: Tercer trimestre
Throughout your pregnancy, you'll want to know how your baby is growing. Prenatal tests can offer valuable information about your health and the health of your growing child.
If your doctor recommends a screening or test, be sure to learn about the risks and benefits. Most parents find that prenatal tests offer them peace of mind while helping to prepare them for their baby's arrival. But it's your choice to accept or decline a test.
But it's your choice to accept or decline a test.
Routine Screenings & Other Tests
Your first visit to the obstetrician should have included a full physical, urine (pee) test, and blood test to check for things like:
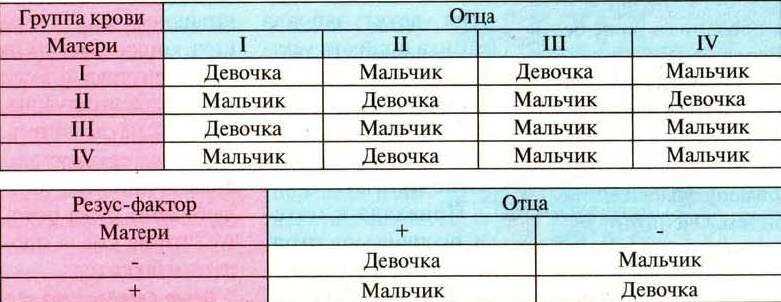
- your blood type and Rh factor. If your blood is Rh negative and your partner's is Rh positive, you may develop antibodies that prove dangerous to your fetus. This can be prevented through an injection given around the 28th week of pregnancy.
- anemia, a low red blood cell count
- hepatitis B, syphilis, and HIV
- immunity to German measles (rubella) and chickenpox (varicella)
- cystic fibrosis and spinal muscular atrophy. Health care providers now routinely offer to screen for these disorders even when there's no family history.
You can expect to get your urine tested and your weight and blood pressure checked at every (or almost every) visit until you deliver. These tests can identify conditions such as gestational diabetes and preeclampsia (dangerously high blood pressure).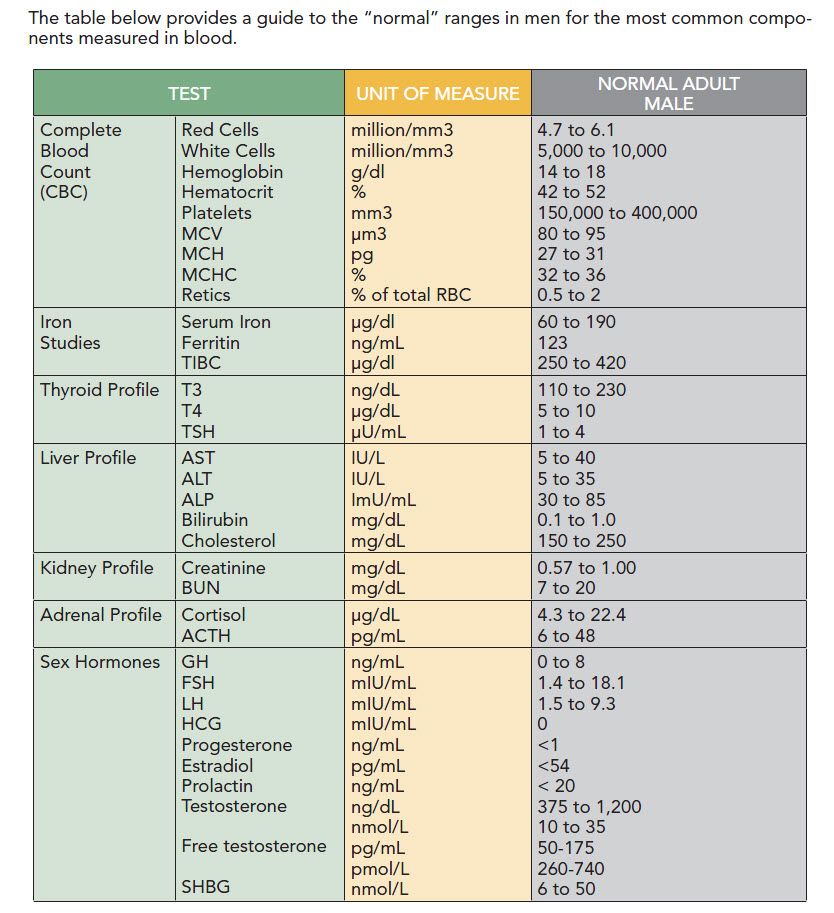
Throughout your third trimester, you'll be offered more tests depending on your age, health, family medical history, and other things. These can include:
- Ultrasound: An ultrasound is a safe and painless test that uses sound waves to make images that show the baby's shape and position in the uterus. Third-trimester ultrasounds can examine the placenta, and sometimes are part of a test called a biophysical profile (BPP) to see whether the baby is getting enough oxygen. Women with high-risk pregnancies may have multiple ultrasounds in their third trimester.
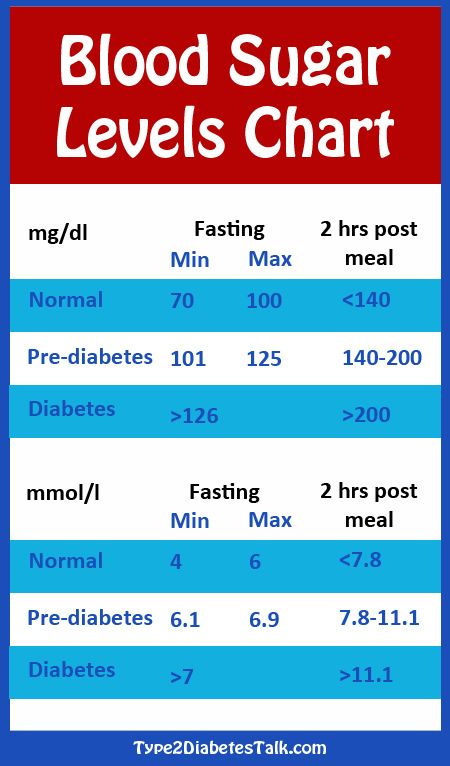
- Glucose screening: This test checks for gestational diabetes, a short-term form of diabetes that develops in some women during pregnancy and can cause health problems for the baby, especially if it is not diagnosed or treated. You'll drink a sugary liquid, then have a blood test an hour later to check glucose levels.
- Group B strep test: Between your 35th and 37th weeks of pregnancy, the doctor will check you for group B streptococcus (GBS) infection.
 GBS bacteria are found naturally in the vaginas of many women but can cause serious infections in newborns. This test involves swabbing the vagina and rectum. A woman whose test comes back positive must go to the hospital as soon as labor begins so that intravenous (IV) antibiotics can be started to help protect the baby from becoming infected.
GBS bacteria are found naturally in the vaginas of many women but can cause serious infections in newborns. This test involves swabbing the vagina and rectum. A woman whose test comes back positive must go to the hospital as soon as labor begins so that intravenous (IV) antibiotics can be started to help protect the baby from becoming infected. - Nonstress test: A nonstress test (NST) is usually done when a health care provider wants to check on the health of the fetus, such as in a high-risk pregnancy or when the due date has passed. The test checks to see if the baby responds normally to stimulation and is getting enough oxygen. A baby that doesn't respond isn't necessarily in danger, but more testing might be needed.
- Contraction stress test: This test stimulates the uterus with pitocin, a synthetic form of oxytocin (a hormone secreted during childbirth), to determine the effect of contractions on fetal heart rate. It may be recommended when an earlier test indicated a problem and can see whether the baby's heart rate is stable during contractions.

Remember that tests are offered to you — it's your choice whether to have them.
To decide which tests are right for you, talk with your health care provider about why a test is recommended, its risks and benefits, and what the results can — and can't — tell you.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
Citizens | Ministry of Health of the Kaliningrad Region
| Gestational age | Analyzes | Events (registration, medical examinations, doctor visit schedule) |
| Up to 12 weeks | Early registration in the antenatal clinic nine0020 Taking medications: folic acid throughout the first trimester, no more than 400 mcg / day; potassium iodide 200-250 mcg/day (in the absence of thyroid disease) | |
| At first appearance | An obstetrician-gynecologist collects anamnesis, conducts a general physical examination of the respiratory, circulatory, digestive, urinary system, mammary glands, anthropometry (measurement of height, body weight, determination of body mass index), measurement of the size of the pelvis, examination of the cervix in the mirrors, bimanual vaginal study nine0007 | |
| Not later than 7-10 days after the initial visit to the antenatal clinic | Inspections and consultations: - general practitioner; - a dentist; - an otolaryngologist; - an ophthalmologist; - other medical specialists - according to indications, taking into account concomitant pathology nine0007 | |
| First trimester (up to 13 weeks) (and at first visit) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol. 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. nine0007 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, to the herpes simplex virus (HSV), to cytomegalovirus (CMV), determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of the main blood groups (A, B, 0) and Rh-affiliation. In Rh-negative women: a) examination of the father of the child for group and Rh-affiliation. 7. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 8. Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 9. PCR chlamydial infection, PCR gonococcal infection, PCR mycoplasma infection, PCR trichomoniasis. | Visiting an obstetrician-gynecologist every 3-4 weeks (with the physiological course of pregnancy). nine0007 Electrocardiography (hereinafter - ECG) as prescribed by a general practitioner (cardiologist). Up to 13 weeks of pregnancy are accepted: - folic acid no more than 400 mcg / day; - potassium iodide 200-250 mcg / day (in the absence of thyroid disease) |
| 1 time per month (up to 28 weeks) | Blood test for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) nine0007 | |
| 11-14 weeks | Biochemical screening for serum marker levels: - pregnancy-associated plasma protein A (PAPP-A), - free beta subunit of human chorionic gonadotropin (hereinafter - beta-CG) | In the office of prenatal diagnostics, an ultrasound examination (hereinafter referred to as ultrasound) of the pelvic organs is performed. According to the results of complex prenatal diagnostics, a conclusion of a geneticist is issued. |
| After 14 weeks - once | Culture of midstream urine | To exclude asymptomatic bacteriuria (the presence of bacterial colonies more than 105 in 1 ml of an average portion of urine, determined by a culture method without clinical symptoms) to all pregnant women. nine0008 |
| In the second trimester (14-26 weeks) | General (clinical) analysis of blood and urine. | Visiting an obstetrician-gynecologist every 2-3 weeks (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), uterine tone, palpation of the fetus, auscultation of the fetus with a stethoscope. nine0007 Potassium iodide 200-250 mcg/day |
| 1 time per month (up to 28 weeks) | Blood for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 16-18 weeks | Blood test for estriol, alpha-fetoprotein, beta-hCG | Only at late turnout unless biochemical screening for serum marker levels at 11-14 weeks nine0007 |
| 18-21 weeks | The second screening ultrasound of the fetus is performed in the antenatal clinic | |
| In the third trimester (27-40 weeks) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol). nine0007 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. nine0007 7. | A visit to an obstetrician-gynecologist every 2 weeks, after 36 weeks - weekly (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, VDM, uterine tone, fetal palpation, auscultation of the fetus with a stethoscope. nine0007 Potassium iodide 200-250 mcg/day |
| 24-28 weeks | Oral glucose tolerance test (OGTT) | |
| 28-30weeks | In Rh-negative women with Rh-positive blood of the child's father and the absence of Rh antibodies in the mother's blood | Administration of human immunoglobulin antirhesus RHO[D] nine0007 |
| 30 weeks | A certificate of incapacity for work is issued for maternity leave | |
| 30-34 weeks | The third screening ultrasound of the fetus with dopplerometry in the antenatal clinic. - general practitioner; - a dentist. nine0007 | |
| After 32 weeks | At each visit to the doctor of the antenatal clinic, in addition to determining the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), the tone of the uterus, determine the position of the fetus, the presenting part, the doctor auscultates the fetus with a stethoscope. | |
| After 33 weeks | Cardiotocography (hereinafter referred to as CTG) of the fetus is performed nine0007 | |
| Throughout pregnancy | In antenatal clinics there are schools for pregnant women, which are attended by expectant mothers along with fathers. In the process of learning, there is an acquaintance with the changes in the body of a woman during physiological pregnancy, acquaintance with the process of childbirth, the correct behavior in childbirth, the basics of breastfeeding. | |
| Over 37 weeks nine0007 | Hospitalization with the onset of labor. According to indications - planned antenatal hospitalization. | |
| 41 weeks | Planned hospitalization for delivery | |
| No later than 72 hours after delivery | All women with an Rh-negative blood group who gave birth to a child with a positive Rh-belonging, or a child whose Rh-belonging is not possible to determine, regardless of their compatibility according to the AB0 system nine0007 | Re-introduction of human immunoglobulin anti-rhesus RHO[D] |
| postpartum period | 1. Early breastfeeding 2. Recommendations for breastfeeding. 3. Consultation of medical specialists on concomitant extragenital disease (if indicated). 4. Toilet of the external genital organs. nine0007 5. 6. Removal of external non-absorbable sutures (if any) on the 5th day. 7. Early discharge. | |
| Daily postpartum | 1. Examination by an obstetrician-gynecologist; 2. Inspection and palpation of the mammary glands. | |
| 3 days after birth nine0007 | Ultrasound of the pelvic organs | |
| After delivery by caesarean section | 1. Complete blood count, general urinalysis. 2. Biochemistry of blood (according to indications). | Ultrasound of the pelvic organs |
Normal blood count during pregnancy. Hemoglobin, platelets, hematocrit, erythrocytes and leukocytes during pregnancy. Clinical blood test during pregnancy. Hematological changes during pregnancy. nine0001
A normal pregnancy is characterized by significant changes in almost all organs and systems to adapt to the requirements of the fetoplacental complex, including changes in blood tests during pregnancy.
Pregnancy blood test norms: article summary
- Significant hematological changes during pregnancy are physiological anemia, neutrophilia, moderate thrombocytopenia, increased blood clotting factors and decreased fibrinolysis. nine0451
- By 6-12 weeks of gestation, plasma volume increases by approximately 10-15%. The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little.
- Red blood cell count begins to increase at 8-10 weeks of gestation and by the end of pregnancy increases by 20-30% (250-450 ml) of the normal level for non-pregnant women by the end of pregnancy A significant increase in plasma volume relative to the increase in hemoglobin and red blood cell volume leads to moderate decrease in hemoglobin levels (physiological anemia of pregnancy), which is observed in healthy pregnant women. nine0451
- Pregnant women may have a slightly lower platelet count than healthy non-pregnant women.

- The neutrophil count begins to rise in the second month of pregnancy and stabilizes in the second or third trimester, at which time the white blood cell count. The absolute number of lymphocytes does not change.
- The level of some blood clotting factors changes during pregnancy. nine0462
- Increased plasma volume and decreased hematocrit
- Physiological anemia, low hemoglobin
- Elevated white blood cells during pregnancy
- Neutrophilia
- Moderate thrombocytopenia
- Increased procoagulant factors
- Fibrinolysis reduction
- The Centers for Disease Prevention and Control defined anemia as hemoglobin levels less than 110 g/l (hematocrit less than 33%) in the first and third trimesters and less than 105 g/l (hematocrit less than 32%) in the second trimester. nine0451
- WHO defined anemia in pregnancy as a decrease in hemoglobin less than 110 g/l (11 g/dl) or hematocrit less than 6.83 mmol/l or 33%. Severe anemia in pregnancy is determined by a hemoglobin level of less than 70 g/l and needs medical treatment. Very severe anemia is defined as a hemoglobin level of less than 40 g/L and is a medical emergency due to the risk of congestive heart failure.
- Due to hormonal changes during pregnancy, the activity of total protein S antigen, free protein S antigen and protein S is reduced.
- Activated protein C resistance increases in the second and third trimesters. These changes have been identified in first-generation tests using pure blood plasma (i.e., not lacking factor V), but this test is rarely used clinically and is of only historical interest. nine0451
- Fibrinogen and factors II, VII, VIII, X, XII and XIII are increased by 20-200%.
- Von Willebrand factor rises.
- Increased activity of fibrinolysis inhibitors, TAF1, PAI-1 and PAI-2. The level of PAI-1 also increases markedly.
- Levels of antithrombin III, protein C, factor V and factor IX most often remain unchanged or increase slightly.
- Iron deficiency anemia.
- Thrombocytopenia.
- Neonatal alloimmune thrombocytopenia.
- Acquired hemophilia A.
- Venous thrombosis.
- Rh and non-Rh alloimmunization. For diagnosis, an analysis is carried out for Rh antibodies and anti-group antibodies.
- A manifestation of a previously unrecognized coagulation disorder, such as von Willebrand disease, most commonly manifests in women during pregnancy and childbirth.
 For screening for von Willebrand disease, an assay is given to assess platelet aggregation with ristocetin. nine0451
For screening for von Willebrand disease, an assay is given to assess platelet aggregation with ristocetin. nine0451 - Aplastic anemia.
-
ToRCH infections and pregnancy
What are ToRCH infections, what are the dangers of these infections during pregnancy, how and when is the examination performed, how to interpret the results. Perinatal infections account for approximately 2-3% of all congenital fetal anomalies.
-
Pregnancy tests at CIR Laboratories
In our laboratory you can undergo a complete examination upon pregnancy, take tests at any time, and in our clinics you can conclude an agreement on pregnancy management.
-
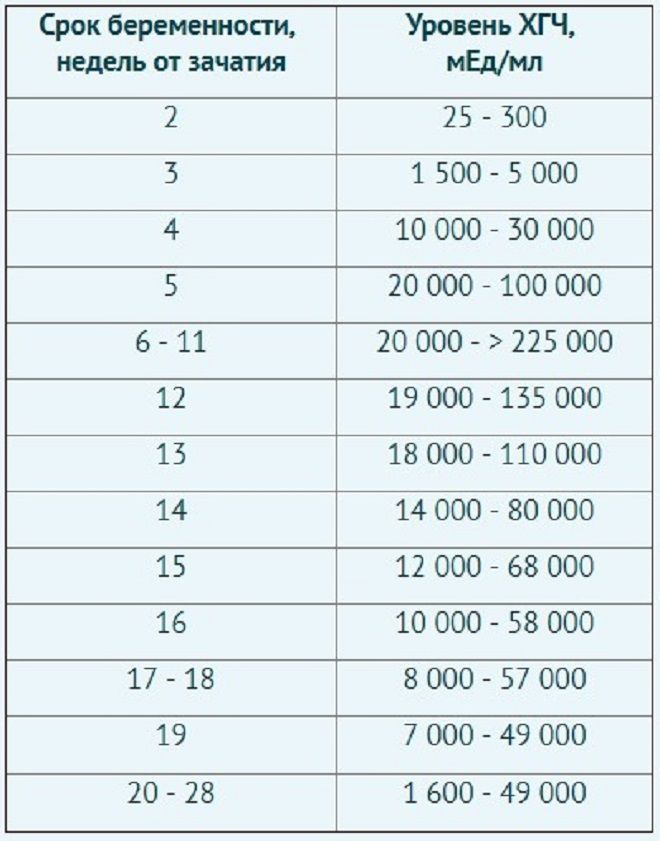
Online hCG calculator during pregnancy
The hCG calculator is used to calculate the increase in hCG (the difference between two tests taken at different times).
The increase in hCG is important for assessing the development of pregnancy.
 Normally, in the early stages of pregnancy, hCG increases by about 2 times every two days. As the hormone levels increase, the rate of increase decreases. nine0007
Normally, in the early stages of pregnancy, hCG increases by about 2 times every two days. As the hormone levels increase, the rate of increase decreases. nine0007 -
False positive pregnancy test or why hCG is positive but not pregnant?
When can a pregnancy test be positive?
-
The norm of hCG during pregnancy. Table of hCG values by week. Elevated HCG. Low HCG. HCG in ectopic pregnancy. hCG during IVF (hCG after replanting, hCG at 14 dpo).
hCG or beta-hCG or total hCG - human chorionic gonadotropin - a hormone produced during pregnancy. HCG is formed by the placenta, which nourishes the fetus after fertilization and implantation (attachment to the wall of the uterus). nine0007
-
Risk assessment of pregnancy complications using prenatal screening
Prenatal screening data allow assessing not only the risks of congenital pathology, but also the risk of other pregnancy complications: intrauterine fetal death, late toxicosis, intrauterine hypoxia, etc.

-
Parvovirus B19 and parvovirus infection: what you need to know when planning and getting pregnant.
What is a parvovirus infection, how is the virus transmitted, who can get sick, what is the danger of the virus during pregnancy, what tests are taken for diagnosis. nine0445
-
Pregnancy planning
Obstetrics differs from other specialties in that during the physiological course of pregnancy and childbirth, in principle, it is not part of medicine (the science of treating diseases), but is part of hygiene (the science of maintaining health). Examination during pregnancy planning.
-
1st and 2nd trimester prenatal screening ("double", "triple" and "quadruple" tests)
Prenatal screening are tests performed on pregnant women to identify risk groups for pregnancy complications.
-
Testosterone during pregnancy. Androgens: their formation and metabolism during normal pregnancy.
This article describes the hematological changes that occur during pregnancy, the most important of which are:
Tests mentioned in the article
How to take blood tests and get a 5% discount? Go to the CIR laboratories online store!
Blood plasma volume
By 6-12 weeks of pregnancy, the volume of blood plasma increases by approximately 10-15%.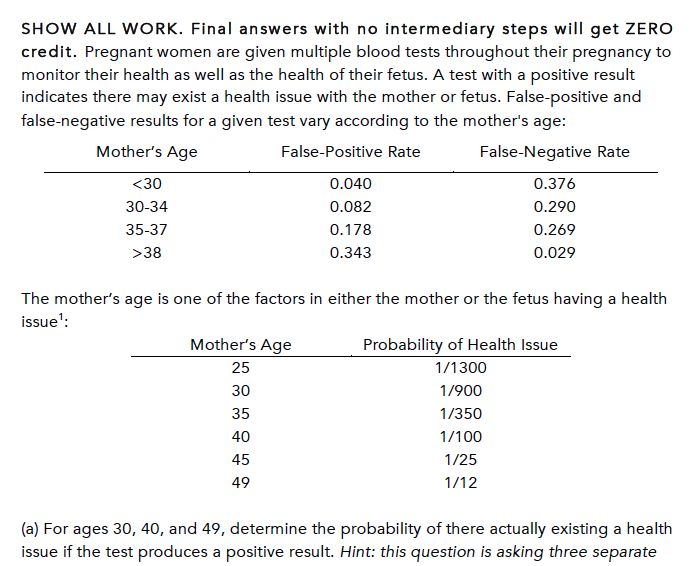 The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little. On average, plasma volume increases by 1100-1600 ml per trimester, and as a result, plasma volume during pregnancy increases to 4700-5200 ml, which is 30 to 50% higher than plasma volume in non-pregnant women. nine0007
The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little. On average, plasma volume increases by 1100-1600 ml per trimester, and as a result, plasma volume during pregnancy increases to 4700-5200 ml, which is 30 to 50% higher than plasma volume in non-pregnant women. nine0007
During pregnancy, plasma renin activity tends to increase, while the level of atrial natriuretic peptide decreases slightly. This suggests that the increase in plasma volume is caused by insufficiency of the vascular system, which leads to systemic vasodilation (dilation of blood vessels throughout the body) and an increase in vascular capacity. Since it is the volume of blood plasma that initially increases, its effect on the renal and atrial receptors leads to opposite effects on the hormonal background (a decrease in plasma renin activity and an increase in natriuretic peptide). This hypothesis is also supported by the observation that an increase in sodium intake does not lead to a further increase in plasma volume. nine0007
nine0007
Plasma volume immediately decreases after delivery, but rises again 2-5 days later, possibly due to increased aldosterone secretion occurring at this time. Plasma volume then gradually decreases again: 3 weeks postpartum, it is still elevated by 10-15% of the normal level for non-pregnant women, but usually returns to normal by 6 weeks postpartum.
RBCs in pregnancy, ESR in pregnancy
RBCs begin to increase at 8-10 weeks of gestation and increase by 20-30% (250-450 ml) of normal non-pregnant levels by the end of pregnancy, especially in women taking drugs iron during pregnancy. Among pregnant women who did not take iron supplements, the number of red blood cells may increase by only 15-20%. The lifespan of red blood cells decreases slightly during a normal pregnancy. nine0007
The level of erythropoietin during normal pregnancy increases by 50% and its change depends on the presence of pregnancy complications. An increase in plasma erythropoietin leads to an increase in the number of red blood cells, which partially provide for the high metabolic oxygen requirements during pregnancy.
In women who do not take iron supplements, the average volume of red blood cells decreases during pregnancy and in the third trimester averages 80-84 fl. However, in healthy pregnant women and in pregnant women with moderate iron deficiency, the average volume of erythrocytes increases by about 4 fl. nine0007
ESR increases during pregnancy, which has no diagnostic value.
Anemia in pregnancy, hemoglobin in pregnancy, hematocrit in pregnancy, low hemoglobin in pregnancy
Decreased hemoglobin in pregnancy
pregnant), which is observed in healthy pregnant women. The biggest difference between the growth rate of blood plasma volume and the number of red blood cells in the maternal circulation is formed during the end of the second, beginning of the third trimester (a decrease in hemoglobin usually occurs at 28-36 weeks of pregnancy). The hemoglobin concentration rises due to the cessation of the increase in plasma volume and the continuation of the increase in the amount of hemoglobin..jpg) Conversely, the absence of physiological anemia is a risk factor for stillbirth. nine0007
Conversely, the absence of physiological anemia is a risk factor for stillbirth. nine0007 Anemia in pregnancy
Defining anemia in pregnant women is difficult because it consists of pregnancy-related changes in plasma volume and red blood cell count, physiological differences in hemoglobin concentration between women and men, and the frequency of iron supplementation during pregnancy.
Women with hemoglobin values below these levels are considered anemic and should undergo routine tests (CBC with peripheral blood smear evaluation, reticulocyte count, serum iron, ferritin, transferrin). If no abnormalities were detected during the examination, then hemoglobin reduced to a level of 100 g / l can be considered physiological anemia with a wide variety of factors affecting the normal level of hemoglobin in a particular person. nine0007
Chronic severe anemia is most common among women in developing countries. A decrease in maternal hemoglobin below 60 g / l leads to a decrease in the volume of amniotic fluid, vasodilation of the cerebral vessels of the fetus and a change in the heart rate of the fetus. It also increases the risk of preterm birth, miscarriage, low birth weight and stillbirth. In addition, severe anemia (hemoglobin less than 70 g/l) increases the risk of maternal death. There is no evidence that anemia increases the risk of congenital malformations of the fetus. nine0007
nine0007
Severe chronic anemia is usually associated with insufficient iron stores (due to insufficient dietary intake or intestinal worm infestations), folate deficiency (due to insufficient intake and chronic hemolytic conditions such as malaria). Thus, prevention of chronic anemia and improvement of pregnancy outcome is possible with the use of nutritional supplements and the use of infection control measures.
Administering blood and packed red cell transfusions (where safe blood transfusion is available) is a reasonable aggressive treatment for severe anemia, especially if there are signs of fetal hypoxia. nine0007
Signs of physiological anemia of pregnancy disappear 6 weeks after delivery, when plasma volume returns to normal.
Iron requirement
In a singleton pregnancy, the iron requirement is 1000 mg per pregnancy: approximately 300 mg for the fetus and placenta and approximately 500 mg, if any, to increase hemoglobin. 200 mg is lost through the intestines, urine and skin.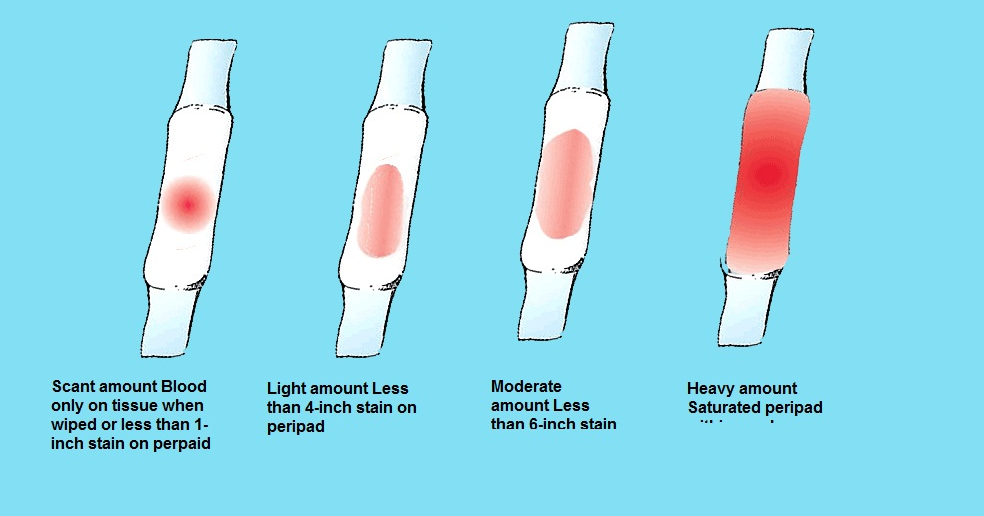 Since most women do not have an adequate supply of iron to meet their needs during pregnancy, iron is usually prescribed as part of a multivitamin, or as a separate element. In general, women taking iron supplements have a 1 g/dL higher hemoglobin concentration than women not taking iron. nine0007
Since most women do not have an adequate supply of iron to meet their needs during pregnancy, iron is usually prescribed as part of a multivitamin, or as a separate element. In general, women taking iron supplements have a 1 g/dL higher hemoglobin concentration than women not taking iron. nine0007
Folate requirement
The daily folate requirement for non-pregnant women is 50-100 micrograms. An increase in the number of red blood cells during pregnancy leads to an increase in the need for folic acid, which is provided by increasing the dose of folic acid to 400-800 mcg per day, to prevent neural tube defects in the fetus.
Pregnancy platelets
In most cases, the platelet count during an uncomplicated pregnancy remains within the normal range for non-pregnant women, but it is also possible for pregnant women to have a lower platelet count compared to healthy non-pregnant women. The platelet count begins to rise immediately after childbirth and continues to increase for 3-4 weeks until it returns to normal values. nine0007
nine0007
Thrombocytopenia in pregnancy
The most important obstetrical change in platelet physiology during pregnancy is thrombocytopenia, which may be associated with pregnancy complications (severe preeclampsia, HELLP syndrome), drug disorders (immune thrombocytopenia) or may be gestational thrombocytopenia.
Gestational or occasional thrombocytopenia is asymptomatic in the third trimester of pregnancy in patients without prior thrombocytopenia. It is not associated with maternal, fetal, or neonatal complications and resolves spontaneously after delivery. nine9/l. The white blood cell count drops to the reference range for non-pregnant women by the sixth day after birth.
Pregnant women may have a small number of myelocytes and metamyelocytes in the peripheral blood. According to some studies, there is an increase in the number of young forms of neutrophils during pregnancy. Lobe bodies (blue staining of cytoplasmic inclusions in granulocytes) are considered normal in pregnant women.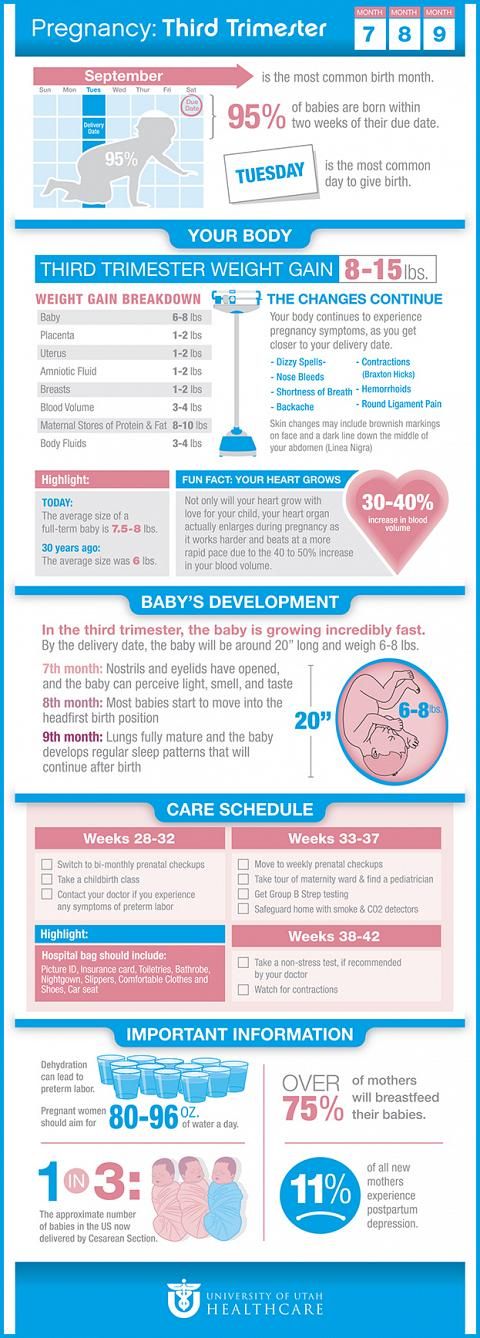
In healthy women during uncomplicated pregnancy, there is no change in the absolute number of lymphocytes and there are no significant changes in the relative number of T- and B-lymphocytes. The number of monocytes usually does not change, the number of basophils may decrease slightly, and the number of eosinophils may increase slightly. nine0007
Coagulation factors and inhibitors
During normal pregnancy, the following changes in clotting factor levels occur, leading to physiological hypercoagulation:
The end result of these changes is an increase in the tendency to thrombosis, an increase in the likelihood of venous thrombosis during pregnancy and, especially, in the postpartum period. Along with contraction of the myometrium and an increase in the level of decidual tissue factor, hypercoagulability protects the pregnant woman from excessive bleeding during labor and delivery of the placenta. nine0007
APTT remains normal during pregnancy, but may decrease slightly. Prothrombin time may be shortened. Bleeding time does not change.
The timing of normalization of blood clotting activity in the postpartum period may vary depending on factors, but everything should return to normal within 6-8 weeks after delivery. The hemostasiogram should not be assessed earlier than 3 months after delivery and after lactation is completed to exclude the influence of pregnancy factors. nine0007
The hemostasiogram should not be assessed earlier than 3 months after delivery and after lactation is completed to exclude the influence of pregnancy factors. nine0007
The influence of acquired or inherited thrombophilia factors on pregnancy is an area for research.
Postpartum
Hematological changes associated with pregnancy return to normal 6-8 weeks after delivery. The rate and nature of the normalization of changes associated with pregnancy, specific hematological parameters are described above in the section on each parameter.
 General (clinical) blood test.
General (clinical) blood test.  nine0007
nine0007 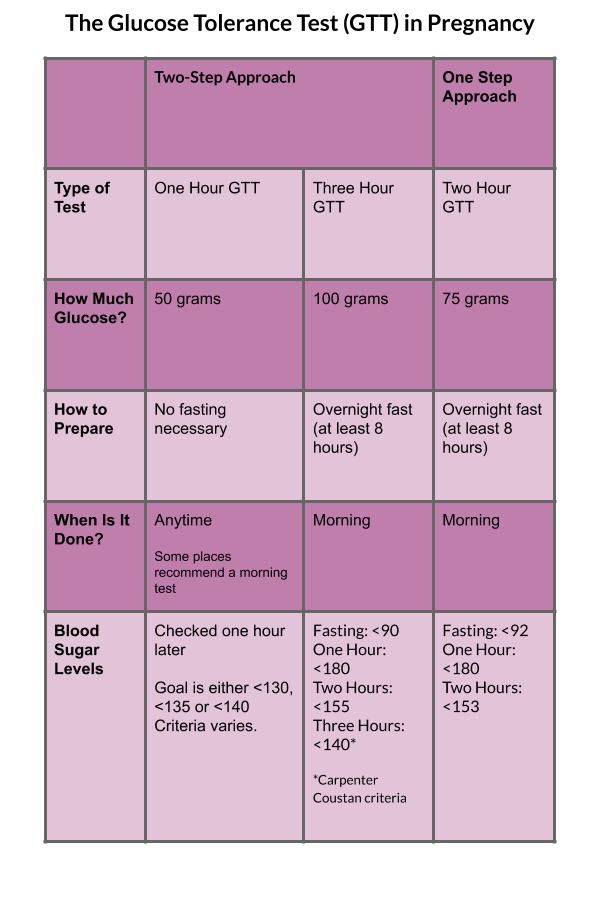 nine0007
nine0007  General (clinical) blood test.
General (clinical) blood test.  Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.
Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 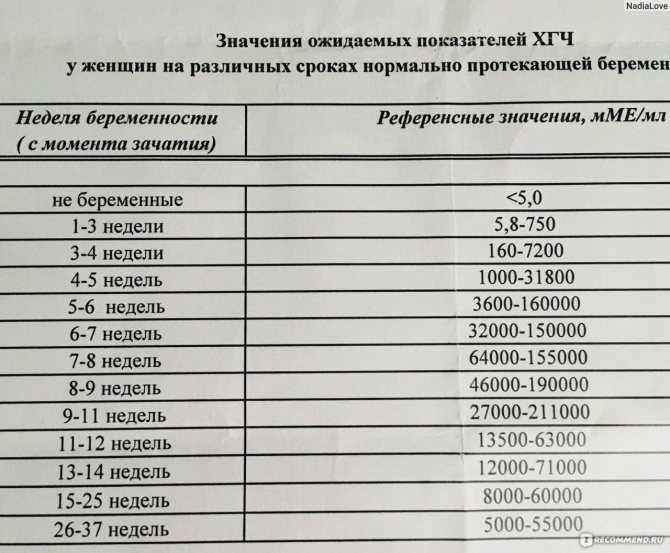 Inspections and consultations:
Inspections and consultations: 
 Dry processing of seams (if any).
Dry processing of seams (if any).