Is colostrum clear
Colostrum Colours: What Colour Should It Be?
Breast milk is one of the most beneficial sources of vitamins and nutrients for your baby.
If you decide to breastfeed, you might be curious about what is and isn't normal when it comes to the colour of your breast milk.
It's important to remember that the colour and consistency of your breast milk will change throughout your postpartum journey.
In the first few days after birth, you'll notice your first milk is a thick yellow consistency.
As time goes on, your breast milk will likely become thinner and lighter in colour as more mature milk comes in.
Colostrum (a.k.a. your first form of breast milk) is packed with nutrients and antibodies that help to establish your baby's immune system.
While it's usually thicker and more yellow than traditional milk, that's not always the case.
If you're worried about the colour and consistency of your colostrum, keep reading to find out what you need to know and what could be causing your breast milk to change colour.
What is colostrum?
As we've mentioned, colostrum is the first kind of breast milk your body produces.
In fact, your mammary glands (also known as your breasts) will begin producing colostrum during pregnancy, usually from 20 weeks.
What makes colostrum so important is the spectrum of vitamins, minerals and ingredients it contains.
Every drop of colostrum is packed with vitamins, minerals and antibodies that help to seed your baby's microbiome and establish a healthy immune system.
In fact, research has shown that breast milk (such as protein-rich colostrum) helps to transfer beneficial bacteria from your own immune system into your baby's gut and can support long-term health benefits.
Other studies have shown that beneficial gut bacteria can lower a child's risk of chronic diseases (such as asthma, obesity, allergies, and dermatitis) and can even play a role in regulating anxiety, mood, and cognition.
But let's get back to colostrum. This nutrient-dense food delivers a potent dose of vitamins and minerals to newborns, including:
- Immunoglobulin A (a beneficial antibody)
- Lactoferrin (a type of protein shown to prevent infection)
- Leukocytes (beneficial white blood cells)
- Epidermal growth factor (a type of protein known to stimulate cell growth)
Colostrum colour typically appears as yellow breast milk. You'll likely produce this milk in the first two to four days after birth.
You'll likely produce this milk in the first two to four days after birth.
Plus, your baby only needs to consume a small amount to reap the benefits (as colostrum is incredibly nutrient-dense and contains concentrated health benefits).
Why is colostrum important?
Colostrum plays a really important role in your baby's health. It contains a unique combination of nutrients and proteins that aren't found in more mature milk.
Specifically, colostrum offers newborns a range of benefits, including:
- Colostrum is packed with double the amount of protein as breast milk.
- Colostrum has four times the amount of zinc in breast milk.
- Colostrum is lower in fat and sugar, making it easier for newborns to digest.
- It strengthens your baby's immune system and coats their intestines in beneficial bacteria to establish a healthy gut.
- Colostrum boasts a laxative effect that can clear your baby's meconium (their first bowel movement) and reduce the chance of jaundice.

Plus, since colostrum begins to form during your pregnancy, it can be expressed by hand prior to your baby's arrival.
Hand expressing colostrum can help you understand your breasts better and gives you some extra time for breastfeeding mums to practice the movements involved in breastfeeding.
Colostrum can also be expressed and stored safely ahead of birth to ensure you've got an extra supply of food ready for when your baby arrives.
Having this frozen breast milk on hand is especially helpful as it allows others to help feed the baby in the first few days after birth.
What colour is colostrum?
What sets colostrum apart from other types of breast milk is its colour and consistency.
Typically, colostrum is yellow in appearance and is a thicker, stickier consistency to mature milk.
The yellow shade of colostrum and its potent health benefits are why many refer to this first milk as 'liquid gold'.
Is it safe to express colostrum during pregnancy?
While your body will begin to produce colostrum from 18 to 20 weeks pregnant, it's best to wait until 37 weeks before attempting to express colostrum.
Why? Well, some research suggests that stimulating your breasts through hand expressing milk can increase the chance of premature labour.
Once you reach the end of your pregnancy, you can try hand expressing two to three times each day.
The key is to start gently and slowly and increase the duration of each session to up to five minutes per breast.
Make sure to chat with your healthcare provider before giving this a try to make sure it's safe for you and your baby.
Can colostrum be different colours?
In most cases, colostrum will appear as a thick, yellow substance. However, there is a range of factors that can change the colour of your breast milk.
What you eat and the ingredients in your diet can influence the colour of your breast milk.
Plus, if you're navigating a breastfeeding issue or breast infection such as mastitis you might notice your breast change colour (or even contain small amounts of blood).
In most cases, you'd expect to see your milk ducts producing thick, yellow colostrum in the first few days postpartum.
If you're concerned about your milk or feel like something isn't right, make sure to chat with your doctor or get in touch with a lactation specialist.
Why is your colostrum clear and watery?
As we mentioned, your first breast milk will typically be a thicker consistency before it thins out in the mature milk stage. However, that isn't the case for everyone.
In some instances, you might notice your colostrum is clear, thin and watery.
Plus, the first milk produced might not be the slightly yellow shade you were anticipating.
The truth is that milk production rates vary from woman to woman.
If your flow of colostrum takes a little longer than usual, your breast milk may be thinner and lighter in colour than you'd expect.
However, by three to four days after giving birth, your should notice your milk ducts producing thicker milk that is a light yellow shade.
Again, clear and watery colostrum is nothing to worry about, but make sure to chat with your doctor if something doesn't feel right.
What is the colour of breast milk?
The answer to this question really depends on what stage of your breastfeeding journey you're at and even what kind of food you're eating.
That's right: a change in breast milk colour can actually be influenced by the nutrients, ingredients and food dyes you're consuming.
While mature breast milk is usually a cream or white colour, here are some of the other colours of breast milk you might experience:
Pink breast milk
If you've consumed a large amount of red-coloured foods (such as beetroot), you might notice you're producing pink milk.
Yellow or orange breast milk
This shade of dark yellow or orange is usually caused by eating orange-coloured foods such as carrots, sweet potatoes, pumpkin or even orange soft drinks.
Green breast milk
Green breast milk can be caused by consuming large quantities of green vegetables or green foods, kelp or even vitamins containing seaweed. Plus, you might even notice blue breast milk if you consume foods with a green tint or blue tint food dyes.
Black breast milk
This breast milk colour can be caused by certain types of medication or can also be a sign of blood-tinged milk.
Red breast milk
This breast milk colour usually means there is blood or broken down blood products in your milk ducts.
Is it normal for breast milk to change colour?
In most cases, a change in breast milk colour is harmless. That's because your milk goes through a number of different stages, including:
- Colostrum: the first milk your breasts will produce.
- Transitional milk: your milk transitions begin within four days of giving birth and last for roughly two weeks.
- Mature milk: once your milk supply has come in, you'll experience a more consistent colour and consistency in your milk until you decide to stop breastfeeding.
However, it's important to know what might cause your milk to change.
Blood staining in your breast milk is common and doesn't necessarily hint at a more serious health problem (like breast cancer).
Often, you'll notice blood in your colostrum in the first few days after giving birth.
This is known as rusty pipe syndrome and is usually caused by the growth of your ducts and milk-producing cells.
Another common cause of blood in your breast milk is cracked nipples or even an infection like mastitis.
However, this blood and red milk is harmless to your baby and shouldn't be a cause for concern.
When should you be concerned?
Usually, any changes in your milk colour or the presence of blood will clear up within a few days.
However, if something doesn't feel right or you continue to notice blood in your breast milk, it's best to chat with your doctor and seek professional medical advice.
We know that many mothers experience discomfort or breastfeeding challenges.
From sore nipples to breast leaks, we've designed Kin's Breastfeeding Essentials kit to help you through Australia's most common breastfeeding challenges.
Along with learning about the changes in your breast milk, taking care of your breasts is one of the best things you can do once you've started breastfeeding.
Photo credit: Helena Jankovičová Kováčová via Pexels
Colostrum: Why It’s Beneficial for Your Newborn Baby
If you’ve heard the terms "first milk," "pre-milk," "early milk," or "practice milk," you may have wondered what they mean. They all refer to a form of breast milk called colostrum — a type of nutrient-rich milk that comes in before your regular breast milk.
Whether you’ve noticed colostrum leak onto your bra during pregnancy or you’re considering breastfeeding and want to know more, it’s helpful to understand what colostrum is, how long it lasts, and how much your newborn may need. Read on to find out all this, and more.
What Is Colostrum?
Colostrum is a highly concentrated form of breast milk that contains immune-boosting properties for your newborn. It’s packed with protein, salts, antibodies, and protective properties, all of which are beneficial for your baby. When compared with regular breast milk, colostrum is higher in protein but lower in sugar, fat, and calories.
If you're nursing your baby, the feeds you give your newborn in the first few days after she’s born would be of colostrum, before your regular breast milk starts flowing.
Colostrum Benefits
Breastfeeding moms may want to think of colostrum as their baby’s first meal — one that offers health benefits such as:
Helping to immunize your baby against harmful germs by coating his intestines, and helping to shield his immune system against germs
Providing some protection from inflammation and killing potentially harmful microorganisms
Having laxative properties that can help get meconium (your little one’s first stool) moving along, which can help lessen the chance of jaundice
Helping to prevent low blood sugar levels if your baby was born full term
Offering a nutritional boost to a baby born prematurely, as it can provide your preemie with extra nutrition.
What Does Colostrum Look Like?
Since it’s so concentrated, colostrum is thick and sticky. It may look orange, yellow, clear, or white in color.
It may look orange, yellow, clear, or white in color.
Typically, it is yellowish because it contains beta-carotene (the same thing that makes carrots yellow), but if your colostrum is thinner and more watery, don’t worry — it’s normal for it to be a little different for every mom.
When Does Colostrum Come In?
An expectant mom's breasts may be ready to produce colostrum as early as 16 weeks of pregnancy or later in the second trimester. So don't be surprised if you see signs of leaking colostrum long before you’re due to give birth.
Leaking colostrum does not necessarily mean that labor is close. Although it may seem a little odd, it’s actually completely normal to leak a little breast milk during pregnancy.
Conversely, some moms-to-be don’t notice any signs of colostrum leaking during pregnancy, but this doesn’t mean that colostrum production isn’t happening. Behind the scenes, your breasts are getting prepped for breastfeeding — just one more way your body is getting ready for motherhood.
If you are leaking colostrum, you might want to buy some disposable or reusable breast pads that line your bra. These help absorb the liquid and protect your clothing.
How Long Does Colostrum Last?
Your body will typically produce colostrum for several days after the birth of your baby before this early milk transitions into regular breast milk.
After the initial two to five days of colostrum production, your breasts will begin to increase in size and feel firmer. This indicates that your milk supply is increasing and has started to transition from colostrum to regular breast milk — a process that happens over a few weeks.
How Much Colostrum Does a Newborn Baby Need?
New moms may produce anywhere from 10 to 100 milliliters of colostrum per day. Typically, though, it’s around 30 milliliters or about an ounce a day, which is right around the amount that your baby needs. But don’t worry if you’re producing less than this amount — any amount is good for your baby. As your breasts transition into producing more milk than colostrum, your baby’s stomach will also expand to accept more milk.
But don’t worry if you’re producing less than this amount — any amount is good for your baby. As your breasts transition into producing more milk than colostrum, your baby’s stomach will also expand to accept more milk.
For more on breastfeeding in general, check out these breastfeeding tips. And if you're concerned about your milk supply, consult your healthcare provider for advice. You can also read this article on increasing breast milk production.
Colostrum is important in so many ways for your baby. It's the perfect first meal for a newborn, fortifying her with antibodies for a beneficial jump-start in life.
While we’re on the important topic of feeding your baby, you might want to learn more interesting facts about breastfeeding as well as more about formula feeding.
Alongside all those feedings, you’re bound to have plenty of diaper changes. Download the Pampers Club app today and start earning rewards, like gift cards and cash back, for your diaper and wipes purchases.
A new look at colostrum pasteurization
colostrum, pasteurization, health
A new look at colostrum pasteurization
Colostrum is a complex blend of nutrients, immune components, cells and growth factors, and hormones that are vital for a newborn calf. Many studies show that contamination of colostrum with bacteria, especially fecal bacteria, reduces the absorption of immunoglobulins G (IgG) and negatively affects the health of the calf.
Many studies show that contamination of colostrum with bacteria, especially fecal bacteria, reduces the absorption of immunoglobulins G (IgG) and negatively affects the health of the calf.
Like other body fluids, colostrum spoils very quickly. The amount of bacterial contamination depends on how correctly the colostrum was collected and prepared. Pasteurization reduces bacterial contamination and improves IgG uptake. Heating colostrum to 60°C for an hour reduces the total number of bacteria and improves the efficiency of IgG absorption by 15-25%.
Scientists at Pennsylvania State University report a new study that addresses colostrum pasteurization and its effect on IgG quality and absorption.
Colostrum was collected from freshly calved cows and frozen prior to testing. In total, they collected 114 liters. Then all the colostrum was thawed, mixed, and then frozen again [control; KOH] or pasteurized (60 °C for an hour) and frozen [pasteurized; PASS].
Scientists monitored total bacterial contamination and IgG concentration in all samples. 26 Holstein calves were fed colostrum in the amount of 8% of their weight within 4.5 hours after birth. Blood samples were taken from the calves immediately after birth and then 24-48 hours later to determine serum IgG and calculate the apparent IgG uptake efficiency (ERE). Apparent absorption efficiency is the proportion of consumed IgG that can be recovered in the blood.
26 Holstein calves were fed colostrum in the amount of 8% of their weight within 4.5 hours after birth. Blood samples were taken from the calves immediately after birth and then 24-48 hours later to determine serum IgG and calculate the apparent IgG uptake efficiency (ERE). Apparent absorption efficiency is the proportion of consumed IgG that can be recovered in the blood.
Colostrum pasteurization reduces total bacterial contamination from 4.1 CFU/mL to 1.3. If expressed as a standard value, then the number of bacteria before and after pasteurization was 12,589 and 20 CFU/ml, respectively. Clearly, the colostrum used in the study was very pure and carefully harvested even before pasteurization. Colostrum <100,000 cfu/mL is generally considered acceptable for calf feeding.
The amount of IgG in pasteurized colostrum decreased by almost 10% - from 117.3 to 106.3. Although the loss of IgG was significant, the total amount of IgG in colostrum was still quite high. This study shows that heating colostrum to 60°C for an hour can reduce the concentration of IgG in colostrum. The calves were fed colostrum according to their body weight, so the total amount drunk varied. Since there was less IgG in colostrum after pasteurization, IgG intake in control group (KOH) calves was somewhat lower. However, neither serum IgG nor REP differed in calves, the control group and the PAS group.
The calves were fed colostrum according to their body weight, so the total amount drunk varied. Since there was less IgG in colostrum after pasteurization, IgG intake in control group (KOH) calves was somewhat lower. However, neither serum IgG nor REP differed in calves, the control group and the PAS group.
In this study, pasteurization of colostrum slightly reduced IgG levels and did not increase serum IgG in newborn calves. Why was this data different from other studies in which REP was better after pasteurization? There are several options:
- The colostrum used in this study was very pure. Even before pasteurization, the total bacterial contamination and the number of coliforms were quite low. This suggests that "pure colostrum" (e.g., total bacterial contamination <15,000 CFU/mL and coliform <1,000 CFU/L) did not benefit from pasteurization.
- Preliminary tests with colostrum pasteurization generally used colostrum with a high initial bacterial count.
 In this study, pasteurization did not affect the concentration of serum IgG and REP. In general, calves absorbed enough IgG to be well protected against disease, whether or not colostrum was pasteurized.
In this study, pasteurization did not affect the concentration of serum IgG and REP. In general, calves absorbed enough IgG to be well protected against disease, whether or not colostrum was pasteurized.
Bacterial contamination can markedly affect the ability of calves to absorb IgG from colostrum. However, it turns out that if colostrum is carefully harvested and kept clean, then pasteurization will not be necessary.
translated from dairyherd.com
colostrum, pasteurization, health
Please enable JavaScript to view the comments powered by Disqus.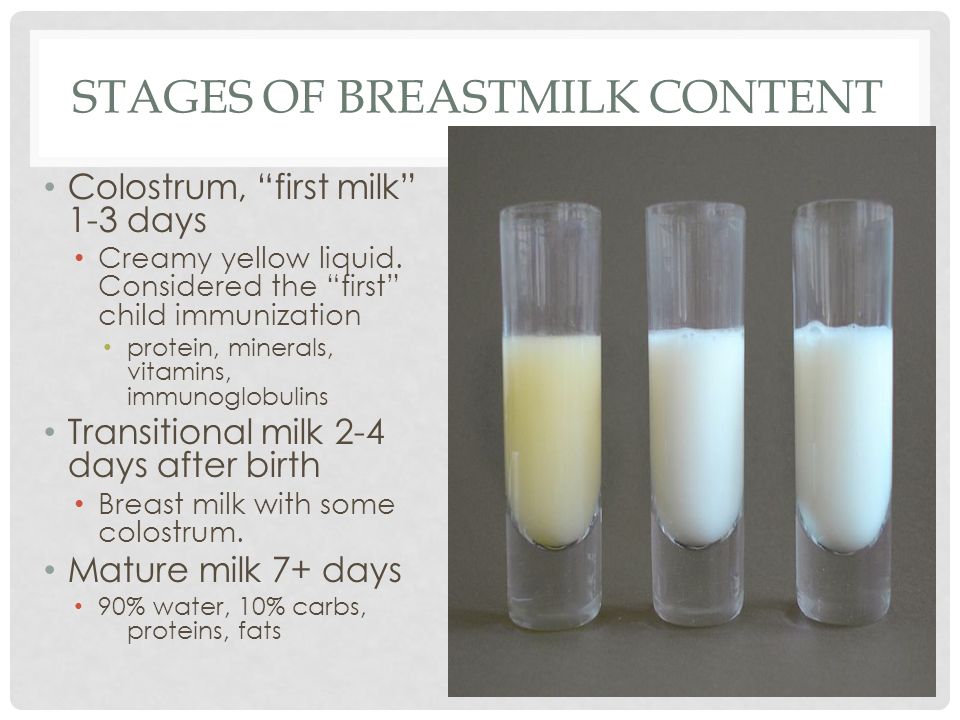 comments powered by Disqus
comments powered by Disqus Rules for the first two months of a calf's life
Author: Anisimova Olga, technical specialist in cattle and horses.
Practices for successfully rearing newborn calves include
- proper feeding organization
- creating comfortable conditions for growth and development
- ensuring proper hygiene
- disease prevention
- permanent surveillance
We tell you what actions need to be taken at each stage of a calf's life up to 2 months of age.
Birth
Immediately after birth, it is necessary to control the breathing of the calf, remove mucus from the mouth and nasal cavity, wipe the calf with a clean towel or straw. If desired, and observing the conditions of hygiene, you can give the calf to be licked by the cow - this has a positive effect on the health of the newborn calf and the cow itself (it stimulates the eating of the feed mixture, promotes the separation of the afterbirth and increases the amount of colostrum). We process the umbilical cord with 5-7% iodine solutions. Be sure to dip the entire remaining cord stump into the solution, a post-milking udder bottle is best suited for this. Next, we weigh and number the calf.
We process the umbilical cord with 5-7% iodine solutions. Be sure to dip the entire remaining cord stump into the solution, a post-milking udder bottle is best suited for this. Next, we weigh and number the calf.
We transport the calf to an individual cage or house with plenty of bedding. The best bedding for newborn calves is dry, clean straw. The amount of this straw should be such that the calf can burrow into it, when he lies down, his elbow joints and nose should be hidden. This will allow the calf to form its own comfortable microclimate inside the house or cage and establish heat exchange for the calf itself. For more complete drying, it is possible to place the calf for an hour in a drying box or under an infrared lamp. At the same time, the drying box should not be hermetically closed and have sufficient ventilation so as not to disturb the heat exchange of the calf. The infrared lamp should be suspended no higher than 80-90 cm from the floor. It is important that the newborn calf cart has a well-disinfected surface, plastic is best for this purpose.
At the time of birth, calves have no resistance to disease. A large number of studies indicate that the survival rate of calves is significantly increased if the calf is placed immediately after birth in a clean and dry environment and fed with quality colostrum within the first hour after birth in a volume of at least 10% of live weight . In addition to its high nutritional value, colostrum provides the newborn calf with the antibodies it needs to protect against many infections that lead to diarrhea and death. According to numerous studies conducted in world practice, 40% of calves do not receive enough immunoglobulins in the colostrum and have an immunoglobulin content in the blood of less than 10-20 g/l.
First drink
Only the first colostrum, obtained from healthy adult cows that are not carriers of infectious diseases and do not have signs of metabolic disorders, is of the highest quality and is most suitable for the first feeding of newborn calves. The density of such colostrum should be at least 1046-1075 units. It is important to milk and freeze colostrum within the first hour after calving, as colostrum quality decreases by 10% every hour. Colostrum antibodies freely penetrate the intestinal walls of the calf only 6-12 hours after birth, and after 36 hours colostrum immunoglobulins are no longer absorbed by the body.
The density of such colostrum should be at least 1046-1075 units. It is important to milk and freeze colostrum within the first hour after calving, as colostrum quality decreases by 10% every hour. Colostrum antibodies freely penetrate the intestinal walls of the calf only 6-12 hours after birth, and after 36 hours colostrum immunoglobulins are no longer absorbed by the body.
The first feeding of a calf is carried out either with freshly milked colostrum of a proven high quality, or thawed from a colostrum bank, collected at the enterprise. The company's colostrum bank is a freezer with special bags or bottles of 1-2 liters of high quality frozen colostrum. The temperature of the freezer is about 18-20 degrees below zero. Packages and bottles must be signed when and from which animal they were received and what density of colostrum. The shelf life of frozen colostrum should not exceed one year. It is necessary to defrost such colostrum at a temperature of 40-50 degrees, make sure that the colostrum is evenly thawed and does not delaminate. Calf feeding with colostrum must be approached individually. It is best if the calf drinks by itself, to drink colostrum from a bottle with a nipple. But not every calf is able to drink the prescribed volume of colostrum. With a large number of calving and to better ensure immunity in newborn calves, it is recommended to use special drains that allow you to force the calf to pour in the required amount of colostrum.
Calf feeding with colostrum must be approached individually. It is best if the calf drinks by itself, to drink colostrum from a bottle with a nipple. But not every calf is able to drink the prescribed volume of colostrum. With a large number of calving and to better ensure immunity in newborn calves, it is recommended to use special drains that allow you to force the calf to pour in the required amount of colostrum.
At the birth of a calf, its digestive system is not fully developed, but it quickly completes its development in the first few months. The digestive system of a calf immediately after birth functions like an animal with a single stomach, since the only fully developed and functioning department is the abomasum. As a result, only liquid feed can be digested by a calf at a few days of age. Further, the task of rearing is to develop and populate the calf rumen as quickly as possible.
Feeding the calf with milk and milk replacer
When feeding calves with milk or milk replacer, the following factors should be taken into account:
- amount of milk
- type of milk dispensed
- feeding frequency
- feeding methods
- milk temperature
The amount of milk drunk per day for a calf and the frequency of feeding is determined by the feeding scheme developed at the enterprise, but it is important to consider: the more milk a calf drinks during the milk period, the more the future cow will give milk during lactation. Modern watering schemes involve feeding calves two or three times a day with equal intervals between feedings. A single amount of milk drunk by a calf is from 1.5 to 4 liters. The duration of the milk period is from 80 to 120 days. The volume of milk drunk during the drinking period varies from 240 to 450 liters per 1 calf.
Modern watering schemes involve feeding calves two or three times a day with equal intervals between feedings. A single amount of milk drunk by a calf is from 1.5 to 4 liters. The duration of the milk period is from 80 to 120 days. The volume of milk drunk during the drinking period varies from 240 to 450 liters per 1 calf.
How and how to feed a calf? Regardless of what we feed the calves with - milk or milk replacer, the watering temperature should be 39-40 degrees. At a temperature below milk clotting slows down, the esophageal trough closes incompletely, and then part of the milk can get into an underdeveloped scar. At higher temperatures, damage to the gastric mucosa occurs. The only exception to the temperature mode of drinking may be fermented milk, which can be drunk at room temperature.
The most physiological food for a calf during this period is whole milk, but it is very expensive. Therefore, farms often use conditionally suitable milk from cows treated with antibiotics and milk from cows less than 5 days after calving. This milk is pasteurized and fed to the calves. It is important to remember that antibiotics found in milk do not decompose when heated, so animals that drink such milk may become resistant to certain types of antibiotics in the future. Whole milk for drinking should be collected in closed tanks and cooled to a temperature of less than 10 degrees, just like commercial milk. Storage of uncooled milk in open containers leads to rapid contamination of milk with pathogenic microflora and the presence of a high concentration of bacteria. Whole milk is a substitute for milk replacer. It is important to ensure that the milk replacer at the beginning of the growing period is of high quality and provides a constant high intake and habituation. It is important that the concentration of the mixture of milk replacer and water should be at least 145 gr. milk replacer per liter of water. Otherwise, the curdling process will not work properly. The quality of milk replacer is indicated by such properties as solubility in water: it should completely, without lumps, immediately dissolve in warm water.
This milk is pasteurized and fed to the calves. It is important to remember that antibiotics found in milk do not decompose when heated, so animals that drink such milk may become resistant to certain types of antibiotics in the future. Whole milk for drinking should be collected in closed tanks and cooled to a temperature of less than 10 degrees, just like commercial milk. Storage of uncooled milk in open containers leads to rapid contamination of milk with pathogenic microflora and the presence of a high concentration of bacteria. Whole milk is a substitute for milk replacer. It is important to ensure that the milk replacer at the beginning of the growing period is of high quality and provides a constant high intake and habituation. It is important that the concentration of the mixture of milk replacer and water should be at least 145 gr. milk replacer per liter of water. Otherwise, the curdling process will not work properly. The quality of milk replacer is indicated by such properties as solubility in water: it should completely, without lumps, immediately dissolve in warm water. And the stability of milk replacer should not delaminate into fractions for at least two hours. These properties indicate the composition of milk replacer, the presence in it of protein sources of animal or vegetable origin. The best sources of milk replacer protein are skimmed milk powder, whey powder. Worse are protein sources from soy protein, egg protein, or protein from animal blood plasma. The requirement for milk replacer crude protein is not less than 20%, crude fat 18-20%, crude fiber 0.15-0.20%, crude ash up to 10%.
And the stability of milk replacer should not delaminate into fractions for at least two hours. These properties indicate the composition of milk replacer, the presence in it of protein sources of animal or vegetable origin. The best sources of milk replacer protein are skimmed milk powder, whey powder. Worse are protein sources from soy protein, egg protein, or protein from animal blood plasma. The requirement for milk replacer crude protein is not less than 20%, crude fat 18-20%, crude fiber 0.15-0.20%, crude ash up to 10%.
Watering is best done from teat buckets throughout the calf's watering period. At the same time, calves drink more slowly, a sufficient amount of saliva is formed, and the esophageal trough reflex is maintained. Proper curdling of milk occurs, large lumps do not form, and milk is better absorbed. The diameter of the nipple opening should be no more than 2-3 mm. The nipple itself should be at a height of no more than 80 cm from the floor of the cage.
Feeding the calf with roughage
The calf must be provided with water from the first day of life 24 hours a day. The water temperature is 18-20 degrees. It is necessary to change the water 2 times a day in winter, in summer it is recommended to do this more often - up to 4 times a day. Water stimulates starter feed intake and promotes rumen bacteria growth.
The water temperature is 18-20 degrees. It is necessary to change the water 2 times a day in winter, in summer it is recommended to do this more often - up to 4 times a day. Water stimulates starter feed intake and promotes rumen bacteria growth.
When grain particles of feed enter the rumen, microflora settles in it, which processes grain carbohydrates into volatile fatty acids. VFAs contribute to the growth and development of scar papillae. A large number of scar papillae increase the ability of the scar to absorb nutrients. For faster and more complete development of the rumen, starter feeds must be given to the calf from the 3rd day of life. Starter feeds should have good palatability and high digestibility. Crude protein content should be 19.5-20.5%, the best source of protein for calves is soybean meal. The content of crude fiber should be at least 4.5%, but not more than 10%. Crude fat 3-4%, crude ash content should not exceed 10%. For better development of rumen papillae, whole grain corn can be mixed with starter feeds in an amount of 20% of the feed volume. Access to compound feed should be constant, they should always be clean and fresh. It is impossible to allow stagnation and molding of feed in the feeders. During the first 6 weeks, calf weight gain is 75% dependent on starter intake, by 3 months of age the calf should consume 1-1.5 kg of starter. Teaching calves to consume roughage starts at 3 weeks of age. Roughage performs the function of developing and increasing the capacity of the rumen. If hay is given to calves, it must be of the best quality. One kilogram of such hay should contain at least 10 MJ of energy, 12-14% of crude protein and no more than 25% fiber. You can introduce a complete feed mixture from high-yielding cows into the diet of calves, this will allow you to get used to the taste of the feed mixture, at weaning it will reduce stress and leave familiar feeds available. This will increase feed intake immediately after weaning. If the calf has adapted normally to the consumption of roughage, its development rate and body weight should constantly increase.
Keeping calves up to 2 months
Up to 1.5-2 months of age, calves are kept in individual cages in a calf barn, or in individual houses in open areas. Individual housing reduces the risk of infection of calves from each other with various diseases. Provides an individual approach to each calf. Individual houses are installed facing south, with a slope of 3-5 degrees on a hard-surface site. A prerequisite is a deep (dry) straw bedding. When a calf is transferred to an individual house, a natural process of self-regulation is activated already during the first day. In hot summer time, it is necessary to monitor the presence of ventilation in the house. It is best to equip sites where individual houses are installed with a special canopy to reduce the penetration of sunlight in summer and protection from snow in winter.
When keeping calves in a calf barn, it is necessary to ensure air exchange there. Air exchange at the level of the nose of a calf in an individual cage in winter is up to 6 times air change per hour, in summer the need for air exchange increases 10 times and reaches 60 air changes per hour.