Indigestion with headache
What's the link, prevention, treatment
Acid reflux is when a person’s stomach contents flow back into their esophagus. Certain people who have acid reflux experience headaches or migraine.
Acid reflux can be a symptom of gastroesophageal reflux (GER). GER can cause symptoms such as heartburn or regurgitation. If a person has frequent and severe episodes of GER, they may have gastroesophageal reflux disease (GERD).
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) notes that around 20% of people in the United States have GERD.
A person who has GERD may also experience headaches or migraine. A review from 2016 found that people with headaches or migraine can have reflux symptoms.
Read on to learn more about the connection between GER and headaches, as well as symptoms, treatments, and prevention.
There is currently limited information on how or why acid reflux can cause a person to have headaches. Additionally, researchers are unsure whether acid reflux causes headaches or if headaches cause acid reflux.
It is also possible that acid reflux and headaches can simply occur together without one causing the other. There may also be certain conditions that have both headache and acid reflux as symptoms.
Current research
What researchers do know is that a person’s brain has a connection to their gut via the gut-brain axis.
The gut-brain axis allows the gut and the brain to communicate with each other. Additionally, the gut-brain axis links a person’s gut to their autonomic nervous system (ANS).
A person’s ANS deals with involuntary processes, such as respiration and digestion. The ANS contains three divisions:
- Sympathetic nervous system (SNS): The SNS is in charge of a person’s “fight or flight” response. This is the body’s automatic reaction to threats.
- Parasympathetic nervous system (PNS): The PNS controls a person’s “rest and digest” response. This response relaxes the body once the threat has passed.
- Enteric nervous system (ENS): The ENS regulates certain digestive functions, such as muscle contractions and secretions.
A study from 2017 noted that there is a link between ANS dysfunction, headaches, and gastrointestinal (GI) disorders.
Another study from 2015 stated that GERD associates with impaired PNS function. This means that the link between GERD and headaches may be caused by a malfunctioning ANS.
There may also be a link between glutamate, GERD, and migraine. Glutamate is a neurotransmitter, which is a chemical that passes on signals from nerve cells to target cells.
Research from 2020 found that issues with glutamate levels, or transmission, can lead to GER or migraine headaches.
Currently, there is limited research regarding the link between GERD and headaches.
Studies indicate that GERD and headaches could be co-occurring symptoms of certain conditions or imbalances within the body.
However, researchers believe that that may be a link between proton pump inhibitors (PPIs) and headaches.
Doctors use PPIs to treat certain gastric conditions, such as GERD or gastritis. A person taking PPIs to treat their GERD could potentially develop headaches as a result, although more research is needed to confirm this effect.
A person taking PPIs to treat their GERD could potentially develop headaches as a result, although more research is needed to confirm this effect.
Researchers believe that there may be a link between acid reflux and dizziness.
Research from 2015 noted that within a study group of 153 patients, peripheral vertigo was more common among those who had GERD, compared with those who did not. However, further research is required to explore why this might have been the case.
Peripheral vertigo occurs due to a problem inside a person’s inner ear. Peripheral vertigo can cause:
- dizziness
- spinning sensation
- loss of hearing in one ear
- ringing in one or both ears
- difficulty focusing eyes
- loss of balance
The authors of the study mentioned above theorize that a possible cause of peripheral vertigo is stomach acid moving up the throat and into the Eustachian tubes. However, it is important to note that this is only a theory and has not been scientifically proven.
The Eustachian tubes are small passages that connect a person’s throat to their middle ear. The Eustachian tubes pass through a person’s inner ear, which contains fluid and sensors that help a person maintain their balance.
According to the researchers’ theory, disruption to the inner ear due to stomach acid moving through the Eustachian tubes may cause peripheral vertigo symptoms. Again, more research is needed to test this theory.
Dizziness may occur due to shortness of breath caused by GERD. Reflux can cause inflammation and irritation of a person’s airways, which may lead to shortness of breath. If a person is unable to take in enough oxygen, they may feel dizzy.
Headaches can also cause a person to feel dizzy. The American Migraine Foundation notes that between 30–50% of people who experience migraine also have dizziness or loss of balance.
These latter two factors could potentially lead to the occurrence of acid reflux, headaches, and dizziness alongside each other.
GERD symptoms can make it difficult for a person to fall asleep. If a person is unable to sleep properly, they may become fatigued.
When a person is sitting or standing, their stomach contents are at the bottom of their stomach. However, when a person lies down, their stomach contents may travel back into their esophagus.
Information from the International Foundation for Gastrointestinal Disorders (IFFGD) states that up to 4 out of 5 people with GERD have nighttime symptoms. Additionally, 75% of people who had heartburn as a symptom stated that it affected their sleep.
Research from 2017 found that there was a link between tension headaches and lack of sleep. This connection worked both ways, with sleep deprivation causing headache and headache causing sleep deprivation.
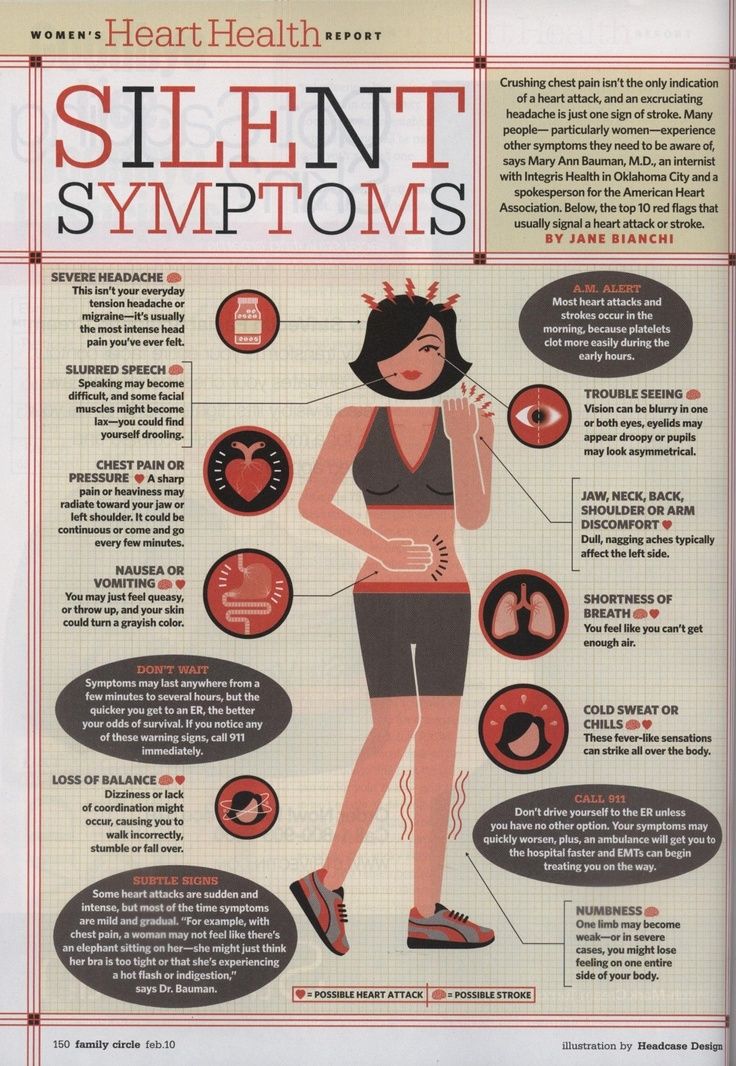
Acid reflux can cause symptoms such as:
- chest pain
- nausea
- difficulty swallowing
- pain when swallowing
- symptoms of additional complications, such as chronic cough or hoarseness
Current research does not mention specific symptoms of headaches that occur alongside GERD.
Since the relationship between acid reflux and headaches is not yet known, it is hard to know how it can be treated.
If a link does exist between reflux and headaches, treating reflux symptoms may also result in headache relief. However, further research is required to confirm this.
According to the United Kingdom’s National Health Service (NHS), the following can be treatments for acid reflux:
- eat smaller, more regular meals
- try and lose excess weight if a person has obesity
- try and find ways to relax
- elevate the head and chest when sleeping
- antacids
- PPIs
Remedies for headaches can include:
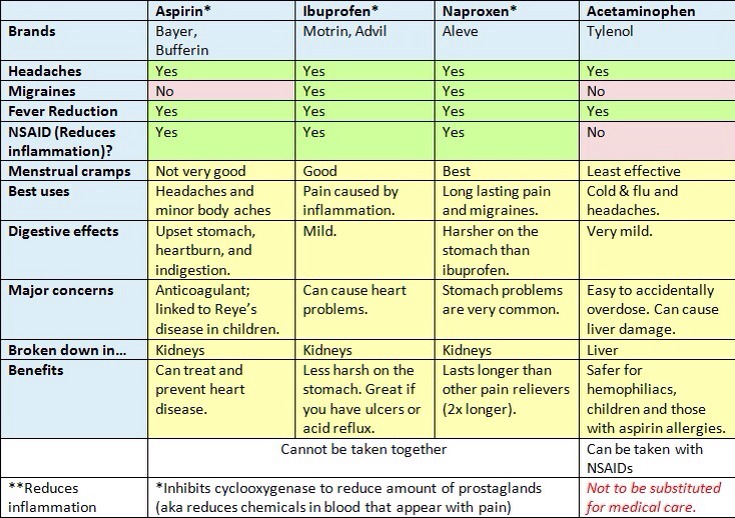
- pain medication
- drinking water
- rest
If there is a link between headaches and GERD, a person may have headache relief by treating their GERD symptoms.
Treatments for GERD include:
Medications
There is a variety of over the counter and prescription drugs that can help with GERD and headache symptoms, such as:
- antacids, which help relieve mild GERD symptoms
- h3 blockers, which reduce stomach acid production
- PPIs, which reduce stomach acid levels
Surgery
A doctor may recommend surgery if a person’s GERD does not respond to treatment or lifestyle changes.
Surgery for GERD includes:
- fundoplication, a procedure where a surgeon wraps the top of a person’s stomach around their lower esophagus to increase pressure and reduce reflux
- weight loss surgery
- endoscopy, which is when a surgeon inserts a tube with a camera attached into a person’s throat to examine their esophagus and stomach
If a link does exist between headaches and GERD, a person may benefit from preventing or reducing their GERD symptoms. However, there is currently no scientific evidence for this.
Avoiding certain foods
A person who has GERD should limit or avoid foods that trigger their symptoms. Food and drinks that research has associated with GERD include:
- acidic foods, such as citrus fruits
- alcohol
- chocolate
- coffee
- caffeine
- high fat food
- mint
- spicy foods
The NIDDK suggests that people who have GERD when lying down do not eat for at least 3 hours before sleeping.
Routine adjustments
There are various changes a person can make in their daily routines to help improve their GERD symptoms, such as:
- losing weight if a person has obesity
- elevating the head during sleep by 6–8 inches
- quitting smoking
A person should speak with their doctor if they have GERD symptoms and headache that does not go away with treatment.
Additionally, a person should see a doctor if they develop complications such as:
- chest pain
- loss of appetite
- persistent vomiting
- difficulty or pain while swallowing
- vomit that contains blood or resembles coffee grounds
- stool that contains blood or is black and tarry
- unexplained weight loss
Acid reflux can occur alongside headaches. However, researchers do not know the nature of the link between these conditions. One theory is that problems with a person’s ANS or glutamate levels may link acid reflux and headaches.
GERD and headaches may cause a person to experience fatigue or dizziness.
There are various treatments and lifestyle changes a person can use to treat GERD or acid reflux. If these do not work, a person can speak with their doctor about surgery.
A person should speak with their doctor if they have GERD alongside any serious symptoms.
What's the link, prevention, treatment
Acid reflux is when a person’s stomach contents flow back into their esophagus. Certain people who have acid reflux experience headaches or migraine.
Acid reflux can be a symptom of gastroesophageal reflux (GER). GER can cause symptoms such as heartburn or regurgitation. If a person has frequent and severe episodes of GER, they may have gastroesophageal reflux disease (GERD).
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) notes that around 20% of people in the United States have GERD.
A person who has GERD may also experience headaches or migraine. A review from 2016 found that people with headaches or migraine can have reflux symptoms.
A review from 2016 found that people with headaches or migraine can have reflux symptoms.
Read on to learn more about the connection between GER and headaches, as well as symptoms, treatments, and prevention.
There is currently limited information on how or why acid reflux can cause a person to have headaches. Additionally, researchers are unsure whether acid reflux causes headaches or if headaches cause acid reflux.
It is also possible that acid reflux and headaches can simply occur together without one causing the other. There may also be certain conditions that have both headache and acid reflux as symptoms.
Current research
What researchers do know is that a person’s brain has a connection to their gut via the gut-brain axis.
The gut-brain axis allows the gut and the brain to communicate with each other. Additionally, the gut-brain axis links a person’s gut to their autonomic nervous system (ANS).
A person’s ANS deals with involuntary processes, such as respiration and digestion. The ANS contains three divisions:
The ANS contains three divisions:
- Sympathetic nervous system (SNS): The SNS is in charge of a person’s “fight or flight” response. This is the body’s automatic reaction to threats.
- Parasympathetic nervous system (PNS): The PNS controls a person’s “rest and digest” response. This response relaxes the body once the threat has passed.
- Enteric nervous system (ENS): The ENS regulates certain digestive functions, such as muscle contractions and secretions.
A study from 2017 noted that there is a link between ANS dysfunction, headaches, and gastrointestinal (GI) disorders.
Another study from 2015 stated that GERD associates with impaired PNS function. This means that the link between GERD and headaches may be caused by a malfunctioning ANS.
There may also be a link between glutamate, GERD, and migraine. Glutamate is a neurotransmitter, which is a chemical that passes on signals from nerve cells to target cells.
Research from 2020 found that issues with glutamate levels, or transmission, can lead to GER or migraine headaches.
Currently, there is limited research regarding the link between GERD and headaches.
Studies indicate that GERD and headaches could be co-occurring symptoms of certain conditions or imbalances within the body.
However, researchers believe that that may be a link between proton pump inhibitors (PPIs) and headaches.
Doctors use PPIs to treat certain gastric conditions, such as GERD or gastritis. A person taking PPIs to treat their GERD could potentially develop headaches as a result, although more research is needed to confirm this effect.
Researchers believe that there may be a link between acid reflux and dizziness.
Research from 2015 noted that within a study group of 153 patients, peripheral vertigo was more common among those who had GERD, compared with those who did not. However, further research is required to explore why this might have been the case.
Peripheral vertigo occurs due to a problem inside a person’s inner ear. Peripheral vertigo can cause:
- dizziness
- spinning sensation
- loss of hearing in one ear
- ringing in one or both ears
- difficulty focusing eyes
- loss of balance
The authors of the study mentioned above theorize that a possible cause of peripheral vertigo is stomach acid moving up the throat and into the Eustachian tubes. However, it is important to note that this is only a theory and has not been scientifically proven.
The Eustachian tubes are small passages that connect a person’s throat to their middle ear. The Eustachian tubes pass through a person’s inner ear, which contains fluid and sensors that help a person maintain their balance.
According to the researchers’ theory, disruption to the inner ear due to stomach acid moving through the Eustachian tubes may cause peripheral vertigo symptoms. Again, more research is needed to test this theory.
Dizziness may occur due to shortness of breath caused by GERD. Reflux can cause inflammation and irritation of a person’s airways, which may lead to shortness of breath. If a person is unable to take in enough oxygen, they may feel dizzy.
Headaches can also cause a person to feel dizzy. The American Migraine Foundation notes that between 30–50% of people who experience migraine also have dizziness or loss of balance.
These latter two factors could potentially lead to the occurrence of acid reflux, headaches, and dizziness alongside each other.
GERD symptoms can make it difficult for a person to fall asleep. If a person is unable to sleep properly, they may become fatigued.
When a person is sitting or standing, their stomach contents are at the bottom of their stomach. However, when a person lies down, their stomach contents may travel back into their esophagus.
Information from the International Foundation for Gastrointestinal Disorders (IFFGD) states that up to 4 out of 5 people with GERD have nighttime symptoms. Additionally, 75% of people who had heartburn as a symptom stated that it affected their sleep.
Research from 2017 found that there was a link between tension headaches and lack of sleep. This connection worked both ways, with sleep deprivation causing headache and headache causing sleep deprivation.
Acid reflux can cause symptoms such as:
- chest pain
- nausea
- difficulty swallowing
- pain when swallowing
- symptoms of additional complications, such as chronic cough or hoarseness
Current research does not mention specific symptoms of headaches that occur alongside GERD.
Since the relationship between acid reflux and headaches is not yet known, it is hard to know how it can be treated.
If a link does exist between reflux and headaches, treating reflux symptoms may also result in headache relief. However, further research is required to confirm this.
According to the United Kingdom’s National Health Service (NHS), the following can be treatments for acid reflux:
- eat smaller, more regular meals
- try and lose excess weight if a person has obesity
- try and find ways to relax
- elevate the head and chest when sleeping
- antacids
- PPIs
Remedies for headaches can include:
- pain medication
- drinking water
- rest
If there is a link between headaches and GERD, a person may have headache relief by treating their GERD symptoms.
Treatments for GERD include:
Medications
There is a variety of over the counter and prescription drugs that can help with GERD and headache symptoms, such as:
- antacids, which help relieve mild GERD symptoms
- h3 blockers, which reduce stomach acid production
- PPIs, which reduce stomach acid levels
Surgery
A doctor may recommend surgery if a person’s GERD does not respond to treatment or lifestyle changes.
Surgery for GERD includes:
- fundoplication, a procedure where a surgeon wraps the top of a person’s stomach around their lower esophagus to increase pressure and reduce reflux
- weight loss surgery
- endoscopy, which is when a surgeon inserts a tube with a camera attached into a person’s throat to examine their esophagus and stomach
If a link does exist between headaches and GERD, a person may benefit from preventing or reducing their GERD symptoms. However, there is currently no scientific evidence for this.
Avoiding certain foods
A person who has GERD should limit or avoid foods that trigger their symptoms. Food and drinks that research has associated with GERD include:
- acidic foods, such as citrus fruits
- alcohol
- chocolate
- coffee
- caffeine
- high fat food
- mint
- spicy foods
The NIDDK suggests that people who have GERD when lying down do not eat for at least 3 hours before sleeping.
Routine adjustments
There are various changes a person can make in their daily routines to help improve their GERD symptoms, such as:
- losing weight if a person has obesity
- elevating the head during sleep by 6–8 inches
- quitting smoking
A person should speak with their doctor if they have GERD symptoms and headache that does not go away with treatment.
Additionally, a person should see a doctor if they develop complications such as:
- chest pain
- loss of appetite
- persistent vomiting
- difficulty or pain while swallowing
- vomit that contains blood or resembles coffee grounds
- stool that contains blood or is black and tarry
- unexplained weight loss
Acid reflux can occur alongside headaches. However, researchers do not know the nature of the link between these conditions. One theory is that problems with a person’s ANS or glutamate levels may link acid reflux and headaches.
However, researchers do not know the nature of the link between these conditions. One theory is that problems with a person’s ANS or glutamate levels may link acid reflux and headaches.
GERD and headaches may cause a person to experience fatigue or dizziness.
There are various treatments and lifestyle changes a person can use to treat GERD or acid reflux. If these do not work, a person can speak with their doctor about surgery.
A person should speak with their doctor if they have GERD alongside any serious symptoms.
Headaches in diseases of the gastrointestinal tract / Blog / Clinic EXPERT
Chkalovskaya
St. Pionerskaya, 63
+7 (812) 426-35-35+7 (921) 587-81-81
+7 (812)-42 35
Zinovieva Evgenia Nikolaevna
Chief physician, internist, gastroenterologist, hepatologist of the highest category, candidate of medical sciences, associate professor
About the doctor
Cover Maria Viktorovna
Psychiatrist, psychotherapist, Ph. D. 11 February 2020
D. 11 February 2020
Headaches in diseases of the gastrointestinal tract
Complaints of headache (cephalgia) do not have a direct or independent significance in diseases of the gastrointestinal tract (GIT), but they reflect the severity of the problem as a whole.
It is extremely important to conduct a differential diagnosis of the causes of this pain. In the Expert clinic, not only gastroenterologists, but cardiologists and neurologists work on solving such problems.
What are the main causes of the combination of gastrointestinal diseases and headaches?
- The manifestations of functional disorders (gastric dyspepsia) can begin in childhood with irregular and malnutrition. In the case of a long period of fasting or dry food, a headache may subsequently occur as a signal from the body that there is no replenishment of the necessary substances and fluids.
- In diseases of the gastrointestinal tract, accompanied by pain and frequent stools at night, it can disrupt the physiological rhythm of sleep, which can lead to overwork, lack of adequate rest and, as a result, to headache.

- On the other hand, with prolonged diarrhea, dehydration develops with a loss of blood electrolytes, which can also lead to headache due to a violation of systemic balance - homeostasis.
- The presence of persistent constipation leads to intoxication, as well as any food poisoning, which is manifested by a headache.
- Repeated vomiting in intestinal dyspepsia or pancreatitis may, by increasing intra-abdominal pressure, lead to an increase in systemic arterial pressure, causing headache.
- Severe diseases of the gastrointestinal tract, characterized by severe inflammation of various nature (viral, bacterial, autoimmune, parasitic) can also give systemic manifestations, including headache, as an indicator of intoxication.
Parallel existing conditions are not excluded - comorbidity. When one patient has several directly unrelated diseases (pathology of the gastrointestinal tract, diseases of the cardiovascular and neurological profile). Only a thorough collection of complaints, anamnesis and an objective examination can help to place the right emphasis and prescribe the right treatment: eliminate intoxication (a state of poisoning), treat the underlying disease that led to it, and also exclude or confirm various groups of vascular diseases, both arteries and veins, pathologies of the spine, which can cause persistent headaches.
Only a thorough collection of complaints, anamnesis and an objective examination can help to place the right emphasis and prescribe the right treatment: eliminate intoxication (a state of poisoning), treat the underlying disease that led to it, and also exclude or confirm various groups of vascular diseases, both arteries and veins, pathologies of the spine, which can cause persistent headaches.
Headache, gastritis and immunodeficiency Medical On Group St. Petersburg
Headache, gastritis and immunodeficiency... You might be surprised by this combination of diseases, but they have more in common than you might think.
Whatever they write on the Internet about the causes of headaches: increased intracranial pressure, and cervical osteochondrosis, and brain tumors, and problems with blood vessels, and even intolerance to cheeses or nitrates. In fact, these are probably the rarest causes of its occurrence.
The accumulation of excess fluid around the brain is a potentially dangerous condition, and it occurs in no more than 0.01% of people. Pain with increased intracranial pressure is daily and intensifies when lying down, this does not creep up suddenly, and you don’t need to think about it with periodic discomfort.
Hernias and protrusions of the spine cause pain only in 4% of cases, and even if you have them, this is not a reason to blame them for the pain. It has been unambiguously proven that people with and without them have headaches equally often.
The notorious osteochondrosis is not even a disease, but a manifestation of the natural withering of the body, and over time (by the age of forty) appears in everyone. But not all the older half of the people in the world suffer from this.
Brain tumors do not hurt, except in the last stages, when they start to put pressure on something. But at this point, many other symptoms will appear (impaired perception, gait, speech), so you should not think about cancer with a headache at all, unless you are an elderly person who has suddenly and greatly lost weight.
The only thing that can be said about vascular disorders is that the obstruction of the blood supply to the brain does not lead to pain, at most to fainting and a decrease in mental abilities. The only exception is a hemorrhagic stroke (including from an aneurysm rupture), but here it’s not a headache that will alert you, but a lack of coordination of movements and slurred speech.
It has recently become fashionable to attribute headaches to food intolerances as the cause. The list of possible provocateurs includes all the most delicious things: from cheese and fruits to olives and bacon. Of course, there are individual food allergic reactions, but then the cause is still the gastritis itself, and not the allergy itself.
And so we come to the more common, though less "obvious" causes of headaches, which include gastritis, dehydration, infections, eye strain, and emotional stress.
Gastritis
With gastritis, 27% of people, even without complaints about the stomach, experience a headache, especially if they forget to eat on time. Sometimes a headache is the only symptom that points to an ulcer. When digestion is disturbed, the stomach starts a mechanism aimed at finding food. Signals amplified by inflammation “overstrain” the brain, and the head begins to hurt. By the way, hunger itself (low blood sugar) can cause a headache by the same mechanism. The paradox is that an increased level of sugar can create similar inconveniences for a person due to an increase in adrenaline and norepinephrine after a hearty meal. In general, eat in moderation.
Sometimes a headache is the only symptom that points to an ulcer. When digestion is disturbed, the stomach starts a mechanism aimed at finding food. Signals amplified by inflammation “overstrain” the brain, and the head begins to hurt. By the way, hunger itself (low blood sugar) can cause a headache by the same mechanism. The paradox is that an increased level of sugar can create similar inconveniences for a person due to an increase in adrenaline and norepinephrine after a hearty meal. In general, eat in moderation.
What does a person with a headache do? He takes painkillers, which, by an unfortunate coincidence, themselves cause gastritis. Paracetamol, analgin, ibuprofen, celecoxib, ketanol, diclofenac, nimesulide - they all irritate the gastric mucosa and increase acid production, although ibuprofen is the most relatively safe in this matter. And here you can meet another paradox: taking painkillers can cause pain in the head (this is in the instructions). This happens because this is how the vicious circle of "headache - painkiller - gastritis - headache" closes.
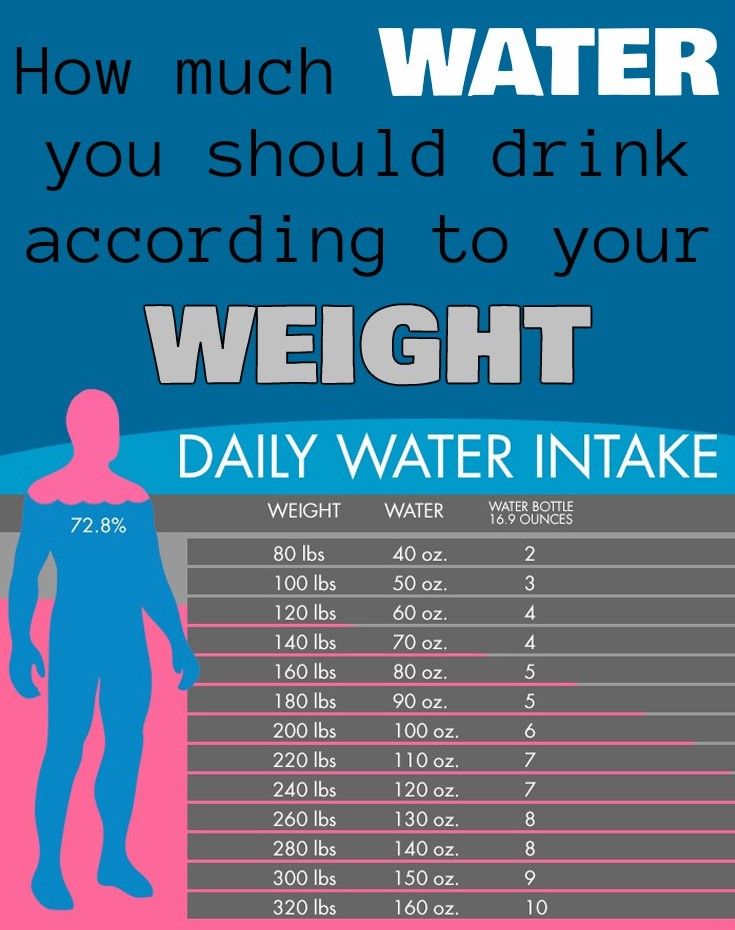
Dehydration
Who does not drink coffee at work, he drinks tea. And he does it right. Coffee is a diuretic drink, but we perceive it as a consumed liquid and do not notice creeping dehydration. Although it would be worth considering why in many cafes, along with espresso, they immediately bring you a glass of water. The same goes for beer, about the need for a restroom after which everyone knows. In addition, most of the working population snacks on something fatty (sandwiches with cheese or sausage, nuts, chocolate), and more water is required to break down fats. And it’s not even about the sensational “need for 2 liters a day” - it is actually different not only for different people, but also for the same person on different days. The point is the ratio of consumed and wasted moisture. When breathing and sweating in a dry climate (as in our apartments during the heating season), more water is required than on a cool summer evening on the seashore. It is curious that you always want to drink after taking a shower, where everything seems to be in order with humidity. It’s just that in hot water we still sweat a lot, but the sweat is immediately washed off and does not help the body to cool down; the body tries to produce more and more sweat, losing more and more moisture, leading to dehydration and post-bath headaches.
It’s just that in hot water we still sweat a lot, but the sweat is immediately washed off and does not help the body to cool down; the body tries to produce more and more sweat, losing more and more moisture, leading to dehydration and post-bath headaches.
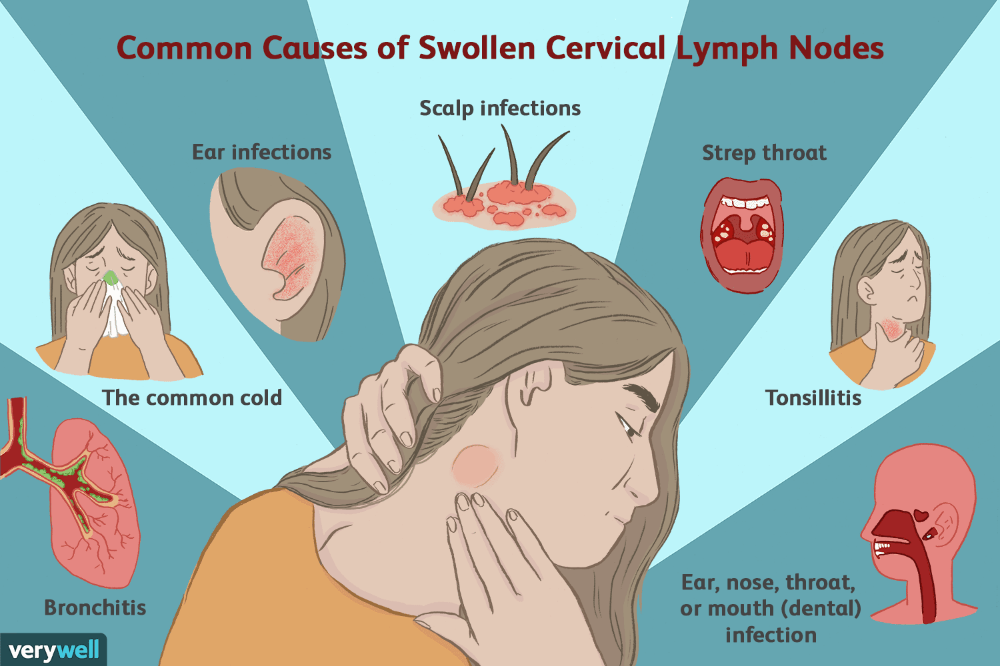
Infections
If it hurts from behind, everyone will suspect the neck, and if it hurts from the front, it is logical to think about the nose. More precisely, the sinuses of the nose are frontal (in the forehead), maxillary (under the eyes) and ethmoid (deep behind the nose). When the mucous membrane of the sinuses swells, the outflow from them deteriorates, and this is felt as a bursting pain in the head. In this case, a runny nose may not be at all, as well as other manifestations of a cold. Similarly, an ear infection begins - only a headache, although hearing loss or congestion, as in an airplane, with swelling of the Eustachian tube, may join. But it's not just about swelling of the sinuses or ear canals. An infection that has settled in a chronic way in your nose or anywhere else is bacteria and viruses, the particles of which are toxins for us. As a result, any chronic infectious disease is a source of constant intoxication, and it makes your head hurt.
As a result, any chronic infectious disease is a source of constant intoxication, and it makes your head hurt.
Eye strain
Since childhood, mothers have been telling all of us: “Do not sit in front of the screen for a long time, you will plant your eyesight.” And then, at work, most people got monitors that you just need to look at for a long time. Eye strain has become invisible due to the daily use of smartphones, tablets and laptops. It is difficult for the brain to imagine that something permanent can be harmful (as with the atmospheric air that we breathe, usually without thinking about the exhaust gases in it). And the constant load on the eye muscles without refocusing leads to eye pain, which we can perceive as a headache. Of course, in the process of peering into the depths of the screen, we do not notice the overstrain of the neck muscles, but true neck pain occurs in only 1% of cases and it is associated with subluxation of the vertebra, and this is a completely different story.
Surprisingly, not all people with poor eyesight are aware of their inferiority, and not everyone starts wearing glasses in time. The principle of a headache with uncorrected myopia or suddenly creeping farsightedness is the same: overstrain of the eye muscles. You should also visit an ophthalmologist to rule out glaucoma, a disease with increased intraocular pressure, which also makes you reach for painkillers.
Emotional stress
“I already have a headache from this whole situation” is a typical expression. Yes, stress is the favorite cause of headaches, tension pains. The mechanisms of chronic headache in anxiety-depressive disorder, which manifests itself to one degree or another in half of the people in the Western world, have long been described. (Where to go, retribution for the race of progress with its frantic pace of life, constant lack of sleep, scandalous bosses and deadlines). In short, stress is excess arousal running around in a circle in a certain area of the brain. This zone is constantly active and cannot “rest”, neurons do not have time to get rid of decay products and send a signal for help in the form of pain and anxiety. If stress becomes chronic, then the receptors on nerve cells are rearranged, as a result of which the exchange of neurotransmitters is disrupted and depression develops. And one of the masks of depression (a link to my “why it hurts”) is just a headache.
This zone is constantly active and cannot “rest”, neurons do not have time to get rid of decay products and send a signal for help in the form of pain and anxiety. If stress becomes chronic, then the receptors on nerve cells are rearranged, as a result of which the exchange of neurotransmitters is disrupted and depression develops. And one of the masks of depression (a link to my “why it hurts”) is just a headache.
A separate discussion about migraine, a severe unilateral throbbing headache accompanied by nausea, intolerance to bright light and strong odors, preceded by a migraine aura (repetitive unusual visual effects). Migraine attacks turn off performance, and should be treated by a neurologist without any self-medication.
What NOT to do for headaches (unless, of course, a neurologist referred you):
- MRI of the brain - completely different symptoms indicate cancer, and not pain at all, so what should we look for there?
- MRI of the neck - even if there are protrusions and hernias, this will not say anything about the cause of the pain and will not affect the treatment in any way.
- Ultrasound of the vessels of the neck is not necessary if you do not faint. This study is prescribed by cardiologists to assess atherosclerosis, headache has nothing to do with it.
- EEG is an old method, effective for detecting only epilepsy. Popular only because of its price, when you need to "assign something."
How to get examined if your head often bothers you:
- Go to a neurologist: he is the “pain chief”, during the examination he will immediately (usually even without additional examinations) tell you about the causes of your illness and prescribe treatment.
- See an ophthalmologist: Glaucoma and blurred vision are common causes of headaches. It will also eliminate the swelling of the fundus, and you will be sure that everything is in order with your intracranial pressure.
- Make FGDS (gastroscopy): almost everyone has digestive problems, and, if cured in time, they will not create complications, including a headache.

- Donate blood for clinical analysis, check immunity and do cultures from the intestines, from the tonsils and the reproductive system to exclude chronic infections.
- Control of blood pressure: a cardiologist or therapist will help you do this, if necessary, directing you to daily monitoring of pressure.
- Consult a psychotherapist: if stress is constant and has already begun to affect health, it is better not to delay it and learn how to deal with it in time before it develops into something more serious.
- And you also need to exclude the simplest possible causes - annoying spirits of your neighbor, an uncomfortable sofa for sleeping, or even clips that press on your ears. Sometimes it happens "and the casket just opened."
Pain is an important signal, and despite the fact that 9 out of 10 times the head hurts “by itself”, from overexertion, in 10% of cases, pain can indicate the presence of a problem that can be dangerous to ignore.