Keratosis pilaris pregnancy
Your skin during pregnancy: a guide to all the lumps and bumps other than your belly
- Home
- Blog
- Skin Care
- Your skin during pregnancy: a guide to all the lumps and bumps other than your belly
Published on Feb 5th, 2019 by Robin Travers
Congratulations, mommy-to-be! You most likely have stacks of books at your bedside describing the fascinating changes your body will undergo on this 40-week journey. Yet few will offer details about some of the most glaringly obvious changes that will face you in the mirror: on your skin! Pregnancy-related hormone changes can induce new bumps and spots to appear on your skin, or may also alter pre-existing skin conditions. Use the following guide to help decipher these changes and learn how to treat and prevent them.
Acne
Some women find their acne actually improves during pregnancy. If you are among the unluckier women who were prone to breakouts before your menstrual cycle pre- pregnancy, then you may find that your acne will worsen as pregnancy related hormones cause your sebaceous glands to secrete more oil. Many prescription acne medications are unsafe during pregnancy, but there are some strategies that may help you fend off these breakouts.
Doctor’s Orders: Use gentle soapless cleansers, such as Cetaphil Cleanser, twice daily, and resist the urge to scrub or use astringents frequently. These will merely irritate your sensitive skin. Use non-comedogenic facial moisturizers if needed, such as Neutrogena facial moisturizers. If your inflammatory acne persists, your dermatologist can prescribe topical medications that may be safely used during pregnancy.
Melasma
Almost 70% of pregnant women experience the “mask of pregnancy”, or melasma, which appears as mottled brown pigmentation on the forehead, cheeks, and upper lip. Elevated levels of estrogen, progesterone and melanocyte stimulating hormone during pregnancy work together to produce this increased pigment in response to sun exposure. Melasma often subsides after delivery, but in some cases can be persistent.
Doctor’s Orders: Ultraviolet light exposure worsens melasma. Use a broad-spectrum, high-spf sunscreen, such as Aveeno Positively Radiant spf 30 Daily Moisturizer. Applying this on a daily basis, even on cloudy or wintery days, may prevent or lessen this pigmentation. Your dermatologist may prescribe a combination of tretinoin, hydroquinone and topical steroids to treat persistent post-partum melasma.
Itchiness and Rashes
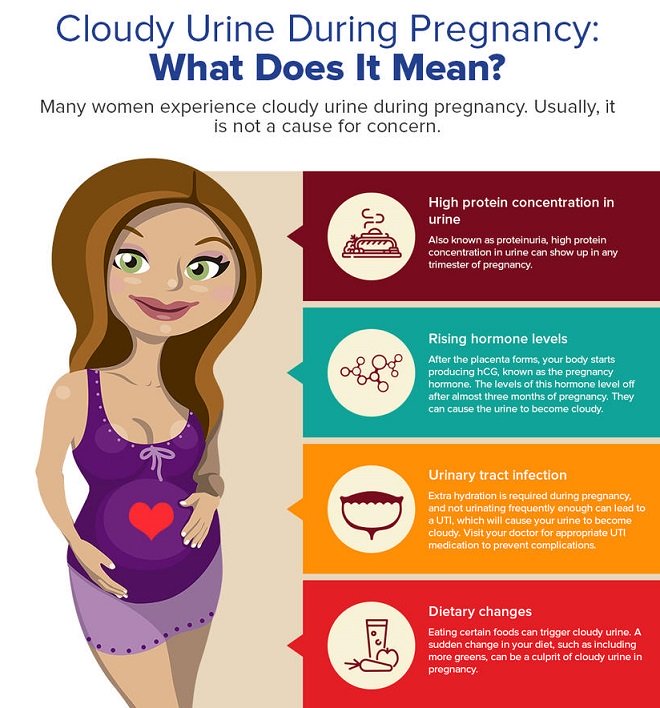
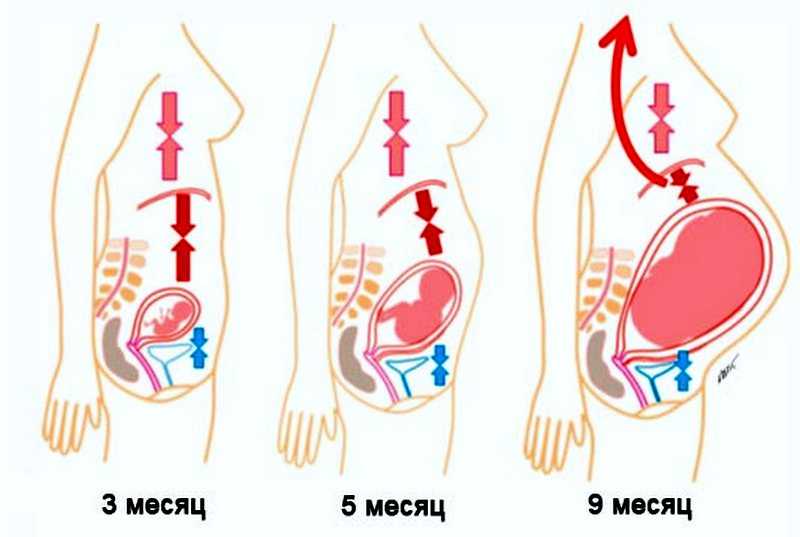
As your belly and breasts enlarge during the second and third trimester, your skin may become itchier. Pregnancy-related hormones may also trigger increased sweating, which can cause heat rash or irritation in the skin creases. You may notice small, itchy bumps around the hair follicles on your upper arms: this benign condition, called keratosis pilaris (KP), is often worsened or triggered during pregnancy. Rarely, women in their third trimester can develop an itchy, hive-like rash on their abdomen. Called pruritic, urticarial papules and plaques of pregnancy (or PUPPP), this rash can produce maddening itching for women in late pregnancy.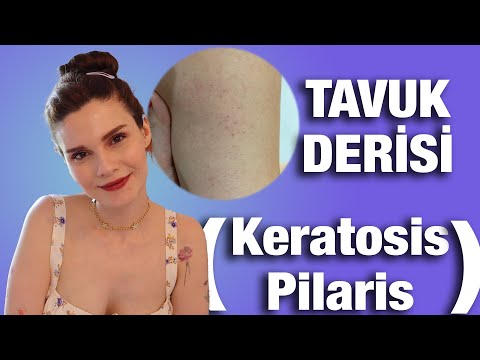
Doctor’s Orders: Hydrate your skin at every opportunity, particularly immediately after your shower. Cerave Lotion is particularly good at restoring your skin’s barrier function, and Am-Lactin Cream (which may be ordered by your pharmacist) can work wonders at smoothing KP. Speaking of showers: use the least amount of soap possible! Even so-called moisturizing bars can prove irritating. If your itching persists, contact your dermatologist, who may prescribe anti-inflammatory lotions or creams that are safe during pregnancy.
Stretch Marks
These dreaded pink, red, or brown depressed streaks can appear on your belly, buttocks, thighs, hips and breasts. The straight truth is that there is no way to prevent stretch marks during pregnancy. If you are genetically predisposed to develop them, they will appear.
Doctor’s Orders: Enjoy your pregnancy and motherhood. We know of no treatments that are medically proven to diminish stretch marks. If your stretching skin is itchy, then by all means apply an emollient. Rest assured that most stretch marks fade into faint, silvery lines post-partum. After delivery, your dermatologist may be able to treat resistant marks with tretinoin cream or a pulsed dye laser.
If your stretching skin is itchy, then by all means apply an emollient. Rest assured that most stretch marks fade into faint, silvery lines post-partum. After delivery, your dermatologist may be able to treat resistant marks with tretinoin cream or a pulsed dye laser.
Hair Loss
Your hair, which grew so lush and thick during pregnancy, is now falling out! You have a lovely 3 month-old infant at home, but are despairing at your hair shedding, which is called telogen effluvium. The hormonal changes of pregnancy and delivery trigger a shift of your growing hairs into the resting, or telogen, phase. 1-3 months later, these hairs are normally shed.
Doctors Orders: Never fear! Your hairs are normal, they are simply resting. After they have shed, they will most likely go back into their normal growth phase and will regrow. In the unlikely event that your hair loss persists beyond 6 months, a dermatologist may be able to evaluate and treat other causes of hair shedding.
Changing Moles
Pregnancy-related hormones can cause skin darkening, particularly along the linea nigra, the areola, and any freckles. Occasionally, moles will also enlarge and change with pregnancy. Although most of these changing moles will be benign, they should be evaluated by a dermatologist to ensure that they have not evolved into melanoma, a dangerous and potentially deadly form of skin cancer among young women.
Doctor’s Orders: Any changing mole during pregnancy should be evaluated by your dermatologist to be certain that it is benign. Some enlarging moles that become irritated along the neck or under the arms can be easily removed in your dermatologist’s office to help you feel more comfortable as your pregnancy progresses.
Sign Up for Our Blog
Keep up on the latest medical treatments and cosmetic dermatology services.
Request a Consultation
What Our Patients Are Saying
"The staff at SkinCare Physicians is highly professional and informative. I like to think of them as my SkinCare consultants."
I like to think of them as my SkinCare consultants."
AW, Natick, MA
"Excellent Greetings – Personal phone calls for reminders and listening professionals plus my medical problem is resolved after 40 years."
RF, Brockton, MA
"I really enjoy and appreciate the doctors and Dr. Kim’s kindness. She has helped me out so much. I would recommend this office any day."
MC, Canton, MA
"Dr. Phillips is a SUPERB physician! She kept us informed in a timely manner and follow-up was excellent."
AN
"The staff is always pleasant and takes good care of the clients. Dr. Sobell is always upbeat and encouraging."
PT, Blackstone, MA
"Dr. Kaminer is a genius. My ears are perfect like brand new. Thanks so much."
PA, Cambridge, MA
Unilateral Generalized Keratosis Pilaris Following Pregnancy
Article
By
Author and Disclosure Information
Keratosis pilaris (KP) is a common inherited disorder characterized by small folliculocentric keratotic papules that may have surrounding erythema, which gives the skin a stippled appearance resembling gooseflesh. The extensor surfaces of the upper arms, thighs, and buttocks commonly are affected, but a generalized presentation may occur. We report the case of a 29-year-old woman with unilateral generalized KP in the second month of her second pregnancy. Both a genetic mutation and pregnancy-induced hormonal changes played possible roles in the development and progress of unilateral generalized KP in this patient.
The extensor surfaces of the upper arms, thighs, and buttocks commonly are affected, but a generalized presentation may occur. We report the case of a 29-year-old woman with unilateral generalized KP in the second month of her second pregnancy. Both a genetic mutation and pregnancy-induced hormonal changes played possible roles in the development and progress of unilateral generalized KP in this patient.
Practice Points
- Keratosis pilaris (KP) is a common disorder, with a genetic background and hormonal changes playing possible roles in its development. It also may be associated with a number of diseases.
- The skin lesions of KP usually are bilaterally distributed, either in a generalized or localized distribution. Unilateral lesions are rare. The underlying mechanism of unilateral generalized KP remains unknown.
References
1. Hwang S, Schwartz RA. Keratosis pilaris: a common follicular hyperkeratosis. Cutis. 2008;82:177-180.
2. Odom RB, James WD, Berger TG. Andrews’ Diseases of the Skin. 9th ed. Philadelphia, PA: WB Saunders; 2000.
3. Jackson JB, Touma SC, Norton AB. Keratosis pilaris in pregnancy: an unrecognized dematosis of pregnancy? W V Med J. 2004;100:26-28.
4. Poskitt L, Wilkinson JD. Natural history of keratosis pilaris. Br J Dermatol. 1994;130:711-713.
5. Griffiths WAD, Judge MR, Leigh IM. Disorders of keratinisation. In: Champion RH, Burton JL, Burns DA, et al, eds. Textbook of Dermatology. 6th ed. Oxford, MA: Blackwell Scientific; 1998.
6. Nico MM, Valente NY, Sotto MN. Folliculitis ulerythematosa reticulata (atrophoderma vermiculata): early detection of a case with unilateral lesions. Pediatr Dermatol. 1998;15:285-286.
7. Ehsani A, Namazi MR, Barikbin B, et al. Unilaterally generalized keratosis pilaris. J Eur Acad Dermatol Venereol. 2003;17:361-362.
8. Barth JH, Wojnarowska F, Dawber RP. Is keratosis pilaris another androgen-dependent dermatosis? Clin Exp Dermatol. 1988;13:240-241.
1988;13:240-241.
Keratosis pilaris (KP), also known as lichen planopilaris, is a common inherited disorder characterized by the presence of small folliculocentric keratotic papules that may have surrounding erythema, which gives the skin a stippled appearance resembling gooseflesh.1 Keratosis pilaris has a predilection for the extensor surfaces of the upper arms, thighs, and buttocks; however, a generalized presentation may occur.1-3 Patients usually are asymptomatic with concerns regarding cosmetic appearance. A number of diseases are associated with KP, such as KP atrophicans, erythromelanosis follicularis faciei et colli, and ichthyosis vulgaris. Treatment of KP mainly focuses on avoiding skin dryness and adding keratolytic agents when necessary.1 We report the case of a 29-year-old woman who presented with unilateral generalized KP in the second month of her second pregnancy.
Case Report
A 29-year-old woman presented in the second month of pregnancy with follicular hyperkeratotic papules on the right side of the face, neck, trunk, buttocks, arms, and legs with mild pruritus (Figure 1). According to the patient, when she found out she was pregnant, she discovered several reddish gray papules on the right cheek and dorsal aspect of the right hand that rapidly spread to the neck and trunk but remained restricted to the right side of the body. She occasionally experienced mild pruritus.
According to the patient, when she found out she was pregnant, she discovered several reddish gray papules on the right cheek and dorsal aspect of the right hand that rapidly spread to the neck and trunk but remained restricted to the right side of the body. She occasionally experienced mild pruritus.
Figure 1. Several reddish gray follicular papules formed red patches on the right side of the face (A). Numerous small hyperpigmented follicular papules were scattered on the right side of the neck; the left side was devoid of lesions, revealing a sharp distinct demarcation line between the involved and uninvolved skin (B). Reddish gray or pigmented lesions were distributed on the hands and thighs but were restricted to the right side (C and D). | |
Physical examination revealed numerous small reddish or hyperpigmented follicular papules scattered on the right side of the body, both in the flexor and extensor aspects. The distribution of the lesions did not follow the lines of Blaschko. Strangely, the left side was devoid of lesions, and a sharp distinct line of demarcation separated the involved and uninvolved sides. Physical examination of the scalp, hair, nails, and oral cavity was normal with no atrophy or scarring. The patient’s first pregnancy was aborted in the third month of pregnancy (14 months prior to presentation), but no skin lesions were reported at that time. The patient’s medical history was otherwise unremarkable, and there was no known family history of similar skin lesions. Histopathologic examination of a biopsy taken from a lesion on the right side of the neck showed hyperpigmentation of the basal layer, follicular and interfollicular hyperkeratosis, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration (Figure 2).
The distribution of the lesions did not follow the lines of Blaschko. Strangely, the left side was devoid of lesions, and a sharp distinct line of demarcation separated the involved and uninvolved sides. Physical examination of the scalp, hair, nails, and oral cavity was normal with no atrophy or scarring. The patient’s first pregnancy was aborted in the third month of pregnancy (14 months prior to presentation), but no skin lesions were reported at that time. The patient’s medical history was otherwise unremarkable, and there was no known family history of similar skin lesions. Histopathologic examination of a biopsy taken from a lesion on the right side of the neck showed hyperpigmentation of the basal layer, follicular and interfollicular hyperkeratosis, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration (Figure 2).
Based on the clinical and pathologic findings, a diagnosis of unilateral generalized KP was made. No treatment was administered due to the pregnancy. The patient’s skin condition continued to worsen throughout her pregnancy with more widespread and hyperpigmented lesions, but they remained unilateral. The patient showed no obvious improvement 4 months following delivery, and no treatment was administered because the patient was breastfeeding.
No treatment was administered due to the pregnancy. The patient’s skin condition continued to worsen throughout her pregnancy with more widespread and hyperpigmented lesions, but they remained unilateral. The patient showed no obvious improvement 4 months following delivery, and no treatment was administered because the patient was breastfeeding.
| Figure 2. Histopathologic examination revealed hyperpigmentation of the basal layer, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration, which suggested typical keratosis pilaris (A and B)(H&E, original magnifications ×40 [inset, original magnification ×100] and ×100). |
Comment
Keratosis pilaris is a common hyperkeratotic condition that typically presents as flesh-colored follicular papules surrounded by varying degrees of perifollicular erythema. Occasionally, inflammatory acneform pustules and papules may appear.1,2 Keratosis pilaris usually presents between the ages of 2 and 3 years, flourishes until 20 years of age, and usually subsides in adulthood.4 Xerotic or atopic individuals are prone to develop KP.2 Other conditions associated with KP include ichthyosis follicularis, atrichia with papular lesions, cardiofasciocutaneous syndrome, ectodermal dysplasia with corkscrew hairs, and keratitis-ichthyosis-deafness syndrome.5 Although its etiology is uncertain, KP is thought to be inherited in an autosomal-dominant fashion.
Occasionally, inflammatory acneform pustules and papules may appear.1,2 Keratosis pilaris usually presents between the ages of 2 and 3 years, flourishes until 20 years of age, and usually subsides in adulthood.4 Xerotic or atopic individuals are prone to develop KP.2 Other conditions associated with KP include ichthyosis follicularis, atrichia with papular lesions, cardiofasciocutaneous syndrome, ectodermal dysplasia with corkscrew hairs, and keratitis-ichthyosis-deafness syndrome.5 Although its etiology is uncertain, KP is thought to be inherited in an autosomal-dominant fashion.
Histologically, the lesions result from the formation of an orthokeratotic plug, which may contain twisted hairs, that blocks and dilates the orifice and upper portion of the follicular infundibulum. Mild perivascular mononuclear cell infiltrates usually are present in the adjacent dermis.5 Most cases of KP involve lesions that are bilaterally distributed.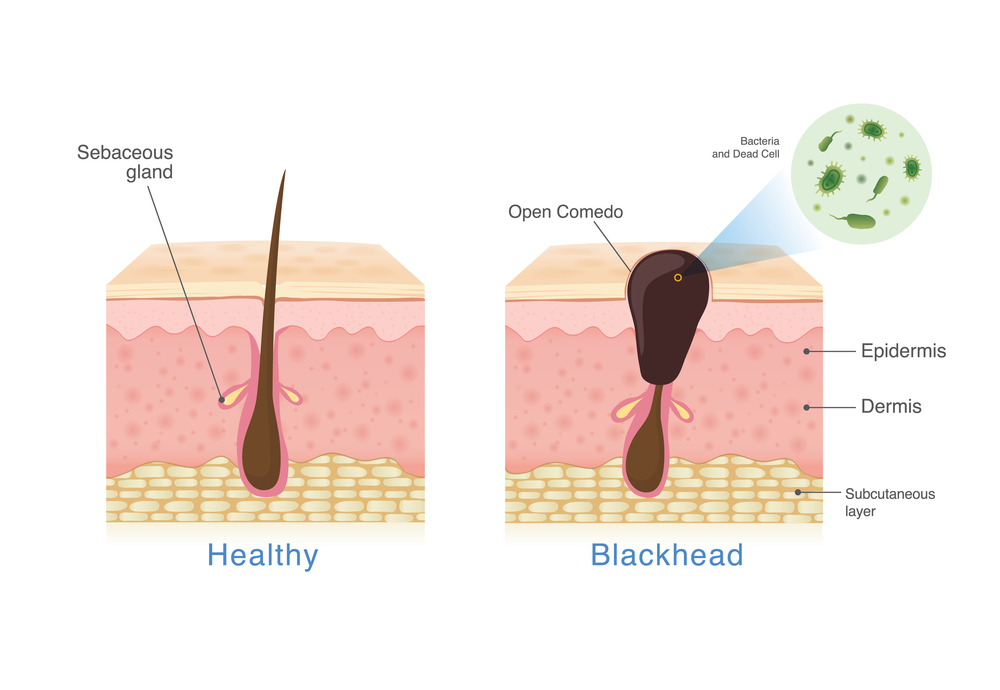 One report described a 5-year-old girl with lesions that were limited to the right cheek. They were diagnosed as atrophoderma vermiculata, a form of KP atrophicans, which is a less common variant of KP.6 Another report described a 2-year-old girl who developed KP 7 months after birth, which was the only case we found in the English-language literature, according to a PubMed search of articles indexed for MEDLINE using the search terms keratosis pilaris, hemicorporal, and pregnancy, with near-total involvement of one side of the body. The authors believed this peculiar manifestation was probably caused by an inherited segmental anomaly from a postzygotic genetic mutation.7
One report described a 5-year-old girl with lesions that were limited to the right cheek. They were diagnosed as atrophoderma vermiculata, a form of KP atrophicans, which is a less common variant of KP.6 Another report described a 2-year-old girl who developed KP 7 months after birth, which was the only case we found in the English-language literature, according to a PubMed search of articles indexed for MEDLINE using the search terms keratosis pilaris, hemicorporal, and pregnancy, with near-total involvement of one side of the body. The authors believed this peculiar manifestation was probably caused by an inherited segmental anomaly from a postzygotic genetic mutation.7
Pages
- 1
- 2
- last »
Recommended Reading
Dermabrasion Versus Tretinoin: The Stretch Mark Showdown
MDedge Dermatology
US Dermatology Residency Program Rankings
MDedge Dermatology
Granulomatous Changes Associated With Pigmented Purpuric Dermatosis
MDedge Dermatology
Some docs get another chance at 'meaningful use' hardship exemption
MDedge Dermatology
Industry payments to docs, hospitals top $4. 5 billion
5 billion
MDedge Dermatology
Related Articles
-
Original Research
- Author:
- Menter A
- Vamvakias G
- Jorizzo J
Actinic keratoses (AKs) are common in fair-skinned individuals with a history of chronic and excessive sun exposure and may progress to squamous...
-
Pediatric Dermatology
- Author:
- Hwang S
- Schwartz RA
Keratosis pilaris (KP) is a common inherited disorder of follicular hyperkeratosis. It is characterized by small, folliculocentric keratotic...
-
Case Letter
- Author:
- Jun-Hua Liu, MMS
- Di-Qing Luo, MMS
- Liang-Cai Wu, MMS
Acrokeratoelastoidosis (AKE) is a rare disease first described in 1953.

Follicular hyperkeratosis of the skin: symptoms, treatment, diagnosis of the disease
Follicular hyperkeratosis is a skin pathology, which consists in the formation of nodules of keratinized epidermis at the mouths of hair follicles. The skin on the affected areas becomes dry and rough, covered with numerous reddish nodules that resemble goose bumps. Most often, the disease affects the elbows and knees, the gluteal zones, and the outer surfaces of the thighs. It does not cause a deterioration in well-being, although it causes some discomfort due to a feeling of dry skin and dissatisfaction with one's appearance.
Types of disease
There are two types of follicular skin hyperkeratosis.
- Type I develops with a lack of vitamin A. It is characterized by increased dryness of the skin on the elbows, knees, extensor surfaces of the limbs and buttocks and the appearance of spiny nodules at the mouths of the hair follicles.

- Type II develops with a lack of vitamin C. Its difference is the dark color of the nodules that clog the mouths of the follicles, since they consist of blood or pigment. The outer thighs and abdomen are most commonly affected.
The disease can be congenital or acquired.
Symptoms
The main symptom of follicular hyperkeratosis is "goose bumps", which is accompanied by increased dryness and roughening of the skin in the affected areas. Horny nodules look like a small reddish or yellowish rash that appears on the arms and thighs, knees, buttocks, less often on other parts of the body. They are located at the base of the hair follicles with the formation of a small red rim around each horn element. Nodules and plaques do not exceed the size of a match head and can remain on the affected skin for many years. In some cases, manifestations of follicular hyperkeratosis appear on the face or on the scalp. The generalized form of the disease is characterized by extensive lesions of the skin on the trunk and extremities.
Reasons for the development of pathology
Normally, epithelial cells appear in the basal layer of the skin, fill with keratin and harden as they grow. As new cells appear, the old ones are almost imperceptibly exfoliated and leave the surface of the skin. The cell renewal cycle takes about two days.
If it is disturbed, old cells do not have time to fully mature and keratinize, therefore, when replaced by young cells, they do not exfoliate, but accumulate, increasing the thickness of the stratum corneum. In this case, the gaps of the hair follicles may be closed by a thickened layer of horny cells. The follicles become clogged, due to which the growth of new hairs is limited to the subcutaneous space. This is how follicular hyperkeratosis develops with acne or nodules on the affected areas of the skin.
In some cases, the disease is hereditary, but there are a number of reasons that trigger this mechanism. Among them:
- hormonal imbalance characteristic of adolescence and youth, or taking hormonal drugs;
- stress, increased emotional stress or high physical activity;
- malnutrition, hypovitaminosis or beriberi;
- winter period and associated irritation of the skin with layers of clothing.

The causes that cause acquired follicular hyperkeratosis, as a rule, are:
- lack of vitamins A, C, B, E and K;
- thyroid dysfunction;
- systemic diseases of the body;
- severe infectious diseases - tuberculosis, syphilis, HIV, etc.;
- violations of the development of connective tissue;
- traumatic external influences - chemical burns, radioactive radiation;
- tight and uncomfortable synthetic fiber clothing.
Follicular hyperkeratosis most often develops in children, adolescents and adolescence, but it also occurs in adults.
Diagnostic methods
Follicular hyperkeratosis, as a rule, does not require special diagnostic studies. An experienced dermatologist is usually quite satisfied with the results of an external examination and questioning the patient to determine the nature of the disease. In adolescents, cornification nodules can sometimes be confused with acne, but close examination reveals dryness and roughness of the skin, in contrast to the soft structure inherent in acne. In some cases, it may be necessary to make a differential diagnosis if the manifestations of follicular hyperkeratosis are similar to:
In some cases, it may be necessary to make a differential diagnosis if the manifestations of follicular hyperkeratosis are similar to:
- lichen erythematosus;
- pityriasis versicolor;
- Darier disease;
- follicular psoriasis;
- lenticular keratosis.
In these cases, a histological examination of the nodules is carried out in order to study the nature of the skin formations and determine the cause of their occurrence.
Treatment of pathology
Since the disease is chronic, the treatment of follicular hyperkeratosis of the skin continues for a long time. Often the patient has to deal with its manifestations throughout his life. Therapy, as a rule, is aimed at improving the condition of the skin, preventing skin infections and inflammatory processes. Quite often, a disease that began in childhood or adolescence regresses on its own with the onset of maturity, and its manifestations become less noticeable. However, the need for medical care remains.
However, the need for medical care remains.
An integrated approach to the treatment of follicular hyperkeratosis allows to achieve a significant improvement in skin condition. For this you need:
- normalize the diet, including a large amount of vegetables and fruits, fatty fish, lean meat;
- take drugs prescribed by a dermatologist - retinoids, vitamin complexes;
- regularly use external agents containing corticosteroids, salicylic acid, AHA acids, urea;
- in the presence of a fungal infection, use antifungal drugs;
- attend physiotherapy sessions - quartz treatment, laser therapy, photodynamic therapy and other prescribed procedures;
- take warm baths with salt, baking soda or starch.
The implementation of all the recommendations of the doctor allows you to achieve a long-term stable remission, getting rid of the manifestations of the disease for a long time.
Diagnostics and treatment of follicular hyperkeratosis in Moscow
Clinic "Medicina" offers an effective treatment of follicular hyperkeratosis in children, adolescents and adult patients. Benefit from the services of qualified dermatologists, as well as the widest range of the latest diagnostic and treatment equipment, to restore healthy and smooth skin. Make an appointment with a specialist online on our website or by phone. We are waiting for you any day of the week at a convenient time for you.
Benefit from the services of qualified dermatologists, as well as the widest range of the latest diagnostic and treatment equipment, to restore healthy and smooth skin. Make an appointment with a specialist online on our website or by phone. We are waiting for you any day of the week at a convenient time for you.
Questions and answers
Which doctor treats follicular hyperkeratosis?
For the diagnosis of follicular hyperkeratosis and subsequent treatment, consult a highly qualified dermatologist.
Why is follicular hyperkeratosis dangerous?
By itself, follicular hyperkeratosis is not a dangerous disease, but in some cases it is complicated by pustular skin infections, irritation and inflammation of the affected areas of the skin, as well as the development of eczema. In some, very rare cases, it is possible for the affected tissues to degenerate into malignant tumor cells.
Follicular hyperkeratosis: what helps from folk remedies?
Some traditional medicine recipes help soften the skin, reduce breakouts and relieve irritation. Most effective:
Most effective:
- aloe leaves kept in the refrigerator for several days, applied overnight to the affected area;
- gruel of grated raw potatoes or raw beets;
- bee propolis.
Crocker-Adamson spiny follicular keratosis in an 8-year-old patient
In a number of dermatoses, pathomorphological events occur predominantly in the epidermis, in particular, in dyskeratosis, in which cell keratinization is impaired. At the same time, in some cases, hyperkeratosis develops (significant thickening of the stratum corneum without structural changes in the cells), in others - keratosis (moderate thickening of the stratum corneum).
H. Crocker (1901) and H. Adamson (1905) described a keratosis characterized by the formation of follicular papules, in the central part of which vellus hairs were found, as well as spiny filiform horny processes. The authors called this dermatosis spiny follicular keratosis (SPK, lichen pilaris spinulusus ), which now bears their names [1–4]. SFC is associated with various factors: deficiency of vitamins, A and C, endo- and exogenous intoxications, and others. Lichen spinous is also associated with follicular keratosis, Siemens syndrome, frinoderma, multiple myeloma, Little-Lassuer syndrome, and other pathological conditions [2–6].
SFC is associated with various factors: deficiency of vitamins, A and C, endo- and exogenous intoxications, and others. Lichen spinous is also associated with follicular keratosis, Siemens syndrome, frinoderma, multiple myeloma, Little-Lassuer syndrome, and other pathological conditions [2–6].
The disease usually appears in childhood, more often in boys; with a frequency of one case per 200 patients with a dermatological profile [7]; inherited in an autosomal dominant manner. Clinically, CFC is manifested by many follicular horny nodules (often flesh-colored), which, grouped together, form rounded or irregularly shaped plaques, 2–3 cm in diameter [8–11], localized on the neck, chest, abdomen, thighs, buttocks , area of the shoulder girdle. Sometimes rashes appear against a background of mild erythema, but more often on normal skin. When holding the palm over the surface of the lesion, the feeling of a "grater" is determined. Subjectively, the disorders are absent or mild. The general condition is not disturbed [1, 6, 9, 12].
Although the course of the disease is long, the prognosis for recovery is favorable. The rash may spontaneously regress after a few months or years, more often this occurs during puberty [1, 9, 12].
Histologically, CFC is manifested by moderate hyperkeratosis with horny plugs in dilated follicle orifices, weak lymphocytic perifollicular infiltration [1, 6, 10, 12, 13].
The range of dermatoses for the differential diagnosis of CFC includes Devergy's tinea pilaris, follicular mucinosis, tinea pilaris, ichthyosis, lichenoid tuberculosis, trichophytosis, Doha squamous follicular keratosis. The diagnosis is usually clinical; in doubtful cases, a histological examination is used [3, 6, 10, 12].
In the treatment of dermatosis, vitamin A, aromatic retinoids, neotigazon, aevit, vitamins B 1 and C are used. Soap or soda baths, keratolytic ointments containing 1-3% salicylic acid, 5-10% sulfur, ointments with vitamin A are indicated , 2-3% resorcinol, cream with urea, ointments based on glucocorticosteroids, total ultraviolet irradiation [2, 5, 6, 12, 14].
We observed patient T ., 8 years old, who was admitted to the pediatric dermatovenerology department on December 15, 2015 with a presumptive diagnosis of lichen planus. For 4 years of illness, rashes were located on different parts of the skin. For the first time they appeared on the extensor surface of the area of the elbow joints in the form of limited slightly erythematous rough plaques. The reason for their occurrence remains unknown. A few months later, the process spread to the skin of the abdomen.
Outpatient treatment under the supervision of a dermatologist (antihistamines, external uniderm, cindol) was carried out with a short-term improvement. Despite two courses of treatment in August 2015, the pathological process progressed, the number of foci and their size increased. Further treatment included vitamin A 3300 IU 3 times a day for 1 month, externally - radevit ointment and advantan. After a short period of improvement, an exacerbation occurred again and the patient was sent for inpatient treatment to the Kolomensky branch.
Child from the third pregnancy, the third urgent physiological delivery. The neonatal period is normal, development by age. Past illnesses - SARS, chicken pox (2013), obstructive bronchitis, tonsillitis. Tuberculosis, oncological and mental diseases, diabetes mellitus was not. Heredity is not burdened. Vaccinated in accordance with the vaccination schedule. Lymph nodes are not palpable. Pulse 90 beats / min.
Status localis : chronic pathological process is widespread. The lesions have irregular rounded outlines and clear contours. Their components are multiple hyperkeratotic follicular papules the size of a pinhead flesh-colored. They do not merge with each other, they are located on a slightly erythematous background with increased dryness of the skin (see figure).
Clinical manifestations of spiny follicular keratosis in patient T., 8 years old. Lesions localized on the skin of the abdomen (a), thigh (b), shoulder and back (c), on the buttock (d).
When running the palm over the surface of the foci, a "grater symptom" is determined. Lesions are localized on the face, trunk, shoulder girdle, upper and lower extremities, buttocks; the foci are large, 10-15 cm in diameter. There is a slight hyperpigmentation of the eyelids and their pronounced folding. Dermographism is mixed. Nails and hair are not changed. Subjectively, the rash does not bother.
Clinical and biochemical analyzes of blood, urine within the age norm.
The results of the analysis of feces for eggs of helminths, protozoa, scrapings for enterobiz are negative.
Endocrinologist's consultation: no pathology detected.
Concomitant diseases: ultrasound picture of gallbladder deformation (kink in the body), chronic tonsillitis.
Hospital treatment included: aevit (1 capsule per day), externally 1% salicylic cream, 2% naftalan paste, general ultraviolet irradiation. Most of the lesions regressed within 2 weeks.