How long does miscarriage pain last
Treating miscarriage | The Royal Women's Hospital
If a miscarriage has begun, there is nothing that can be done to stop it. Any treatment you have will be aimed at avoiding heavy bleeding and infection.
A discussion with the doctor or nurse will help you to work out which treatment options are best and safest for you.
On this page:
- No treatment (expectant management)
- Treatment with medicine
- Surgical treatment (curette)
- Waiting for treatment
- After a miscarriage
No treatment (expectant management)
You can choose to wait and see what will happen. This is called 'expectant management'. If nothing is done, sooner or later the pregnancy tissue will pass naturally. If it is an incomplete miscarriage (where some but not all pregnancy tissue has passed) it will often happen within days, but for a missed miscarriage (where the fetus or embryo has stopped growing but no tissue has passed) it might take as long as three to four weeks.
While you are waiting you may have some spotting or bleeding, much like a period. When the pregnancy tissue passes, you are likely to have heavier bleeding with crampy, period-like pains. You can use sanitary pads and take pain relieving tablets, such as paracetamol.
If your miscarriage is incomplete, with just a small amount of pregnancy tissue remaining, it’s probably best to take a wait and see approach. But if there is heavy bleeding or signs of infection you will need treatment.
If the tissue does not pass naturally or you have signs of infection, the doctor will recommend a dilatation and curettage (D&C). You and the doctor can discuss and decide the preferred option for you.
Things to know
- There are many reasons why some women prefer to wait and see. It may feel more natural, it may help with the grieving process or it may give you more of a sense of control.
- Some women become worried or frightened when the bleeding gets heavier, especially if blood clots, tissue or even a recognisable embryo is passed.

- Usually, the wait and see approach takes longer than any other approaches such as surgery or medication. Sometimes bleeding can last for up to four weeks.
- Although excessive bleeding and blood transfusion are very rare, they are slightly more common with expectant management than with surgery.
- A few women still need to have surgery – sometimes urgently – if they develop infection, bleed heavily or if the tissue does not pass naturally.
- The waiting time can be emotionally draining for some women.
Treatment with medicine
Medicine is available that can speed up the process of passing the pregnancy tissue. For an incomplete miscarriage, the medicine will usually encourage the pregnancy tissue to pass within a few hours. At most it will happen within a day or two. For a missed miscarriage, it may happen quickly, but it can take up to two weeks and, occasionally, longer.
- Medication is not suitable if there is very heavy bleeding or signs of infection.
 It is usually not recommended for pregnancies that are older than about nine weeks.
It is usually not recommended for pregnancies that are older than about nine weeks. - If the tissue does not pass naturally, eventually your doctor will recommend a dilatation and curettage (D&C).
Things to know
- The pregnancy tissue will pass between four to six hours after taking the medicine, during which time you may be in hospital. After a few hours, if the pregnancy hasn’t passed, you may be sent home to wait. This will depend on where you are and which hospital you are in.
- The medicine has side effects which usually pass in a few hours but can be unpleasant, such as nausea, vomiting, diarrhoea, fever and chills. The tablets can be swallowed or dissolved under the tongue, or inserted in the vagina.
- After receiving the medication there may be some spotting or bleeding like a period. When the pregnancy tissue passes, you are likely to notice heavier bleeding and clots with strong cramping, period-like pains. You can use sanitary pads and take pain relieving tablets such as paracetamol.
- Some women may need stronger pain killers or a pain relieving injection.
- A few women still need to have surgery, sometimes urgently, if they develop infection, bleed heavily or if the tissue does not pass.
Surgical treatment (curette)
A D&C (or ‘curette’) is a minor operation. The full name is dilatation and curettage. It is done in an operating theatre, usually under general anaesthetic. There is no cutting involved because the surgery happens through the vagina. The cervix (neck of the uterus) is gently opened and the remaining pregnancy tissue is removed so that the uterus is empty. Usually the doctor is not able to see a recognisable embryo.
The actual procedure usually only takes five to ten minutes, but you will usually need to be in the hospital for around four to five hours. Most of this time will be spent waiting and recovering.
You may have to wait a day or two to have a curette and sometimes, while you are waiting, the pregnancy tissue will pass on its own. If this happens and all of the tissue is passed you may not need to have a curette.
If this happens and all of the tissue is passed you may not need to have a curette.
A curette is done in the following circumstances:
- You have heavy or persistent bleeding and/or pain.
- The medical staff advise that this is a better option for you; this may be because of the amount of tissue present, especially with a missed miscarriage.
- This is an option you prefer.
Things to know
The risks of a D&C are very low, but include:
- some pregnancy tissue remains in uterus. This can cause prolonged or heavy bleeding and the operation may need to be repeated
- infection needing antibiotics
- damage to the cervix or uterus. This is very rare (around 1 in 1000) and, when it does happen, it is usually a small hole or tear which will heal itself
- excessive bleeding (very rare)
- anaesthetic risks. These are very low for healthy women, but no anaesthetic or operation is without risk.
Waiting for treatment
If you have heavy bleeding with clots and crampy pain, it is likely that you are passing the pregnancy tissue. The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed. Sometimes the bleeding will continue to be heavy and you may need further treatment.
The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed. Sometimes the bleeding will continue to be heavy and you may need further treatment.
You should go to your nearest emergency department if you have:
- increased bleeding, for instance soaking two pads per hour and/or passing golf ball sized clots
- severe abdominal pain or shoulder pain
- fever or chills
- dizziness or fainting
- vaginal discharge that smells unpleasant
- diarrhoea or pain when you open your bowels.
What to do while you are waiting
- You can try to rest and relax at home.
- Usual activity that is not too strenuous will not be harmful. You can go to work if you feel up to it.
- If you have pain you can take paracetamol.
- If there is bleeding, use sanitary pads rather than tampons.
After a miscarriage
- It is usual to have pain and bleeding after a miscarriage.
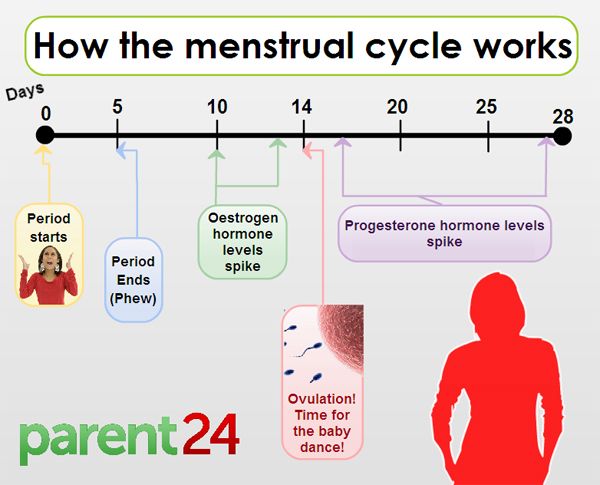
 It will feel similar to a period and will usually stop within two weeks. You can take ordinary painkillers for the pain. Your next period will usually come in four to six weeks after a miscarriage.
It will feel similar to a period and will usually stop within two weeks. You can take ordinary painkillers for the pain. Your next period will usually come in four to six weeks after a miscarriage. - See a doctor or attend a hospital emergency department if you have strong pain and bleeding (stronger than period pain), abnormal discharge, (especially if it is smelly), or fever. These symptoms may mean that you have an infection or that tissue has been left behind.
- Try and avoid vaginal sex until the bleeding stops and you feel comfortable.
- Use sanitary pads until the bleeding stops (do not use tampons).
- All contraceptive methods are safe after a miscarriage
- See a GP (local doctor) in four to six weeks for a check-up.
Anti-D injection after a miscarriage
It is important to have your blood group checked. If you’re RhD negative and the fetus is RhD positive this can cause problems for future pregnancies. This is because the fetus’s blood cells have RhD antigen attached to them, whereas yours do not. If small amounts of the fetus’s blood mixes with your blood, your immune system may perceive this difference in blood cells as a threat and produce antibodies to fight against the fetus’s blood. Once your body has made these antibodies they can’t be removed. This is unlikely to have caused your miscarriage and is more likely to affect future pregnancies. Women with a negative blood type usually need an Anti-D injection, which will stop the antibodies forming.
If small amounts of the fetus’s blood mixes with your blood, your immune system may perceive this difference in blood cells as a threat and produce antibodies to fight against the fetus’s blood. Once your body has made these antibodies they can’t be removed. This is unlikely to have caused your miscarriage and is more likely to affect future pregnancies. Women with a negative blood type usually need an Anti-D injection, which will stop the antibodies forming.
Future pregnancies after a miscarriage
One of the most common concerns following a miscarriage is that it might happen again. However, if you have had one miscarriage the next pregnancy will usually be normal.
If you do try for another pregnancy, try and avoid smoking, alcohol and excess caffeine as they increase the risk of miscarriage. It is recommended that all women take folic acid while trying to conceive, and continue until three months of pregnancy. In your next pregnancy you are encouraged to see your GP and have an ultrasound at about seven weeks. If ultrasound is done too early in pregnancy the findings are often uncertain and cause unnecessary worry.
If ultrasound is done too early in pregnancy the findings are often uncertain and cause unnecessary worry.
Feelings and reactions
There is no ‘right’ way to feel following a miscarriage. Some degree of grief is very common, even if the pregnancy wasn’t planned. Partners may react quite differently, just as people can respond differently to a continuing pregnancy. Feelings of loss may persist for some time and you may have mixed feelings about becoming pregnant again. Some friends and family may not understand the depth of emotion that can be attached to a pregnancy and may unreasonably expect for you to move on before you are ready.
Some couples decide that they want to try for a pregnancy straight away, while others need time to adjust to their loss. If you feel anxious about a possible loss in future pregnancies, you may find it helpful to talk to someone about this. If it’s difficult to speak with your friends and family about these issues, your doctor, community support group and counsellors can provide information and assistance.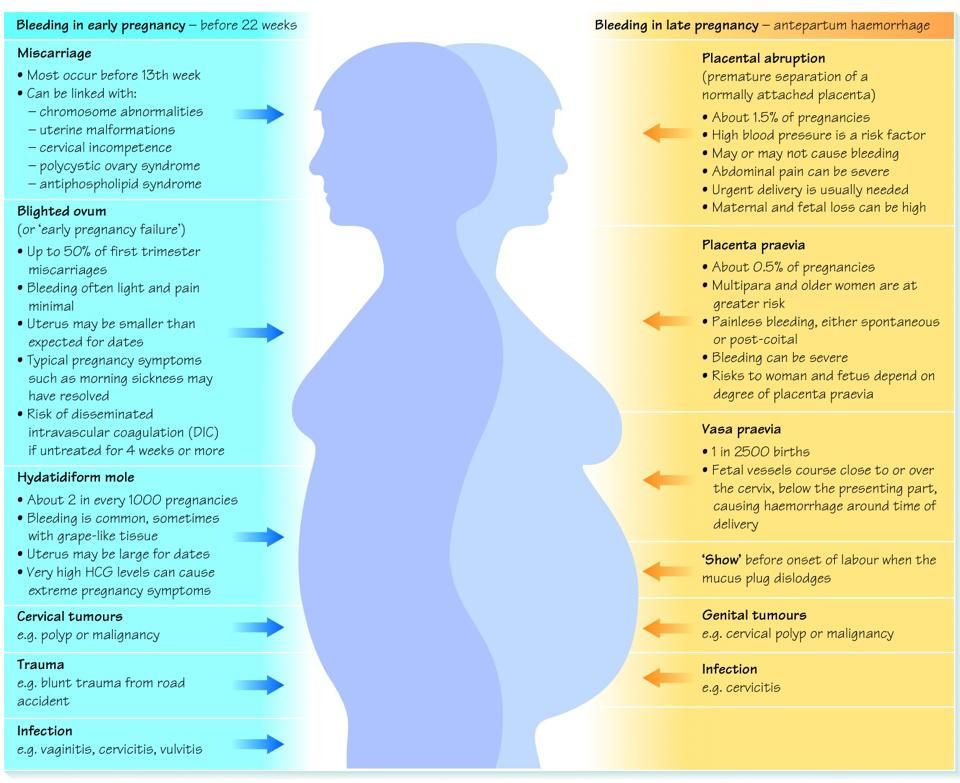
Related Health Topics
-
- Treatment for miscarriage
Treatment for miscarriage is aimed at avoiding heavy bleeding and infection. It is also aimed at looking after you, physically and emotionally.
-
- (English) PDF (302 KB)
- Treatment for miscarriage
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
How Long Does a Miscarriage Last?
How Long Does a Miscarriage Last?- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Holly Ernst, PA-C — By Valencia Higuera on June 13, 2018
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Overview
A miscarriage is the loss of a pregnancy before week 20. About 10 to 20 percent of pregnancies end in miscarriage, though the actual percentage is likely higher because some pregnancies are lost very early, before a woman realizes she is pregnant.
How long a miscarriage lasts can vary, depending on several factors. Read on to learn more about miscarriages.
Risks of having a miscarriage
The risk of a miscarriage increases with age. Women under age 35 have about a 15 percent chance of miscarriage. Women between the ages of 35 and 45 have a 20–35 percent chance.
If you become pregnant after the age of 45, your chance of miscarriage increases to 80 percent.
A miscarriage can happen to anyone, but the risk is higher if you’ve had prior miscarriages, have a chronic condition such as diabetes, or have uterine or cervical problems.
Other contributing factors include being:
- smoking
- alcohol abuse
- being underweight
- being overweight
How long does a miscarriage last?
If you experience a miscarriage before realizing you’re pregnant, you may think the bleeding and cramping are due to your menstrual cycle. So, some women have miscarriages and never realize it.
The length of a miscarriage differs for every woman, and it depends on different factors, including:
- how far along you are in the pregnancy
- whether you were carrying multiples
- how long it takes your body to expel the fetal tissue and placenta
A woman early in her pregnancy may have a miscarriage and only experience bleeding and cramping for a few hours. But another woman may have miscarriage bleeding for up to a week.
The bleeding can be heavy with clots, but it slowly tapers off over days before stopping, usually within two weeks.
Symptoms of a miscarriage
A miscarriage is the spontaneous loss of a fetus. Most miscarriages take place before week 12 of pregnancy.
Symptoms of a miscarriage may include:
- vaginal spotting or bleeding
- abdominal or pelvic pain
- cramping in the lower back
- fluid or discharge from the vagina
What are the causes of a miscarriage?
Miscarriages can be caused by many things. Some miscarriages occur because of abnormalities with a developing fetus, such as:
Some miscarriages occur because of abnormalities with a developing fetus, such as:
- blighted ovum
- molar pregnancy, a noncancerous tumor in the uterus that in rare cases develops into cancer
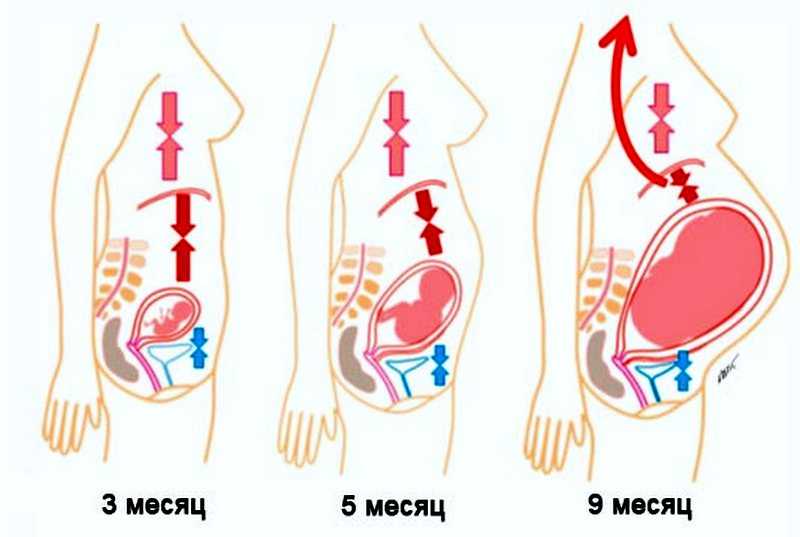
Chromosomal abnormalities caused by an abnormal egg or sperm account for about half of all miscarriages. Another potential cause is trauma to the stomach due to invasive procedures, such as chorionic villus sampling. Early in pregnancy, it would be unlikely that an accident or fall could result in miscarriage, since the uterus is so small and well protected within the bony pelvis.
Other causes include certain maternal diseases that put pregnancies at risk. Some miscarriages are unexplained with no cause known.
Daily activities do not typically cause a pregnancy loss. These include activities like exercise (once your doctor says it’s OK) and sex.
What to do if you have a miscarriage
If you think you’re having a miscarriage, seek medical help immediately. Any vaginal bleeding or pelvic pain should be evaluated. There are different tests your doctor can run to determine a miscarriage.
Any vaginal bleeding or pelvic pain should be evaluated. There are different tests your doctor can run to determine a miscarriage.
Your doctor will check your cervix during a pelvic examination. Your doctor might perform an ultrasound to check the fetal heartbeat. A blood test can look for the pregnancy hormone.
If you’ve passed pregnancy tissue, bring a sample of the tissue to your appointment so your doctor can confirm the miscarriage.
Types of miscarriage
There are different types of miscarriages. These include:
Threatened miscarriage
During a threatened miscarriage your cervix isn’t dilated, but you do experience bleeding. There is still a viable pregnancy present. There’s a risk of miscarriage, but with observation and medical intervention, you may be able to continue the pregnancy.
Inevitable miscarriage
An inevitable miscarriage is when your cervix is dilated and your uterus is contracting. You may already be passing some of the pregnancy tissue vaginally. This is a miscarriage already in progress.
This is a miscarriage already in progress.
Incomplete miscarriage
Your body releases some fetal tissue, but some of the tissue remains in your uterus.
Missed miscarriage
During a missed miscarriage, the embryo has died, but the placenta and embryonic tissue remain in your uterus. You may not have any symptoms, and the diagnosis is made incidentally on an ultrasound exam.
Complete miscarriage
During a complete miscarriage your body passes all the pregnancy tissue.
If you ignore a possible miscarriage, you could develop septic miscarriage, which is a rare but serious uterine infection. Symptoms of this complication include a fever, chills, abdominal tenderness, and foul-smelling vaginal discharge.
Ways to treat a miscarriage
Treatments vary according to the type of miscarriage. With a threatened miscarriage, your doctor may recommend you rest and limit activity until the pain and bleeding stop. If there’s a continued risk for a miscarriage, you may have to remain on bed rest until labor and delivery.
In some cases, you can let a miscarriage progress naturally. This process can take up to a couple of weeks. Your doctor will review bleeding precautions with you and what to expect. A second option is for your doctor to give you medication to help you pass the pregnancy tissue and placenta faster. This medication can be taken orally or vaginally.
Treatment is usually effective within 24 hours. If your body doesn’t expel all the tissue or placenta, your doctor can perform a procedure called dilation and curettage (D and C). This involves dilating the cervix and removing any remaining tissue. You could also discuss having a D and C with your doctor as first-line treatment, without using medication or letting your body pass the tissue on its own.
Next steps
A pregnancy loss can occur even if you do eliminate risk factors like smoking and drinking. Sometimes, there’s nothing you can do to prevent a miscarriage.
After a miscarriage, you can expect a menstrual cycle within about four to six weeks.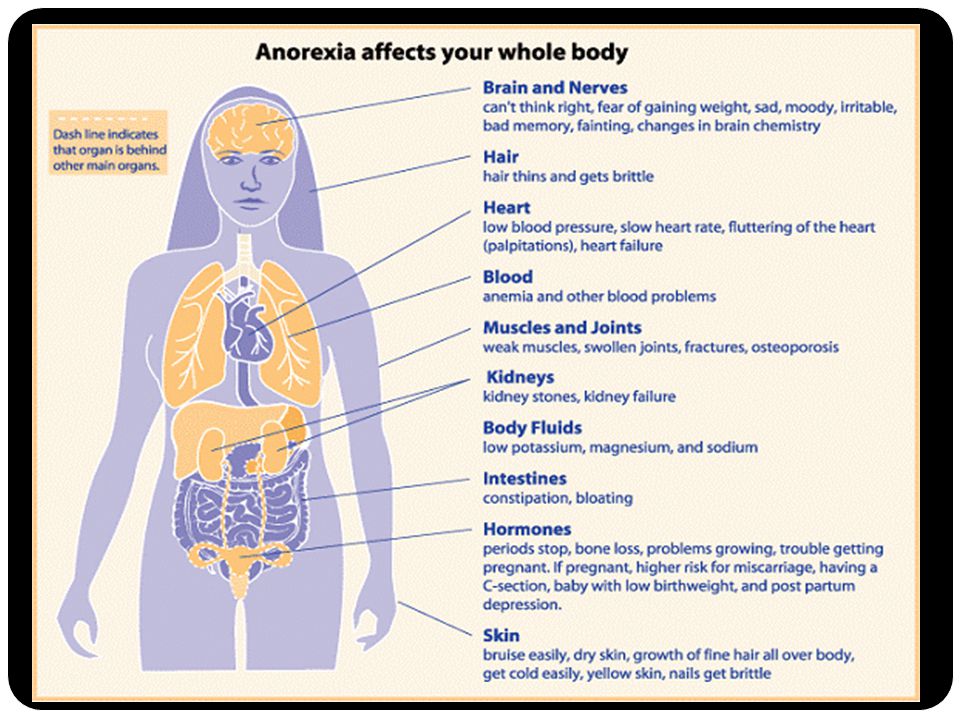 After this point, you can conceive again. You can also take precautions against having a miscarriage. These include:
After this point, you can conceive again. You can also take precautions against having a miscarriage. These include:
- taking prenatal vitamins
- limiting your caffeine intake to 200 milligrams per day
- managing other medical conditions you may have, such as diabetes or high blood pressure
Shop for prenatal vitamins.
Having a miscarriage doesn’t mean you can’t have a baby. But if you have multiple miscarriages, your doctor may suggest testing to determine if there is an underlying cause.
Last medically reviewed on June 13, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- American College of Obstetricians and Gynecologists. (2010). ACOG Committee Opinion No. 462: Moderate caffeine consumption during pregnancy. DOI:
10.1097/AOG.0b013e3181eeb2a1 - Andersen N, et al. (2000). Maternal age and fetal loss: population based register linkage study.
ncbi.nlm.nih.gov/pubmed?term=10864550 - Management of miscarriage: Your options. (2016).
miscarriageassociation.org.uk/wp/wp-content/leaflets/Management-of-miscarriage.pdf - Mayo Clinic Staff. (2016). Miscarriage.
mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/basics/causes/con-20033827 - Miscarriage. (2017).
americanpregnancy.org/pregnancy-complications/miscarriage/ - Nelson DB, et al. (2003). Violence does not influence early pregnancy loss.
ncbi.nlm.nih.gov/pubmed?term=14607576 - Hirsch L. (2015). Understanding miscarriage.
kidshealth.org/en/parents/miscarriage. html
html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Jun 13, 2018
Written By
Valencia Higuera
Edited By
Frank Crooks
Medically Reviewed By
Holly Ernst, PA-C
Share this article
Medically reviewed by Holly Ernst, PA-C — By Valencia Higuera on June 13, 2018
related stories
What Does a Miscarriage Look Like?
What to Know About Your First Period After a Miscarriage
How Soon Can You Ovulate After Miscarriage?
How to Tell if You’re Having a Miscarriage Without Bleeding
Am I Having a Miscarriage? What It May Feel Like
Read this next
What Does a Miscarriage Look Like?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Bleeding in pregnancy could be a sign of miscarriage.
 Learn what miscarriage bleeding looks like, plus other signs of pregnancy loss, including how…
Learn what miscarriage bleeding looks like, plus other signs of pregnancy loss, including how…READ MORE
What to Know About Your First Period After a Miscarriage
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
After a miscarriage, your period will likely take four to six weeks to come back. This depends on how long you were pregnant before the miscarriage…
READ MORE
How Soon Can You Ovulate After Miscarriage?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
It’s possible to ovulate as early as two weeks following a miscarriage. That means you could become pregnant again before having a period. Talk to…
READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
Am I Having a Miscarriage? What It May Feel Like
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Every woman and every pregnancy is different when it comes to what a miscarriage feels like. Signs and symptoms may also vary depending on your stage…
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Maintaining a Healthy Pregnancy
Medically reviewed by Stacy Sampson, D.O.
Pregnant people who eat well and exercise regularly along with regular prenatal care are less likely to have complications during pregnancy.
READ MORE
Pregnancy Complications
Medically reviewed by Michael Weber, MD
Sometimes a pregnant woman’s existing health conditions can contribute to problems, and other times new conditions arise because of body and hormonal…
READ MORE
Premature Birth Complications
Medically reviewed by Karen Gill, M.D.
Premature birth complications can occur when a baby is born early, usually before 37 weeks of pregnancy. Learn about short-term and long-term…
READ MORE
Treatment and prevention of miscarriage
Miscarriage. Symptoms
Symptoms
Causes of a miscarriage
Questions to ask your doctor about a miscarriage
Diagnosis of a miscarriage
If there is a risk of a miscarriage, your doctor may recommend rest until the bleeding or pain stops. Your doctor may also recommend that you abstain from sports and sexual activity. It is better not to travel, and especially not to travel to places where it is difficult to get emergency medical care.
Thanks to the widespread use of ultrasound, it is much easier these days to know if an embryo has died or not formed at all, and to know for sure that a miscarriage will occur. In this case, there are several options:
Expectant tactics. Before ultrasound was used in early pregnancy, most women had no idea that they were going to have a miscarriage. Some women allow the process to develop naturally. Usually a miscarriage occurs a few weeks after the death of the embryo is established. Unfortunately, this process can take three to four weeks. From an emotional point of view, this can be quite a difficult period.
From an emotional point of view, this can be quite a difficult period.
Conservative treatment for miscarriage. If, after diagnosing a miscarriage, a woman decides to speed up the process, then the removal of the embryonic tissue and placenta from the body can be provoked by taking certain drugs. Some medications are taken by mouth, but your doctor may prescribe intravaginal medications to increase their effectiveness and reduce the risk of side effects such as nausea, abdominal pain, and diarrhea. Most likely, a miscarriage will occur at home. The time of action of the drug may vary. You may also need more than one dose of the drug. In 70% of cases, the drug begins to act within a day, and a miscarriage occurs in the next few days or weeks.
Surgical treatment. Another treatment option is vacuum aspiration and curettage. During this procedure, the doctor opens the cervix and, using a special device, gently sucks tissue from the uterus. Sometimes a special metal surgical instrument with a loop at the end (curette) is used to scrape the walls of the uterus after vacuum aspiration. Complications are rare, but the connective tissue of the cervix or the wall of the uterus may be damaged.
Sometimes a special metal surgical instrument with a loop at the end (curette) is used to scrape the walls of the uterus after vacuum aspiration. Complications are rare, but the connective tissue of the cervix or the wall of the uterus may be damaged.
In the event of an unavoidable miscarriage, surgery is necessary to stop the bleeding.
Lifestyle and home care
Physical recovery
In most cases, physical recovery after a miscarriage takes a few hours to a few days. It will take 4-6 weeks to return to a normal lifestyle. During this period, if you experience heavy bleeding, fever, chills or severe pain, you should contact your doctor. These signs and symptoms may indicate an infection. For two weeks after a miscarriage, you should not have sex, use tampons, or flush your vagina.
Subsequent pregnancy
It is possible to become pregnant during your period immediately after a miscarriage. If you and your partner decide to try for a baby, make sure you are emotionally and physically ready for it. The doctor may recommend to postpone this process until the next menstruation, and maybe even more.
The doctor may recommend to postpone this process until the next menstruation, and maybe even more.
More than three miscarriages in a row should be investigated to determine the underlying causes, such as uterine abnormalities, coagulation problems, or abnormalities at the chromosomal level. In some cases, the doctor will suggest that you get tested after two miscarriages in a row, but two miscarriages still may not have hidden medical reasons. If the cause of miscarriages cannot be determined, do not lose hope. 60-70% of women who have had consecutive miscarriages can become pregnant in the future, even without treatment.
Coping with illness and finding support
Psychological recovery can take much longer than physical recovery. A miscarriage is a painful loss that others will not be able to fully understand. You can experience completely different feelings: from anger to despair. Give yourself time to process this grief and find support from loved ones.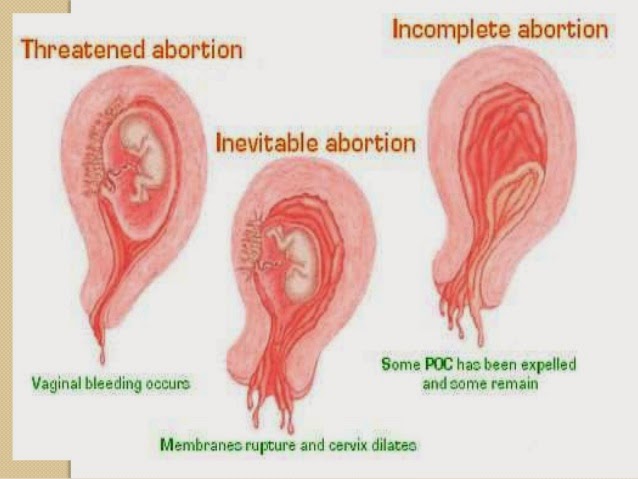 Don't blame yourself for what happened. You may not be able to forget all the hopes and dreams you had for this pregnancy, but over time, acceptance will ease the pain. Talk to your healthcare provider if you are experiencing deep sadness or depression.
Don't blame yourself for what happened. You may not be able to forget all the hopes and dreams you had for this pregnancy, but over time, acceptance will ease the pain. Talk to your healthcare provider if you are experiencing deep sadness or depression.
Prevention
With so many possible causes of miscarriage, there is simply no way to prevent it. It is better to concentrate all your energy on taking care of yourself and your unborn child. Seek medical attention and avoid known risk factors such as smoking and drinking alcohol. In the presence of chronic diseases, you need to consult with your doctor in order to monitor your health.
You can get more detailed information about miscarriage from the gynecologists of the Health 365 clinic in Yekaterinburg.
Prices
Gynecologist, initial appointment
2300 I
miscarriage, Symptoms - Health Clinic 365 G. Yekaterinburg
Causes of miscarriage
Questions to the doctor about miscarriage
Diagnostics of miscarriage
Treatment and prevention of miscarriage 9000,0002 Pass0016 for up to 20 weeks. According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is a fairly common occurrence, but this fact does not make things easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Symptoms of miscarriage .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although this is common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common.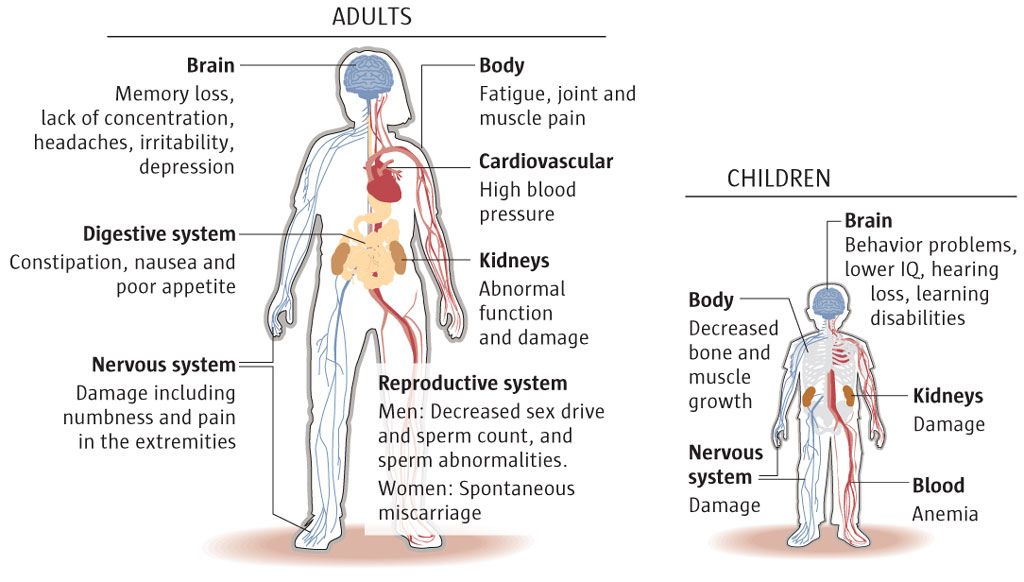 In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Contact your doctor in the following cases:
- Bleeding, even if there is only light spotting
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can place a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy.