Itching rash during pregnancy
Symptoms and what they look like
Some people develop skin rashes during pregnancy. The medical name for this is pregnancy dermatosis. Rashes can vary in severity and duration, depending on what causes them.
Hormone levels, stretching skin, genetics, and blood flow can all play a role.
This article discusses seven types of rash that can occur during pregnancy, including their symptoms and treatments. It also looks at how people can manage the symptoms at home.
Itchy skin is common during pregnancy, and some people also develop rashes. Some types of rash are specific to pregnancy, while others can occur at any time. However, some rashes may be more likely during pregnancy for some people due to the physical changes their body is going through.
In most cases, skin rashes are not serious and do not indicate a problem with the fetus. However, identifying the cause early on is important, as some rashes are a symptom of an underlying condition.
Some rashes that can occur during pregnancy include:
- heat rash
- hives
- atopic eruption of pregnancy
- pruritic urticarial papules and plaques of pregnancy (PUPPP) rash
- intrahepatic cholestasis of pregnancy (ICP)
- impetigo herpetiformis
- pemphigoid gestationis
Pregnancy can cause people to feel unusually warm because of increased blood supply to the skin. As a result, a person may find that they sweat more, which, in some cases, may lead to a heat rash.
A heat rash, or prickly heat, causes an itchy patch of tiny blisters on the skin. Staying cool and dry can help heat rashes heal. If a person experiences heat rashes, they can try:
- wearing loose clothing made from natural fibers, such as cotton
- working and sleeping in cool, well-ventilated rooms
- changing out of wet clothing as soon as possible
- using cool water compresses on the rash
Hives look like raised bumps or welts on the skin. They itch and often occur due to an allergic reaction. However, there are other possible causes, including:
- heat
- scratching the skin
- stress
- pressure on the skin
Feeling hot and itchy is common during pregnancy and may lead to hives. In addition, the authors of a 2013 article suggest that hormonal changes may also induce hives.
A person can treat mild hives at home by cooling the skin. If the hives are severe or occur alongside swelling or difficulty breathing, a person should seek immediate medical help.
If the hives are severe or occur alongside swelling or difficulty breathing, a person should seek immediate medical help.
Atopic eruption of pregnancy is the most common pregnancy-specific skin disorder. The term groups several similar pregnancy rashes together. These include:
- atopic eczema
- prurigo of pregnancy
- pruritic folliculitis of pregnancy
Eczema is a very dry and itchy rash that appears red in lighter skin and gray or brown in darker skin. People who develop eczema during pregnancy may find that lesions flare up more than usual during the first and second trimesters.
Prurigo of pregnancy involves a rash that consists of papules, which are small bumps filled with fluid. Pruritic folliculitis causes papules that resemble pimples, or acne.
These conditions are uncomfortable but do not pose a risk to the pregnant person or the fetus. The rash will often disappear after delivery. Until then, a doctor may prescribe emollients, steroid creams, or antihistamines to reduce itching.
PUPPP rash affects about 1 in every 160 pregnancies. This condition is more common in people carrying multiple fetuses, as with twins or triplets.
A PUPPP rash develops when the skin stretches, damaging the layer of tissue underneath. This causes inflammation, which appears as a rash. A PUPPP rash sometimes begins in the second trimester but usually develops in the final 3 months of pregnancy. It goes away after giving birth.
A PUPPP rash is itchy and produces bumps on the skin, but it does not cause complications. A doctor may suggest using oral antihistamines, skin emollients, or steroid medication to treat it.
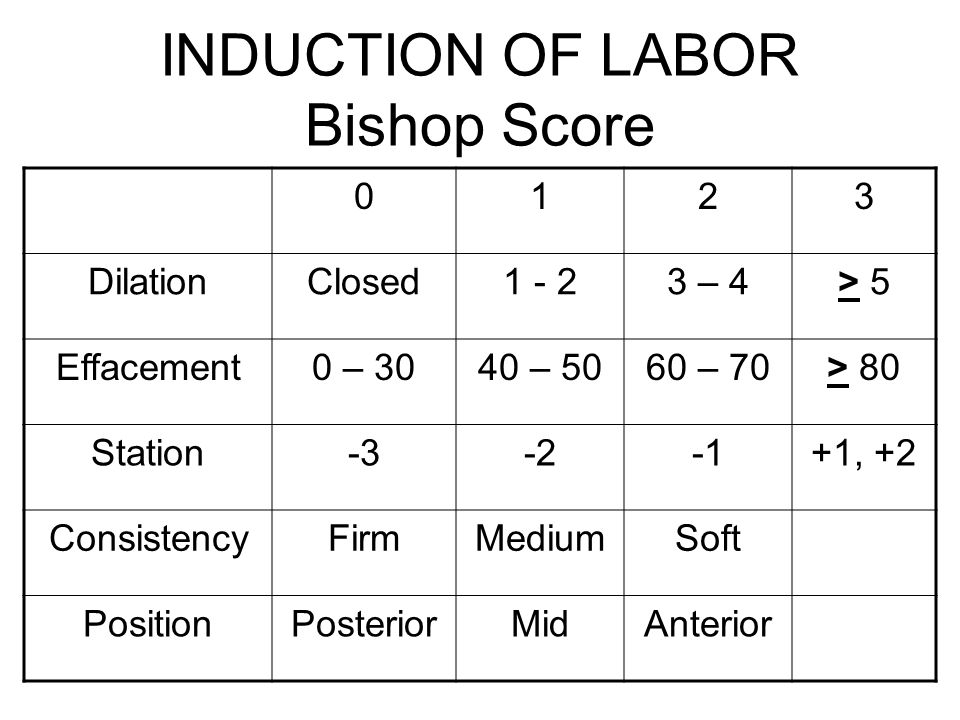
ICP, or obstetric cholestasis (OC), is a potentially serious liver condition that can occur during pregnancy. It causes severe itching that begins on the palms of the hands and the soles of the feet before spreading to other parts of the body. The itching may occur with or without a rash.
Sometimes, itching is the only symptom of ICP. Occasionally, a person may also develop jaundice, which causes the nails, skin, and eyes to become slightly yellow. ICP typically occurs in the third trimester.
ICP typically occurs in the third trimester.
The likelihood of developing ICP differs among ethnic groups. The condition affects 1% of females of Northern European ancestry. It is more common in people of Scandinavian or Araucanian Indian descent.
ICP can cause pregnancy complications, so early recognition, diagnosis, treatment, and close surveillance are very important. Severe itching in pregnancy is not normal, so a person should see a doctor immediately if this occurs.
Impetigo herpetiformis is a rare skin condition that appears during pregnancy, often in the last trimester. It is similar to pustular psoriasis, which causes severe skin inflammation.
This rash begins as lesions in the skin folds. These can then spread across the surface of the skin, covering large patches. The skin may crust or become infected. People can also experience:
- fever
- diarrhea
- dehydration
- rapid heartbeat
- seizures
Impetigo herpetiformis usually resolves after a person gives birth, but there is a risk of stillbirth. In rare cases, this condition is fatal. Doctors manage the condition and reduce these risks by prescribing systemic corticosteroids and antibiotics.
In rare cases, this condition is fatal. Doctors manage the condition and reduce these risks by prescribing systemic corticosteroids and antibiotics.
If a person experiences impetigo herpetiformis during one pregnancy, they may experience it again in future pregnancies.
Pemphigoid gestationis is a rare autoimmune disease that affects 1 in every 50,000 pregnancies. It causes an itchy, hive-like rash that begins around the navel and then spreads to other parts of the body. The rash may also include blisters.
This condition often begins in the second or third trimester. It can resolve during late pregnancy, but it often flares up before delivery. After pregnancy, the menstrual cycle or use of oral birth control pills may trigger the rash to return.
In 5–10% of pemphigoid gestationis cases, newborns are born with skin lesions. However, the exact risk that this condition poses to the fetus is unclear.
Mild rashes, such as hives, heat rash, or mild eczema, can improve with home management.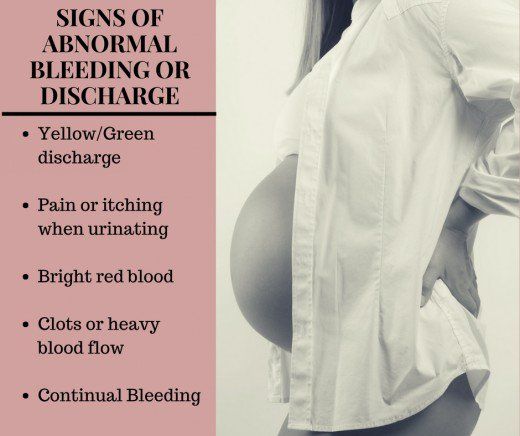 A person can try the following methods to soothe irritated skin and ease itching:
A person can try the following methods to soothe irritated skin and ease itching:
- keeping the skin clean and dry using a gentle, unscented cleanser
- washing with cool or lukewarm water rather than hot or cold water
- moisturizing the skin using an unscented emollient, particularly after bathing, showering, or washing the hands
- avoiding products that may irritate the skin, such as harsh soaps or perfumes
- wearing loose, soft fabrics, such as cotton or linen
- using cool compresses, colloidal oatmeal baths, or calamine lotion to soothe itching
- avoiding scratching the skin, as this can make some skin conditions worse
Many forms of pregnancy rash are harmless, but it is always best to see a doctor so that they can identify the cause and confirm that a person does not need medical treatment. A doctor can also advise on the best way to care for skin conditions during pregnancy.
A person should seek immediate treatment if a rash:
- appears suddenly and spreads quickly
- causes severe itching or pain
- co-occurs with difficulty breathing and swelling
- is weeping pus or looks infected
A person should also see a doctor as soon as possible if they experience severe itchiness without a rash.
Rashes and itchy skin are common during pregnancy. Many rashes are harmless and may resolve after giving birth. However, in rare cases, rashes can be a sign of a more serious condition.
If a person does not know the cause of a pregnancy rash, they should see a doctor for a diagnosis.
PUPPP rash in pregnancy: Natural treatments and prevention
PUPPP rash in pregnancy: Natural treatments and prevention- Health Conditions
- Health Conditions
- Alzheimer's & Dementia
- Anxiety
- Arthritis
- Asthma & Allergies
- Breast Cancer
- Cancer
- Cardiovascular Health
- COVID-19
- Dermatology & Skincare
- Diabetes
- Environment & Sustainability
- Exercise & Fitness
- Eye Health
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Inflammatory Bowel Disease
- Leukemia
- LGBTQIA+
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Nutrition
- Parkinson's Disease
- Psoriasis
- Sexual Health
- Women's Health
- Health Conditions
- Discover
- News
- Latest News
- Original Series
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- Podcasts
- What makes breast cancer come back?
- How to understand chronic pain
- What is behind vaccine hesitancy?
- The amazing story of hepatitis C, from discovery to cure
- New directions in dementia research
- Can psychedelics rewire a depressed, anxious brain?
- News
- Tools
- General Health
- Drugs A-Z
- Health Hubs
- Health Tools
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- Health Products
- Affordable Therapy Options
- Blood Pressure Monitors
- Diabetic Supplies
- Fitness Trackers
- Home Gyms
- Green Cleaning Products
- How to Shop for CBD
- Quizzes
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- General Health
- Connect
- About Medical News Today
- Who We Are
- Our Editorial Process
- Content Integrity
- Conscious Language
- Newsletters
- Sign Up
- Follow Us
- About Medical News Today
Medically reviewed by Valinda Riggins Nwadike, MD, MPH — By Jennifer Huizen on August 9, 2018
A pruritic urticarial papules and plaques of pregnancy rash is a common skin condition. Natural remedies, including oatmeal, chamomile, and peppermint, can help.
Natural remedies, including oatmeal, chamomile, and peppermint, can help.
This type of rash usually starts in stretch marks on the abdomen and spreads to the legs and chest.
It causes itchy, red, hive-like bumps to form in the creases of stretch marks, and the rash can develop into larger red, swollen patches. In lighter-skinned people, the rashes may appear to be surrounded by a thin, white halo.
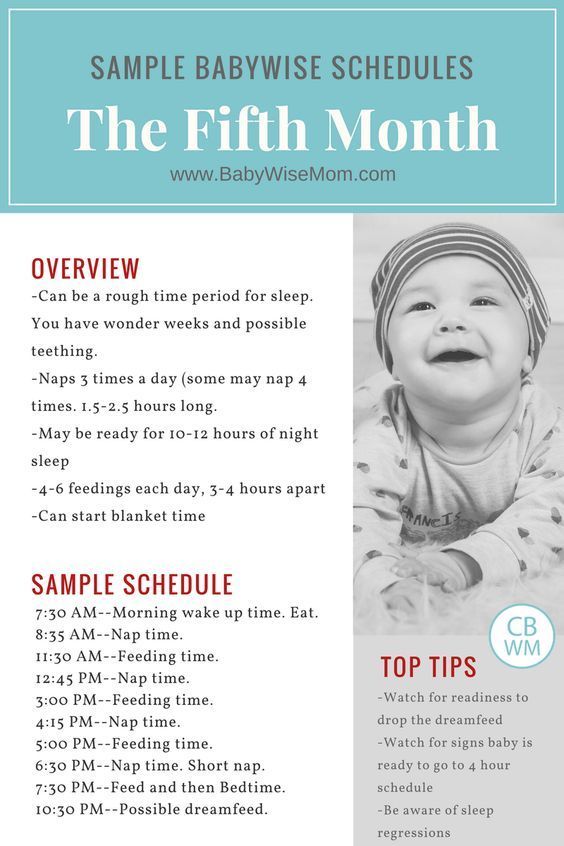
Pruritic urticarial papules and plaques of pregnancy (PUPPP) often develop in the third trimester of pregnancy. In most cases, the rash resolves within 15 days of giving birth.
While some medications can reduce the symptoms of a PUPPP rash, there is currently no cure.
Share on PinterestStudies suggest that peppermint oil applied to the skin can decrease itchiness.Last medically reviewed on August 9, 2018
- Dermatology
- Pregnancy / Obstetrics
- Complementary Medicine / Alternative Medicine
- Parenthood
- 3rd Trimester
How we reviewed this article:
Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Akhavan Amjadi, M., Mojab, F., & Kamranpour, S. B. (2012, Autumn). The effect of peppermint oil on symptomatic treatment of pruritus in pregnant women. Iranian Journal of Pharmaceutical Research : IJPR, 11(4), 1073–1077
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3813175/ - Chamomile. (2016, November 29)
https://nccih.nih.gov/health/chamomile/ataglance.htm - Cortés-Rojas, D. F., Fernandes de Souza, C. R., & Oliveira, W. P. (2014, February). Clove (Syzygium aromaticum): A precious spice. Asian Pacific Journal of Tropical Biomedicine, 4(2), 90–96
https://www. ncbi.nlm.nih.gov/pmc/articles/PMC3819475/
ncbi.nlm.nih.gov/pmc/articles/PMC3819475/ - Fowler, J. F. (2014, October). Colloidal oatmeal formulations and the treatment of atopic dermatitis. Journal of Drugs in Dermatology: JDD, 13(10), 1180–1183
http://jddonline.com/articles/dermatology/S1545961614P1180X/1 - Ibrahim, I. M., Elsaie, M. L., Almohsen, A. M., & Mohey‐Eddin, M. H. (2017, April 5). Effectiveness of topical clove oil on symptomatic treatment of chronic pruritus [Abstract]. Journal of Cosmetic Dermatology, 16(4), 508–511
https://onlinelibrary.wiley.com/doi/abs/10.1111/jocd.12342 - Lopez Jornet, P., & Aznar‐Cayuela, C. (2016, June 21). Efficacy of topical chamomile management vs. placebo in patients with oral lichen planus: A randomized double‐blind study. Journal of the European Academy of Dermatology and Venereology, 30(10), 1783–1786
https://onlinelibrary.wiley.com/doi/full/10. 1111/jdv.13770
1111/jdv.13770 - Oakley, A., & Elghblawi, E. (2017, September). Polymorphic eruption of pregnancy
https://www.dermnetnz.org/topics/polymorphic-eruption-of-pregnancy/ - Pruritic urticarial papules and plaques of pregnancy. (n.d.)
https://www.aocd.org/page/PUPPP
Share this article
Medically reviewed by Valinda Riggins Nwadike, MD, MPH — By Jennifer Huizen on August 9, 2018
Related Coverage
Are breast rashes related to cancer?
Rashes and skin changes can affect the breasts for many reasons. In rare cases, they may indicate cancer. Get tips on what to look for and when to…
READ MORE
What is causing my rash?
Medically reviewed by Daniel Murrell, MD
There is a huge variety of rashes that can vary significantly in appearance. Some may appear in small patches on the body, and others may spread…
READ MORE
Everything you need to know about lichen planus
Medically reviewed by University of Illinois
Lichen planus is an inflammatory skin condition marked by an itchy, bumpy, pink or purple rash on the arms and legs.
 Specialists believe that may be…
Specialists believe that may be…READ MORE
What does a psoriasis rash look like?
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Psoriasis causes an itchy, scaly red rash that can be uncomfortable and some people find it embarrassing. Find out what different kinds of psoriasis…
READ MORE
Adult diaper rash: What you need to know
Medically reviewed by Cynthia Cobb, DNP, APRN, WHNP-BC, FAANP
While diaper rash is most common in infants, adults are also at risk of developing the condition, particularly those who wear adult diapers…
READ MORE
Treatment of PREGNANT POLYMORPHOUS RASH - Recommendations of the British Dermatological Association (translated and adapted by Prof. Svyatenko)
What is the purpose of this article?
This article is intended to tell you more about mumps . She will tell you what the condition is, what causes it, what can be done about it, and where to learn more about it.
She will tell you what the condition is, what causes it, what can be done about it, and where to learn more about it.
What is mumps rash of pregnancy?
Polymorphic rash of pregnancy is a relatively common skin disorder that can occur in women during pregnancy. It usually appears during the first pregnancy of women. It is characterized by an itchy rash that usually starts in the abdomen, especially in the stretch marks (striations). It most often develops in the later stages of pregnancy (third trimester), but can also be present immediately after the birth of a child.
Previously called PUPPP (pruritic and urticarial papules and plaques of pregnancy).
What causes polymorphic rash of pregnancy?
The cause of rash is unknown. It is believed that this is due to stretching of the skin on the abdomen and due to hormonal changes during pregnancy. This happens more often with multiple pregnancies (twins or triplets). Previous studies have shown an association with maternal weight gain during pregnancy, birth weight gain, and sex hormones, but this has not been proven.
Previous studies have shown an association with maternal weight gain during pregnancy, birth weight gain, and sex hormones, but this has not been proven.
Is polymorphic rash of pregnant women hereditary?
No.
What are the symptoms of mumps rash and what does it look like?
Itching begins and spreads on the skin of the abdomen, often sparing the umbilical cord (navel) in late pregnancy (3rd trimester). If stretch marks (striae) are present, itching may begin within them. Itching is followed by a blistering rash (as from a nettle sting), small raised areas on the skin (papules) and large red inflamed areas of the skin (plaques). It usually extends to the torso, lower abdomen, under the breasts, and on the extremities. The face, scalp and mucous membranes (oral cavity and genital organs) are practically not affected. Sometimes small blisters appear, from which, if damaged, a straw-colored liquid can seep and form crusts.
It is important to seek the advice of your dermatologist if you develop multiple rashes because mumps maternity rash may resemble an early form of another skin condition during pregnancy called pemphigoid. This condition may require different treatment and care for you and your baby.
This condition may require different treatment and care for you and your baby.
How to diagnose polymorphic rash of pregnancy?
Diagnosis is usually made by a dermatologist or other physician based on a typical appearance and spread of rash . However, if the appearance is not typical, your dermatologist may do a skin biopsy (a skin sample is removed under local anesthesia) and a blood test to help diagnose and rule out other causes of the rash.
Is polymorphic rash of pregnancy curable?
In most cases, this condition is self-limiting and improves towards the end of pregnancy or immediately after delivery. It can be suppressed with treatment. In most cases, symptoms resolve within a few weeks after delivery.
How can polymorphic rash of pregnancy be treated?
The main goal of treatment is to relieve itching and reduce inflammation and redness of the skin.
Calming agents can help relieve itching and soreness. These include cool baths, wet compresses, and wearing cotton clothing. Emollient baths and soap substitutes, followed by emollient creams or ointments, will help hydrate the skin. Menthol in water cream can be especially helpful.
These include cool baths, wet compresses, and wearing cotton clothing. Emollient baths and soap substitutes, followed by emollient creams or ointments, will help hydrate the skin. Menthol in water cream can be especially helpful.
WARNING. This article mentions "emollients" (moisturizers). When paraffin-containing emollient products come into contact with dressings, clothing, bedding or hair, there is a danger that open flames or cigarette smoking can cause ignition. To reduce the risk of fire, patients using paraffin-containing skin and hair products are advised to avoid open flames, including cigarette smoking and being near people who smoke or use open flames. It is also recommended to wash clothes and bedding regularly, preferably daily.
Topical steroid creams or ointments are often prescribed to reduce skin inflammation and are safe to use during pregnancy.
Oral antihistamines (only those suitable for use during pregnancy, such as loratadine) can be used to relieve itching.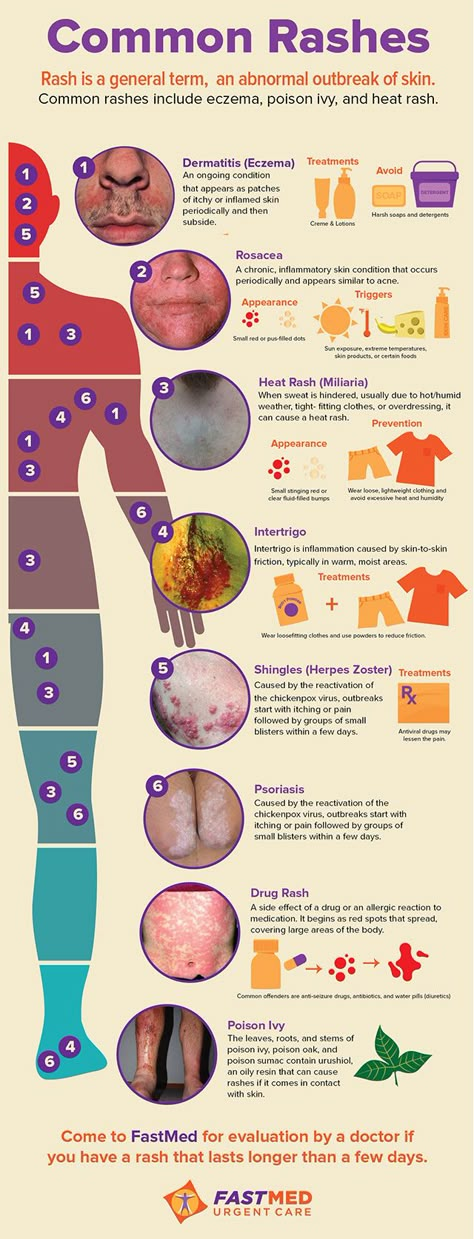
Rarely, if the condition is very severe, a short course of oral steroids may be prescribed.
Is the child affected?
No. There were no reports that the child was hurt.
Is natural delivery possible?
Yes. A caesarean section is not required.
Can women with mumps of pregnancy breastfeed?
Yes. Breastfeeding does not appear to affect mumps rash pregnant. It is safe to breastfeed a baby even if you are taking steroid tablets as only a tiny amount of the steroid passes into your breast milk.
Is any special monitoring required?
No, but it is important to visit the antenatal clinic regularly during pregnancy. It is recommended that your midwife and/or obstetrician be informed of this diagnosis.
Will polymorphic rash of pregnancy recur?
The condition tends not to recur except in subsequent pregnancies.
This article was translated from the recommendations of the British Association of Dermatologists "Overview information for the patient", adapted into Russian by Professor TV Svyatenko, Dnipro, Ukraine.
Be healthy and attractive!
Consult professionals only.
Use only evidence-based medicine, such as the one in this article, when researching information about your problem.
Dermatoses of pregnancy
Cost: from 1500 rubles
Sign up
Pregnancy is a wonderful time for any woman, especially when it is a planned and desired event in the life of a couple. Unfortunately, due to various circumstances, pregnancy does not always occur naturally - in such cases, modern medicine offers various procedures for assisted reproductive technologies. This makes the woman's attitude to such a natural process even more reverent. And here, often, our skin can present surprises. A number of skin conditions can worsen during pregnancy. However, traditionally prescribed drugs have limitations for use in such a situation. And here it is important that the specialist has experience in treating such situations.
Our Clinic is unique in some way, since many years of experience in managing women with skin diseases during pregnancy is not only the head physician, who has been a consultant at the D.O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
Now let's try to explain the causes and identify the most common skin diseases during pregnancy.
During pregnancy, the main cause of skin lesions is considered to be changes in the immune system of the pregnant woman. Pathological processes can be manifested by an exacerbation of chronic skin diseases or the appearance of specific pregnancy-associated dermatosis, the so-called "pregnancy dermatosis".
Changes on the skin are very diverse both in manifestations and in the mechanisms of development. Conventionally, they can be divided into 3 groups:
I. Pregnancy stigmas:
Chloasma is the most famous of them. As a development mechanism, various functional endocrine-metabolic changes during pregnancy are assumed. It appears as brownish spots of indefinite outlines, often symmetrical, on the skin of the cheeks, forehead, chin, neck without subjective sensations. Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots.
As a development mechanism, various functional endocrine-metabolic changes during pregnancy are assumed. It appears as brownish spots of indefinite outlines, often symmetrical, on the skin of the cheeks, forehead, chin, neck without subjective sensations. Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots.
Pregnancy melanosis - changes on the skin in the form of hyperpigmentation in the nipples, genitals, white line of the abdomen, also without subjective sensations or inflammation. After childbirth, these disorders disappear. Chloasma and melanosis usually do not require special treatment and spontaneously regress after delivery.
II. Skin diseases that are relatively often registered during pregnancy:
This group includes a variety of skin changes and diseases that often accompany pregnancy, as well as some common dermatoses, the course of which usually worsens during gestation. The main mechanism is a change in hormonal ratios in the body of a pregnant woman. This, in turn, affects the functionality of the immune and nervous systems, the state of the gastrointestinal tract, kidneys, cardiovascular activity, water-salt metabolism, etc.
The main mechanism is a change in hormonal ratios in the body of a pregnant woman. This, in turn, affects the functionality of the immune and nervous systems, the state of the gastrointestinal tract, kidneys, cardiovascular activity, water-salt metabolism, etc.
This group includes: hyperhidrosis
- hypertrichosis
- palmoplantar telangiectasias
- erythema of the palms
- alopecia - hair loss
- onychodystrophy - changes in the nail plate
Most of these and other conditions, as a rule, disappear after childbirth. Their treatment, if necessary, is symptomatic.
The course and severity of symptoms of other skin diseases also change during pregnancy. These primarily include eczema, atopic dermatitis, psoriasis, lichen planus, acne, Dühring's herpetiformis. During pregnancy, they often worsen, and exacerbations are usually more pronounced, more severe than before gestation. Sometimes, on the contrary, during pregnancy, a remission occurs, which continues until childbirth, after which another exacerbation occurs. Correction of exacerbations of these dermatoses during pregnancy is very difficult. Many medicines used under normal conditions affect the development of the fetus. Therefore, external symptomatic therapy becomes the leading method.
Correction of exacerbations of these dermatoses during pregnancy is very difficult. Many medicines used under normal conditions affect the development of the fetus. Therefore, external symptomatic therapy becomes the leading method.
III. Actually dermatoses of pregnant women
The four skin diseases characteristic of pregnancy, gestational pemphigoid, polymorphic dermatosis of pregnancy, atopic dermatitis of pregnancy, and cholestasis of pregnancy can be distinguished by clinical presentation, histopathology, risk of fetal complications. Only gestational pemphigoid and intrahepatic cholestasis of pregnancy are associated with significant risk to the fetus. Because all of these dermatoses are characterized by pruritus, careful evaluation of any pruritic pregnancies is necessary.
Pregnancy pemphigoid , formerly known as herpes gestationis, is the rarest of the skin disorders of pregnancy and is an autoimmune disease. Clinically, it manifests itself in the form of papules and plaques, transforming into vesiculobullous elements, localized in the umbilical region with spread to the chest, back and limbs.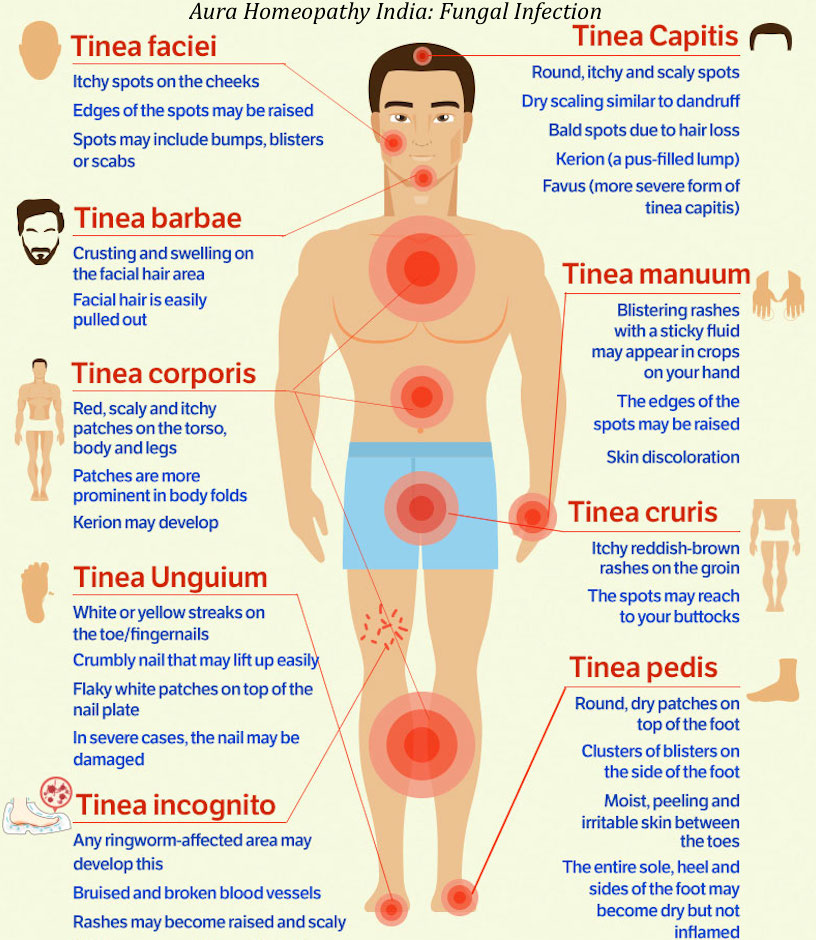 Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Polymorphic dermatosis of pregnancy (PEP) is a benign, pruritic inflammatory disease. It usually occurs at the end of the third trimester or immediately after delivery in the first pregnancy. Urticarial papules and plaques appear first on the abdomen and, unlike gestational pemphigoid, do not affect the umbilical region. The rash usually spreads to the thighs and buttocks, and can rarely be widespread. Eruptions with clear boundaries regress spontaneously within 4-6 weeks without treatment. Treatment for PEP is based on symptomatic relief with topical corticosteroids and antihistamines. If the rash becomes generalized, a short course of systemic corticosteroids may be used.
If the rash becomes generalized, a short course of systemic corticosteroids may be used.
Atopic dermatitis of pregnancy (AEP) - is the most common skin disorder in pregnancy. AEP is a benign disease characterized by an pruritic eczematous or papular rash. Two-thirds of AEP cases are characterized by eczematous skin changes localized to atopic areas of the body such as the neck and flexor surfaces of the extremities. The remaining cases are characterized by a papular rash in the abdomen and extremities. Lesions usually respond well to treatment and resolve spontaneously after delivery. However, AEP is more likely to recur in subsequent pregnancies. Dermatosis does not significantly affect the fetus, but there is an increased risk of developing atopic dermatitis in an infant.
Intrahepatic cholestasis of pregnancy (ICP) - characterized by itching with acute onset, which often begins on the palms and soles, and then generalizes. The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
Treatment is aimed at normalizing the level of bile acids in the blood serum in order to reduce the risk to the fetus and to control symptoms in the mother. Treatment with ursodeoxycholic acid (UDCA) is recommended. Other drugs that reduce itching may be used, such as antihistamines, dexamethasone. Treatment of pregnant women with dermatoses is very difficult, especially in the first trimester of pregnancy. If dermatosis is detected in a pregnant woman, it is necessary to jointly manage it by a dermatologist, an obstetrician-gynecologist. Treatment of dermatoses in pregnant women requires a differentiated approach to therapy, taking into account the duration of pregnancy, exacerbation of the disease and the prevalence of the process.