Let down reflex definition
Let-down reflex | Pregnancy Birth and Baby
Let-down reflex | Pregnancy Birth and Baby beginning of content3-minute read
Listen
The let-down reflex is an important part of breastfeeding that starts milk flowing when your baby feeds. Each woman feels it differently, and some may not feel it at all. It can be affected by stress, pain and tiredness but once feeding is established, it requires little or no thought.
What is the let-down reflex?
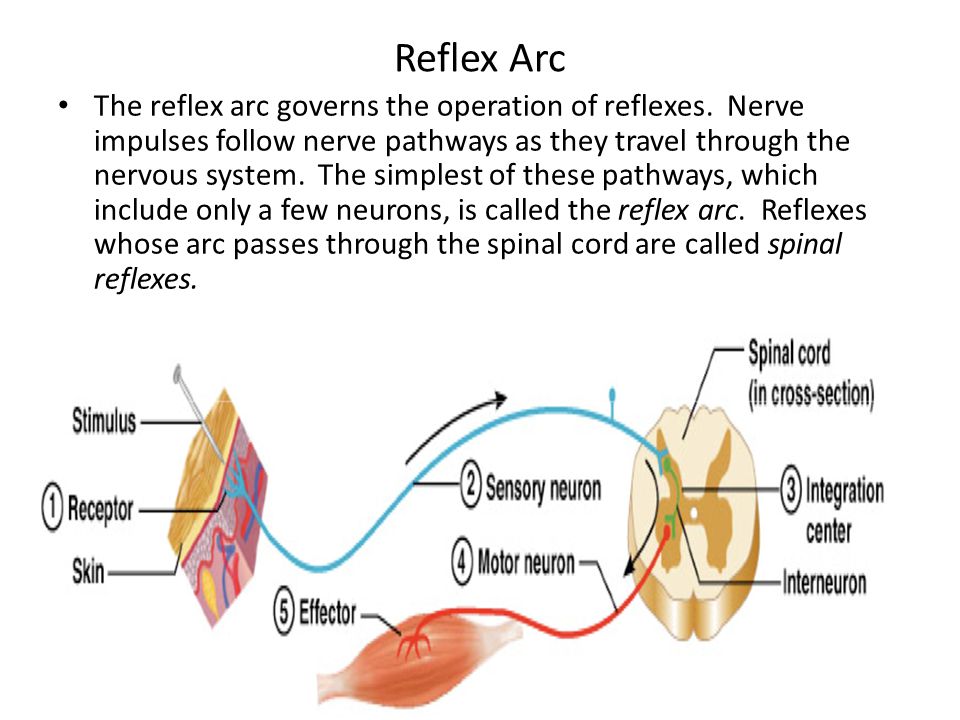
The let-down reflex is what makes breastmilk flow. When your baby sucks at the breast, tiny nerves are stimulated. This causes two hormones – prolactin and oxytocin – to be released into your bloodstream. Prolactin helps make the milk, while oxytocin causes the breast to push out the milk. Milk is then released or let down through the nipple.
Some women feel the let-down reflex as a tingling sensation in the breasts or a feeling of fullness, although others don’t feel anything in the breast.
Most women notice a change in their baby’s sucking pattern as the milk begins to flow, from small, shallow sucks to stronger, slower sucks.
Some women also notice, while feeding or expressing from one breast, that milk drips from the other.
Your let-down reflex needs to be established and maintained to ensure a good supply of milk. This reflex requires no thought, unless you are having problems with breastfeeding.
When does it occur?
The let-down reflex occurs:
- in response to your baby sucking at the breast
- hearing, seeing or thinking about your baby
- using a breast pump, hand expressing or touching your breasts or nipples
- looking at a picture of your baby
- hearing your baby (or another baby) cry
The let-down reflex generally occurs 2 or 3 times a feed. Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
The let-down reflex can also occur with other stimulation of the breast, such as by your partner.
Strategies to encourage the reflex
The let-down reflex can be affected by stress, pain and tiredness. There are many things to try if you are experiencing difficulty.
- Ensure that your baby is correctly attached to the breast. A well-attached baby will drain a breast better.
- Feed or express in a familiar and comfortable environment.
- Try different methods to help you to relax: calming music, a warm shower or a warm washer on the breast, some slow deep breathing, or a neck and shoulder massage.
- Gently hand express and massage your breast before commencing the feed.
- Look at and think about your baby.
- If you are away from your baby, try looking at your baby’s photo.
- Always have a glass of water nearby.
Milk let-down can be quite forceful, particularly at the beginning of a feed. This fast flow of milk can upset your baby, but it might not mean you have oversupply. It can be managed through expressing before a feed, reclining slightly and burping your baby after the first few minutes. If you continue to have problems, seek advice.
How to deal with unexpected let-down
Until you and your baby fine-tune breastfeeding, many sensations and thoughts can trigger your let-down reflex. Leaking breasts can be embarrassing, but should stop once breastfeeding is fully established.
In the meantime you can feed regularly, apply firm pressure to your breasts when you feel the first sensation of let-down, use breast pads and wear clothing that disguises milk stains.
If you need help and advice:
- Pregnancy Birth and Baby on 1800 882 436
- your maternal child health nurse
- a lactation consultant (your maternity hospital might be able to help)
- Australian Breastfeeding Association on 1800 686 268
Sources:
Australian Breastfeeding Association (Breastfeeding - naturally : the Australian Breastfeeding Association's guide to breastfeeding - from birth to weaning), Australian Breastfeeding Association (Let-down reflex)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Breastfeeding your baby
- How to increase breast milk supply
- Oversupply of breastmilk
Need more information?
Breastfeeding challenges - Ngala
Sometimes breastfeeding can be challenging
Read more on Ngala website
Breast refusal and baby biting breast | Raising Children Network
Breast refusal or baby biting breast are common breastfeeding issues. These issues might resolve themselves, or your child and family health nurse can help.
Read more on raisingchildren.net.au website
Breastfeeding - expressing breastmilk - Better Health Channel
Expressing breast milk by hand is a cheap and convenient method.
Read more on Better Health Channel website
Breast feeding your baby - MyDr.com.au
Breast milk has long been known as the ideal food for babies and infants. Major health organisations recommend that women breast feed their babies exclusively until they are 6 months old, and continue breast feeding, along with solids, until they are 12 months old or more. Breast milk has many benefits.
Read more on myDr website
Expressing and storing breast milk
This page includes information about expressing, storing, cleaning equipment, transporting and preparing expressed breastmilk for your baby.
Read more on WA Health website
Expressing breastmilk & storing breastmilk | Raising Children Network
You can express breastmilk by hand, or with a manual or an electric pump. Store expressed breastmilk in special bags or containers in the fridge or freezer.
Store expressed breastmilk in special bags or containers in the fridge or freezer.
Read more on raisingchildren.net.au website
Mastitis, blocked duct & breast abscess | Raising Children Network
If you think you have a blocked milk duct, you can treat it at home to start with. If you think you have mastitis or a breast abscess, see your GP as soon as possible.
Read more on raisingchildren.net.au website
Weaning at 6 Months | Tresillian
Babies start weaning when they begin consuming foods other than breastmilk. For advice on weaning check out Tresillian's tip page.
Read more on Tresillian website
Frequently asked questions about alcohol and pregnancy | FASD Hub
We've answered some common questions about alcohol use during pregnancy and breastfeeding, and about living with fetal alcohol spectrum disorder (FASD).
Read more on FASD Hub Australia website
Breastfeeding challenges - Ngala
Many new mothers experience breastfeeding challenges
Read more on Ngala website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Is Yours Normal, Tips to Improve It, and More
What are some benefits of breastfeeding?
Breastfeeding not only creates a bond between you and your baby, it also provides your baby with nutrients that promote healthy growth.
Breast milk has antibodies that strengthen your baby’s immune system, protecting them from infections and diseases.
Breastfeeding also has long-term benefits. For example, breastfed babies are less likely to be obese or develop type 2 diabetes later in life.
Even if you’re convinced that breast milk is the best choice for your baby, you may have questions. Among your list of concerns, you may wonder whether your let-down reflex is normal. Find out more here.
What is the let-down reflex?
Between sore nipples, latching issues, and problems with milk flow, breastfeeding can be tricky. The let-down reflex, however, can make breastfeeding easier for both you and your baby.
“Let-down” is the release of milk from the breast. It’s a normal reflex that occurs when nerves in your breasts are stimulated, usually as a result of your baby sucking. This sets in motion a chain of events, and hormones are released into your bloodstream.
The hormone prolactin stimulates milk production, and the hormone oxytocin causes your breast to release or “let down” milk.
What is a normal let-down reflex?
Let-down, or the availability of milk, is different for every mother. Some women let down within seconds of their baby beginning to suck, but it takes others several minutes to let down. Therefore, you shouldn’t compare your reflex with another mother’s reflex.
Knowing what to expect during let-down can help you determine whether your reflex is normal.
Some breastfeeding mothers can feel their milk flow from their ducts to their nipples, but others don’t. You may notice different sensations in or around your breasts, such as:
- a tingling sensation, which feels like pins and needles
- a feeling of fullness
- milk leaking from your other breast
These sensations can develop immediately after giving birth, or they may not start until several weeks into breastfeeding. It varies from mother to mother.
Other bodily responses
Let-down can also trigger other natural responses. Although you may only feed your baby from one breast, let-down typically happens in both breasts simultaneously.
You shouldn’t be surprised if your other breast begins to leak. Also, don’t be alarmed if you feel your uterus contract when you let down. This is also normal.
Pacing
Your milk may let down at a slow and steady pace. Sometimes, however, let down is fast and forceful.
Your baby could choke if they suck too much milk at once. The flow of milk does gradually slow down, though, and it becomes more comfortable for your baby.
If you don’t want to risk your baby choking, use your hand and squeeze out a little milk before each feeding. Fast-flowing milk not only increases the likelihood of choking, but some people believe it can cause gas and colic.
Which actions can prompt let-down?
Let-down is a normal reflex when your baby sucks on your breasts, but it can also take place before your baby latches on. You may notice your milk let down when you hear your baby cry or if you’re overdue for a feeding.
Additionally, touching your breasts or using a breast pump can prompt let-down.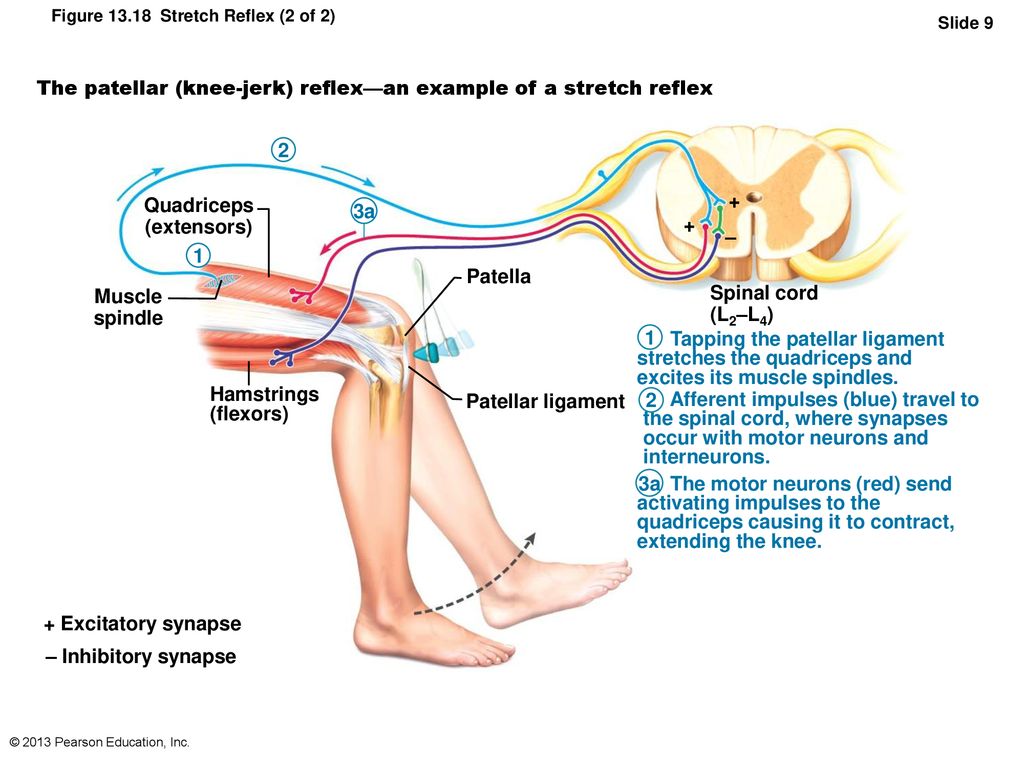 This is called “expressing.”
This is called “expressing.”
How can you improve your let-down reflex?
Let-down comes easily and naturally for some breastfeeding mothers, but others have trouble getting their milk to flow.
If you have trouble with let-down — whether you’re feeding or expressing — there are several things you can do to help the process:
- sip on a warm beverage
- listen to soothing, calm music
- take a warm shower before feeding
- hold your baby close to your body
- gently massage your breasts to stimulate milk flow
What is the takeaway?
It’s important to remember that let-down is different for every person. You may have a physical response and feel tingling or fullness around the breasts every time milk is ready to flow, or you may feel nothing.
If you have concerns about your let-down reflex, talk to your doctor. Also, let your doctor know if you’re having pain during let-down. A painful let-down reflex isn’t unusual, and the pain typically goes away once you adjust to breastfeeding.
If pain doesn’t improve, it can be a sign of:
- a clogged milk duct
- a breast infection
- a strained muscle from giving birth
- your breasts producing too much milk
Study of oculomotor functions and their disorders in the Moscow Eye Clinic
To understand how the eyeball moves, it is necessary to understand the geometry of the eye and the functional tasks of the oculomotor muscles. The eyeball can rotate along three main axes - vertical (z), horizontal (y) and nasoccipital (x). The center of the eyeball is the point of intersection of these axes.
Eye rotations are provided by coordinated contractions and relaxation of six oculomotor muscles - four straight and two oblique each eye. The actions of the muscles of the eyeball are determined in the center of rotation of the eyeball, it also determines the course and attachment of each of the muscles. The movements of the eyeball and muscles are also influenced by the connective tissue formations (pulleys) of the extraocular muscles.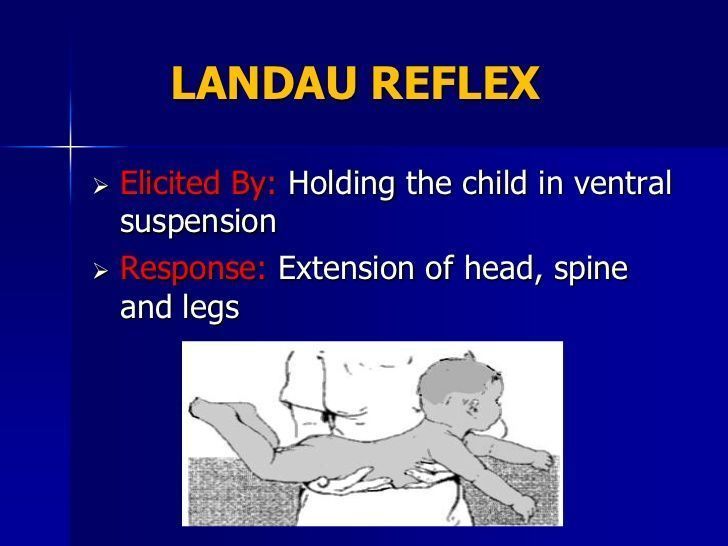 A person performs at least 100,000 saccades with his eyes daily, so the oculomotor muscles are resistant to fatigue. From other skeletal muscles, the oculomotor muscles are also distinct. For example, the eye fibers are provided with multiple innervations, with each motor neuron (the smallest motor unit of the human body) innervating up to 10 or 20 muscle fibers.
A person performs at least 100,000 saccades with his eyes daily, so the oculomotor muscles are resistant to fatigue. From other skeletal muscles, the oculomotor muscles are also distinct. For example, the eye fibers are provided with multiple innervations, with each motor neuron (the smallest motor unit of the human body) innervating up to 10 or 20 muscle fibers.
Prices for treatment
Find out the price of the procedure, make an appointment at the "Moscow Eye Clinic" by calling 8 (800) 777-38 81 and (499) 322-36-36 (daily from 9:00 to 21:00 ) or using the online registration form.
Make an appointment
Basic eye movements
Monocular eye movements include inductions - these are movements of abduction, adduction, raising, lowering, turning the eyeball inward or outward.
Binocular friendly movements of both eyes are called versions, they are responsible for moving the visual axes in one direction. Versions - this is a simultaneous turn of the eyes to the left and right, raising and lowering them, rotational movements.
Binocular disjunctive movement is vergence, it provides movement of the visual axes of the eyes in opposite directions - convergence, divergence (divergence, with rotation).
Eye rotation is provided by the coordinated contraction of six muscles in each eye.
Functions of the muscles of the eyeball, determined by the center of rotation, the place of attachment and the course of each muscle. Through connective tissue formations located slightly behind the equator and 10 mm behind the points of attachment of the muscles, the tendons of the rectus muscles of the eye pass.
Connective tissue formations of the rectus muscles, consisting of smooth muscle fibers and fibrous tissue, which allows you to limit excessive movements during the rotation of the eyes.
The agonist muscle provides eye movement in a given direction, and the antagonist muscle produces eye movement in the opposite direction from the given direction.
According to Sherrington's law of reciprocal innervation, when the agonist muscle receives an excitation signal to begin contraction, at the same time, a suppression signal is sent to the antagonist muscle of that eye.
This reciprocal connection is due to central connections that exist in the brainstem. In one direction, the eyes move pairs of muscles, one from each eye. For example, the right outer straight line with the left inner straight line simultaneously contract when looking to the right.
In accordance with Hering's law of innervation identity, during eye movements of the same name, the pairs of synergist muscles receive the same signal and both eyes move together.
The vertically acting muscles are also paired (the right superior rectus pairs with the left inferior oblique and the right inferior rectus pairs with the left superior oblique). The nature of their interaction is very complex, because even with horizontal ordinary movements, all the muscles of the eye are involved.
Oculomotor functions
In clinical studies, all eye positions are determined: primary - when looking forward, as well as secondary position - when looking to the right, left, down and up. Tertiary positions up and left, down and left, up and right, down and right.
Tertiary positions up and left, down and left, up and right, down and right.
For example, the main elevator when looking to the right is the superior rectus muscle of the right eye, as well as the inferior oblique muscle of the left eye.
In this position, the right superior rectus muscle becomes the main elevator in the abduction of the right eye (under the influence of the external rectus muscle), due to its attachment to the eyeball with the formation of an angle with the visual axis of 23 degrees.
The left oblique inferior muscle becomes the main elevator during adduction of the left eye (under the action of the internal rectus muscle) due to its attachment to the eyeball and the formation of an angle of 51 degrees with the visual axis.
The cardinal positions of gaze in this case cannot correspond to the primary, secondary or tertiary action of the muscles. When the gaze of the right eye is directed to the right and upward, for raising or abducting the eyeball, the right superior rectus muscle is not responsible. The tertiary action of the superior rectus muscle is adduction, not abduction. When looking with the right eye upwards to the right, the lifting of the eyeball is provided by the contraction of the superior rectus muscle, while abduction is provided by the contraction of the external rectus muscle.
The tertiary action of the superior rectus muscle is adduction, not abduction. When looking with the right eye upwards to the right, the lifting of the eyeball is provided by the contraction of the superior rectus muscle, while abduction is provided by the contraction of the external rectus muscle.
Among the main tasks of the motor system, it is customary to single out:
- Increasing the volume of observation when transforming the field of view into a fixation zone;
- Transferring images of objects of attention to the fovea with holding them;
- Ensuring the correct position of the eyes, for normal binocular vision.
Functional classification of eye movement systems, includes:
- Fixation system: holds the image of a static object steadily for
fossa, with a motionless head. - Optokinetic: Provides a stable retinal image during prolonged head movements.
- Movements directing the fovea towards the object of interest and rapidly transferring the image of the object of interest to the fovea via saccades.

- Drift: Image retention on the fovea of a small moving target.
- Vergences: moving the eyes in opposite directions (convergence or divergence) to hold the image of a single object on both pits at the same time.
Methods of clinical research
In the course of diagnosing oculomotor disorders, an anamnesis is first taken, which includes the patient's complaints. Then an examination is carried out, with a mandatory inspection of the state of the pupils, their reaction to light, the presence of anisoroots (the position of the head and chin), and the absence of nystagmus. The angle gamma (kappa) is detected and determined.
Important examination in the primary position of the eyes, checking their mobility in nine positions. Investigation of monocular movements (ductions) and binocular friendly movements (versions), detection of mobility disorders and assessment of possible muscle hyperfunction, respectively, of the corneal reflex in relation to the midline passing through the middle of the pupil.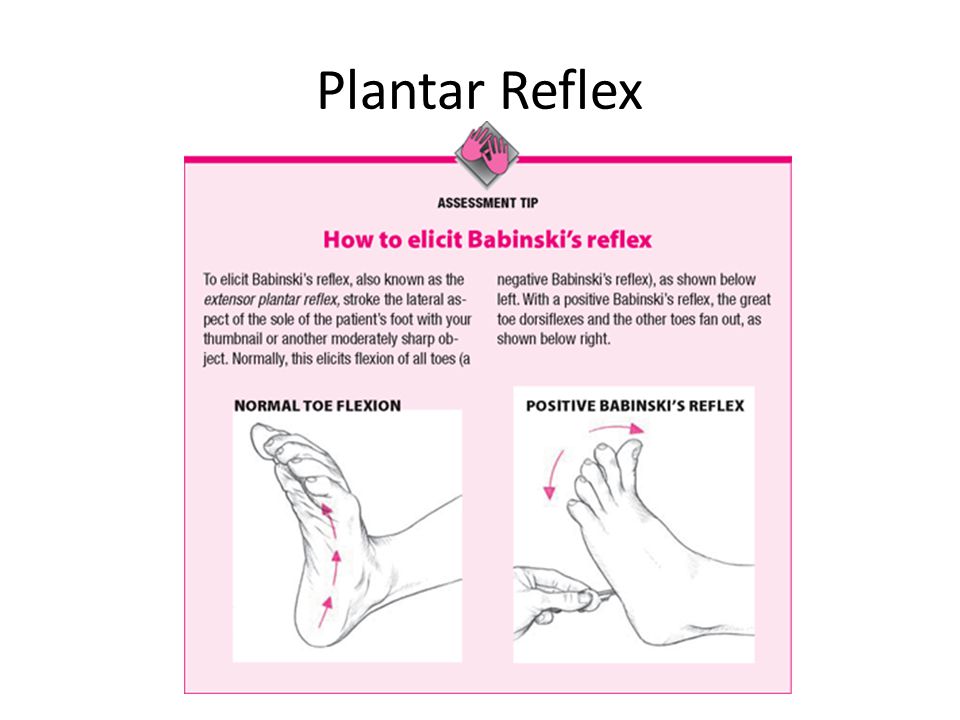
Cover-test or Сover/uncover-test are important for determining preferred fixation, occult strabismus, unfriendly movements. The alternation test allows you to distinguish a clear deviation from a latent one and measure the tropia. The prism test measures apparent deviation by simultaneously occluding the fixing eye and placing the prism in front of the squinting eye. In the absence of a fixation movement, the value of the prism indicates the value of the angle.
For dissociated vertical strabismus (DVD), the Under-cover test will be used. It is performed with a prism and makes it possible to measure the apparent deviation. For its implementation, occlusion of the fixing eye is performed, and at the same time a prism is installed in front of the squinting eye. If there is no fixation movement, then the value of the prism is equal to the entire value of the angle.
When examining vergence, determine the close point of convergence on the synoptophore using prisms. Testing for diplopia, color test, Bagolini test, method of successive images are carried out.
Testing for diplopia, color test, Bagolini test, method of successive images are carried out.
For the study of phoria and fusion, a double Muddox test with an assessment of vertical strabismus or with a rotational component is used. In order to evaluate aniseikonia, a duochrome test and a Lancaster test are used to assess muscle balance.
Binocular vision is tested with Titmus test, Random test, Frisbee test and Lang test.
In case of obvious strabismus, to check visual functions, the measurement of the angle of deviation is carried out according to Hirschberg (the position of the corneal reflex relative to the pupillary edge). The Crimean test is performed (a prism placed in front of the squinting eye) and a test using a synoptophore.
For the study of vertical and horizontal saccades, the patient is asked to look from object to object 30 degrees on either side of the midline at a distance of 40 cm. Small saccades.
normal 1-5 deg, 200 ms. Saccades of 5-20 degrees indicate cerebellar disease and multiple sclerosis. Unclear fixation indicates disturbances in the stem centers of saccade and supranuclear regulation. To assess the state of the saccadic (fixation) system of the eyes, such tests are used: Devik, Griffin, etc.
Saccades of 5-20 degrees indicate cerebellar disease and multiple sclerosis. Unclear fixation indicates disturbances in the stem centers of saccade and supranuclear regulation. To assess the state of the saccadic (fixation) system of the eyes, such tests are used: Devik, Griffin, etc.
Vestibular movements are assessed according to the following criteria: vestibular nystagmus increases without an object of fixation, with eyes closed during a test with a +20.0D lens with a visual acuity deterioration of one line (the study is carried out before and after turning the head left-right). A caloric test to determine the damage to the vestibular, nuclear and infranuclear pathways is carried out as follows: cold and warm water is instilled into the ear. Determines the state: with cold water (fast phase of OKN in the opposite direction from the ear), with warm water (fast phase of OKN towards the ear).
Optokinetic nystagmus (return of the image in the fovea in case of object movement) is examined with a rotating drum and subsequent assessment, nystagmus (its symmetry and direction of eye movement). Electronystagmography can also be used. Its indicators are violated in case of damage in the temporal and parietal areas of the brain, as well as in the vessels of the head and neck.
Electronystagmography can also be used. Its indicators are violated in case of damage in the temporal and parietal areas of the brain, as well as in the vessels of the head and neck.
The condition of the eye muscles is assessed using electromyography.
The defining moment for a good test result is the level and choice of equipment, practical training of the doctor. The Moscow Eye Clinic employs specialists with a high level of practical training who own the equipment we have for vision diagnostics.
In our center, all patients can be examined using diagnostic equipment, and, based on the results, they can get advice from a specialist. We are open seven days a week and are open daily from 9 a.m. to 9 p.m.
5/5 (1 rating)
Med. portal:
Appointment
The essence of the problem:
What is the sucking reflex? – Drink-Drink
Overview
Newborn babies are born with several important reflexes that help them in their first weeks and months of life. These reflexes are involuntary movements that occur either spontaneously or in response to various actions. For example, the sucking reflex occurs when a child touches the palate. The baby will start to suck when this area is stimulated, which helps with breastfeeding or bottle feeding.
These reflexes are involuntary movements that occur either spontaneously or in response to various actions. For example, the sucking reflex occurs when a child touches the palate. The baby will start to suck when this area is stimulated, which helps with breastfeeding or bottle feeding.
Reflexes can be strong in some babies and weak in others depending on a number of factors, including how early the baby was born before due date. Read on to learn about the sucking reflex, its development, and other reflexes.
When does the sucking reflex occur?
The sucking reflex develops while the baby is still in the womb. Its earliest development is at the 32nd week of pregnancy. It usually develops fully by 36 weeks of gestation. You can even see this reflex in action during a routine ultrasound. Some babies will suck on their thumbs or hands, indicating that this important ability is developing.
Babies born prematurely may not have a strong sucking reflex at birth. They may also not have enough stamina to complete a feeding session. Premature babies sometimes need extra help to get their nutrients through a feeding tube, which is passed through the nose into the stomach. It can take weeks for a premature baby to coordinate sucking and swallowing, but many realize this by the time their initial due date is reached.
They may also not have enough stamina to complete a feeding session. Premature babies sometimes need extra help to get their nutrients through a feeding tube, which is passed through the nose into the stomach. It can take weeks for a premature baby to coordinate sucking and swallowing, but many realize this by the time their initial due date is reached.
Sucking reflex and feeding
The sucking reflex occurs in two stages. When a pacifier - from a breast or from a bottle - is placed in the baby's mouth, he will automatically begin to suckle. When breastfeeding, the baby puts his lips on the areola and squeezes the nipple between the tongue and palate. They will use a similar motion when feeding a bottle.
The next stage occurs when the baby moves the tongue to the nipple to suckle, in effect milking the breast. This action is also called an expression. Suction helps to keep the breast in the baby's mouth during the process due to negative pressure.
Rooting versus the sucking reflex
There is another reflex that accompanies sucking called rooting. Babies will instinctively dig or search for the breast before suckling on it. Although the two reflexes are related, they serve different purposes. Rooting helps the baby find the breast and nipple. Suckling helps the baby extract breast milk for nourishment.
Babies will instinctively dig or search for the breast before suckling on it. Although the two reflexes are related, they serve different purposes. Rooting helps the baby find the breast and nipple. Suckling helps the baby extract breast milk for nourishment.
How to Test Your Baby's Sucking Reflex
You can test your baby's sucking reflex by placing a pacifier (breast or bottle), a clean finger or a pacifier in your baby's mouth. If the reflex is fully developed, the child should clasp the object with his lips, and then squeeze it rhythmically between the tongue and the palate.
Talk to your child's pediatrician if you suspect your child has problems with the sucking reflex. Since the sucking reflex is important for feeding, disruption of this reflex can lead to malnutrition.
Care problems and seeking help
Breathing and swallowing while suckling can be a difficult combination for premature babies and even some newborns. As a result, not all babies are professionals—at least not at first. However, with practice, children can master this task.
However, with practice, children can master this task.
What you can do to help:
- Kangaroo care. Give your baby as much skin-to-skin contact or what is sometimes called a kangaroo as possible. This helps keep your baby warm and may even increase milk supply. The kangaroo method is not suitable for all children, especially children with certain medical conditions.
- Nursing wake-up call. Wake your child up every 2-3 hours to eat. Your healthcare provider can help you determine when you no longer need to wake your baby for feeding. Premature babies may need to be fed more often or woken up to eat longer than other babies.
- Take position. Keep your baby in the breastfeeding position, even if he is formula-fed. You can even try moistening cotton balls with breast milk and placing them next to your baby. The idea is to get them to recognize the smell of your milk.
- Try other positions. Experiment with holding your baby in different positions while breastfeeding.
 Some children do well in the “twin” (or “football hold”) position, where they are tucked under the arm and their body is supported by a pillow.
Some children do well in the “twin” (or “football hold”) position, where they are tucked under the arm and their body is supported by a pillow. - Increase the downward reflex. Work on increasing the milk flush reflex that causes milk to come out. This will make it easier for the baby to express milk. You can massage, hand pump, or apply a warm compress to your chest to speed up the process.
- Stay positive. Try your best not to lose heart, especially in the early days. The most important thing is to get to know your child. Over time, they should begin to consume more milk with longer feedings.
Lactation Counselors
If you are having trouble breastfeeding, a certified lactation consultant (IBCLC) can also help. These specialists focus exclusively on feeding and everything related to nursing. They can help with anything from blockages and airway blockages to assessing and correcting other feeding issues such as positioning. They may suggest using a variety of devices, such as nipple shields, to help with a better latch.
Your baby's pediatrician, your OB/GYN or midwife can recommend a breastfeeding consultation. In the United States, you can find an IBCLC near you by searching the US Lactation Consultants Association database. You can request home visits, private consultations, or help at a breastfeeding clinic. You can also rent equipment such as hospital grade breast pumps. Some hospitals offer free consultations while you are in the delivery room or even after you have gone home.
Baby reflexes
Babies develop several reflexes to help them adjust to life outside the womb. In premature babies, the development of some reflexes may be delayed, or they may retain the reflex longer than average. Talk to your child's doctor if your child's reflexes are bothering you.
Root reflex
Sucking and digging reflexes go hand in hand. Your child will turn their head when they are stroked on the cheek or corner of their mouth. It's like they're trying to find a nipple.
To test the root reflex:
- Stroke your child's cheek or mouth.
- Follow rooting from side to side.
As your baby gets older, usually around three weeks of age, he will turn more quickly to the side being stroked. The rooting reflex usually disappears by 4 months.
Moro reflex
The Moro reflex is also known as the startle reflex. This is because this reflex often occurs in response to loud noises or movements, most commonly the sensation of falling backwards. You may notice that your child throws up his arms and legs in response to unexpected sounds or movements. After extension of the limbs, your child will contract them.
The Moro reflex is sometimes accompanied by crying. It can also affect your child's sleep by waking them up. Sometimes swaddling helps reduce the Moro reflex while the baby is sleeping.
To test the Moro reflex:
- Observe your child's reaction to loud sounds such as a barking dog.
- If your child jerks his arms and legs and then bends them back, this is a sign of the Moro reflex.
The Moro reflex usually disappears by 5-6 months.
Tonic neck
Asymmetric neck tone or “fencing reflex” occurs when your child's head is turned to one side. For example, if their head is turned to the left, the left arm will be extended while the right arm will be bent at the elbow.
To check neck tone:
- Gently turn the child's head to one side.
- Watch their hands move.
This reflex usually disappears by about 6-7 months of age.
The grasp reflex
The grasp reflex allows babies to automatically grab your finger or small toys when they place them in their palm. It develops in utero, usually around 25 weeks after conception. To test this reflex:
- Stroke your child's hand firmly.
- They should cling to your finger.
The grip can be quite strong and usually lasts until the child is 5-6 months old.
Babinski's reflex
Babinski's reflex occurs when the child's sole is rubbed hard. This causes the big toe to bend towards the top of the foot. The other fingers will also be splayed out. Test:
This causes the big toe to bend towards the top of the foot. The other fingers will also be splayed out. Test:
- Rub firmly on the bottom of your child's foot.
- Watch their toes fan out.
This reflex usually disappears by the time your child is 2 years old.
Step reflex
The step or “dance” reflex can cause your baby to be able to walk (with assistance) shortly after birth.
Test:
- Hold the child upright over a flat hard surface.
- Place the child's feet on the surface.
- Continue to give full support to your child's body and head and watch him take a few steps.
This reflex usually disappears by about 2 months of age.
Reflexes at a glance
| suckling | at 36 weeks pregnant; observed in most newborns, but may be delayed in preterm infants | 4 months |
| children | 5 at 6 months | |
| neck tone | observed in most term and premature babies | 6 at 7 months |
| seizure | by 26 weeks of gestation; observed in the majority of term and premature infants | 5 at 6 months |
| Babinsky | observed in the majority of term and premature infants | 2 years |
| step7 observed in most premature infants
| 0271 | 2 months |
Conclusion
Although babies do not have instructions for use, they do have a range of reflexes to help them survive the first weeks and months of life.