Human milk line
Extra (supernumerary or accessory) nipples or breast tissue • KellyMom.com
by Kelly Bonyata, BS, IBCLC
Extra nipples or breast tissue is fairly common (1-6% of women) and is a result of incomplete regression of the mammary ridge (milk line) during the development of the embryo before birth.
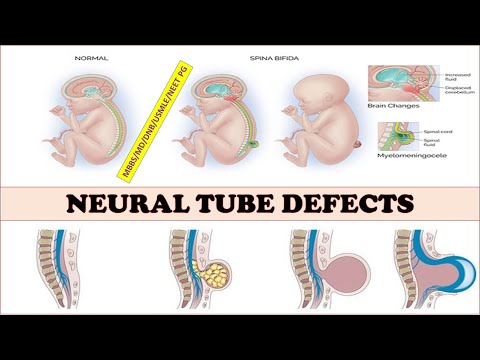
What causes this? Extra breast tissue is a common developmental variation in human anatomy. Breast development begins around week four of gestation, with two parallel lines of glandular tissue called the milk line (or mammary ridge) extending from slightly beyond the underarm area, down the chest and abdomen, to the groin area and ending near the groin at the inner sides of the thighs (see figure). Breasts eventually develop from these lines of tissue, and the remaining tissue regresses. Occasionally, there is an incomplete regression of the mammary ridge during embryo development, and extra (supernumerary) nipples and/or breast tissue forms, usually along this line but occasionally in other parts of the body. This can occur in both males and females. An extra nipple, areola, and/or glandular tissue may be present anywhere along this line (a nipple without glandular tissue is most common), and it is not at all unusual to have more than one.
What is typical when it comes to extra breast tissue? The term hypermastia (or polymastia, or ectopic breast tissue) refers to the presence of accessory mammary tissue in addition to the two main glands. It can occur in a number of different forms. Some examples include:
Now infants can get
all their vitamin D
from their mothers’ milk;
no drops needed with
our sponsor's
TheraNatal Lactation Complete
by THERALOGIX. Use PRC code “KELLY” for a special discount!
- breast tissue with a nipple and areola
- breast tissue with a nipple but no areola
- breast tissue without a nipple (hyperadenia)
- nipple without glandular tissue (hyperthelia or polythelia)
- areola without nipple or glandular tissue
- an ectopic milk duct that leaks milk through the skin without visible breast tissue or nipple
Extra nipples usually occur right below the breasts or in the underarm area, and extra mammary tissue is usually located in the underarm area. Most studies show extra nipples to be more common in males, and they can sometimes run in families.
Most studies show extra nipples to be more common in males, and they can sometimes run in families.
Accessory, or supernumerary, breast tissue is not functionally connected to the breast at all, even though it may be near the breast, in the underarm area or anywhere else along the milk line. This is different than the breast tissue that normally extends into the underarm area, called the Tail of Spence (see figure), which is connected to the main ductal system of the breast.
What does it look like? Accessory breast tissue can appear as a complete breast if both a nipple, areola, and glandular tissue are present. If mammary tissue without a nipple or areola is present, it may appear as a lump or swelling under the skin. An accessory nipple may look like a freckle, a mole or a dimple, or it may look like a typical nipple (though it is usually smaller). Often, accessory nipples or breast tissue are not noticed until hormonal changes make them more apparent. Sometimes a new mom will not know she has accessory breast tissue until she notices milk dripping from a “freckle” or pore in the skin.
Sometimes a new mom will not know she has accessory breast tissue until she notices milk dripping from a “freckle” or pore in the skin.
What happens during pregnancy & lactation? The hormonal changes during pregnancy and lactation can cause accessory breast tissue to increase in size and/or produce milk. You may also experience fluctuating swelling and/or tenderness (this may also occur during adolescence and/or menstruation). Accessory nipples and areolas may darken. If you experience skin irritation when clothing rubs against an accessory nipple, try covering it with a bandaid or gauze.
As with any breast tissue, accessory breast tissue can become engorged at the beginning of lactation, and may leak milk. Accessory breast tissue does not typically produce much milk, and does not interfere with breastfeeding. The usual methods for easing engorgement can be helpful. If the extra breast tissue is not drained by a ductal system (so that no milk can leak or be expressed), comfort measures such as cold compresses can help until the extra tissue involutes and stops producing milk. Mothers with leaking milk from accessory nipples have found that a breast pad or sometimes just a bandaid can be effective for catching leaks. As with any leaking, applying pressure straight in toward the chest may help stop the leaking.
Mothers with leaking milk from accessory nipples have found that a breast pad or sometimes just a bandaid can be effective for catching leaks. As with any leaking, applying pressure straight in toward the chest may help stop the leaking.
Uncommon problems: Since this is breast tissue, it has the potential for the same problems as any other breast tissue, including inflammation, mastitis, abscesses, cysts, benign lumps, or malignant changes. The accessory nipple or breast tissue can be surgically removed, but this is not necessary unless it is causing problems. Some people do have accessory breast tissue or nipples removed for cosmetic reasons.
Excuse Me, But Is That A Third Boob In My Armpit?
Supernumerary Nipple by Aryeh Metzker, MD, from Medscape
Lawrence RA, Lawrence RM. Breastfeeding, A Guide for the Medical Profession (7th ed.). Elsevier Health Sciences; 2011; 44-46.
Mohrbacher N. Breastfeeding answers made simple: a guide for helping mothers. Hale Publishing, LP; 2010; 703.
Hale Publishing, LP; 2010; 703.
Riordan J, Wambach K. Breastfeeding and Human Lactation (4th ed.). Jones and Bartlett Publishers; 2010; 84-85.
Velanovich V. Ectopic breast tissue, supernumerary breasts, and supernumerary nipples. South Med J. 1995;88(9):903-6.
Wilson-Clay B, Hoover K. The Breastfeeding Atlas (5th ed.). Lactnews Press; 2013; 66-67, 184.
Human Milk Composition: Nutrients and Bioactive Factors
1. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–841. [PubMed] [Google Scholar]
2. WHO . Infant and young child nutrition. Geneva: 2003. [Google Scholar]
3. Oftedal OT. The evolution of milk secretion and its ancient origins. Animal : an international journal of animal bioscience. 2012;6(3):355–368. [PubMed] [Google Scholar]
4. Castellote C, Casillas R, Ramirez-Santana C, Perez-Cano FJ, Castell M, Moretones MG, Lopez-Sabater MC, Franch A. Premature delivery influences the immunological composition of colostrum and transitional and mature human milk. The Journal of nutrition. 2011;141(6):1181–1187. [PubMed] [Google Scholar]
The Journal of nutrition. 2011;141(6):1181–1187. [PubMed] [Google Scholar]
5. Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. Journal of mammary gland biology and neoplasia. 2007;12(4):211–221. [PubMed] [Google Scholar]
6. Kulski JK, Hartmann PE. Changes in human milk composition during the initiation of lactation. Aust J Exp Biol Med Sci. 1981;59(1):101–114. [PubMed] [Google Scholar]
7. Henderson JJ, Hartmann PE, Newnham JP, Simmer K. Effect of preterm birth and antenatal corticosteroid treatment on lactogenesis II in women. Pediatrics. 2008;121(1):e92–100. [PubMed] [Google Scholar]
8. Nommsen-Rivers LA, Dolan LM, Huang B. Timing of stage II lactogenesis is predicted by antenatal metabolic health in a cohort of primiparas. Breastfeed Med. 2012;7(1):43–49. [PMC free article] [PubMed] [Google Scholar]
9. Cregan MD, De Mello TR, Kershaw D, McDougall K, Hartmann PE. Initiation of lactation in women after preterm delivery. Acta obstetricia et gynecologica Scandinavica. 2002;81(9):870–877. [PubMed] [Google Scholar]
Acta obstetricia et gynecologica Scandinavica. 2002;81(9):870–877. [PubMed] [Google Scholar]
10. Nommsen LA, Lovelady CA, Heinig MJ, Lonnerdal B, Dewey KG. Determinants of energy, protein, lipid, and lactose concentrations in human milk during the first 12 mo of lactation: the DARLING Study. The American journal of clinical nutrition. 1991;53(2):457–465. [PubMed] [Google Scholar]
11. Bauer J, Gerss J. Longitudinal analysis of macronutrients and minerals in human milk produced by mothers of preterm infants. Clinical nutrition (Edinburgh, Scotland) 2011;30(2):215–220. [PubMed] [Google Scholar]
12. Geraghty SR, Davidson BS, Warner BB, Sapsford AL, Ballard JL, List BA, Akers R, Morrow AL. The development of a research human milk bank. J Hum Lact. 2005;21(1):59–66. [PubMed] [Google Scholar]
13. Prentice A. Regional Variations in the Composition of Human Milk. In: Jensen RG, editor. Handbook of Milk Composition. Academic Press, Inc.; San Diego, CA: 1995. p. 919. [Google Scholar]
14. Liao Y, Alvarado R, Phinney B, Lonnerdal B. Proteomic characterization of human milk whey proteins during a twelve-month lactation period. J Proteome Res. 2011;10(4):1746–1754. [PubMed] [Google Scholar]
Liao Y, Alvarado R, Phinney B, Lonnerdal B. Proteomic characterization of human milk whey proteins during a twelve-month lactation period. J Proteome Res. 2011;10(4):1746–1754. [PubMed] [Google Scholar]
15. Gao X, McMahon RJ, Woo JG, Davidson BS, Morrow AL, Zhang Q. Temporal changes in milk proteomes reveal developing milk functions. J Proteome Res. 2012;11(7):3897–3907. [PubMed] [Google Scholar]
16. Lonnerdal B. Human milk proteins: key components for the biological activity of human milk. Advances in experimental medicine and biology. 2004;554:11–25. [PubMed] [Google Scholar]
17. Jensen RG. Handbook of Milk Composition. Academic Press, Inc.; San Diego, CA: 1995. [Google Scholar]
18. Valentine CJ, Morrow G, Fernandez S, Gulati P, Bartholomew D, Long D, Welty SE, Morrow AL, Rogers LK. Docosahexaenoic Acid and Amino Acid Contents in Pasteurized Donor Milk are Low for Preterm Infants. The Journal of pediatrics. 2010;157(6):906–910. [PubMed] [Google Scholar]
19. Saarela T, Kokkonen J, Koivisto M. Macronutrient and energy contents of human milk fractions during the first six months of lactation. Acta Paediatr. 2005;94(9):1176–1181. [PubMed] [Google Scholar]
Saarela T, Kokkonen J, Koivisto M. Macronutrient and energy contents of human milk fractions during the first six months of lactation. Acta Paediatr. 2005;94(9):1176–1181. [PubMed] [Google Scholar]
20. Kent JC, Mitoulas LR, Cregan MD, Ramsay DT, Doherty DA, Hartmann PE. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3):e387–395. [PubMed] [Google Scholar]
21. Valentine CJ, Morrow G, Pennell M, Morrow AL, Hodge A, Haban-Bartz A, Collins K, Rogers LK. Randomized Controlled Trial of Docosahexaenoic Acid Supplementation in Midwestern U.S. Human Milk Donors. Breastfeed Med. 2012 EPub doi:10.1089/bfm.2011.0126. [PMC free article] [PubMed] [Google Scholar]
22. Martin MA, Lassek WD, Gaulin SJ, Evans RW, Woo JG, Geraghty SR, Davidson BS, Morrow AL, Kaplan HS, Gurven MD. Fatty acid composition in the mature milk of Bolivian forager-horticulturalists: controlled comparisons with a US sample. Matern Child Nutr. 2012;8(3):404–418. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
23. Newburg DS, Ruiz-Palacios GM, Morrow AL. Human milk glycans protect infants against enteric pathogens. Annual review of nutrition. 2005;25:37–58. [PubMed] [Google Scholar]
24. Morrow AL, Ruiz-Palacios GM, Jiang X, Newburg DS. Human-milk glycans that inhibit pathogen binding protect breast-feeding infants against infectious diarrhea. The Journal of nutrition. 2005;135(5):1304–1307. [PubMed] [Google Scholar]
25. Gabrielli O, Zampini L, Galeazzi T, Padella L, Santoro L, Peila C, Giuliani F, Bertino E, Fabris C, Coppa GV. Preterm milk oligosaccharides during the first month of lactation. Pediatrics. 2011;128(6):e1520–1531. [PubMed] [Google Scholar]
26. Michaelsen KF, Skafte L, Badsberg JH, Jorgensen M. Variation in macronutrients in human bank milk: influencing factors and implications for human milk banking. Journal of pediatric gastroenterology and nutrition. 1990;11(2):229–239. [PubMed] [Google Scholar]
27. Arslanoglu S, Moro GE, Ziegler EE, The Wapm Working Group On Nutrition Optimization of human milk fortification for preterm infants: new concepts and recommendations. Journal of perinatal medicine. 2010;38(3):233–238. [PubMed] [Google Scholar]
Journal of perinatal medicine. 2010;38(3):233–238. [PubMed] [Google Scholar]
28. Greer FR. Do breastfed infants need supplemental vitamins? Pediatric clinics of North America. 2001;48(2):415–423. [PubMed] [Google Scholar]
29. Allen LH. B vitamins in breast milk: relative importance of maternal status and intake, and effects on infant status and function. Adv Nutr. 2012;3(3):362–369. [PMC free article] [PubMed] [Google Scholar]
30. Dawodu A, Zalla L, Woo JG, Herbers PM, Davidson BS, Heubi JE, Morrow AL. Heightened attention to supplementation is needed to improve the vitamin D status of breastfeeding mothers and infants when sunshine exposure is restricted. Matern Child Nutr. 2012 [PMC free article] [PubMed] [Google Scholar]
31. Pediatrics AAo. Pediatric Nutrition Handbook. 6th ed American Academy of Pediatrics; Elk Gove Village, IL: 2009. [Google Scholar]
32. Schrezenmeir J, Korhonen H, Williams C, Gill HS, Shah N. Foreword. The British journal of nutrition. 2000;84(S1):1. [Google Scholar]
2000;84(S1):1. [Google Scholar]
33. Garofalo R. Cytokines in human milk. The Journal of pediatrics. 2010;156(2 Suppl):S36–40. [PubMed] [Google Scholar]
34. Cavaletto M, Giuffrida MG, Conti A. The proteomic approach to analysis of human milk fat globule membrane. Clinica chimica acta; international journal of clinical chemistry. 2004;347(1-2):41–48. [PubMed] [Google Scholar]
35. Van de Perre P. Transfer of antibody via mother’s milk. Vaccine. 2003;21(24):3374–3376. [PubMed] [Google Scholar]
36. Kobata R, Tsukahara H, Ohshima Y, Ohta N, Tokuriki S, Tamura S, Mayumi M. High levels of growth factors in human breast milk. Early human development. 2008;84(1):67–69. [PubMed] [Google Scholar]
37. Patki S, Patki U, Patil R, Indumathi S, Kaingade P, Bulbule A, Nikam A, Pishte A. Comparison of the levels of the growth factors in umbilical cord serum and human milk and its clinical significance. Cytokine. 2012;59(2):305–308. [PubMed] [Google Scholar]
38. Hirai C, Ichiba H, Saito M, Shintaku H, Yamano T, Kusuda S. Trophic effect of multiple growth factors in amniotic fluid or human milk on cultured human fetal small intestinal cells. JPGN. 2002;34:524–528. [PubMed] [Google Scholar]
Trophic effect of multiple growth factors in amniotic fluid or human milk on cultured human fetal small intestinal cells. JPGN. 2002;34:524–528. [PubMed] [Google Scholar]
39. Chailler P, Menard D. Ontogeny of EGF receptors in the human gut. Frontiers in Biosci. 1999;4:87–101. [PubMed] [Google Scholar]
40. Wagner CL, Taylor SN, Johnson D. Host factors in amniotic fluid and breast milk that contribute to gut maturation. Clinic. Rev. Allerg. Immunol. 2008;34:191–204. [PubMed] [Google Scholar]
41. Read LC, Upton FM, Francis GL, Wallace JC, Dahlenberg GW, Ballad FJ. Changes in the growth-promoting activity of human milk during lactation. Pediatr. Res. 1984;18(2):133–139. [PubMed] [Google Scholar]
42. Chang C-Y, Chao JC-J. Effect of human milk and epidermal growth factor on growth of human intestinal caco-2 cells. JPGN. 2002;34:394–401. [PubMed] [Google Scholar]
43. Khailova L, Dvorak K, Arganbright KM, Williams CS, Halpern MD, Dvorak B. Changes in hepatic cell junctions structure during experimental necrotizing enterocolitis: effect of EGF treatment. Pediatr. Res. 2009;66(2):140–144. [PMC free article] [PubMed] [Google Scholar]
Pediatr. Res. 2009;66(2):140–144. [PMC free article] [PubMed] [Google Scholar]
44. Radulescu A, Zhang H-Y, Chen C-L, Chen Y, Zhou Y, Yu X, Otabor I, Olson JK, Besner GE. Heparin-Binding EGF-Like Growth Factor promotes intestinal anastomotic healing. J. Surg. Res. 2011;171:540–550. [PMC free article] [PubMed] [Google Scholar]
45. Dvorak B, Fituch CC, Williams CS, Hurst NM, Schanler RJ. Increased epidermal growth factor levels in human milk of mothers with extremely premature infants. Pediatr. Res. 2003;54(1):15–19. [PubMed] [Google Scholar]
46. Dvorak B, Fituch CC, Williams CS, Hurst NM, Schanler RJ. Concentrations of epidermal growth factor and Transforming Growth Factor-Alpha in preterm milk. In: al. Pe., editor. Protecting Infants Through Human Milk. Kluwer Academic/Plenum Publishers; 2004. pp. 407–409. [PubMed] [Google Scholar]
47. Rodrigues D, Li A, Nair D, Blennerhassett M. Glial cell line-derived neurotrophic factor is a key neurotrophin in the postnatal enteric nervous system. Neurogastroenterol. Motil. 2011;23:e44–e56. [PubMed] [Google Scholar]
Neurogastroenterol. Motil. 2011;23:e44–e56. [PubMed] [Google Scholar]
48. Boesmans W, Gomes P, Janssens J, Tack J, Berghe PV. Brain-derived neurotrophic factor amplifies neurotransmitter responses and promotes synaptic communication in the enteric nervous system. Gut. 2008;57:314–322. [PubMed] [Google Scholar]
49. Sánchez M, Silos-Santiago I, Frisén J, He B, Lira S, Barbacid M. Renal agenesis and the absence of enteric neurons in mice lacking GDNF. Nature. 1996;382(6586):70–73. [PubMed] [Google Scholar]
50. Li R, Xia W, Zhang Z, Wu K. S100B protein, brain-derived neurotrophic factor, and glial cell line-derived neurotrophic factor in human milk. PloS ONE. 2011;6(6) [PMC free article] [PubMed] [Google Scholar]
51. Fichter M, Klotz M, Hirschberg DL, Waldura B, Schofer O, Ehnert S, Schwarz LK, Ginneken CV, Schafer K-H. Breast milk contains relevant neurotrophic factors and cytokines for enteric nervous system development. Mol. Nutr. Food Res. 2011;55:1592–1596. [PubMed] [Google Scholar]
52. Blum JW, Baumrucker CR. Colostral and milk insulin-like growth factors and related substances: mammary gland and neonatal (intestinal and systemic) targets. Dom. Anim. Endocrin. 2002;23:101–110. [PubMed] [Google Scholar]
Blum JW, Baumrucker CR. Colostral and milk insulin-like growth factors and related substances: mammary gland and neonatal (intestinal and systemic) targets. Dom. Anim. Endocrin. 2002;23:101–110. [PubMed] [Google Scholar]
53. Burrin DG. Is milk-borne insulin-like growth factor-I essential for neonatal development? J. Nutr. 1997;127:975S–979S. [PubMed] [Google Scholar]
54. Philipps AF, Kling PJ, Grille JG, Dvorak B. Intestinal transport of insulin-like growth factor-I (IGF-I) in the suckling rat. JPGN. 2002;35:539–544. [PubMed] [Google Scholar]
55. Milsom SR, Blum WF, Gunn AJ. Temporal changes in insulin-like growth factors I and II and in insulin-like growth factor binding proteins 1, 2, and 3 in human milk. Horm. Res. 2008;69:307–311. [PubMed] [Google Scholar]
56. Prosser CG. Insulin-like growth factors in milk and mammary gland. J. Mammary Gland Biol. & Neoplas. 1996;1(3):297–306. [PubMed] [Google Scholar]
57. Elmlinger MW, Hochhaus F, Loui A, Frommer KW, Obladen M, Ranke MB. Insulin-like growth factors and binding proteins in early milk from mothers of preterm and term infants. Horm. Res. 2007;68:124–131. [PubMed] [Google Scholar]
Insulin-like growth factors and binding proteins in early milk from mothers of preterm and term infants. Horm. Res. 2007;68:124–131. [PubMed] [Google Scholar]
58. Peterson CA, Gillingham MB, Mohapatra NK, Dahly EM, Adamo ML, Carey HV, Lund PK, Ney DM. Enterotrophic effect of insulin-like growth factor-I but not growth hormone and localized expression of insulin-like growth factor-I, insulin-like growth factor binding protein-3 and -5 mRNAs in jejunum of parenterally fed rats. JPEN. 2000;24(5):288–295. [PubMed] [Google Scholar]
59. Murali SG, Nelson DW, Draxler AK, Liu X, Ney DM. Insulin-like growth factor-I (IGF-I) attenuates jejunal atrophy in association with increased expression of IGF-I binding protein-5 in parenterally fed mice. J. Nutr. 2005;135(11):2553–2559. [PubMed] [Google Scholar]
60. Corpeleijn WE, Vliet Iv, Dana-Anne H, de Gast-Bakker, Schoor SRDvd, Alles MS, Hoijer M, Tibboel D, Goudoever JBv. Effect of enteral IGF-1 supplementation on feeding tolerance, growth, and gut permeability in enterally fed premature neonates. JPGN. 2008;46:184–190. [PubMed] [Google Scholar]
JPGN. 2008;46:184–190. [PubMed] [Google Scholar]
61. Büyükkayhan D, Tanzer F, Erselcan T, Cinar Z, Yönem O. Umbilical serum insulin-like growth factor 1 (IGF-1) in newborns: effects of gestational age, postnatal age, and nutrition. Int J Vitam Nutr Res. 2003;73(5):343–346. [PubMed] [Google Scholar]
62. Philipps AF, Dvorak B, Kling PJ, Grille JG, Koldovsky O. Absorption of milk-borne insulin-like growth factor-I into portal blood of sucklin rats. JPGN. 2000;31:128–135. [PubMed] [Google Scholar]
63. Kling PJ, Taing KM, Dvorak B, Woodward SS, Philipps AF. Insulin-like growth factor-I stimulates erythropoiesis when administered enterally. Growth Factors. 2006;24(3):218–223. [PubMed] [Google Scholar]
64. Loui A, Eilers E, Strauss E, Pohl-Schickinger A, Obladen M, Koehne P. Vascular endothelial growth factor (VEGF) and soluble VEGF Receptor 1 (Sflt-1) levels in early and mature human milk from mothers of preterm versus term infants. J Hum. Lact. 2012 [PubMed] [Google Scholar]
65. Reynolds JD. The management of Retinopathy of Prematurity. Paediatr Drugs. 2001;3(4):263–272. [PubMed] [Google Scholar]
Reynolds JD. The management of Retinopathy of Prematurity. Paediatr Drugs. 2001;3(4):263–272. [PubMed] [Google Scholar]
66. DiBiasie A. Evidence-based review of Retinopathy of Prematurity prevention in VLBW and ELBW Infants. Neonat. Network. 2006;25(6):393–403. [PubMed] [Google Scholar]
67. Kett JC. Anemia in infancy. Pediatr. Rev. 2012;33(4):186–187. [PubMed] [Google Scholar]
68. Soubasi V, Kremenopoulos G, Diamanti E, Tsantali C, Sarafidis K, Tsakiris D. Follow-up of very low birth weight infants after erythropoietin treatment to prevent anemia of prematurity. J. Pediatr. 1995;127:291–297. [PubMed] [Google Scholar]
69. Carbonell-Estrany X, Figueras-Aloy J, Alvarez E. Erythropoietin and prematurity – where do we stand? J. Perinat. Med. 2005;33:277–286. [PubMed] [Google Scholar]
70. Kling PJ, Willeitner A, Dvorak B, Blohowiak SE. Enteral erythropoietin and iron stimulate erythropoiesis in suckling rats. JPGN. 2008;46:202–207. [PubMed] [Google Scholar]
71. Pasha YZ, Ahmadpour-Kacho M, Hajiahmadi M, Hosseini M. Enteral erythropoietin increases plasma erythropoietin level in preterm infants: a randomized controlled trial. Indian Pediatr. 2008;45:25–28. [PubMed] [Google Scholar]
Pasha YZ, Ahmadpour-Kacho M, Hajiahmadi M, Hosseini M. Enteral erythropoietin increases plasma erythropoietin level in preterm infants: a randomized controlled trial. Indian Pediatr. 2008;45:25–28. [PubMed] [Google Scholar]
72. Shiou S-R, Yu Y, Chen S, Ciancio MJ, Petrof EO, Sun J, Claud EC. Erythropoietin protects intestinal epithelial barrier function and lowers the incidence of experimental neonatal necrotizing enterocolitis. J. Biol. Chem. 2011;286(14):12123–12132. [PMC free article] [PubMed] [Google Scholar]
73. Arsenault JE, Webb AL, Koulinska IN, Aboud S, Fawzi WW, Villamor E. Association between breast milk erythropoietin and reduced risk of mother-to-child transmission of HIV. JID. 2010;202(3):370–373. [PMC free article] [PubMed] [Google Scholar]
74. Claud EC, Savidge T, Walker WA. Modulation of human intestinal epithelial cell IL-8 secretion by human milk factors. Pediatr. Res. 2003;53:419–425. [PubMed] [Google Scholar]
75. Struck J, Almeida Pd, Bergmann A, Morgenthaler NG. High Concentrations of Procalcitonin but Not Mature Calcitonin in Normal Human Milk. Horm. Metab. Res. 2002;34:460–465. [PubMed] [Google Scholar]
High Concentrations of Procalcitonin but Not Mature Calcitonin in Normal Human Milk. Horm. Metab. Res. 2002;34:460–465. [PubMed] [Google Scholar]
76. Wookey PJ, Turner K, Furness JB. Transient expression of the calcitonin receptor by enteric neurons of the embryonic and early post-natal mouse. Cell Tissue Res. 2012;347:311–317. [PubMed] [Google Scholar]
77. Rao RK, Davis TP, Williams C, Koldovsky O. Effect of milk on somatostatin degradation in suckling rat jejunum in vivo. JPGN. 1999;28(1):84–94. [PubMed] [Google Scholar]
78. Gama P, Alvares EP. LHRH and somatostatin effects on the cell proliferation of the gastric epithelium of suckling and weaning rats. Reg. Peptides. 1996;63:73–78. [PubMed] [Google Scholar]
79. Newburg DS, Woo JG, Morrow AL. Characteristics and potential functions of human milk adiponectin. J. Pediatr. 2010;156:S41–S46. [PMC free article] [PubMed] [Google Scholar]
80. Martin LJ, Woo JG, Geraghty SR, Altaye M, Davidson BS, Banach W, Dolan LM, Ruiz-Palacios GM, Morrow AL. Adiponectin is present in human milk and is associated with maternal factors. Am. J. Clin. Nutr. 2006;83:1106–1111. [PubMed] [Google Scholar]
Adiponectin is present in human milk and is associated with maternal factors. Am. J. Clin. Nutr. 2006;83:1106–1111. [PubMed] [Google Scholar]
81. Woo JG, Guerrero ML, Guo F, Martin LJ, Davidson BS, Ortega H, Ruiz-Palacios GM, Morrow AL. Human milk adiponectin affects infant weight trajectory during the second year of life. Journal of pediatric gastroenterology and nutrition. 2012;54(4):532–539. [PMC free article] [PubMed] [Google Scholar]
82. Savino F, Sorrenti M, Benetti S, Lupica MM, Liguori SA, Oggero R. Resistin and leptin in breast milk and infants in early life. Early Hum. Devel. 2012;88:779–782. [PubMed] [Google Scholar]
83. Savino F, Liguori SA. Update on breast milk hormones: Leptin, ghrelin and adiponectin. Clin. Nutr. 2008;27:42–47. [PubMed] [Google Scholar]
84. Palou A, Sánchez J, Picó C. Nutrient–gene interactions in early life programming: leptin in breast milk prevents obesity later on in life. In: Koletzko B, editor. Early Nutrition Programming and Health: Outcomes in Later Life: Obesity and Beyond. Springer Science + Business Media B.V.; 2009. pp. 95–104. [PubMed] [Google Scholar]
Springer Science + Business Media B.V.; 2009. pp. 95–104. [PubMed] [Google Scholar]
85. Dündar NO, Dündar B, Cesur G, Yılmaz N, Sütçu R, özgüner F. Ghrelin and adiponectin levels in colostrum, cord blood and maternal serum. Pediatr. Int. 2010;52:622–625. [PubMed] [Google Scholar]
86. Goldman AS. Modulation of the Gastrointestinal Tract of Infants by Human Milk. Interfaces and Interactions. An Evolutionary Perspective1. J. Nutr. 2000;130:426S–431S. [PubMed] [Google Scholar]
87. Jarvinen KM, Suomalainen H. Leucocytes in human milk and lymphocyte subsets in cow’s milk-allergic infants. Pediatr Allergy Immunol. 2002;13(4):243–254. [PubMed] [Google Scholar]
88. Patki S, Kadam S, Chandra V, Bhonde R. Human breast milk is a rich source of multipotent mesenchymal stem cells. Human cell. 2010;23(2):35–40. [PubMed] [Google Scholar]
89. Ichikawa M, Sugita M, Takahashi M, Satomi M, Takeshita T, Araki T, Takahashi H. Breast milk macrophages spontaneously produce granulocyte-macrophage colony-stimulating factor and differentiate into dendritic cells in the presence of exogenous interleukin-4 alone. Immunology. 2003;108(2):189–195. [PMC free article] [PubMed] [Google Scholar]
Immunology. 2003;108(2):189–195. [PMC free article] [PubMed] [Google Scholar]
90. Indumathi S, Dhanasekaran M, Rajkumar JS, Sudarsanam D. Exploring the stem cell and non-stem cell constituents of human breast milk. Cytotechnology. 2012 [PMC free article] [PubMed] [Google Scholar]
91. Riskin A, Almog M, Peri R, Halasz K, Srugo I, Kessel A. Changes in immunomodulatory constituents of human milk in response to active infection in the nursing infant. Pediatric research. 2012;71(2):220–225. [PubMed] [Google Scholar]
92. Sabbaj S, Ibegbu CC, Kourtis AP. Cellular immunity in breast milk: implications for postnatal transmission of HIV-1 to the infant. Advances in experimental medicine and biology. 2012;743:161–169. [PubMed] [Google Scholar]
93. Yagi Y, Watanabe E, Watari E, Shinya E, Satomi M, Takeshita T, Takahashi H. Inhibition of DC-SIGN-mediated transmission of human immunodeficiency virus type 1 by Toll-like receptor 3 signalling in breast milk macrophages. Immunology. 2010;130(4):597–607. [PMC free article] [PubMed] [Google Scholar]
2010;130(4):597–607. [PMC free article] [PubMed] [Google Scholar]
94. Agarwal S, Karmaus W, Davis S, Gangur V. Immune markers in breast milk and fetal and maternal body fluids: a systematic review of perinatal concentrations. J Hum Lact. 2011;27(2):171–186. [PubMed] [Google Scholar]
95. Groer MW, Beckstead JW. Multidimensional scaling of multiplex data: human milk cytokines. Biological research for nursing. 2011;13(3):289–296. [PubMed] [Google Scholar]
96. Kverka M, Burianova J, Lodinova-Zadnikova R, Kocourkova I, Cinova J, Tuckova L, Tlaskalova-Hogenova H. Cytokine profiling in human colostrum and milk by protein array. Clinical chemistry. 2007;53(5):955–962. [PubMed] [Google Scholar]
97. Penttila IA. Milk-derived transforming growth factor-b and the infant immune response. J. Pediatr. 2010;156:S21–S25. [PubMed] [Google Scholar]
98. Kalliomäki M, Ouwehand A, Arvilommi H, Kero P, Isolauri E. Transforming growth factor-β in breast milk: A potential regulator of atopic disease at an early age. J. Allergy Clin. Immunol. 1999:1251–1257. [PubMed] [Google Scholar]
J. Allergy Clin. Immunol. 1999:1251–1257. [PubMed] [Google Scholar]
99. Saito S, Yoshida M, Ichijo M, Ishizaka S, Tsujii T. Transforming growth factor-beta (TGF-f) in human milk. Clin. Exp. Immunol. 1993;94:220–224. [PMC free article] [PubMed] [Google Scholar]
100. Nakamura Y, Miyata M, Ando T, Shimokawa N, Ohnuma Y, Katoh R, Ogawa H, Okumura K, Nakao A. The latent form of transforming growth factor-b administered orally is activated by gastric acid in mice. J. Nutr. 2009;139:1463–1468. [PubMed] [Google Scholar]
101. Letterio JJ, Geiser AG, Kulkarni Ashok B., Roche NS, Sporn MB, Roberts AB. Maternal rescue of transforming growth factor-b1 null mice. Science. 1994;264:1936–1938. [PubMed] [Google Scholar]
102. Ando T, Hatsushika K, Wako M, Ohba T, Koyama K, Ohnuma Y, Katoh R, Ogawa H, Okumura K, Luo J, Wyss-Coray T, Nakao A. Orally administered TGF-b is biologically active in the intestinal mucosa and enhances oral tolerance. J. Allergy Clin. Immunol. 2007;120:916–923. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
103. Ozawa T, Miyata M, Nishimura M, Ando T, Ouyang Y, Ohba T, Shimokawa N, Ohnuma Y, Katoh R, Ogawa H, Nakao A. Transforming growth factor-b activity in commercially available pasteurized cow milk provides protection against inflammation in mice. J. Nutr. 2009;139:69–75. [PubMed] [Google Scholar]
104. Donnet-Hughes A, Duc N, Serrant P, Vidal K, Schiffrin EJ. Bioactive molecules in milk and their role in health and disease: The role of transforming growth factor-b. Immunol. Cell Biol. 2000;78:74–79. [PubMed] [Google Scholar]
105. Gilmore W, McKelvey-Martin V, Rutherford S, Strain J, Loane P, Kell M, Millar S. Human milk contains granulocyte colony stimulating factor. Eur J Clin Nutr. 1994;48(3):222–224. [PubMed] [Google Scholar]
106. Gersting JA, Kotto-Komeb CA, Dua Y, Christensen RD, Calhoun DA. Bioavailability of granulocyte colony-stimulating factor administered enterally to suckling mice. Pharmacol. Res. 2003;48:643–647. [PubMed] [Google Scholar]
107. Calhoun DA, Maheshwari A, Christensen RD. Recombinant Granulocyte Colony-Stimulating Factor administered enterally to neonates is not absorbed. Pediatrics. 2003;112(2):421–423. [PubMed] [Google Scholar]
Calhoun DA, Maheshwari A, Christensen RD. Recombinant Granulocyte Colony-Stimulating Factor administered enterally to neonates is not absorbed. Pediatrics. 2003;112(2):421–423. [PubMed] [Google Scholar]
108. Gersting JA, Christensen RD, Calhoun DA. Effects of enterally administering granulocyte colony-stimulating factor to suckling mice. Pediatr Res. 2004;55(5):802–806. [PubMed] [Google Scholar]
109. Ngom P, Collinson A, Pido-Lopez J, Henson S, Prentice A, Aspinall R. Improved thymic function in exclusively breastfed infants is associated with higher interleukin 7 concentrations in their mothers’ breast milk. Am. J. Clin. Nutr. 2004;80(3):722–728. [PubMed] [Google Scholar]
110. Aspinall R, Prentice AM, Ngom PT. Interleukin 7 from maternal milk crosses the intestinal barrier and modulates T-cell development in offspring. PloS ONE. 2011;6(6) [PMC free article] [PubMed] [Google Scholar]
111. Ustundag B, Yilmaz E, Dogan Y, Akarsu S, Canatan H, Halifeoglu I, Cikim G, Aygun AD. Levels of cytokines (IL-1beta, IL-2, IL-6, IL-8, TNF-alpha) and trace elements (Zn, Cu) in breast milk from mothers of preterm and term infants. Mediators of inflammation. 2005;2005(6):331–336. [PMC free article] [PubMed] [Google Scholar]
Levels of cytokines (IL-1beta, IL-2, IL-6, IL-8, TNF-alpha) and trace elements (Zn, Cu) in breast milk from mothers of preterm and term infants. Mediators of inflammation. 2005;2005(6):331–336. [PMC free article] [PubMed] [Google Scholar]
112. Buescher ES, McWilliams-Koeppen P. Soluble Tumor Necrosis Factor-α (TNF-α) Receptors in human colostrum and milk bind to TNF-α and neutralize TNF-α bioactivity. Pediatr Res. 1998;44:37–42. [PubMed] [Google Scholar]
113. Buescher E, Malinowska I. Soluble receptors and cytokine antagonists in human milk. Pediatr Res. 1996;40(6):839–844. [PubMed] [Google Scholar]
114. Erbağci A, Cekmen M, Balat O, Balat A, Aksoy F, M. MT. Persistency of high proinflammatory cytokine levels from colostrum to mature milk in preeclampsia. Clin. Biochem. 2005;38(8):712–716. [PubMed] [Google Scholar]
115. Meki A-RMA, Saleem TH, Al-Ghazali MH, Sayed AA. Interleukins -6, -8 and -10 and tumor necrosis factor alpha and its soluble receptor I in human milk at different periods of lactation. Nutr. Res. 2003;23:845–855. [Google Scholar]
Nutr. Res. 2003;23:845–855. [Google Scholar]
116. Maheshwari A, Lu W, Lacson A, Barleycorn AA, Nolan S, Christensen RD, Calhoun DA. Effects of Interleukin-8 on the developing human intestine. Cytokine. 2002;20(6):256–267. [PubMed] [Google Scholar]
117. Maheshwari A, Lacson A, Lu W, Fox SE, Barleycorn AA, Christensen RD, Calhoun DA. Interleukin-8/CXCL8 forms an autocrine loop in fetal intestinal mucosa. Pediatr Res. 2004;56(2):240–249. [PubMed] [Google Scholar]
118. Maheshwari A, Christensen RD, Calhoun DA. ELR+ CXC chemokines in human milk. Cytokine. 2003;24:91–102. [PubMed] [Google Scholar]
119. Mizuno K, Hatsuno M, Aikawa K, Takeichi H, Himi T, Kaneko A, Kodaira K, Takahashi H, Itabashi K. Mastitis is associated with IL-6 Levels and milk fat globule size in breast milk. J. Hum. Lact. 2012 [PubMed] [Google Scholar]
120. Hunt KM, Williams JE, Shafii B, Hunt MK, Behre R, Ting R, McGuire MK, McGuire MA. Mastitis Is Associated with Increased Free Fatty Acids, Somatic Cell Count, and Interleukin-8 Concentrations in Human Milk. Breastfeeding Med. 2012 [PMC free article] [PubMed] [Google Scholar]
Breastfeeding Med. 2012 [PMC free article] [PubMed] [Google Scholar]
121. Hrdý J, Novotná O, Kocourková I, Prokeśová L. Cytokine expression in the colostral cells of healthy and allergic mothers. Folia Microbiologica. 2012;57(3):215–219. [PubMed] [Google Scholar]
122. Strand TA, Sharma PR, Gjessing HK, Ulak M, Chandyo RK, Adhikari RK, Sommerfelt H. Risk factors for extended duration of acute diarrhea in young children. PloS ONE. 2012;7(5) [PMC free article] [PubMed] [Google Scholar]
123. Lamberti LM, Walker CLF, Noiman A, Victora C, Black RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Pub. Health. 2011;11(Supp. 3) [PMC free article] [PubMed] [Google Scholar]
124. Brandtzaeg P. The mucosal immune system and its integration with the mammary glands. The Journal of pediatrics. 2010;156(2 Suppl):S8–15. [PubMed] [Google Scholar]
125. Kadaoui KA, Corthésy B. Secretory IgA mediates bacterial translocation to dendritic cells in mouse peyer’s patches with restriction to mucosal compartment. J. Immunol. 2007;179:7751–7757. [PubMed] [Google Scholar]
J. Immunol. 2007;179:7751–7757. [PubMed] [Google Scholar]
126. Corthesy B. Secretory immunoglobulin A: well beyond immune exclusion at mucosal surfaces. Immunopharmacology and immunotoxicology. 2009;31(2):174–179. [PubMed] [Google Scholar]
127. Hurley WL, Theil PK. Perspectives on immunoglobulins in colostrum and milk. Nutrients. 2011;3(4):442–474. [PMC free article] [PubMed] [Google Scholar]
128. Velona T, Abbiati L, Beretta B, Gaiaschi A, Flauto U, Tagliabue P, Galli CL, Restani P. Protein profiles in breast milk from mothers delivering term and preterm babies. Pediatr Res. 1999;45(5):658–663. [PubMed] [Google Scholar]
129. Adamkin DH. Mother’s milk, feeding strategies, and lactoferrin to prevent necrotizing enterocolitis. JPEN. 2012:36. [PubMed] [Google Scholar]
130. Beljaars L, van der Strate BW, Bakker HI, Reker-Smit C, van Loenen-Weemaes AM, Wiegmans FC, Harmsen MC, Molema G, Meijer DK. Inhibition of cytomegalovirus infection by lactoferrin in vitro and in vivo. Antiviral Res. 2004;63(3):197–208. [PubMed] [Google Scholar]
Antiviral Res. 2004;63(3):197–208. [PubMed] [Google Scholar]
131. Kuipers ME, de Vries HG, Eikelboom MC, Meijer DK, Swart PJ. Synergistic fungistatic effects of lactoferrin in combination with antifungal drugs against clinical Candida isolates. Antimicrobial agents and chemotherapy. 1999;43(11):2635–2641. [PMC free article] [PubMed] [Google Scholar]
132. Leitch EC, Willcox MD. Lactoferrin increases the susceptibility of S. epidermidis biofilms to lysozyme and vancomycin. Current eye research. 1999;19(1):12–19. [PubMed] [Google Scholar]
133. Manzoni P, Rinaldi M, Cattani S, Pugni L, Romeo MG, Messner H, Stolfi I, Decembrino L, Laforgia N, Vagnarelli F, Memo L, Bordignon L, Saia OS, Maule M, Gallo E, Mostert M, Magnani C, Quercia M, Bollani L, Pedicino R, Renzullo L, Betta P, Mosca F, Ferrari F, Magaldi R, Stronati M, Farina D. Bovine lactoferrin supplementation for prevention of late-onset sepsis in very low-birth-weight neonates: a randomized trial. Jama. 2009;302(13):1421–1428. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
134. Sherman MP, Bennett SH, Hwang FF, Yu C. Neonatal small bowel epithelia: enhancing anti-bacterial defense with lactoferrin and Lactobacillus GG. Biometals. 2004;17(3):285–289. [PubMed] [Google Scholar]
135. Stubbs J, Lekutis C, Singer K, Bui A, Yuzuki D, Srinivasan U, Parry G. cDNA cloning of a mouse mammary epithelial cell surface protein reveals the existence of epidermal growth factor-like domains linked to factor VIII-like sequences. PNAS. 1990;87(21):8417–8421. [PMC free article] [PubMed] [Google Scholar]
136. Peterson J, Hamosh M, Scallan C, Ceriani R, Henderson T, Mehta N, Armand M, Hamosh P. Milk fat globule glycoproteins in human milk and in gastric aspirates of mother’s milk-fed preterm infants. Pediatr Res. 1998;44(4):499–506. [PubMed] [Google Scholar]
137. Newburg D, Peterson J, Ruiz-Palacios G, Matson D, Morrow A, Shults J, Guerrero M, Chaturvedi P, Newburg S, Scallan C, MRTaylor, Ceriani R, Pickering L. Role of human-milk lactadherin in protection against symptomatic rotavirus infection. The Lancet. 1998;351(9110):1160–1164. [PubMed] [Google Scholar]
The Lancet. 1998;351(9110):1160–1164. [PubMed] [Google Scholar]
138. Aziz M, Jacob A, Matsuda A, Wang P. Review: milk fat globule-EGF factor 8 expression, function and plausible signal transduction in resolving inflammation. Apoptosis. 2011;16:1077–1086. [PubMed] [Google Scholar]
139. Shi J, Heegaard CW, Rasmussen JT, Gilbert GE. Lactadherin binds selectively to membranes containing phosphatidyl-l-serine and increased curvature. Biochim Biophys Acta. 2004;1667:82–90. [PubMed] [Google Scholar]
140. Kusunoki R, Ishihara S, Aziz M, Oka A, Tada Y, Kinoshita Y. Roles of Milk Fat Globule-Epidermal Growth Factor 8 in intestinal inflammation. Digestion. 2012;85:103–107. [PubMed] [Google Scholar]
141. Chogle A, Bu H-F, Wang X, Brown JB, Chou PM, Tan X-D. Milk Fat Globule–EGF Factor 8 is a critical protein for healing of dextran sodium sulfate–induced acute colitis in mice. Mol. Med. 2011;17(5):502–207. [PMC free article] [PubMed] [Google Scholar]
142. Baghdadi M, Chiba S, Yamashina T, Yoshiyama H, Jinushi M. MFG-E8 regulates the immunogenic potential of dendritic cells primed with necrotic cell-mediated inflammatory signals. PloS ONE. 2012;7(6) [PMC free article] [PubMed] [Google Scholar]
MFG-E8 regulates the immunogenic potential of dendritic cells primed with necrotic cell-mediated inflammatory signals. PloS ONE. 2012;7(6) [PMC free article] [PubMed] [Google Scholar]
143. Landberg E, Huang Y, Stromqvist M, Mechref Y, Hansson L, Lundblad A, Novotny MV, Påhlsson P. Changes in glycosylation of human Bile-Salt-Stimulated Lipase during lactation. Arch. Biochem. Biophys. 2000;377(2):246–254. [PubMed] [Google Scholar]
144. Stax MJ, Naarding MA, Tanck MWT, Lindquist S, Hernell O, Lyle R, Brandtzaeg P, Eggesbø M, Pollakis G, Paxton WA. Binding of human milk to pathogen receptor DC-SIGN varies with bile salt-stimulated lipase (BSSL) gene polymorphism. PloS ONE. 2011;6(2) [PMC free article] [PubMed] [Google Scholar]
145. Naarding MA, Dirac AM, Ludwig IS, Speijer D, Lindquist S, Vestman E-L, Stax MJ, Geijtenbeek TBH, Pollakis G, Hernell O, Paxton WA. Bile Salt-Stimulated Lipase from human milk binds DC-SIGN and inhibits Human Immunodeficiency Virus type 1 transfer to CD4+ T cells Antimicrob. Agents Chemother. 2006;50(10):3367–3374. [PMC free article] [PubMed] [Google Scholar]
Agents Chemother. 2006;50(10):3367–3374. [PMC free article] [PubMed] [Google Scholar]
146. Ruvoen-Clouet N, Mas E, Mariounneau S, Guillon P, Lombardo D, Pendu JL. Bile-salt-stimulated lipase and mucins from milk of ‘secretor’ mothers inhibit the binding of Norwalk virus capsids to their carbohydrate ligands. Biochem J. 2006;393:627–634. [PMC free article] [PubMed] [Google Scholar]
147. Hettinga K, Valenberg Hv, Vries Sd, Boeren S, Hooijdonk Tv, Arendonk Jv, Vervoort J. The host defense proteome of human and bovine milk. PloS ONE. 2011;6(4) [PMC free article] [PubMed] [Google Scholar]
148. Saeland E, Jong MAWPd, Nabatov AA, Kalay H, Geijtenbeek TBH, Kooyk Yv. MUC1 in human milk blocks transmission of human immunodeficiency virus from dendritic cells to T cells. Mol. Immunol. 2009;46:2309–2316. [PubMed] [Google Scholar]
149. Yolken RH, Peterson JA, Vonderfecht SL, Fouts ET, Midthun K, Newburg DS. Human milk mucin inhibits rotavirus replication and prevents experimental gastroenteritis. J. Clin. Invest. 1992;90:1984–1987. [PMC free article] [PubMed] [Google Scholar]
J. Clin. Invest. 1992;90:1984–1987. [PMC free article] [PubMed] [Google Scholar]
150. Parker P, Sando L, Pearson R, Kongsuwan K, Tellam RL, Smith S. Bovine Muc1 inhibits binding of enteric bacteria to Caco-2 cells. Glycoconj. 2010;27:89–97. [PubMed] [Google Scholar]
151. Liu B, Yu Z, Chen C, Kling DE, Newburg DS. Human milk mucin 1 and mucin 4 inhibit Salmonella enterica serovar typhimurium invasion of human intestinal epithelial cells in vitro. J. Nutr. 2012;142:1504–1509. [PMC free article] [PubMed] [Google Scholar]
152. Bode L, Kuhn L, Kim HY, Hsiao L, Nissan C, Sinkala M, Kankasa C, Mwiya M, Thea DM, Aldrovandi GM. Human milk oligosaccharide concentration and risk of postnatal transmission of HIV through breastfeeding. The American journal of clinical nutrition. 2012;96(4):831–839. [PMC free article] [PubMed] [Google Scholar]
153. De Leoz ML, Gaerlan SC, Strum JS, Dimapasoc LM, Mirmiran M, Tancredi DJ, Smilowitz JT, Kalanetra KM, Mills DA, German JB, Lebrilla CB, Underwood MA. Lacto-N-tetraose, fucosylation, and secretor status are highly variable in human milk oligosaccharides from women delivering preterm. J Proteome Res. 2012;11(9):4662–4672. [PMC free article] [PubMed] [Google Scholar]
Lacto-N-tetraose, fucosylation, and secretor status are highly variable in human milk oligosaccharides from women delivering preterm. J Proteome Res. 2012;11(9):4662–4672. [PMC free article] [PubMed] [Google Scholar]
154. Hunt KM, Foster JA, Forney LJ, Schutte UM, Beck DL, Abdo Z, Fox LK, Williams JE, McGuire MK, McGuire MA. Characterization of the diversity and temporal stability of bacterial communities in human milk. PLoS ONE. 2011;6(6):e21313. [PMC free article] [PubMed] [Google Scholar]
155. Cabrera-Rubio R, Collado MC, Laitinen K, Salminen S, Isolauri E, Mira A. The human milk microbiome changes over lactation and is shaped by maternal weight and mode of delivery. The American journal of clinical nutrition. 2012;96(3):544–551. [PubMed] [Google Scholar]
156. Rasmussen KM, Geraghty SR. The quiet revolution: breastfeeding transformed with the use of breast pumps. Am J Public Health. 2011;101(8):1356–1359. [PMC free article] [PubMed] [Google Scholar]
157. Baro C, Giribaldi M, Arslanoglu S, Giuffrida MG, Dellavalle G, Conti A, Tonetto P, Biasini A, Coscia A, Fabris C, Moro GE, Cavallarin L, Bertino E. Effect of two pasteurization methods on the protein content of human milk. Front Biosci (Elite Ed) 2011;3:818–829. [PubMed] [Google Scholar]
Effect of two pasteurization methods on the protein content of human milk. Front Biosci (Elite Ed) 2011;3:818–829. [PubMed] [Google Scholar]
158. Chantry CJ, Wiedeman J, Buehring G, Peerson JM, Hayfron K, K’Aluoch O, Lonnerdal B, Israel-Ballard K, Coutsoudis A, Abrams B. Effect of flash-heat treatment on antimicrobial activity of breastmilk. Breastfeed Med. 2011;6(3):111–116. [PMC free article] [PubMed] [Google Scholar]
159. Israel-Ballard K, Donovan R, Chantry C, Coutsoudis A, Sheppard H, Sibeko L, Abrams B. Flash-heat inactivation of HIV-1 in human milk: a potential method to reduce postnatal transmission in developing countries. J Acquir Immune Defic Syndr. 2007;45(3):318–323. [PubMed] [Google Scholar]
160. Peroni D, Piacentini G, Bodini A, Pigozzi R, Boner A. Transforming growth factor-b1 is elevated in unpasteurized cow’s milk. Pediatr. Allergy Immunol. 2009;20:42–44. [PubMed] [Google Scholar]
161. [August 23, 2012];Agennix. Phase 1/2 Study of Talactoferrin Oral Solution ofr Nosocomial Infection in Preterm Infants. http://clinicaltrials.gov/ct2/show/{"type":"clinical-trial","attrs":{"text":"NCT00854633","term_id":"NCT00854633"}}NCT00854633.
http://clinicaltrials.gov/ct2/show/{"type":"clinical-trial","attrs":{"text":"NCT00854633","term_id":"NCT00854633"}}NCT00854633.
162. Ewaschuk JB, Unger S, O’Connor DL, Stone D, Harvey S, Clandinin MT, Field CJ. Effect of pasteurization on selected immune components of donated human breast milk. J Perinatol. 2011;31(9):593–598. [PubMed] [Google Scholar]
163. Akinbi H, Meinzen-Derr J, Auer C, Ma Y, Pullum D, Kusano R, Reszka KJ, Zimmerly K. Alterations in the host defense properties of human milk following prolonged storage or pasteurization. Journal of pediatric gastroenterology and nutrition. 2010;51(3):347–352. [PubMed] [Google Scholar]
164. Valentine CJ. Optimizing Humn Milk Fortification for the Preterm Infant. PNPG Building Block for Life. 2011;34(4):9–11. [Google Scholar]
165. Steinhoff MC, Omer SB. A review of fetal and infant protection associated with antenatal influenza immunization. American journal of obstetrics and gynecology. 2012;207(3 Suppl):S21–27. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
166. Neville MC, Anderson SM, McManaman JL, Badger TM, Bunik M, Contractor N, Crume T, Dabelea D, Donovan SM, Forman N, Frank DN, Friedman JE, German JB, Goldman A, Hadsell D, Hambidge M, Hinde K, Horseman ND, Hovey RC, Janoff E, Krebs NF, Lebrilla CB, Lemay DG, Maclean PS, Meier P, Morrow AL, Neu J, Nommsen-Rivers LA, Raiten DJ, Rijnkels M, Seewaldt V, Shur BD, Vanhouten J, Williamson P. Lactation and neonatal nutrition: defining and refining the critical questions. Journal of mammary gland biology and neoplasia. 2012;17(2):167–188. [PMC free article] [PubMed] [Google Scholar]
Breastfeeding Products | products for breastfeeding |
There are many baby care products, accessories and clothes on the market. But which ones are really necessary for breastfeeding? More on this in our helpful list.
Share this information
If you are planning to breastfeed, the right kit will make it so much easier. However, it is not so easy to understand which accessories are really needed for this, and which ones can be dispensed with. To help you, we have divided the whole breastfeeding period into several stages, as your needs are likely to change over time. In addition, we asked breastfeeding moms for tips and tricks on the most useful nursing accessories.
However, it is not so easy to understand which accessories are really needed for this, and which ones can be dispensed with. To help you, we have divided the whole breastfeeding period into several stages, as your needs are likely to change over time. In addition, we asked breastfeeding moms for tips and tricks on the most useful nursing accessories.
Breastfeeding supplies for the early days
The first few days after your baby is born can be stressful, so it's best to prepare ahead of time. Here are some things you're sure to need, whether you're staying in the hospital for a few days or heading straight home:
- nursing bras, nursing night bras and nursing tops;
- nursing nightgowns or pajamas;
- breastfeeding pillow;
- disposable or reusable bra pads;
- diapers;
- nipple remedy for dry skin and cracks;
- shapers* for flat or inverted nipples;
- book on breastfeeding;
- contacts of a lactation consultant, supervising doctor or hotline.

If you are having trouble breastfeeding, your lactation consultant or healthcare provider may recommend the following accessories:
- Nursing pads* if your baby cannot latch on or your nipples are sore. Do not use nursing pads for a long time. If you have any problems or pain, contact your lactation consultant or your healthcare provider.
- Breast pump** to relieve symptoms of breast swelling and/or stimulate milk production.
- Some mums like to use the cooling hydrogel pads* which provide relief in the first days after delivery, especially when milk begins to flow.
Nursing Tips
“Pillows help a lot to support your back, legs and arms. I also need bra pads in case of milk leaks, a nursing bra and loose tops for quick access to the breasts (I converted regular quality bras into nursing bras that better support the breasts). And we also used a sling all the time,” advises Zaria, a mother of two from South Africa.
“Hydrogel pads were my number one product. They were given to me in the first days of breastfeeding, so I never had sore or cracked nipples. I highly recommend hydrogel pads and buy them for anyone who plans to breastfeed,” shares her experience Camilla, a mother from Australia.
“You absolutely need someone to bring you something to drink. I kept forgetting to prepare myself a glass of water before feeding!” says Meg, mother of two from France.
Thermos to drink hot while sitting in bed. Delicious food and light snacks. My mother-in-law cooked me amazing beef stew and delicious pancakes (I had to eat well!). A pillow to put the baby on because I didn't have the strength to hold it. A comfortable chair, a nightlight for feeding at night and a pillow to sit on (I had stitches - not a pleasant feeling!) ”advises Felicia, a mother of two from the UK.
“A caring spouse, girlfriend or grandmother to bring tea and anything else you might need while you sit and feed. And also an e-book to read with one hand!” says Julie, a mom from Spain.
And also an e-book to read with one hand!” says Julie, a mom from Spain.
Initial Breastfeeding Supplies
You and your baby will likely get comfortable with breastfeeding in the first couple of weeks. Feeding will occur frequently and take a long time. Here are some tools that will make your life easier and make breastfeeding more comfortable as your milk production begins to stabilize:
- feeding chair;
- breastfeeding mobile application;
- disposable or reusable bra pads;
- breast milk collection pads*;
- Large stock of healthy snacks, drinks and ways to pass the time.
Sooner or later you will get bored with the comfort of home and want to start walking with your baby. For tips on breastfeeding outside the home, see our article on breastfeeding in public.
Tips for breastfeeding moms
“For me, the most useful things were breastfeeding bras, disposable bra pads and large diapers to wipe up leaking milk, cover the baby or cover the chest. With cracked nipples, I saved myself with lanolin cream, and loose tops and cardigans made the feeding process easier, ”says Tatiana, mother of three children from Switzerland.
With cracked nipples, I saved myself with lanolin cream, and loose tops and cardigans made the feeding process easier, ”says Tatiana, mother of three children from Switzerland.
“I find the most useful accessory to be a good quality U-shaped breastfeeding pillow. I also had a rocking chair, in which, at a certain inclination, it was very convenient for me to feed the child. To relax, I always listened to music,” says Violeta, a mother from Romania.
“A sports water bottle that doesn't leak, even when open, so you can put it next to you on a sofa or bed. And also an application to track feedings and remind me which breast I fed last time, ”says Francesca, a mother from the UK.
“Breast milk collection pads that are placed inside a bra to collect leaking milk. I had an overabundance of milk, that was the only way I was saved, ”says Lisa-Maria, a mother of two from Switzerland.
“I really liked the D-ring feeding cover to cover my baby and not distract him when feeding outside the house. The slightly rocking chair turned out to be a great alternative to outrageously expensive rocking chairs. Reusable bra pads, in my opinion, perfectly absorb milk, and diapers, as it turns out, can be used in a thousand ways. I regret that I didn’t buy the Medela Easy Expression bustier, it would have been much easier to pump with it!” says Camilla, a mother from Australia.
The slightly rocking chair turned out to be a great alternative to outrageously expensive rocking chairs. Reusable bra pads, in my opinion, perfectly absorb milk, and diapers, as it turns out, can be used in a thousand ways. I regret that I didn’t buy the Medela Easy Expression bustier, it would have been much easier to pump with it!” says Camilla, a mother from Australia.
Breastfeeding accessories for pumping
During breastfeeding, you may need a breast pump to express your milk. The right type of breast pump depends on the individual case and how much milk you want to get. If you plan to express milk regularly, you may also need:
- steam sterilizer, cold water sterilizer, or microwave sterilization bags;
- breast milk storage bags;
- bustier top for hands-free pumping;
- cool bag.
Advice for breastfeeding moms
“At first, when I thought my breasts were about to explode, I used the Medela Electronic Breast Pump** just to get rid of excess milk without overstimulating my breasts. He made my life a lot easier,” says Tatiana, a mother of three from Switzerland.
He made my life a lot easier,” says Tatiana, a mother of three from Switzerland.
“I used a Medela Freestyle Dual Electronic Breastpump** to increase my milk supply and fixed it with an Easy Expression bustier to keep my hands free. It turned out to be a wonderful decision,” says Amy, a mother from the UK.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. FZ 2010/07352 dated 07/19/2010
** RU No. FZ 2010/06525 dated 03/17/2021
Guidelines for breastfeeding a child.
Home » Information for patients
The benefits of breastfeeding for the baby.
Most parents are well aware of the benefits of breastfeeding for term babies. Just as important, if not more so, is breast milk for premature babies. To date, it is known that the milk of mothers who have given birth prematurely has a special composition and differs from the milk of women who have carried the pregnancy to term, as it contains in large quantities substances called enzymes that contribute to the development of the immature stomach and intestines of the child. In addition, these enzymes break down the nutrients in milk and reduce the chance that a child will develop a food intolerance.
In addition, these enzymes break down the nutrients in milk and reduce the chance that a child will develop a food intolerance.
An important benefit of mother's milk is that it provides protection against infections.
This is important because children have limited ability to fight off bacteria and viruses on their own.
Mother's milk contains many specialized protective factors, including antibodies, that protect babies from infection.
Some substances found in breast milk form a protective layer on the surface of the intestine and prevent bacteria and viruses from entering the bloodstream.
Other compounds kill microorganisms directly or prevent their growth. Some of the nutrients found in milk can perform both of these tasks at the same time.
These substances may continue to protect the baby from infection even when the baby is no longer receiving breast milk.
Breast milk contains anti-inflammatory agents that help protect the baby's delicate intestinal tissues from swelling and irritation. These compounds are believed to prevent the development of serious intestinal pathology in children.
These compounds are believed to prevent the development of serious intestinal pathology in children.
Breast milk is the main source of nutrition for children. The milk of a mother who gave birth prematurely contains much more protein, the need for which in a premature baby is much higher than in a full-term baby. Of particular importance is the type of fat contained in breast milk.
During the first or second day there is very little milk, only a few drops of a yellowish color. This "early" milk is called colostrum. Even a small dose of it contains a large amount of substances that help protect the child from infection. Therefore, for feeding, you should collect any, even
very small quantities of milk. Over the next few days, the milk will gradually start to increase in volume, and its color and consistency will change.
Because even small amounts of mother's milk can have a significant impact on a baby's health, it is important to start breastfeeding as soon as possible after delivery.
Maternal nutrition and well-being
Almost all mothers are concerned about whether they are eating properly in order to provide their baby with good milk. However, it should be emphasized that the milk that is produced in the mother's body will be nutritious, even if her diet is not ideal.
But in the process of milk production in the body, the reserves of some nutrients can be depleted, and in order to fill the needs of the mother's body, it is necessary to continue taking vitamins specially designed for lactating women.
Diet does not affect the quality of milk, but it may cause a decrease in its quantity, especially if the lack of appetite is mainly due to stress and anxiety.
Mom should not forget about her diet by filling out a diary every day, where the volume of milk is noted.
Mothers should consult their doctor before taking any medications or supplements. The neonatologist will recommend drugs that are compatible with breastfeeding and, if necessary, will consult with other specialists on this issue.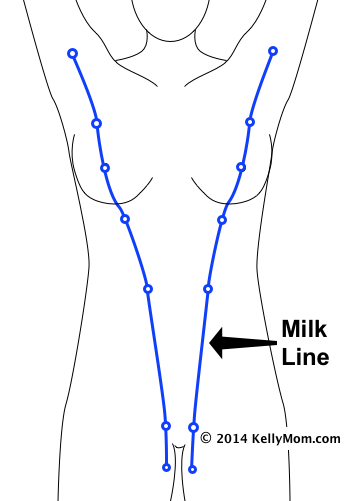
First breastfeeding and breastfeeding
The baby's general health will determine when breastfeeding can begin. There are no specific parameters for the weight or age of the child, which will allow you to say when the baby can be attached to the breast. The ability to start breastfeeding is determined by the newborn's ability to suck and swallow.
Breastfeeding positions, baby clothes
Keep the baby's head, shoulders and torso in a straight line and use the hand that holds the head to bring it closer to the breast. The child's arms should be separated and placed around the mother's chest, and his nose should
touch the surface of the breast. The other hand must hold the chest.
Two postures are particularly comfortable: the soccer ball hold and the lateral support. Both of them allow the mother to grasp the baby's head with one hand and support the breast with the other. A pillow under her forearm will help her relax her shoulders and back, and possibly allow her milk to flow more freely.
The first method allows you to better control the position of the baby's head and check whether he takes the breast correctly. It is worth trying this position if the mother is worried that the baby is very small and the breasts are large, and also if the mother is experiencing abdominal pain after a caesarean section.
Football Hold
* Place a pillow to your side to support your elbow and baby's lower body. Place the baby's head in the palm of your hand.
* Raise the baby's head to chest level.
* Support the base of the baby's head with your thumb and forefinger.
* If the baby does not seem to like it, put a soft blanket between your arm and the baby's head as a pad.
Lateral Holding Position
Lateral Holding Position is another comfortable feeding position for the baby, while the mother controls the position of the baby's head and can better see how he takes the breast.
* Hold the baby's head on your forearm perpendicular to your body, opposite the breast from which he will suckle.
* The baby will be in the same position as normal motion sickness, but you can use your other hand to hold him.
* The baby should be at chest level with the whole body pressed against the mother.
The baby does not need to be swaddled tightly - just a diaper and cap is sufficient. An undershirt is not needed because the skin of the mother's breasts is warm, the mother's skin temperature can be around 37 ° C, as heat is generated during milk production. To protect the child from heat loss, you can cover him with a blanket from above.
How to know if your baby is getting enough breast milk
Milk intake can be determined using a procedure called weighing. The baby is weighed on a very accurate scale just before and after breastfeeding. The difference between a baby's weight before and after a feed (measured in grams) is the amount of milk (measured in cubic centimeters, or milliliters) that the baby gets during a feed. For example, if the difference between the weight of the child before and after feeding is 30 grams, this indicates that he sucked 30 ml of milk from the breast. However, it should be remembered that when weighing before and after breastfeeding, the baby must be in the same clothes, which will accurately measure the amount of milk consumed. Changing the diaper between two weighings will result in inaccurate measurements.
However, it should be remembered that when weighing before and after breastfeeding, the baby must be in the same clothes, which will accurately measure the amount of milk consumed. Changing the diaper between two weighings will result in inaccurate measurements.
How to make sure your baby is breastfeeding correctly
The way your baby latch is one of the most important factors in determining the success of breastfeeding. For proper latch-on, the baby's mouth should be positioned over the milk sinuses, which are about 2.5 to 4 cm deeper than the nipple. With this arrangement, the baby will receive more milk, this will help to avoid pain in the mother during feeding and prevent the formation of nipple cracks.
Gently lift and support the chest so that the thumb is on top of the chest and the other fingers are below, well below the areola. This position is called "C-capture".
Lightly tap the baby's bottom lip with the nipple down a few times.