Labor pain relief
Labor Pain: Signs, Symptoms & Management
Labor PainYou’re having a baby! You’re likely excited and no doubt nervous about several things — including the hard work and pain of labor and giving birth. Fortunately, there are many ways to ease labor pain and help you relax, including medications and breathing techniques.
There are many ways to ease labor pain and help you relax, including medications and breathing techniques.
Every woman’s pain during labor is different. Talking with your health care providers, including your anesthesiologist, will help you decide which pain management methods will help you have the best possible labor and delivery experience. You may decide to use no medication, or you might choose from different types and levels of medications. Depending on how your labor progresses, you may choose to change your pain management plan or use a combination of methods. Whatever you decide, your anesthesiologist is available to help you.
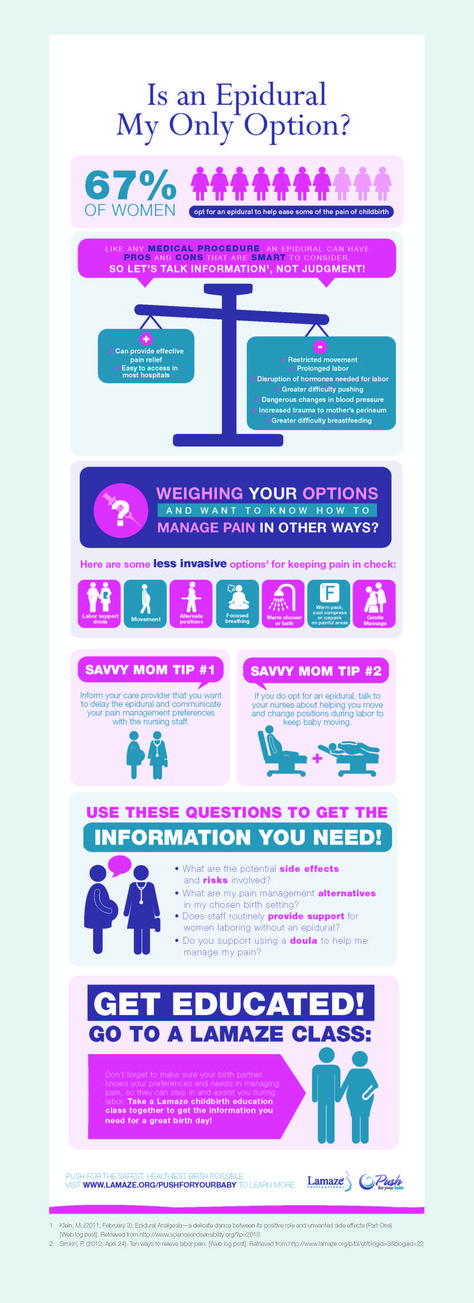
Here are some of the most common options for managing labor pain:
- Epidural: This is the most common type of pain relief used during labor. If you choose to have an epidural, an anesthesiologist will insert a needle and a tiny tube, called a catheter, in the lower part of your back. An epidural numbs only the lower part of your body below your belly button and allows you to be awake and alert throughout labor, as well as to feel pressure. You will be able to push when it’s time to give birth to your baby. It can take about 15 minutes for the pain medication to work, and you can continue to receive it as needed. Epidurals are very safe; however, as with all medications and medical procedures, there are some potential side effects to be aware of.
- Decrease in blood pressure – The medication may lower your blood pressure, which may slow your baby’s heart rate. To make this less likely, you will be given extra fluids through a tube in your arm (IV line) and may need to lie on your side.
 Sometimes, your anesthesiologist will give you a medication to maintain your lower blood pressure.
Sometimes, your anesthesiologist will give you a medication to maintain your lower blood pressure. - Sore back – Your lower back may be sore where the needle was inserted to deliver the medication. This soreness should last no more than a few days.
- Headache – On rare occasions, the needle pierces the covering of the spinal cord, which can cause a headache that may last for a few days if left untreated.
- Decrease in blood pressure – The medication may lower your blood pressure, which may slow your baby’s heart rate. To make this less likely, you will be given extra fluids through a tube in your arm (IV line) and may need to lie on your side.
Women sometimes ask if an epidural can slow labor or lead to a cesarean delivery, also known as a C-section. There is no evidence that it does either.
- Spinal block: This can be used alone or in combination with an epidural, which is referred to as a combined spinal epidural (CSE). For this, an anesthesiologist provides medication through a needle inserted in the lower back into the spinal canal. The relief from pain is immediate and lasts from an hour and a half to three hours. You will be numb from your abdomen to your legs and feel no pain.
 A spinal block can be used for vaginal childbirth as well as for a planned C-section.
A spinal block can be used for vaginal childbirth as well as for a planned C-section. - Analgesics: These pain medications are delivered through an IV line into a vein or injected into a muscle. Analgesics can include bothopioid and non-opioid medications and temporarily relieve pain but do not eliminate it.
- General anesthesia: This is the only type of pain medication used during labor that makes you lose consciousness. With general anesthesia, you will not be awake for the birth of your baby. It works quickly and is typically used only if you need an emergency C-section or have another urgent medical problem (such as bleeding).
- Additional and complementary pain management methods: There are also ways to help you cope with labor pain without medication, or in combination with medication:
- Massage – Have your partner massage your back or feet.
- Breathing – Deep, slow breaths and grunting are two examples of the many different ways to breathe through the pain of a contraction.

- Visualization –You may find it helpful to picture yourself somewhere enjoyable, such as on a beach or walking through a forest.
- Water – Soak in a tub or take a shower to soothe some tension.
Nitrous oxide – Often referred to as “laughing gas,” this option had not traditionally been used in the U.S. for labor and delivery, but is becoming more common. It may help reduce anxiety, but does not eliminate pain. Nitrous oxide may potentially affect your breathing, decrease awareness and cause nausea, vomiting, and dizziness. More research is needed to determine how effective nitrous oxide is, potential complications it could cause, in addition to any possible long-term side effects for you or baby.
How can you ensure your safety before, during, and after labor?Thanks to the miracles of modern medicine, more women are giving birth in their late 30s and 40s. But older age and conditions such as diabetes, high blood pressure, and obesity increase the risk of complications for you and your baby. If you are an expectant mother, you should talk with your obstetrician and your anesthesiologist to develop a plan that ensures the safest possible pregnancy, childbirth, and recovery.
But older age and conditions such as diabetes, high blood pressure, and obesity increase the risk of complications for you and your baby. If you are an expectant mother, you should talk with your obstetrician and your anesthesiologist to develop a plan that ensures the safest possible pregnancy, childbirth, and recovery.
Share:
Here are some of the things you can do:
- Take care of yourself: If you are older, overweight, or have diabetes, high blood pressure, or other health conditions, work closely with your physicians to address your condition prior to labor and delivery so you understand all possible complications and have a plan. About halfway through your pregnancy, meet with your anesthesiologist, who will provide information to help keep you safe by developing an optimal labor, delivery, and recovery plan.
- Express your concerns: If you have had a bad experience with anesthesia or have any fears about childbirth, let your physicians know.
 Never brush off your concerns — if something doesn’t feel right, tell your obstetrician and anesthesiologist. Be sure to ask about other issues of possible concern, such as whether having a slipped disk or a lower back tattoo would prevent you from having an epidural.
Never brush off your concerns — if something doesn’t feel right, tell your obstetrician and anesthesiologist. Be sure to ask about other issues of possible concern, such as whether having a slipped disk or a lower back tattoo would prevent you from having an epidural. - Ask about an emergency plan. Your physicians will always prioritize your safety as well as your baby’s. But it’s important to know your hospital has an emergency plan in place. Anesthesiologists have extensive critical care training and are experts in treating emergencies such as postpartum hemorrhage (bleeding) and preeclampsia (high blood pressure).
- Know experts are working to improve care. Anesthesiologists are leading the way to develop protocols that improve safety during and after childbirth. Efforts include:
- “Safety bundles” and best practices for managing common causes of maternal death, including postpartum hemorrhage and high blood pressure, which can lead to preeclampsia and, if not treated, to seizures, coma, brain damage, blood clots, and death.

- Early warning systems that trigger an immediate evaluation if a mother’s health declines rapidly.
- Refinement of labor and delivery pain management techniques, including epidurals and spinal anesthesia, which has led to significant reductions in maternal deaths.
- Multi-disciplinary review committees at the state level to examine maternal deaths and identify the causes, determine preventability, and implement prevention efforts.
- “Safety bundles” and best practices for managing common causes of maternal death, including postpartum hemorrhage and high blood pressure, which can lead to preeclampsia and, if not treated, to seizures, coma, brain damage, blood clots, and death.
- Plan your pain management: Untreated post-delivery pain (after vaginal as well as C-section birth) can lead to post-traumatic stress disorder in some women, so don’t downplay your pain. Ask your obstetrician to reach out to your anesthesiologist if you have questions about how to manage pain after birth. Ask whether opioids are an option or should be avoided.
Anesthesiologists are committed to patient safety and high-quality care, and have the necessary knowledge to understand and treat the entire human body.
Childbirth - pain relief options
Actions for this page
Summary
Read the full fact sheet- Childbirth is usually a painful experience.
- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
Labour and childbirth is usually a painful experience and women vary in their response to it. Some women are keen to avoid drugs or other medical interventions while others are happy to consider all available options. For a woman having her first baby, the experience of labour (and her reaction to it) is unpredictable.
For this reason, it is a good idea to be aware of the options for pain relief that are available and to know something about the different methods. You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
Non-medical pain relief options for childbirth
Research suggests that adequate preparation can help to reduce pain or at least modify the perception of pain and reduce anxiety, which can help you to better cope with labour. There are several non-drug pain relief options:
- Being in good physical condition is important. Exercise gently and regularly throughout your pregnancy, avoid cigarettes and alcohol, and eat a healthy, balanced diet.
- Knowing what to expect during the various stages of labour can help reduce anxiety. Antenatal classes are strongly recommended.
- Breathing techniques may help you to ‘ride the waves’ of each contraction.
- Constant, close support from your partner (or a trusted friend or loved one) for the duration of labour can reduce anxiety.

- Using distractions like music can help to take your mind off the pain.
- Hot or cold packs, massage, a warm shower or immersion in a warm bath, and keeping active may all be helpful.
- Hypnosis, acupuncture and acupressure are areas in which there has been little research but these may be considered also.
Transcutaneous electrical nerve stimulation (TENS)
TENS is a technique in which nerves in the lower back are stimulated using a small hand-held device controlled by the woman. It has no known side effects for mother or baby and many women find it helpful either alone or in combination with other methods of pain relief.
Medical pain relief options for childbirth
The three main medical pain-relieving options for labour include:
- Nitrous oxide
- Pethidine
- Epidural anaesthesia.
Nitrous oxide
Nitrous oxide, known as ‘laughing gas’, is mixed with oxygen and administered to the mother through a face mask or a tube held in the mouth. The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.
The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.
Nitrous oxide doesn’t stop the pain entirely, but takes the ‘edge’ off the intensity of each contraction. Many women prefer nitrous oxide because it allows them direct control – you can hold the mask yourself and take deep breaths whenever you feel the need.
Nitrous oxide doesn’t interfere with contractions and it doesn’t linger in either the woman’s or the baby’s body.
Possible problems with using nitrous oxide include:
- Nausea and vomiting
- Confusion and disorientation
- Claustrophobic sensations from the face mask
- Lack of pain relief – in some cases, nitrous oxide doesn’t offer any pain relief at all (this applies to around one-third of women).
Pethidine
Pethidine is a strong pain reliever (related to morphine and heroin), usually injected directly into a muscle in the buttock. It may also be administered intravenously (directly into a vein). Depending on various factors, the effect of pethidine can last anywhere from two to four hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Depending on various factors, the effect of pethidine can last anywhere from two to four hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Possible problems with pethidine for the mother include:
- Giddiness and nausea
- Disorientation and altered perception
- Respiratory depression (reduced breathing)
- Lack of pain relief, in some cases.
Possible problems with pethidine for the baby include:
- The unborn baby is exposed to the drug via the umbilical cord and may experience respiratory depression at birth, particularly if several doses are given or the baby delivers soon after a pethidine injection. This effect can be reversed by an injection given to the baby.
- The baby’s sucking reflex may also be depressed, as well as other normal reflexes. Debate persists over the effects of pethidine on newborns.
Epidural anaesthesia
Epidural injections are the most effective pain relief available. They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth. Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth. Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
Possible side effects and complications of epidural anaesthesia include:
- The anaesthesia may not be complete and you may still experience some pain. This may require the procedure to be repeated.
- After the epidural has been inserted, your blood pressure may drop, causing you to feel faint and nauseated. This may also cause stress to your baby. This is treated by giving intravenous fluid.
- An epidural often causes some muscle weakness in the legs, so women who have had an epidural anaesthetic may be confined to bed.
- The lack of sensation in the lower body means that you will not be able to tell when you need to urinate.
 A urinary catheter will be inserted in most cases.
A urinary catheter will be inserted in most cases. - Epidurals can lengthen the second stage of labour.
- The likelihood of having a normal vaginal delivery is reduced.
- If you are unable to push effectively, due to altered sensation and reduced muscle strength, the baby may have to be delivered by forceps or vacuum cup.
- Around one per cent of women experience headache immediately following the procedure.
- Some women experience itchiness after having an epidural. This can usually be effectively treated using antihistamines.
- Some women experience pain or tenderness where the epidural was injected.
- Around one in 550 women experience ongoing patches of numbness on the back near the injection site.
- Very rare complications include infection, blood clots and difficulty breathing.
An epidural does not:
- Increase the length of the first stage of labour
- Increase the likelihood of a caesarean section
- Cause long-term backache.
Where to get help
- Your doctor
- Obstetrician
- Midwife
Things to remember
- Childbirth is usually a painful experience.
- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
- Continuous support for women during childbirth, 2007, Cochrane Database of Systematic Reviews, Issue 2. More information here.
- Using water for pain relief during labour, 2007, The Royal Women’s Hospital, Melbourne.
- Epidural information, 2013, The Royal Women’s Hospital, Melbourne.
- Pain relief during labour and birth, Women’s and Children’s Health Network, Department of Health, South Australian Government.
 More information here.
More information here. - Epidural anaesthesia – side effects, 2011, NHS Choices, UK. More information here.
- Epidural anaesthesia, NHS, UK. More information here.
This page has been produced in consultation with and approved by:
This page has been produced in consultation with and approved by:
Give feedback about this page
Was this page helpful?
More information
Content disclaimer
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Reviewed on: 31-08-2014
Labor Pain: You can handle it!
For many expectant mothers, the pain that may be in childbirth is a real "sore topic". Wander from mouth to mouth "horror stories" of grandmothers and girlfriends. Meanwhile, these sensations are fundamentally different from pain during injuries, diseases and other unpleasant incidents. It is not enough to say that childbirth is a pleasant event, it is a holiday, it is a sacrament. And contractions and attempts are the way to the holiday. Just to make the holiday a success - you have to work hard. "Work", "work" is the period of contractions in English and French. Thinking of them as a difficult path to the joy of meeting a baby is the first step to not hurting. And the joyful acceptance of contractions is almost one hundred percent painkiller. But this is already a feat of maternal love.
"Work", "work" is the period of contractions in English and French. Thinking of them as a difficult path to the joy of meeting a baby is the first step to not hurting. And the joyful acceptance of contractions is almost one hundred percent painkiller. But this is already a feat of maternal love.
Childbirth is not painful or scary,
because there are many simple and natural pain relief methods. In our age, many means have been invented to facilitate any work, in any way. And in such a primordial human business as obstetrics, there are dozens of such methods, both ancient and modern.
Remember that there will be no task beyond your strength! There will be a job that suits you.
All people are different - and from everything that will be described here, you will definitely choose something of your own. You should think, try and take with you on the road what is useful for you. We will only make a reservation that only natural childbirth can be effectively anesthetized by natural methods, that is, those that are not "caused" artificially and go without medical interventions. Then, believe me, looking back immediately after giving birth, you will say: it was wonderful! But when will I give birth next time ...
Then, believe me, looking back immediately after giving birth, you will say: it was wonderful! But when will I give birth next time ...
Relaxation
The more relaxed you are during the contraction, the easier it will be for you to “work through” it, the better the cervix will open, releasing the baby. And this is the meaning of your work. Actually, your body will do the work, you just need to help yourself and your baby in the right way ... Everyone has their own way to relax: focusing on a visual or auditory image, breathing, posture, sound.
Concentration
From practice it is known that focusing on something helps to relax during a fight. You must choose for yourself individually what will be close to you. Some prefer to focus on what is happening inside: they imagine how the cervix opens, how the baby's head moves forward.
Visual images are closer to others: they imagine themselves in some beautiful and pleasant place (on the seashore, in the mountains) or imagine a fight in the form of an obstacle that must be overcome (for example, in the form of a big wave). Sometimes it is convenient for a woman to focus her eyes on a certain object or follow a line with her eyes in the course of a fight.
Sometimes it is convenient for a woman to focus her eyes on a certain object or follow a line with her eyes in the course of a fight.
There are people who find it easier to focus on a sound, whether produced by themselves or heard from outside. It can be music, the voice of a husband or a midwife, the sound of the sea or rain. Sometimes it's easier to focus on the tactile sensation: massages, firm pressure, and even hugs can help distract and relax. You can focus on a short prayer, verse, phrase, as well as on a certain rhythmic movement - which is closer to whom.
Breathing and sound
Instinctively holding one's breath and straining is a natural human response to a disturbing stimulus. We will do the opposite - breathe evenly and calmly. And surprisingly, the irritant will bother us less!
- Long exhalation. A deep, calm breath in through the nose and a long, calm (not forced!) exhalation through the mouth. To make the exhalation longer, you can fold your “lips into a tube”, as if blowing on a flame.

- Intermittent exhalation. A deep, calm breath in and a long, interrupted exhalation that sounds like "poo-poo-poo-poo ...".
- "Engine". You shortly inhale and exhale, while the sounds are similar to how a steam locomotive puffs.
- "Dog breath". Frequent short breathing: this is how a dog breathes in the heat. This breathing helps to prevent pushing too early or to hold it back (preventing ruptures).
Sounds. It is much easier for many to “sound” in a fight than to remain silent. This is by no means a cry, but lingering sounds of different heights on the exhalation. From the outside it looks like a primitive song. You need to choose the height of the sound for yourself individually.
Movement and various postures
Movement. Usually, immobility and the supine position are the least comfortable during contractions. Hence the main advice: find your posture and move! In addition to anesthesia, the movement contributes to the correct insertion of the baby's head at the exit from the small pelvis. Between contractions, you can walk around, and if the contractions are weak and rare, then you need to walk quite quickly - this gives mild stimulation. Movements resembling the rotation of a hoop around the waist or an oriental dance work wonderfully.
Between contractions, you can walk around, and if the contractions are weak and rare, then you need to walk quite quickly - this gives mild stimulation. Movements resembling the rotation of a hoop around the waist or an oriental dance work wonderfully.
The following positions are good during contractions:
- Standing posture, leaning forward. This position is very convenient if you walk during contractions. You stop where the fight caught you and, leaning on a table or wall, "work through" the fight.
- "Pose of a cat" or position on all fours. Remember how old Hank carried the Chief of the Redskins on his back when they played Indians. The pose is convenient in the active phase of contractions, when it is no longer possible to walk.
- "Child's Pose" is similar to the previous one, the difference is that the arms are bent at the elbows and the head is low. Your baby is in the same position in the womb. Pillows can be placed on the sides for comfort.
 In this position, it is good to both “work through” contractions and rest between them.
In this position, it is good to both “work through” contractions and rest between them. - Side lying position. Also good for contractions and relaxation. For convenience, the upper leg, bent at the knee, can be placed on a large pillow.
- Hanging position. Sometimes, during contractions, it is comfortable for mommy to hang: on the sports complex or in a squatting position, leaning on her husband supporting her from behind. The meaning of the hanging position is to relax the lower body, which softens the sensations. In addition, the force of gravity helps the child move from the inside out.
Stroking, massage, pressure
Most women enjoy being touched during contractions. The sacrum is the area where the nerves leading to the uterus come from. If you look closely at the lower back, you will see a rhombus, which is formed by the muscles of the back and buttocks. Often, stroking from top to bottom, or vigorous rubbing at points on the sides of the rhombus, significantly changes the sensations. For some, just applying firm pressure to the area helps. A woman can do a massage with her own hands only at the initial stage of childbirth, in the future it sometimes has to be done by her husband or someone who helps in childbirth.
For some, just applying firm pressure to the area helps. A woman can do a massage with her own hands only at the initial stage of childbirth, in the future it sometimes has to be done by her husband or someone who helps in childbirth.
Heat and cold
- Hot compress. Try to apply a hot compress from a towel folded several times to the sacrum area during a contraction. You can add a few drops of lavender essential oil to the water.
- Heating pad. This is dry heat on the sacrum. Very convenient electric heating pad with adjustable heat. Sometimes a mother is pleased when heat is applied not to the sacrum, but to the stomach, groin or perineum.
- Ice. All people are different: in rare cases, not heat, but ice should be applied to the sacrum (sliced frozen vegetables usually act as ice - they easily take the shape of the body). However, at the same time, the mother as a whole should be warm.
Water
Water has a wonderful analgesic and relaxing effect.
- Warm shower. Once you are comfortable and relaxed, direct the shower jet to where you feel most comfortable. The shower gives local warmth and light massage.
- Pool. Contractions are greatly facilitated by immersion in water. It is enough just to sit comfortably in the pool or bath, relaxing well. If the contractions are very strong - some mothers dive under the water and find that it is an excellent pain reliever. If you add 5-6 drops of verbena essential oil diluted in milk or yogurt to the water, the analgesic effect will increase, and the air around the mother will be filled with a delicate and wonderful aroma (be careful if the mother is prone to allergies!).
Aromatic oils
Verbena and lavender oils have already been mentioned above, which are used for water procedures. They also work great as a relaxing and analgesic, if you rub a drop in your palms and inhale the vapors, as well as if you use an aroma lamp. Allergy sufferers should test with a very small amount of oil and observe their reaction.
Homeopathy
This is the science that says that the symptoms are the language of the human body, in which he speaks what specific remedy he needs in a given situation. Therefore, according to a vivid picture of symptoms, even a person who is superficially familiar with homeopathy can successfully prescribe a harmless and very effective medicine. Here are the "pictures" (look closely!).
- Caulophyllum 30. Sharply painful contractions that occur in the lower abdomen. Despite this, the midwife or doctor says that the cervix does not dilate. Mom feels tired, trembling, thirsty.
- Cimicifuga 30. Also, during contractions, sharply painful sensations in the lower part of the abdomen, they "jump" from place to place. He talks a lot and rather randomly, "jumps". Mom is full of fears and forebodings (in fact, often such women have a difficult past experience of pregnancy and childbirth, failures in married life). Her deepest feeling is "I can't!".
- Gelsemin 30.
 Feeling of trembling and tiredness, eyes literally closing. Trembling in the fight. The cervix does not open. Internal tension, bad forebodings.
Feeling of trembling and tiredness, eyes literally closing. Trembling in the fight. The cervix does not open. Internal tension, bad forebodings. - Coffea 30. Contractions seem unbearable. Sharp emotional arousal, as if drinking coffee.
- Hamomilla 30. Contractions seem unbearable. Extremely sensitive and misbehaving. Screaming, cursing and bickering. Sensation of heat, flushed face.
- Pulsatilla 30. The main indications for this remedy are tearfulness, self-doubt, need for comfort and support. Does not tolerate stuffiness. The contractions are sluggish and weak in this remedy. Its use will avoid harsh drug stimulation leading to painful contractions.
- Arnika 30. Mom doesn't want to be touched: she claims that she's all right and sends everyone away. Feeling of muscle weakness and soreness. In childbirth relieves fatigue, prevents bleeding. After childbirth - accelerates recovery.
These drugs are freely sold in homeopathic pharmacies.
How to use the medicine: Take 3 grains and observe your reaction. If there are changes for the better, it is not necessary to repeat the reception while the improvement lasts. Take again if symptoms return. Choose another medicine if there is no effect. It is reasonable to visit a homeopathic doctor at the end of pregnancy, who, after talking with you individually, will select such medicines for childbirth that will be useful for you, and will also prescribe prophylactic agents to make childbirth easier.
Listen to your body
Take it on faith: you know how to give birth (this has been encoded in the genes of every cell of your body since ancient times) and you know exactly what you and your baby need to make childbirth easier and better. You just need to understand your own body language. The famous Canadian midwife Gloria Lemay finds it useful to look at childbirth as a excretory process, like other excretory processes: coughing, stool, crying. “They don’t need a mind - they require a different state. Each person is able to carry out his excretory processes without special instructions from his neighbors ...,” she writes.
Each person is able to carry out his excretory processes without special instructions from his neighbors ...,” she writes.
But all people are different. Many give birth on their own, many need help (even in finding themselves). If you are not one of those who know with their inner instinct what to do, take courses for expectant mothers. If you are not one of those who finds the strength to give birth completely on their own, find good helpers.
Traditional midwives know many other ways to make childbirth easier. Moreover, experience allows them to see what is best for you. Find such assistants who, having all the necessary professional knowledge and experience, would have the wisdom to respect your opinion, follow the nature of your body and not interfere with natural processes unless absolutely necessary.
Veronica Maslova, family doctor, homeopath
Anti-inflammatory drugs for pain relief in the perineum after childbirth
This translation is out of date. Please click here for the latest English version of this review.
Please click here for the latest English version of this review.
What is the problem (question)?
After giving birth, many women experience pain in the perineum, the area between the anus and the vagina. This Cochrane review addresses the question of whether this pain can be relieved with a single dose of a non-steroidal anti-inflammatory drug (NSAID) such as aspirin or ibuprofen.
Why is this important?
Some women experience particularly severe pain in the perineum after childbirth if the perineum ruptures during childbirth or an incision is required (a procedure known as an episiotomy). Even women who give birth without a perineal tear or surgery often experience some discomfort in the perineal area, which can affect a woman's activity as well as her ability to care for a baby. This review is part of a series of reviews looking at the effectiveness of various pain relief medications for perineal pain immediately after childbirth. This review looked at NSAIDs such as aspirin and ibuprofen.
This review looked at NSAIDs such as aspirin and ibuprofen.
What evidence did we find?
We found 28 studies involving 4181 women that studied 13 different NSAIDs (aspirin, ibuprofen, etc.). We included studies up to 31 March 2016. The studies we found only included women who had suffered perineal injuries and were not breastfeeding. Studies were conducted between 1967 and 2013 and were small and of low quality.
Studies have shown that a single dose of NSAIDs provides greater pain relief when assessed 4 hours (low-quality evidence) or 6 hours (very low-quality evidence) after administration, compared with placebo (a pill that mimics a drug) or no treatment in lactating women who have suffered trauma to the perineum during childbirth. Women who received single doses of NSAIDs also needed less additional pain relief 4 hours (low-quality evidence) or 6 hours (low-quality evidence) after their initial dose compared with women who took placebo or received no treatment.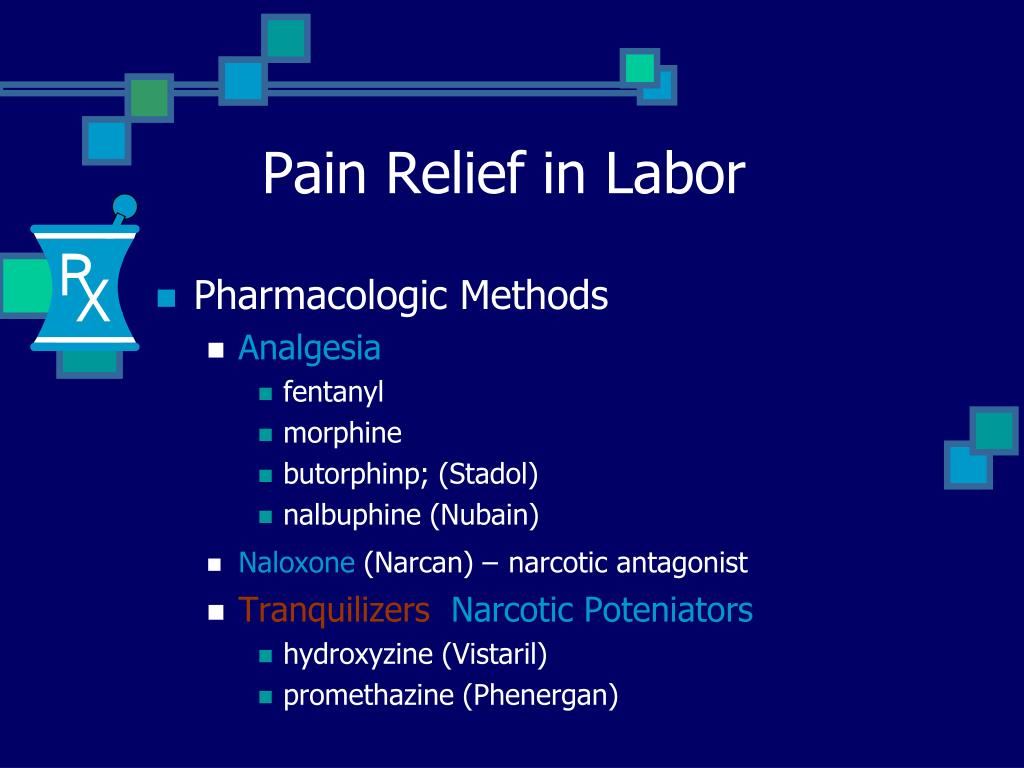 Not all studies assessed the adverse effects of the intervention, but some reported adverse effects in mothers such as drowsiness, headache, weakness, nausea, and stomach discomfort. However, there was no clear difference in the incidence of adverse effects 6 hours after drug administration between the groups (very low-quality evidence). One small study reported no adverse effects in mothers 4 hours after drug administration (low-quality evidence). None of the studies assessed possible adverse effects in children.
Not all studies assessed the adverse effects of the intervention, but some reported adverse effects in mothers such as drowsiness, headache, weakness, nausea, and stomach discomfort. However, there was no clear difference in the incidence of adverse effects 6 hours after drug administration between the groups (very low-quality evidence). One small study reported no adverse effects in mothers 4 hours after drug administration (low-quality evidence). None of the studies assessed possible adverse effects in children.
NSAIDs also appeared to be better than paracetamol in relieving pain when assessed 4 hours (but not 6 hours) after drug administration, although such a comparison was made only in three small studies. Women who received a single dose of NSAIDs also needed less additional pain relief 6 hours (but not 4 hours) after taking the medication, compared with women who received paracetamol. There were no adverse effects in mothers 4 hours after taking the drug (according to one small study). Three small studies reported adverse effects in mothers assessed 6 hours after drug administration, but there were no clear differences between the groups. No adverse effects were reported in children in any of the included studies. Breastfeeding women were also excluded from all studies.
Three small studies reported adverse effects in mothers assessed 6 hours after drug administration, but there were no clear differences between the groups. No adverse effects were reported in children in any of the included studies. Breastfeeding women were also excluded from all studies.
Comparisons of different NSAIDs and different doses of the same NSAID did not show any clear difference in their efficacy for the main outcomes assessed in this review. However, there were few data available for some NSAIDs.
None of the included studies reported any of the secondary outcomes considered in this review, including: increased length of stay or readmissions for perineal pain; breastfeeding, perineal pain 6 weeks postpartum, women's opinion, postpartum depression, and disability due to perineal pain.
What does this mean?
In non-breastfeeding women, a single dose of NSAIDs may relieve perineal pain when assessed 4 and 6 hours after drug administration.